Little Tykes Terror Managing Pediatric Emergence Delirium Leianne

- Slides: 63
Little Tykes Terror: Managing Pediatric Emergence Delirium Leianne O. Knoll Krajewski, CRNA, DNP
Pediatric Emergence Delirium
Pediatric Emergence Delirium
Pediatric Emergence Delirium
Pediatric Emergence Delirium
Outline Definition Incidence Risk Factors Etiology Prevention Identification Management
Emergence Delirium: Definition Delirium is a complex psychiatric syndrome that includes perceptual disturbances, hallucinations and psychomotor agitation. “A disturbance in a child’s awareness of and attention to his or her environment with disorientation and perceptual alterations including hypersensitivity to stimuli and hyperactive motor behavior in the immediate post-anesthesia period. ” American Psychiatric Association (2000) Sikich and Lerman, Anesthesiology (2004)
Definition? Clear as MUD The term “delirium” is often replaced with the descriptive terms “agitation” or “excitation” as it is not feasible to fully evaluate a young child’s psycho- logical state during emergence EA (Emergence agitation) is a state of mild restlessness and mental distress that, unlike delirium, does not always suggest a significant change in behavior Choen, et al (2001) Galford (1992)
More Mud…. Agitation can indicate any number of sources, including pain, physiological compromise or anxiety. Delirium may be confused with agitation, but it may also be a cause of agitation. Voepel-Lewis, et al (2004)
Emergence Delirium Usually within the first 30 minutes of recovery from general anesthesia Brief (10 -15 minutes) Self-limited and resolves spontaneously However, agitation and regressive behavior that lasted up to 2 days were also described in the literature.
How often does this happen? Incidence The incidence of EA/ED largely depends on definition, age, anesthetic technique, surgical procedure and application of adjunct medication. First described by Eckenhoff, et al in 1961 Pediatric: Generally ranged 10 -50% but may be as high as 80% Adult: 3 -4% Vlaikovic, et al (2007) Lepouse, et al (2006)
