Life Flight Command Physician Orientation Aircraft Five EC145



- Slides: 37

Life. Flight Command Physician Orientation
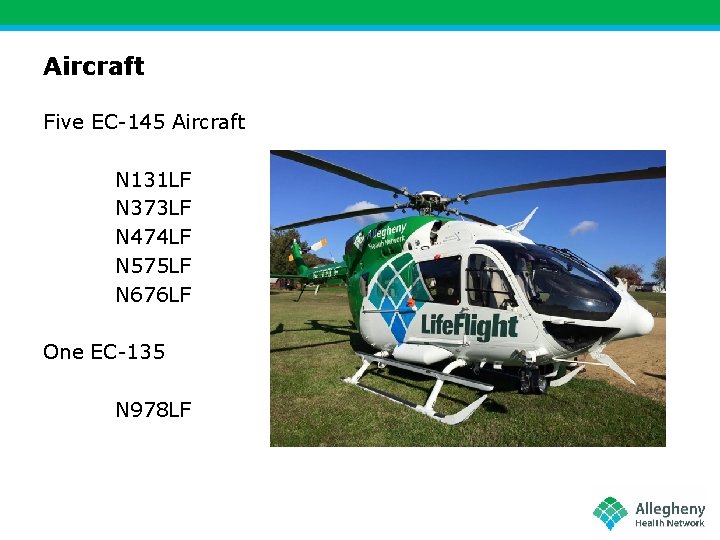
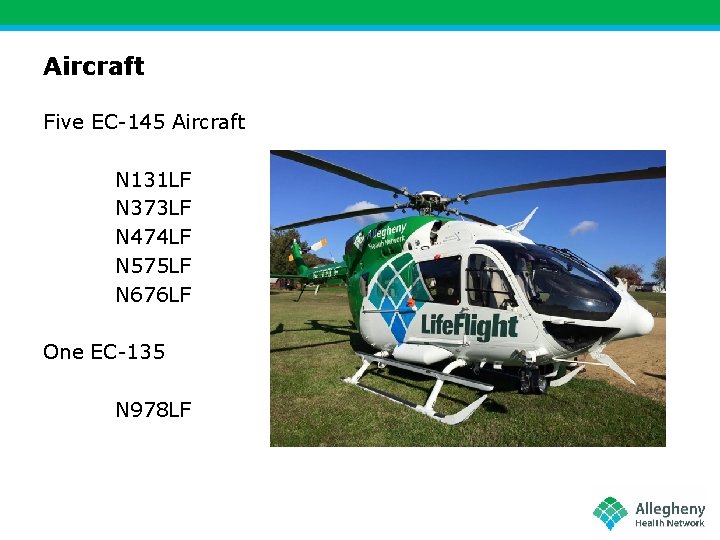
Aircraft Five EC-145 Aircraft N 131 LF N 373 LF N 474 LF N 575 LF N 676 LF One EC-135 N 978 LF
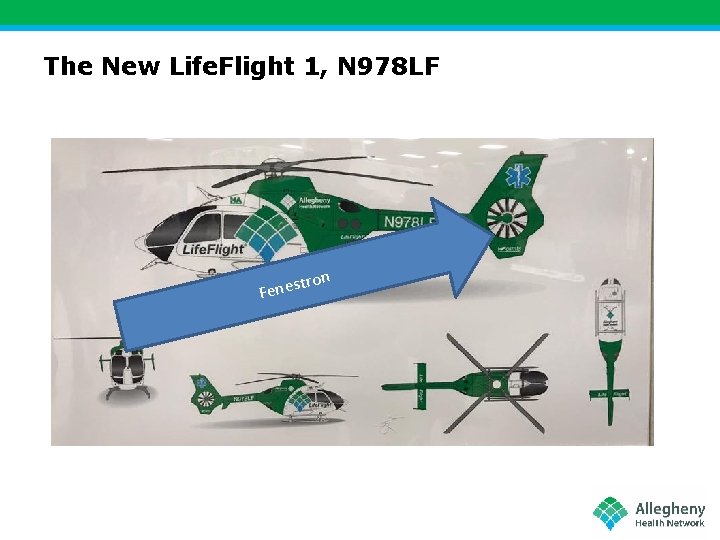
The New Life. Flight 1, N 978 LF n tro Fenes

Life. Flight added a new Helicopter, based at Clarion Hospital
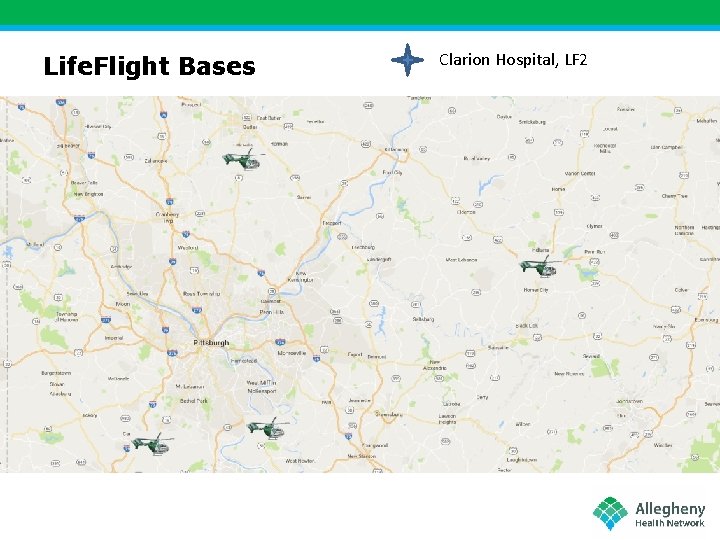
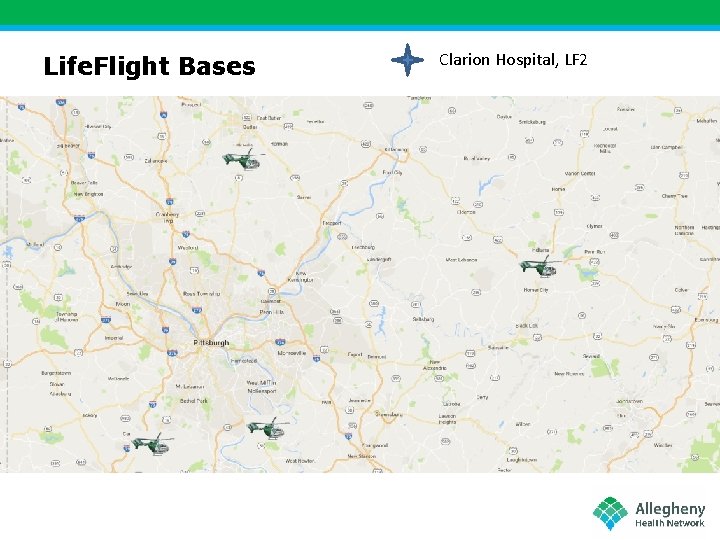
Life. Flight Bases Clarion Hospital, LF 2
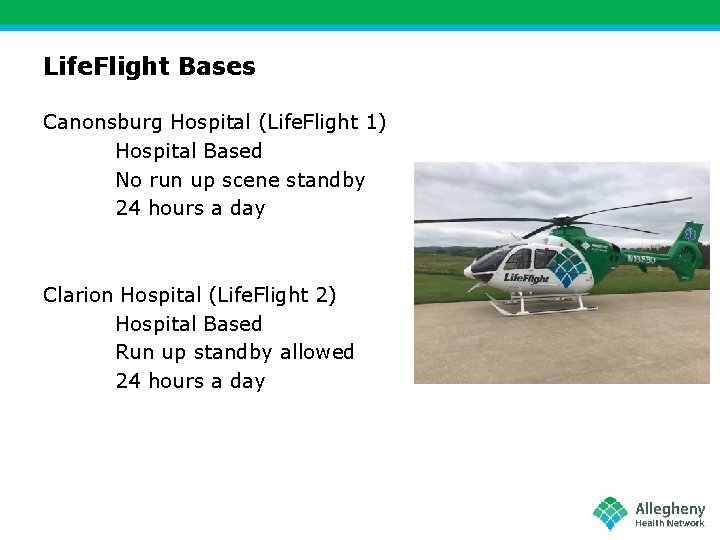
Life. Flight Bases Canonsburg Hospital (Life. Flight 1) Hospital Based No run up scene standby 24 hours a day Clarion Hospital (Life. Flight 2) Hospital Based Run up standby allowed 24 hours a day
Life. Flight Bases Indiana Regional Medical Center (Life. Flight 3) Hospital Based No run up scene standby 16 Hours a day (7 a-11 p)
Life. Flight Bases Rostraver Airport (Life. Flight 5) Airport Based Run up scene standby allowed 24 hours Butler Airport (Life. Flight 4) Airport Based Run up scene standby allowed 24 hours
Specialty Flights NICU Flights These flights will require one LF nurse and a NICU team. The aircraft will repo to West Penn Hospital prior to the destination to pick up the NICU team. No report is necessary to the NICU team. ECMO Flights These flights will require two LF Clinical Team and a perfusionist. The aircraft will repo to AGH prior to the destination to pick up the perfusionist. Report will be given to the team as usual. Be sure to include ECMO information.
