Lisfranc Injury of the Foot A Commonly Missed













- Slides: 60
Lisfranc Injury of the Foot: A Commonly Missed Diagnosis James J. Lehman, DC, MBA, FACO Director UB Clinics and Community Health Clinical Education University of Bridgeport
Contact Information n James J. Lehman, DC, MBA jlehman@bridgeport. edu 505 -238 -9501
Learning Objectives • Identify injured and painful tissues through careful assessment of the foot and intelligent use of neuromusculoskeletal testing to document the findings.
History of Lisfranc Injury Lisfranc injuries are named after Jacques Lisfranc, a French surgeon in the early 1800 s. In the army, a lot of the soldiers would get thrown from their horses, and their foot would get caught in the stirrup. This would cause an injury to the middle of the foot.
Now we have rodeo
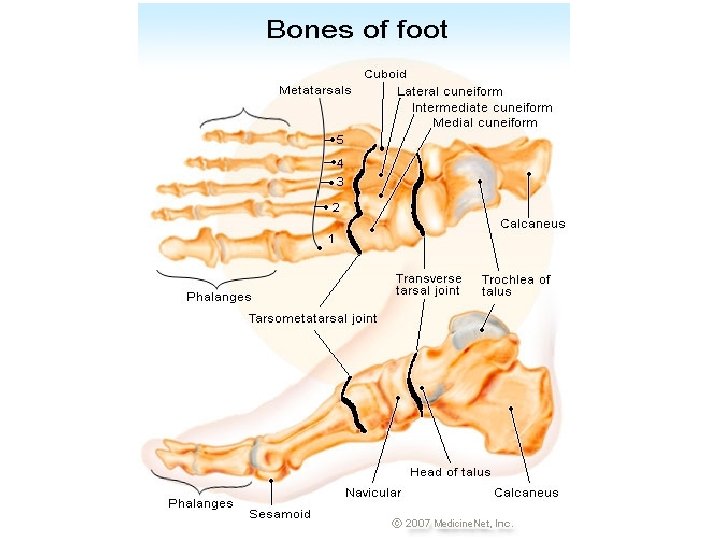
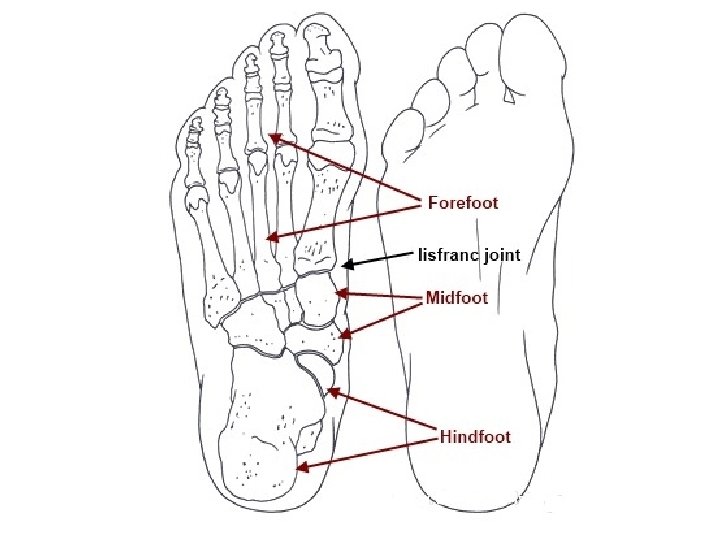
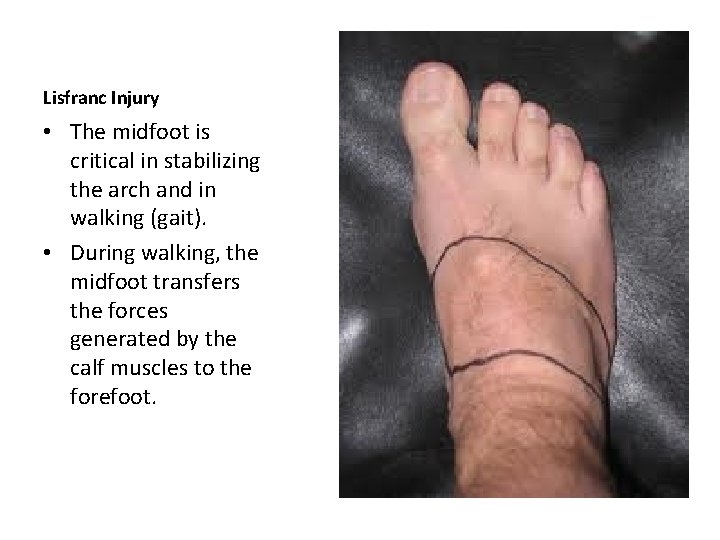
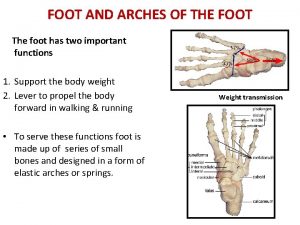
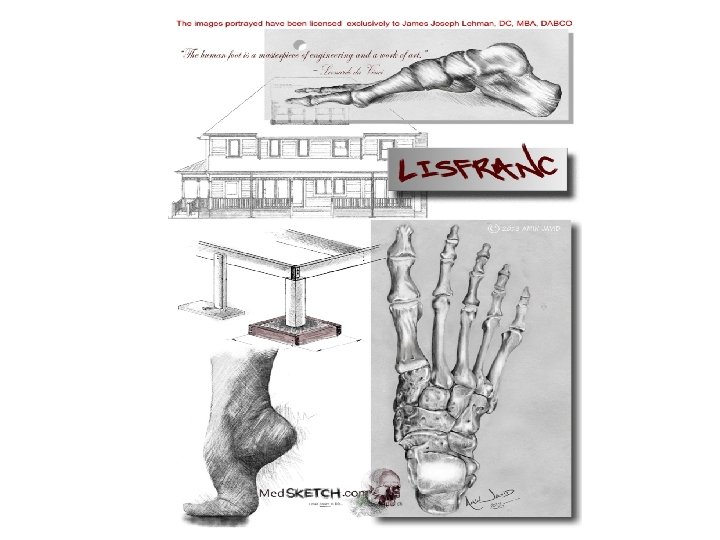
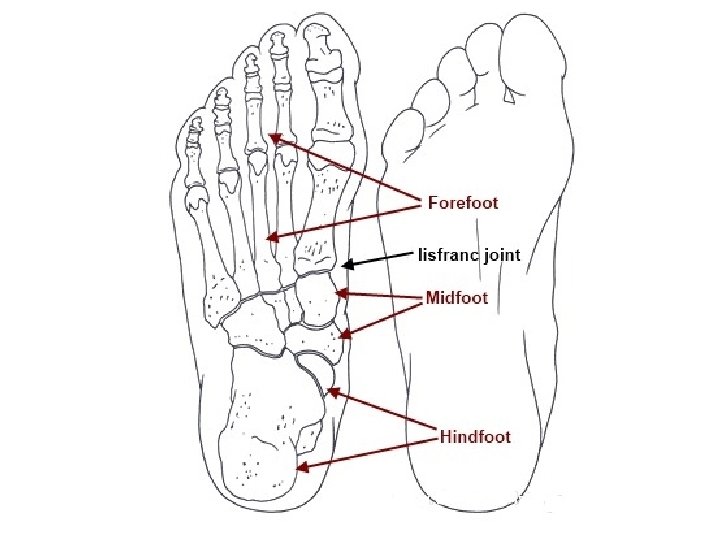
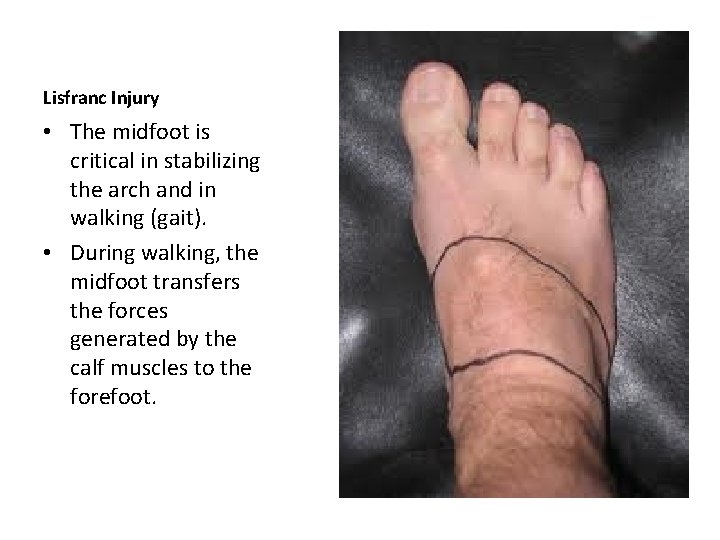
Lisfranc Injury • The midfoot is critical in stabilizing the arch and in walking (gait). • During walking, the midfoot transfers the forces generated by the calf muscles to the forefoot.
