LINKING PEOPLE WITH ALZHEIMERS DISEASE AND OTHER DEMENTIAS












- Slides: 45
LINKING PEOPLE WITH ALZHEIMER’S DISEASE AND OTHER DEMENTIAS TO SUPPORT, INFORMATION AND OTHERS WHO CAN HELP Serving People with Dementia

FIRST LINK ™ A referral program that will: link people diagnosed with dementia to support, information and services that can help. assist caregivers of people with dementia by linking them to services as early as possible in the disease process.
BENEFITS FROM PARTICIPATING IN FIRST LINK ™ People with dementia will have increased health information enabling them to make informed decisions about their health care needs. People with dementia and their caregivers will have more information about dementia, health services and non-medical community services.
BENEFITS FROM PARTICIPATING IN FIRST LINK ™ Caregivers have will increased knowledge, skills and confidence. be encouraged to develop self care strategies.
FIRST LINK ™ REFERRAL RESOURCES To First Link ™ Referral by physicians and other health care professionals, diagnostic and treatment services and community service providers. Self referral by the person with dementia or their family.

FIRST LINK ™ REFERRAL RESOURCES To Other Services The Alzheimer Society will provide information about primary health and community-based non-medical services. Alzheimer Society services such as Safely Home™ - the Alzheimer Wandering Registry.

FIRST LINK ™ SUPPORT SERVICES The Alzheimer Society provides phone conversations personal appointments support groups for people with dementia caregivers – in person and distance telephone groups
FIRST LINK ™ INFORMATION SERVICES Alzheimer Society services include Print material Website Information sessions Caregiving: Building Your Team Caregiving with Confidence

is your link to Help for Today and Hope for Tomorrow Serving People with Dementia
CLICK TO EDIT MASTER Winnipeg Regional Health Authority (WRHA): GERIATRIC MENTAL HEALTH TEAMS