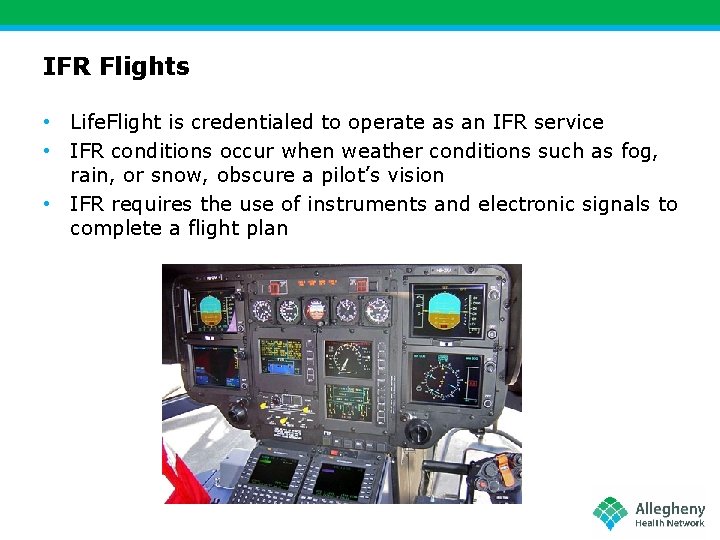
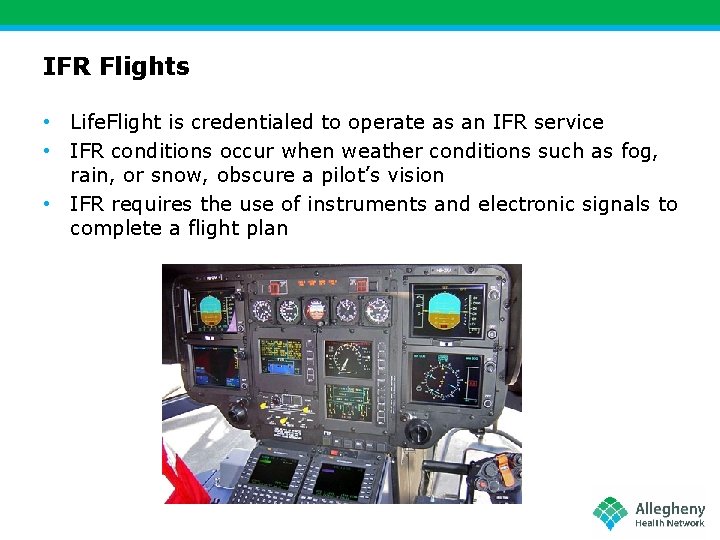
IFR Flights • Life. Flight is credentialed to operate as an IFR service • IFR conditions occur when weather conditions such as fog, rain, or snow, obscure a pilot’s vision • IFR requires the use of instruments and electronic signals to complete a flight plan
IFR Flights Each aircraft is equipped to complete Instrument Flight Rule flights. This will be decided by the Pilot and the Operational Control Center at Metro Aviation. This will add approximately 15 – 30 minutes to each flight. The referring facility needs to be informed of this time delay. If an aircraft is going by IFR, dispatch will update of the command physician with any changes.
Ground Transports If the weather is severe and IFR is not possible the crew can completed Critical Care Ground Transports. If this occurs dispatch will request an ambulance to meet the crew at their base and take them to their destination. Report will be given via telephone to the flight crew. Life. Flight Medical Command Record still needs to be completed.
Scene Flights Life. Flight like any EMS agency can be dispatched to a scene. This will require no report from you. The crew will be activated by the 911 center and they will respond. The crew when enroute to a hospital will call with an update. This is similar to how ground EMS completes trips. If they are heading to a AHN facility LF dispatch will be given an update. If they are heading to UPMC, Pittsburgh Medic Command will be given the update. Scene flights still require a Life. Flight Medical Command Record. *** Limited information will be obtained from scene flights***
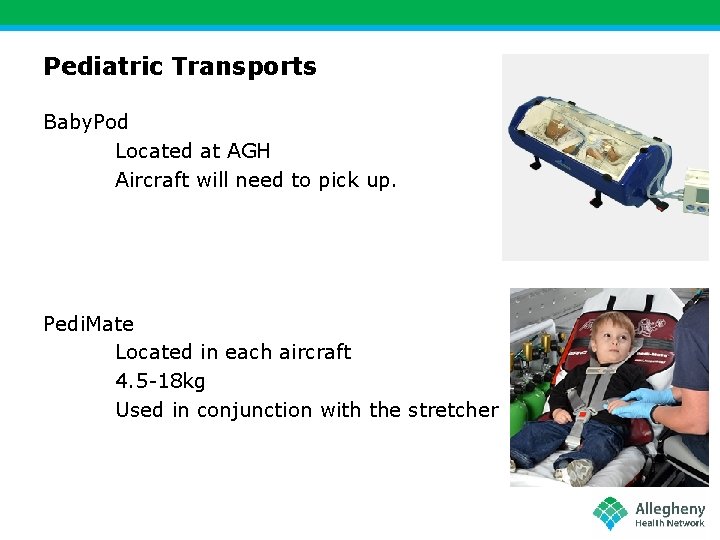
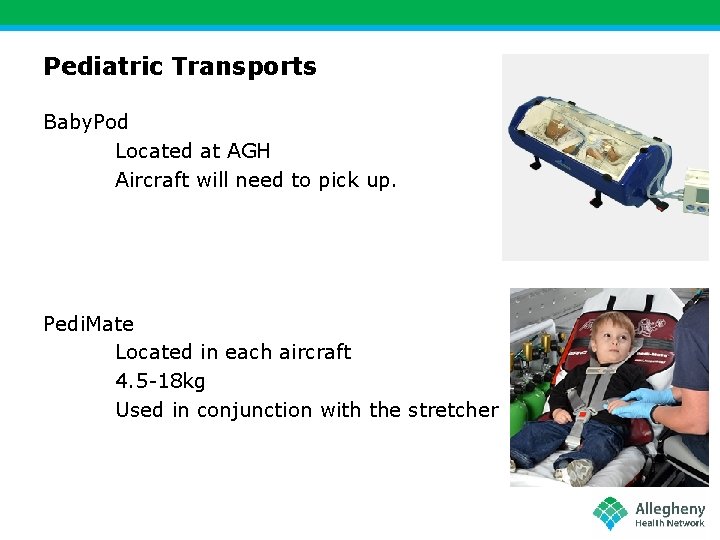
Pediatric Transports Baby. Pod Located at AGH Aircraft will need to pick up. Pedi. Mate Located in each aircraft 4. 5 -18 kg Used in conjunction with the stretcher
Pediatric Flights Car Seat Provided by EMS/Parents Can be secured to stretcher Can be used for patient regardless of size Cannot be used if vehicle is involved in an accident Stretcher Appropriate for patients > 18 kg
