Lecture outlines Definition mechanism and clinical types of


- Slides: 42

Lecture outlines • Definition, mechanism and clinical types of hypersensitivity reactions. • Type I, II, IV hypersensitivity reactions; pathogenesis, clinical types, diagnosis and treatment)
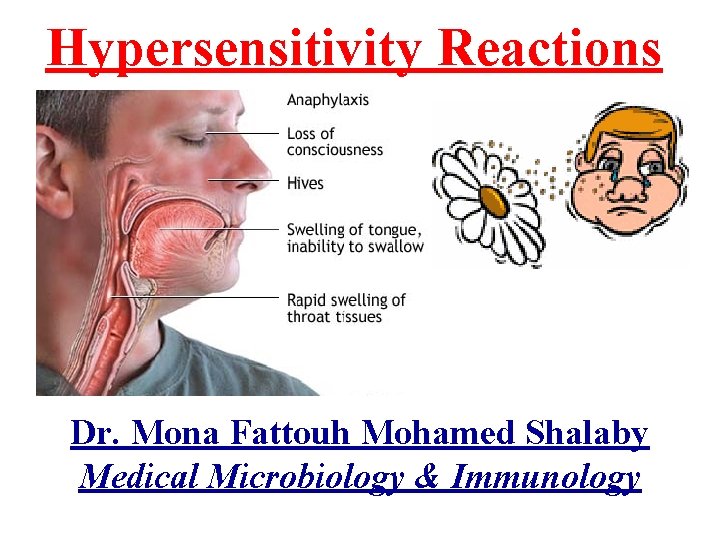
Hypersensitivity Reactions Dr. Mona Fattouh Mohamed Shalaby Medical Microbiology & Immunology
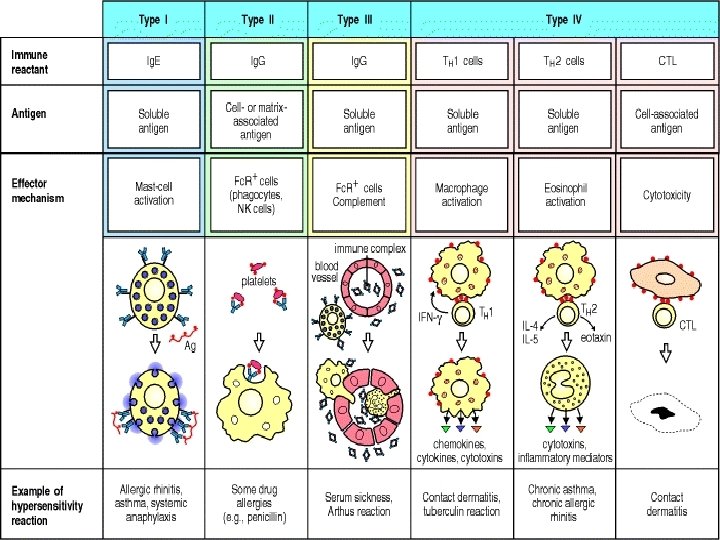
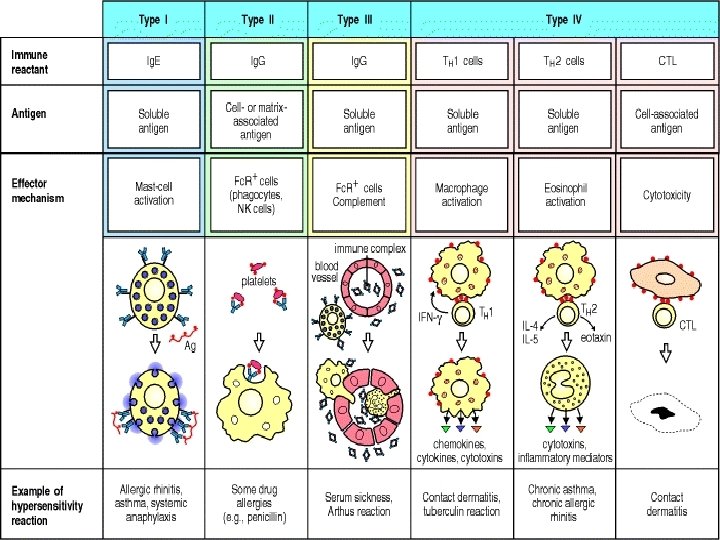
Immunologic Mechanisms of Tissue Damage • Immuopathology: Exaggerated immune response may lead to different forms of tissue damage: 1) An overactive immune response: produce damage e. g. hypersensitivity reactions and graft rejection 2) Failure of proper antigen recognition: e. g. autoimmune diseases
Hypersensitivity Reactions • Hypersensitivity or Allergy: • An immune response that results in exaggerated reactions harmful to the host. • (4) types of hypersensitivity reactions: • Type I, Type III, Type IV. • Types I, II and III are antibody mediated. • Type IV is cell mediated (No role for antibodies).
