Live Donor Kidney Transplant in 2020 Linda J


- Slides: 53
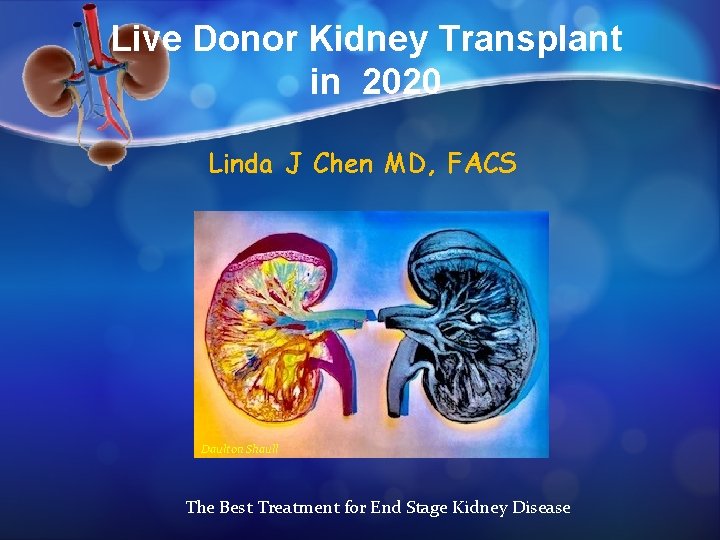
Live Donor Kidney Transplant in 2020 Linda J Chen MD, FACS Daulton Shaull The Best Treatment for End Stage Kidney Disease
Kidney Transplant vs Dialysis • Significantly lower mortality • Relative magnitude of benefit increase over time (p, 0. 001) • Risk of CV events is significantly reduced • Quality of life is significantly & substantially better • Increase in age and co-morbidities of contemporary transplant patients • Relative benefits of transplant are increasing over time Tonelli. AJT 2011; 11: 2093 -2109
Kidney Transplant vs Dialysis Cheaper “A Study of quality of life and cost utility of kidney transplantation” Conclusions: Over the two years, transplantation was both more effective and less costly than dialysis. This was true for all subgroups of patients examined, including patients older than 60 and diabetics. Muirhead. Kidney Intl 1996; 50: 235 -242

MTI Lap Donor Protocol Donor Length of Stay 100% Hand- assisted Laparoscopic Unique pain control protocols (gabapentin, IV Tylenol, 0. 5 dose IV NSAID’s x 24 hr , PCA first night, then Tramadol or Percosett) Clear liquids and coffee x 24 hrs, advance diet prn LOS =2 days (set expectations for discharge) Lap donor Open donor
Modified Technique for Cosmesis
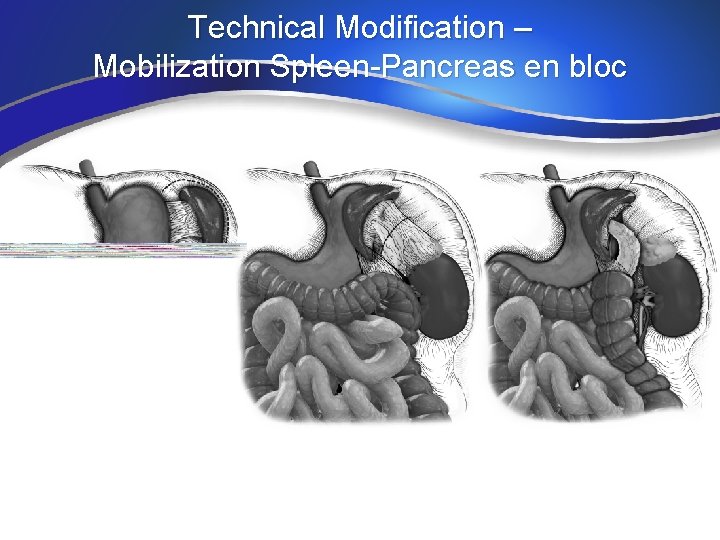
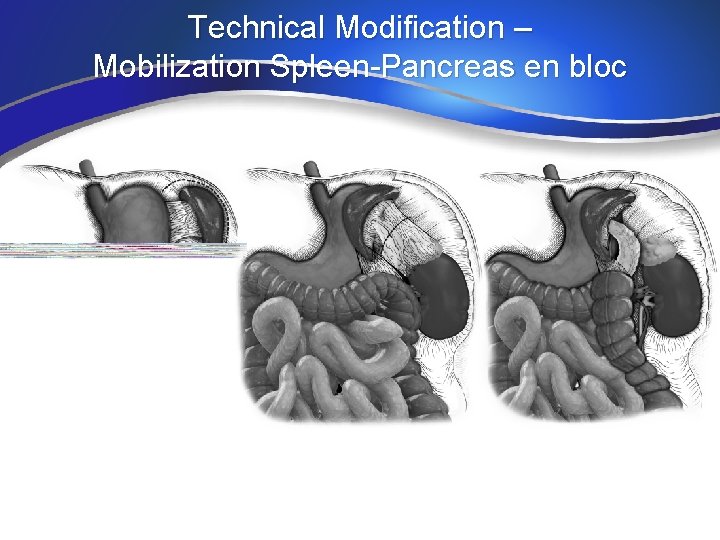
Technical Modification – Mobilization Spleen-Pancreas en bloc
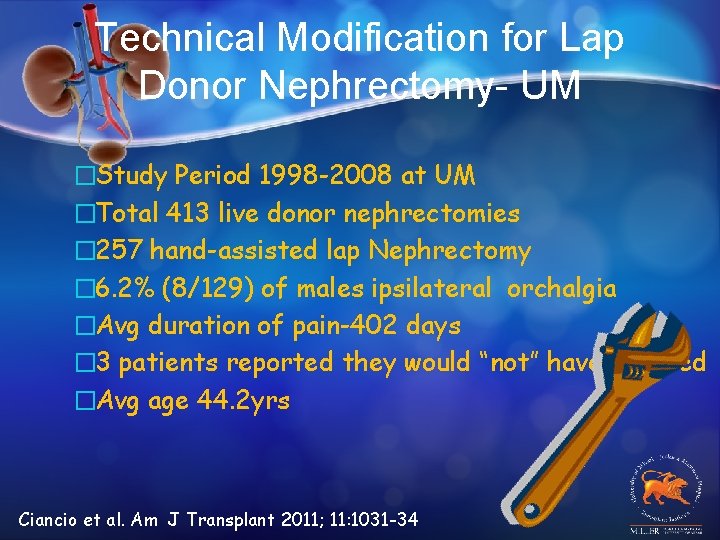
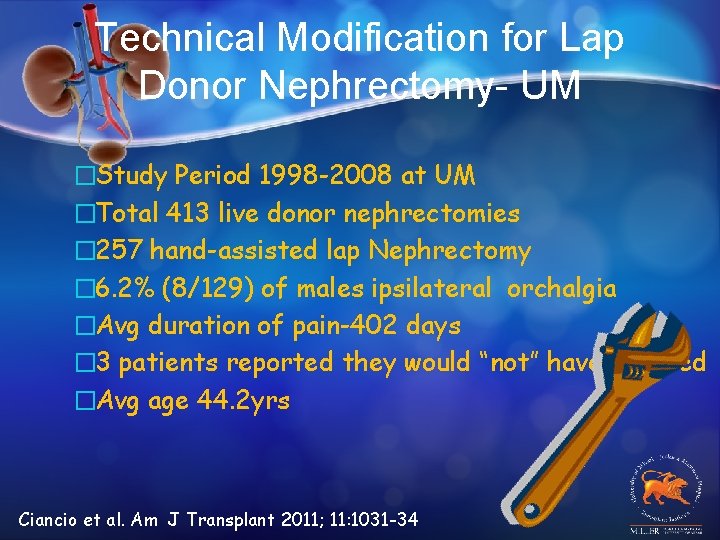
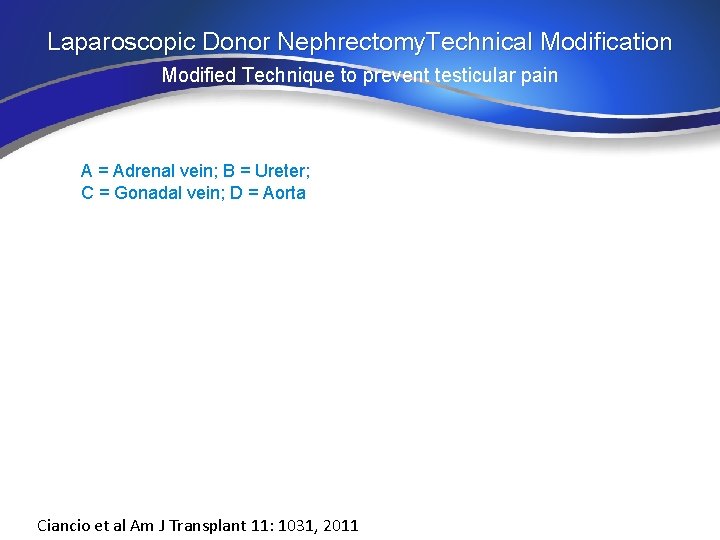
