LESSON 5 CARPIOPULMONARY RESUSCITATION CPR 2011 National Safety




- Slides: 35
LESSON 5 CARPIOPULMONARY RESUSCITATION (CPR) © 2011 National Safety Council 5 -1

Basic Life Support (BLS) • First aid given if victim’s breathing or heart stops • Often needed for victims of: - Heart attack Drowning Choking Other injuries/conditions © 2011 National Safety Council 5 -2
Overview of BLS • CPR = chest compressions + rescue breaths • Gets oxygen into lungs and oxygenated blood to vital organs © 2011 National Safety Council 5 -3
Overview of BLS continued • Choking care - Includes chest compressions - Expels an obstructing object from airway © 2011 National Safety Council 5 -4
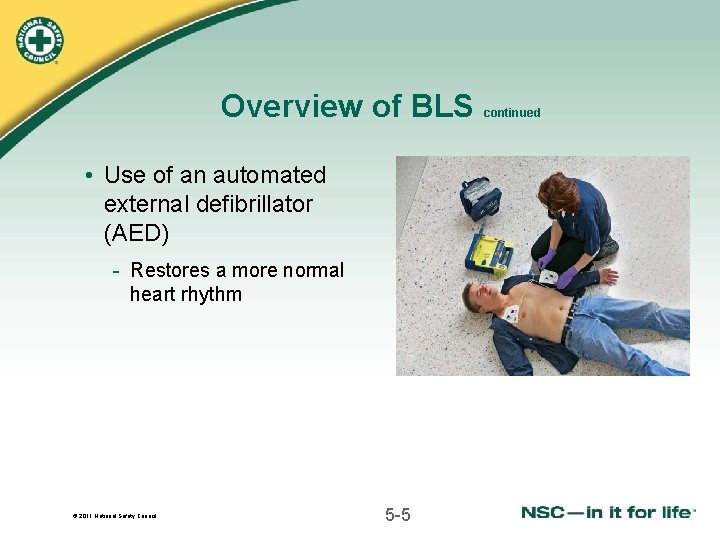
Overview of BLS • Use of an automated external defibrillator (AED) - Restores a more normal heart rhythm © 2011 National Safety Council 5 -5 continued
BLS Age Differences Infant = birth to 1 year Child = age 1 to the onset of puberty (for CPR and choking care); age 1 to 8 for AED Adult = past the age of puberty (or over age 8 for AED) © 2011 National Safety Council 5 -6
Respiratory Emergencies • Any illness or injury resulting in stopped breathing or inadequate breathing • Two types - Respiratory arrest - Respiratory distress © 2011 National Safety Council 5 -7
Respiratory Emergencies: Examples • Obstructed airway • Penetrating injury to chest • Carbon monoxide poisoning • Heart problem reducing tissue oxygen • Electrical shock disrupting breathing or heartbeat • Drug overdose or poisoning © 2011 National Safety Council 5 -8
Respiratory Arrest and Respiratory Distress • Respiratory arrest - Breathing has completely stopped • Respiratory distress - Breathing is difficult and may become ineffective © 2011 National Safety Council 5 -9

