Lecture Title General objectives of the emergency room
Lecture Title: General objectives of the emergency room management Lecturer name: Dr. Hossam Hassan Lecture Date:
Lecture Objectives. . Students at the end of the lecture will be able to: 1. Recognize and be aware of the basic management of common BLS and ACLS protocols. 2. Gain experience in the evaluation and management of patients presenting to the ER for acute care. 3. Developing proficiency with emergency procedures 4. Expanding the knowledge in acute care medicine to include , Acute Chest pain, Trauma , and shock management. .
Objectives • • Acute medical illnesses Acute surgical illnesses Acute Obstetrical emergencies Trauma Acute mental illnesses Acute ENT & Ophthalmological emergencies Environmental hazards

Top Ten Leading Causes of Death • • • Heart Disease: 726, 974 Cancer: 539, 577 Stroke: 159, 791 Chronic Obstructive Pulmonary Disease: 109, 029 Accidents: 95, 644 Pneumonia/Influenza: 86, 449 Diabetes: 62, 636 Suicide: 30, 535 Nephritis, Nephrotic Syndrome, and Nephrosis 25, 331 Chronic Liver Disease and Cirrhosis: 25, 175
Reception • 300 – 500 visits per day • Only 20 -50 cases require urgent intervention • Few cases are life-threatening (1 -5)
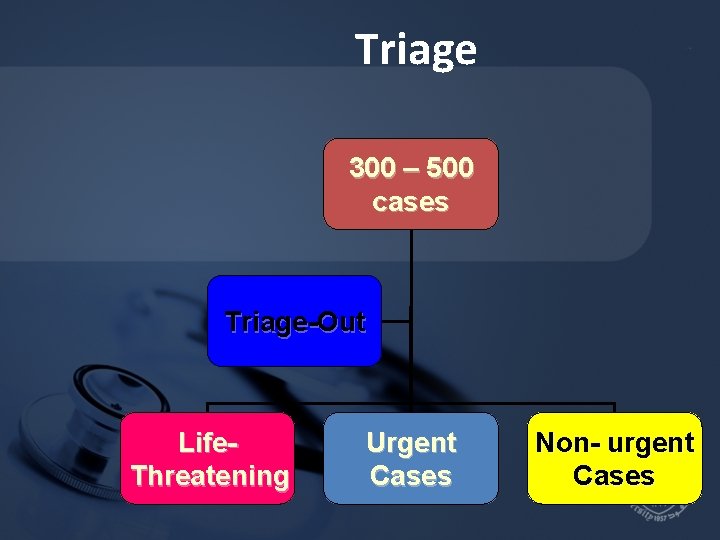
Triage 300 – 500 cases Triage-Out Life. Threatening Urgent Cases Non- urgent Cases
Triage ( Categorization) • Category 1 – 5 • 1 : Life-Threatening • 5 : Triage out
Triage • Physician Triage • Nurse Triage • Clark Triage
Life-Threatening Cases ( C. 1) Need immediate intervention • Arrest • Arrhythmias • Hypoxia • Shock • Acute trauma • Siezure • Status Asthmaticus • Anaphylaxis • Chest pain ( STEMI ) • Delivery – stage 2
C. 2 ( Urgent Cases) Should be treated within 10 min. • Acute asthmatic attack • High Blood Pressure • Intoxication • Drowsy patient • Acute colics • Fractures • Burns
C. 3 ( Acute Cases ) Should be treated within 30 minutes • Chest Pain ( Non cardiac ) • Abdominal pain • Dyspnea • Fever • Old trauma • Gastroeneteritis • Metabolic Derangement • Post ictal state
Cont’d Triage • C 4 : Chronic Abdo pain Minor trauma claimed : Fever-Low BP- Fast HR • C 5 : URTI Long-standing complaints Meds-Refill