WHY CHANGE? Improve Access Reduce Duplication Develop linkages Improve system efficiency
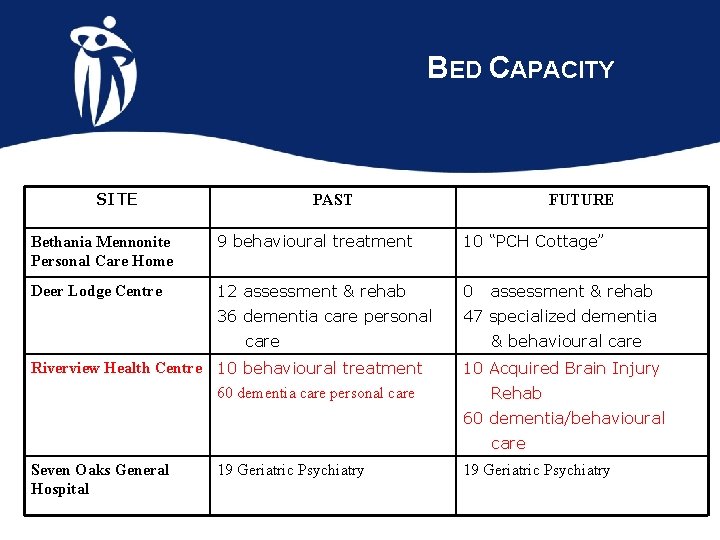
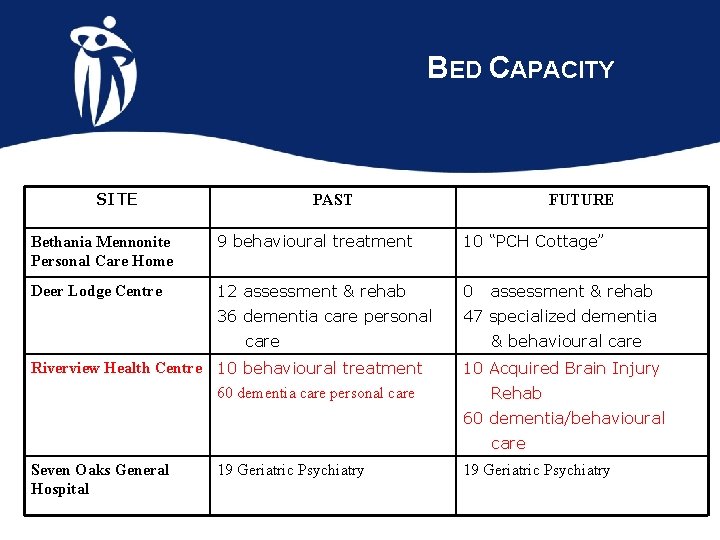
BED CAPACITY SITE PAST FUTURE Bethania Mennonite Personal Care Home 9 behavioural treatment 10 “PCH Cottage” Deer Lodge Centre 12 assessment & rehab 0 36 dementia care personal 47 specialized dementia care Riverview Health Centre 10 behavioural treatment 60 dementia care personal care assessment & rehab & behavioural care 10 Acquired Brain Injury Rehab 60 dementia/behavioural care Seven Oaks General Hospital 19 Geriatric Psychiatry
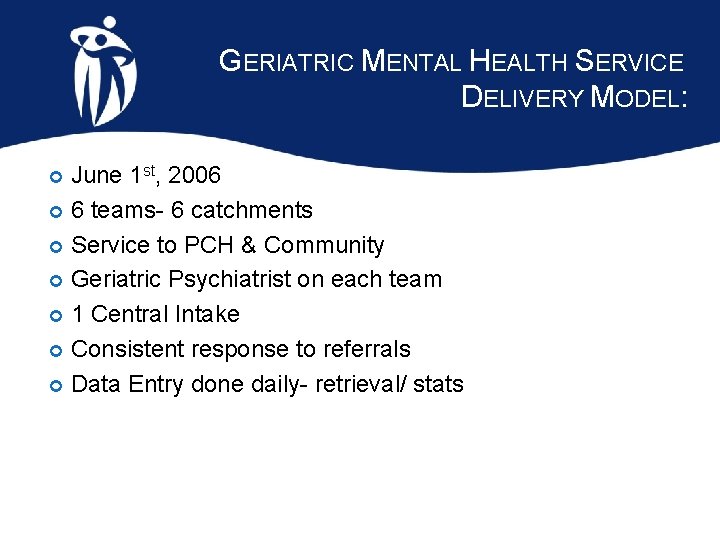
GERIATRIC MENTAL HEALTH SERVICE DELIVERY MODEL: June 1 st, 2006 6 teams- 6 catchments Service to PCH & Community Geriatric Psychiatrist on each team 1 Central Intake Consistent response to referrals Data Entry done daily- retrieval/ stats
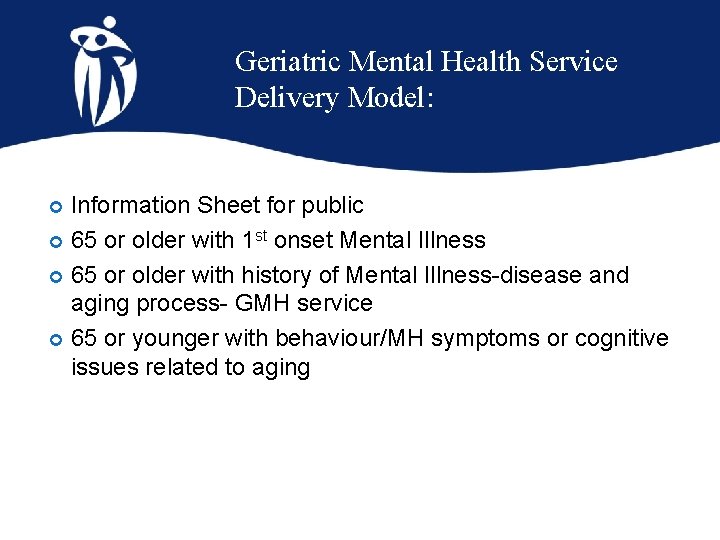
Geriatric Mental Health Service Delivery Model: Information Sheet for public 65 or older with 1 st onset Mental Illness 65 or older with history of Mental Illness-disease and aging process- GMH service 65 or younger with behaviour/MH symptoms or cognitive issues related to aging
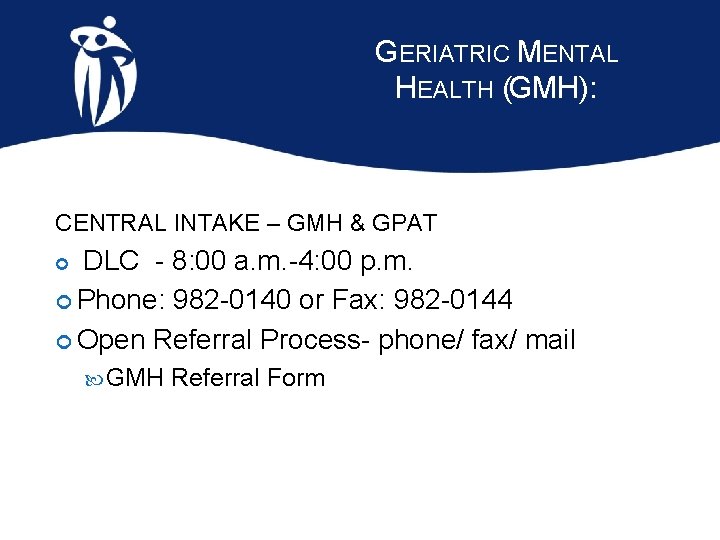
GERIATRIC MENTAL HEALTH (GMH): CENTRAL INTAKE – GMH & GPAT DLC - 8: 00 a. m. -4: 00 p. m. Phone: 982 -0140 or Fax: 982 -0144 Open Referral Process- phone/ fax/ mail GMH Referral Form
GMH Intake: Database Flag Based entry- if known to GMH or GPAT & eventually DH on client address- faxed to appropriate team the same day
GMH TEAMS: River East & Transcona (ARE) St. James-Assiniboia/Assiniboine South (DLC) River Heights/Fort Garry (RHC) St. Boniface/St. Vital (Tache) Inkster/Seven Oaks (1050 Leila) Point Douglas/Downtown (DLC) Each team consists of 2 clinicians + Geriatric Psychiatrist.
GMH SERVICE: Provide timely geriatric mental health assessment Recommendations (Geriatric Psych. ) Short-term intervention Connect with service to clients in the Community or recommend care in Personal Care Homes