Life. Flight Radios Med Channel 6 Most frequently used frequency Does not produce tones on handset when transmitting Westmoreland 800 Radio Used when aircraft are at greater distances Tone will sound when transmitting a signal
Radio Operation NO NAMES OVER THE RADIO Pick up the handset of the designated radio Depress the button on the handset 800 will produce a tone when button is depressed Med Channel 6 will not produce a tone. (wait one second before transmitting) Give Report via instructions
Medical Command Report Use radio designated by Life. Flight Dispatch AGE SEX WT ALLERGIES DIAGNOSIS/REASON FOR TRANSPORT PMH HPI *** PAUSE FOR 1 -2 SECONDS *** Release the radio button when pausing
Medical Command Report VITAL SIGNS TEMP BP PULSE RHYTHYM / MONITOR RESP O 2 SATURATION *** PAUSE FOR 1 -2 SECONDS *** Release the radio button when pausing
Medical Command Report MEDICATED DRIPS (Be mindful LF can manage 6 IV medications on three pumps. You made need to recommend discontinuation of drips if greater than four. ) INTUBATED (tube size, depth) VENT SETTINGS (If applicable) IV ACCESS AND LOCATION ARTERIAL LINES(If applicable) PACEMAKER (If Applicable) VAD (If applicable) Continued…
Medical Command Report Intra-Aortic Balloon Pump (If applicable) Brand Settings ( 1: 1, 1: 2, 1: 3) Insertion location (Anatomic Site) Fiber optic or analog ECMO (If applicable) V/A, V/V Location Blood needed for transport (These flights will require a pickup of a perfusionist for transport) Impella (If applicable) 2. 5 or 5. 0 Site (These flights will require pickup of special equipment at times)
Medical Command Report The Medical Command Report is in exactly the same order as your Life. Flight Medical Command Record. Feel free to read off of the Command Record while transmitting to the crew.
Documentation You will be required to fill out a Life. Flight Medical Command Record for every flight or ground transport the LF Flight Crew complete.
