Lessons Learned Cortisol Why Measure Cortisol Hypercortisolism or



![Awakening Response � Awakening Response (Pruessner, 1997) [30 min post awakening] – [awakening] Awakening Response � Awakening Response (Pruessner, 1997) [30 min post awakening] – [awakening]](https://slidetodoc.com/presentation_image/52656342c647f4871cfadfad0e477110/image-12.jpg)


- Slides: 20

Lessons Learned Cortisol
Why Measure Cortisol? � Hyper-cortisolism or hypo-cortisolism associated with several disease conditions ◦ ◦ ◦ Cushing’s Disease Addison’s Disease Congenital Adrenal Hyperplasia Depression Thyroid Disease � Cortisol is an objective marker of the stress response

What Medium to Use? � Urine � Blood � Saliva (serum or plasma) � Hair ◦ Pros and Cons for each
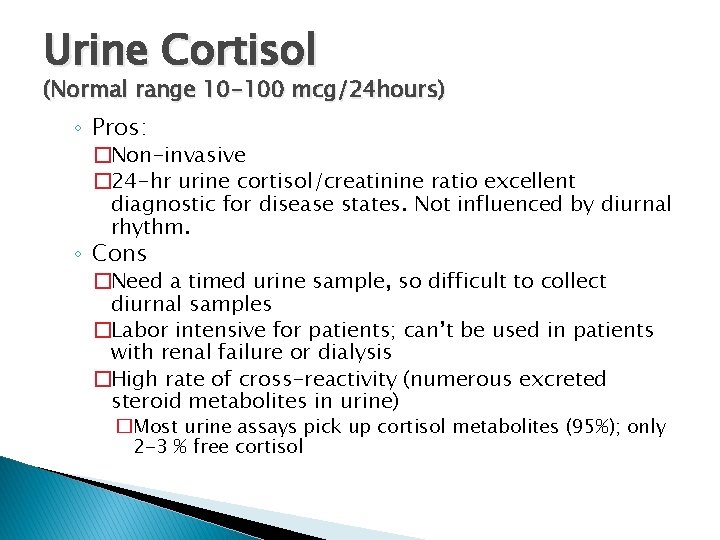
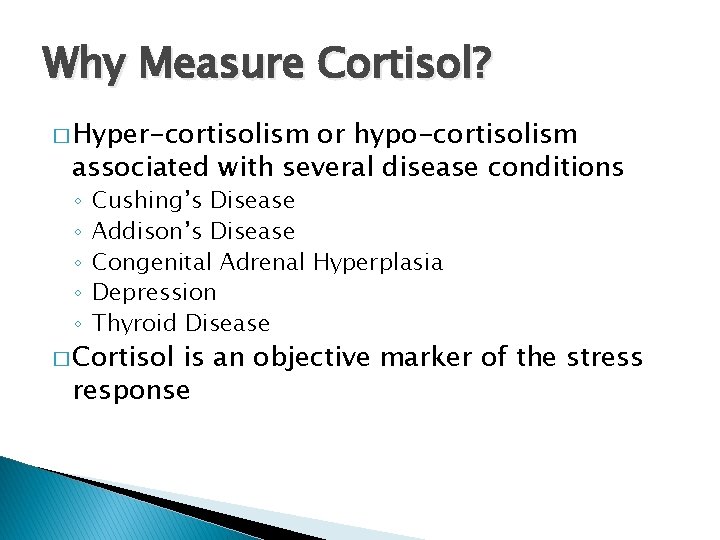
Urine Cortisol (Normal range 10 -100 mcg/24 hours) ◦ Pros: �Non-invasive � 24 -hr urine cortisol/creatinine ratio excellent diagnostic for disease states. Not influenced by diurnal rhythm. ◦ Cons �Need a timed urine sample, so difficult to collect diurnal samples �Labor intensive for patients; can’t be used in patients with renal failure or dialysis �High rate of cross-reactivity (numerous excreted steroid metabolites in urine) �Most urine assays pick up cortisol metabolites (95%); only 2 -3 % free cortisol
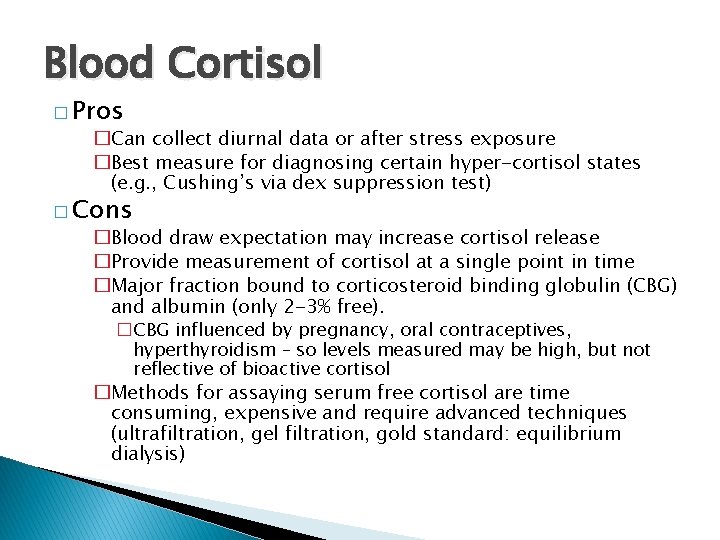
Blood Cortisol � Pros �Can collect diurnal data or after stress exposure �Best measure for diagnosing certain hyper-cortisol states (e. g. , Cushing’s via dex suppression test) � Cons �Blood draw expectation may increase cortisol release �Provide measurement of cortisol at a single point in time �Major fraction bound to corticosteroid binding globulin (CBG) and albumin (only 2 -3% free). �CBG influenced by pregnancy, oral contraceptives, hyperthyroidism – so levels measured may be high, but not reflective of bioactive cortisol �Methods for assaying serum free cortisol are time consuming, expensive and require advanced techniques (ultrafiltration, gel filtration, gold standard: equilibrium dialysis)
