Left Atrial Appendage Thrombus in TAVI Prevalence clinical
Left Atrial Appendage Thrombus in TAVI Prevalence, clinical impact and the role of cardiac computed tomography
Potential conflicts of interest Speaker's name: Paul Williams Educational grant from Edwards Lifesciences Conference support from St Jude Medical
Stroke and TAVI • Stroke is one of most feared complications of TAVI • Incidence of stroke in the PARTNER and Core. Valve trials ~ 5% at 30 days • Multiple mechanisms of periprocedural stroke: o dislodgement of aortic atheromatous debris during wire and device manipulation o embolization of calcific debris from native valve during TAVI deployment o cerebral hypoperfusion from hypotension (rapid ventricular pacing, procedural complications) o thrombus formation o ? left atrial appendage thrombus embolisation (wire, rapid pacing)

Left atrial appendage thrombus

Left atrial appendage cast
Left atrial appendage thrombus • Left atrial appendage thrombus (LAAT) formation and embolisation is the main mechanism for the increased stroke risk in AF patients • TOE is recommended in AF patients scheduled for cardioversion, AF ablation or LA appendage closure All of these procedures are contraindicated in presence of LAAT • AF is very common in patients referred for TAVI o Core. Valve US Pivotal Trial 40% o PARTNER 1 A 32% o PARTNER 2 33% • Patients with LAAT were excluded from the PARTNER trial • Little data on LAAT & TAVI o What is the burden of thrombus in this cohort? o What tis the best diagnostic modality? o Does presence of LAAT affect outcomes?
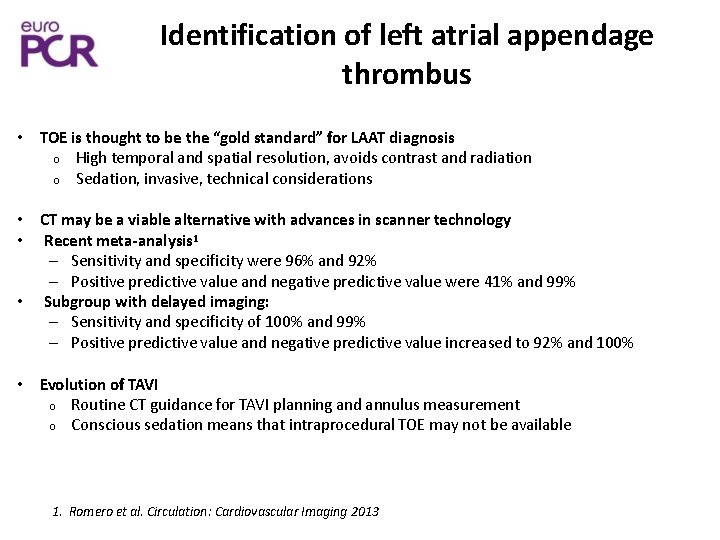
