Legal Aspects of Professional Nursing Catherine Hrycyk MSc






- Slides: 33
Legal Aspects of Professional Nursing Catherine Hrycyk, MSc. N, RN
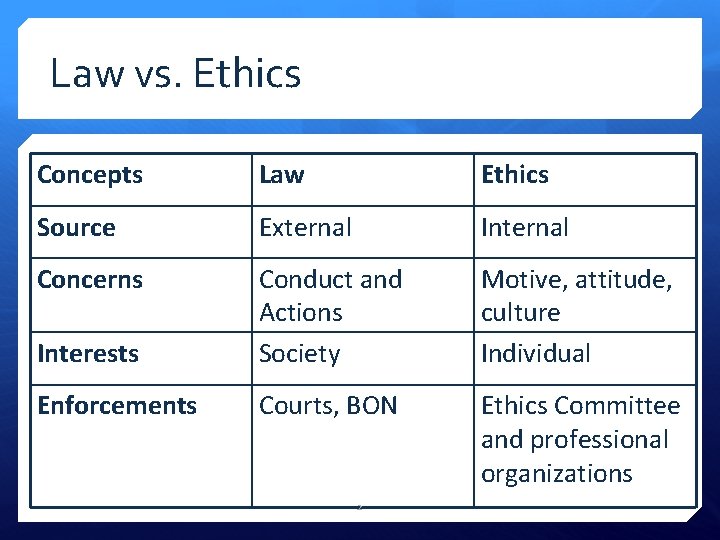
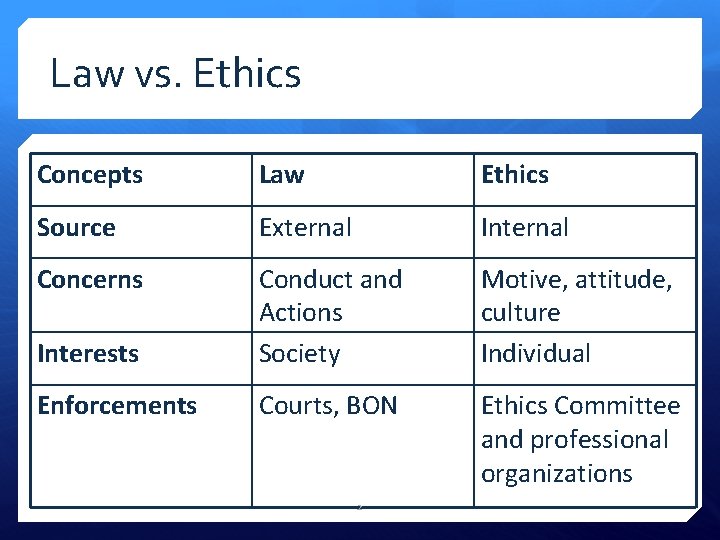
Law vs. Ethics Concepts Law Ethics Source External Internal Concerns Interests Conduct and Actions Society Motive, attitude, culture Individual Enforcements Courts, BON Ethics Committee and professional organizations 2
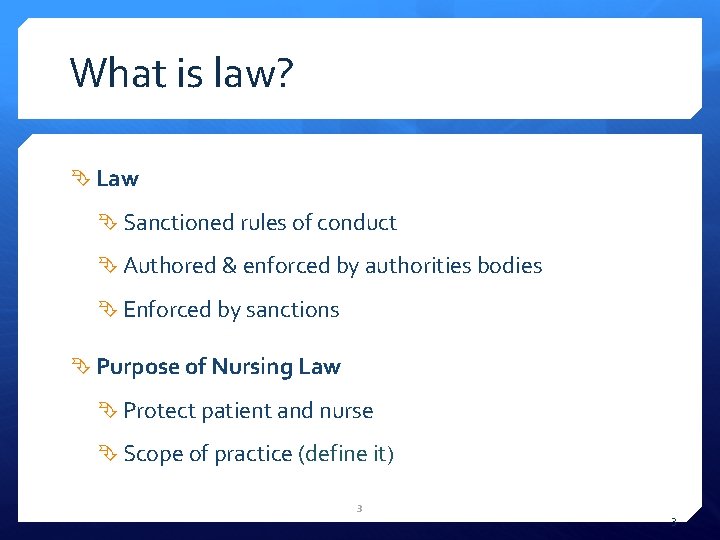
What is law? Law Sanctioned rules of conduct Authored & enforced by authorities bodies Enforced by sanctions Purpose of Nursing Law Protect patient and nurse Scope of practice (define it) 3 3
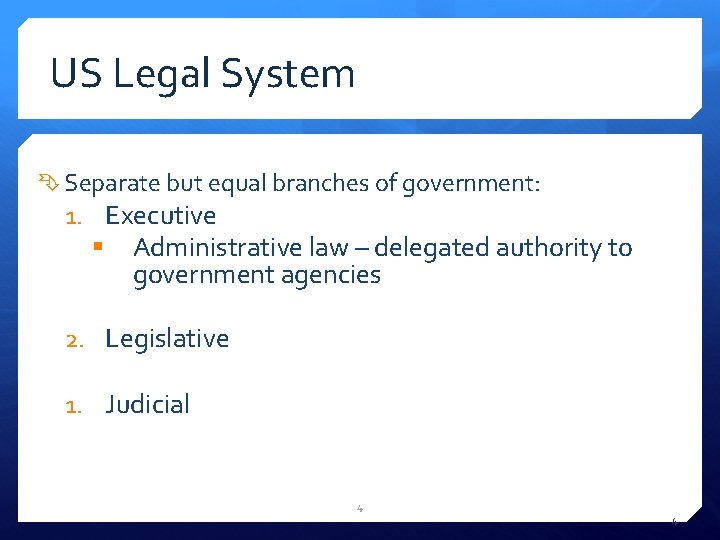
US Legal System Separate but equal branches of government: 1. Executive § Administrative law – delegated authority to government agencies 2. Legislative 1. Judicial 4 4
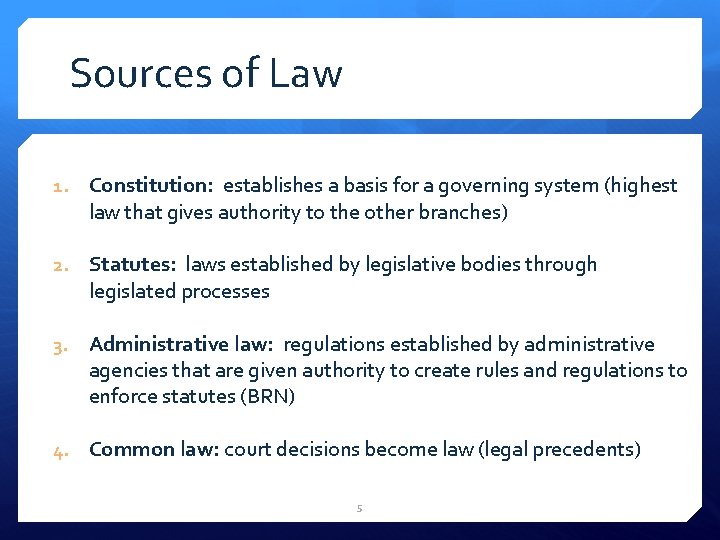
Sources of Law 1. Constitution: establishes a basis for a governing system (highest law that gives authority to the other branches) 2. Statutes: laws established by legislative bodies through legislated processes 3. Administrative law: regulations established by administrative agencies that are given authority to create rules and regulations to enforce statutes (BRN) 4. Common law: court decisions become law (legal precedents) 5

Types of Law Criminal law: Sanctions acts against an individual or society Innocent until proven guilty beyond a reasonable doubt Sanctions range from fine to jail to death penalty Civil law: Regulates right and duties of legal subjects Usually financial sanction, possible imprisonment Administrative law: Regulates work of public agencies (e. g. BRN) Public agencies and bodies specific regulatory powers 6 6