Does it matter? Risk of harming surgical repair Risk of harming self Risk of harming caregivers (nurse, parent) Risk of pulling out IV’s, drains, tubes, catheters, dressings IT’S STRESSFUL, NOT IDEAL AND IT MATTERS! WE CAN DO BETTER!
What’s the big deal? More nursing resources required May require physical or pharmacological restraint (with potential side effects) May prolong recovery room stay May delay hospital discharge Parents/nurses/providers less satisfied with quality of surgical/anesthetic experience

RISK FACTORS Patient related Surgery related Anesthesia related
Risk Factors: Patient related Age Anxiety Preoperative Postoperative Patient Parent Temperament
Risk Factors: Age Generally, younger children are more likely to show altered behavior upon recovery from anesthesia More common in younger children (preschool vs. school age) 2 -5 year-olds thought to be most vulnerable to becoming easily confused and frightened by unfamiliar experiences/surroundings Voepel-Lewis, et al (2003) Vlaikovic, et al (2007)
Risk Factors: Patient Multiple studies show the likelihood of patient preoperative anxiety increasing the risk of postoperative emergence delirium Pre-op anxiety in children may depend primarily on their stages of development. Previous hospital experience Aono, et al (1999) Kain, et al (2004) Banchs, et al (2014)
Risk Factors: Age Infants: less likely to experience separation anxiety 1 -3 y/o: experience separation anxiety but respond positively to distraction and comforting measures 4 -5 y/o: seek explanations and desire control of their enviornment Older children 7 -12 y/o: desire more independence and want to be involved in decision making processes. Adolescents fear losing face and are concerned with their inability to cope Mc. Graw, (1994)
Risk Factors: Parent Anxiety Pre-op PARENT anxiety also increases risk of post-op emergence delirium The higher the level of maternal salivary amylase, the more severe the child’s pre-op anxiety AND the more severe the post-op emergence delirium Kain, et al (2004) Arai , et al (2008)