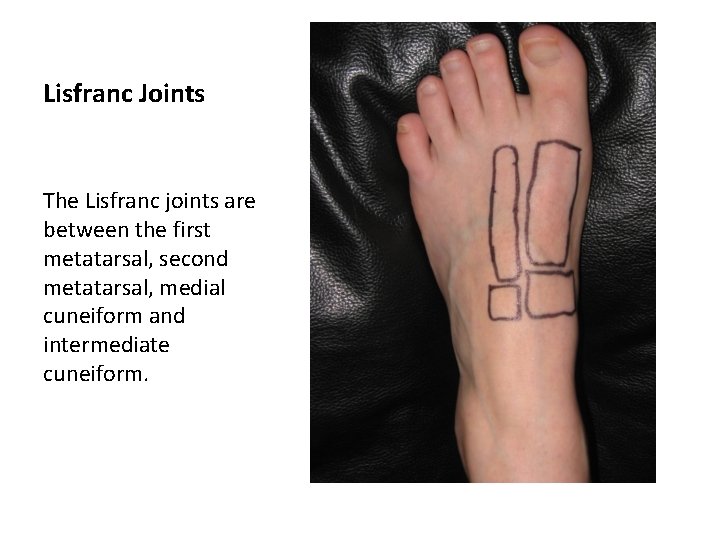
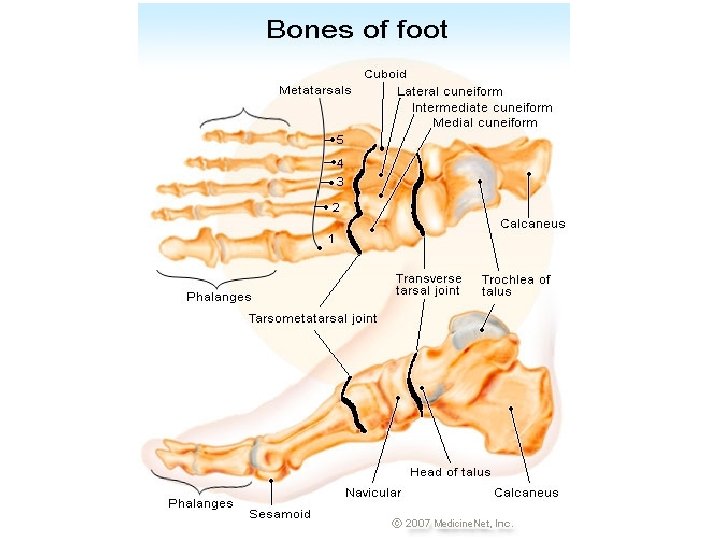
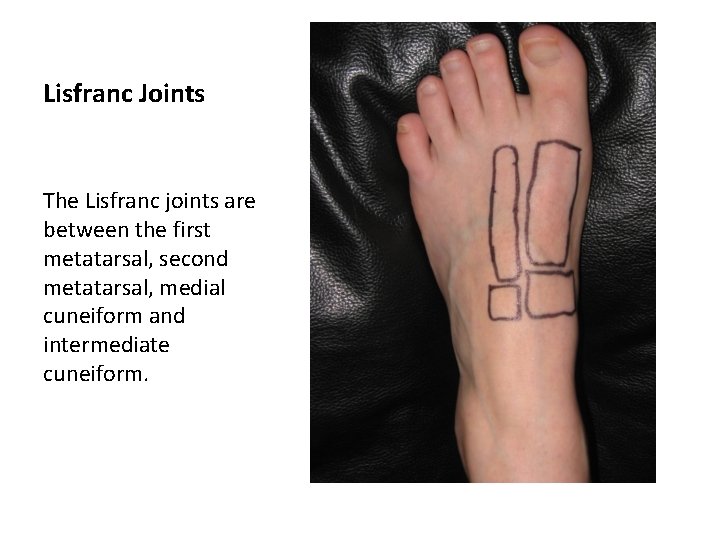
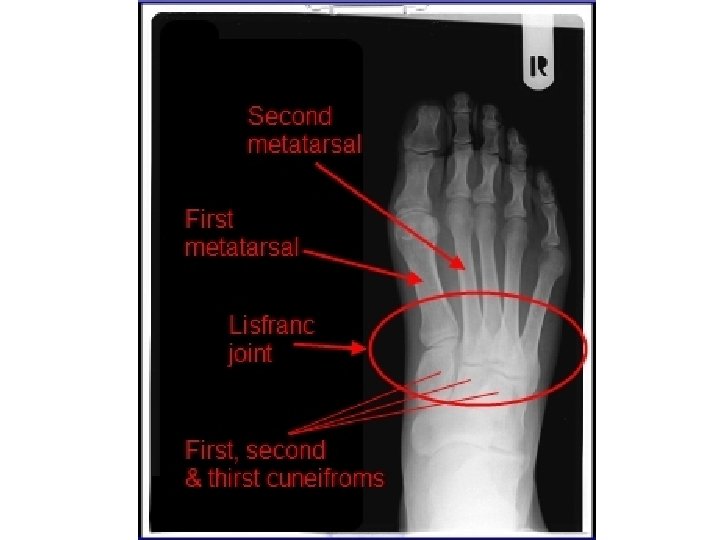
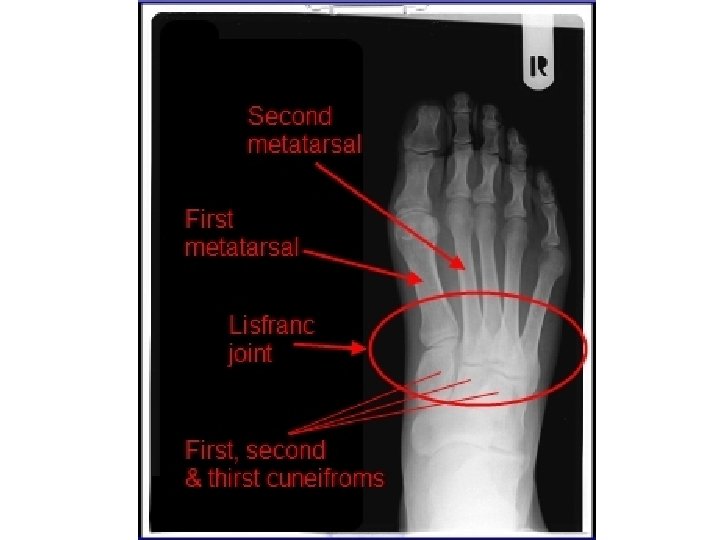
Lisfranc Joints The Lisfranc joints are between the first metatarsal, second metatarsal, medial cuneiform and intermediate cuneiform.
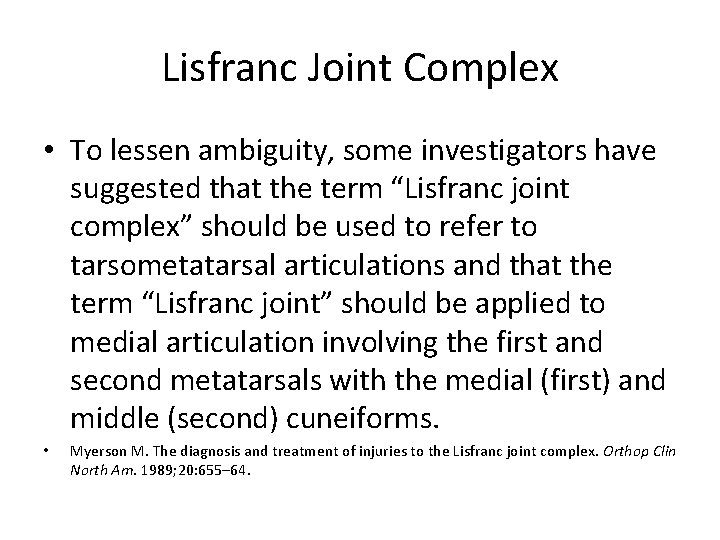
Lisfranc Joint Complex • To lessen ambiguity, some investigators have suggested that the term “Lisfranc joint complex” should be used to refer to tarsometatarsal articulations and that the term “Lisfranc joint” should be applied to medial articulation involving the first and second metatarsals with the medial (first) and middle (second) cuneiforms. • Myerson M. The diagnosis and treatment of injuries to the Lisfranc joint complex. Orthop Clin North Am. 1989; 20: 655– 64.
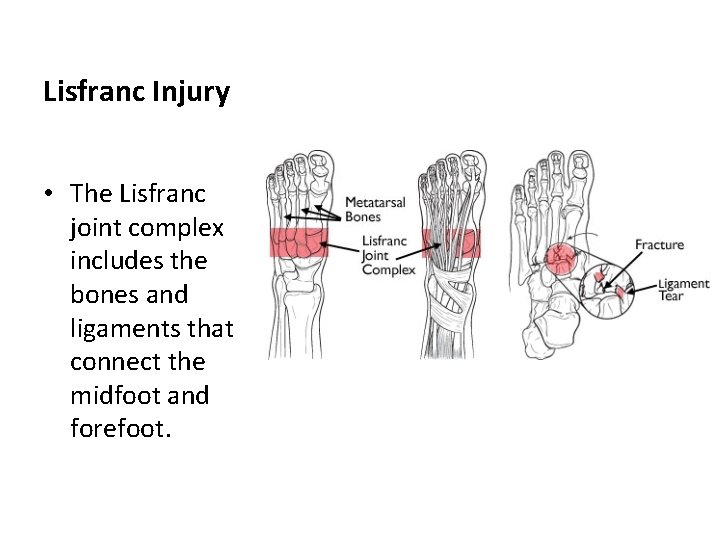
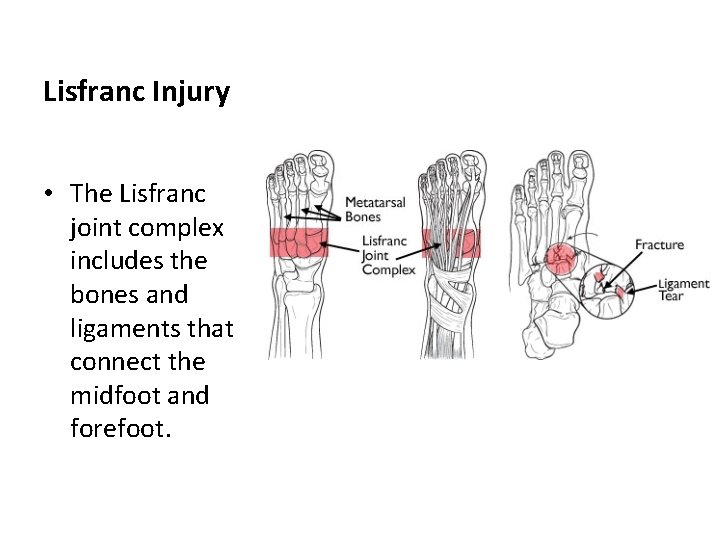
Lisfranc Injury • The Lisfranc joint complex includes the bones and ligaments that connect the midfoot and forefoot.