Appeal of Emergency Medicine • • • 13 Make an immediate difference Life threatening injuries and illnesses Undifferentiated patient population Challenge of “anything” coming in Emergency / invasive procedures Safety net of healthcare
Appeal of Emergency Medicine • • • 14 Team approach Patient advocacy Open job market Academic opportunities Shift work / set hours Evolving specialty
Downside to Emergency Medicine • Interaction with difficult, intoxicated, or violent patients • Finding follow-up or care for uninsured • Working as a patient advocate • Contract management groups • Malpractice targets 15
The Lifestyle: Two Sides of A Coin • Well defined shifts • Usually not on call • Part time employment possible • Evenings and nights • Weekends • Holidays 16

Subspecialties in Emergency Medicine • • • 17 Pediatric Emergency Medicine Toxicology Emergency Medical Services Sports Medicine Critical Care Medicine
Upcoming Areas of Emergency Medicine • Observation units • ED CT 18

Research Opportunities • Broad range of subjects • Limited amount of work published in our relatively new field • Limited number of research mentors • Limited number of clinical trials 19
What to do to get in to Emergency Medicine ? • Observe in ED • Summer research projects with EM staff • EM interest group affiliation • Be open to any medical specialty 20
Trauma
Primary Survey ( A-B-C-D)
Secondary Survey ( Systemic)
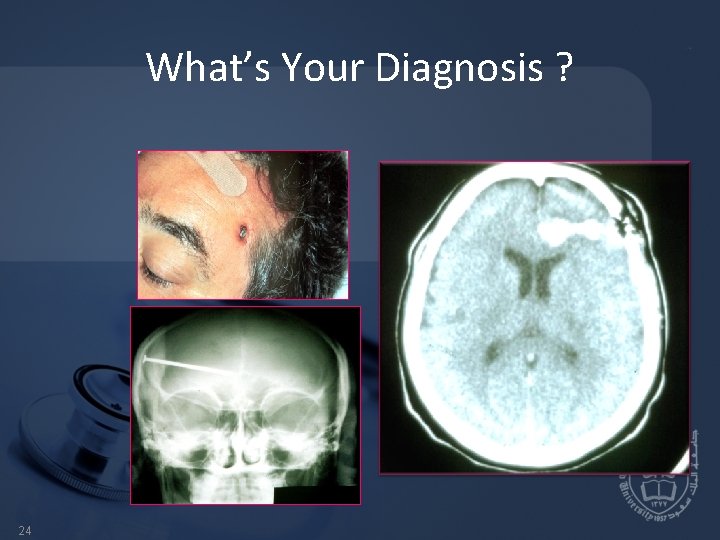
What’s Your Diagnosis ? 24
OR
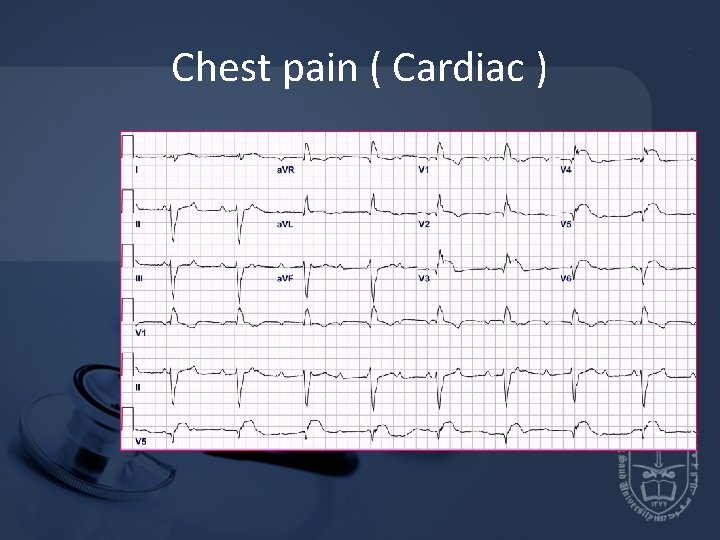
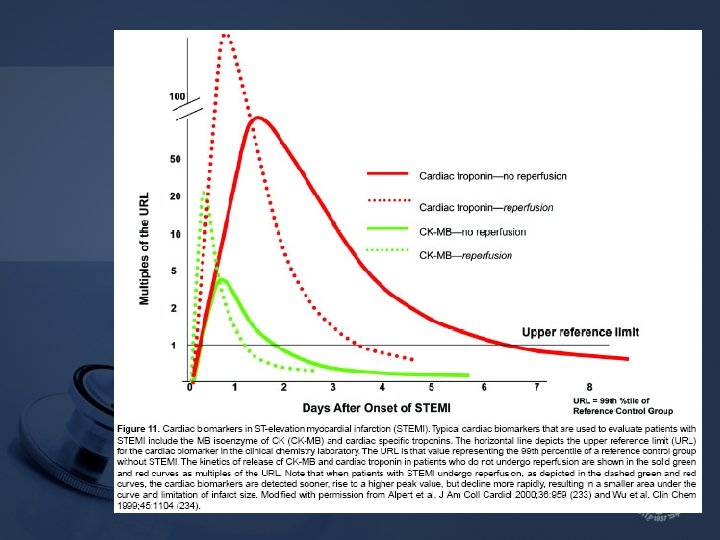
Chest pain ( Cardiac )
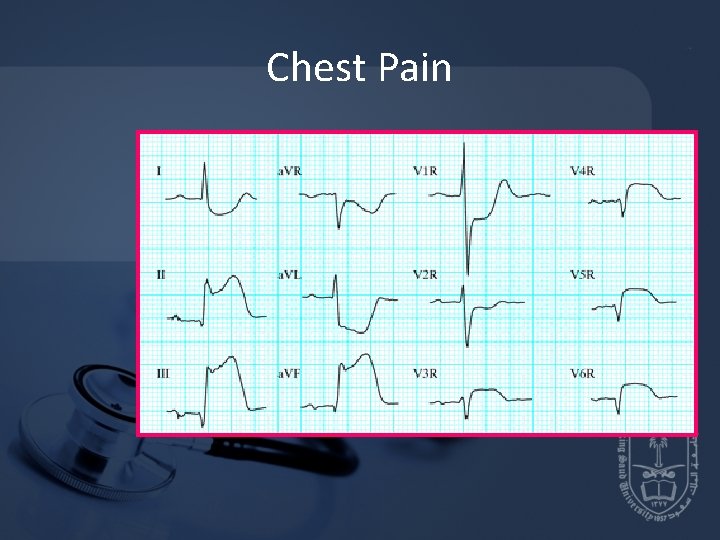
Chest Pain
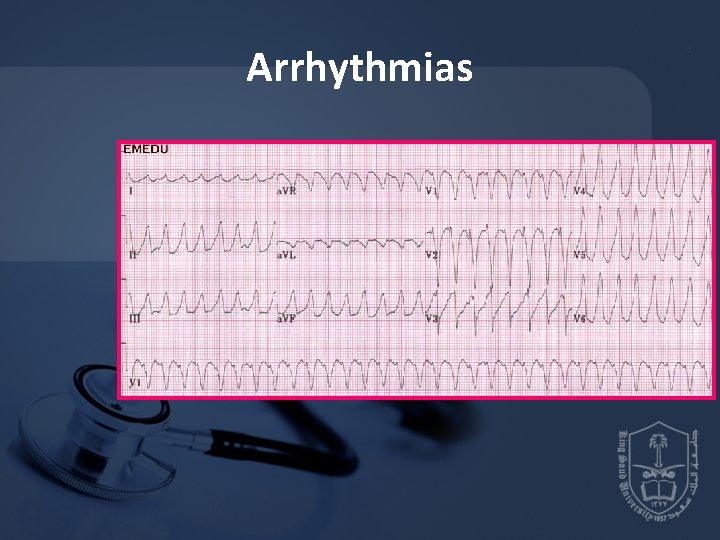
Arrhythmias
Low Blood Pressure • PB = COP * SVR ( 120 / 80 ) mm. Hg • COP = SV * HR ( 4 - 6 ) 4 -6 L/m • SV = EDV - ESV ( 50 – 100 ) ml
Low Blood Pressure • Preload • Contractility • Afterload
Dyspnea ( S. O. B) ABG : 7. 35 40 80 23 O 2 saturation: 99%
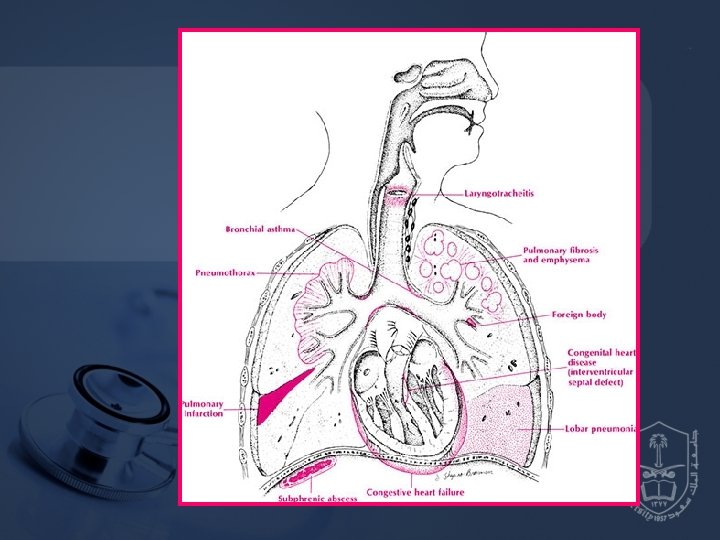
Acute Respiratory Failure • Hypoxemic • Hypercapnic
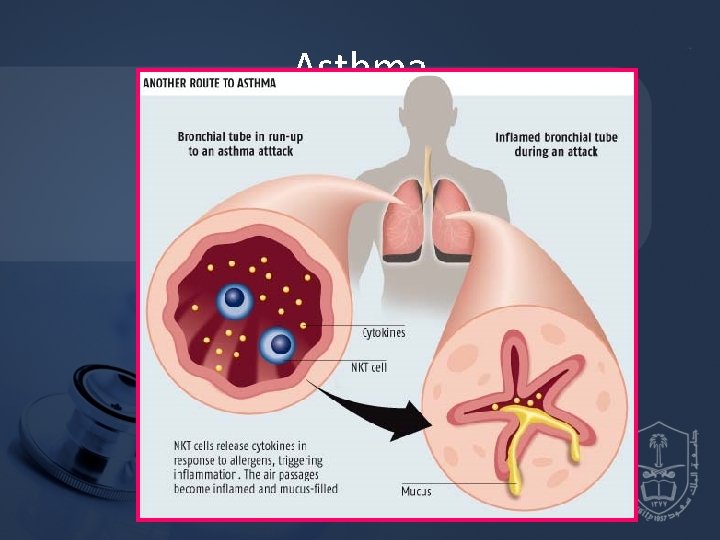
Asthma
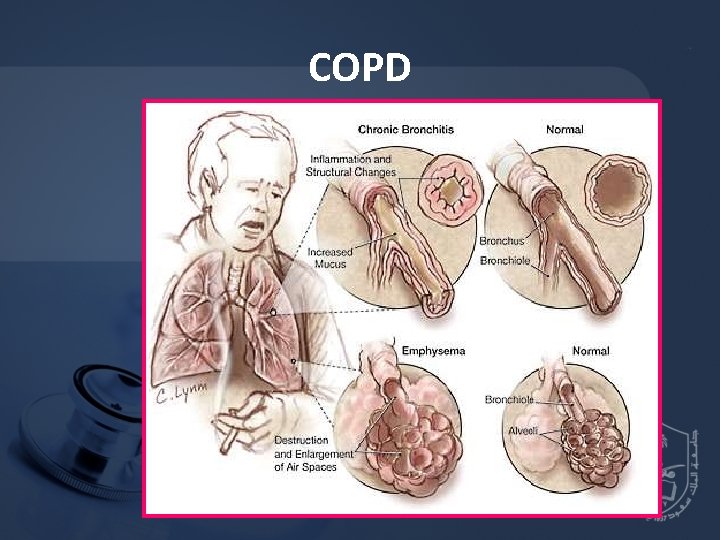
COPD