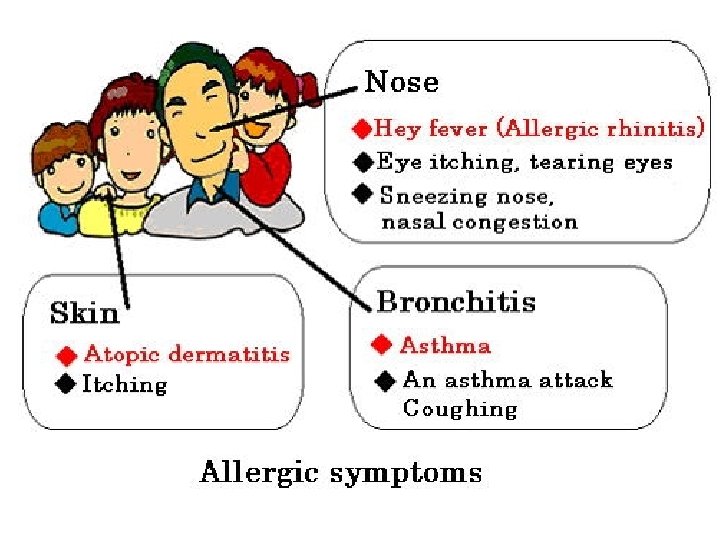
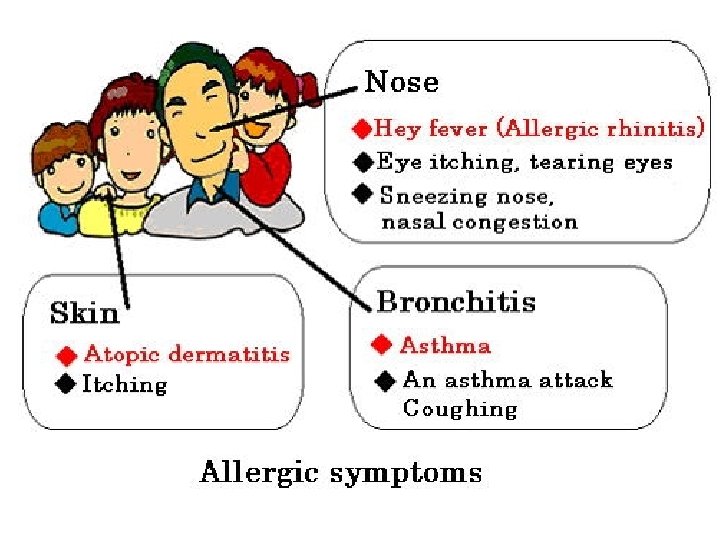
Type I: Immediate hypersensitivity • An antigen (allergen) reacts with (Ig E) (cell fixed antibody on surface of tissue mast cells & blood basophiles) leading to rapid release of soluble molecules (inflammatory mediators) • Released mediators cause the manifestations as: • 1) Systemic life threatening: anaphylactic shock.
• 2) Local atopic reactions: bronchial asthma, allergic rhinitis, allergic conjunctivitis, skin urticaria, drug & food allergies.