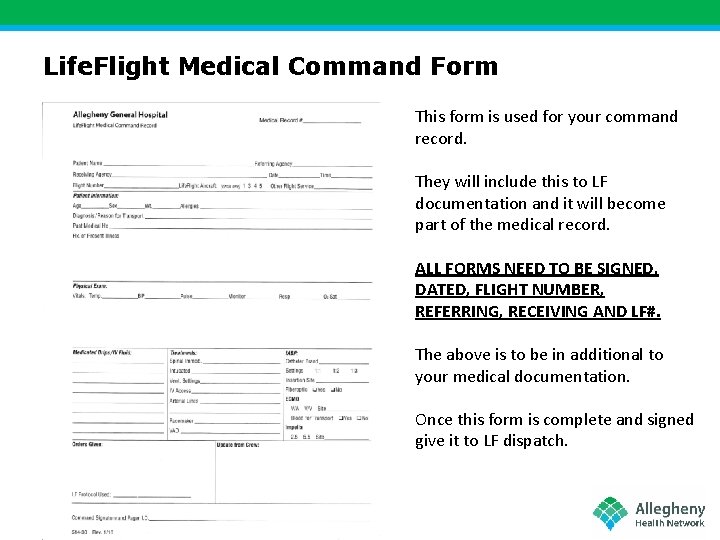
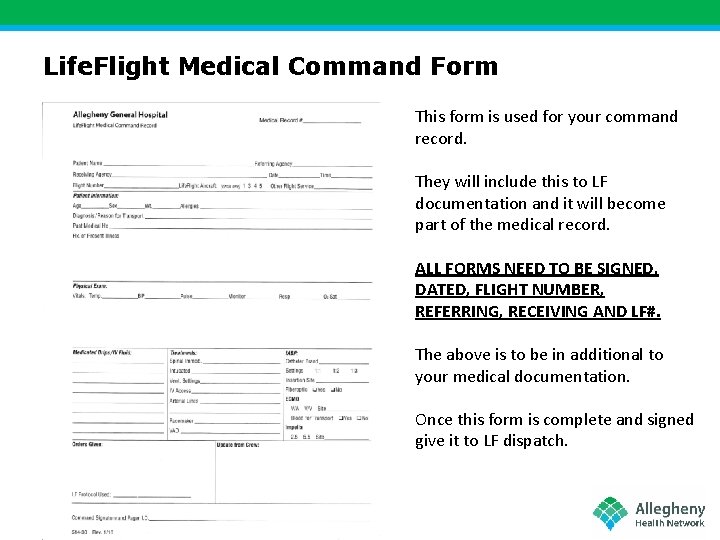
Life. Flight Medical Command Form This form is used for your command record. They will include this to LF documentation and it will become part of the medical record. ALL FORMS NEED TO BE SIGNED, DATED, FLIGHT NUMBER, REFERRING, RECEIVING AND LF#. The above is to be in additional to your medical documentation. Once this form is complete and signed give it to LF dispatch.
Life. Flight DNR Policy • If a patient needs to be transported and has a DNR, the referring facility, POA, patient, and crew, need to review the particulars of transport • Some patients desire maximal medical care but do not want intubation • Ideally, patient transports involving a DNR will be discussed prior to flight/mission acceptance • This discussion is NOT the responsibility of the LF crew.
Medical Command Physician Resources • Current Life. Flight protocols • Attending emergency physicians • The Life. Flight crew • Medical directors
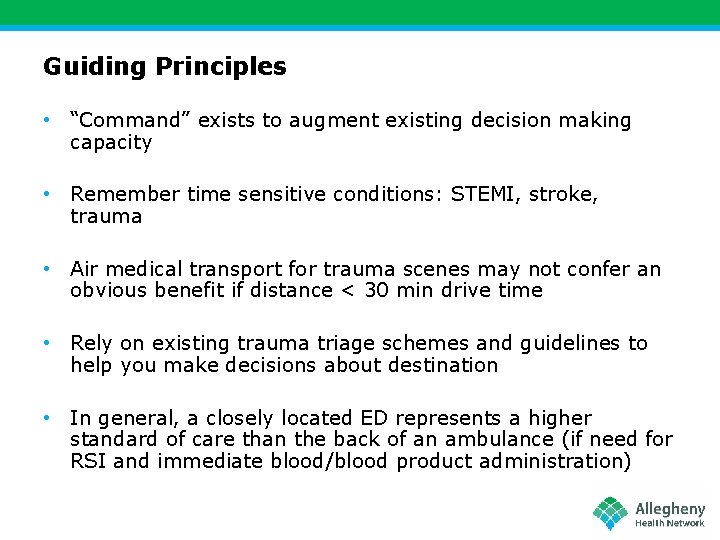
Medical Command Scenarios