Technical Modification for Lap Donor Nephrectomy- UM �Study Period 1998 -2008 at UM �Total 413 live donor nephrectomies � 257 hand-assisted lap Nephrectomy � 6. 2% (8/129) of males ipsilateral orchalgia �Avg duration of pain-402 days � 3 patients reported they would “not” have donated �Avg age 44. 2 yrs Ciancio et al. Am J Transplant 2011; 11: 1031 -34
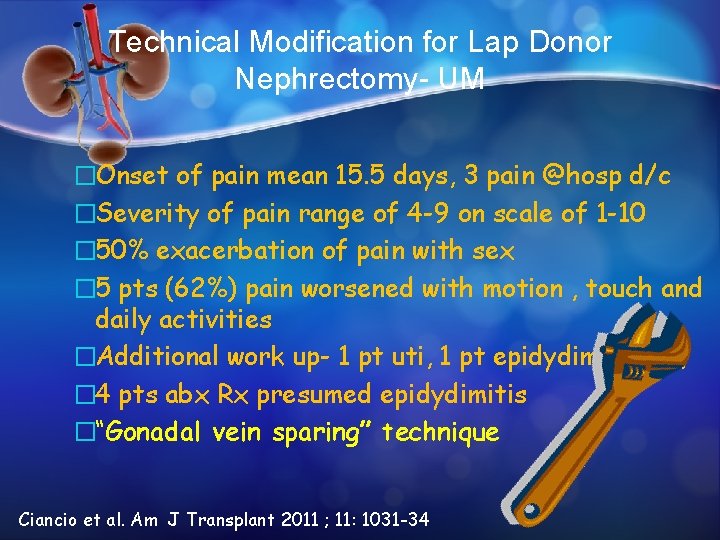
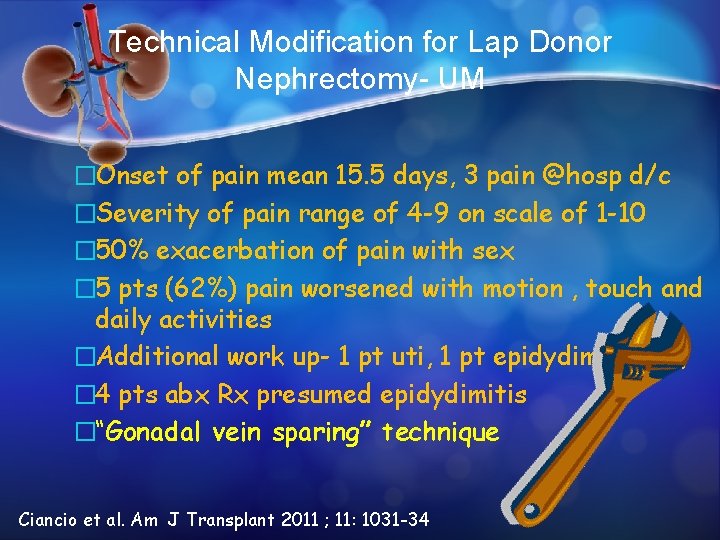
Technical Modification for Lap Donor Nephrectomy- UM �Onset of pain mean 15. 5 days, 3 pain @hosp d/c �Severity of pain range of 4 -9 on scale of 1 -10 � 50% exacerbation of pain with sex � 5 pts (62%) pain worsened with motion , touch and daily activities �Additional work up- 1 pt uti, 1 pt epidydimal cyst, � 4 pts abx Rx presumed epidydimitis �“Gonadal vein sparing” technique Ciancio et al. Am J Transplant 2011 ; 11: 1031 -34
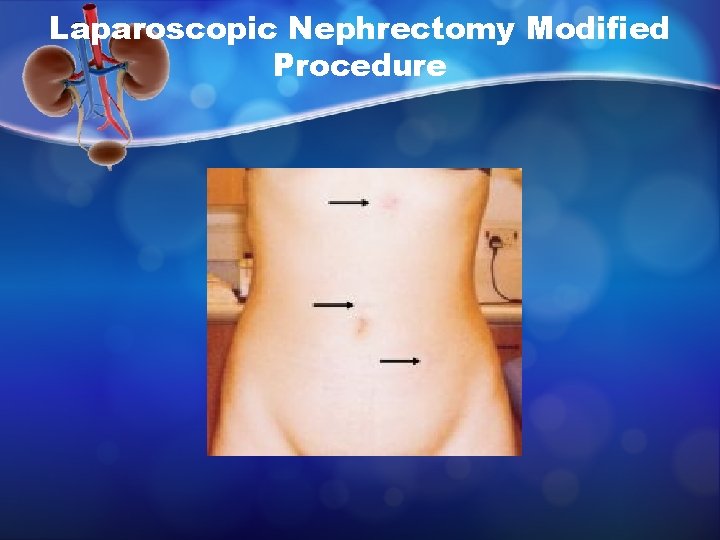
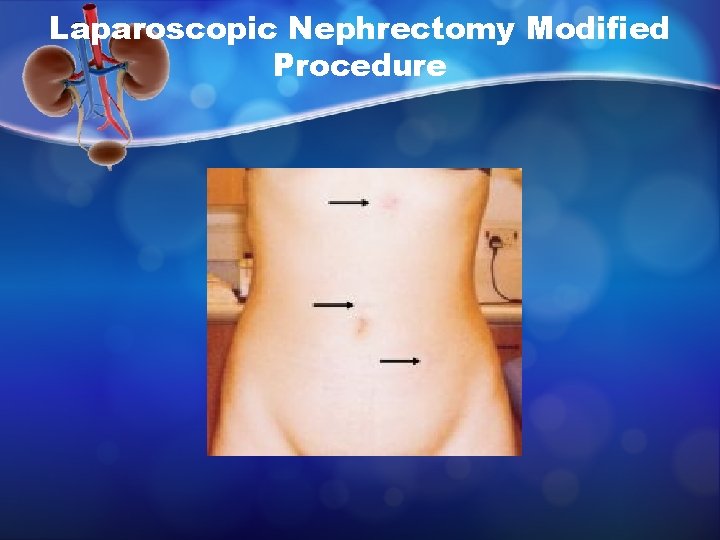
Laparoscopic Nephrectomy Modified Procedure
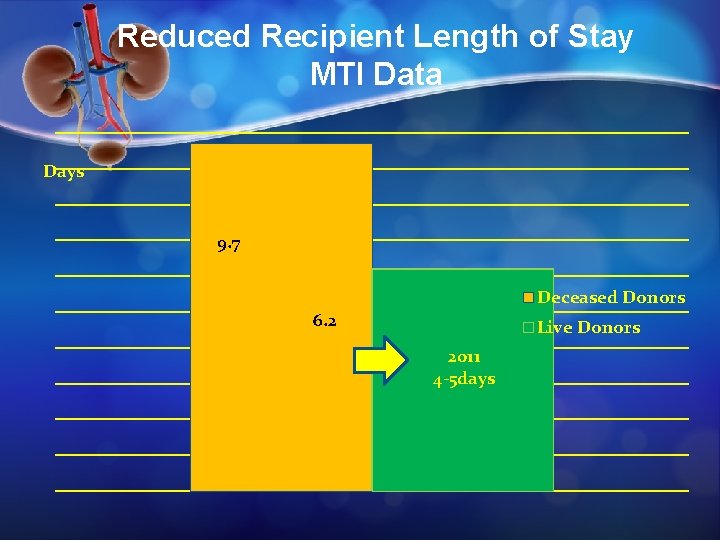
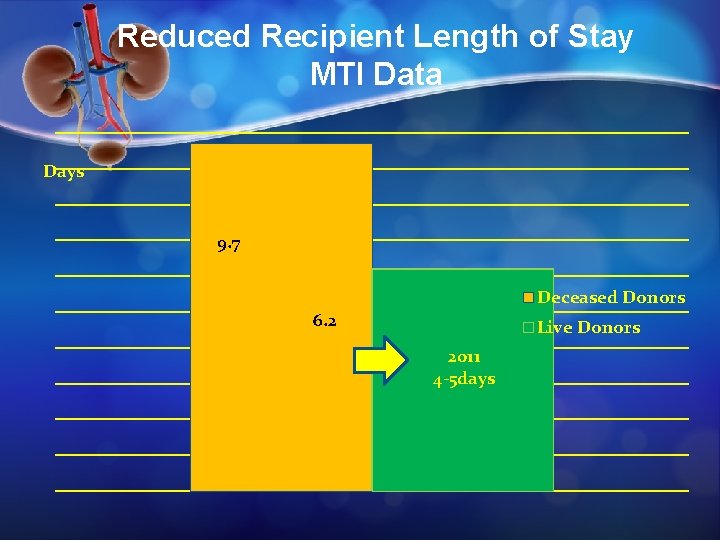
Reduced Recipient Length of Stay MTI Data Days 9. 7 Deceased Donors 6. 2 Live Donors 2011 4 -5 days
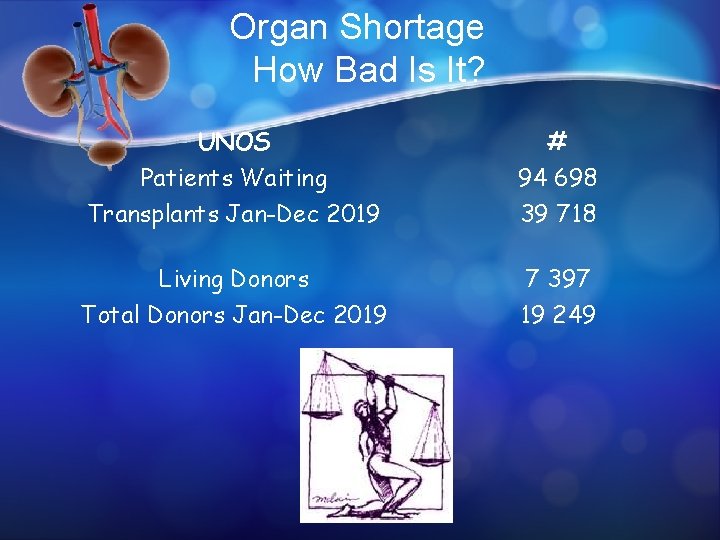
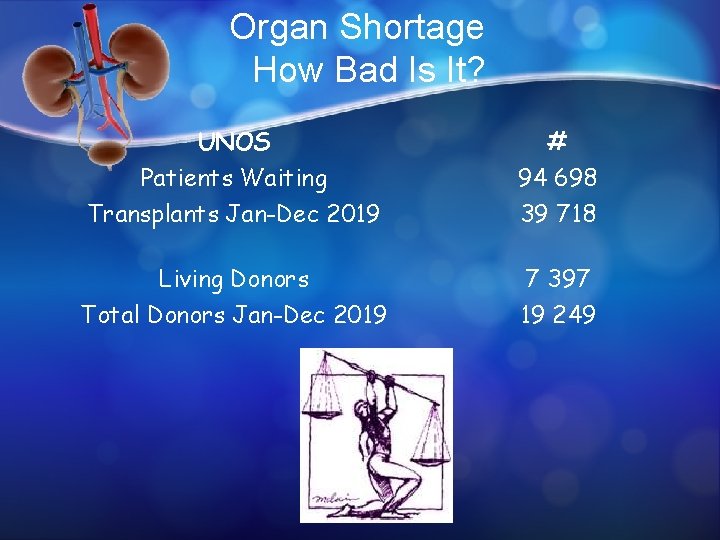
Organ Shortage How Bad Is It? UNOS Patients Waiting Transplants Jan-Dec 2019 # 94 698 39 718 Living Donors Total Donors Jan-Dec 2019 7 397 19 249
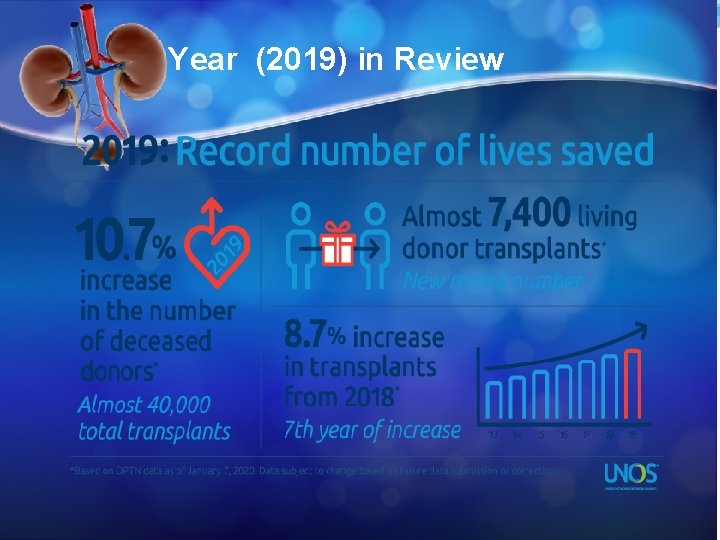
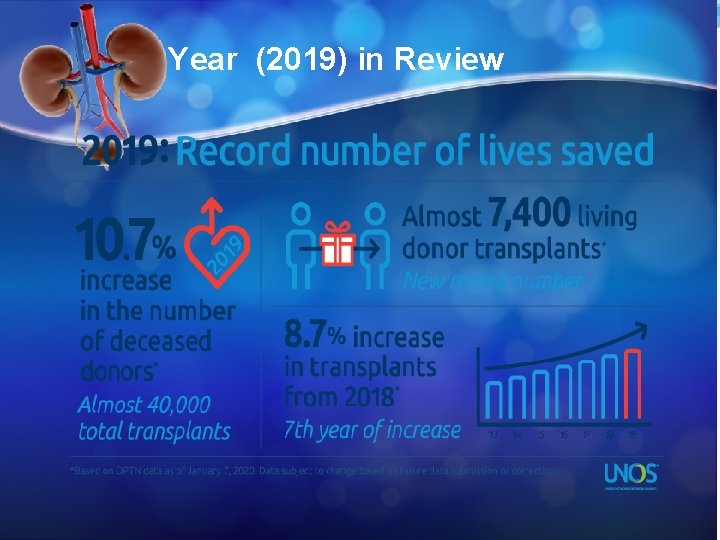
Year (2019) in Review
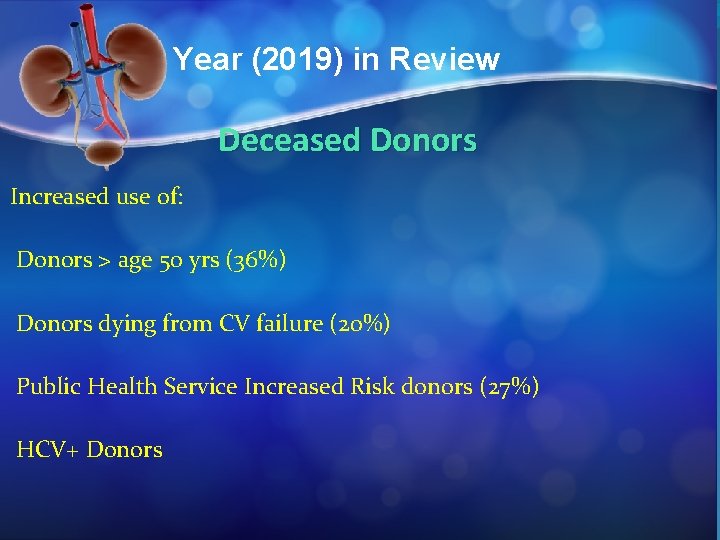
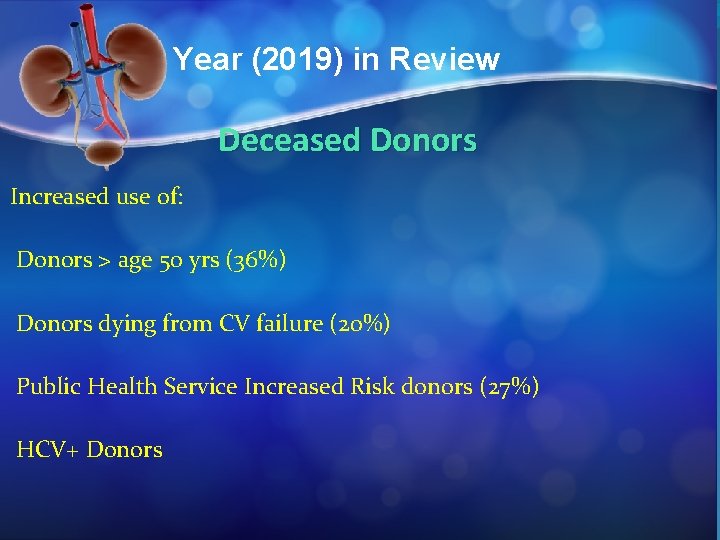
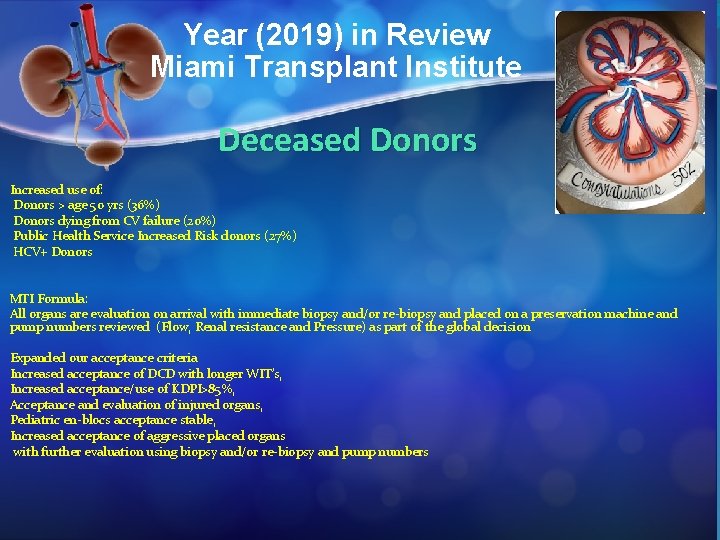