Identification of left atrial appendage thrombus • TOE is thought to be the “gold standard” for LAAT diagnosis o High temporal and spatial resolution, avoids contrast and radiation o Sedation, invasive, technical considerations • CT may be a viable alternative with advances in scanner technology • Recent meta-analysis 1 – Sensitivity and specificity were 96% and 92% – Positive predictive value and negative predictive value were 41% and 99% • Subgroup with delayed imaging: – Sensitivity and specificity of 100% and 99% – Positive predictive value and negative predictive value increased to 92% and 100% • Evolution of TAVI o Routine CT guidance for TAVI planning and annulus measurement o Conscious sedation means that intraprocedural TOE may not be available 1. Romero et al. Circulation: Cardiovascular Imaging 2013
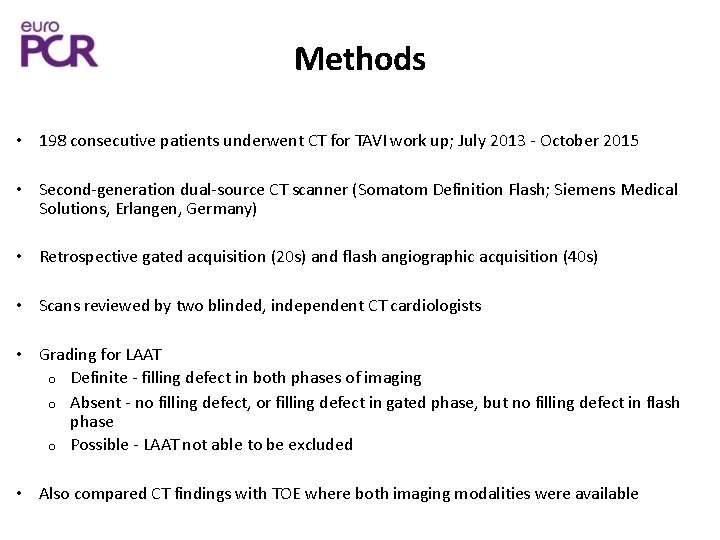
Methods • 198 consecutive patients underwent CT for TAVI work up; July 2013 - October 2015 • Second-generation dual-source CT scanner (Somatom Definition Flash; Siemens Medical Solutions, Erlangen, Germany) • Retrospective gated acquisition (20 s) and flash angiographic acquisition (40 s) • Scans reviewed by two blinded, independent CT cardiologists • Grading for LAAT o Definite - filling defect in both phases of imaging o Absent - no filling defect, or filling defect in gated phase, but no filling defect in flash phase o Possible - LAAT not able to be excluded • Also compared CT findings with TOE where both imaging modalities were available
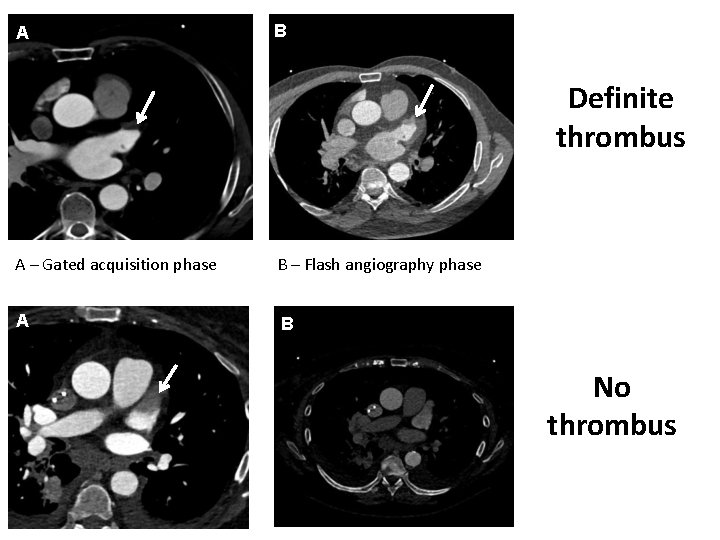
A B Definite thrombus A – Gated acquisition phase B – Flash angiography phase A B No thrombus
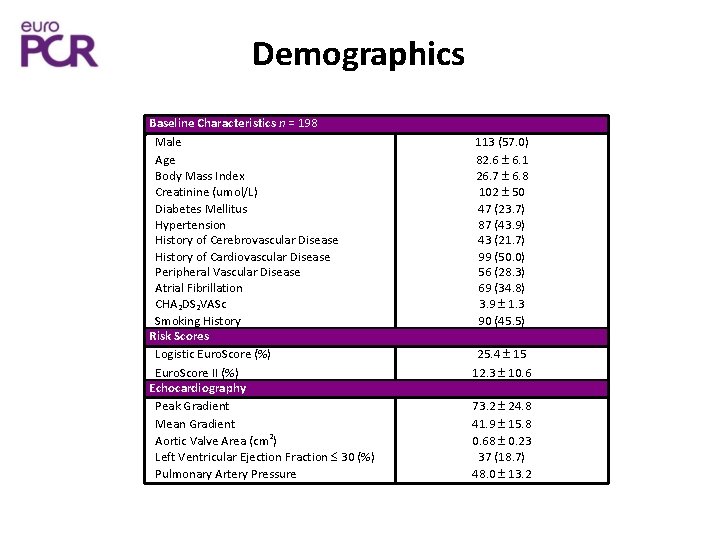
