Lessons Learned from the 2019 Washington State Measles


- Slides: 41

Lessons Learned from the 2019 Washington State Measles Outbreaks Kevin Wickersham, MS Washington State Department of Health
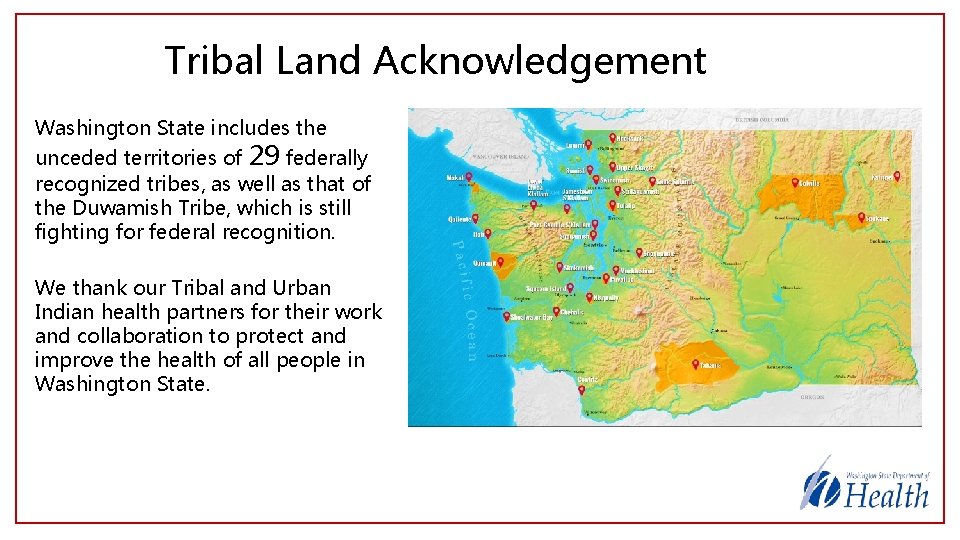
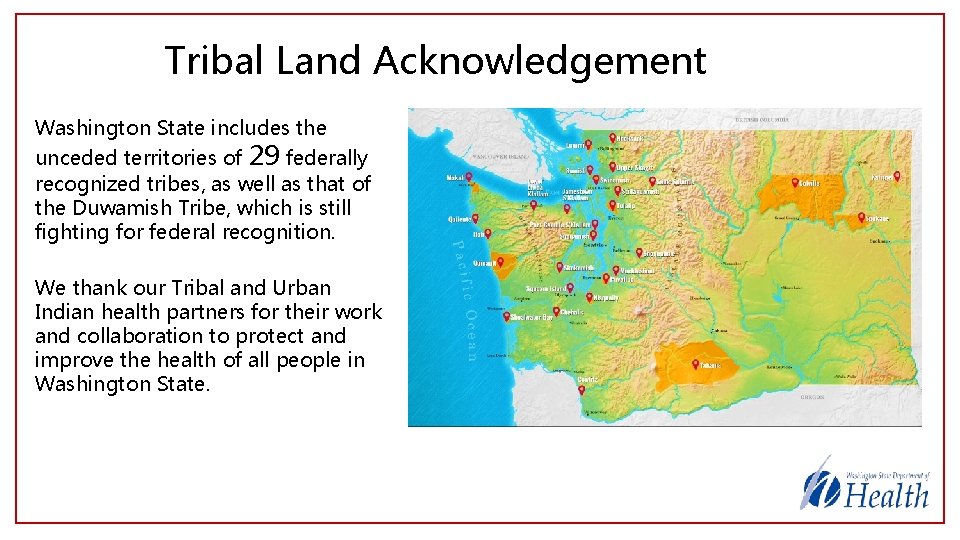
Tribal Land Acknowledgement Washington State includes the unceded territories of 29 federally recognized tribes, as well as that of the Duwamish Tribe, which is still fighting for federal recognition. We thank our Tribal and Urban Indian health partners for their work and collaboration to protect and improve the health of all people in Washington State.
Objectives • Discuss the background of the 2 measles outbreaks in WA in 2019 • Overview the strengths of the responses which led to successful outbreak control • Discuss challenges faced in these responses and planned improvement actions • Describe strategies used to develop improved systems for the management of future measles outbreaks • Throughout the presentation, “Key Takeaways” are highlighted with a key icon
Limitations • These events were highly complex with many novel factors • Each involved huge multiagency responses • The presentation will remain fairly high level • Discussion of some matters will be limited to protect individual privacy
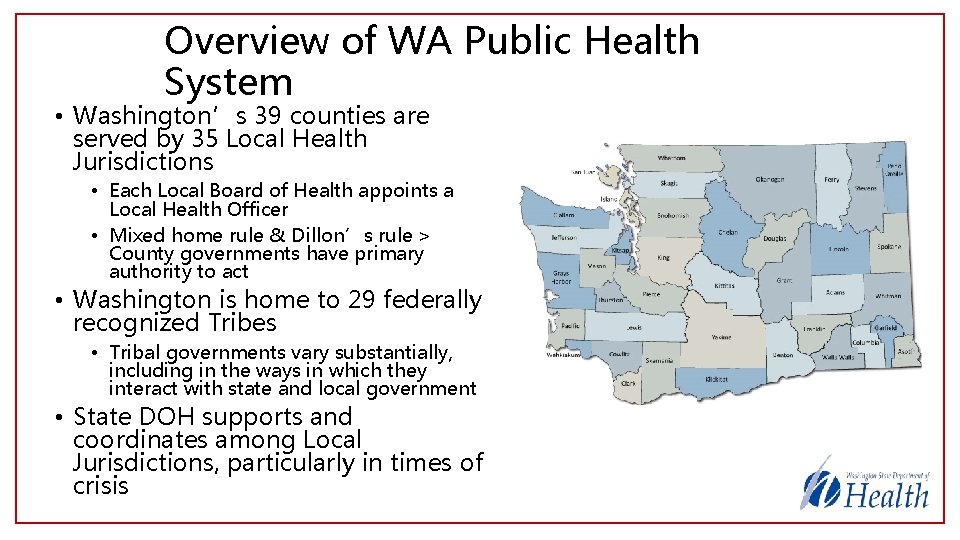
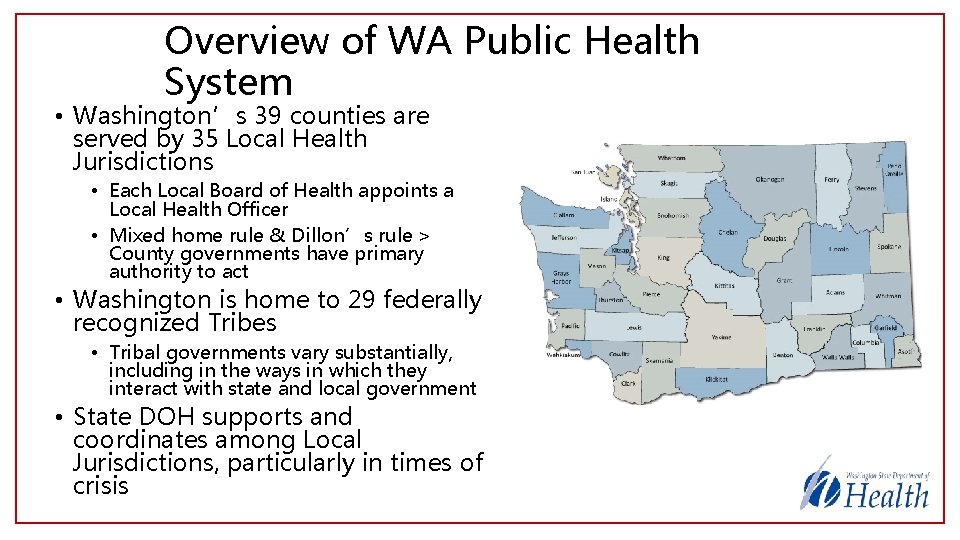
Overview of WA Public Health System • Washington’s 39 counties are served by 35 Local Health Jurisdictions • Each Local Board of Health appoints a Local Health Officer • Mixed home rule & Dillon’s rule > County governments have primary authority to act • Washington is home to 29 federally recognized Tribes • Tribal governments vary substantially, including in the ways in which they interact with state and local government • State DOH supports and coordinates among Local Jurisdictions, particularly in times of crisis
WA DOH Strategic Approach to Response “DOH is a responder agency”
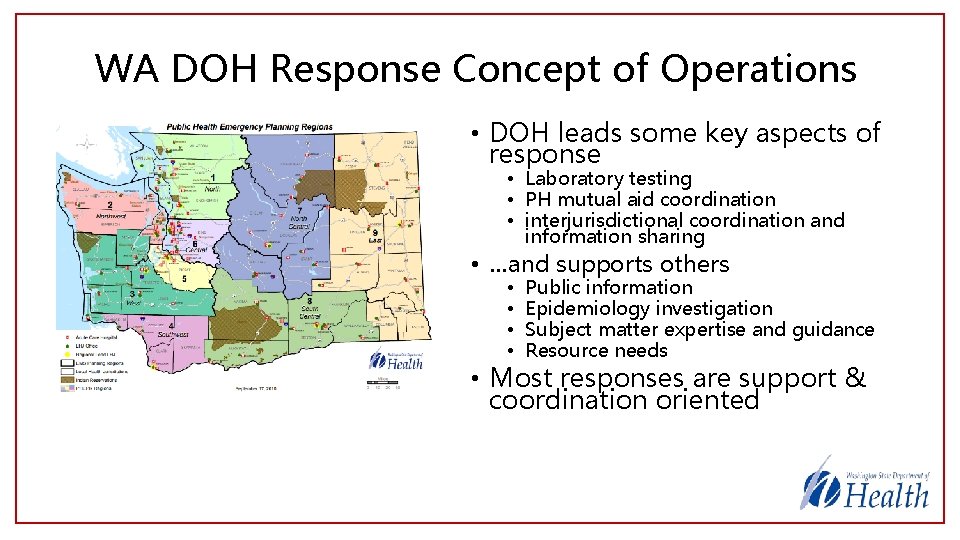
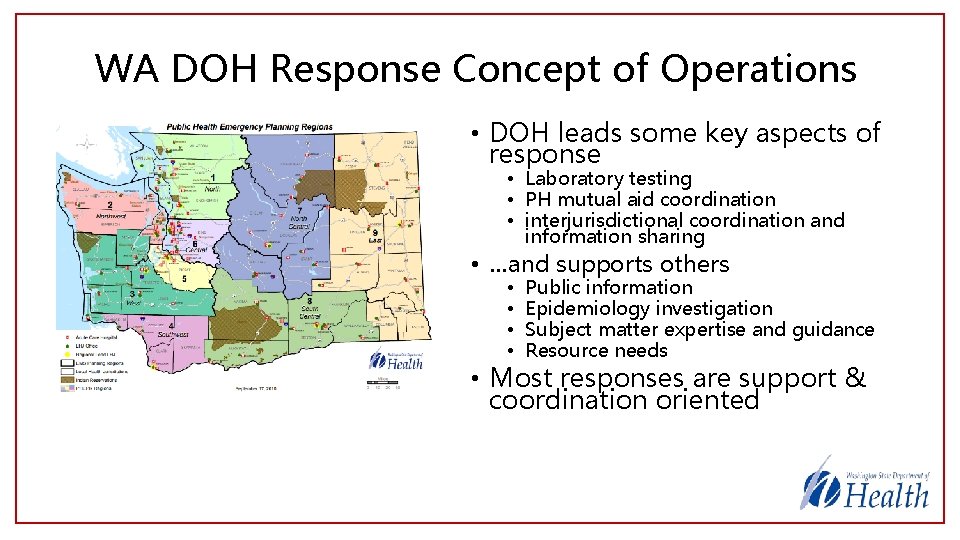
WA DOH Response Concept of Operations • DOH leads some key aspects of response • Laboratory testing • PH mutual aid coordination • interjurisdictional coordination and information sharing • …and supports others • • Public information Epidemiology investigation Subject matter expertise and guidance Resource needs • Most responses are support & coordination oriented