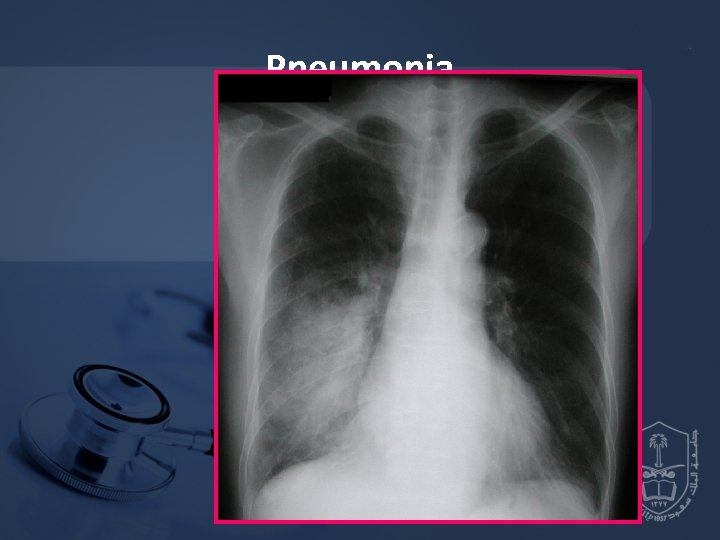
Pneumonia
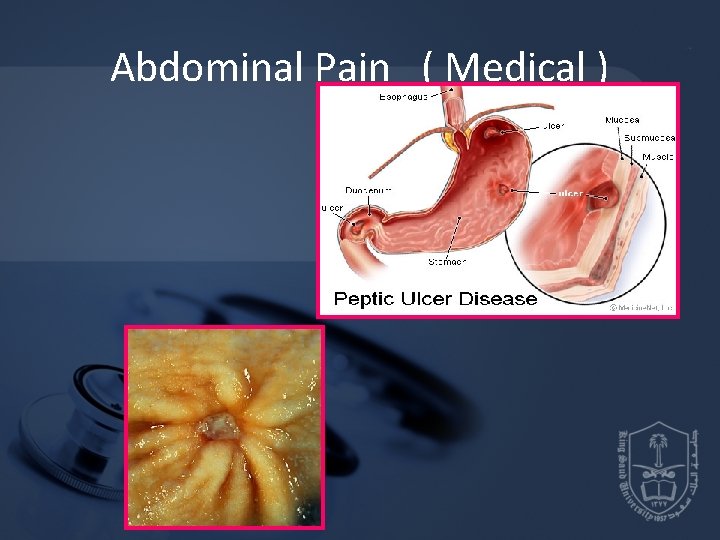
Abdominal Pain ( Medical )
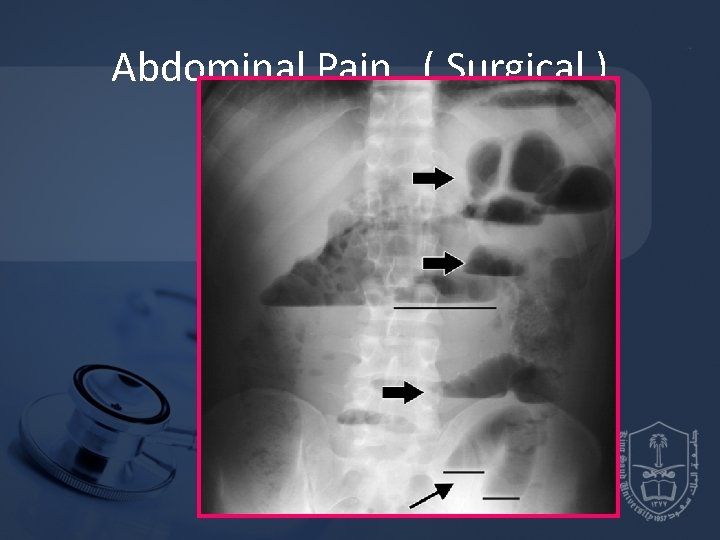
Abdominal Pain ( Surgical )
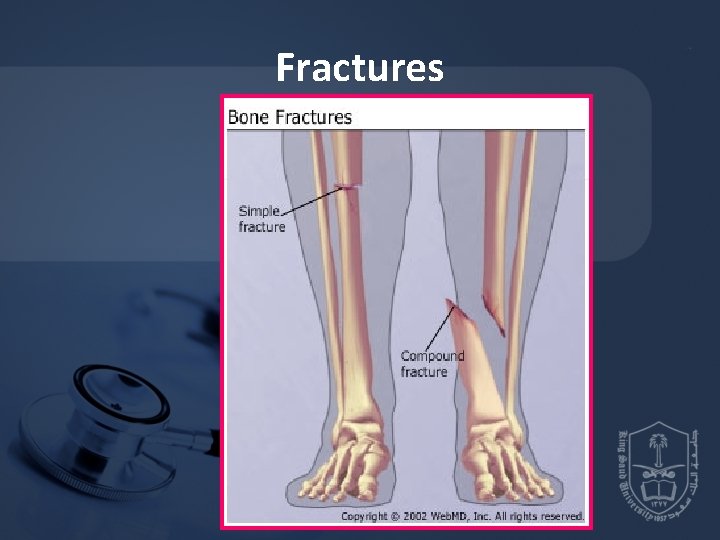
Fractures

Fractures
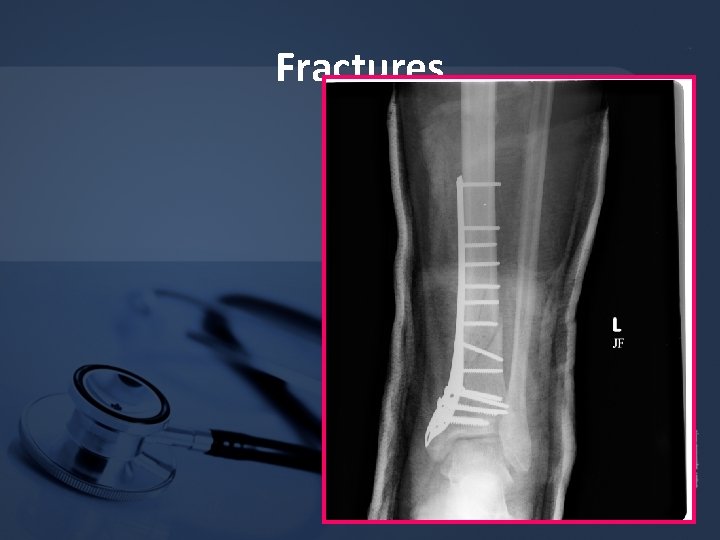
Fractures
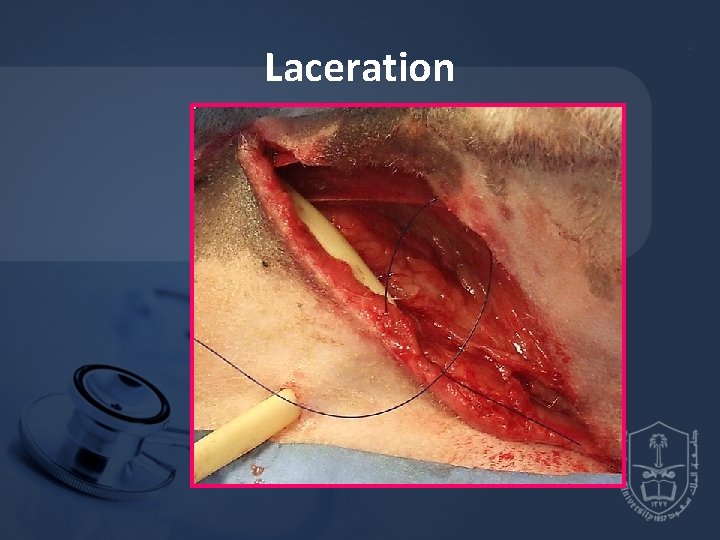
Laceration
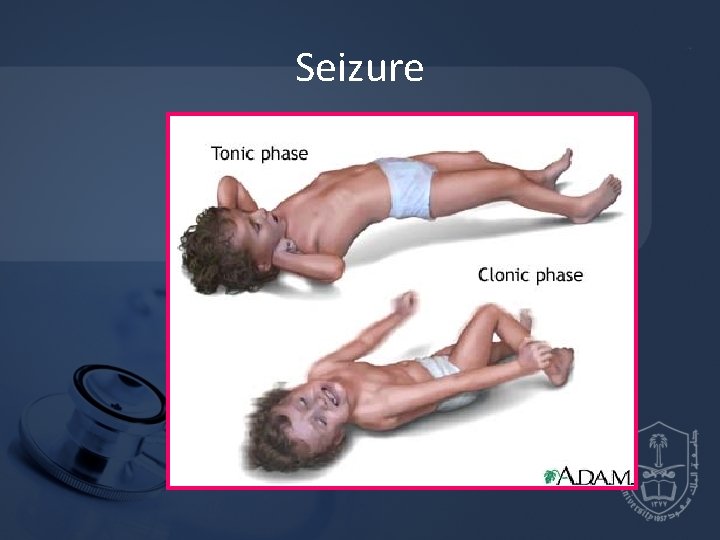
Seizure
Acute Psychiatric Ilnesses
DM
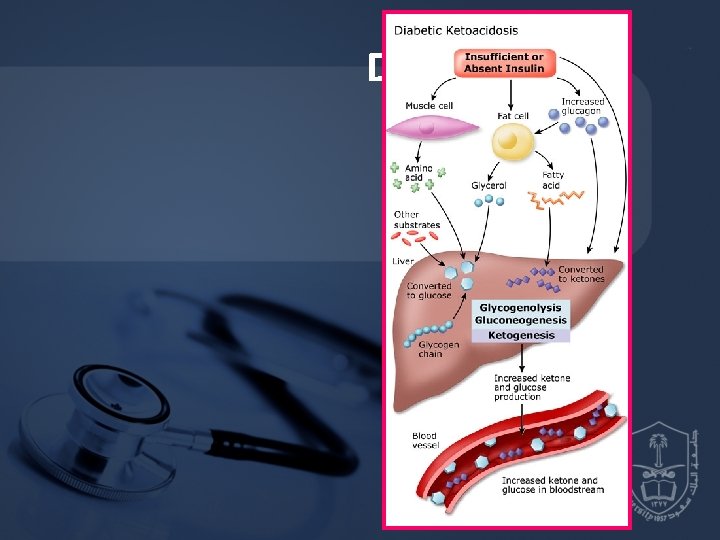
DKA

Skin Rash
• Where do you taiage this Pt. ? • What information do you need to determine if this Pt. is in shock? • What initial interventions are needed to stabilize that Pt. ?
• Shock is a syndrome of impaired tissue oxygenation and perfusion due to a variety of etiologies • If left untreated • Irreversible injury , Organ dysfunction And finally death
Clinical ulterations in shock • The presentation of patients with shock may be Subtle(mild confusion, tachycardia) • Or easily identifiable(profound hypotesion. anuria)
• The clinical manifestation of shock result from • 1 - inadequate tissue perfusion and oxygenation • 2 - Compansatory respnses • 3 - The specific etiology