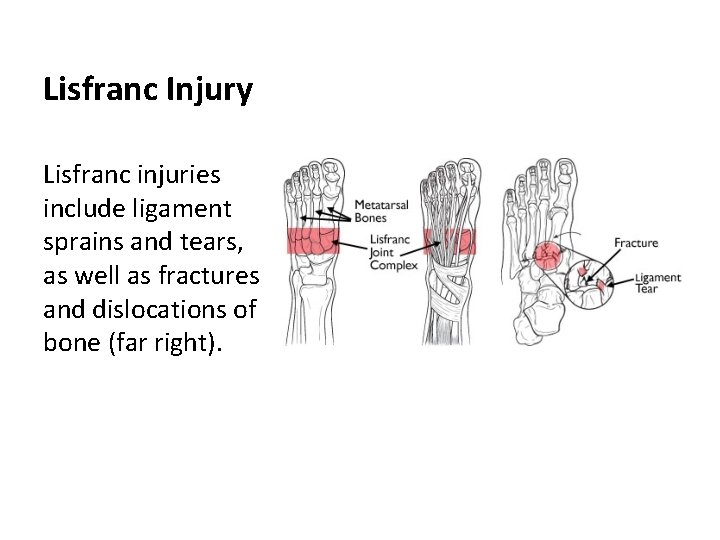
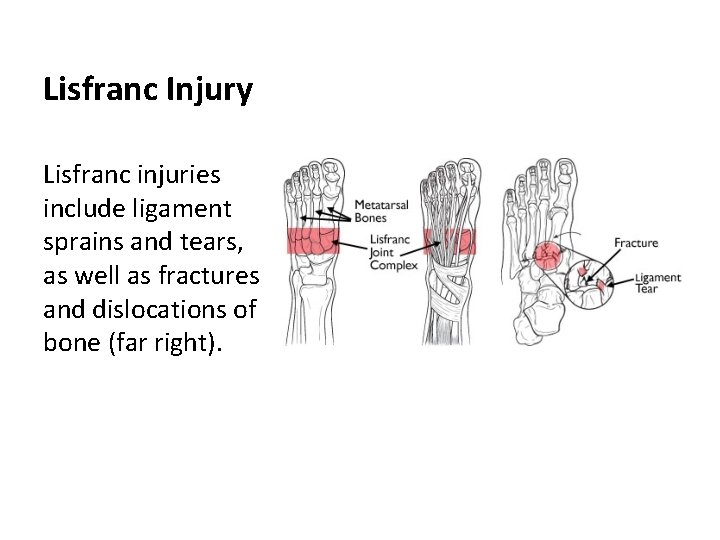
Lisfranc Injury Lisfranc injuries include ligament sprains and tears, as well as fractures and dislocations of bone (far right).
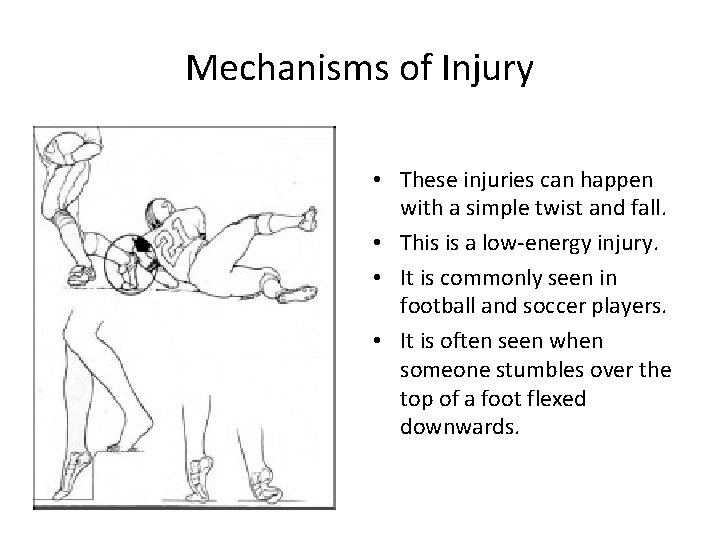
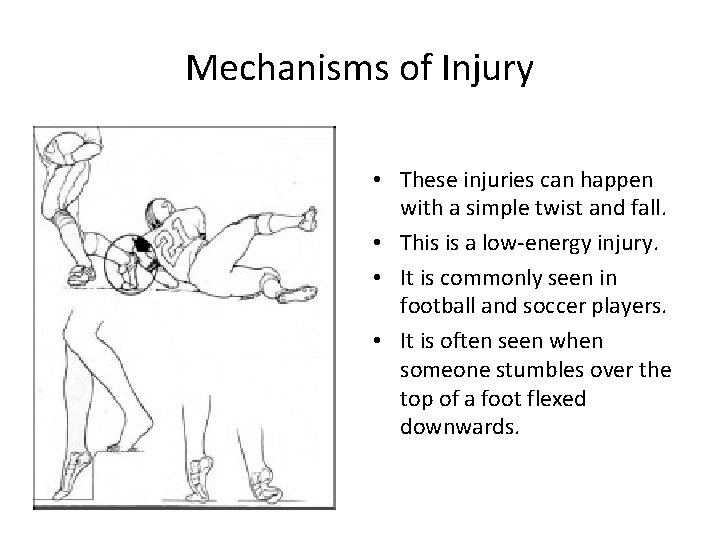
Mechanisms of Injury • These injuries can happen with a simple twist and fall. • This is a low-energy injury. • It is commonly seen in football and soccer players. • It is often seen when someone stumbles over the top of a foot flexed downwards.
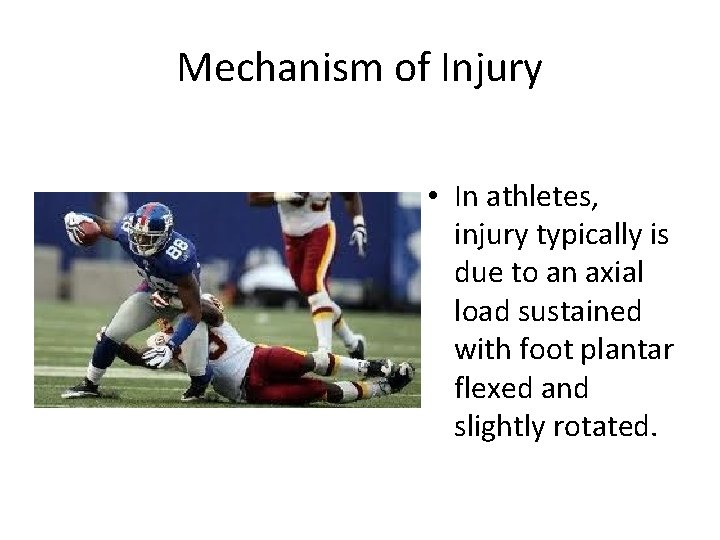
Mechanism of Injury • In athletes, injury typically is due to an axial load sustained with foot plantar flexed and slightly rotated.
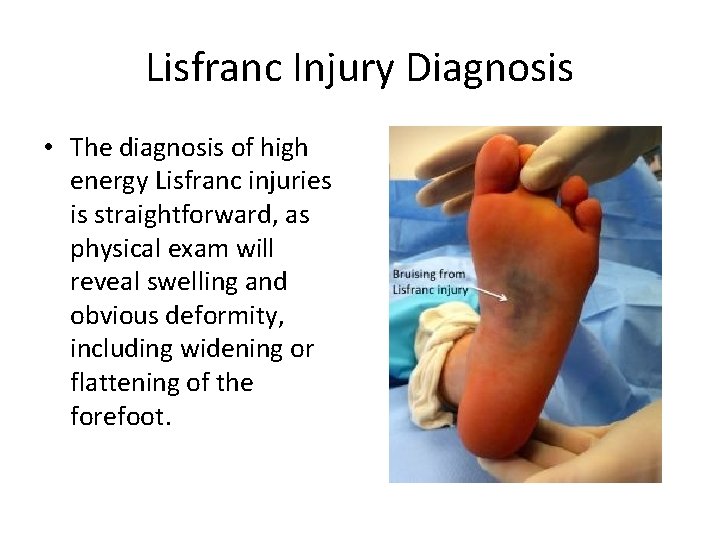
Most common symptoms of Lisfranc injury • The top of foot may be swollen and painful. • There may be bruising on both the top and bottom of the foot. Bruising on the bottom of the foot is highly suggestive of a Lisfranc injury. • Pain that worsens with standing or walking. The pain can be so severe that crutches may be required.
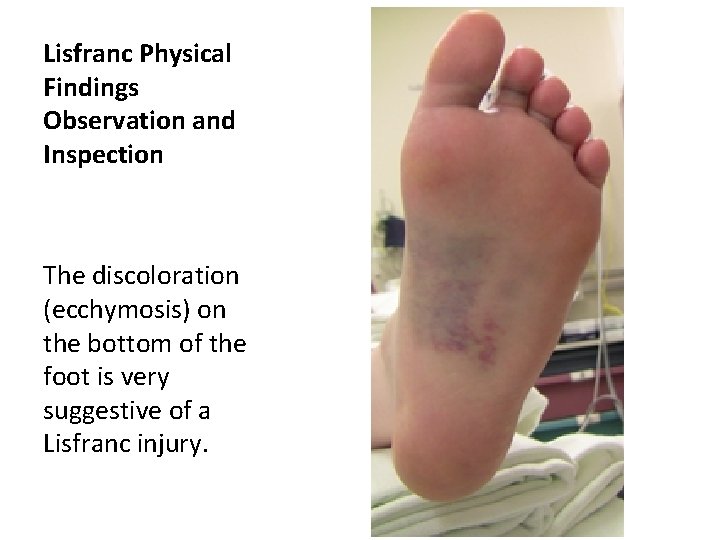
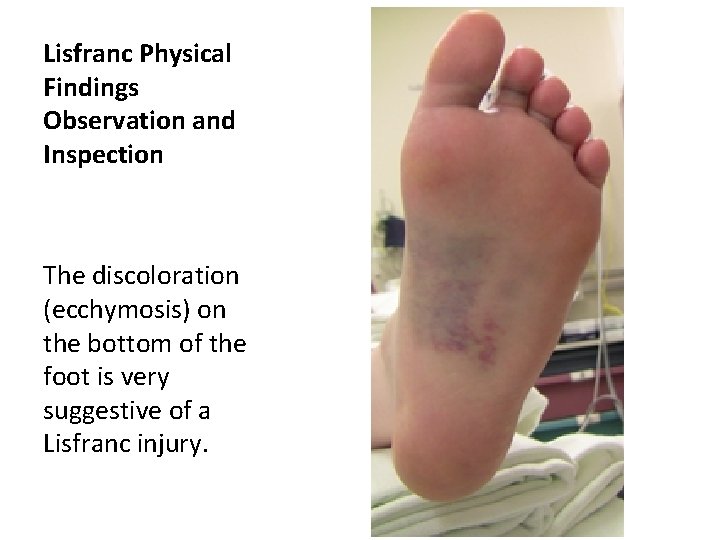
Lisfranc Physical Findings Observation and Inspection The discoloration (ecchymosis) on the bottom of the foot is very suggestive of a Lisfranc injury.