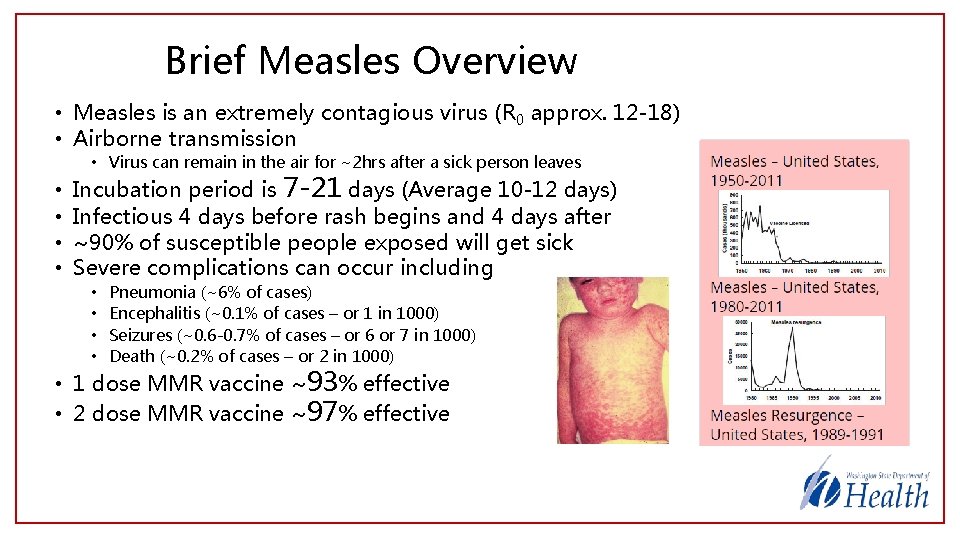
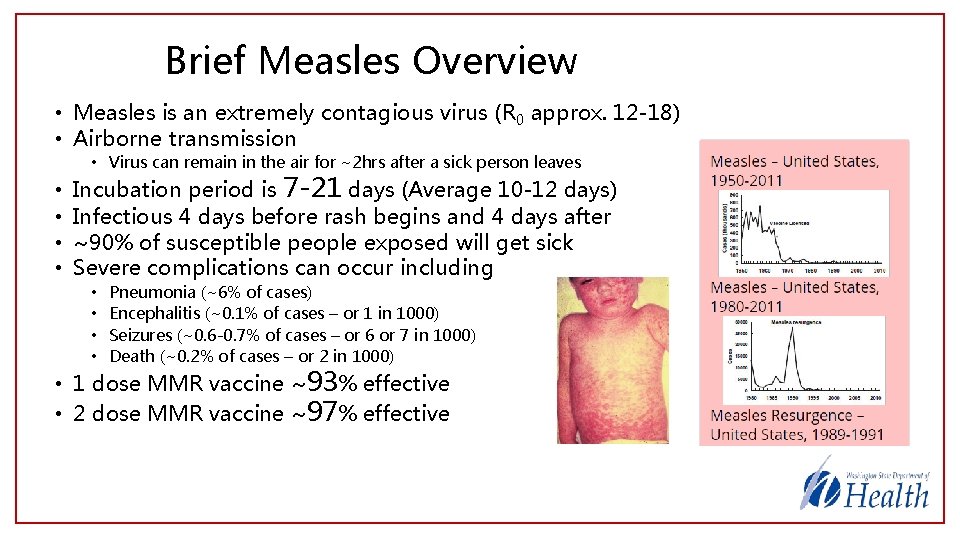
Brief Measles Overview • Measles is an extremely contagious virus (R 0 approx. 12 -18) • Airborne transmission • Virus can remain in the air for ~2 hrs after a sick person leaves • • Incubation period is 7 -21 days (Average 10 -12 days) Infectious 4 days before rash begins and 4 days after ~90% of susceptible people exposed will get sick Severe complications can occur including • • Pneumonia (~6% of cases) Encephalitis (~0. 1% of cases – or 1 in 1000) Seizures (~0. 6 -0. 7% of cases – or 6 or 7 in 1000) Death (~0. 2% of cases – or 2 in 1000) • 1 dose MMR vaccine ~93% effective • 2 dose MMR vaccine ~97% effective
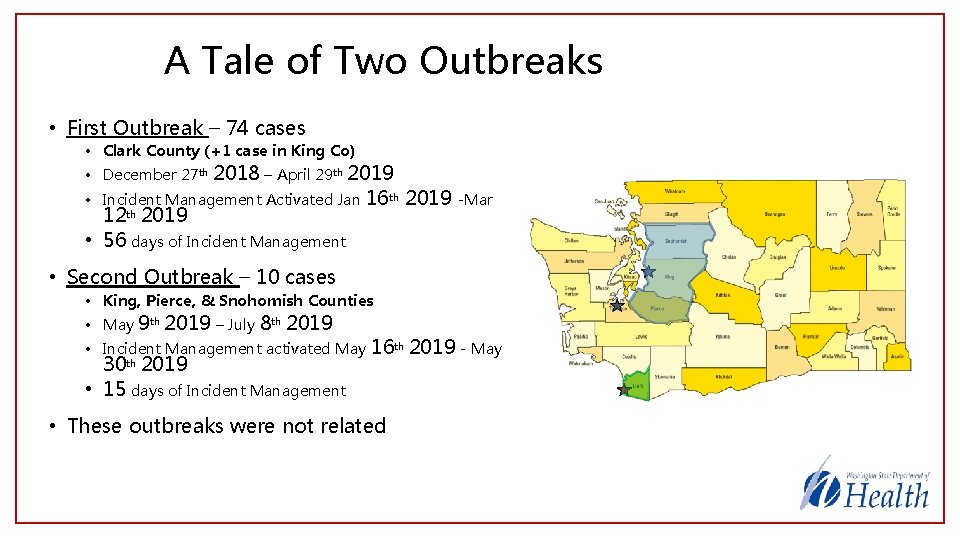
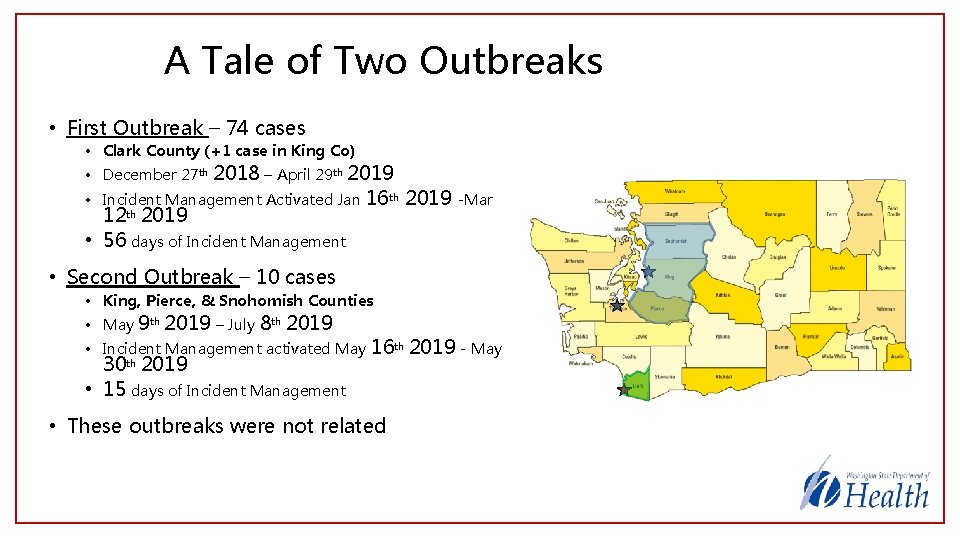
A Tale of Two Outbreaks • First Outbreak – 74 cases • Clark County (+1 case in King Co) • December 27 th 2018 – April 29 th 2019 • Incident Management Activated Jan 12 th 2019 • 56 days of Incident Management 16 th 2019 -Mar • Second Outbreak – 10 cases • King, Pierce, & Snohomish Counties • May 9 th 2019 – July 8 th 2019 • Incident Management activated May 30 th 2019 • 15 days of Incident Management 16 th 2019 - May • These outbreaks were not related
First Outbreak – Clark County, WA December 27 th 2018 – April 29 th 2019
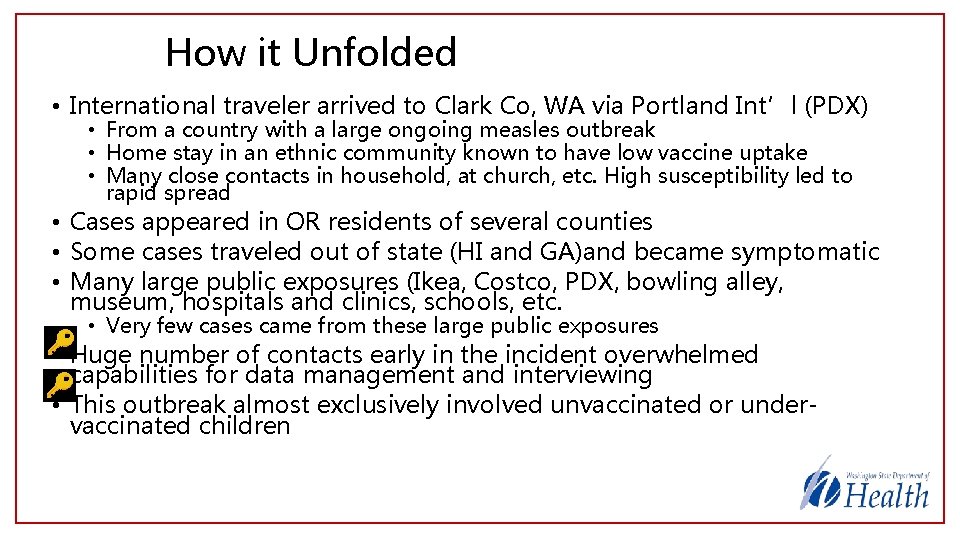
How it Unfolded • International traveler arrived to Clark Co, WA via Portland Int’l (PDX) • From a country with a large ongoing measles outbreak • Home stay in an ethnic community known to have low vaccine uptake • Many close contacts in household, at church, etc. High susceptibility led to rapid spread • Cases appeared in OR residents of several counties • Some cases traveled out of state (HI and GA)and became symptomatic • Many large public exposures (Ikea, Costco, PDX, bowling alley, museum, hospitals and clinics, schools, etc. • Very few cases came from these large public exposures • Huge number of contacts early in the incident overwhelmed capabilities for data management and interviewing • This outbreak almost exclusively involved unvaccinated or undervaccinated children