Year (2019) in Review Deceased Donors Increased use of: Donors > age 50 yrs (36%) Donors dying from CV failure (20%) Public Health Service Increased Risk donors (27%) HCV+ Donors
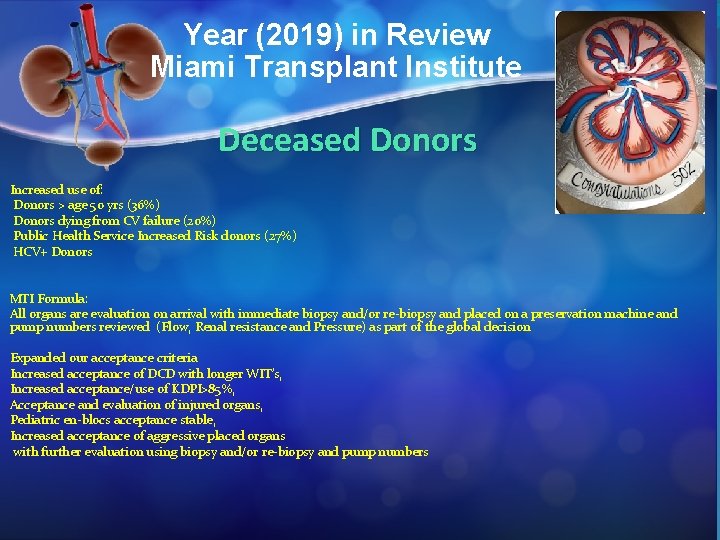
Year (2019) in Review Miami Transplant Institute Deceased Donors Increased use of: Donors > age 50 yrs (36%) Donors dying from CV failure (20%) Public Health Service Increased Risk donors (27%) HCV+ Donors MTI Formula: All organs are evaluation on arrival with immediate biopsy and/or re-biopsy and placed on a preservation machine and pump numbers reviewed (Flow, Renal resistance and Pressure) as part of the global decision Expanded our acceptance criteria Increased acceptance of DCD with longer WIT’s, Increased acceptance/use of KDPI>85%, Acceptance and evaluation of injured organs, Pediatric en-blocs acceptance stable, Increased acceptance of aggressive placed organs with further evaluation using biopsy and/or re-biopsy and pump numbers
Year (2019) in Review Living Donors Crowdsourcing living donors Using online portals to streamline the donor identification and evaluation process Dedicating resources to the kidney paired donation
Year in Review Living Donors Crowdsourcing living donors: Definition: “the practice of obtaining information or input into a task/project by enlisting the service of a large number on people, either paid or unpaid, typically through the internet” My understanding is: “it takes a village” via crowdmarket ie. social media, on line platforms, educational sites, etc. 1. 2. 3. Expeditious Efficient use of limited resources (divides the labor) Share ideas /expertise For 2017 there were 224. 3 million smart phone users in the USA (population 325. 7 million) = 79% In Jamaica as of 2015 : 3. 1 million phone subscribers (population 2. 8 million) = 90%