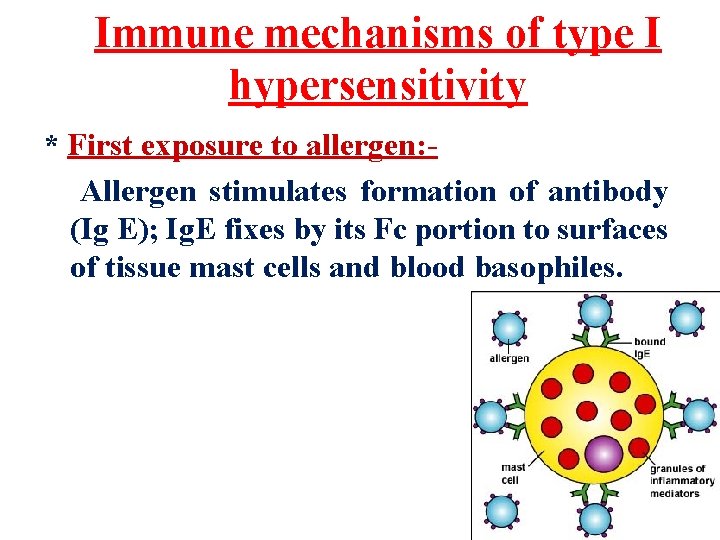
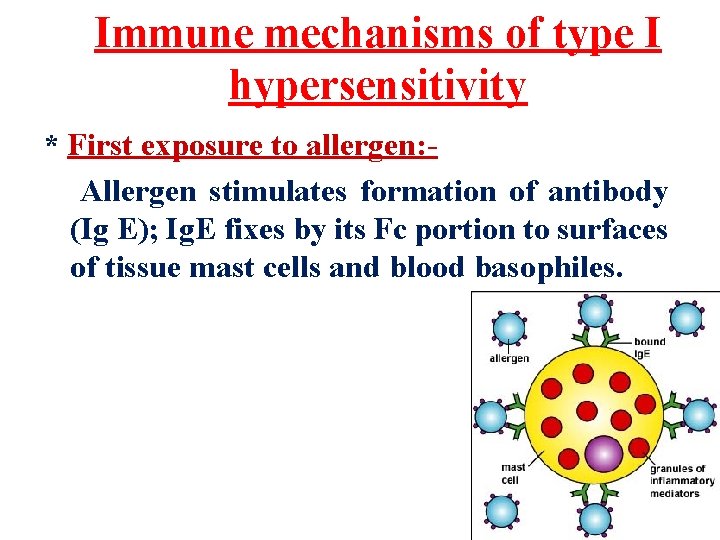
Immune mechanisms of type I hypersensitivity * First exposure to allergen: Allergen stimulates formation of antibody (Ig E); Ig. E fixes by its Fc portion to surfaces of tissue mast cells and blood basophiles.
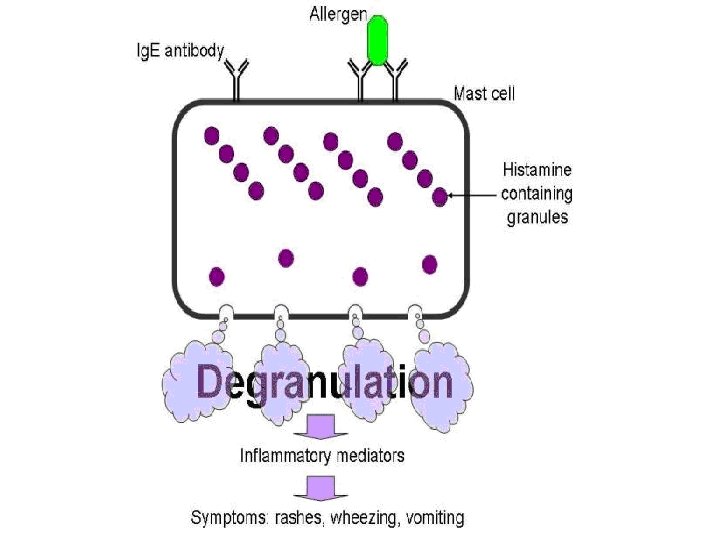
* Second exposure to the same allergen: • The allergen bridges between Ig E molecules fixed to surfaces of mast cells and basophiles. • This leads to activation and degranulation of mast cells and basophiles and release of inflammatory mediators.