Local Response Efforts • Case investigation • Rash onset dates, locations visited while contagious • Public Information • Rumor control, risk communication, health education • Publication of exposure sites • Contact investigation • Tracked contacts from household and public exposures • Ascertained vaccination status to estimate risk • Non-pharmaceutical interventions • School exclusions for unvaccinated students @ exposure sites • Stay at home instructions for high risk contacts identified • Isolation requests for suspect and confirmed cases • Immunizations • Ensuring adequate access to vaccine (including free vaccine) • Pharmaceutical Interventions • Immunoglobulin for high-risk individuals exposed • & much more
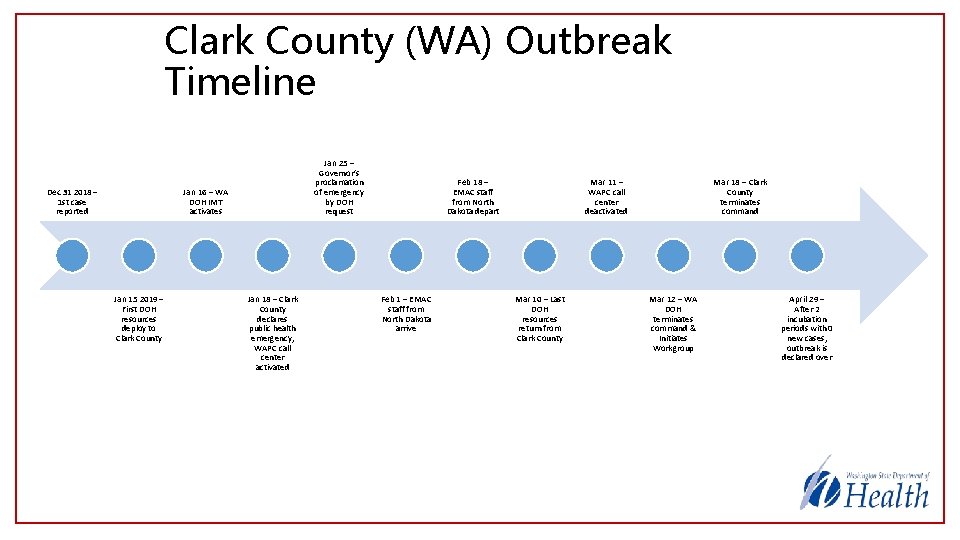
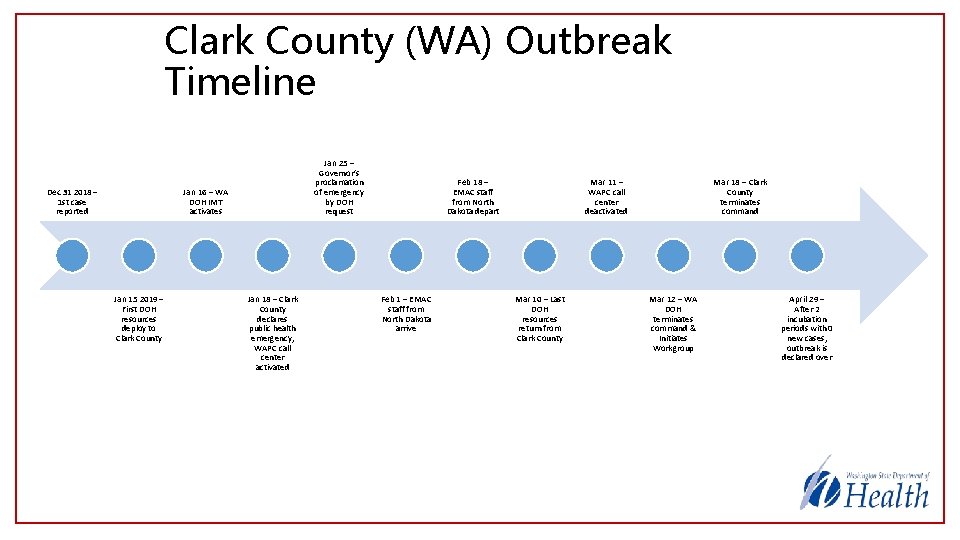
Clark County (WA) Outbreak Timeline Dec 31 2018 – 1 st case reported Jan 25 – Governor’s proclamation of emergency by DOH request Jan 16 – WA DOH IMT activates Jan 15 2019 – First DOH resources deploy to Clark County Jan 18 – Clark County declares public health emergency, WAPC call center activated Feb 18 – EMAC staff from North Dakota depart Feb 1 – EMAC staff from North Dakota arrive Mar 11 – WAPC call center deactivated Mar 10 – Last DOH resources return from Clark County Mar 18 – Clark County terminates command Mar 12 – WA DOH terminates command & Initiates Workgroup April 29 – After 2 incubation periods with 0 new cases, outbreak is declared over
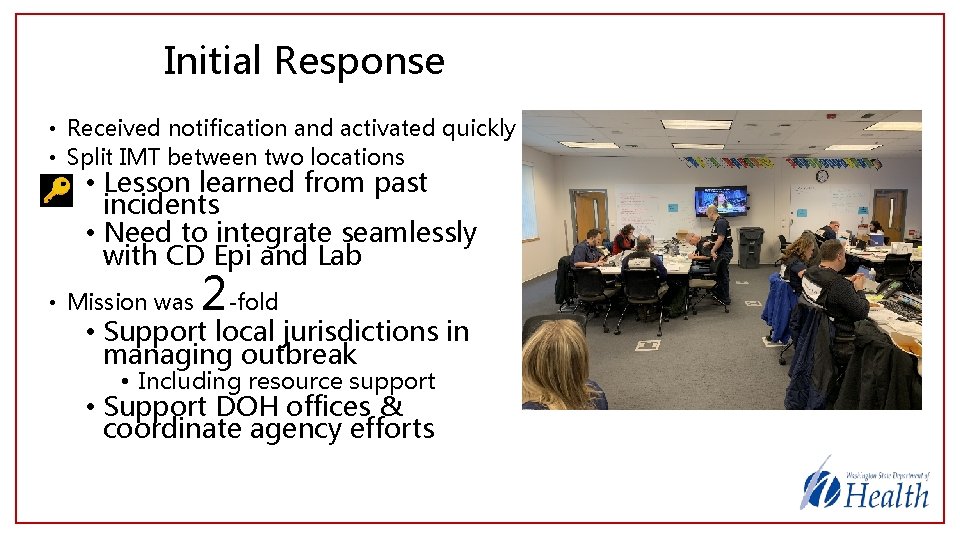
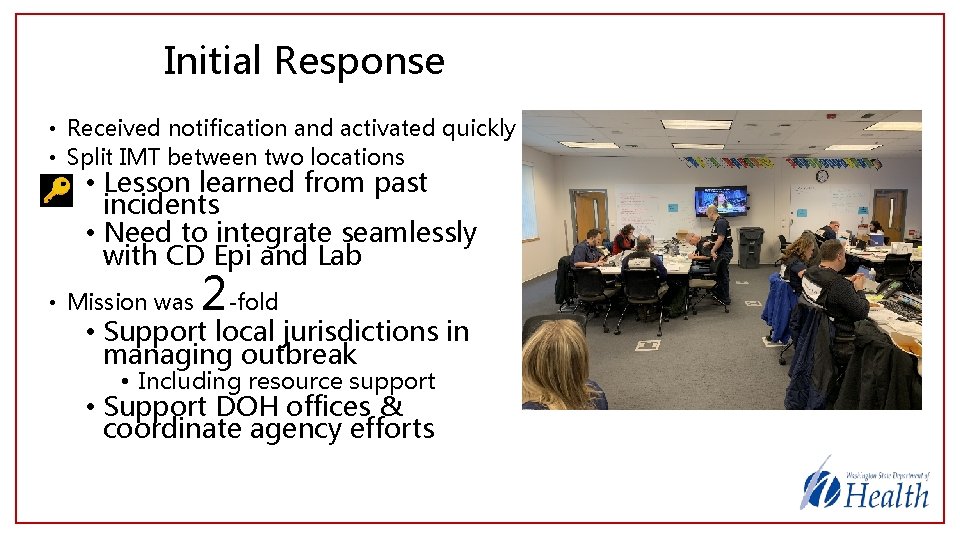
Initial Response • Received notification and activated quickly • Split IMT between two locations • Lesson learned from past incidents • Need to integrate seamlessly with CD Epi and Lab • Mission was 2 -fold • Support local jurisdictions in managing outbreak • Including resource support • Support DOH offices & coordinate agency efforts
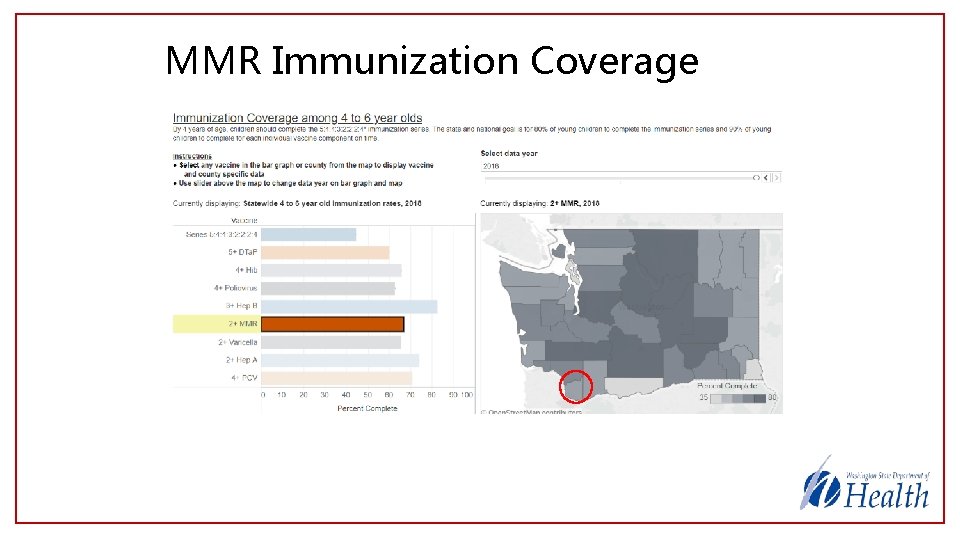
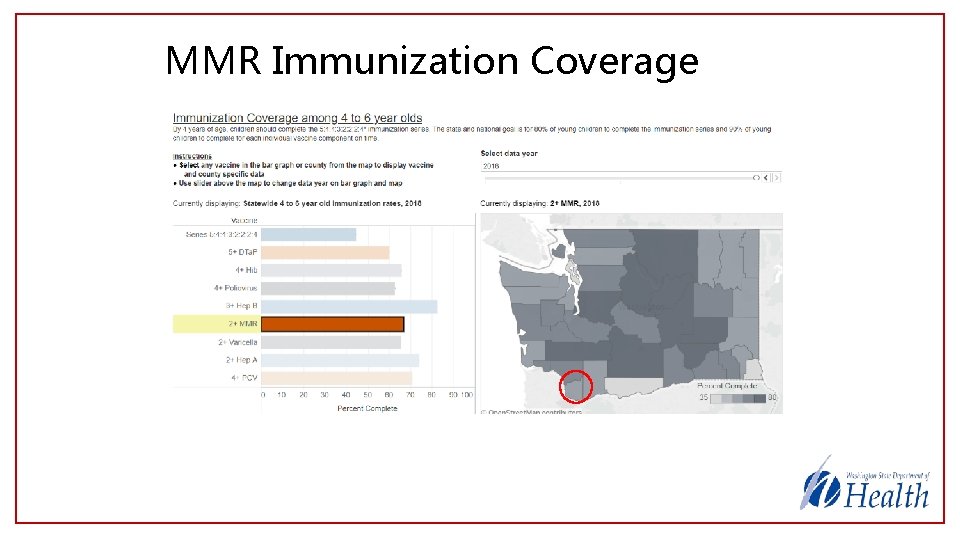
MMR Immunization Coverage
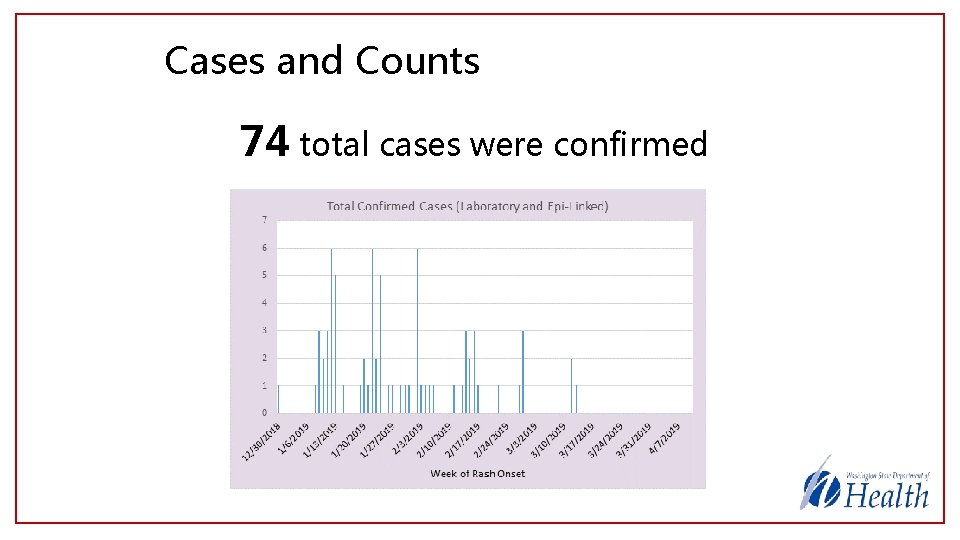
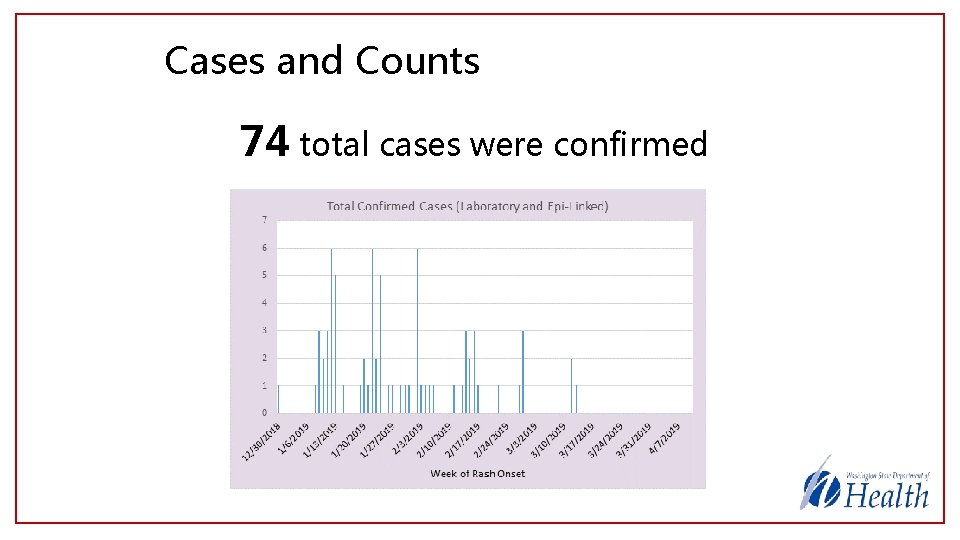
Cases and Counts 74 total cases were confirmed
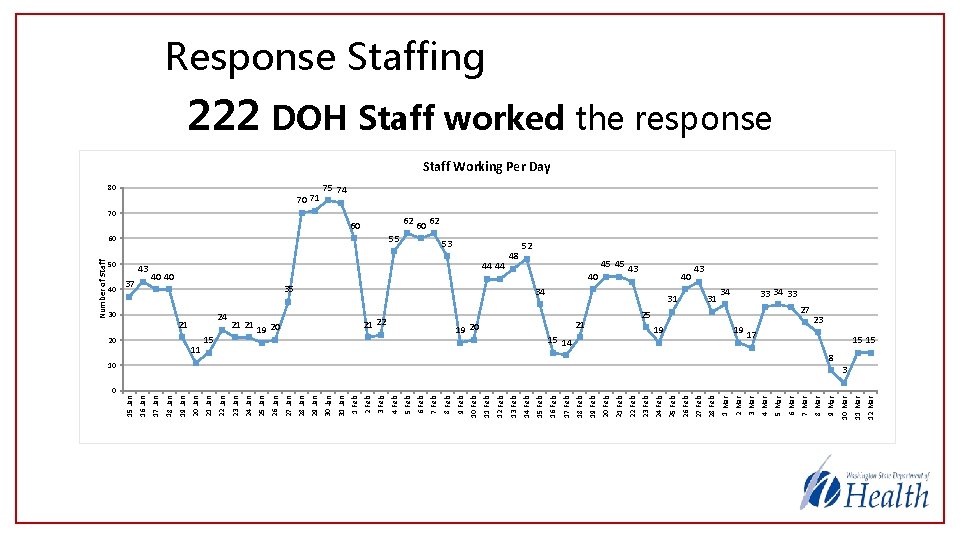
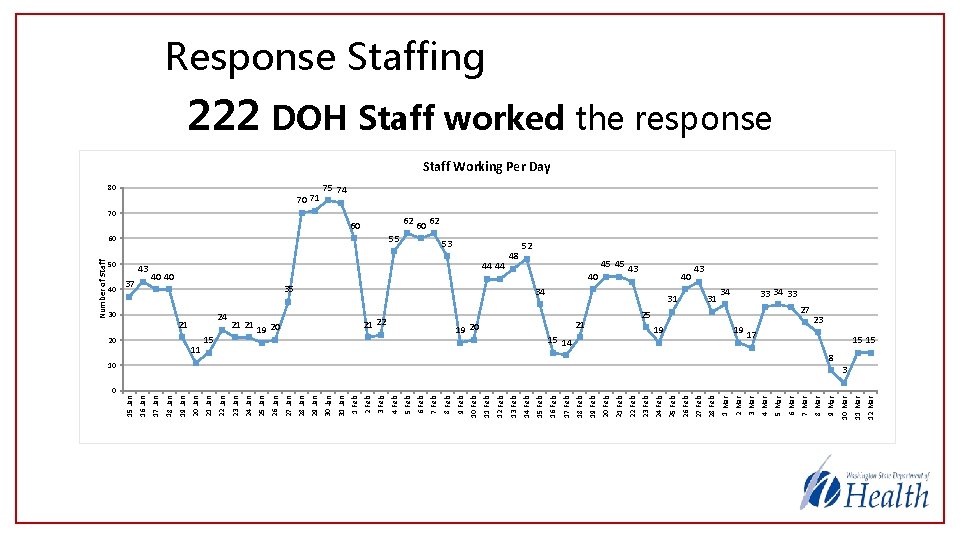
19 -Jan 26 -Jan 18 -Feb 9 -Mar 12 -Mar 17 11 -Mar 10 10 -Mar 27 8 -Mar 25 7 -Mar 6 -Mar 19 5 -Mar 19 3 -Mar 34 4 -Mar 31 2 -Mar 31 1 -Mar 15 14 27 -Feb 40 28 -Feb 43 26 -Feb 34 25 -Feb 21 24 -Feb 45 45 23 -Feb 40 22 -Feb 21 -Feb 20 -Feb 19 20 17 -Feb 35 16 -Feb 48 14 -Feb 53 15 -Feb 44 44 13 -Feb 12 -Feb 40 40 11 -Feb 21 22 9 -Feb 55 10 -Feb 60 8 -Feb 62 7 -Feb 60 6 -Feb 70 5 -Feb 60 4 -Feb 3 -Feb 19 20 2 -Feb 1 -Feb 31 -Jan 70 71 30 -Jan 29 -Jan 80 28 -Jan 15 27 -Jan 21 21 25 -Jan 11 24 -Jan 24 23 -Jan 21 22 -Jan 20 21 -Jan 30 20 -Jan 37 18 -Jan 43 17 -Jan 50 16 -Jan 40 15 -Jan Number of Staff Response Staffing 222 DOH Staff worked the response Staff Working Per Day 75 74 62 52 43 33 34 33 23 15 15 8 3 0
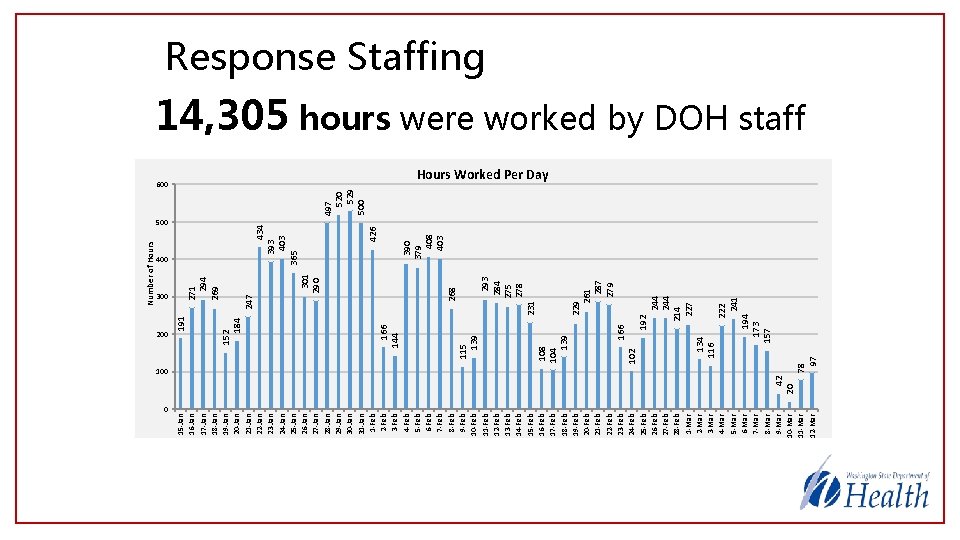
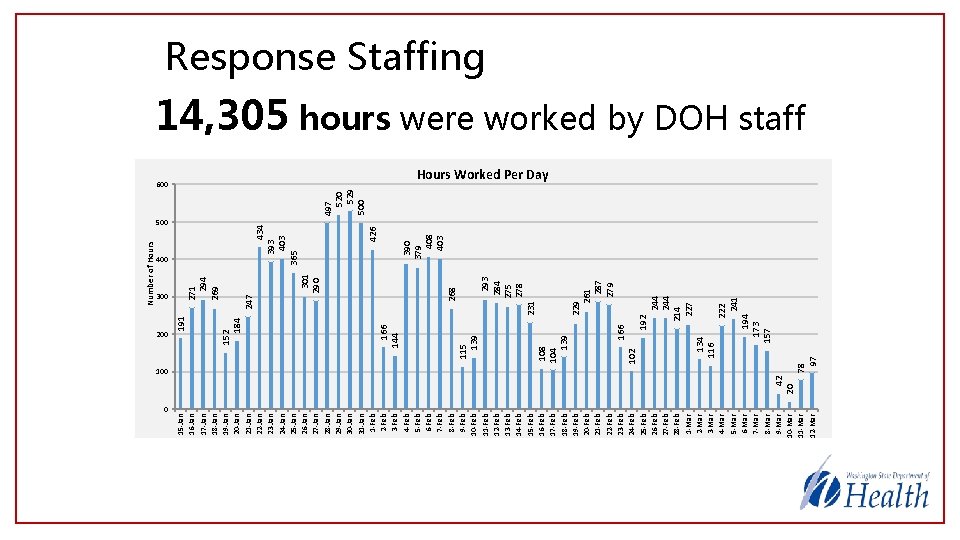
244 214 227 229 261 287 279 231 222 241 194 173 157 192 166 134 116 102 108 104 139 293 284 275 278 268 301 290 379 408 403 426 434 393 403 365 400 115 139 247 500 166 144 152 184 271 294 269 497 520 529 500 600 78 97 100 42 20 200 191 300 15 -Jan 16 -Jan 17 -Jan 18 -Jan 19 -Jan 20 -Jan 21 -Jan 22 -Jan 23 -Jan 24 -Jan 25 -Jan 26 -Jan 27 -Jan 28 -Jan 29 -Jan 30 -Jan 31 -Jan 1 -Feb 2 -Feb 3 -Feb 4 -Feb 5 -Feb 6 -Feb 7 -Feb 8 -Feb 9 -Feb 10 -Feb 11 -Feb 12 -Feb 13 -Feb 14 -Feb 15 -Feb 16 -Feb 17 -Feb 18 -Feb 19 -Feb 20 -Feb 21 -Feb 22 -Feb 23 -Feb 24 -Feb 25 -Feb 26 -Feb 27 -Feb 28 -Feb 1 -Mar 2 -Mar 3 -Mar 4 -Mar 5 -Mar 6 -Mar 7 -Mar 8 -Mar 9 -Mar 10 -Mar 11 -Mar 12 -Mar Number of Hours Response Staffing 14, 305 hours were worked by DOH staff Hours Worked Per Day 0

Public Information Needs Public Information Officers responded to requests 164 media
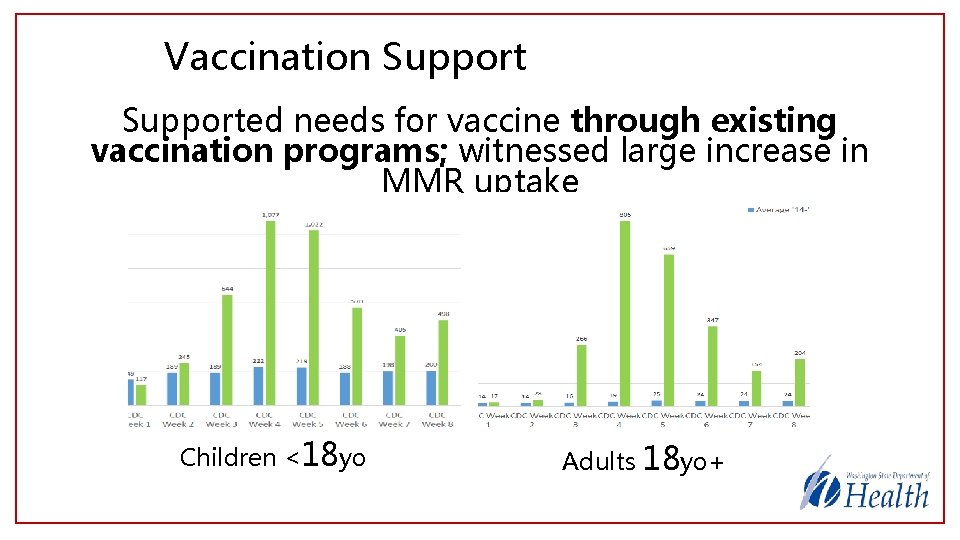
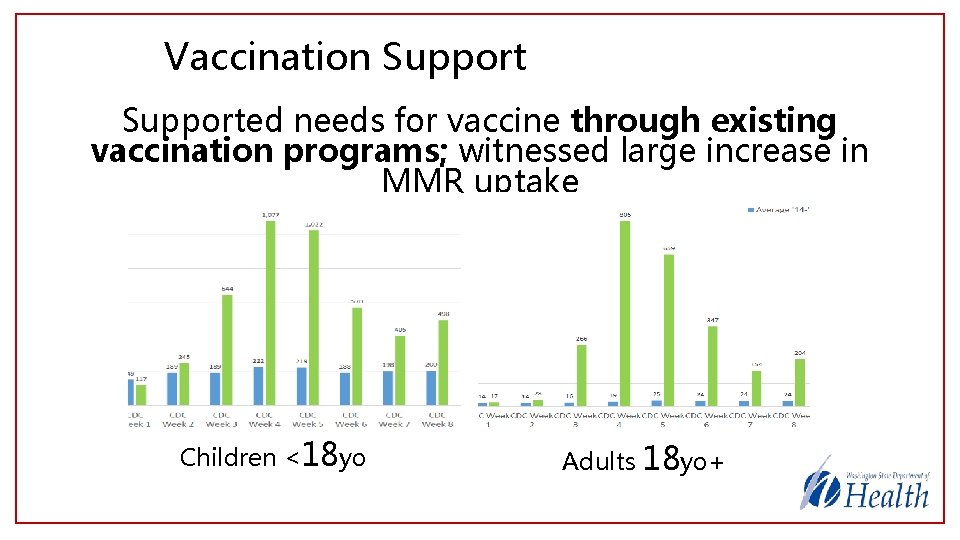
Vaccination Supported needs for vaccine through existing vaccination programs; witnessed large increase in MMR uptake Children <18 yo Adults 18 yo+
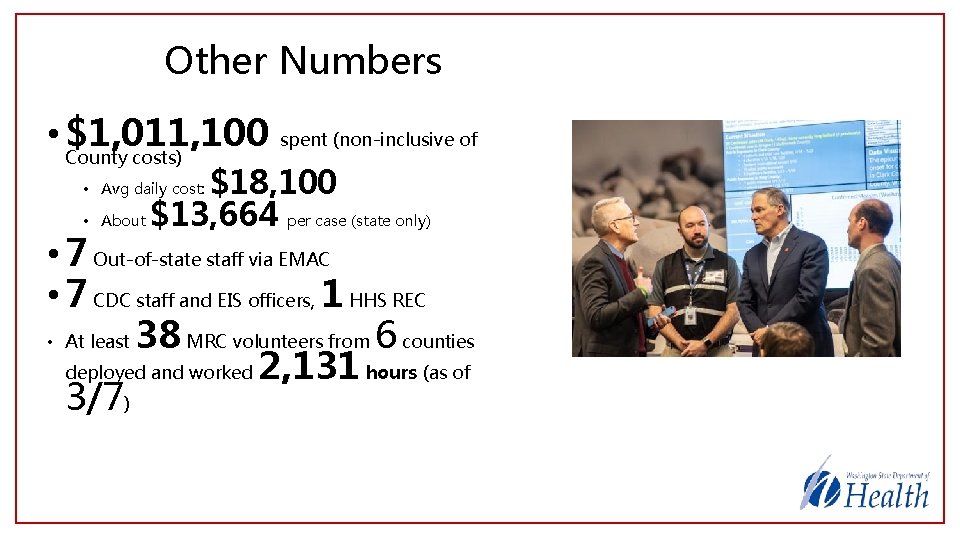
Other Numbers • $1, 011, 100 County costs) spent (non-inclusive of $18, 100 About $13, 664 per case (state only) • Avg daily cost: • • 7 Out-of-state staff via EMAC • 7 CDC staff and EIS officers, 1 HHS REC • At least 38 MRC volunteers from 6 counties deployed and worked 2, 131 hours (as of 3/7)
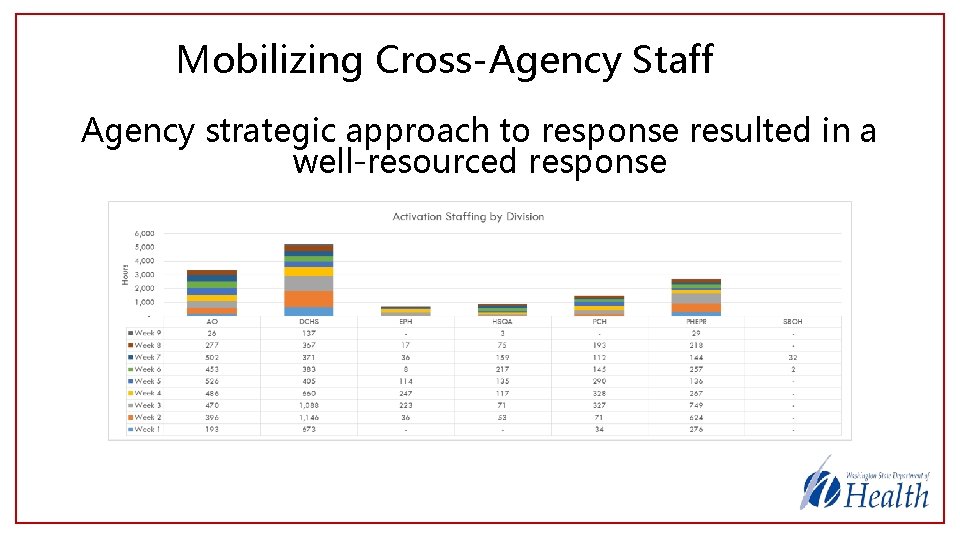
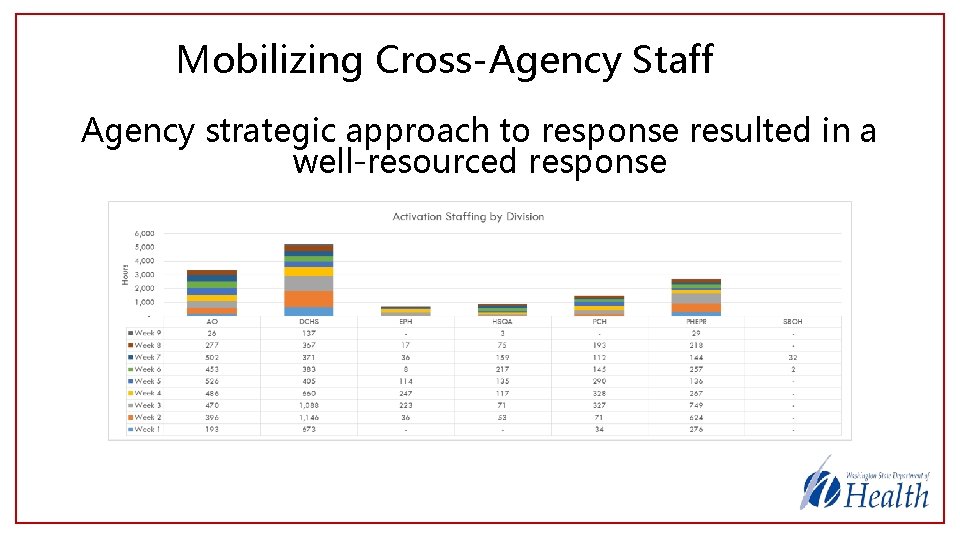
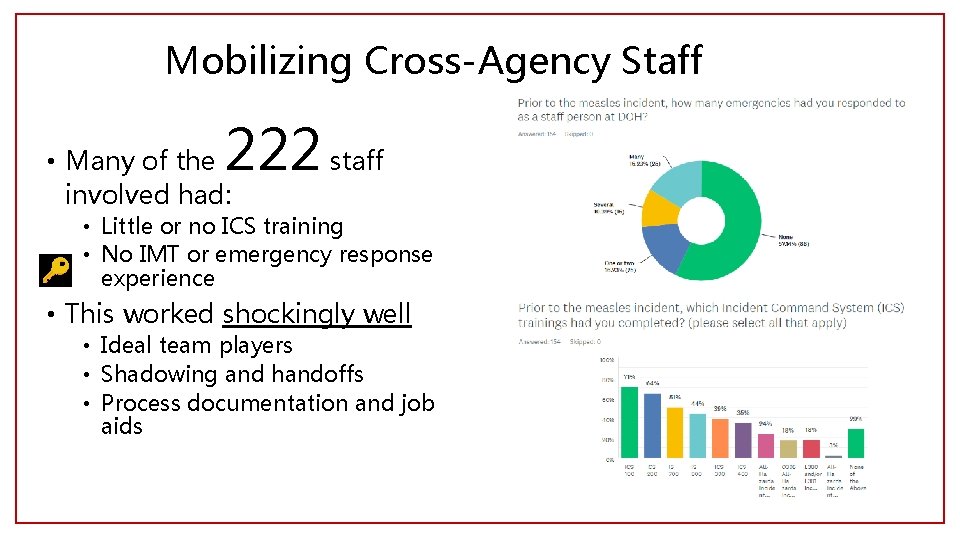
Mobilizing Cross-Agency Staff Agency strategic approach to response resulted in a well-resourced response
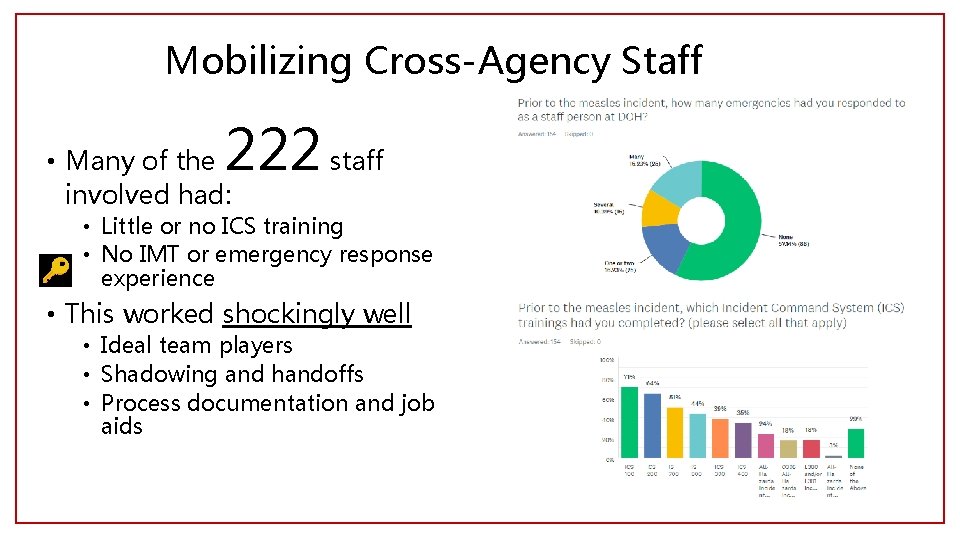
Mobilizing Cross-Agency Staff 222 staff • Many of the involved had: • Little or no ICS training • No IMT or emergency response experience • This worked shockingly well • Ideal team players • Shadowing and handoffs • Process documentation and job aids
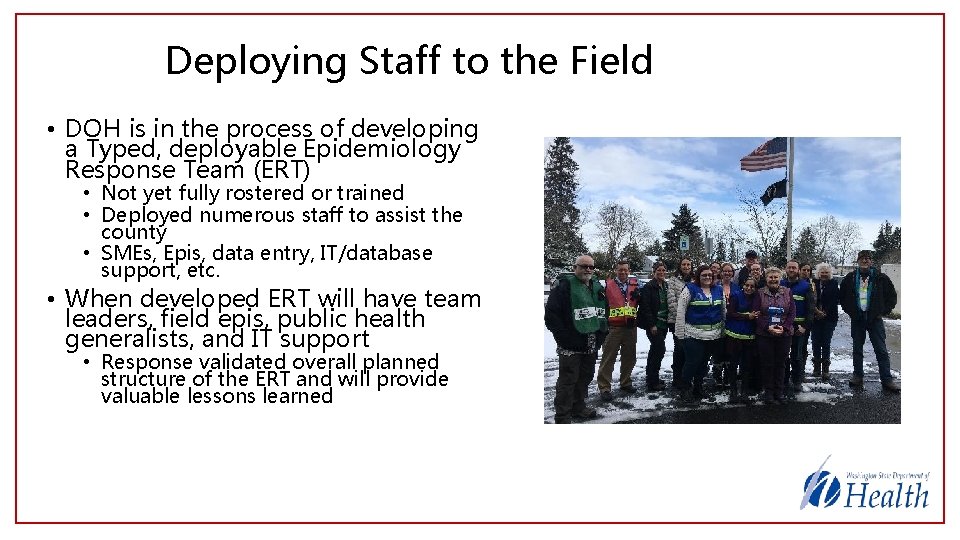
Deploying Staff to the Field • DOH is in the process of developing a Typed, deployable Epidemiology Response Team (ERT) • Not yet fully rostered or trained • Deployed numerous staff to assist the county • SMEs, Epis, data entry, IT/database support, etc. • When developed ERT will have team leaders, field epis, public health generalists, and IT support • Response validated overall planned structure of the ERT and will provide valuable lessons learned
State Public Health Call Center • DOH maintains a contract with the Washington Poison Center (WAPC) for emergency call center capability • We provide the scripts, they take the calls, we pay the bill • Capability can be activated by a county HD • Call center capability was activated by the county for most of the response • 1, 227 calls received for county residents • Numerous calls received for out of county and out of state residents
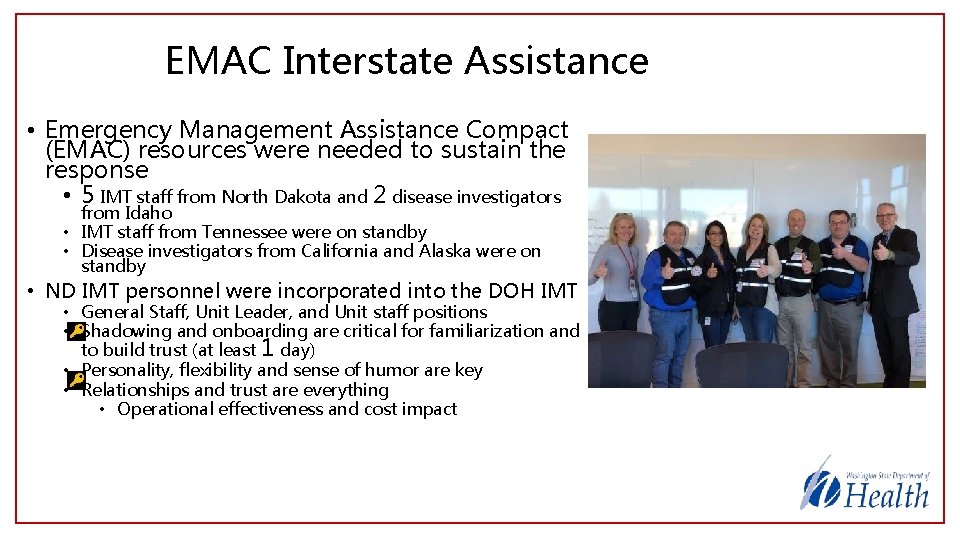
EMAC Interstate Assistance • Emergency Management Assistance Compact (EMAC) resources were needed to sustain the response • 5 IMT staff from North Dakota and 2 disease investigators from Idaho • IMT staff from Tennessee were on standby • Disease investigators from California and Alaska were on standby • ND IMT personnel were incorporated into the DOH IMT • General Staff, Unit Leader, and Unit staff positions • Shadowing and onboarding are critical for familiarization and to build trust (at least 1 day) • Personality, flexibility and sense of humor are key • Relationships and trust are everything • Operational effectiveness and cost impact
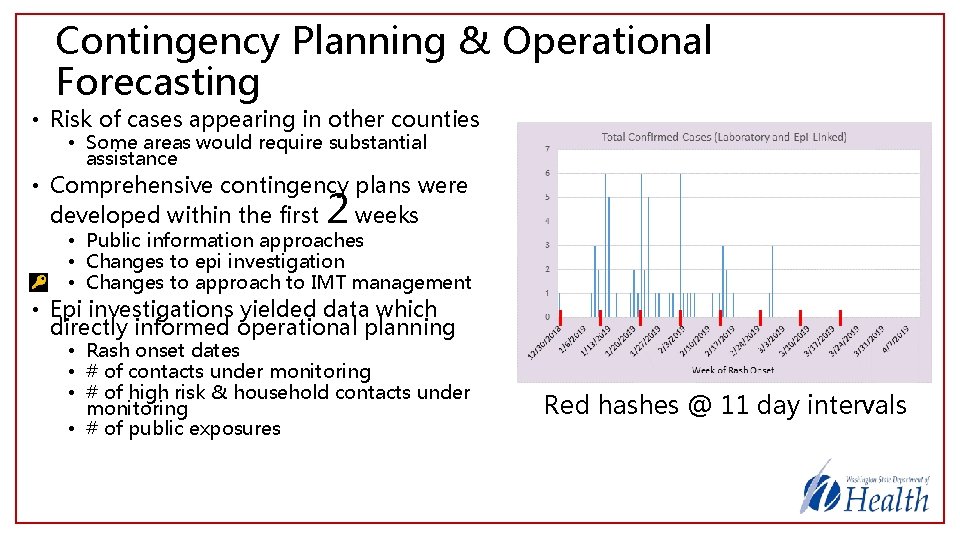
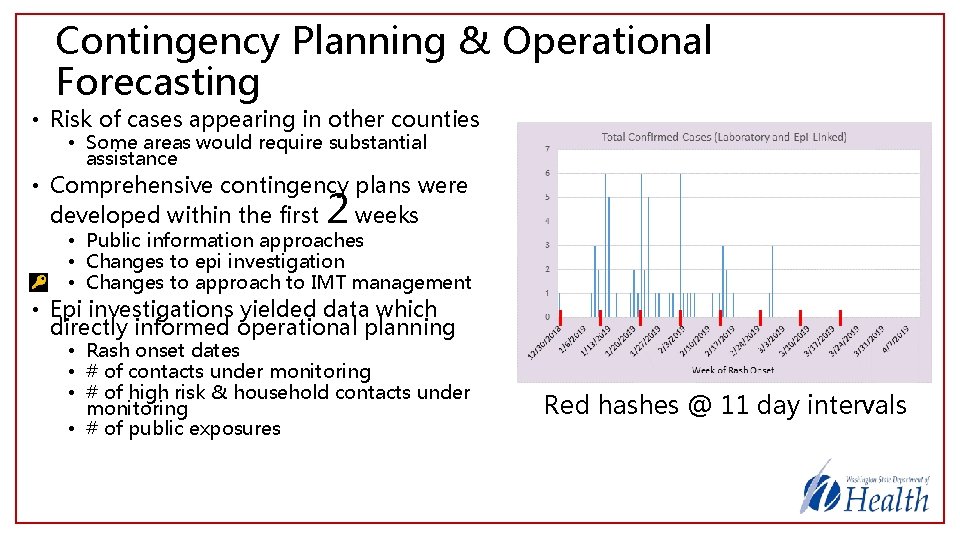
Contingency Planning & Operational Forecasting • Risk of cases appearing in other counties • Some areas would require substantial assistance • Comprehensive contingency plans were developed within the first weeks 2 • Public information approaches • Changes to epi investigation • Changes to approach to IMT management • Epi investigations yielded data which directly informed operational planning • Rash onset dates • # of contacts under monitoring • # of high risk & household contacts under monitoring • # of public exposures Red hashes @ 11 day intervals
Incidents Within the Incident • Historic winter weather events • Difficult travel • Remote working • Agency continuity of operations impacts • Potential for ESF 8 Response • Contingency plan: Incident Complex • Death of a colleague • Staffing & psychosocial impacts • Added substantial complexity • Flexibility, creativity, and teamwork saved the day
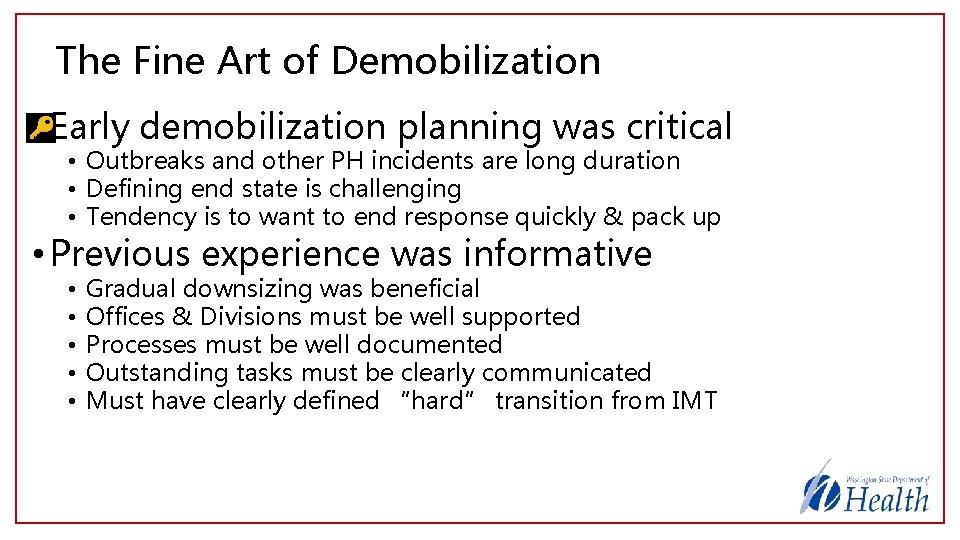
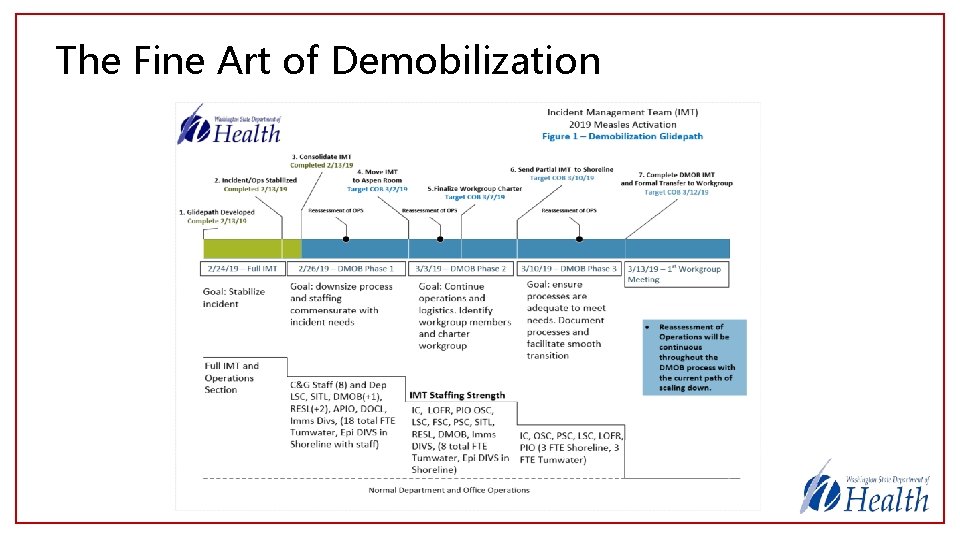
The Fine Art of Demobilization • Early demobilization planning was critical • Outbreaks and other PH incidents are long duration • Defining end state is challenging • Tendency is to want to end response quickly & pack up • Previous experience was informative • • • Gradual downsizing was beneficial Offices & Divisions must be well supported Processes must be well documented Outstanding tasks must be clearly communicated Must have clearly defined “hard” transition from IMT
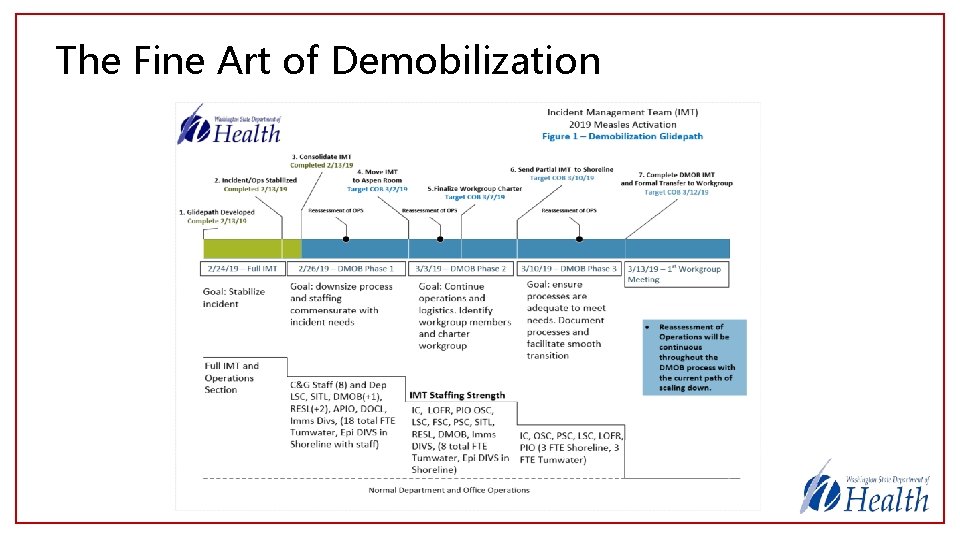
The Fine Art of Demobilization
Incident Workgroup Transition • DOH transitions from IMT to a Cross-Agency Incident Workgroup • Provides structure for ongoing coordination • Allows IMT to terminate command while essential incident management and response activities continue • Workgroup composed of reps from involved offices • Immunizations, Epi, Lab, Public Affairs, Finance, Prep & Response • Sponsored by Division A/S and State Epi for CD
Incident Workgroup Transition • Incorporated lessons learned from previous HCV and Mumps incidents • Work continues within offices • Interdependencies must be identified • Processes must be established for information sharing • Workgroup serves as coordinating body • Workgroup members meet regularly • Ensure adequacy of processes and identify issues • Monitor thresholds for potential IMT reactivation
Intra-Incident Breakthrough • IMT staff had a important realization as we transitioned out of ICS • While we did work to stabilize the incident through ICS, the primary purpose of our response was not to address the incident and its impacts • The primary purpose of the ICS response was to organize a system to address the ongoing impacts of and response to the incident through inter- and intra-agency coordination and cooperation • Establishing and transitioning to this system after incident stabilization allowed effective response to continue without ICS • We deactivated the IMT ~6 weeks before the outbreak was declared over • We will carry this idea forward to future responses • Focus on building systems and capability through the ICS process will enable more efficient management of future incidents
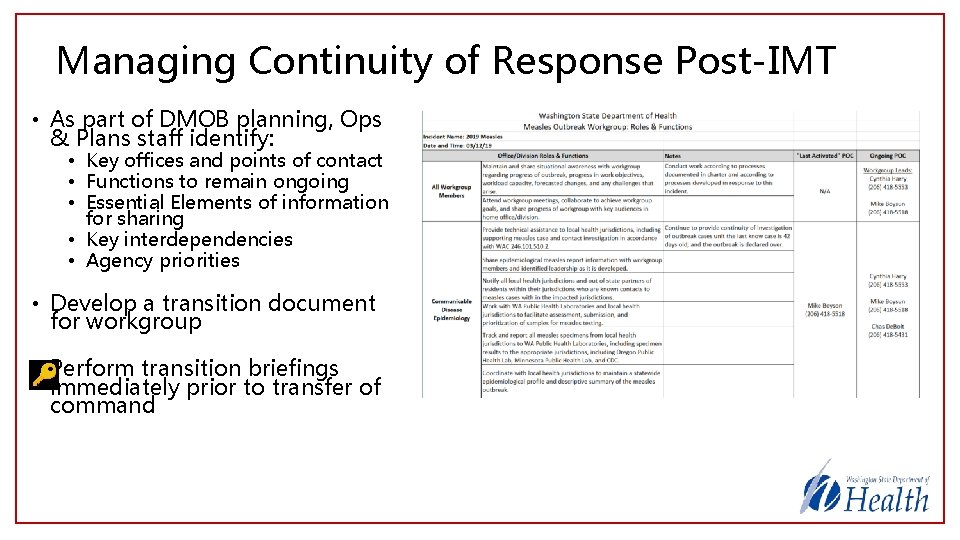
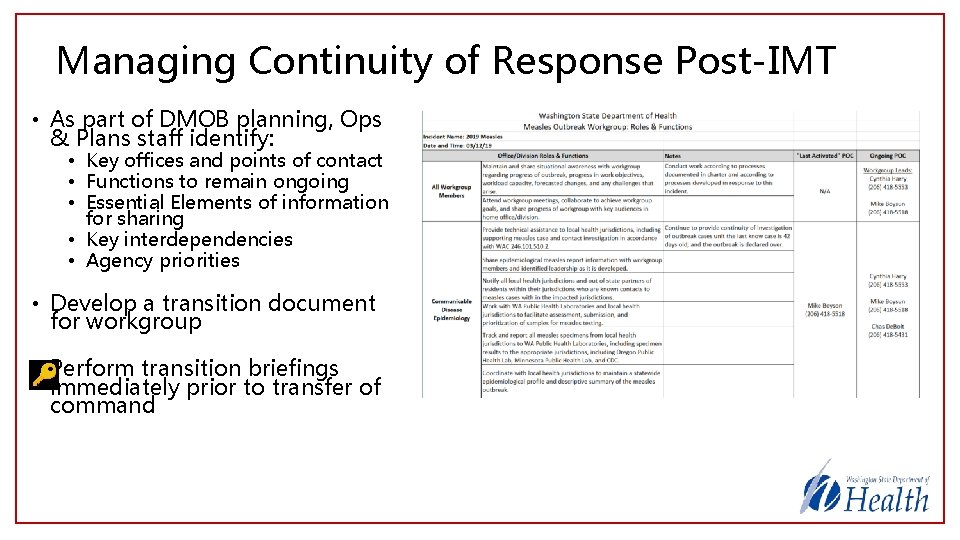
Managing Continuity of Response Post-IMT • As part of DMOB planning, Ops & Plans staff identify: • Key offices and points of contact • Functions to remain ongoing • Essential Elements of information for sharing • Key interdependencies • Agency priorities • Develop a transition document for workgroup • Perform transition briefings immediately prior to transfer of command
Key Improvements & Innovations Implemented • CD Epi Office: rotating Measles Duty Epi • • • Intake, lab coordination, daily reporting of epi EEIs, TA for Counties Consistent phone number & email address Alleviated pressure on VPD epis and team by providing single key contact • CD Epi Office: Regular (daily) “Epi-to-Epi” technical coordinating calls with affected counties • • Promoted open communications and informal information sharing among state and affected locals Watch out for scope creep and keep attendance limited • Agency: Use of Supervisors, rather than Tech Specs as DIVS • • History of placing Tech Specs in leadership positions – creates challenges Rotating schedule of outbreak Epi DIVS led to stability/consistency in leadership • IMT: Deployed Agency Representatives to affected County • • IMT encountered challenges adequately tracking and supporting deployed staff First experience using Agency Reps – was universally seen as beneficial • IMT & Agency: Use of technology & Flexible IMT Deployments • • Deployed IMT to Shoreline (Public Health Lab) facility for the first time Use of loaner laptops and cellular devices for IMT staff to work remotely during inclement weather Use of Maven Outbreak Module drastically improved data management Use of Go. To. Meeting for SA broadcasting among locations
Key Gaps Identified • Responder Health & Safety was a challenge • Luckily, no injuries or other safety incidents, however, • Identified gaps in maintaining accountability for deployed personnel • Improvements are needed in pre-departure briefings, procedures for reporting safety concerns, and procedures for reaching back to the IMT • Gaps were identified in “procedure-level” documentation • There were not adequate job aids, templates, and procedures for resource management, financial reporting and procurement management, and demobilization • This issue was identified primarily through use of staff lacking training and experience • Gaps were identified in briefing practices • Handoff of position responsibilities, debriefing of personnel, subject-matter familiarization, etc. • Information sharing was challenging • EEIs and timelines for reporting of key info were not established in advance • Coordination of volunteer worker missions was difficult • Multijurisdictional efforts paired with relative lack of experience led to confusion
Second Outbreak – King, Pierce, and Snohomish Counties, WA May 9 th 2019 – July 8 th 2019
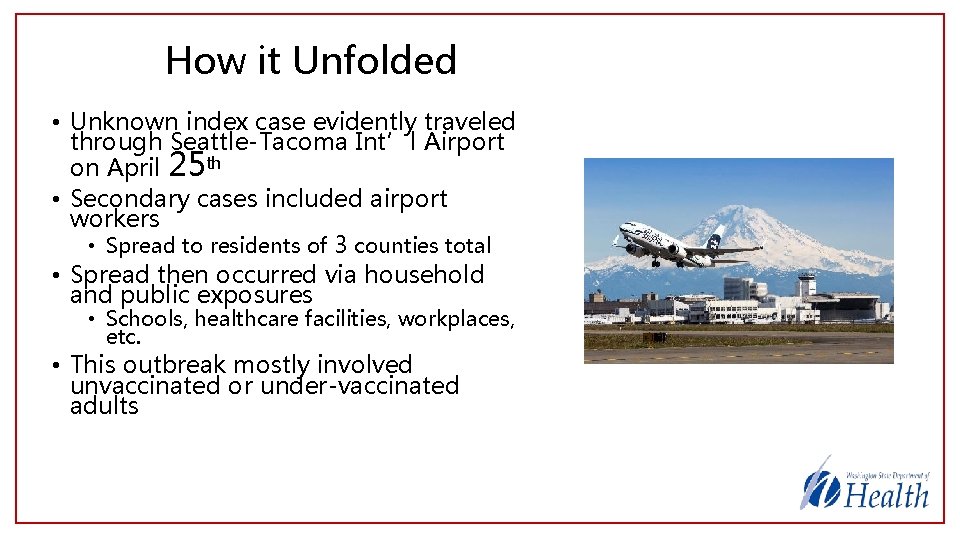
How it Unfolded • Unknown index case evidently traveled through Seattle-Tacoma Int’l Airport on April 25 th • Secondary cases included airport workers • Spread to residents of 3 counties total • Spread then occurred via household and public exposures • Schools, healthcare facilities, workplaces, etc. • This outbreak mostly involved unvaccinated or under-vaccinated adults
What Was Different • Multicounty outbreak enabled DOH to lead investigations • A contingency which was planned for during the first outbreak • IMT activated only at Shoreline facility • Improved collaboration among IMT, Epi, and Lab • Improvements in information sharing • Excellent info sharing among DOH & 3 counties • Great partnership with CDC DGMQ, SEA airport management, and DHS • Supported effective investigation • Resources developed in first incident put to work here • Job aids, process docs, recent experience • Personnel remained in short supply • Improved processes & assets helped us better utilize less experienced responders
Conclusions • 74 cases of measles required full strength of agency capability to effectively support and coordinate • Prepare for concurrent incidents and proactively plan for contingencies • Statewide LHJ mutual aid was utilized, however erosion of public health capacity over many years has produced gaps. Limitations were evident in this incident • EMAC proved essential and valuable. Should serve as a primary resource in PH emergencies even in non-federally declared incidents • Shadowing and on the job training proved almost as valuable as previous ICS training. Ideal Team Players (hungry, humble, people-smart) were always successful with adequate onboarding, even without prior experience. • Continuous improvements implemented during an incident may come in handy more quickly than you think
Questions? Kevin Wickersham, MS kevin. wickersham@doh. wa. gov Washington State Department of Health