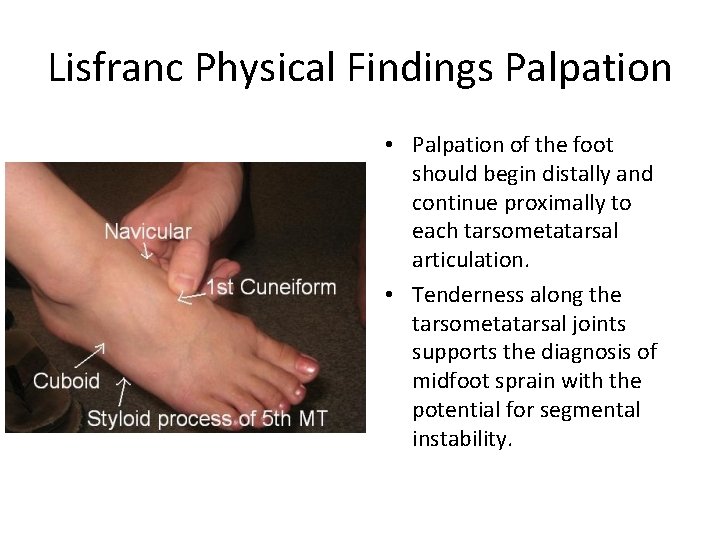
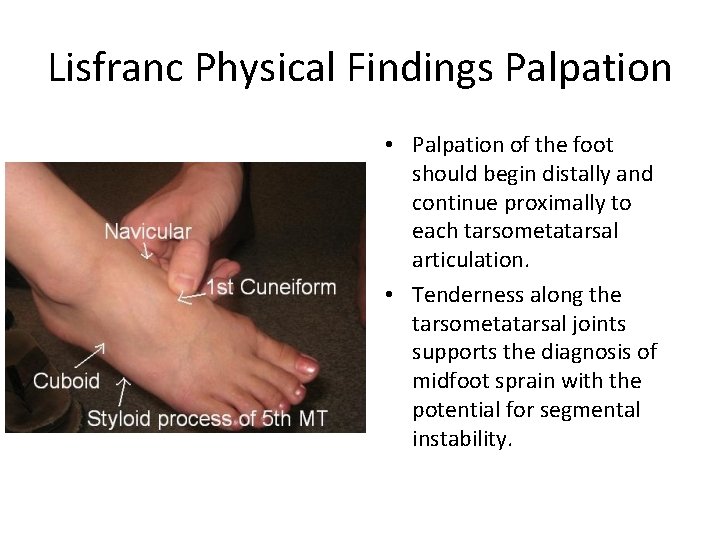
Lisfranc Physical Findings Palpation • Palpation of the foot should begin distally and continue proximally to each tarsometatarsal articulation. • Tenderness along the tarsometatarsal joints supports the diagnosis of midfoot sprain with the potential for segmental instability.
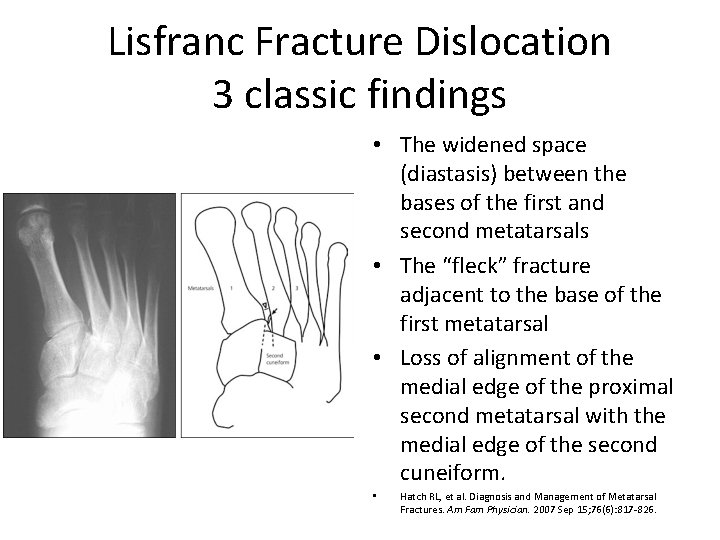
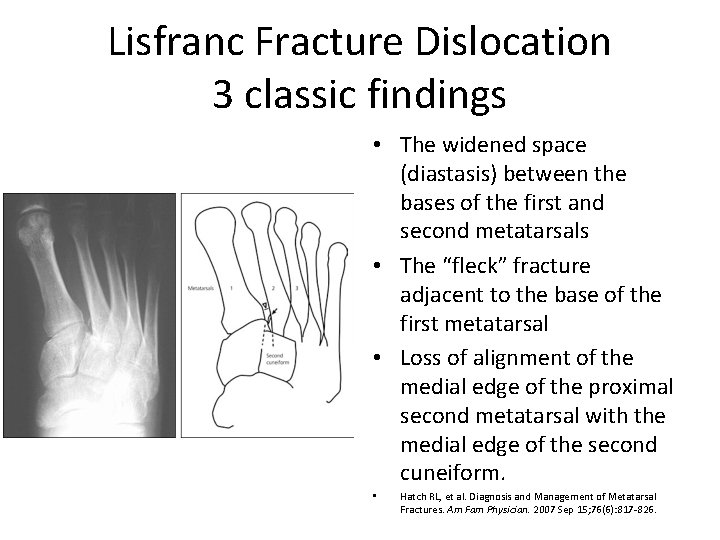
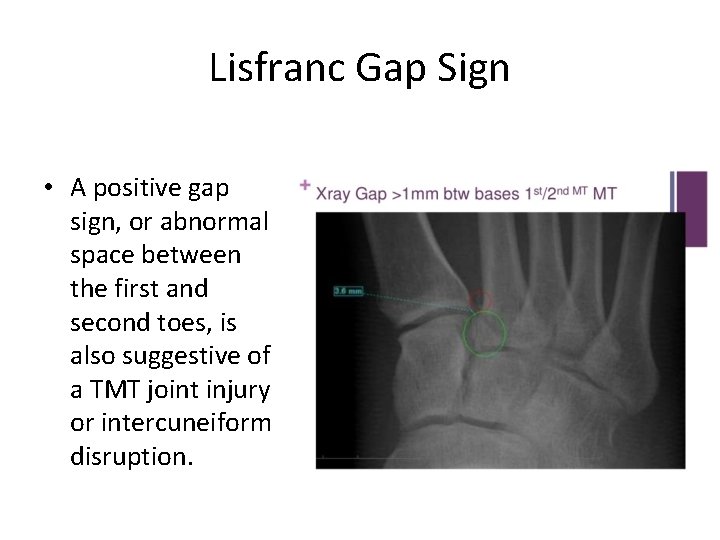
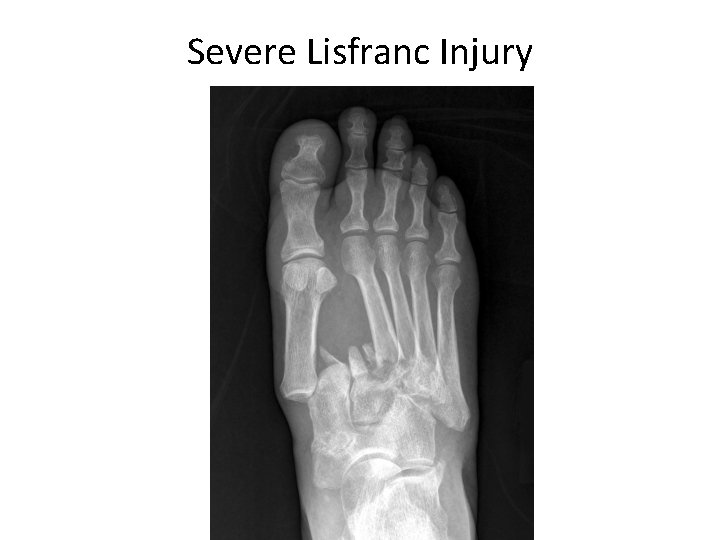
Lisfranc Fracture Dislocation 3 classic findings • The widened space (diastasis) between the bases of the first and second metatarsals • The “fleck” fracture adjacent to the base of the first metatarsal • Loss of alignment of the medial edge of the proximal second metatarsal with the medial edge of the second cuneiform. • Hatch RL, et al. Diagnosis and Management of Metatarsal Fractures. Am Fam Physician. 2007 Sep 15; 76(6): 817 -826.