Demographics Baseline Characteristics n = 198 Male Age Body Mass Index Creatinine (umol/L) Diabetes Mellitus Hypertension History of Cerebrovascular Disease History of Cardiovascular Disease Peripheral Vascular Disease Atrial Fibrillation CHA 2 DS 2 VASc Smoking History Risk Scores Logistic Euro. Score (%) Euro. Score II (%) Echocardiography Peak Gradient Mean Gradient Aortic Valve Area (cm 2) Left Ventricular Ejection Fraction 30 (%) Pulmonary Artery Pressure 113 (57. 0) 82. 6 6. 1 26. 7 6. 8 102 50 47 (23. 7) 87 (43. 9) 43 (21. 7) 99 (50. 0) 56 (28. 3) 69 (34. 8) 3. 9 1. 3 90 (45. 5) 25. 4 15 12. 3 10. 6 73. 2 24. 8 41. 9 15. 8 0. 68 0. 23 37 (18. 7) 48. 0 13. 2
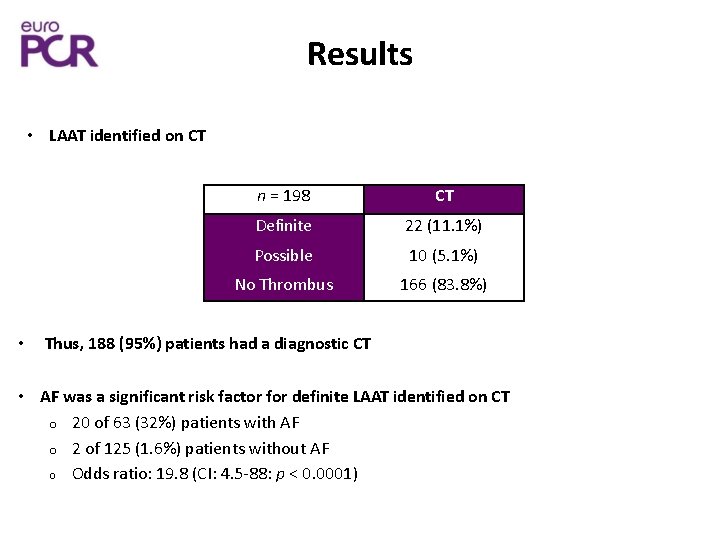
Results • LAAT identified on CT • n = 198 CT Definite 22 (11. 1%) Possible 10 (5. 1%) No Thrombus 166 (83. 8%) Thus, 188 (95%) patients had a diagnostic CT • AF was a significant risk factor for definite LAAT identified on CT o 20 of 63 (32%) patients with AF o 2 of 125 (1. 6%) patients without AF o Odds ratio: 19. 8 (CI: 4. 5 -88: p < 0. 0001)
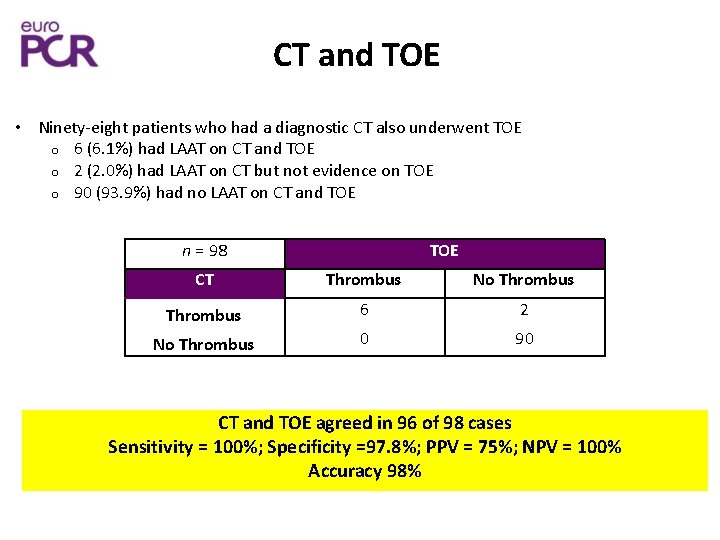
CT and TOE • Ninety-eight patients who had a diagnostic CT also underwent TOE o 6 (6. 1%) had LAAT on CT and TOE o 2 (2. 0%) had LAAT on CT but not evidence on TOE o 90 (93. 9%) had no LAAT on CT and TOE n = 98 TOE CT Thrombus No Thrombus 6 2 No Thrombus 0 90 CT and TOE agreed in 96 of 98 cases Sensitivity = 100%; Specificity =97. 8%; PPV = 75%; NPV = 100% Accuracy 98%
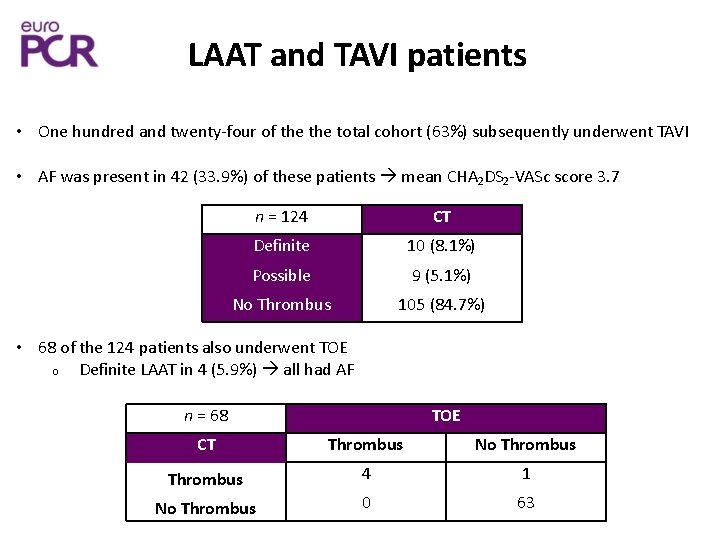