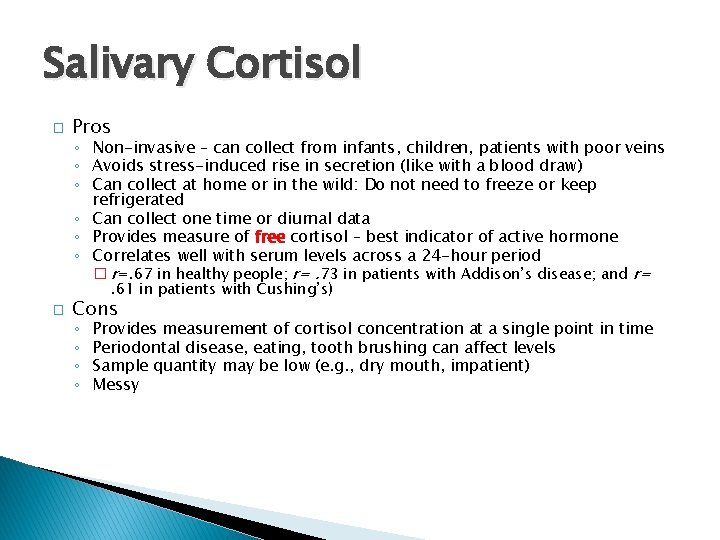
Salivary Cortisol � Pros ◦ Non-invasive – can collect from infants, children, patients with poor veins ◦ Avoids stress-induced rise in secretion (like with a blood draw) ◦ Can collect at home or in the wild: Do not need to freeze or keep refrigerated ◦ Can collect one time or diurnal data ◦ Provides measure of free cortisol – best indicator of active hormone ◦ Correlates well with serum levels across a 24 -hour period � r=. 67 in healthy people; r=. 73 in patients with Addison’s disease; and r=. 61 in patients with Cushing’s) � Cons ◦ ◦ Provides measurement of cortisol concentration at a single point in time Periodontal disease, eating, tooth brushing can affect levels Sample quantity may be low (e. g. , dry mouth, impatient) Messy
Hair Cortisol � Pros Biomarker of chronic stress Relatively non-invasive Only free cortisol represented Easily transported and stored - put in an envelope or vial & store at room temp for months to years ◦ Reflects cortisol levels over past months (Hair grows predictably about 1 cm/month) – ◦ ◦ � 1 cm closest to skull reflects last month; 2 nd cm out reflects preceding month � So may not need to take multiple samples to evaluate chronic stress and perhaps compare months with and without a stressor ◦ Not affected by hair color – but maybe by dying of hair ◦ Significantly correlated with self-reports of stress (Kalra, 2007; Van Uum, 2008) � Cons ◦ No clinically relevant reference range established to date ◦ Exposure to exogenous steroids in lotions or creams may cause sample contamination ◦ Mechanism of incorporation of cortisol into hair not known– is it from blood? Exocrine or sebaceous sources?