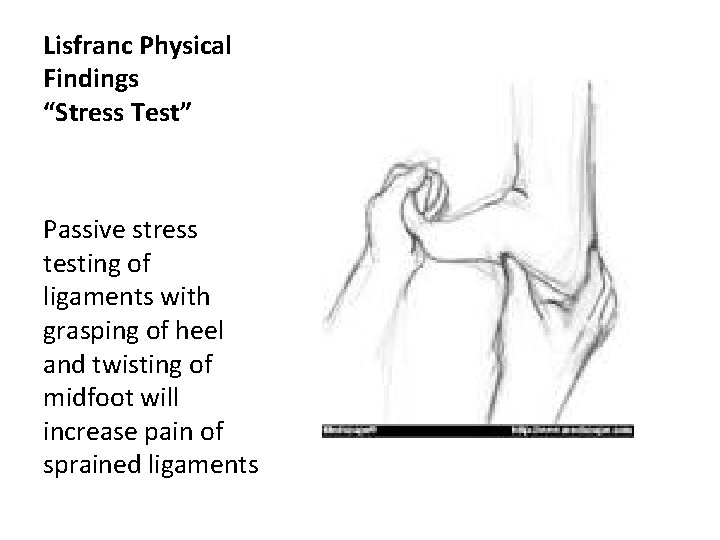
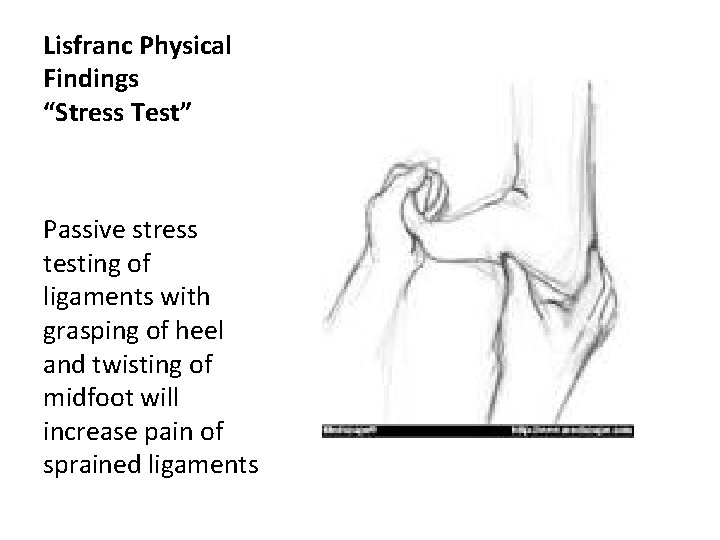
Lisfranc Physical Findings “Stress Test” Passive stress testing of ligaments with grasping of heel and twisting of midfoot will increase pain of sprained ligaments
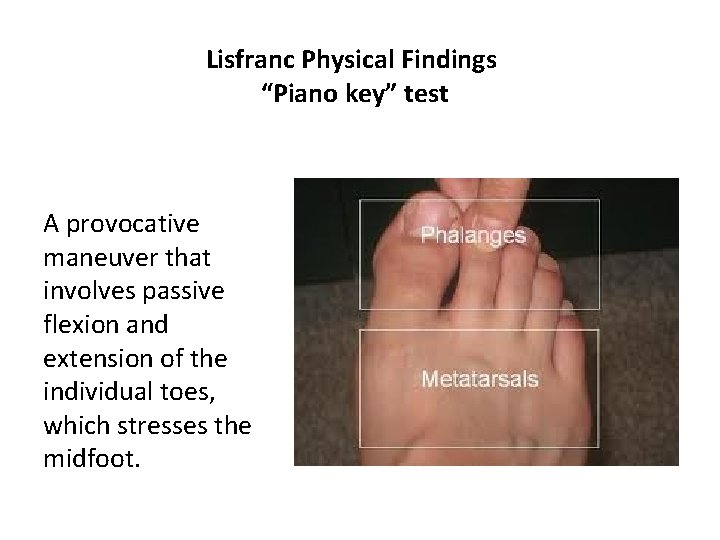
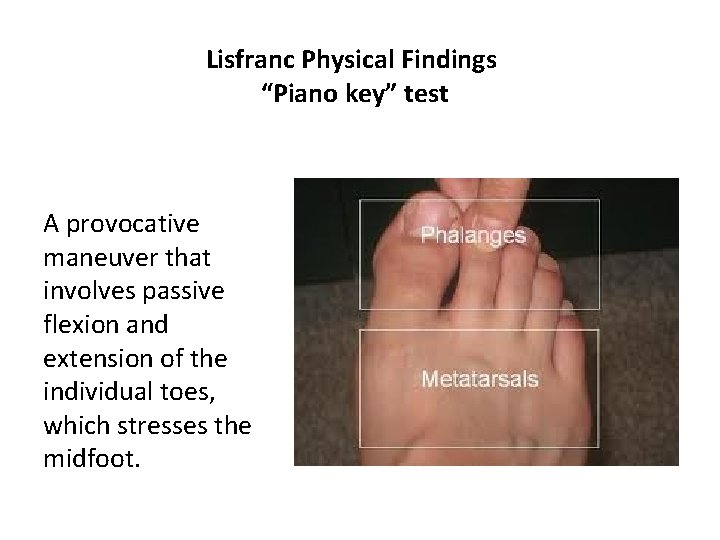
Lisfranc Physical Findings “Piano key” test A provocative maneuver that involves passive flexion and extension of the individual toes, which stresses the midfoot.
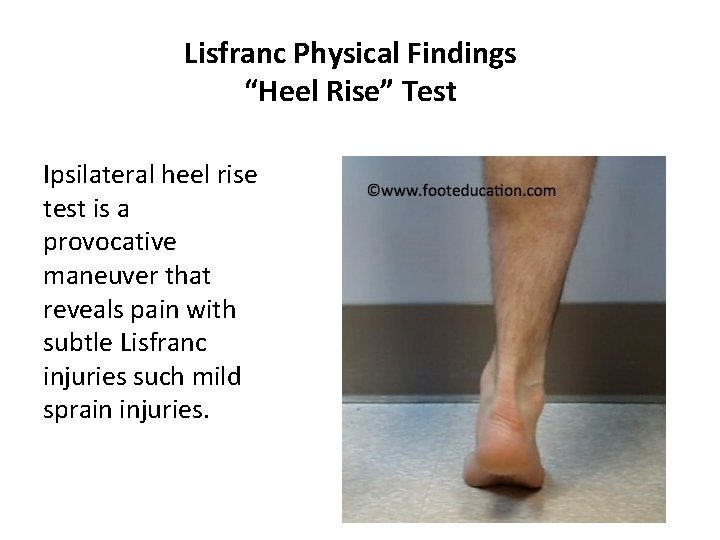
Lisfranc Physical Findings “Heel Rise” Test Ipsilateral heel rise test is a provocative maneuver that reveals pain with subtle Lisfranc injuries such mild sprain injuries.
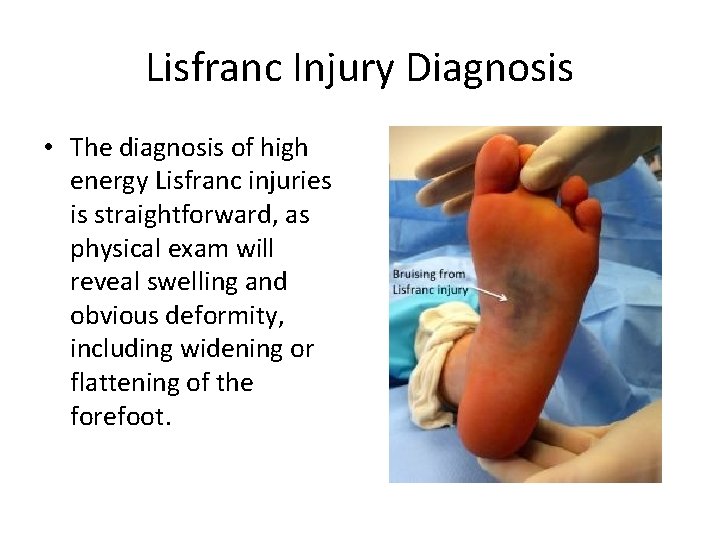
Lisfranc Injury Diagnosis • The diagnosis of high energy Lisfranc injuries is straightforward, as physical exam will reveal swelling and obvious deformity, including widening or flattening of the forefoot.
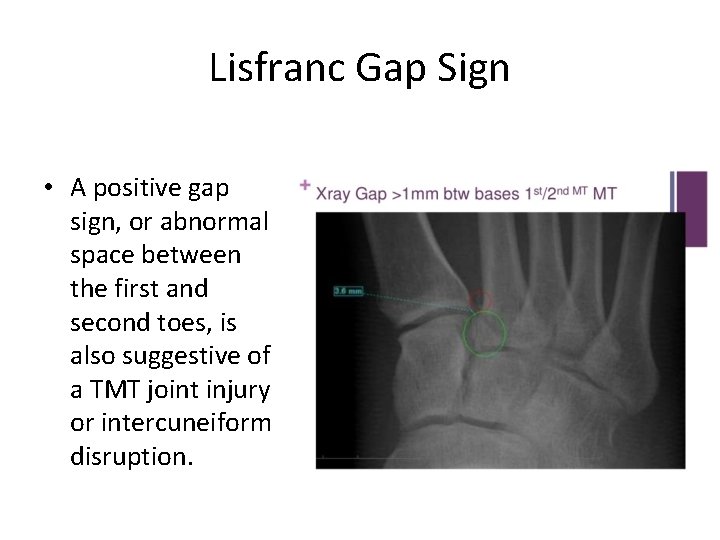
Lisfranc Gap Sign • A positive gap sign, or abnormal space between the first and second toes, is also suggestive of a TMT joint injury or intercuneiform disruption.