Cardiac Chain of Survival © 2011 National Safety Council 5 -10

Heart Attack – Acute Myocardial Infarction (AMI) • Sudden reduced blood flow to heart muscle • Medical emergency that often leads to cardiac arrest • Can occur at any age • Usually results from atherosclerosis © 2011 National Safety Council 16 -11
Facts About Heart Attack • Over 1, 255, 000 heart attacks occur a year in the United States, resulting in over 132, 000 deaths • Many could have been saved by first aid and medical treatment • More likely in those with family history • 1/5 of victims do not have chest pain • Victims typically deny they are having a heart attack © 2011 National Safety Council 16 -12
Symptoms of Heart Attack • Can vary from vague chest discomfort to crushing pain with or without other symptoms • May have no signs and symptoms before suddenly collapsing • May have milder symptoms that come and go before heart attack occurs © 2011 National Safety Council 16 -13
Symptoms of Heart Attack continued • In women chest pain or discomfort most common symptom - Also more likely to have shortness of breath, jaw or back pain, indigestion, nausea and vomiting - http: //www. youtube. com/watch? v=t 7 wm. PWTn. Db. E © 2011 National Safety Council 16 -14
Symptoms of Heart Attack continued • Consider possibility of heart attack with wide range of symptoms - Don’t expect a clearly defined situation • Act quickly because deaths usually occur with an hour or two of symptoms © 2011 National Safety Council 16 -15
Aspirin and Heart Attack • Many patients at risk for cardiovascular disease advised to take one low-dose aspirin daily unless allergic or experience side effects • For victims who do not need to avoid aspirin, chewing one uncoated adult aspirin or two low-dose baby aspirin is now recommended when experiencing heart attack symptoms © 2011 National Safety Council 16 -16
Nitroglycerin for Heart Attack • Increases blood flow by dilating arteries • Often prescribed for angina - Type of chest pain caused by narrowed coronary arteries • Comes in tablets, sprays and patches © 2011 National Safety Council 16 -17
Nitroglycerin for Heart Attack • Can assist victim with prescribed nitroglycerine - Follow victim’s instructions - Do not attempt to give if victim unresponsive © 2011 National Safety Council 16 -18 continued
First Aid for Heart Attack 1. Call 9 -1 -1 immediately. 2. Help victim into comfortable position. Loosen any tight clothing. 3. Ask victim about medications. 4. Encourage the victim to chew one uncoated adult or two low-dose baby aspirin (unless allergic). 5. Stay with victim. Be reassuring. © 2011 National Safety Council 16 -19
Call First/Call Fast Call First (before starting CPR): • Any unresponsive adult who is not breathing normally Call Fast (after giving about two minutes of CPR): • Any infant or child who is unresponsive and not breathing normally © 2011 National Safety Council 5 -20

Use of CPR for unresponsiveness and lack of normal breathing caused by: • Heart attack • Electric shock • Drowning • Certain injuries • Suffocation • Stroke • Allergic reaction • Diabetic emergency • Prolonged seizures • Drug overdose © 2011 National Safety Council 5 -21
CPR Saves Lives • CPR and defibrillation within 3 -5 minutes can save over 50% of cardiac arrest victims • CPR followed by AED saves thousands of lives each year • In most cases CPR helps keep victim alive until EMS or AED arrives © 2011 National Safety Council 5 -22
CPR Technique If unresponsive and not breathing start CPR with chest compressions: • Find correct hand position • Compress chest hard and fast at rate of at least 100 compressions/minute • Alternate 30 compressions and 2 rescue breaths • Give each breath over one second © 2011 National Safety Council 5 -23
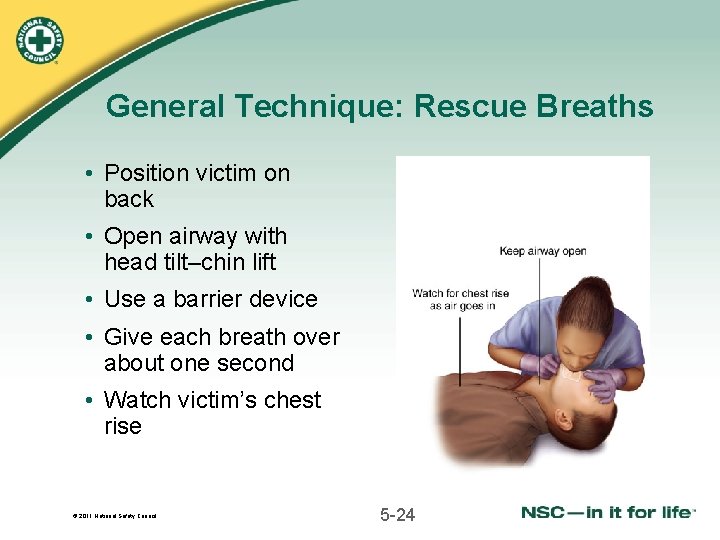
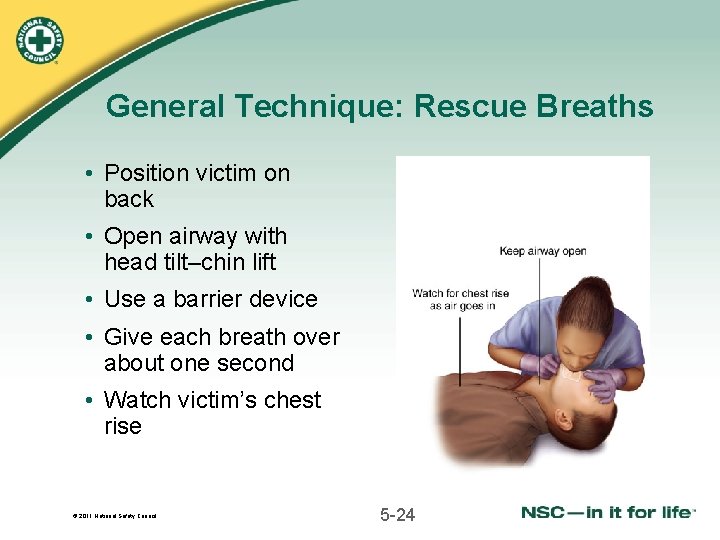
General Technique: Rescue Breaths • Position victim on back • Open airway with head tilt–chin lift • Use a barrier device • Give each breath over about one second • Watch victim’s chest rise © 2011 National Safety Council 5 -24
General Technique: Rescue Breaths continued • Do not blow harder than needed to make chest rise • After each breath let air escape and chest fall • Blowing in too forcefully or for too long may cause vomiting © 2011 National Safety Council 5 -25
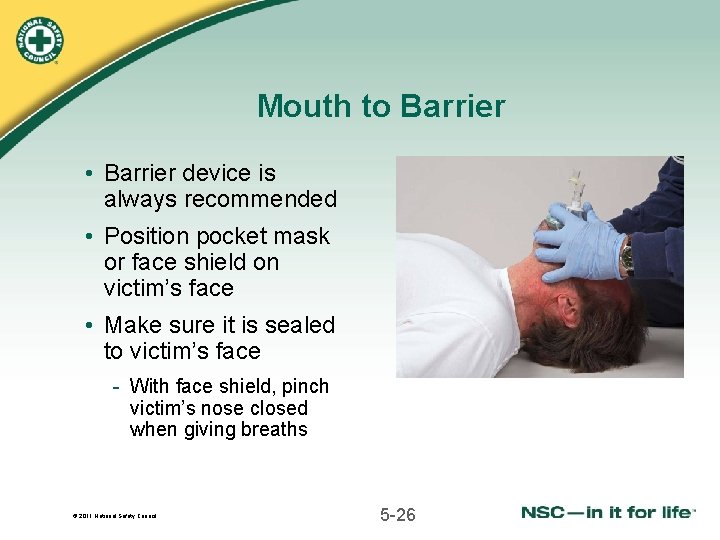
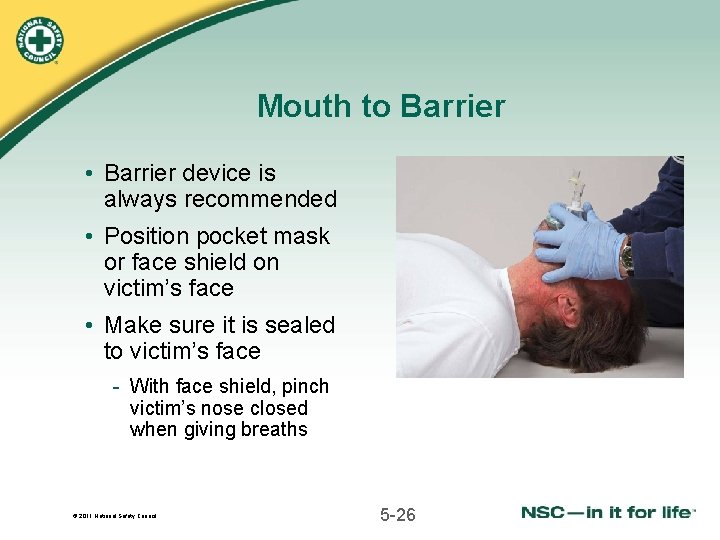
Mouth to Barrier • Barrier device is always recommended • Position pocket mask or face shield on victim’s face • Make sure it is sealed to victim’s face - With face shield, pinch victim’s nose closed when giving breaths © 2011 National Safety Council 5 -26
Potential Problem: Vomiting • To prevent air from entering stomach and causing vomiting - Open airway before giving breaths Watch chest rise as you give breaths Blow slowly and steadily Stop each breath when chest rises Let chest fall after each breath © 2011 National Safety Council 5 -27