Year 2019 in Review Living Donors Using online portals to streamline the donor identification and evaluation process (relieves the burden of the coordinators) BREEZE TM Interactive Web-Based Patient Portal for the Evaluation (health history) of Potential Kidney Transplant Donors Pros: Confidential Avoids coercion Cons: IT skills (? Excludes some potential donors)
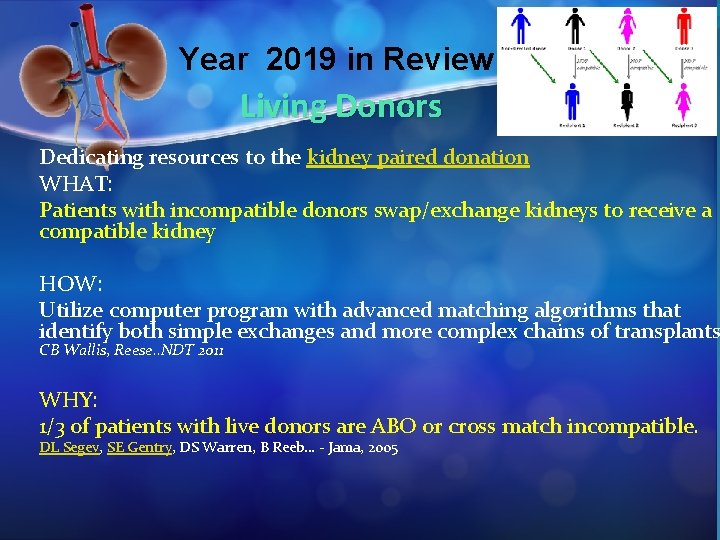
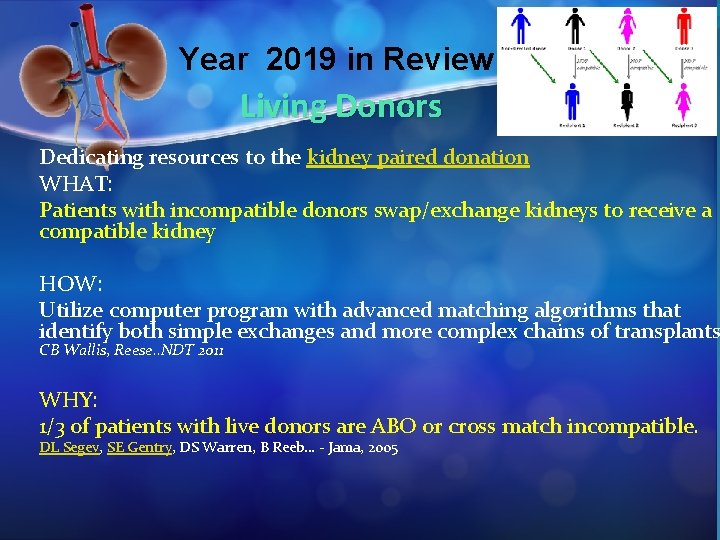
Year 2019 in Review Living Donors Dedicating resources to the kidney paired donation WHAT: Patients with incompatible donors swap/exchange kidneys to receive a compatible kidney HOW: Utilize computer program with advanced matching algorithms that identify both simple exchanges and more complex chains of transplants CB Wallis, Reese. . NDT 2011 WHY: 1/3 of patients with live donors are ABO or cross match incompatible. DL Segev, SE Gentry, DS Warren, B Reeb… - Jama, 2005
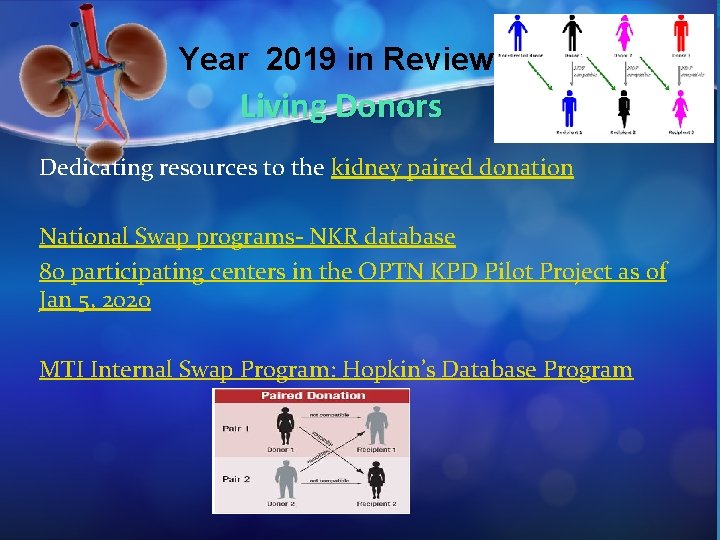
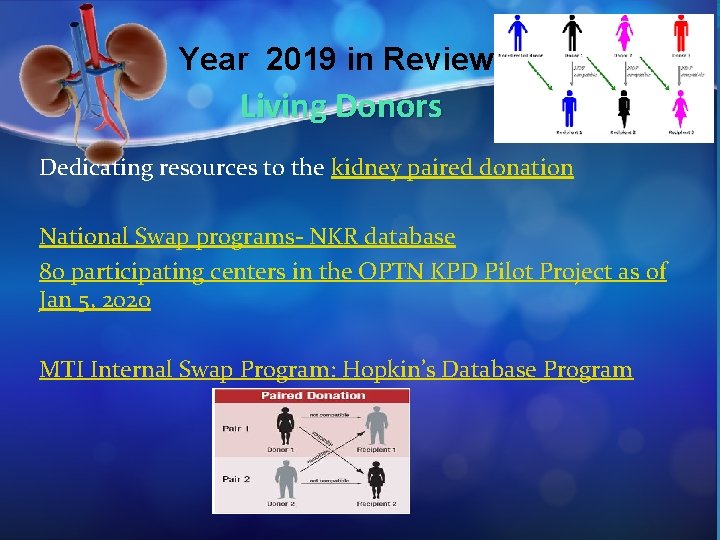
Year 2019 in Review Living Donors Dedicating resources to the kidney paired donation National Swap programs- NKR database 80 participating centers in the OPTN KPD Pilot Project as of Jan 5, 2020 MTI Internal Swap Program: Hopkin’s Database Program
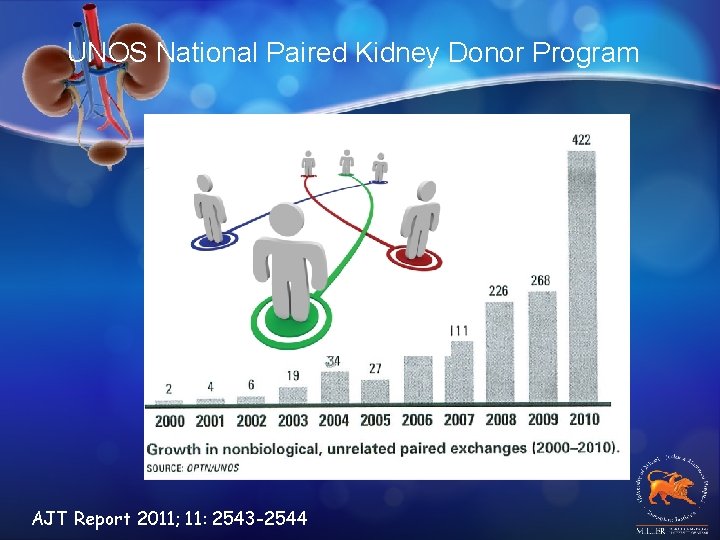
Internal Paired Kidney Donation • Large database of incompatible pairs • (Critical mass is 100 pairs) • A sophisticated immunology lab • Close coordination b/t clinical team & lab • Sophisticated software program to perform • the matching • Desensitization of some patients • Use of compatible pairs AJT Report 2011; 11: 2543 -2544
