Limb Girdle Muscular Dystrophy LGMD Autosomal dominant type
Limb Girdle Muscular Dystrophy LGMD -Autosomal dominant (type 1) or autosomal recessive ( type 2) inheritance. -The onset ranging from late of the first decade to the fourth decade. -Progressive weakness of pelvic and shoulder girdle musculature , Gower's sign positive.
- Respiratory insufficiency from weakness of the diaphragm, and cardiomyopathy may occurs also. - Serum CK level less elevated than in the Duchenne's muscle dystrophy - EMG shows myopathic pattern.

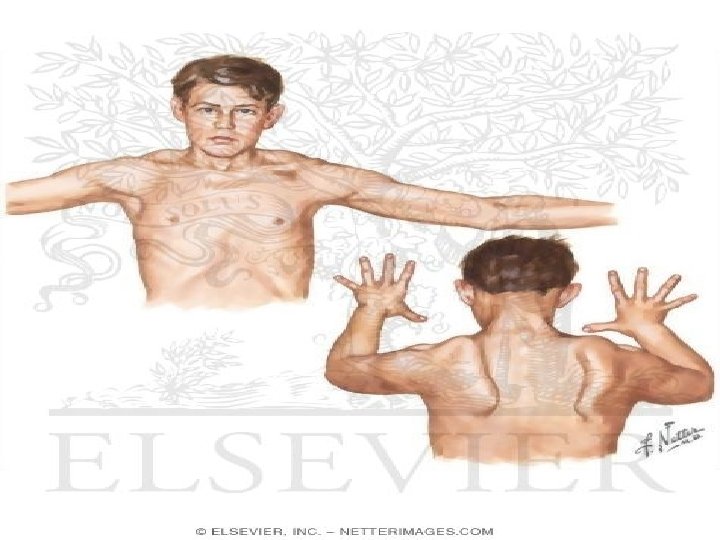
Facioscapulohumeral (FSH ) Muscular Dystrophy -Autosomal dominant -The onset in the childhood or young adulthood. -Facial weakness appear as an inability to smile, whistle or fully close the eyes. -Weakness of shoulder girdles which is usually brings the patient to medical attention.
• loss of scapular stabilizer muscles make arm elevation difficult and scapular winging become apparent with attempts to abduction and forward movement of the arms. • Biceps and triceps muscles severely affected with relative sparing of the deltoid muscle.
- 20 % of patient the weakness progresses to involve the pelvic girdle muscles -Serum CK level may be normal or mildly elevated - EMG indicates myopathic pattern • Treatment No specific treatment is available
Ocular Dystrophy -Typically autosomal dominant, Autosomal recessive and sporadic cases also occur - Onset before the age of - Ptosis is the earliest 30 years manifestation - Progressive external ophthalmoplegia - Facial muscle weakness also common - Subclinical involvement of limb muscle may occur
Oculopharyngeal Dystrophy - Autosomal dominant. - The onset in the third to fifth decade. - Ptosis, total external ophthalmoplegia. - Dysphagia , facial weakness and often proximal muscle weakness. - Serum CK is mildly elevated. - Dysphagia may require nasogastric tube or by
Distal Myopathy - Autosomal dominant, autosomal recessive or sporadic. - Onset after age of 40 years. - Small muscles of hand feet , wrist extensor and dorsiflexor of feet are affected.
Emery – Dreifuss Muscular Dystrophy -X- linked recessive , mutation in emerin gene. - Onset from childhood to late adolescence or adulthood. -Weakness affect first the upper arm and pectoral girdle muscles later pelvic girdle and distal muscles in lower extremities.
-The distinguishing feature is the early appearance of contractures in the flexors of elbow , extensor of the neck , and calf muscles. Facial muscles are affected occasionally - Severe cardiomyopathy with variable sinoaterial and aterioventricular conduction defects.

Myotonia Abnormality of muscle fiber membrane leading to marked delay of relaxation after contraction causing apparent muscle stiffness. ▪On examination -Difficulty in relaxing the hand after sustained grip.
- Persistent contraction after percussion of the belly of the muscle. - EMG show characteristic high-frequency discharge of potential that wax and wane in amplitude and frequency.


Myotonic Dystrophy -Autosomal dominant. -The onset in the third or fourth decade and may appear in early childhood. -Hatchet-face appearance due to facial muscle atrophy and weakness. -Frontal baldness. -sternocliedomastoids and distal limb muscle are involved early.

- Weakness of wrist extensors. - Finger extensor and intrinsic hand muscle impair function. -Ankle dorsiflexor weakness may cause footdrop - Palatal, pharyngeal and tongue involvement produce dysartheric speech and swallowing problems. - Cataract, Diabetes mellitus, testicular atrophy, cardiac and intellectual defect.