RESPONSE TIMES: GOAL: Not a Crisis Response Team Non-Urgent – contact- 3 days, visit in 10 days Urgent – contact-1 day, visit in 3 days Clinician contact made to determine level of risk/ appropriate service & schedule appointment
WEEKLY TEAM REVIEWS: Team Reviews scheduled with Geriatric Psychiatrist -discussion of cases Care Planning/ problem-solving/ resources
CASE CLOSURE: when linked with services required when issues stabilized/ improve when admitted to hospital-not expected to return
WINNIPEG REGIONAL HEALTH AUTHORITY (WRHA): GERIATRIC PROGRAM ASSESSMENT TEAMS (GPAT):
GERIATRIC PROGRAM ASSESSMENT TEAMS (GPAT): • Outreach program within the WRHA Rehab & Geriatrics Program • • Developed in 1999 & modeled from Ottawa/Carlton Geriatric Outreach Teams Started with 2 teams of 3 clinicians in each team then grew to 5 teams of 3 clinicians by Sept. ‘ 99
GPAT (CONT’D) Each clinician receives 12 weeks of specialized geriatric training This enables each clinician to complete a medically based multidimensional assessment in the client’s home assessing the following: physical, functional, cognitive, emotional, psychosocial, mobility, GI/GU, safety, polypharmacy.
GPAT EMERGENCY ROOM (ER) INVOLVEMENT In Aug. ’ 04 ER Task force made recommendations about GPAT as follows: GPAT clinicians will have a standard approach in assessment process in all ER’s in Wpg. to improve care to geriatric clients GPAT clinicians will prioritize the ER in their caseload GPAT will refer directly to Home Care to decrease wait times for clients’ services in the community
GPAT RESPONSE TO ER TASK FORCE Restructured 5 teams to 6 to service 6 ER’s in Wpg. in mid Nov. ‘ 04 Researched database information on clients over age 65 in the community and in Personal Care Homes in 12 community areas Developed new catchment boundaries for 6 teams with no additional resources…some 2 & 3 person teams with Geriatrician

GERIATRIC PROGRAM ASSESSMENT TEAMS (GPAT): There are 6 teams across the city of Winnipeg Concordia Deer Lodge Center Health Science Center Riverview St. Boniface Seven Oaks Hospital Each Team consists of 2 -3 disciplines and a Geriatrician +. 6 float BN, BPT, BOT, BSW
GPAT: CONT’D After the clinician has completed the assessment they review with the Geriatrician and team. Clinicians will make referral to community resources & recommendations to family MD with geriatrician input.

GOALS To ensure the “right care, in the right place at the right time”. Maintain functional ability in their home Partner with community caregivers for management to prevent hospital admission (Home Care, Day Hospital, Age and Opportunity friendly visitor, CNIB)
GOALS (CONT’D) Facilitate the transfer of appropriate clients to geriatric medicine and rehab units. Assist in-patient teams with the discharge planning of complex, frail, elderly (ER). Provide care management/ follow-up, short term intervention
POPULATION SERVED The frailest, at-risk elderly, 65+ years. Complex health concerns affecting their ability to function. Geriatric Issues: mobility, ADL problems, Toileting, Confusion, Depression, Social Support, Medication problems
REFERRALS Open Referral Process: Anyone can refer to our service: Family member, friend, bank manager, Home Care, caregiver, & physicians, etc. To refer to GPAT, either call the Central Intake Line at 982 -0140 or fax Central Intake Form to 982 -0144.
CONTACTS: Marlene Graceffo, Rehab & Geriatrics Regional Manager 831 -2537 Lois Stewart-Archer, Geriatric Mental Health Regional CNS 831 -2179 Jill Moats, Rehab & Geriatrics Regional Educator 831 -2150
QUESTIONS