Clasification of shock • 1 -hypovolemic • a-Hemorrhagic • b-nonhemorrhagic • 2 -Cardiogenic • Ischemic • Myopathy • Mechanical • Arrhythmia
• 3 - Distributive • Septic • Adrenal crises • Neurogenic (spinal shock) • Anaphylactic
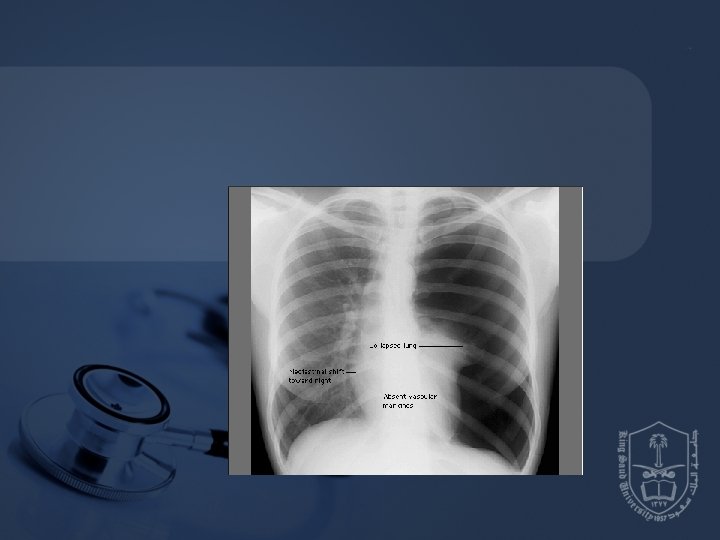
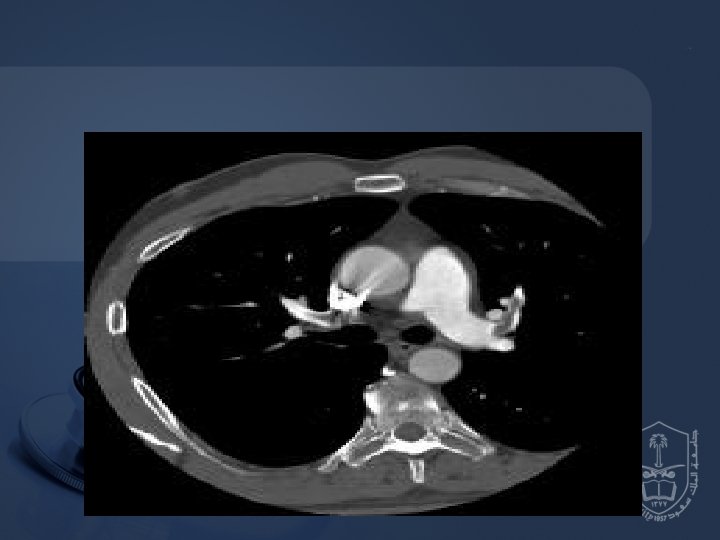
• 4 - Obstructive • Massive Pulmonary embolism • Tension pneumothorax • Cardiac tamponade • Constrictive pericarditis

HYPOVOLEMIC SHOCK • It occure when the intra vascular volume is depleted relative to the vascular capacity as a result of • 1 - Hge. • 2 - G. I. T loss • 3 -urinary loss • 4 -dehydration
HYPOVOLEMIC SHOCK • Management • The goal is to restore the fluid lost • Vasopressors are used only as a temporary method to restore B. P untill fluid resuscitation take place
Distributive shock • It is characterized by loss of vascular tone • The most common form of distributive shock is septic shock • The hemodynamic profile of septic shock include