Cortisol Assays � Radioimmunoassay � Immunoassay - most common but may be at risk of cross reactivity with steroids other than cortisol (problematic in critically ill patients and in urine samples) � High pressure liquid chromatography (HPLC)/mass spectrometry
Measurement and Analysis �A single sample ◦ unreliable unless: �Collected accurately at a specific time of day for all subjects or �Collected accurately at a specific time of day related to known time of awakening � Diurnal Rhythm ◦ Unreliable unless collected accurately at correct times of day
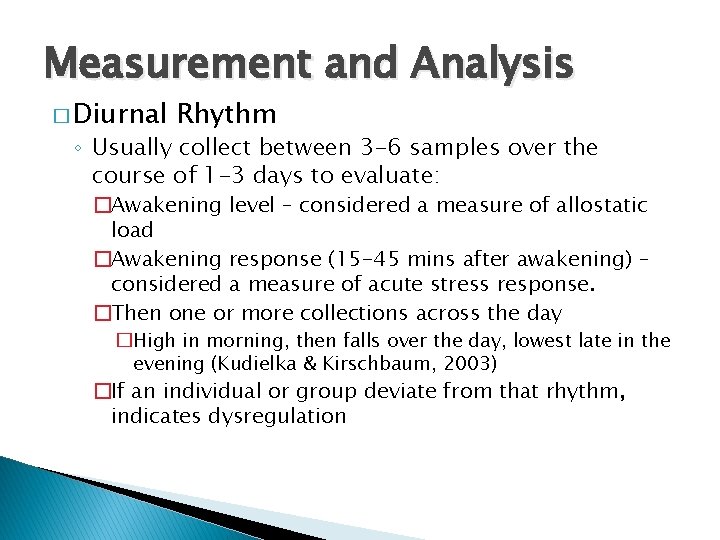
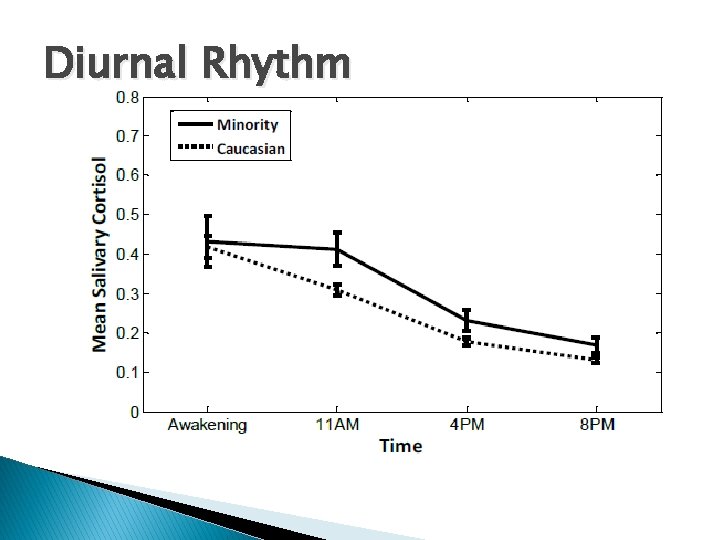
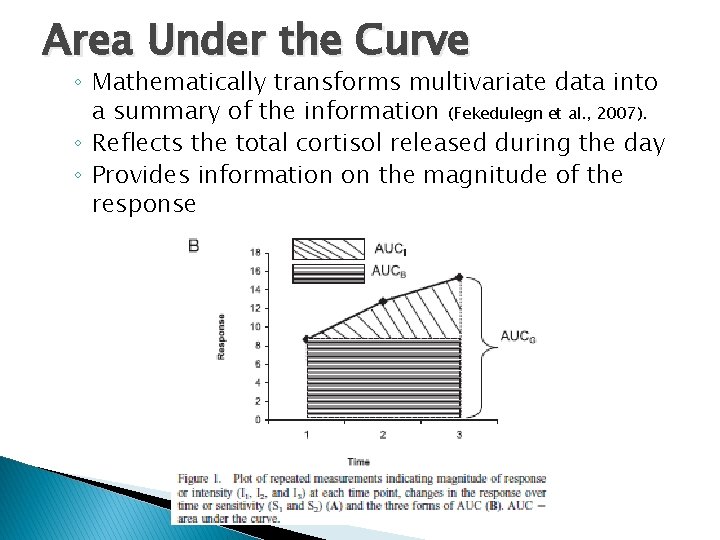
Measurement and Analysis � Diurnal Rhythm ◦ Usually collect between 3 -6 samples over the course of 1 -3 days to evaluate: �Awakening level – considered a measure of allostatic load �Awakening response (15 -45 mins after awakening) – considered a measure of acute stress response. �Then one or more collections across the day �High in morning, then falls over the day, lowest late in the evening (Kudielka & Kirschbaum, 2003) �If an individual or group deviate from that rhythm, indicates dysregulation
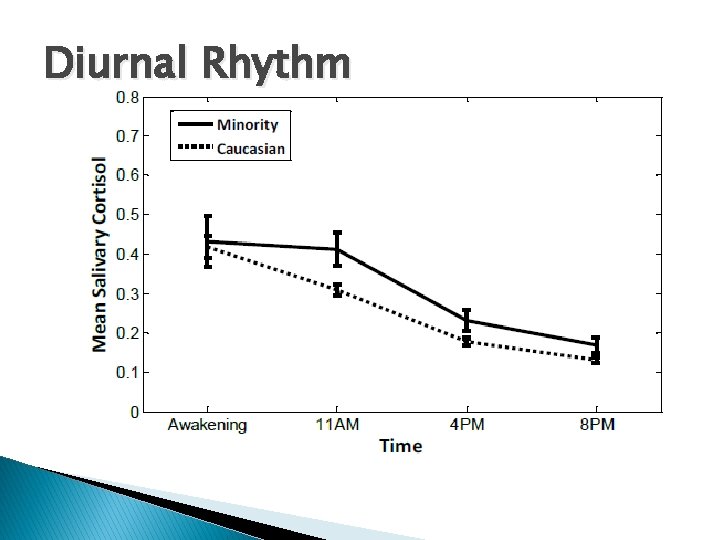
Diurnal Rhythm