PRIME A Health Centre for Seniors
WHO DOES PRIME SERVE? Targets community-dwelling seniors who are: Not functioning well in the community At risk of institutionalization Wish to remain in the community
PRIME GOALS Maintain seniors in the community 2. Enhance care coordination and service delivery for the frail elderly 3. Personal care home placement 4. Hospital/Emergency use 1.
PRIME UMBRELLA OF CARE Case Manager Day Centre Primary Health Clinic After hours support Inpatient beds

DAY CENTRE Transportation Personal care/ grooming/ personal laundry Recreational and social activities Rehabilitation /exercises Health promotion activities Lunch meal
PRIMARY HEALTH CLINIC Transfer of care to PRIME physician Coordination of on-site & off-site appointments Medications provided weekly

AFTER HOURS SUPPORT Evening and weekend nurse Home visits and telephone response Provincial Health Contact Centre
FACILITATE ACCESS TO INPATIENT BEDS Treatment Intensive rehabilitation Emergency respite Assessment
PROGRAM MODEL & OUTCOMES Modelled on Edmonton CHOICE and U. S. A. PACE Edmonton CHOICE results: emergency visits reduced by 62. 9% inpatient days reduced by 70% ambulance claims reduced by 51. 5%
EDMONTON OUTCOMES (CONT’D) High participant & family satisfaction Maintained health status of participants Slowing of health decline Improved quality of life Support community living

PRIME A HEALTH CENTRE FOR SENIORS Judy Ahrens-Townsend Regional Manager Phone: 831 -2192 Email: jahrens@deerlodge. mb. ca
 Dynamic linking vs static linking
Dynamic linking vs static linking Bharathi viswanathan
Bharathi viswanathan Georgia alzheimers planning
Georgia alzheimers planning Fast score dementia
Fast score dementia Alzheimers sjukdom
Alzheimers sjukdom Alzheimers nz conference 2020
Alzheimers nz conference 2020 Site:slidetodoc.com
Site:slidetodoc.com Alzheimers society contented dementia
Alzheimers society contented dementia Alzheimers eye test joke
Alzheimers eye test joke Example of people as media
Example of people as media Respect people's time
Respect people's time 10 commandments of netiquette
10 commandments of netiquette Written and other recorded events of people
Written and other recorded events of people Respect other people's time and bandwidth
Respect other people's time and bandwidth What is internet etiquettes
What is internet etiquettes Other initiated other repair
Other initiated other repair People killin people dyin
People killin people dyin Other people matter mindset
Other people matter mindset Don't be a busybody in other people's matters
Don't be a busybody in other people's matters History contributes to moral understanding.
History contributes to moral understanding. Other people matter
Other people matter 10 commandments computer ethics
10 commandments computer ethics Linking helping and action verbs
Linking helping and action verbs Recovery community
Recovery community People just people
People just people Relocation and linking concepts
Relocation and linking concepts Linking verbs list
Linking verbs list Explain object linking and embedding
Explain object linking and embedding Explain machine independent loader features in detail
Explain machine independent loader features in detail Linking east and west
Linking east and west Linking words for advantage and disadvantage essay
Linking words for advantage and disadvantage essay Transitive intransitive and linking verbs
Transitive intransitive and linking verbs Linking loader and linkage editor
Linking loader and linkage editor Linking sales and distribution management
Linking sales and distribution management Market driven strategies
Market driven strategies What is linking and loading
What is linking and loading Possessives are
Possessives are Main verbs
Main verbs Linking words argumentation
Linking words argumentation Opinion essay ecpe
Opinion essay ecpe Excel cannot use object linking and embedding
Excel cannot use object linking and embedding Linking and intrusive r
Linking and intrusive r Is are a linking verb
Is are a linking verb Diagramming predicate adjectives
Diagramming predicate adjectives What follows a linking verb
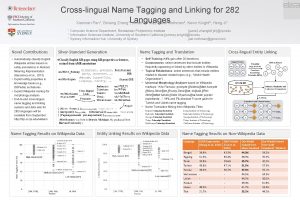
What follows a linking verb Cross-lingual name tagging and linking for 282 languages
Cross-lingual name tagging and linking for 282 languages