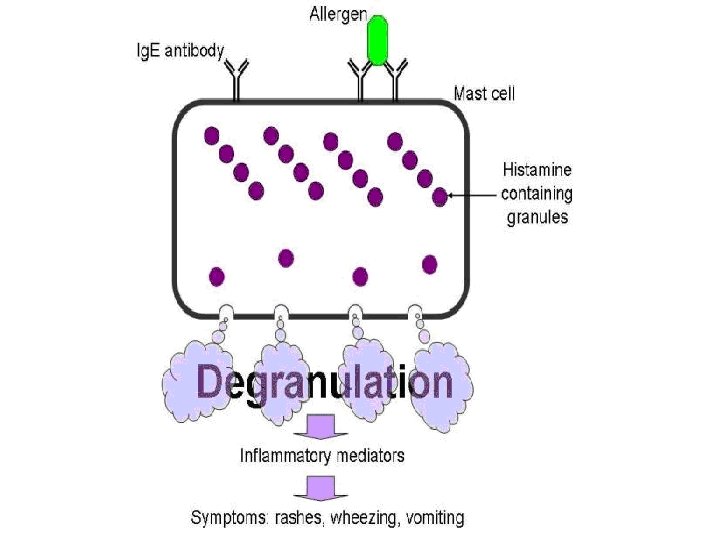
Pathogenic mechanisms • Three classes of mediators released from mast cells: • 1) Preformed mediators stored in granules (histamine). • 2) Newly sensitized mediators: leukotrienes, prostaglandins. • 3) Cytokines produced by activated mast cells, basophiles e. g. TNF, IL 3, IL-4, IL-5 IL -13.
• These mediators cause: smooth muscle contraction & mucous secretion and bronchial spasm, vasodilatation, vascular permeability , edema & low blood pressure.
1. Anaphylaxis *Systemic (generalized) form of Type I hypersensitivity due to exposure to allergen to which a person is sensitized. * Allergens: • Drugs: penicillin • Serum injection : anti-diphtheritic or antitetanic serum (Abs). • anesthetics or insect venom (Bees)
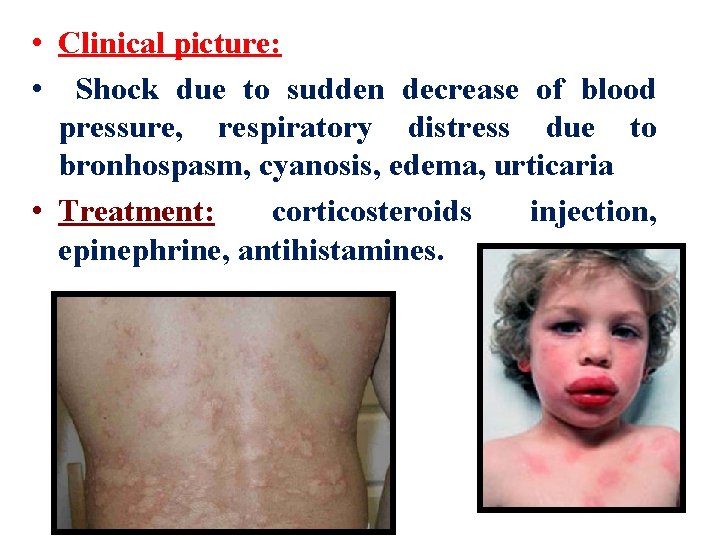
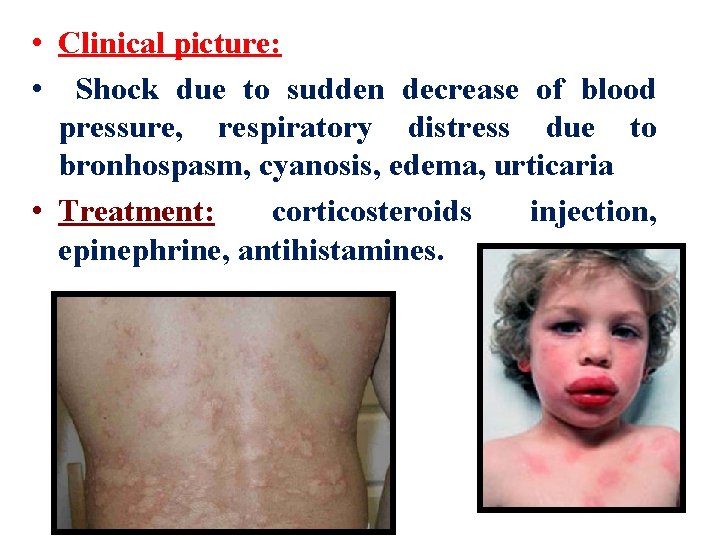
• Clinical picture: • Shock due to sudden decrease of blood pressure, respiratory distress due to bronhospasm, cyanosis, edema, urticaria • Treatment: corticosteroids injection, epinephrine, antihistamines.