LAAT and TAVI patients • One hundred and twenty-four of the total cohort (63%) subsequently underwent TAVI • AF was present in 42 (33. 9%) of these patients mean CHA 2 DS 2 -VASc score 3. 7 n = 124 CT Definite 10 (8. 1%) Possible 9 (5. 1%) No Thrombus 105 (84. 7%) • 68 of the 124 patients also underwent TOE o Definite LAAT in 4 (5. 9%) all had AF n = 68 TOE CT Thrombus No Thrombus 4 1 No Thrombus 0 63
Clinical outcomes in TAVI patients • Six of 124 (4. 8%) patients had a CVA during admission – Two patients had LAAT on CT – Both patients with CVA and LAAT on CT had AF and were anticoagulated (warfarin) – The remaining four patients with CVA did not have AF, were not anticoagulated and had a negative CT for LAAT – Stroke risk with vs without LAAT: 20% vs 3. 8% • Overall, within the TAVI cohort 8 of 10 (80%) patients with LAAT on CT did not have a clinically evident periprocedural stroke
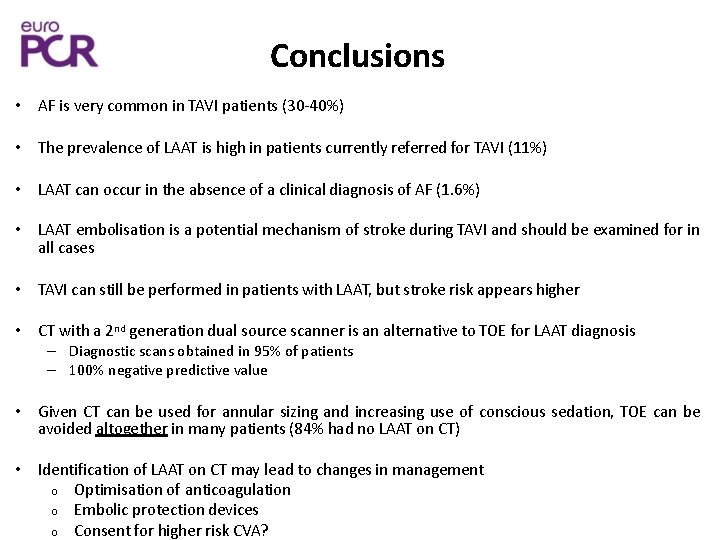
Conclusions • AF is very common in TAVI patients (30 -40%) • The prevalence of LAAT is high in patients currently referred for TAVI (11%) • LAAT can occur in the absence of a clinical diagnosis of AF (1. 6%) • LAAT embolisation is a potential mechanism of stroke during TAVI and should be examined for in all cases • TAVI can still be performed in patients with LAAT, but stroke risk appears higher • CT with a 2 nd generation dual source scanner is an alternative to TOE for LAAT diagnosis – Diagnostic scans obtained in 95% of patients – 100% negative predictive value • Given CT can be used for annular sizing and increasing use of conscious sedation, TOE can be avoided altogether in many patients (84% had no LAAT on CT) • Identification of LAAT on CT may lead to changes in management o Optimisation of anticoagulation o Embolic protection devices o Consent for higher risk CVA?
- Slides: 15