Left Ventricular Failure Pathophysiology Results in increased back
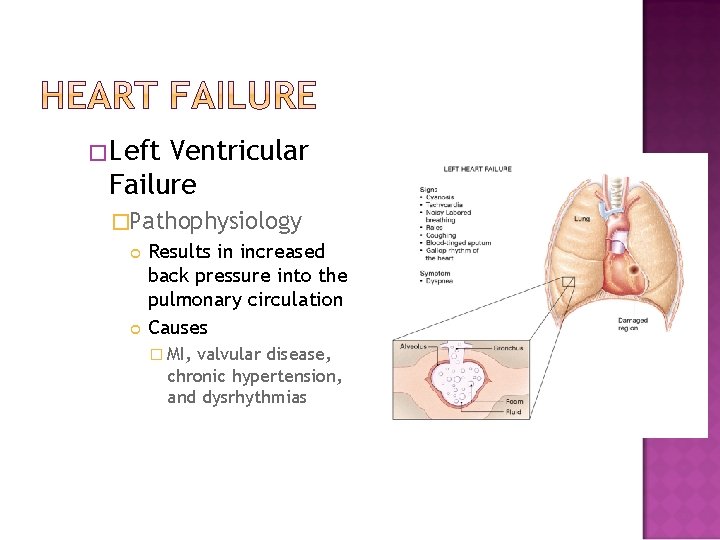
�Left Ventricular Failure �Pathophysiology Results in increased back pressure into the pulmonary circulation Causes � MI, valvular disease, chronic hypertension, and dysrhythmias

Right Ventricular Failure Pathophysiology Results in increased back pressure into the systemic venous circulation Causes Left ventricular failure Pulmonary Embolism

�Congestive Heart Failure �Pathophysiology Reduction in the heart’s stroke volume causes fluid overload throughout the body’s other tissues � Starling’s law no longer able to compensate �Manifestation In the acute setting, pulmonary edema, pulmonary hypertension, or myocardial infarction In the chronic setting as cardiomegally, left ventricular failure, or right ventricular failure

�Field Assessment �Check ABC’s and manage life threats �Chief Complaint OPQRST � Paroxysmal Nocturnal Dyspnea (PND) �Medications: Diuretics Medications to increase cardiac contractile force � Lanoxin Home oxygen

�Mental Status �Mental status changes indicate impending respiratory failure �Breathing �Signs of labored breathing �Tripod positioning �“Number of pillows” �Skin �Color changes �Peripheral and/or sacral edema

�Complications �Pulmonary edema may lead to respiratory failure �Pulsus paradoxus Systolic blood pressure drops more than 10 mm. Hg with inspiration �Pulsus alternans Pulse alternates between weak and strong

�Management �General management: Avoid supine positioning Avoid exertion such as standing or walking �Maintain the airway Administer oxygen �Administer �CPAP Nitroglycerine as soon as possible

�Monitor ECG �Establish IV access Limit fluid administration �Consider medication administration: �Nitrates �Angiotensin-converting Catopril Enalopril �Albuterol �Vasopressor Dopamine �Avoid enzyme (ACE) inhibitor patient refusals if at all possible

Continuous Positive Airway Pressure (CPAP) Can often prevent the need for endotracheal intubation and mechanical ventilation © Scott Metcalfe

�Continuous (CPAP) Positive Airway Pressure �Maintains a constant pressure within the airway throughout the respiratory cycle CPAP will force excess fluid out of the alveoli PEEP is applied only during expiration �Use the lowest effective pressure when applying CPAP A pressure of 2. 5– 5 cm/H 2 O is adequate

Asthma, COPD, pulmonary edema, CHF, or pneumonia Awake and able to follow commands >12 years old and able to fit the CPAP mask Able to maintain an open airway Exhibits two or more of the following A respiratory rate greater than 25 breaths per minute Sp. O 2 of less than 94% at any time Use of accessory muscles during respirations

�Any patient who is in respiratory arrest or apnea �Pneumothorax or has suffered trauma to the chest �Tracheotomy �Patient who is actively vomiting or has upper GI bleeding