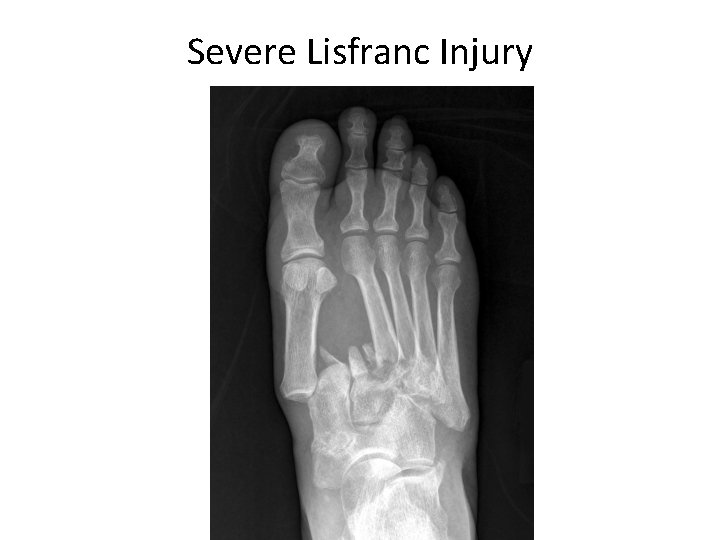
Severe Lisfranc Injury
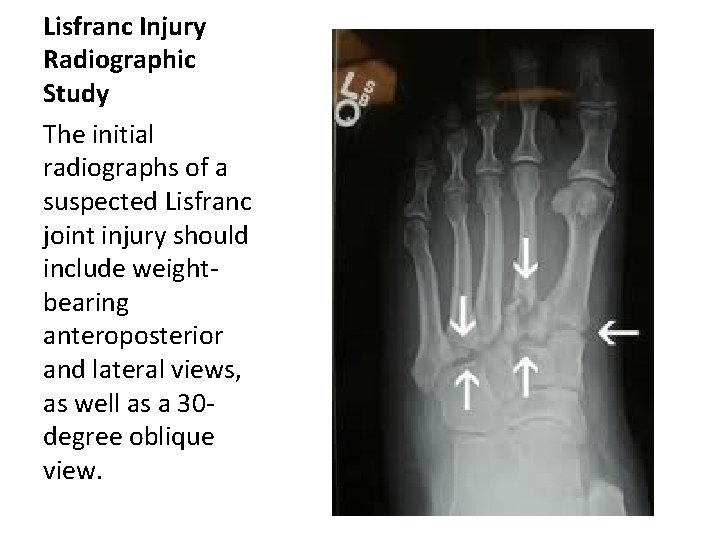
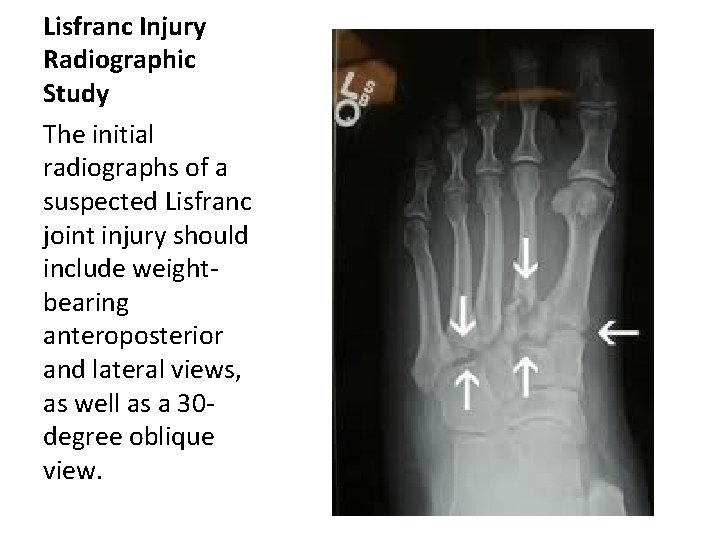
Lisfranc Injury Radiographic Study The initial radiographs of a suspected Lisfranc joint injury should include weightbearing anteroposterior and lateral views, as well as a 30 degree oblique view.
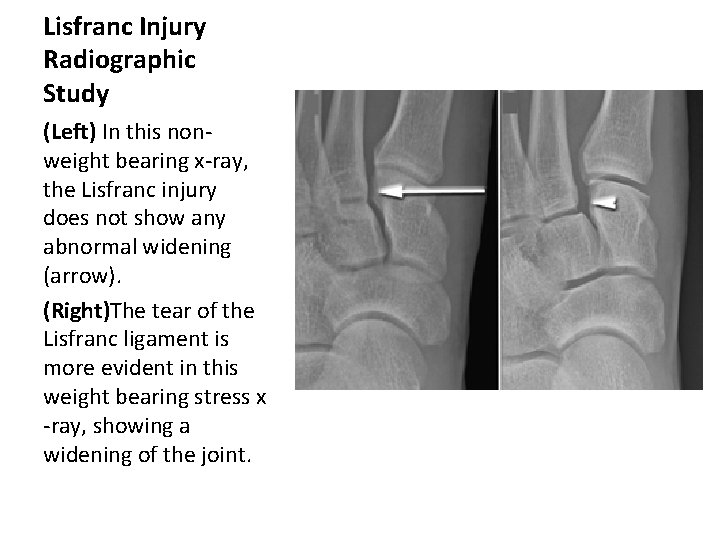
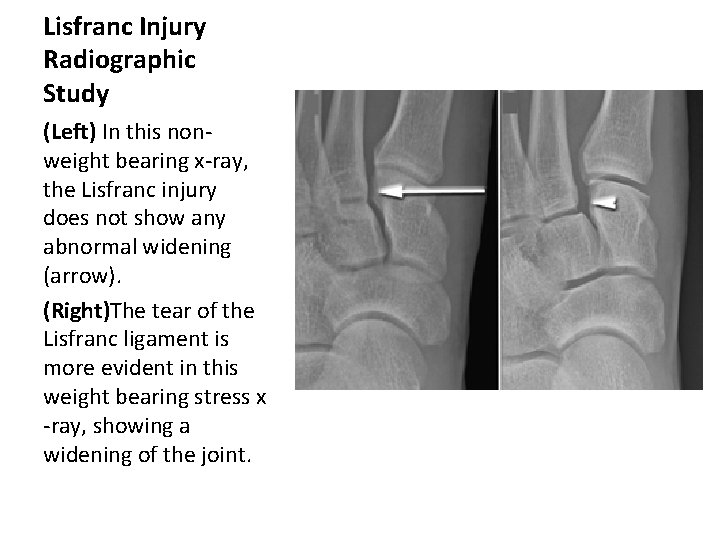
Lisfranc Injury Radiographic Study (Left) In this nonweight bearing x-ray, the Lisfranc injury does not show any abnormal widening (arrow). (Right)The tear of the Lisfranc ligament is more evident in this weight bearing stress x -ray, showing a widening of the joint.
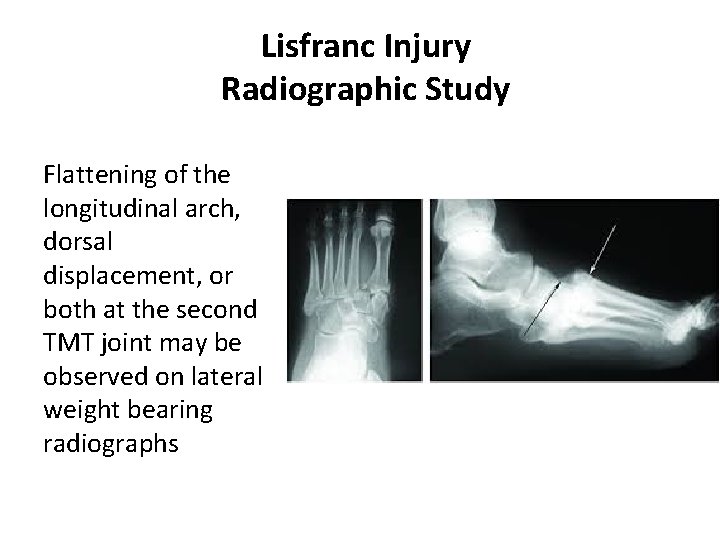
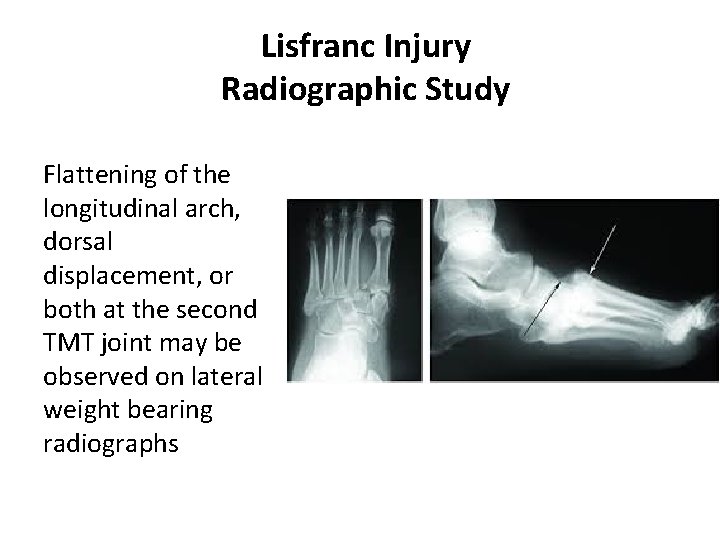
Lisfranc Injury Radiographic Study Flattening of the longitudinal arch, dorsal displacement, or both at the second TMT joint may be observed on lateral weight bearing radiographs
Lisfranc Injury ICD 10 Codes • S 93. 629 S sprain of tarsometatarsal joint • S 93. 315 A Dislocation of tarsal joint of left foot, initial encounter

Surgical Repair
Discussion Has anyone diagnosed and treated a patient with a Lifranc injury?
Case Report Day 1 • 20 year-old male • Injured left foot when thrown from sled • He landed with full weight on his left foot, which was folded under him • ER examination including radiographic study of left foot on day of injury • Impression negative for fracture • RX soft cast with foot placed in slight plantar flexion
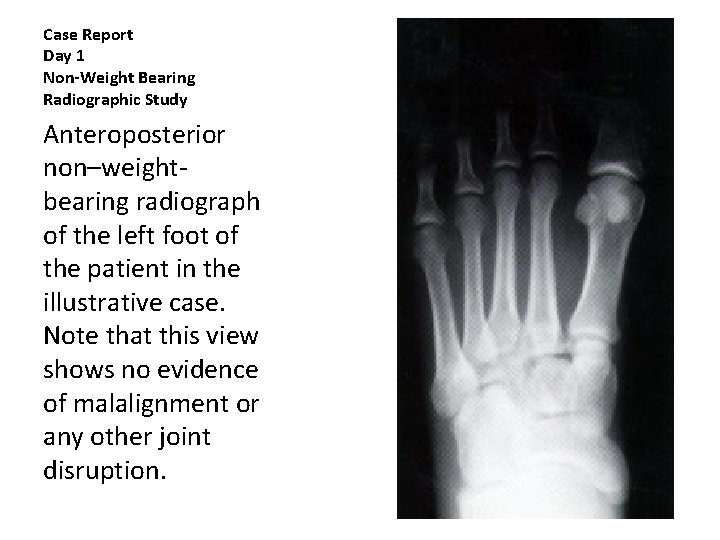
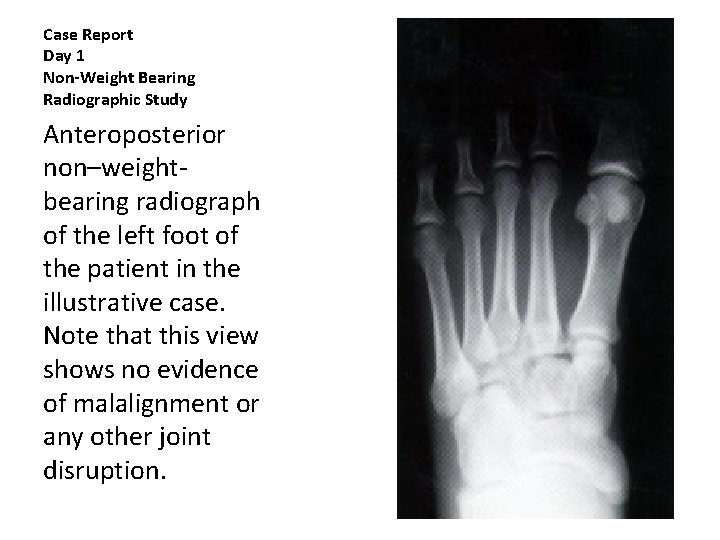
Case Report Day 1 Non-Weight Bearing Radiographic Study Anteroposterior non–weightbearing radiograph of the left foot of the patient in the illustrative case. Note that this view shows no evidence of malalignment or any other joint disruption.