Risk Factors: Parent Anxiety Maternal heart variability just before surgery significantly correlated with emergence behavior of children undergoing general anesthesia Intense preoperative anxiety in children AND their parents has been associated with increased likelihood of restless recovery from anesthesia Arai, et al (2008) Aono, et al (1999) Kain, et al (2004)
Risk Factors: Temperament Children who are more emotional, impulsive, less social and less adaptable to environmental changes are at higher risk for emergence delirium It is likely that there is some substrate innate to each child that will elicit, to a larger or lesser extent, a fearful response to outside stimuli, depending on the interaction between the child and the environment Voepel-Lewis, et al (2003) Kain, et al (2004)
Risk Factors: Temperament This reactivity, which describes the “excitability, responsivity, or arousability” of the child, might be the underlying substrate from which both preoperative anxiety and ED arise. Patient related factors are an important source of variability for ED and are the most difficult to control. Kain, et al (2004) Rothbart, et al (2000)
Risk Factors: Temperament Recent evidence suggests that cultural differences including: Language Ethnicity …Contribute to changes in behavior especially behavior during the recovery period. Fortier, et al (2013)
Risk Factors: Surgery Types of Surgery Speculation that surgery involving the head leads patients into feelings of suffocation thus increased incidence of ED- Not clinically proven ENT Tonsils, adenoids, thyroid, middle ear Ophthalmology Strabismus Voepel-Lewis, et al (2003)
Etiology Pain Intrinsic characteristics of anesthesia Rapid awakening Anxiety Surgery type Psychologically immature Temperament Unfamiliar environment Genetic predisposition
Etiology (continued) Pain Most confounding variable secondary to overlapping clinical picture with ED Difficult to distinguish between pain and ED Inadequate pain relief may cause agitation especially in short procedures where peak effect of analgesics may be delayed until after wake up