�Epidemiology and Pathophysiology �Pathophysiology Result of fluid accumulation between visceral pericardium and parietal pericardium Increased intrapericardial pressure impairs diastolic filling Typically worsens progressively until corrected �Epidemiology Acute onset typically the result of trauma or MI Benign presentations may be caused by cancer, pericarditis, renal disease, and hypothyroidism

�Field Assessment �Patient History Determine precipitating causes Patient relates a history of dyspnea and orthopnea �Exam Rapid, weak pulse Decreasing systolic pressure Narrowing pulse pressures Pulsus paradoxus Faint, muffled heart sounds Electrical alternans � Less than normal voltage in waveforms

�Management �Maintain airway �Administer oxygen �Establish IV access �Consider medication administration: Morphine sulfate Nitrous oxide Furosemide Dopamine/dobutamine

�Rapid Transport �Pericardiocentesis is the definitive treatment Insertion of a cardiac needle and aspiration of fluid from the pericardium �Procedure should be performed only if allowed by local protocol �Procedure should be performed only by personnel adequately trained in the procedure

�Hypertensive Emergency �Causes Typically occurs only in patients with a history of hypertension Primary cause is noncompliance with prescribed antihypertensive medications Also occurs with toxemia of pregnancy �Incidence Risk Factors � Age-related factors � Race-related factors

�Field Assessment �Initial Assessment Alterations in mental state �Signs and Symptoms Headache accompanied by nausea and/or vomiting Blurred vision Shortness of breath Epistaxis Vertigo Tinnitus

�History �Known history of hypertension �Compliance with medications �Exam �BP >160/90 �Signs of left ventricular failure �Strong, bounding pulse �Abnormal skin color, temperature, and condition �Presence of edema

�Management �Maintain airway �Administer oxygen �Establish IV access �Consider medication administration: Nitroglycerin Sodium nitroprusside (Nipride) Labetalol (Trandate, Normodyne)

�Pathophysiology �General Inability of the heart to meet the body’s metabolic needs Often remains after correction of other problems Severe form of pump failure High mortality rate �Causes Tension pneumothorax and cardiac tamponade Impaired ventricular emptying Impaired myocardial contractility Trauma

�Field Assessment �Initial Assessment �Chief Complaint Chief complaint is typically chest pain, shortness of breath, unconsciousness, or altered mental state Onset may be acute or progressive �History of recent MI or chest pain episode Presence of shock in the absence of trauma

�Mental Status �Restlessness �Airway progressing to confusion and Breathing �Dyspnea, labored breathing, and cough �PND, tripod position, accessory muscle retraction, and adventitious lung sounds �ECG �Tachycardia and atrial dysrhythmias �Circulation �Hypotension �Cool, clammy skin

�Management �Maintain CPAP airway �Administer oxygen �Identify and treat underlying problem �Establish IV access Consider aggressive fluid therapy �Consider medication administration: Dopamine, dobutamine, norepinephrine

Click here to view the Cardiogenic Shock diagram.

�The absence of ventricular contraction �Immediately results in systemic circulatory failure �Sudden death is any death that occurs within 1 hour of symptom onset �Severe atherosclerotic disease is common �Risk factors

Acid-base imbalance Drowning Drug intoxication Electrocution Electrolyte imbalance End-stage renal disease Hyperkalemia (high levels of potassium) Hypothermia Hypoxia Pulmonary embolism Stroke Trauma

�Patients who suffer a cardiac arrest resulting from ventricular fibrillation go through several phases leading up to biological death �Electrical �Circulatory �Metabolic �Prehospital intervention required depends on the phase the patient is in


�Electrical Phase �Begins at the time of the cardiac arrest and ends at approximately 3 to 4 minutes postarrest �Adequate oxygen at the level of the myocardial cells Cells are able to maintain energy production through aerobic metabolism �The only beneficial treatment is immediate defibrillation

�Circulatory Phase � 4– 10 minutes post-arrest �Oxygen levels in the myocardial cells are inadequate Shift to anaerobic metabolism �Survival from cardiac arrest during this phase is better if at least 90 seconds of CPR is provided before the application of defibrillation Epinephrine beneficial

�Metabolic Phase �Begins approximately 10 minutes after the onset of cardiac arrest �Failure of the sodium-potassium pump Sodium begins to diffuse into the cell Water follows sodium Cellular swelling and eventually lysis �Current resuscitative measures do not improve survival during the metabolic phase