State Boards of Nursing, Nursing Practice Acts, and Licensure Purpose of licensing: To protect the public health, safety, and welfare Ways to get licensed Nursing Practice Act Defines and controls nursing State Boards of Nursing Regulatory bodies The legislature delegates authority to enforce the law to an executive agency – board of nursing. The board of nursing enforces the laws and publicizes rules and regulations that expand the law 7
Nursing Practice Regulations California Board of Registered Nurses (BRN): Regulates nursing practice in California Creates Rules and Regulations to administer the Nurse Practice Act (NPA) Describes rules of conduct for nurses Registered Nurses Act California 8
Informed Consent Legal expression of the ethical principle of autonomy: Implicit Explicit Obtained by the person performing the procedure When obtained by another practitioner, nurse’s role: witness / monitor Emergency consent is presumed when patient unable to provide Nurses role is to make sure pt. understands everything and that the person that signs is the person who needs to be signing! 9
Capacity to Consent Decision-making capacity (not competency) determined by: Appreciation of right to make the choice Understanding of risks/benefits of procedure Understanding of risks/benefits of opting out of procedure Ability to communicate decision: Communication may not always be verbal Professional interpreter to assist with language issues Use layman jargon 10
Assault and Battery Assault is a threat or an attempt to make bodily contact with another person without the person’s consent No contact required Any action that would make a reasonable person in simillar condition feel threatened Impermissible, unprivileged touching of one person by another Contact required 11
Advance Directives Sometime generically called “Living Will” Allow patient to exercise autonomy if incapacitated Not same as DNR (do not resuscitate) DNR is exactly what it’s called – DNR nothing more and nothing less! Advanced Directives documents stating the pts wishes for healthcare interventions if they should become incapacitated 12
Advance Directives Directive to healthcare providers and family or surrogate Documents patients’ wishes for treatment or withdrawal Durable Power of Attorney for Health Care Patient designates another person as their decision maker Out of Hospital Do-Not-Resuscitate Order Allows competent adults to refuse life sustaining procedures when out of the hospital setting. Can include not wanting to be taken to ER, let me sit here and die… Declaration of Mental Health Treatment Allows a court to determine incapacity and allows the pt to refuse electro convulsive therapy (ECT) and psychoactive drugs 13

Special Situations… Advance directive not available: Autonomy versus “best interest” of clients Substituted judgment Surrogate decision maker appointed Dementia clients: Dementia diagnosis does not necessarily mean the pt is incapable of making their own decisions Careful interprofessional assessment essential 14