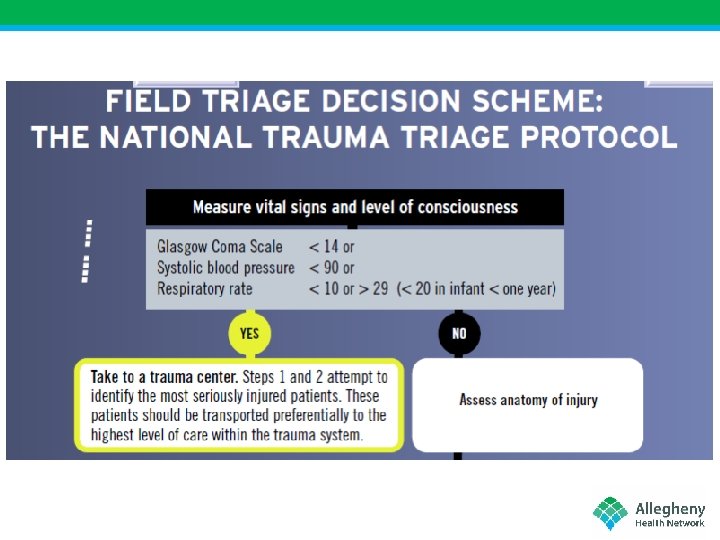
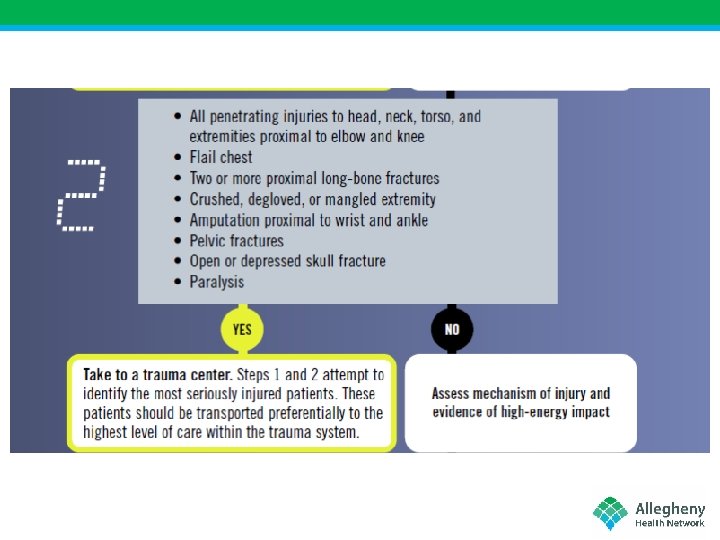
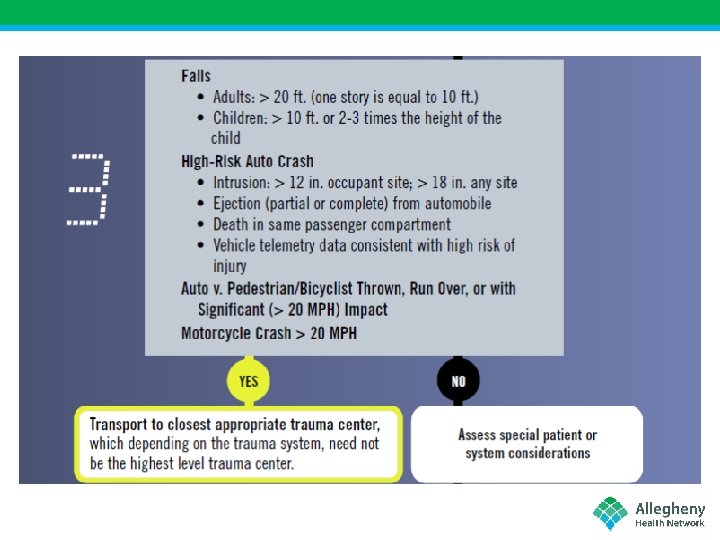
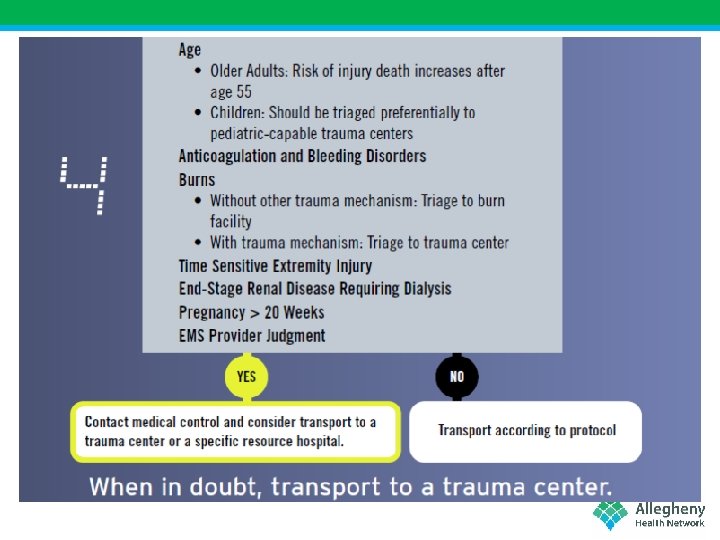
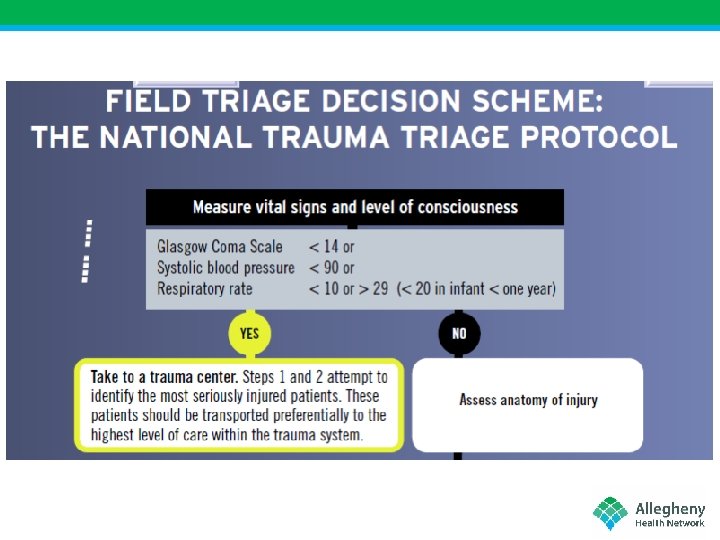
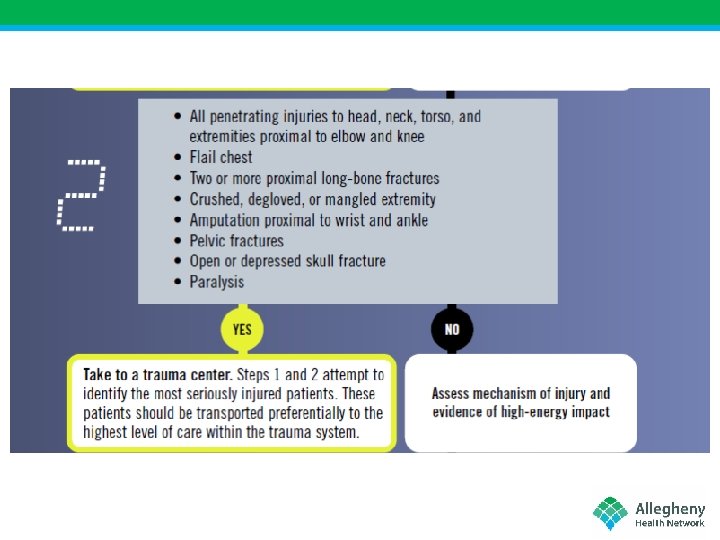
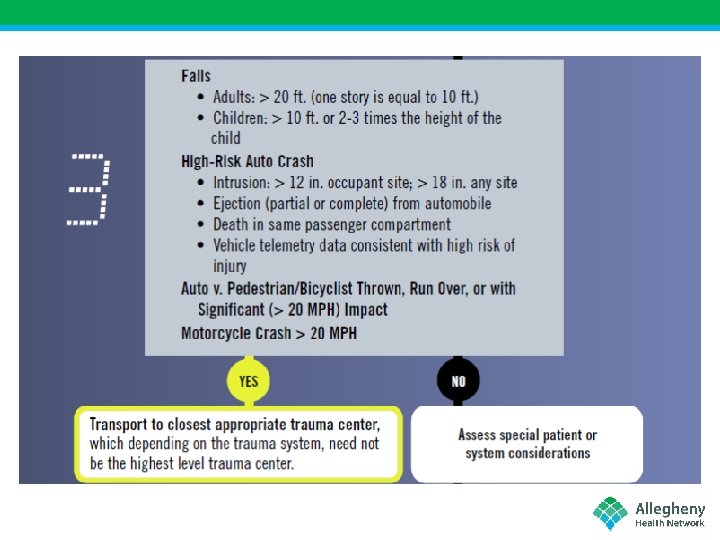
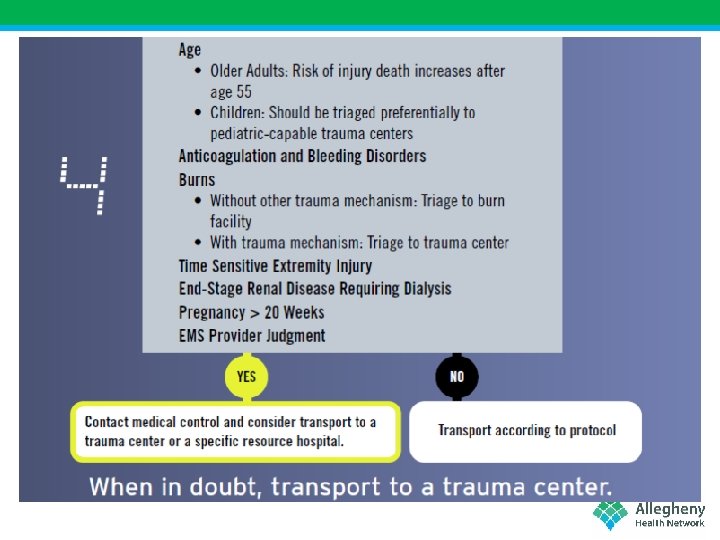
Guiding Principles • “Command” exists to augment existing decision making capacity • Remember time sensitive conditions: STEMI, stroke, trauma • Air medical transport for trauma scenes may not confer an obvious benefit if distance < 30 min drive time • Rely on existing trauma triage schemes and guidelines to help you make decisions about destination • In general, a closely located ED represents a higher standard of care than the back of an ambulance (if need for RSI and immediate blood/blood product administration)
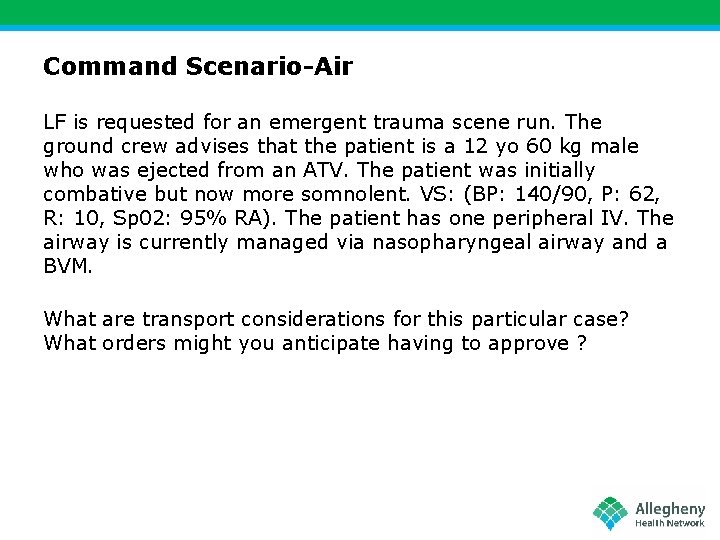