![Awakening Response Awakening Response Pruessner 1997 30 min post awakening awakening Awakening Response � Awakening Response (Pruessner, 1997) [30 min post awakening] – [awakening]](https://slidetodoc.com/presentation_image/52656342c647f4871cfadfad0e477110/image-12.jpg)
Awakening Response � Awakening Response (Pruessner, 1997) [30 min post awakening] – [awakening]

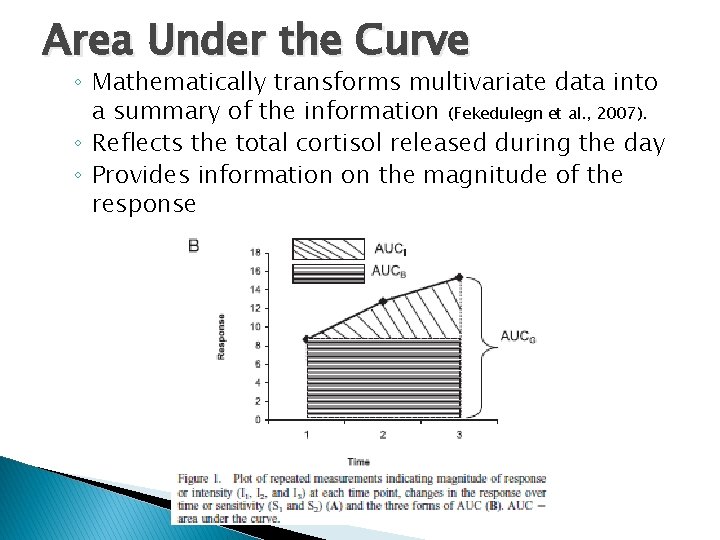
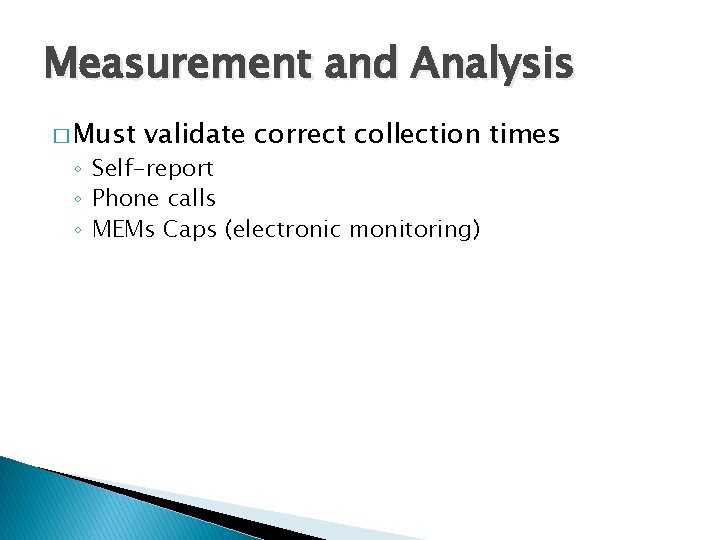
Area Under the Curve ◦ Mathematically transforms multivariate data into a summary of the information (Fekedulegn et al. , 2007). ◦ Reflects the total cortisol released during the day ◦ Provides information on the magnitude of the response
Measurement and Analysis � Must validate correct collection times ◦ Self-report ◦ Phone calls ◦ MEMs Caps (electronic monitoring)
Special Populations � Pregnant women ◦ Levels very high but maintain a diurnal rhythm ◦ Blood levels very high unless measure only free because CBG increases significantly blood = bound + free � Infants and toddlers
Thank you! � Questions?
References � � � Fekedulegn, D. B. , Andrew, M. E. , Burchfiel, C. M, et al. (2007). Area under the curve and other summary indicators of repeated waking cortisol measurements. Psychosomatic Medicine, 69, 