�Field Assessment �Initial Assessment Unresponsive, apneic, pulseless patient �ECG Dysrhythmias �History Prearrest events Bystander CPR “Down time”

�Management �Terms Resuscitation Return of Spontaneous Circulation Survival �Role of Basic Life Support �General Guidelines Manage specific dysrhythmias CPR Advanced airway management Establish IV access

�Pharmacological considerations �Amiodarone �Atropine sulfate �Epinephrine �Lidocaine �Magnesium sulfate �Vasopressin �Follow medications in arrest with a bolus of fluid

Click here to view the Cardiac Arrest diagram. Reproduced with permission from “ 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Care, ” Circulation 2005, Volume 112, IV-59. © 2005 American Heart Association.

�Manage dysrhythmias and problems as presented. �Be alert for PEA �Transport rapidly: Take care to protect intubation and IV access �Withholding �Rigor resuscitation mortis �Dependent lividity �Decapitation, decomposition, incineration �Valid advance directive

�Terminating Resuscitation �Inclusion criteria for termination of resuscitation: Patient over 18 years old Cause is presumed cardiac in origin Successful endotracheal intubation ACLS standards applied throughout the arrest On-scene effort >25 minutes, or four rounds of drug therapy ECG remains asystolic or agonal

�Terminating Resuscitation �Exclusion Criteria: Patient under 18 years old Arrest is of a treatable cause Present or recurring VF/VT Transient return of a pulse Signs of neurological viability Witnessed arrest Family or others opposed to termination of resuscitation �Always follow local protocols related to termination of resuscitation

�Atherosclerosis �Pathophysiology Progressive degenerative disease of the medium-sized and large arteries Results from the buildup of fats on the interior of the artery Fatty buildup results in plaques and eventual stenosis of the artery �Arteriosclerosis �Claudication

�Aneurysm �Pathophysiology Ballooning of an arterial wall, usually the aorta, that results from a weakness or defect in the wall �Types Atherosclerotic Dissecting Infectious Congenital Traumatic

�Abdominal Aortic Aneurysm �Often the result of atherosclerosis �Signs and symptoms: Abdominal pain Back/flank pain Hypotension Urge to defecate

�Dissecting �Caused Aortic Aneurysm by degenerative changes in the smooth muscle and elastic tissue �Blood gets between and separates the wall of the aorta �Can extend throughout the aorta and into associated vessels

�Acute Pulmonary Embolism �Pathophysiology Blockage of a pulmonary artery by a blood clot or other particle The area served by the pulmonary artery fails �Signs and Symptoms Dependent upon size and location of the blockage Onset of severe, unexplained dyspnea History of recent lengthy immobilization

�Acute Arterial Occlusion �Pathophysiology Sudden occlusion of arterial blood flow due to trauma, thrombosis, tumor, embolus, or idiopathic means Frequently involves the abdomen or extremities �Vasculitis �Pathophysiology Inflammation of the blood vessels Commonly stems from rheumatic diseases and syndromes

�Noncritical Peripheral Vascular Conditions �Peripheral Arterial Atherosclerotic Disease Can be acute or chronic Often associated with diabetes Extremities exhibit pain, coldness, numbness, and pallor �Deep Venous Thrombosis Blood clot in a vein Typically occurs in the larger veins of the thigh and calf Swelling, pain, and tenderness, with warm, red skin �Varicose Veins Dilated superficial veins, common with pregnancy and obesity

�General Assessment and Management of Vascular Disorders �Assessment Initial Assessment Circulatory Assessment � Pallor � Pain � Pulselessness � Paralysis � Paresthesia

�Assessment (cont. ) �Chief Complaint OPQRST �Physical Exam Prior history of vascular problems Differences in pulses or blood pressures �Management �Maintain the airway �Administer oxygen if respiratory distress or signs of hypoperfusion present �Consider administration of analgesics �Transport rapidly if signs of hypoperfusion present

�Assessment of the Cardiovascular Patient �Management of Cardiovascular Emergencies �Managing Specific Cardiovascular Emergencies
- Slides: 49