SKILL: CPR FOR ADULTS, CHILDREN AND INFANTS (1 RESCUER) © 2011 National Safety Council 5 -28
Assess the Victim 1 Determine that victim is unresponsive and not breathing normally Have someone call 9 -1 -1, or call yourself if alone, and get an AED Begin CPR © 2011 National Safety Council 5 -29
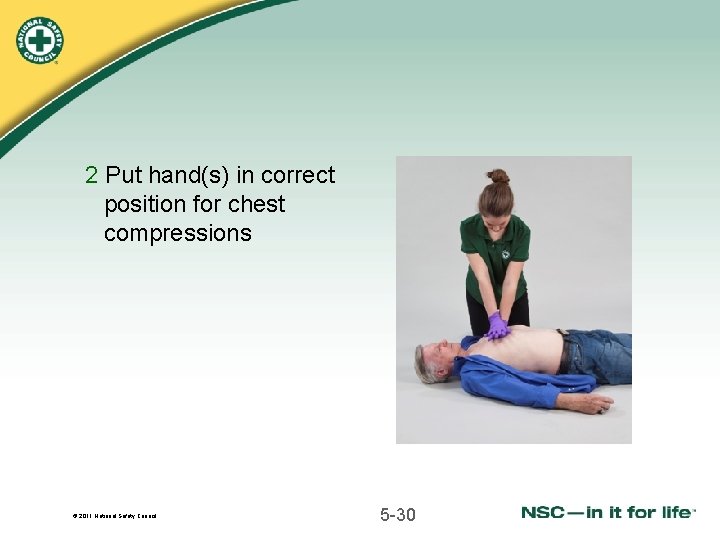
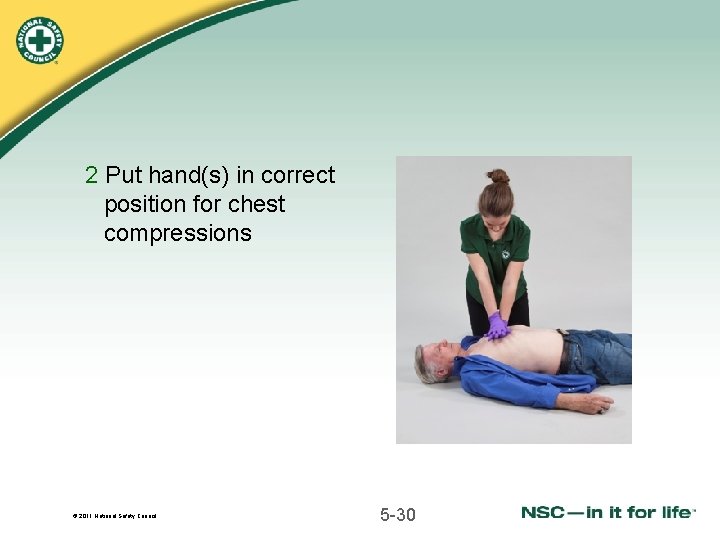
2 Put hand(s) in correct position for chest compressions © 2011 National Safety Council 5 -30
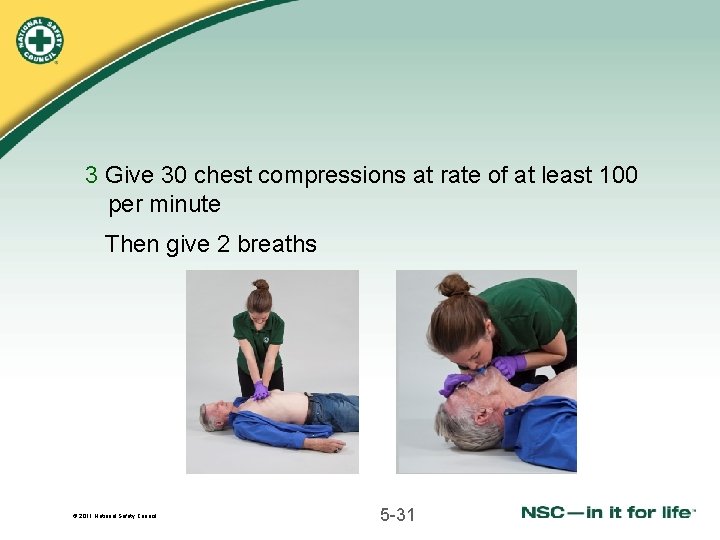
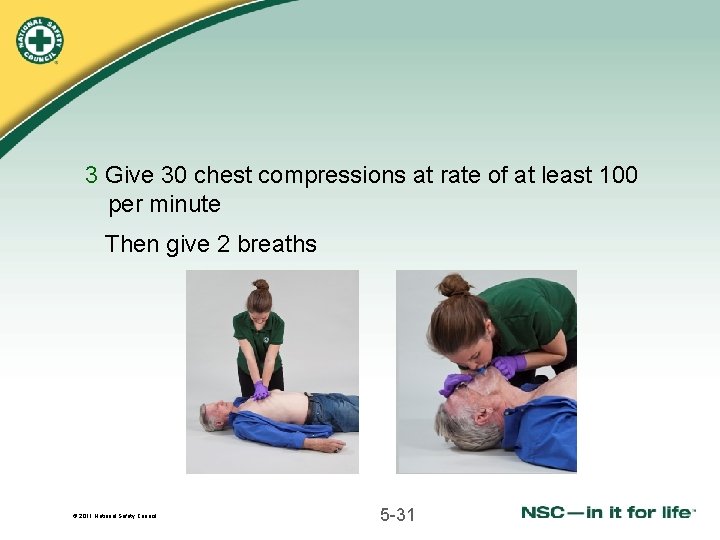
3 Give 30 chest compressions at rate of at least 100 per minute Then give 2 breaths © 2011 National Safety Council 5 -31
4 Open airway Give two rescue breaths, each lasting one second - If first breath does not go in, reposition head and try again - If second breath still does not go in, give care for choking © 2011 National Safety Council 5 -32
5 Continue cycles of 30 compression and two breaths 6 Continue CPR until: • Victim wakes up • AED brought to scene and ready to use • Professional help arrives to take over • Scene becomes dangerous • You become too exhausted © 2011 National Safety Council 5 -33
7 If victim starts breathing normally but is unresponsive, put in recovery position and monitor breathing When AED arrives, start AED sequence © 2011 National Safety Council 5 -34
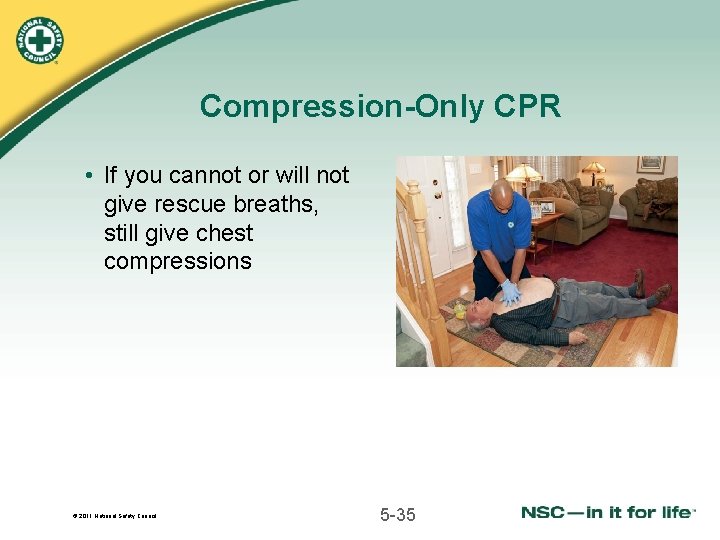
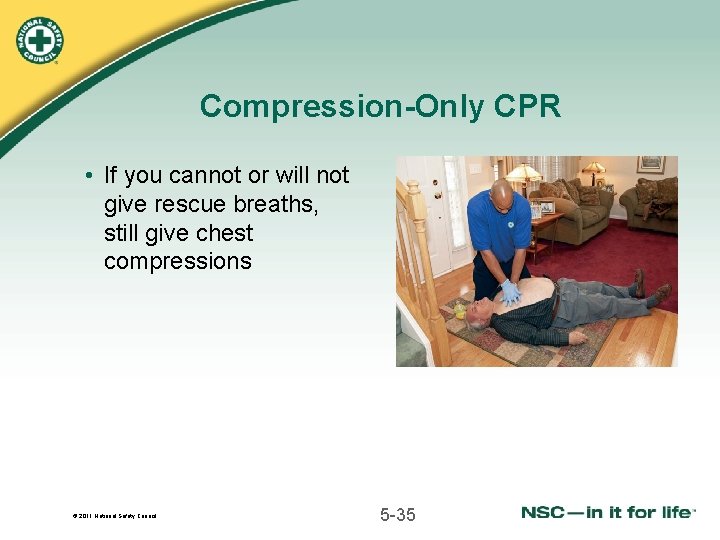
Compression-Only CPR • If you cannot or will not give rescue breaths, still give chest compressions © 2011 National Safety Council 5 -35
 Resuscitation cpr
Resuscitation cpr Introduction for cpr