Etiology (continued) Intrinsic characteristics of anesthesia Postanesthesia agitation has been described not only with sevoflurane and desflurane, but also with isoflu- rane and lesser with halothane (no longer used) Children who received sevoflurane/isoflurane for the induction/maintenance of anesthesia were twice as likely to develop EA when compared with children who had any other anesthetic regimen Children who received total intravenous anesthesia (TIVA)- no documented cases of ED Voepel-Lewis et al (2003)
Etiology (continued) Rapid awakening postulated that rapid awakening after the use of the insoluble anesthetics may initiate EA/ED by worsening a child’s underlying sense of apprehension when finding them self in an unfamiliar environment however…… Delaying emergence by a slow, stepwise decrease in the concentration of inspired sevoflurane at the end of surgery did NOT reduce the incidence of EA Picard, et al (2000) Oh, et al (2005)
Etiology (continued) Temperament/unfamiliar environment Older children and adults usually become oriented rapidly Preschool-aged children, who are less able to cope with environmental stresses, tend to become agitated and delirious Vlajkovic et al (2007)
Prevention Given that the EA/ED etiology is still unknown, a clear -cut strategy for its prevention has not been developed Many conflicting studies on preventative pharmacological measures Difficult to study considering confounding variables and inability to do randomized double blind study accurately
Prevention All aimed at decreasing preoperative anxiety. Preoperative Preparation Programs Parental Presence Induction of Anesthesia (PPIA) Sedative premedication Distraction techniques
Prevention Preoperative Preparation Programs Preoperative booklets or DVD sent to home prior to surgery Child Life Specialist or Child Educator being present during admission to educate parents and child in age appropriate manner Use of anesthesia mask Practice “blowing up the balloon” or anesthesia ventilation bag
Prevention: Preparation A novel preoperative preparation program is the ADVANCE family centered behavioral preparation program which is an acronym for Anxiety-reduction Distraction Video modeling and education Adding parents No excessive reassurance, Coaching Exposure shaping Kain, et al (2007)