The Patient Self-Determination Act Acute care and long-term care facilities must: 1. Provide written information to all adult patients about their rights under state law 2. Ensure institutional compliance with state laws on advance directives 3. Provide for education of staff and the community on advance directives 4. Document in the medical record whether the patient has an advance directive 15 15

Confidentiality Nurses must keep information obtain while providing care confidential Legal and ethical issue: Regulated by federal and state statutes Ethical aspects addressed in ANA Code of Ethics Exceptions and limitations (e. g. mandatory reporting of abuse, public health reporting rules, etc. ) 16
HIPAA Health Information Portability and Accountability Act (1996) Protects the privacy of health information Nurse can communicate patient info to insurance agencies and/or other providers involved in the care of a patient to the extent required to maintain continuity of care or for billing purposes Patients have right to obtain copies of their health records Custodian of the records must provide them within reasonable amount of time 17 17
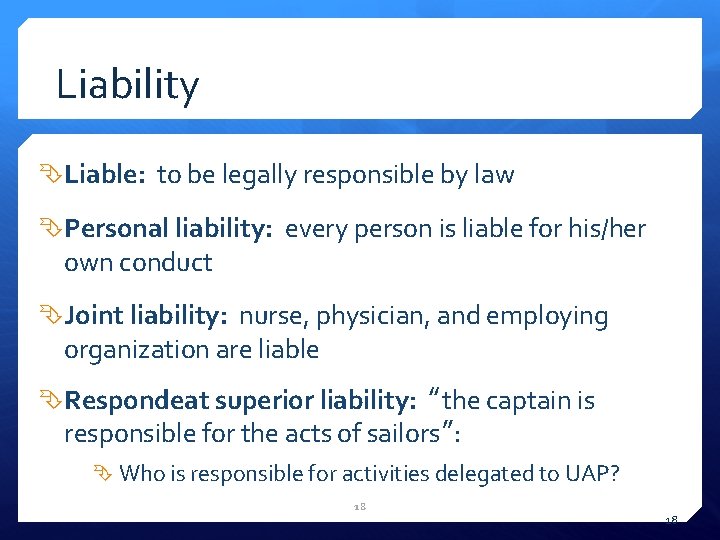
Liability Liable: to be legally responsible by law Personal liability: every person is liable for his/her own conduct Joint liability: nurse, physician, and employing organization are liable Respondeat superior liability: “the captain is responsible for the acts of sailors”: Who is responsible for activities delegated to UAP? 18 18
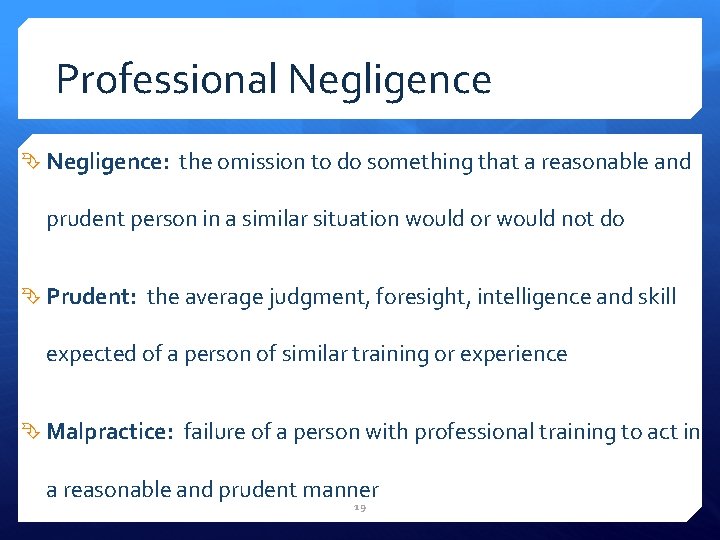
Professional Negligence: the omission to do something that a reasonable and prudent person in a similar situation would or would not do Prudent: the average judgment, foresight, intelligence and skill expected of a person of similar training or experience Malpractice: failure of a person with professional training to act in a reasonable and prudent manner 19