Case Report Day 3 • Examined at student clinic three days posttrauma • Edema and ecchymosis noted on lateral foot • Unable to bear weight • Soft cast removed and replaced with elastic wrap
Case Report Day 7 • He was examined in the sports medicine clinic seven days post-trauma • Unable to bear weight on left foot • Edema extended from the midtarsal area distally into the toes • Ecchymosis along the metatarsophalangeal joint line to the lateral calcaneus
Case Report Day 7 • Marked dorsal tenderness noted over second through fourth tarsometatarsal joints and second through fifth metatarsophalangeal region • Minimal tenderness with palpation of plantar aspect of left foot • Pedal pulse present
Case Report Day 7 • Patient able to dorsiflex all toes against resistance • Left ankle demonstrated physical findings of a grade 1 anterior talofibular ligament sprain • Review of day one radiographic study revealed subtle dorsal displacement of the base of the second metatarsal
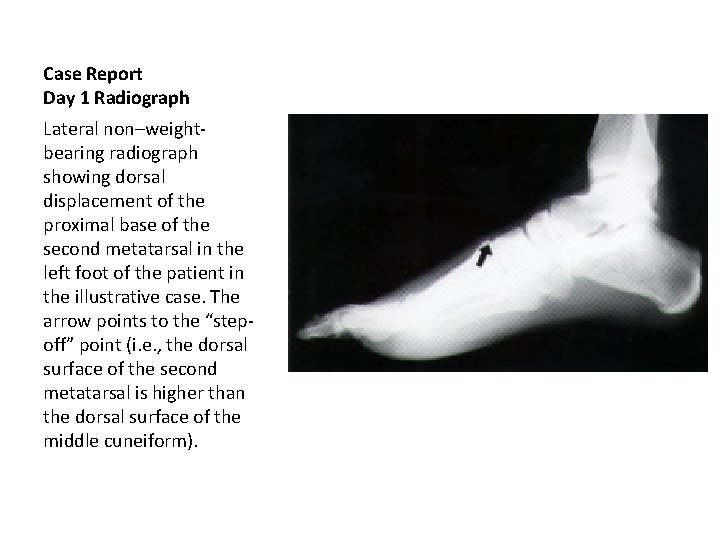
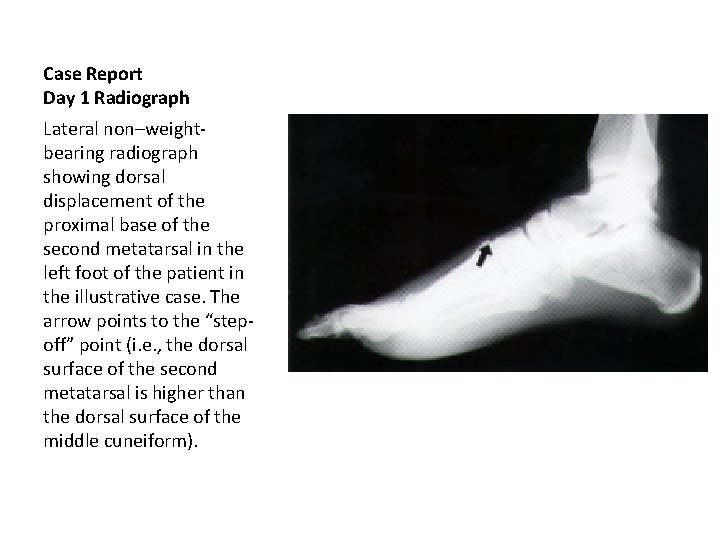
Case Report Day 1 Radiograph Lateral non–weightbearing radiograph showing dorsal displacement of the proximal base of the second metatarsal in the left foot of the patient in the illustrative case. The arrow points to the “stepoff” point (i. e. , the dorsal surface of the second metatarsal is higher than the dorsal surface of the middle cuneiform).
Case Report Day 7 • Weight bearing radiographic study revealed 3 mm separation of the first and second metatarsal bases and a bony fragment (fleck sign) in Lisfranc joint
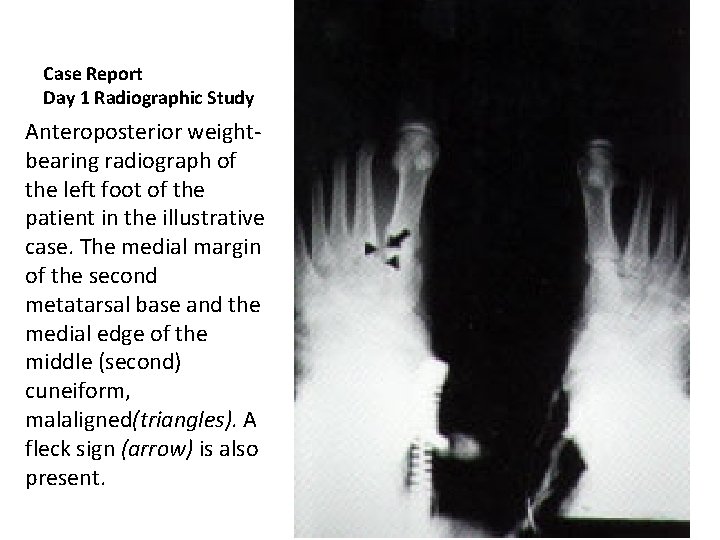
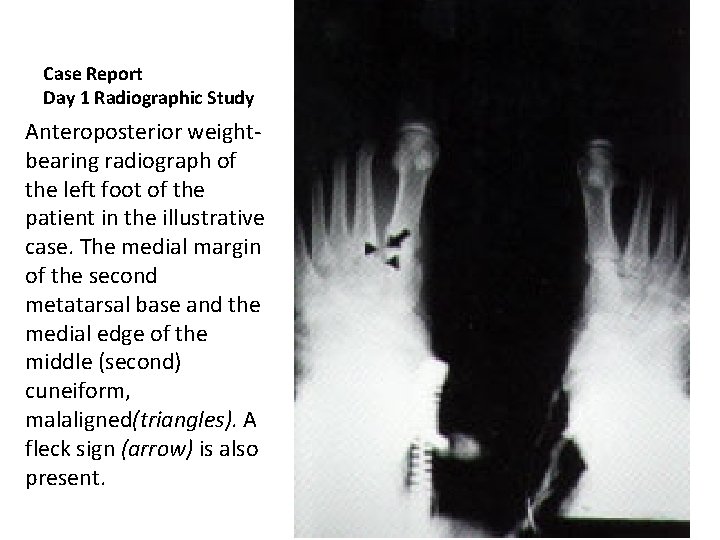
Case Report Day 1 Radiographic Study Anteroposterior weightbearing radiograph of the left foot of the patient in the illustrative case. The medial margin of the second metatarsal base and the medial edge of the middle (second) cuneiform, malaligned(triangles). A fleck sign (arrow) is also present.
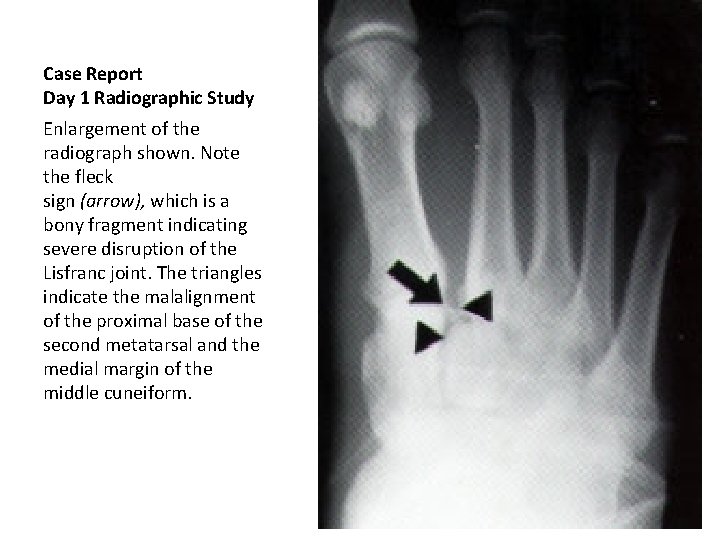
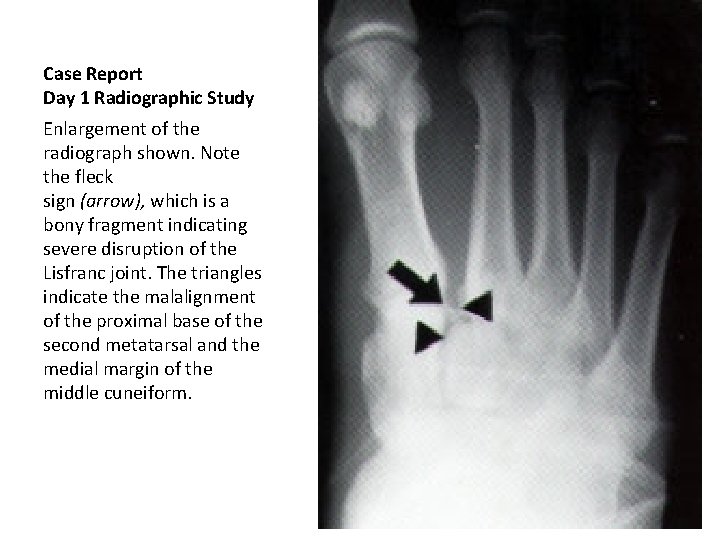
Case Report Day 1 Radiographic Study Enlargement of the radiograph shown. Note the fleck sign (arrow), which is a bony fragment indicating severe disruption of the Lisfranc joint. The triangles indicate the malalignment of the proximal base of the second metatarsal and the medial margin of the middle cuneiform.