Prevention: Preparation ADVANCE Program Effectiveness on pre-op anxiety and post-op was compared with PPIA alone, oral midazolam and control groups Findings: Pre-op Anxiety in the ADVANCE group significantly less than all other groups Less anxiety during induction in ADVANCE group than PPIA and control group Incidence of ED and analgesic requirement less in ADVANCE group Discharge times for children in the ADVANCE group were less Obstacle: large operational costs Kain, et al (2007)
Prevention Parental Presence Induction of Anesthesia (PPIA) Very common practice in Europe, less common in US While 58% of US anesthesia providers agreed with PPIA only 5% of cases where parents allowed in OR 84% of British anesthesia providers allowed PPIA in more than 75% of cases Their belief that PPIA decreased children's anxiety, increased their cooperation and benefited both the parent and anesthesia provider Bowie (1993) Johnson (2012)
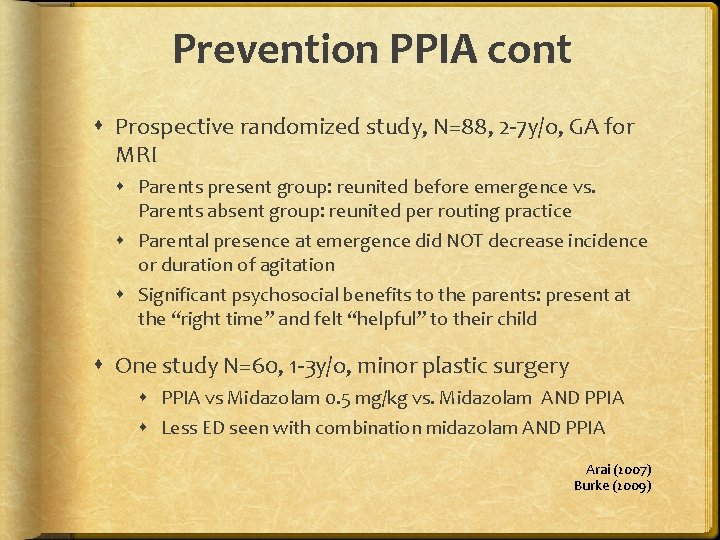
Prevention PPIA cont Prospective randomized study, N=88, 2 -7 y/o, GA for MRI Parents present group: reunited before emergence vs. Parents absent group: reunited per routing practice Parental presence at emergence did NOT decrease incidence or duration of agitation Significant psychosocial benefits to the parents: present at the “right time” and felt “helpful” to their child One study N=60, 1 -3 y/o, minor plastic surgery PPIA vs Midazolam 0. 5 mg/kg vs. Midazolam AND PPIA Less ED seen with combination midazolam AND PPIA Arai (2007) Burke (2009)
If I can’t prevent, then what? Diagnose or Identify Assessment tools Reliability and validity of tools Manage Pharmacological Environmental
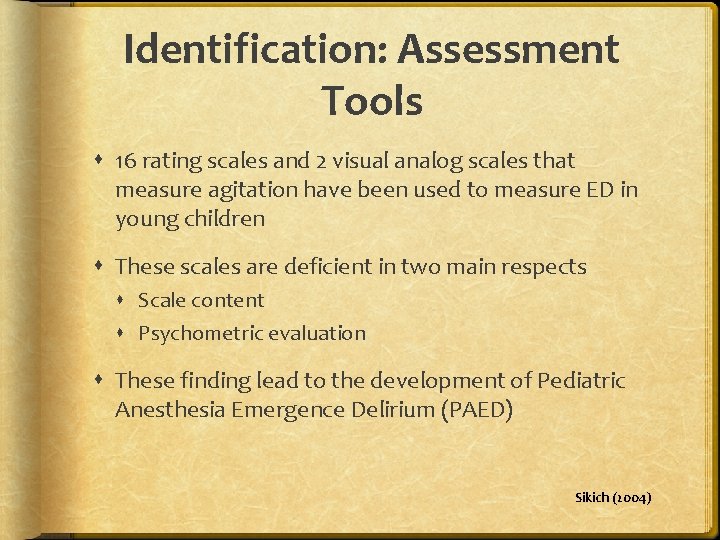
Identification: Assessment Tools 16 rating scales and 2 visual analog scales that measure agitation have been used to measure ED in young children These scales are deficient in two main respects Scale content Psychometric evaluation These finding lead to the development of Pediatric Anesthesia Emergence Delirium (PAED) Sikich (2004)