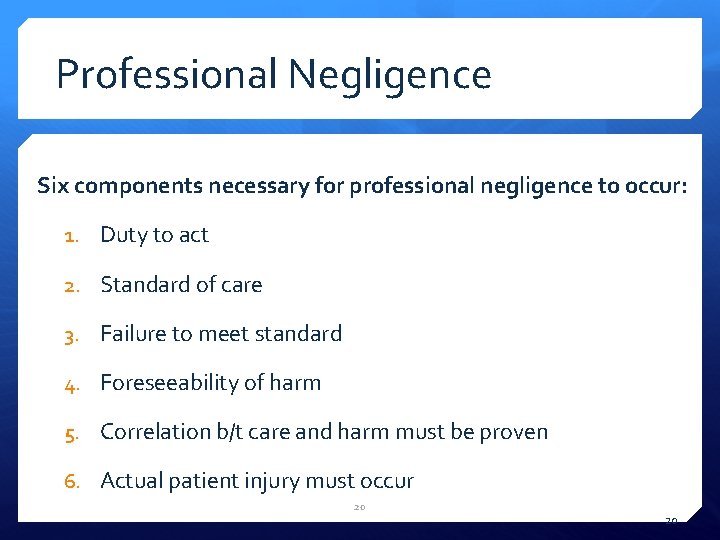
Professional Negligence Six components necessary for professional negligence to occur: 1. Duty to act 2. Standard of care 3. Failure to meet standard 4. Foreseeability of harm 5. Correlation b/t care and harm must be proven 6. Actual patient injury must occur 20 20
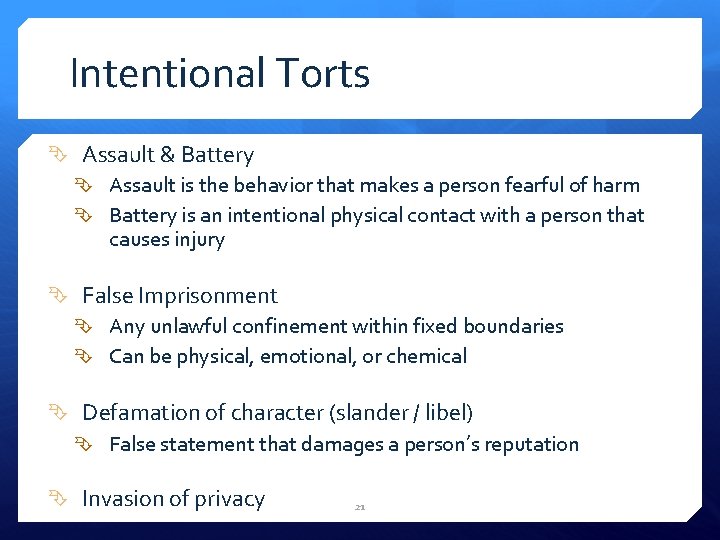
Intentional Torts Assault & Battery Assault is the behavior that makes a person fearful of harm Battery is an intentional physical contact with a person that causes injury False Imprisonment Any unlawful confinement within fixed boundaries Can be physical, emotional, or chemical Defamation of character (slander / libel) False statement that damages a person’s reputation Invasion of privacy 21

Preventing Negligence and Malpractice Meet the standard of care (Including accurate documentation!) Practice in a safe setting Question authority Follow up on unsafe situations / practices The Joint Commission and 2005 Patient Safety Goals Effective communication with patients, families and other health professionals and agencies Carry and understand professional liability insurance Promote positive interpersonal relationships 22
Claims Against Nurses Examples: Inadequate charting. Inadequate communication regarding changes in condition Leaving potentially harmful items within patient reach Unattended patient falls Inaccurate counting of operative instruments & sponges Misidentifying patients for medications, surgeries & tests 23 23