Paired Kidney Donation PROS • Bigger donor pool • More heterogeneous HLA typing CONS • Lengthy evaluation time • Non standardized/incomplete donor work up • Increased center expenses • Center specific shipping/labeling • Donors renege Bingaman AW. New Engl J Med 2010; 363: 1091 -1092
MTI Approach to Living Donation �Emphasis on prioritization by transplant centers (educating patients that LD is the standard and is the best choice) �Barriers: Language, Cultural, Racial (70% Hispanic + 10% peoples of African descent)
Year in Review Living Donors Directed Donation (donating to family member/friend) Non-directed Donation (donation without naming someone) Living non-directed (LND) donors, also known as altruistic, good Samaritan, anonymous, or benevolent community donors-rapidly growing source of organ donors
Live Kidney Donor ? Undergoes a major surgical procedure with absolutely no direct medical benefit How safe is it to donate? Medical , psychosocial, surgical Who Can Be a Living Donor? Inclusion vs exclusion criteria: HTN, obesity, stones, malignancies, Unrecognized kidney dz-proteinuria, Hematuria, Infections, insurance
Strategies to Increase Living Donors �Broaden inclusion criteria: HTN, obesity (up to BMI 35), age (>65 y), diabetes, malignancies (appropriate cancer free survival selectively) �Non-directed Donors; internet donors �Financial Aid program for donors �Paired Kidney Donation (swap programs) �Desensitization protocols �Improved surgical techniques-cosmesis �Educational activities/outreach
On-Line Solicitation of Organs • Ethical dilemmas of altruistic kidney donation • Altruism should be the guiding motivation for all donations “The Beauty Contest” Matching. Donors. com Neidich EM Am J Transplant 2011
Food for thought: “Use of Expanded Living Donor Pool Donors >65 yrs Donors with Cancer Donors with Renal Cell Cancer Donors with Kidney Stones Donors with communicable diseases HIV+ donors- not done HIV+ to HIV+ (? ) (Hope Study) HCV+ to HCV-
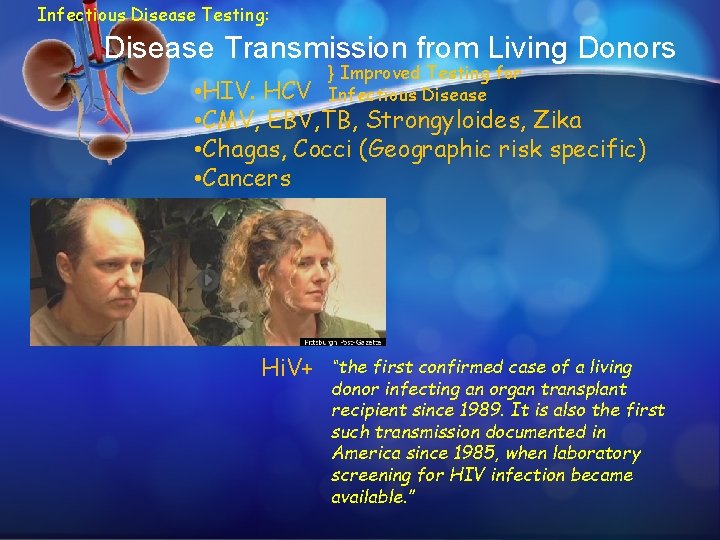
Infectious Disease Testing: Disease Transmission from Living Donors } Improved Testing for Infectious Disease • HIV. HCV • CMV, EBV, TB, Strongyloides, Zika • Chagas, Cocci (Geographic risk specific) • Cancers Hi. V+ “the first confirmed case of a living donor infecting an organ transplant recipient since 1989. It is also the first such transmission documented in America since 1985, when laboratory screening for HIV infection became available. ”
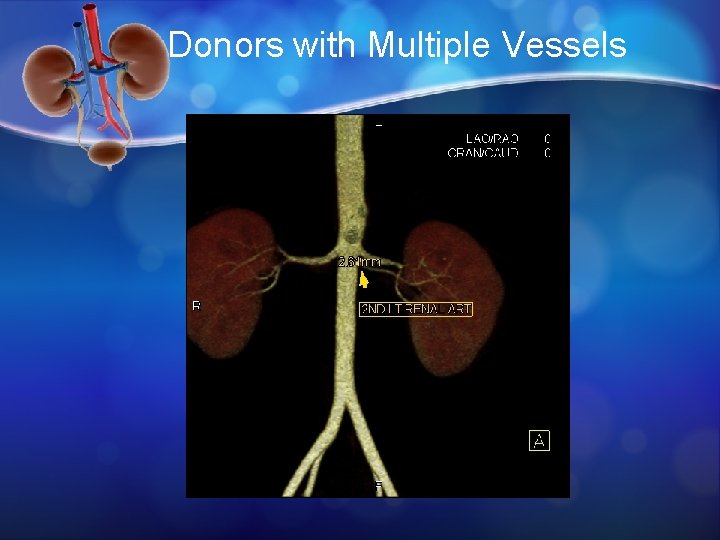
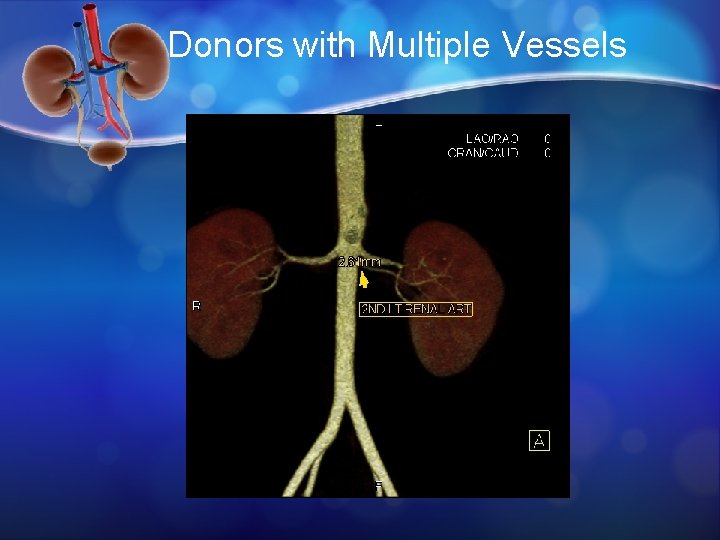
Donors with Multiple Vessels
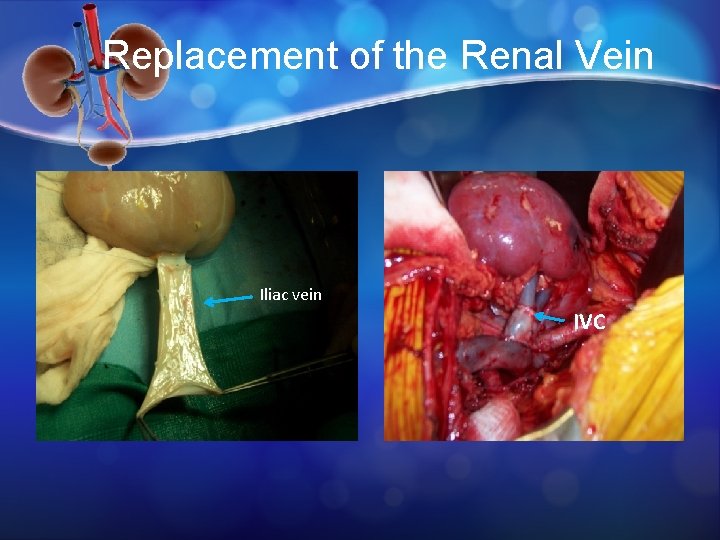
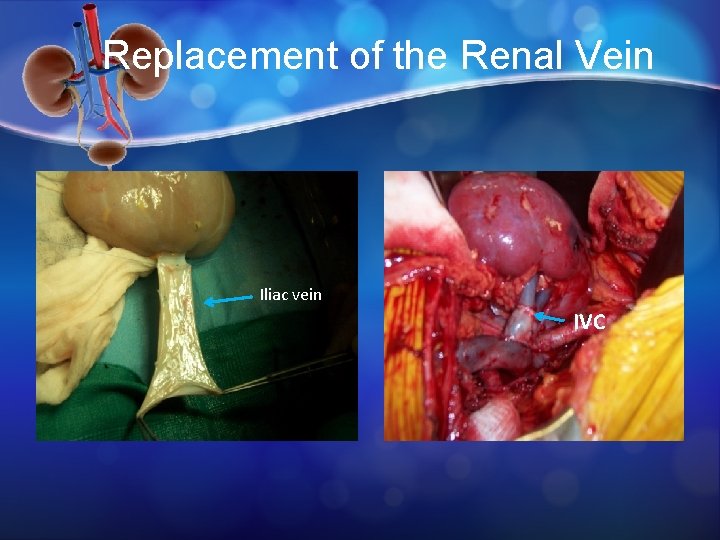
Replacement of the Renal Vein Iliac vein IVC
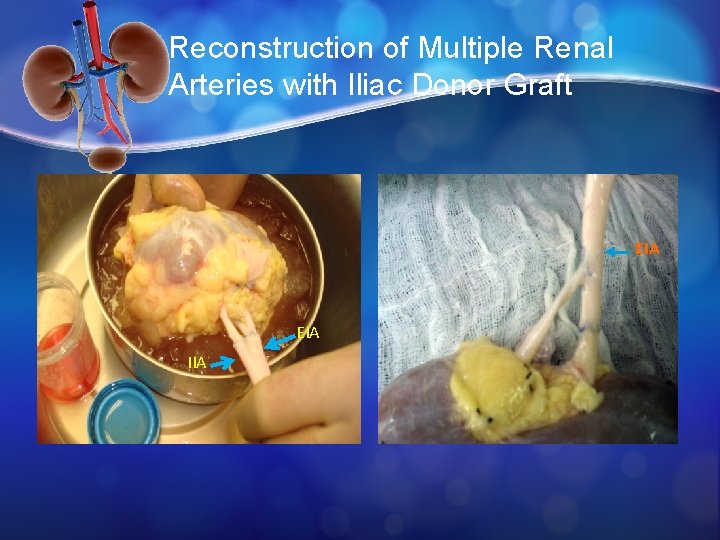
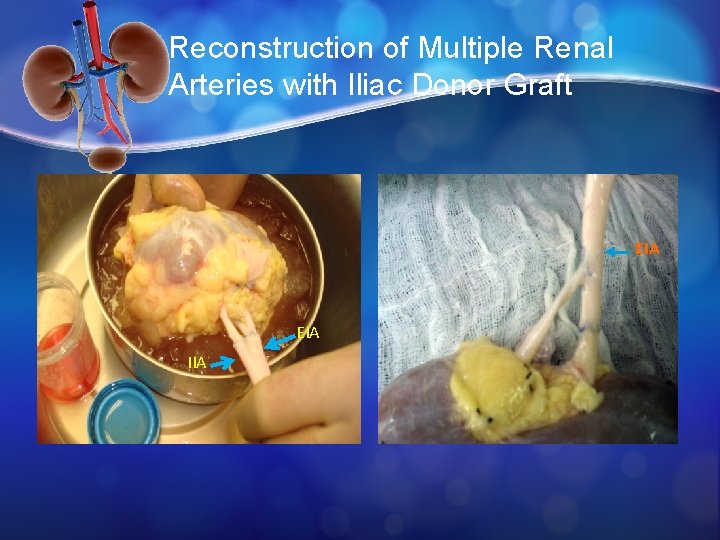
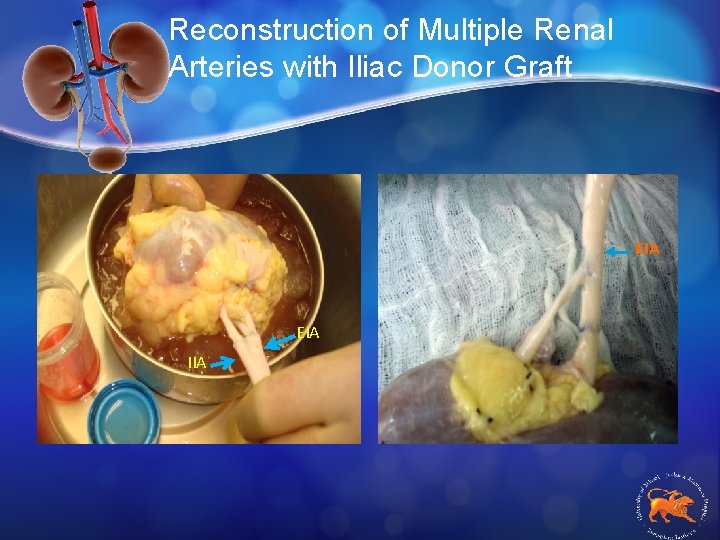
Reconstruction of Multiple Renal Arteries with Iliac Donor Graft EIA IIA
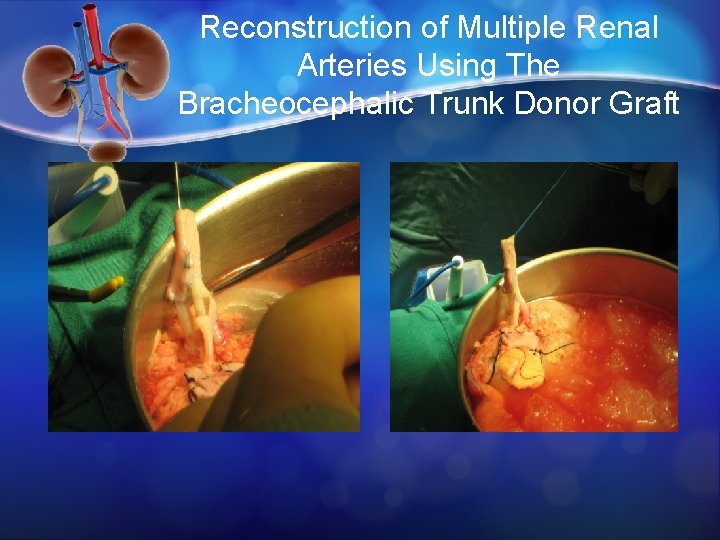
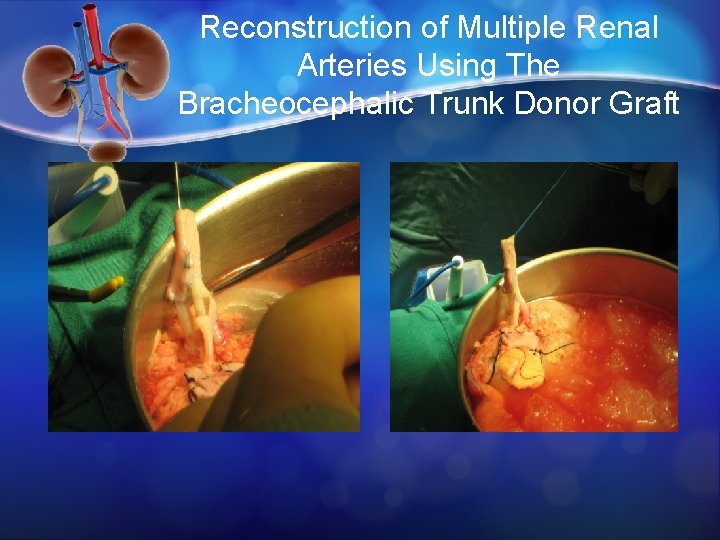
Reconstruction of Multiple Renal Arteries Using The Bracheocephalic Trunk Donor Graft
Program Growth…. �Expanded living donor pool as we learned � 1. Increased technical skills of the donor and recipient surgeons to handle resection of small renal tumors, multiple vessels, obese patients, patients with multiple arteries, comfort to do Jehovas witnesses or hypercoagulable patients
Program Growth…. �Society: Critical organ shortage �Institution: : Volume, Cost, LOS, Research trials, PR & marketing opportunities �Patient: Superior long-term outcome, preemptive transplantation, minimal cold ischemic times, surgery can be scheduled �Advanced technology for Donor �Donor: laparoscopic procedure, decreased pain/infection, return to work 7 -10 days �Better quality of life for recipient - decreased rejection, less immune. Rx, decrease side effects/secondary issues
Thank You
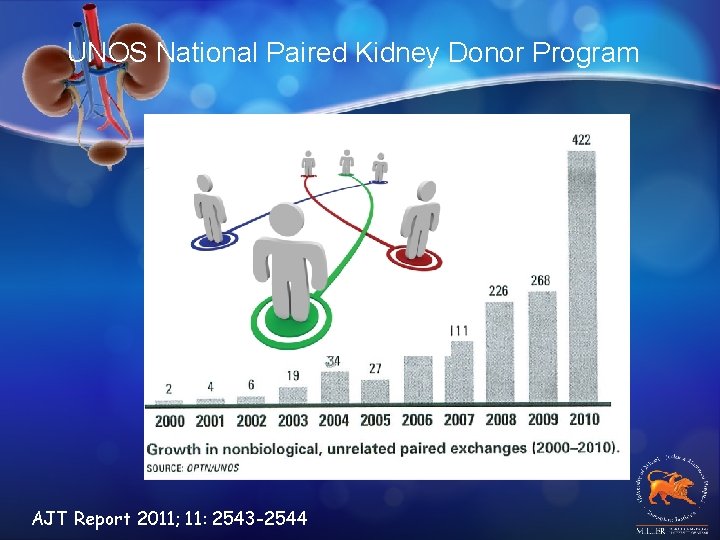
UNOS National Paired Kidney Donor Program AJT Report 2011; 11: 2543 -2544
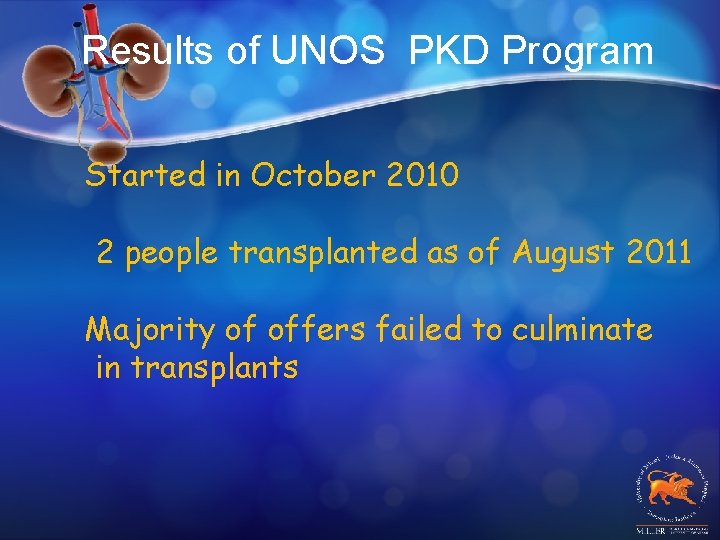
Results of UNOS PKD Program Started in October 2010 2 people transplanted as of August 2011 Majority of offers failed to culminate in transplants
KPD Programs Chains- open and closed NEAD chains-non-simultaneous extended chains altruistic donor DPD-Domino Paired donation chains
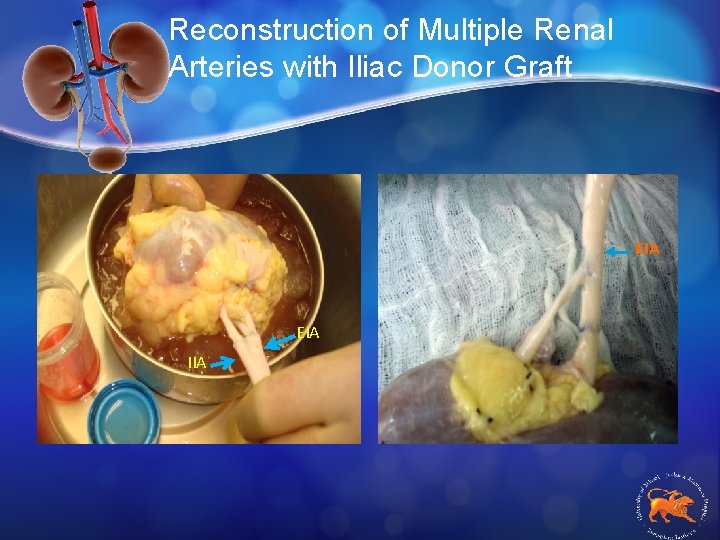
Reconstruction of Multiple Renal Arteries with Iliac Donor Graft EIA IIA
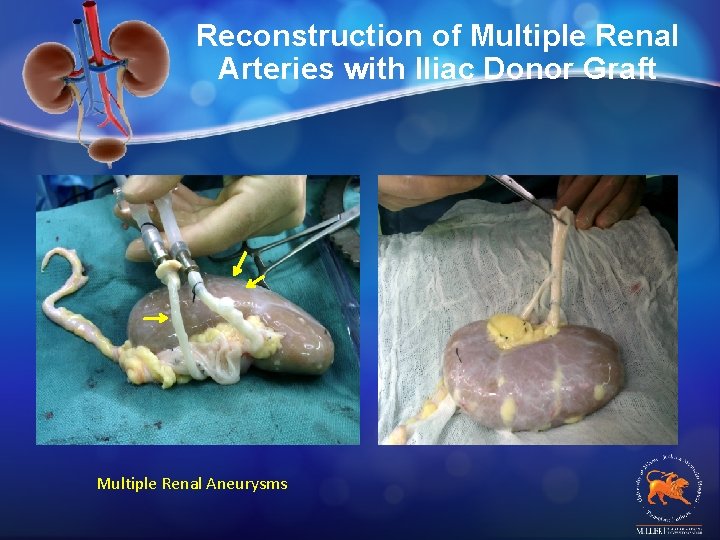
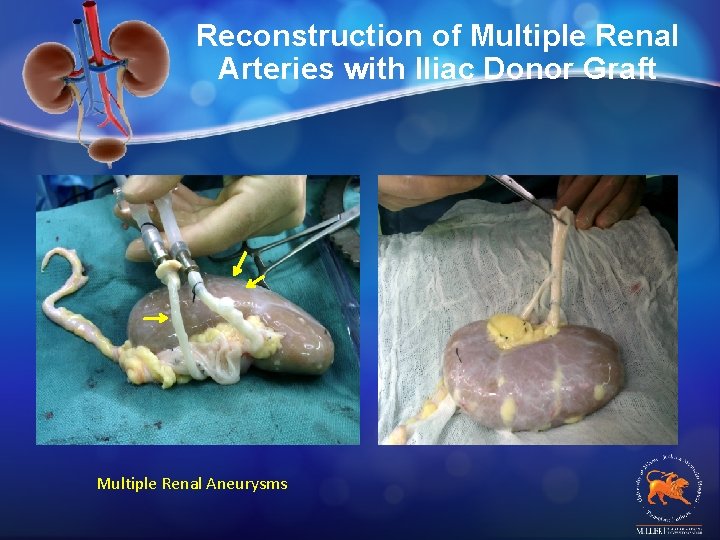
Reconstruction of Multiple Renal Arteries with Iliac Donor Graft Multiple Renal Aneurysms
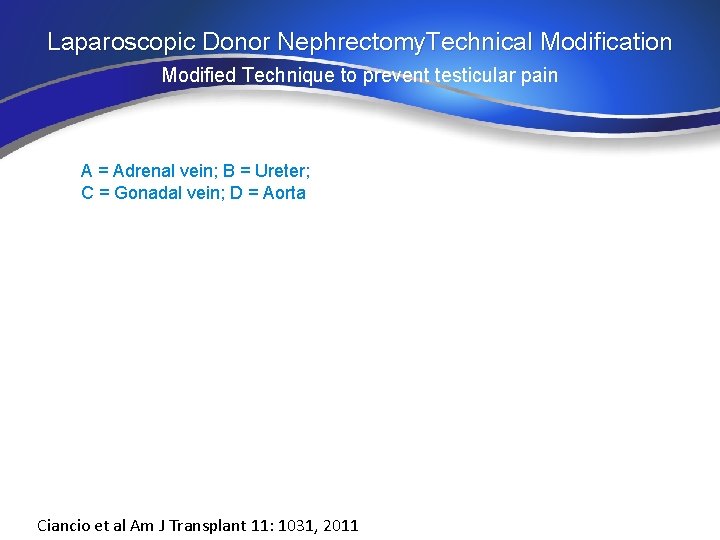
Laparoscopic Donor Nephrectomy. Technical Modification Modified Technique to prevent testicular pain A = Adrenal vein; B = Ureter; C = Gonadal vein; D = Aorta Ciancio et al Am J Transplant 11: 1031, 2011
Transplant Centers have employed innovative options to increase the size of the donor pool & optimize organ donation
Solving the Organ Shortage Crisis: Expanding the Living Donor Pool • Broaden Selection: v Use of donors with small malignancies aka v Transplantation of “restored kidneys” • Use of Kidneys with small renal tumors v Use of donors with small malignancies aka v Japanese data
Small Kidney Tumors
Backtable Resection: Partial Nephrectomy
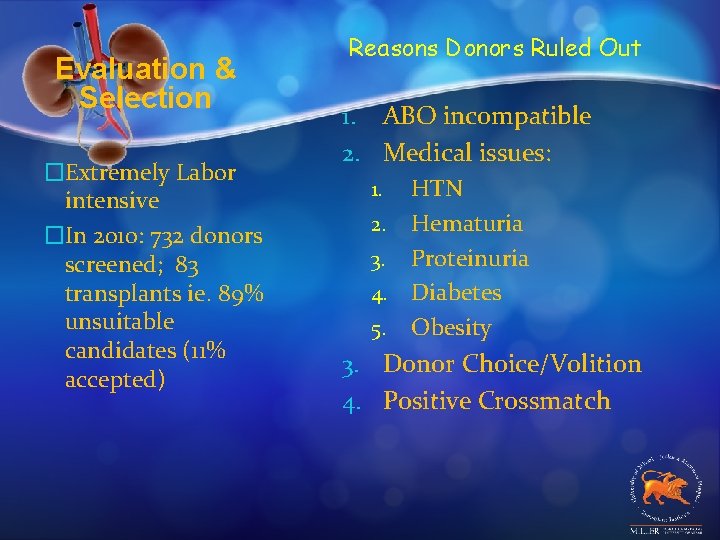
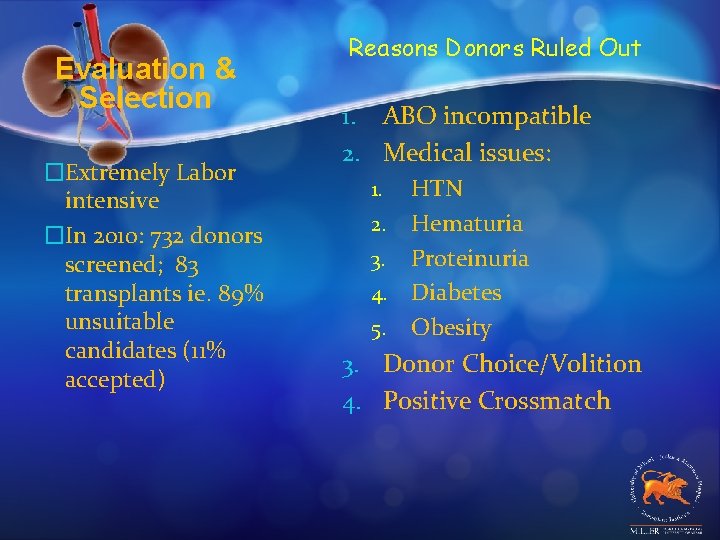
Evaluation & Selection �Extremely Labor intensive �In 2010: 732 donors screened; 83 transplants ie. 89% unsuitable candidates (11% accepted) Reasons Donors Ruled Out 1. ABO incompatible 2. Medical issues: 1. HTN 2. Hematuria 3. Proteinuria 4. Diabetes 5. Obesity 3. Donor Choice/Volition 4. Positive Crossmatch
Original Technique
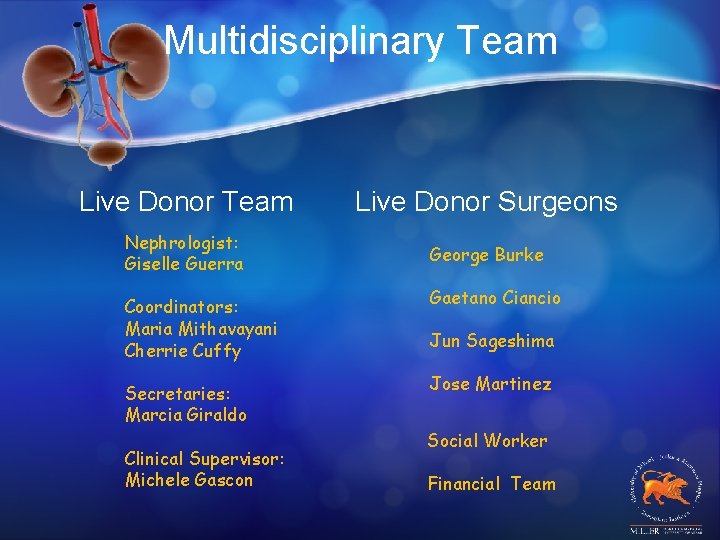
Multidisciplinary Team Live Donor Surgeons Nephrologist: Giselle Guerra George Burke Coordinators: Maria Mithavayani Cherrie Cuffy Secretaries: Marcia Giraldo Clinical Supervisor: Michele Gascon Gaetano Ciancio Jun Sageshima Jose Martinez Social Worker Financial Team
Laparoscopic vs Open Donor Nephrectomy Laparoscopic technique is procedure of choice encompassing b/t 50 -100% all living donor nephrectomy done at tertiary Centers UM In 2010 83% living donors procured by laparosopy vs 50% 2000 Shirodkar SP. Arch Esp Urol 2010; 63: 163 -170
Live Donor Anatomy Surgical Technique
Preoperative Imaging

CT Urogram
Incision of Open Donor Nephrectomy Incision of Hand-Assisted Laparoscopic Live Donor Nephrectomy