Introduction for cpr Srfac
Srfac For adult
For adult Difference between resuscitation and resurrection
Difference between resuscitation and resurrection Acute resuscitation plan
Acute resuscitation plan Dope neonatal resuscitation
Dope neonatal resuscitation Indication of bed bath
Indication of bed bath Amber bundle
Amber bundle Endpoint of resuscitation
Endpoint of resuscitation Pediatric broselow tape
Pediatric broselow tape Principle of resuscitation
Principle of resuscitation European resuscitation council
European resuscitation council European resuscitation council
European resuscitation council Bls
Bls 17:7 providing first aid for heat exposure
17:7 providing first aid for heat exposure Neonatal resuscitation definition
Neonatal resuscitation definition Preterm classification
Preterm classification Management of asphyxia neonatorum after resuscitation
Management of asphyxia neonatorum after resuscitation Apgar
Apgar Cardioprotection resuscitation
Cardioprotection resuscitation Push hard push fast fully recoil
Push hard push fast fully recoil Parkland formula
Parkland formula National population and housing census 2011
National population and housing census 2011 6 ministerial priorities of health
6 ministerial priorities of health Extracorporeal cpr
Extracorporeal cpr Definasi pertolongan cemas
Definasi pertolongan cemas Perbedaan cpr dan mpr
Perbedaan cpr dan mpr Infant cpr algorithm
Infant cpr algorithm Cpr objectives
Cpr objectives Cpr objectives
Cpr objectives Secondary survey first aid
Secondary survey first aid Llf first aid
Llf first aid Sam approach cpr
Sam approach cpr Cpr hand placement sternum
Cpr hand placement sternum For adult
For adult