Incident Reports Administrative documents Intended to improve systems and processes Not part of the patient chart Unusual / unexpected incidents DO: Document incident information, treatment & follow up on chart Notify Nursing Management & Risk Management DO NOT: Leave copy on chart or document form completion in chart 24 Discuss with pt / family
Causes of License Suspension Professional negligence Practicing nursing w/o a license Obtain license by fraud Felony convictions Not reporting substandard medical or nursing care Providing patient care under the influence of drugs/alcohol Giving narcotics w/o order Falsely portraying self to public or any HCP as a nurse 25
Other Important Regulations Whistleblower Act Prevents employers from taking retaliatory action against nurses for reporting improper patient care or business practices Good Samaritan Act Generally, a nurse is not liable for injury that occurs as a result of emergency treatment, provided that: Care is provided at the scene of emergency The care is not grossly negligent 26
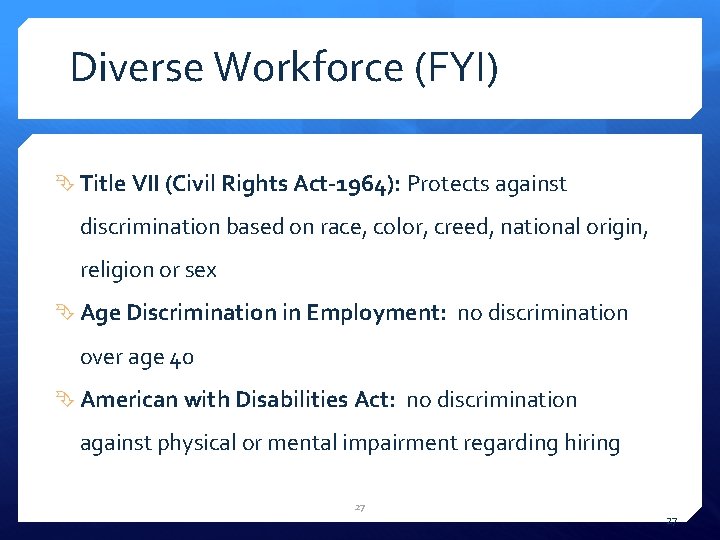
Diverse Workforce (FYI) Title VII (Civil Rights Act-1964): Protects against discrimination based on race, color, creed, national origin, religion or sex Age Discrimination in Employment: no discrimination over age 40 American with Disabilities Act: no discrimination against physical or mental impairment regarding hiring 27 27
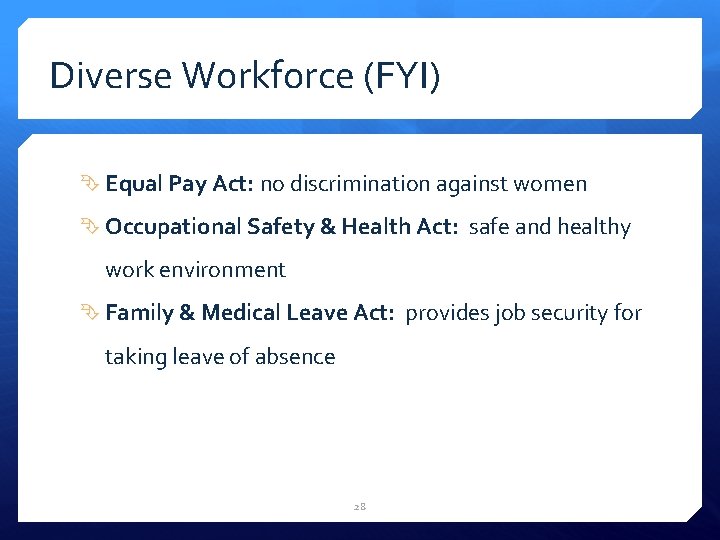
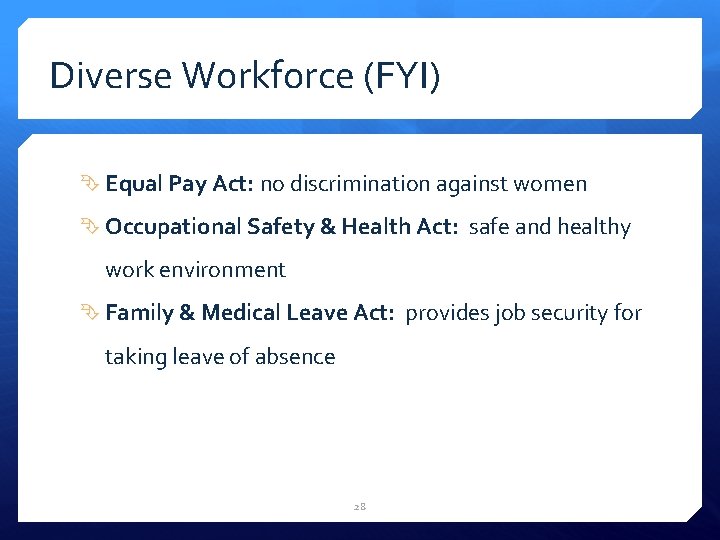
Diverse Workforce (FYI) Equal Pay Act: no discrimination against women Occupational Safety & Health Act: safe and healthy work environment Family & Medical Leave Act: provides job security for taking leave of absence 28
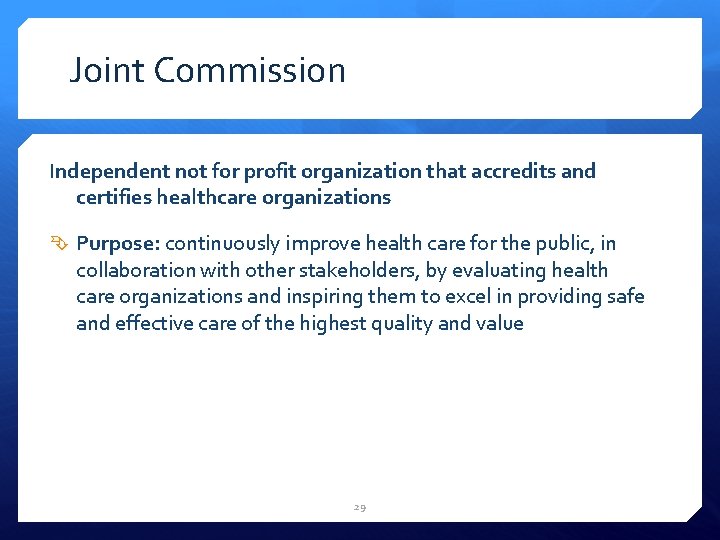