651 -659. Kalra, S. , Einarson, A. , Karaskov, T. , Van Uums, S. , & Koren, G. , (2007). The relationship between stress and hair cortisol in healthy pregnant women. Clinical and Investigative Medicine, 30, E 103 -107. Kudielka, B. M. , Kirschbaum, C. (2003). Awakening cortisol response are influenced by health status and awakening time but not by menstrual cycle phase. Psychoneuroendocrinology, 28, 35 -47. Pruessner, J. , C. , Wolf, O. T. , Hellhammer, D. H. , et al. (1997). Free cortisol levels after awakening: a reliable biological marker for the assessment of adrenocortical activity. Life Science, 61, 2539 -2549. Russell, E. , Koren, G. , Rieder, M. , & Van Uum. (2012). Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology, 37, 589 -601.

Thyroid Stimulating Hormone and Cortisol Concentration � Serum cortisol levels among individuals with TSH levels >2. 0 u. IU/L (N=31) were significantly higher than among those individuals with TSH levels ≤ 2. 0 u. IU/L (N=20) [13. 83 ± 0. 93 ug/d. L vs. 8. 66 ± 0. 59 ug/d. L, respectively, F(1, 48)=14. 24, p<0. 0001]. � Walter, Corwin, Ulbrecht, Demers, Bennett, Whetzel, & Klein (2012). Thyroid Research.
Conversion Factor � To change cortisol from ◦ Microgram to nanomolar �Microgram x 2. 76 ;