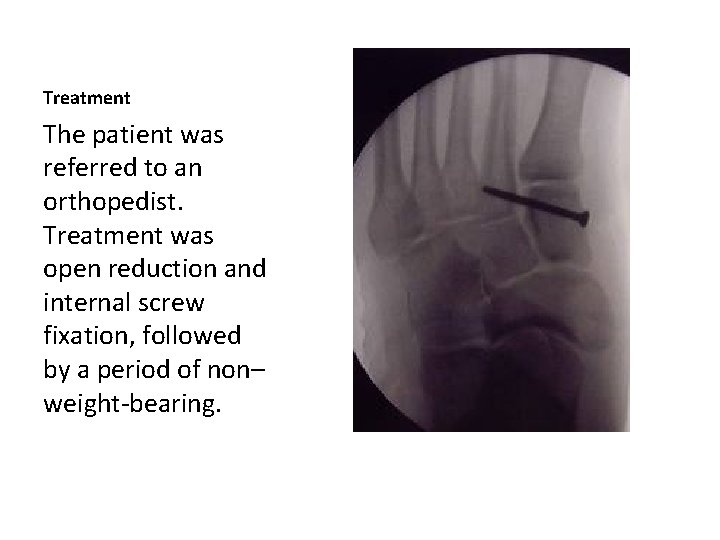
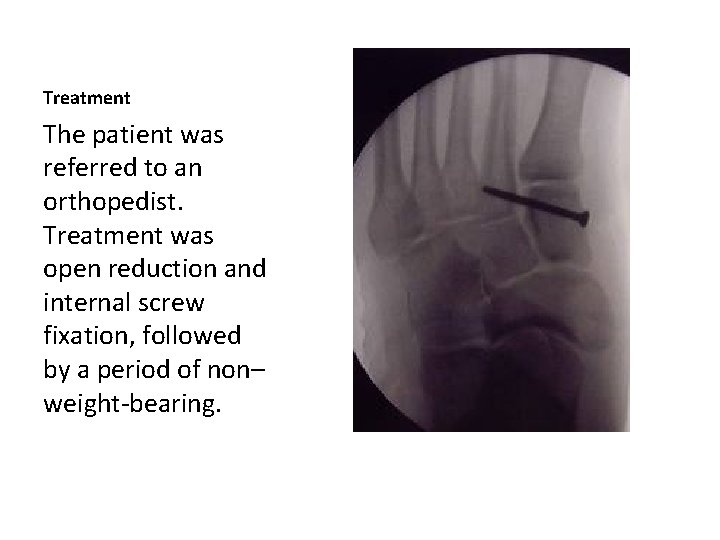
Treatment The patient was referred to an orthopedist. Treatment was open reduction and internal screw fixation, followed by a period of non– weight-bearing.
Lisfranc Injury • Can you name a baseball player who competed in the STL/Boston World Series with a Lisfranc injury? • https: //www. bing. com/videos/search? q=allen+craig+ba seball&&view=detail&mid=169 C 9 B 7165 AFFDE 22235169 C 9 B 7165 AFFDE 22235&&FORM=VRDGAR












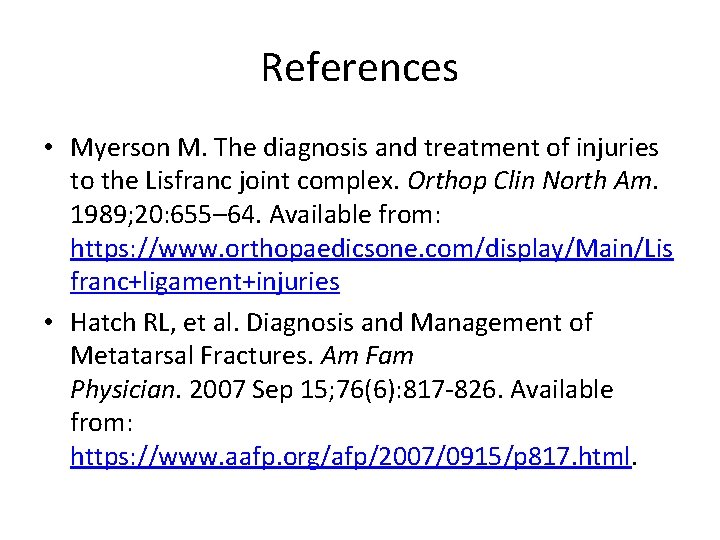
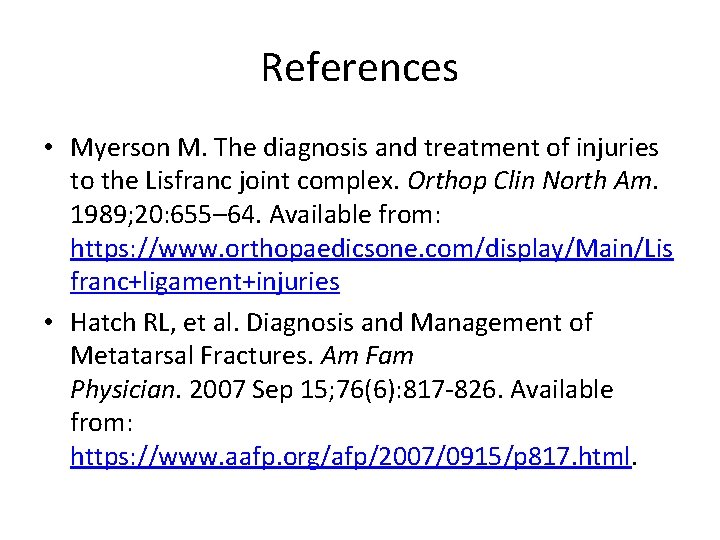
References • Myerson M. The diagnosis and treatment of injuries to the Lisfranc joint complex. Orthop Clin North Am. 1989; 20: 655– 64. Available from: https: //www. orthopaedicsone. com/display/Main/Lis franc+ligament+injuries • Hatch RL, et al. Diagnosis and Management of Metatarsal Fractures. Am Fam Physician. 2007 Sep 15; 76(6): 817 -826. Available from: https: //www. aafp. org/afp/2007/0915/p 817. html.
 How to protect yourself from intentional injuries
How to protect yourself from intentional injuries Piano key test foot
Piano key test foot Canal transversaire
Canal transversaire Boyd amputasyon nedir
Boyd amputasyon nedir Luxation spatulo columnaire
Luxation spatulo columnaire Tiroir antérieur cheville
Tiroir antérieur cheville Ligamento de lisfranc
Ligamento de lisfranc Luxation chopart
Luxation chopart Solving right triangles
Solving right triangles You put your right foot in
You put your right foot in Esterman visual field test dvla
Esterman visual field test dvla Missed connections arlington va
Missed connections arlington va Gsil missed punch form
Gsil missed punch form Gsil missed punch form
Gsil missed punch form Welcome back to school we missed you
Welcome back to school we missed you Romeo script
Romeo script We missed you welcome back
We missed you welcome back Kronos workforce timekeeper
Kronos workforce timekeeper Ebcap
Ebcap Romeo and juliet script oh romeo i've missed you
Romeo and juliet script oh romeo i've missed you Henry ford outlook mail
Henry ford outlook mail Before using a pneumatically powered
Before using a pneumatically powered Sodium hydroxide relaxers are commonly called
Sodium hydroxide relaxers are commonly called What are optical storage devices are most commonly known as
What are optical storage devices are most commonly known as Signing naturally 5:8
Signing naturally 5:8 Commonly misused homonyms
Commonly misused homonyms Paragraph narrative
Paragraph narrative Agaricus is commonly known as
Agaricus is commonly known as Multinational financial management an overview
Multinational financial management an overview History is the lie commonly agreed upon
History is the lie commonly agreed upon Section lining symbols
Section lining symbols What are poriferans
What are poriferans To vs too
To vs too A commonly cited hazard for stairways and or ladders is
A commonly cited hazard for stairways and or ladders is The circle graphs are commonly called
The circle graphs are commonly called Hydroxide relaxers
Hydroxide relaxers Hodgepodge jeopardy
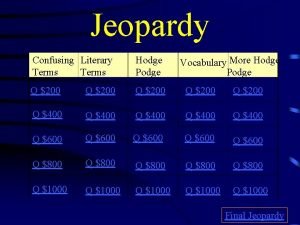
Hodgepodge jeopardy A collection of different websites
A collection of different websites Methods are commonly used to
Methods are commonly used to Computer graphics models are now commonly used for making
Computer graphics models are now commonly used for making Section 17-3 practice commonly abused drugs
Section 17-3 practice commonly abused drugs Homophones of week
Homophones of week Development of truncated cylinder
Development of truncated cylinder Commonly confused words paragraph
Commonly confused words paragraph List the commonly used wet hairstyling tools
List the commonly used wet hairstyling tools Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to Most commonly used system
Most commonly used system Friction clutch
Friction clutch A commonly cited hazard for stairways and or ladders is
A commonly cited hazard for stairways and or ladders is Technician a says that a hoist can be stopped
Technician a says that a hoist can be stopped Financial difficulties are commonly caused by overspending
Financial difficulties are commonly caused by overspending What effect might alcohol and other drug
What effect might alcohol and other drug Abused children commonly exhibit
Abused children commonly exhibit Kinds of hose appliances
Kinds of hose appliances Virtual memory is commonly implemented by
Virtual memory is commonly implemented by List three of the commonly used assembly constraints
List three of the commonly used assembly constraints Tư thế ngồi viết
Tư thế ngồi viết ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật