LEPROSY Period 2 Introduction Leprosy is also commonly



- Slides: 12
LEPROSY Period 2
Introduction ■ Leprosy is also commonly called Hansen’s Disease, after G. H. Armauer Hansen who discovered the cause of the disease in 1873. ■ The disease is caused by the bacteria Mycobacterium leprae or M. lepromatosis bacteria. ■ This bacteria was the first bacterium discovered to be the cause of disease in humans. Mycobacterium leprae

Transmission Structure of M. leprae ■ The transmission of leprosy is airborne. ■ When an infected person sneezes or coughs, tiny droplets containing the fluid are expelled and a nearby person can breathe them in. ■ Contrary to popular belief, prolonged personal contact is needed to catch leprosy. ■ Leprosy is only found in humans and armadillos, specifically armadillos found in the Southern United States. However, the risk of transmission from aardvarks to humans is very low. ■ M. leprae is known to have the largest doubling period of any known bacteria, meaning it is nearly impossible to grow in a lab. It is aerobic and gram-positive, while also being surrounded by a waxy coating that is unique to it.

Symptoms ■ Leprosy is characterized by: -Hair loss, specifically eyebrows or eyelashes -Ulcers on soles of feet -Swelling or lumps on face or earlobes -Growths on the skin (Nodules) Hands of someone with untreated leprosy -Flat, faded, discolored patches of skin -Facial disfigurement -Loss of digits ■ When nerves are damaged, the following symptoms may occur: -Numbness of affected skin -Eye problems/blindness -Muscle weakness/paralysis -enlarged nerves ■ Other Symptoms include: -Stuffy nose -Nosebleeds
Progression ■ Because of M. leprae’s long cycle of multiplication, Leprosy has a long incubation period. ■ The average incubation period is five years, but has been known to last as long as 20. ■ The progression of leprosy depends on the type of leprosy the person has. Tuberculoid leprosy is less serious, and usually only results in skin lesions. Lepromatous leprosy can result in nerve damage, destruction of bones and cartilage, and blindness. ■ Symptoms usually get more serious over time if left untreated, and can result in permanent disfigurement Progression of Symptoms: Early Symptoms: • Loss of temperature sensation • Loss of touch sensation • Numbness • Pins and Needles Sensation Advanced Symptoms: • Blindness • Crippling of hands and feet • Face disfigurement • Shortening of toes and fingers • Chronic Ulcers • Hair loss
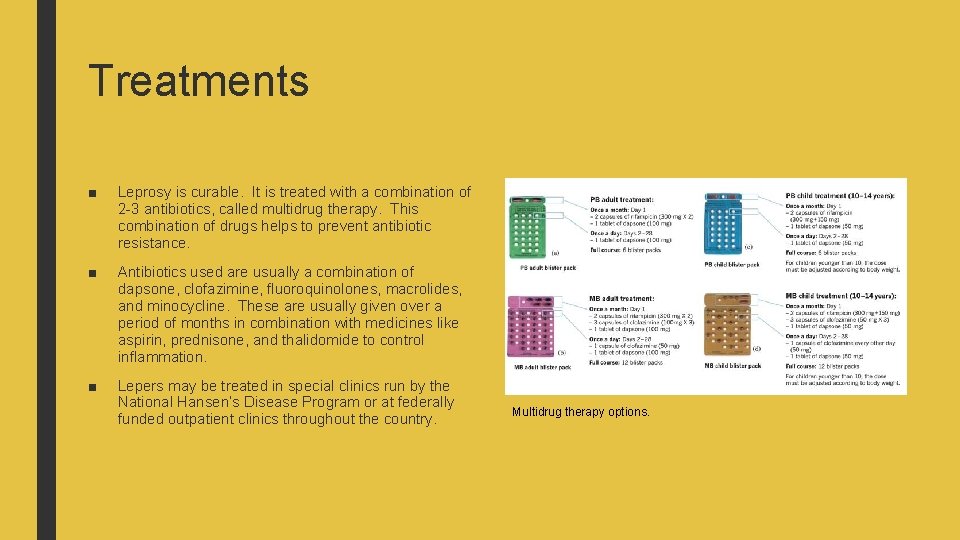
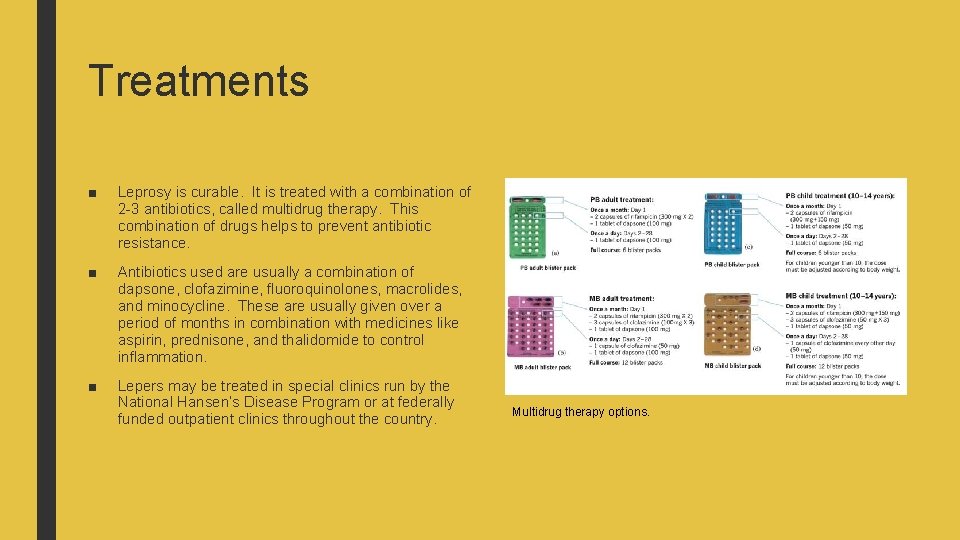
Treatments ■ Leprosy is curable. It is treated with a combination of 2 -3 antibiotics, called multidrug therapy. This combination of drugs helps to prevent antibiotic resistance. ■ Antibiotics used are usually a combination of dapsone, clofazimine, fluoroquinolones, macrolides, and minocycline. These are usually given over a period of months in combination with medicines like aspirin, prednisone, and thalidomide to control inflammation. ■ Lepers may be treated in special clinics run by the National Hansen’s Disease Program or at federally funded outpatient clinics throughout the country. Multidrug therapy options.
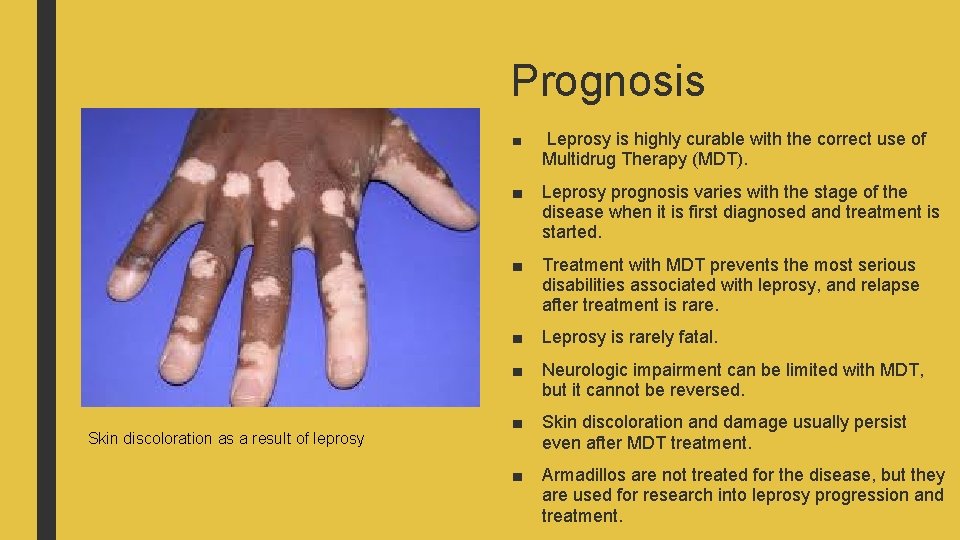