• • • Cardiac output normal or increased Ventricular filing pressure normal or low SVR low Diastolic pressure low Pulse pressure wide
Management of septic shock • The initial approach to the patient with septic shock is the restoration and maintenance of adequate intravascular volume • Prompt institution of appropriate antibiotic
CARDIOGENIC SHOCK • Forward flow of blood is inadequate bec. Of pump failure due to loss of functional myocardium • It is the most severe form of heart failure and it is distinguished from chronic heart failure by the presence of hypotension, hypoperfusion and the need for different therapuetic inteventions
• • • Hemodynamic chracteristics Cardiac output low Ventricular filing pressure high SVR High Mixed venous o 2 sat low
MANAGEMENT OF CARDIOGENIC SHOCK • The main goal is to improve myocardial function • Arrhythmia should be treated • Reperfusion PCI is the treatment of choice in ACS • Inotropes and vasopresor
Obstructive shock • Obstruction to the outflow due to impaired cardiac filling and excessive after load • Cardiac tamponade and constrictive pericarditis impair diastolic filling of the Rt. ventricle • Tension pneumothorax limit Rt. ventricular filing by obstruction of venous return • Massive pulmonary embolism increase Rt. ventricular afterload
• • • Hemodynamic profile in obst. Shock Cardiac output low Afterload high Lt. Vent. filling pressure variable Pulsus paradoxicus in Tamponade Distended Jugular viens
Management Of Obstructive Shock Directed Mainly to Management of the cause
GENERAL Principles of shock management • The overall goal of shock management is to improve oxygen delivery or utilization in order to prevent cellular and organ injury • Effective therapy requires treatment of the underlying etiology
• Restoration of adequate perfusion, monitoring and comperhensive supportive care • Interventions to restore perfusion center on achieving an adequate B. P, increasing cardiac output and optimizing oxygen content of the blood
• Oxygen demand should also be reduced
In Summery • • • Management of shock 1 - Monitoring 2 - Fluid Therapy 3 - Vasoactive agents 4 - Treat the cause
Reference book and the relevant page numbers. .

Thank You Dr.
- Slides: 76