Command Scenario-Air LF is requested for an emergent trauma scene run. The ground crew advises that the patient is a 12 yo 60 kg male who was ejected from an ATV. The patient was initially combative but now more somnolent. VS: (BP: 140/90, P: 62, R: 10, Sp 02: 95% RA). The patient has one peripheral IV. The airway is currently managed via nasopharyngeal airway and a BVM. What are transport considerations for this particular case? What orders might you anticipate having to approve ?
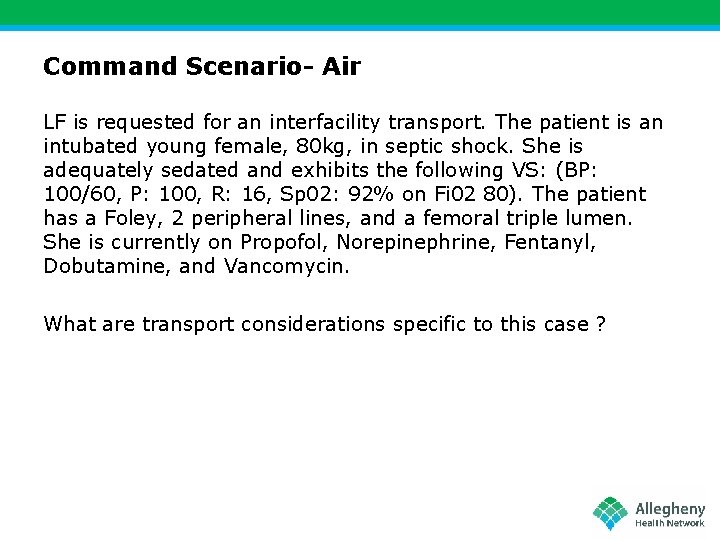
Command Scenario- Air LF is requested for an interfacility transport. The patient is an intubated young female, 80 kg, in septic shock. She is adequately sedated and exhibits the following VS: (BP: 100/60, P: 100, R: 16, Sp 02: 92% on Fi 02 80). The patient has a Foley, 2 peripheral lines, and a femoral triple lumen. She is currently on Propofol, Norepinephrine, Fentanyl, Dobutamine, and Vancomycin. What are transport considerations specific to this case ?
Command Scenario- Ground Patient was found unconscious and unresponsive. Initial vitals revealed BP: 180/90, R: 3/assisted, P: 110. Sp 02 was 90 and assisted with BVM. EMS crews administer a total of 2 mg naloxone. Patient is now awake, alert, combative, and vehemently refusing EMS cannot obtain vitals and calls command to “authorize” refusal. What are transport considerations specific to this case ? What would you tell EMS crews ?
Command Scenario- Ground CPR is in progress for a patient found hanging from a clothes belt. After several rounds of CPR, providers detect the presence of a peripheral pulse. The patient exhibits trismus and agonal respirations. An ALS crew is on-scene and cannot effectively ventilate the patient. Vitals: BP: 80/P, P: 120, R: 18 and assisted. Sp 02: 92%. Physical exam reveals trismus and no other trauma. The crew is 20 minutes from a local hospital. Life. Flight 5 (Dr. Poremba quickly checks his phone and uplinks to the LF dispatch cloud) is on the pad. EMS calls you to request aviation and asks if there’s “anything else” they should do.

Questions/Comments Feel free to contact us with any questions or concerns. Dr. Matthew Poremba Matthew. Poremba@ahn. org Cell: 412 -228 -7813 Dr. Ben Lawner blawner@ahn-emp. com Cell: 954 -829 -1367