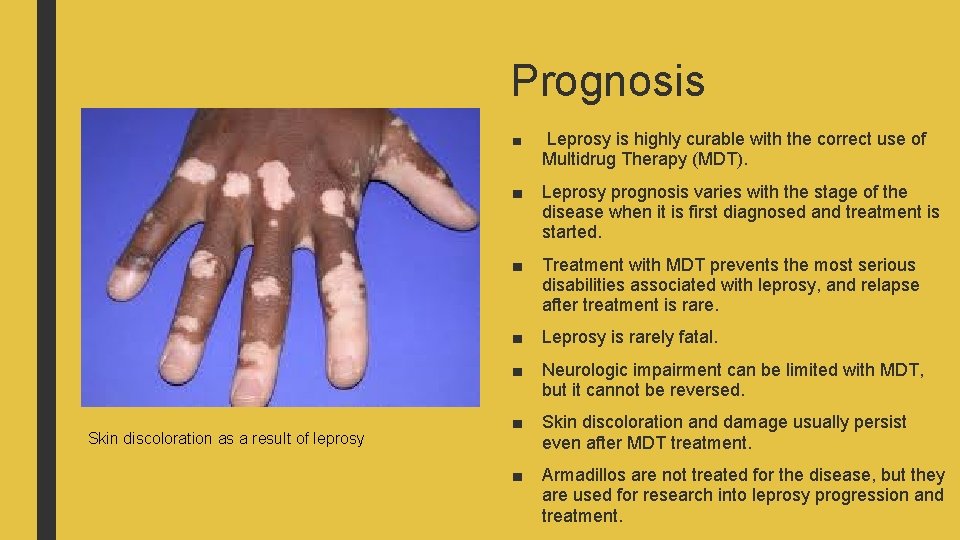
Prognosis Skin discoloration as a result of leprosy ■ Leprosy is highly curable with the correct use of Multidrug Therapy (MDT). ■ Leprosy prognosis varies with the stage of the disease when it is first diagnosed and treatment is started. ■ Treatment with MDT prevents the most serious disabilities associated with leprosy, and relapse after treatment is rare. ■ Leprosy is rarely fatal. ■ Neurologic impairment can be limited with MDT, but it cannot be reversed. ■ Skin discoloration and damage usually persist even after MDT treatment. ■ Armadillos are not treated for the disease, but they are used for research into leprosy progression and treatment.
Prevention ■ The biggest step in the prevention of leprosy is early diagnosis and treatment to prevent the further spread of the disease. ■ There is no vaccine against leprosy, but the vaccine against tuberculosis, called the BCG vaccine, may offer some protection. This is because the two diseases are closely related. ■ If someone is known to be infected with leprosy, they should be kept out of school, preschool, childcare, and work to avoid spreading the disease. ■ Because Leprosy requires close, prolonged contact to spread, travelers are not at high risk for the disease.
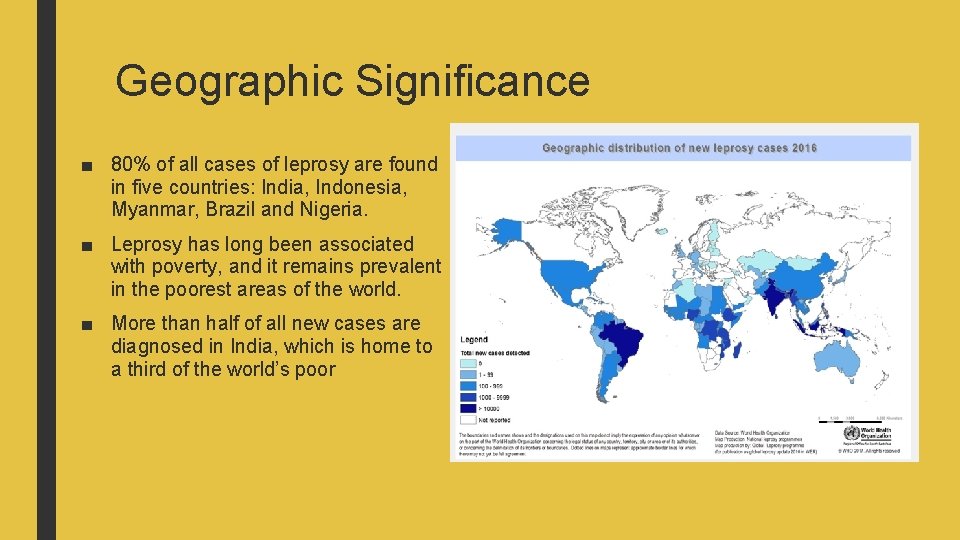
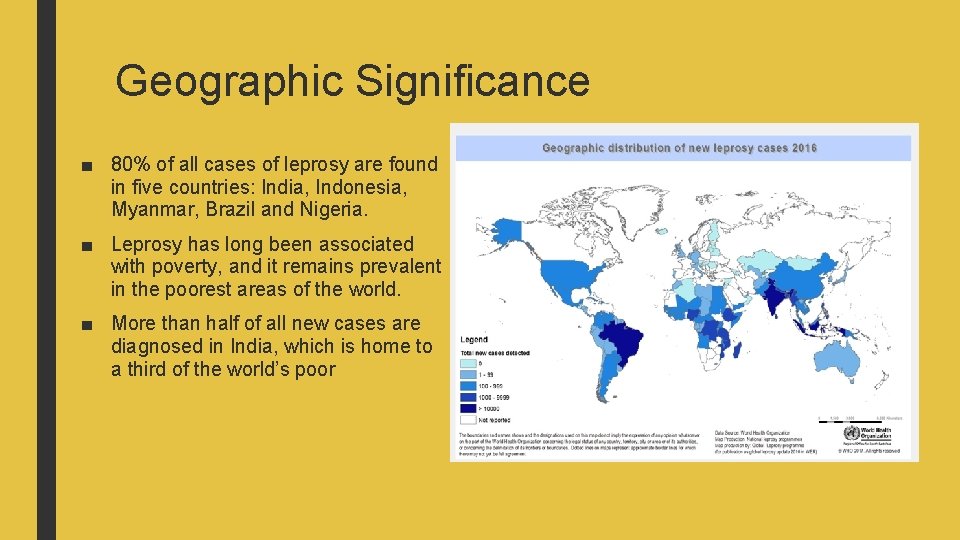
Geographic Significance ■ 80% of all cases of leprosy are found in five countries: India, Indonesia, Myanmar, Brazil and Nigeria. ■ Leprosy has long been associated with poverty, and it remains prevalent in the poorest areas of the world. ■ More than half of all new cases are diagnosed in India, which is home to a third of the world’s poor