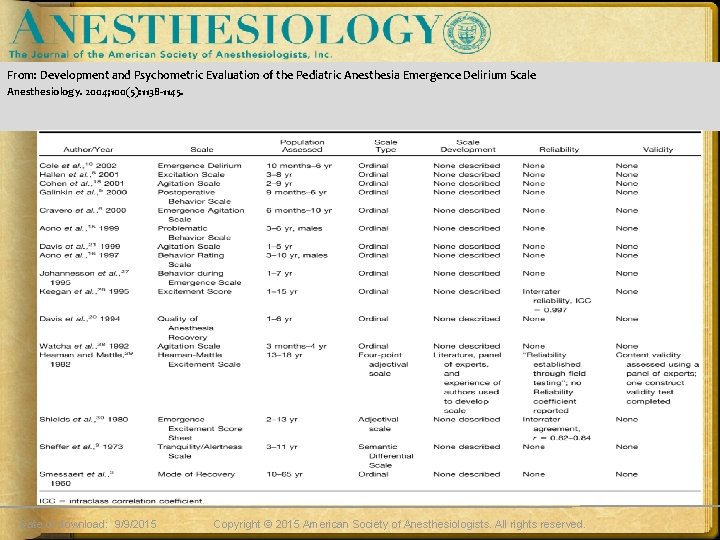
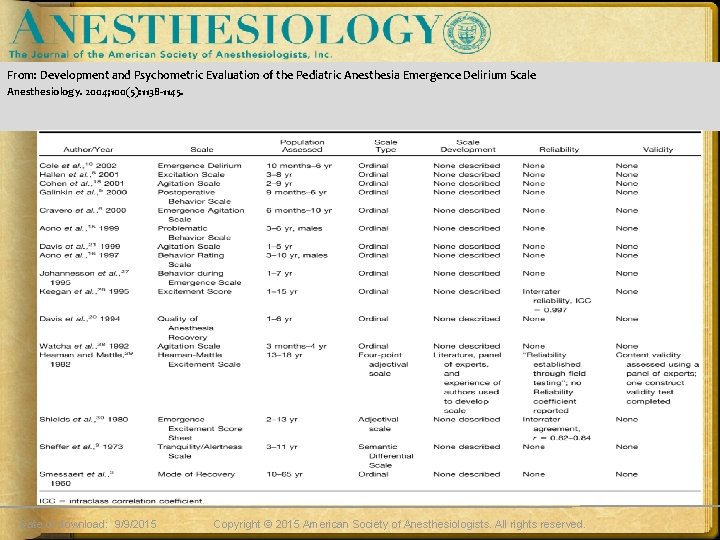
From: Development and Psychometric Evaluation of the Pediatric Anesthesia Emergence Delirium Scale Anesthesiology. 2004; 100(5): 1138 -1145. Date of download: 9/9/2015 Copyright © 2015 American Society of Anesthesiologists. All rights reserved.
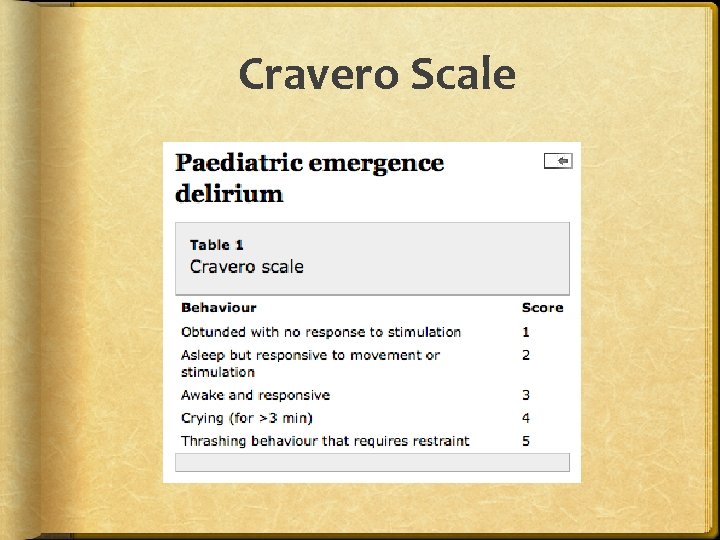
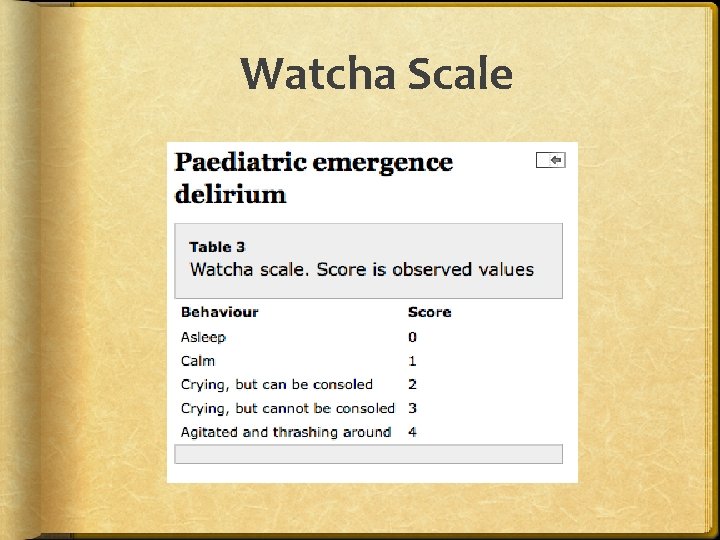
Identify 2010 comparison of these 3 emergence delirium scales Findings include: All three scales correlate reasonably well with each other Each have individual limitations All patients in this study assessed by the experienced pediatric anesthetist observer has having ED scored highly on all three scales
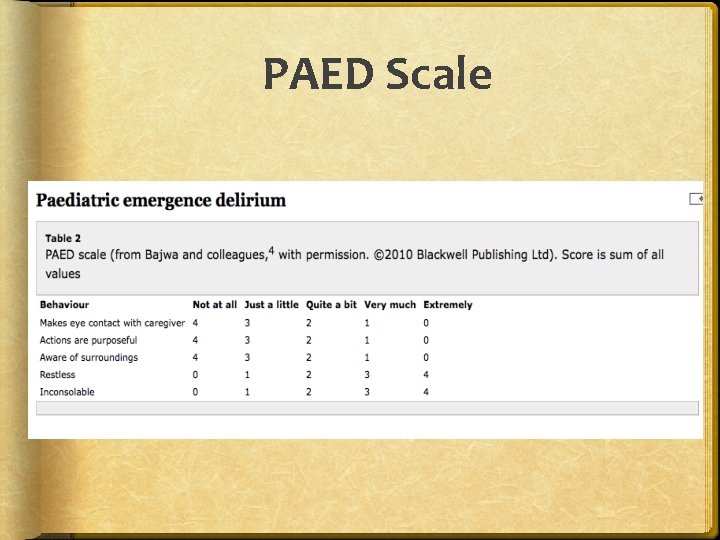
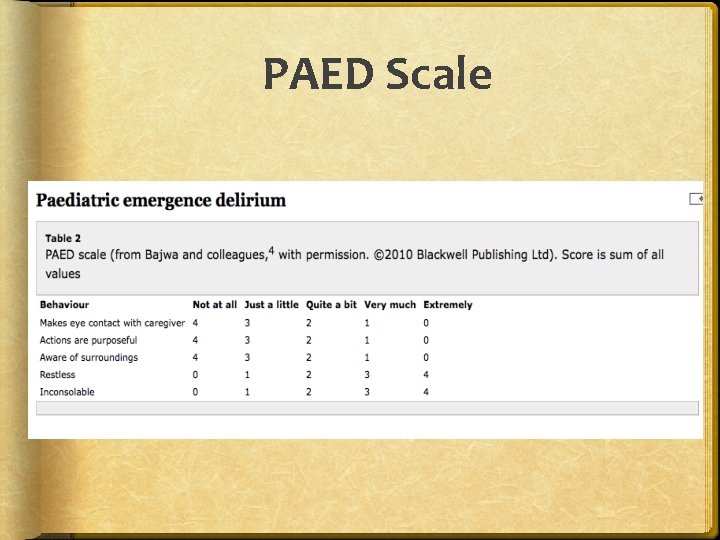
PAED Scale
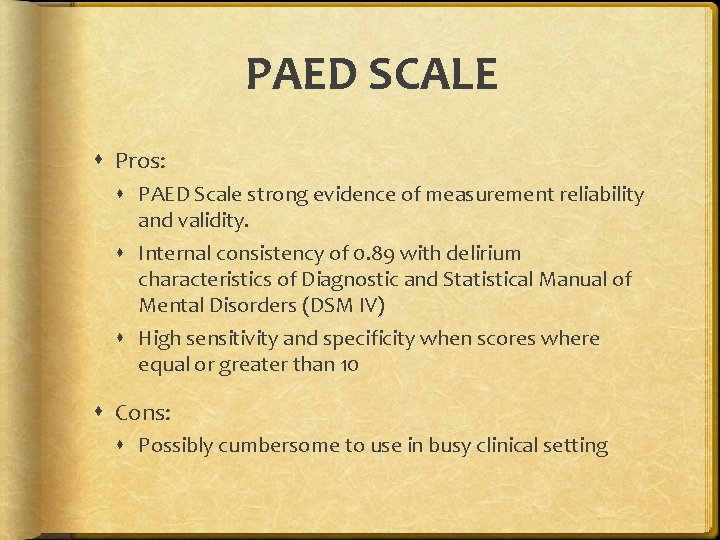
PAED SCALE Pros: PAED Scale strong evidence of measurement reliability and validity. Internal consistency of 0. 89 with delirium characteristics of Diagnostic and Statistical Manual of Mental Disorders (DSM IV) High sensitivity and specificity when scores where equal or greater than 10 Cons: Possibly cumbersome to use in busy clinical setting
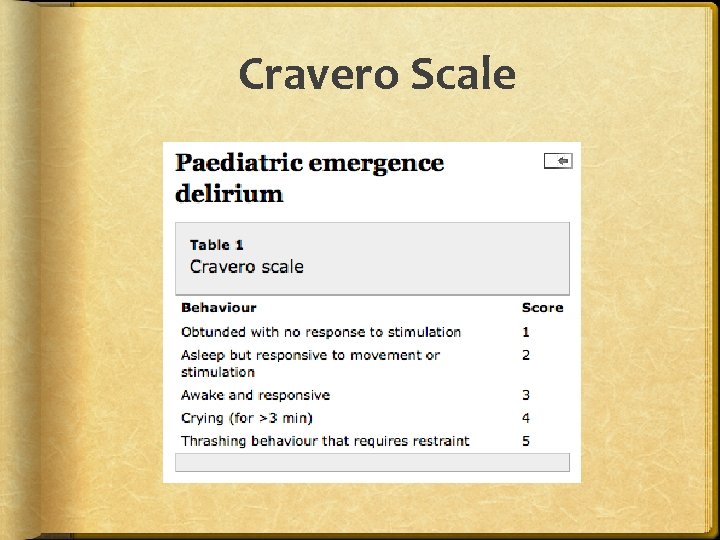
Cravero Scale
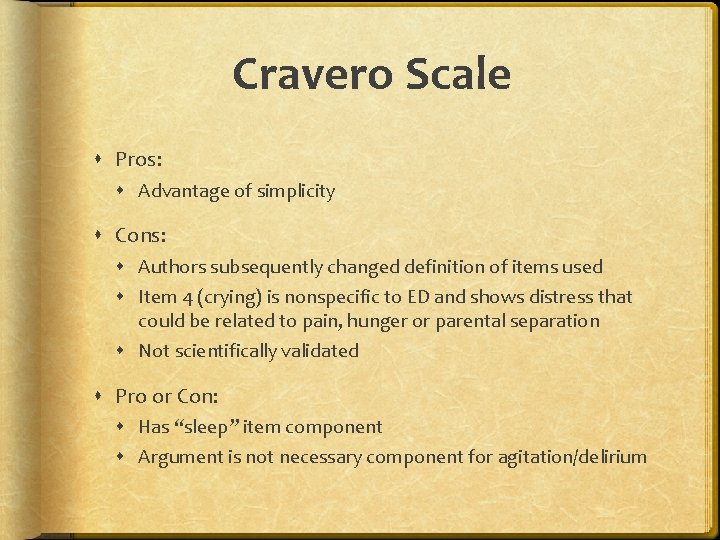
Cravero Scale Pros: Advantage of simplicity Cons: Authors subsequently changed definition of items used Item 4 (crying) is nonspecific to ED and shows distress that could be related to pain, hunger or parental separation Not scientifically validated Pro or Con: Has “sleep” item component Argument is not necessary component for agitation/delirium
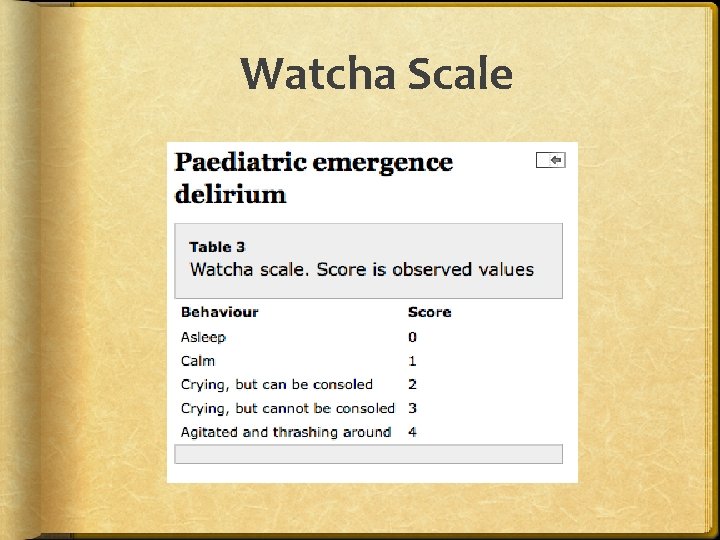
Watcha Scale
Watcha Scale Pro: Watcha scale has higher correlation than Cravero with respect to the PAED scale PAED score >12 and Watcha scale have maximal sensitivity and high specificity in detecting ED Ease of use Cons: No evidence of validation Minimal research using just Watcha scale is effective for determining ED Cannot rule out other causes for high ratings, pain, anxiety etc.