Treatment Is treatment of myotonia by Quinine sulphate 300 mg-400 mg tds or procainamide 0. 5 -1 g/qd or phenytoin 100 mg tds
Myotonia congenita 1 -Autosomal dominant ((thomsen's disease)) mutation in chromosome 7. -Generalized myotonia , the symptoms may not appear until early childhood -Muscle stiffness enhanced by cold and inactivity, relieved by exercise. -Muscle hypertrophy pronounced sometime


2 -Autosomal recessive form Later onset, slight weakness, and atrophy of distal muscle. Treatment Is treatment of myotonia.

Metabolic Myopathy Osteomalacia: characterized by proximal muscle weakness with bone pain and tenderness mild decrease in serum ca++ and increased ALK phosphatase. Treatment with vit D Acute or chronic hypo or hyperkalemia leading to proximal muscle weakness reversed by correcting the metabolic disturbances.
Periodic Paralysis Syndromes May be familial, autosomal dominant. -Episodes of flaccid weakness or paralysis. -The power is normal between the attacks. Hypokalemic periodic paralysis - Occurs at adolescence - Men are affected more than women because of decrease penetrance in women
-It may associated with thyrotoxicosis -The attacks provoked by meals high in carbohydrate or sodium or after prolong exercise -Weakness usually affect proximal limbs muscles more than distal muscles -Ocular and bulbar muscles are less likely to be affected -Respiratory muscles are usually spared but when involved may be fatal
-Life threatening cardiac arrhythmias related to hypokalemia may occur during the attack. -The weakness may take as long as 24 hours to resolve. Diagnosis of Hypo KPP -A low serum potassium level during an attack with excluding secondary causes establish the diagnosis.
-Interattacks muscle biopsies show the presence of single or multiple centrally placed vacuoles or tubular aggregates. -EMG shows electrical silence in severely weak muscle. Treatment of Hypo KPP -The acute paralysis improve by oral KCL (0. 2 -0. 4 mmol/kg) should be given every 30 min. -Only rarely is IV therapy necessary (e. g. swallowing problem or vomiting).
And mannitol is preferred vehical for administration of IV potassium. Prophylaxis -low carbohydrate, low-sodium diet and avoid intense exercise. -Acetazolamide (125 -1000 mg/day) in divided doses by beneficial effect of metabolic acidosis. -If weakness persist oral KCL should be added.
-Spironolactone (25 -100 mg/day) may be used. -Thyrotoxicosis if present should be treated also.
Hyperkalemic Periodic Paralysis (Hyper KPP) -The attacks of weakness are precipitated by potassium administration is the best definition of the disease ((the patients are often normokalemic during attacks )). -The onset is in the first decade. -The attacks brief and mild lasting 30 min to 4 hours.
-Some times associated with myotonia without weakness but the muscle stiff, painful aggravated by cold. Diagnosis of Hyper KPP -Serum potassium may be slightly elevated but mal during the attack. -Muscle biopsy shows vacuole that are smaller, less numerous and more peripheral than in the Hypo KPP.
Treatment of Hyper KPP Treatment of acute attack by calcium Gluconat IV, diuretics ((furosemide 20 -40 mg)) or Glucose IV fluid. Prevention Acetazolamide or chlorothiazide. mexiletine may be helpful in patient with significant myotonia.
Normokalemic Periodic Paralysis Affected patients are sensitive to K ingestion and have episodes of mild weakness that occur without any change in serum K. Treatment of normo KPP Treatment with large dose of Na alleviate the weakness.

Inflammatory myopathy Polymyositis and Dermatomyositis Characterized by distruction of muscle fibers and inflammatory cells infiltration of the muscles. - occur at any age. - low grade fever, muscle pain, tenderness and wasting affect proximal limb and girdle muscles.
Arthralgia , malaise , weight loss respiratory difficulties. , dysphagia, - Raynaud phenomena may occur. - In dermatomyositis there is erythematous rash around the eyes and eyelids ((heliotrop rash)) May be associated with autoimmune diseases e. g. scleroderma, SLE and Rh artheritis. - In adult it may associated with cancer. -Serum CK level elevated, if normal dont exclude the diagnosis. -EMG shows myopathic pattern.

Treatment With steroid prednisolone 60 -80 mg/day and when improvement occur and CK decreased the dose of prednisolone decrease to 10 -20 mg/day for 2 -3 years; azathioprine or methotrexate used in steroid resistant patient.
Polymyalgia Rhumatica -More in women above 50 years. -Muscles pain and stiffness about the neck and girdle muscles. -Headache, Anorexia, weight loss and low grade fever. -Serious complication may occur such as Giant cell arteritis. -Raised ESR. -Enzyme, EMG and muscle biopsy are normal.
Treatment Prednisolone 10 -15 mg/d for one year. Endocrine myopathy - hyper or hypothyroidism. - Hyper or hypoparathyroidism. - Hyper or hypoadrenalism. - Hypopituitarism. - Acromegaly.
Drug induced myopathy - Steroid - Chloroquine - Clofibrate - B-Blockers - Colchicine - Zidovudine
- Slides: 41