Notable Outbreaks ■ It is thought that leprosy originated in India or Africa. In the ancient world, it was prevalent throughout the Middle East, Africa, the Mediterranean, and India. ■ During the Middle Ages in Europe, leprosy was though to be a punishment from God. Excessive poverty and ignorance of germ theory led to large outbreaks of the disease. By the year 1200, there were around 19, 000 leper colonies throughout Europe. ■ During the Crusades, there was an especially large outbreak of leprosy along trade routes in Europe and throughout European-occupied areas of the holy Land. ■ In Norway, the disease remained fairly common until the 20 th century. ■ Small outbreaks of leprosy occurred in Louisiana in 1775 and in Minnesota among people of Scandinavian heritage in the mid-1900 s.
Additional Resources ■ CDC, “Hansen’s Disease (Leprosy)” https: //www. cdc. gov/leprosy/index. html ■ Medline. Plus, “Leprosy” https: //medlineplus. gov/ency/article/001347. htm ■ Leprosy (Hansen’s Disease) -- an overview https: //youtu. be/Yn. Gv. LVk 2 BD 0
References ■ Leprosy. (2018). Retrieved from http: //www. who. int/news-room/fact■ Leprosy (Hansen’s Disease). (n. d. ). Retrieved from https: //www 2. health. vic. gov. au/public-health/infectious-diseases/diseaseinformation-advice/leprosy ■ Leprosy (Hansen’s Disease). (n. d. ). Retrieved from https: //www. betterhealth. vic. gov. au/health/conditionsandtreatments/leprosy ■ Ngan, V. (2003). Leprosy. Retrieved from https: //www. dermnetnz. org/topics/leprosy/