Diagnosis Rule out other factors: begin with basics Hypoxemia: using adhesive sat probe vs. clip on Dehydration: case dependent, fluid status, urine output, surgical blood loss Hypotension: fluid status, medication related etc. Hypoglycemia: patient dependent Anxiety Narcotic side effects: itching, urinary retention etc. Pain: case dependent, procedure, VS, anesthetic technique, intra op medications
Diagnosis Critical Thinking is a necessary component to diagnosing ED Ruling out other causative factors in combinations with…. Use of diagnostic tools DIAGNOSIS IS ED……NOW WHAT?
MANAGEMENT Decision to treat ED in PACU is often influenced by the severity and duration of symptoms. Likely to treat pharmacologically when concerns of safety of the child, disruption of surgical site or accidental removal of lines or drains Two strategies: Non Pharmacologic
Management Non-pharmacologic Allow child to wake up in their own time (preventative) Decrease stimulation Consider foregoing EKG lead (per anesthesia or department policy) Dark and quiet environment Soothing verbal reassurance and orientation if appropriate
Management Non-pharmacologic (continued) Allowing familiar objects (blanket, stuffed animal) Parental reuniting- if appropriate Soothing music or i. Pad cartoons Physical restraint- may “wrap” in warm blankets in lieu of restraints
Management Pharmacologic- used as preventative and for management. Fentanyl Morphine Midazolam Dexmedetomidine Clonidine Ketorolac Propofol
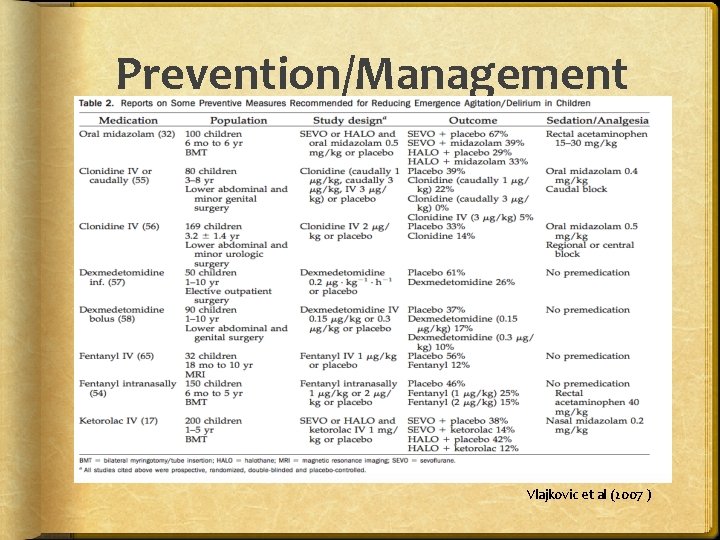
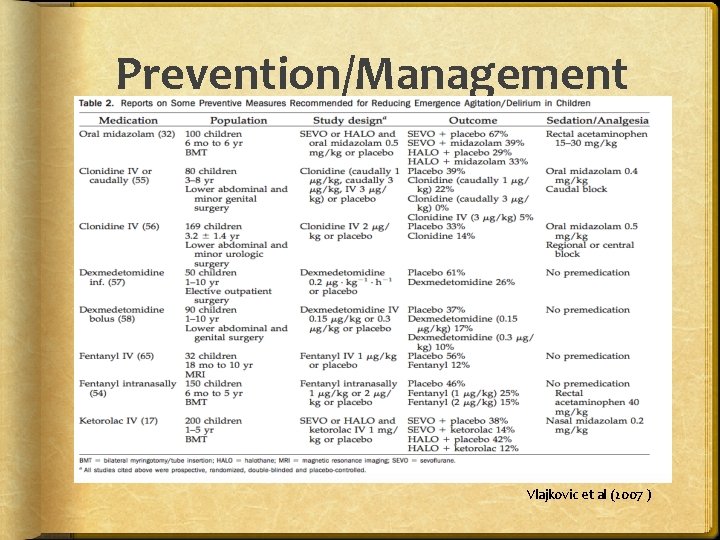
Prevention/Management Vlajkovic et al (2007 )
Management Large meta-analysis 2010 37 articles, 3172 patients Midazolam, propofol, ketamine, A 2 antagonists, fentanyl, 5 HT 3 inhibitors Primary outcomes: incidence of emergence agitation Results in brief: Midazolam, and 5 HT 3 inhibitors not found to have protective effect against EA/ED Propofol, ketamine, A 2 agonists, fentanyl and preop analgesia were all found to have a preventative effect. BJA (2010)
Management Research has found PACU nurses have first utilized pain management orders such as fentanyl If assertive treatment is necessary… Single bolus of propofol 0. 5 -1 mg/kg IV Fentanyl 1 -2. 5 mcg/kg IV Dexmedetomidine 0. 5 mcg/kg IV Has been successful in decreasing the severity and duration of ED episode. Banchs (2014)
Emergence Delirium: Conclusion ED is common and self limiting ED is usually brief, but pharmacological management may be required Potentially harmful to patient and caregivers Challenging to manage Good post-op pain control is crucial
Emergence Delirium Conclusion Pre-op sedation is probably helpful for anxious patients NO evidence that if left untreated ED had long-term sequelae in children More research is necessary to find better anesthetic agents, diagnostic tools and preventative measures.