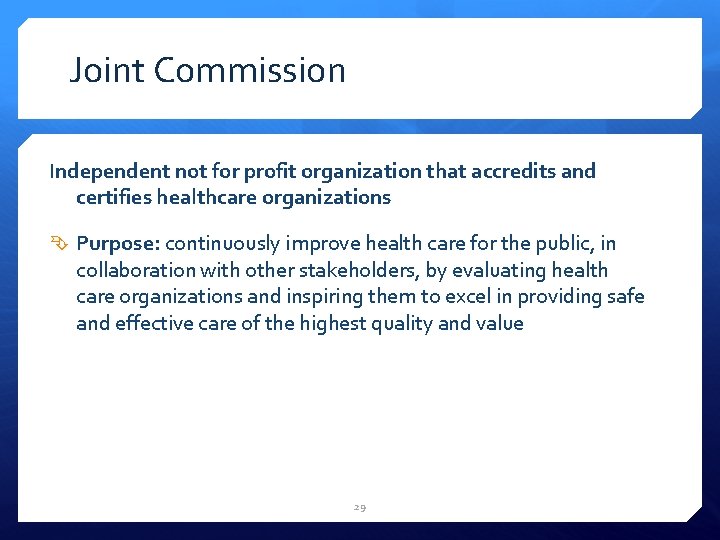
Joint Commission Independent not for profit organization that accredits and certifies healthcare organizations Purpose: continuously improve health care for the public, in collaboration with other stakeholders, by evaluating health care organizations and inspiring them to excel in providing safe and effective care of the highest quality and value 29
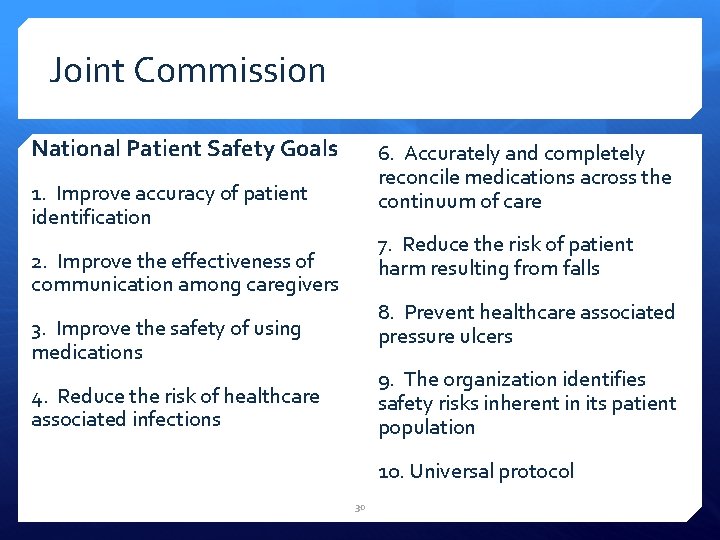
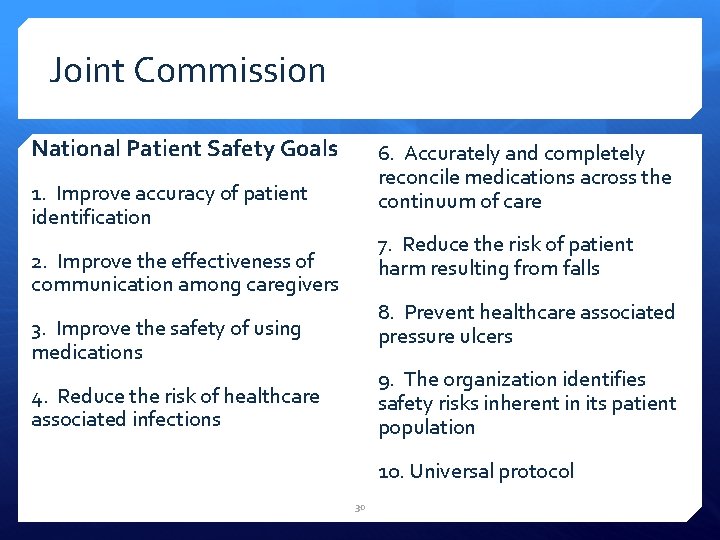
Joint Commission National Patient Safety Goals 6. Accurately and completely reconcile medications across the continuum of care 1. Improve accuracy of patient identification 7. Reduce the risk of patient harm resulting from falls 2. Improve the effectiveness of communication among caregivers 8. Prevent healthcare associated pressure ulcers 3. Improve the safety of using medications 9. The organization identifies safety risks inherent in its patient population 4. Reduce the risk of healthcare associated infections 10. Universal protocol 30

31
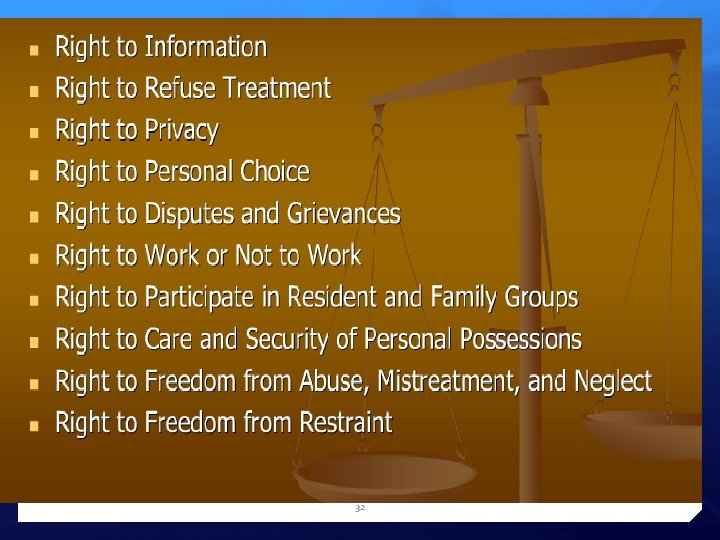
32
33
 Professional issues ethics and computer law
Professional issues ethics and computer law Legal aspects of nursing documentation
Legal aspects of nursing documentation Legal aspects of documentation
Legal aspects of documentation Nflpn code of ethics
Nflpn code of ethics Legal aspects of project management
Legal aspects of project management Legal aspects of doing business in canada
Legal aspects of doing business in canada Legal aspects of community health
Legal aspects of community health Legal aspects of special education
Legal aspects of special education Legal aspects definition