We like Happy Tykes
References American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4 th ed. Arlington, VA: American Psychiatric Publishing, 2000. Aono J, Mamiya K, Manabe M. Preoperative anxiety is associated with a high incidence of problematic behavior on emergence after halothane anesthesia in boys. Acta Anaesthesiol Scand 1999; 43: 542– 4. Bajwa S, Costi, D, Cyna, A, A comparison of emergence delirium scales following general anesthesia in children. Pediatric Anesthesia 2010; 20: 704 -11 Bowie, JR. Parents in the operating room? Anesthesiology 1993: 78: 1192 -3 Cohen IT, Hannallah RS, Hummer KA. The incidence of emergence agitation associated with desflurane anesthesia in children is reduced by fentanil. Anesth Analg 2001; 93: 88– 91.
References Cravero J, Surgenor S, Whalen K. Emergence agitation in paediatric patients after sevoflurane anesthesia and no surgery: a comparison with halothane. Paediatr Anaesth 2000; 10: 419 – 24. Eckenhoff JE, Kneale DH, Dripps RD. The incidence and etiol- ogy of postanesthetic excitement. A clinical survey. Anesthesiology 1961; 22: 667– 73. Fortier MA, Tan ET, Mayes LC, et al. Ethnicity and parental report of postoperative behavioral changes in children. Paediatr Anesthe 2013; 23: 422 -8 Galford RE. Problems in anesthesiology: approach to diagnosis. Boston, MA: Little, Brown & Company, 1992: 341– 3.
References Johnson, YJ, Nickerson M, Quezado ZM. An unforeseen peril of parental presence during induction of anesthesia. Anesth Analg 2012; 115: 1371 -4 Kain ZN, Caldwell-Andrews AA, Mayes LC, et al. Family-centered preparation for surgery improves perioperative outcomes in children. Anesthesiology 2007; 106: 65 74 Kain ZN, Caldwell-Andrews AA, Maranets I, et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg 2004; 99: 1648– 54. Kulka PJ, Bressem M, Tryba M. Clonidine prevents sevoflurane- induced agitation in children. Anesth Analg 2001; 93: 335– 8.
References Lepouse et al. BJA 2006: 96(6): 747 -753 Mc. Graw T. Preparing children for the operating room: psychological issues. Can J Anesth 1994; 41: 1094 -103 Oh AY, Seo KS, Kim SD, et al. Delayed emergence process does not result in a lower incidence of emergence agitation after sevoflurane anesthesia in children. Acta Anaesthesiol Scand 2005; 49: 297– 9. Picard V, Dumont L, Pellegrini M. Quality of recovery in children: sevoflurane versus propofol. Acta Anaesthesiol Scand 2000; 44: 307– 10. Przybylo HJ, Martini DR, Mazurek AJ, et al. Assessing behaviour in children emerging from anesthesia: can we apply psychiatric diagnostic techniques? Paediatr Anaesth 2003; 13: 609 – 16.
References Rothbart MK, Ahadi SA, Evans DE. Temperament and personality: origins and outcomes. J Pers Soc Psychol 2000; 78: 122– 35 Sikich, N, Lermann J. Development and psychometric evaluation of the Pediatric Anesthesia Emergence Delirium Scale. Anesthesiology 2004; 11: 1138 -1145 Vlajkovic & Sindjelic, Anesth Analg 2007: 104(1): 84 -91 Voepel-Lewis T, Burke C. Differentiating pain and delirium is only part of assessing the agitated child. J Perianesth Nurs 2004; 19: 298 – 9. Voepel-Lewis T, Malviya S, Tait AR. A prospective cohort study of emergence agitation in the pediatric postanesthesia care unit. Anesth Analg 2003; 96: 1625– 30.