Legal aspects definition Legal aspects of catering premises
Legal aspects of catering premises Legal aspects of advertising
Legal aspects of advertising Mario full screen
Mario full screen Psychological aspects of nursing
Psychological aspects of nursing Dimensions of nursing practice
Dimensions of nursing practice Legal implications in nursing practice
Legal implications in nursing practice Legal implications of nursing documentation
Legal implications of nursing documentation Legal issues in nursing practice
Legal issues in nursing practice Legal implications in nursing practice
Legal implications in nursing practice Ethical and legal issues affecting the nursing assistant
Ethical and legal issues affecting the nursing assistant Beneficence
Beneficence Legal issues in psychiatric nursing
Legal issues in psychiatric nursing Contemporary professional nursing
Contemporary professional nursing Professional nursing practice concepts and perspectives
Professional nursing practice concepts and perspectives 5 levels of prevention leavell and clark
5 levels of prevention leavell and clark Accountability examples
Accountability examples Socialization into professional nursing ati
Socialization into professional nursing ati Professional curiosity in nursing
Professional curiosity in nursing Professional advancement in nursing
Professional advancement in nursing Model of professional nursing practice regulation
Model of professional nursing practice regulation Definition of nursing
Definition of nursing Nurses touch socialization into professional nursing
Nurses touch socialization into professional nursing Languagr
Languagr Msc.252(83)
Msc.252(83) Prof msc
Prof msc