2. Atopy • Local form of type I hypersensitivity. • Exposure to certain allergens that induce production of specific Ig E. • Allergens : • Inhalants: dust mite feces, pollens, mould spores. • Ingestants: milk, egg, fish, chocolate. • Contactants: wool, nylon, animal fur. • Drugs: penicillin, salicylates, anesthestics, insect venom.
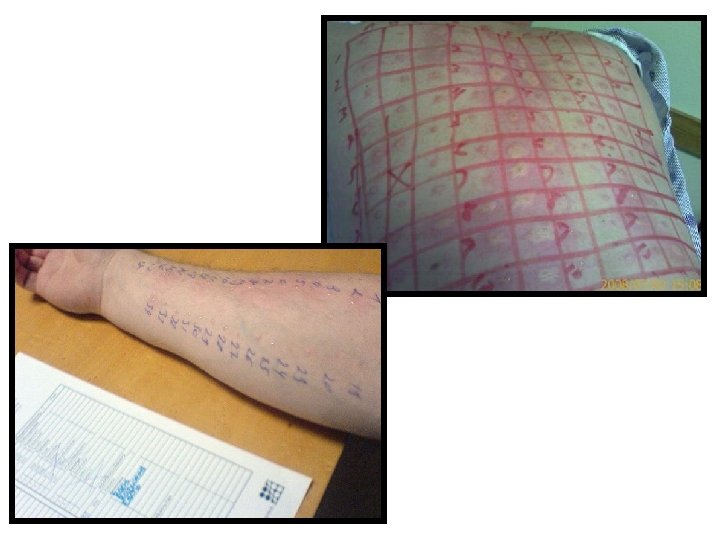
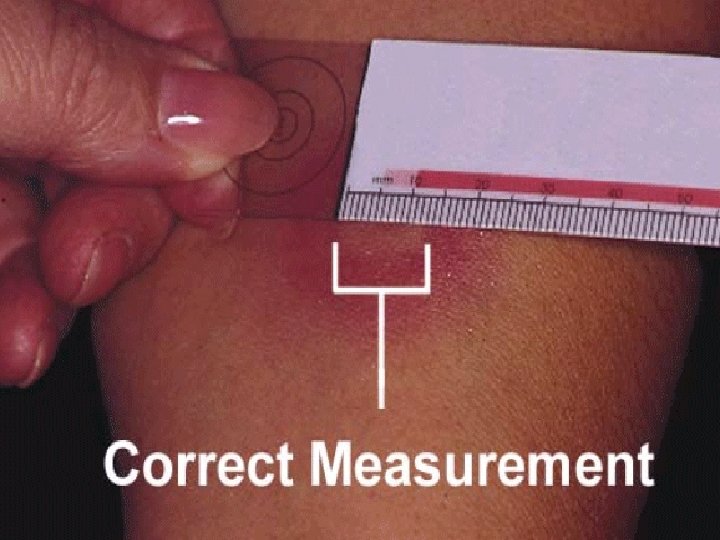
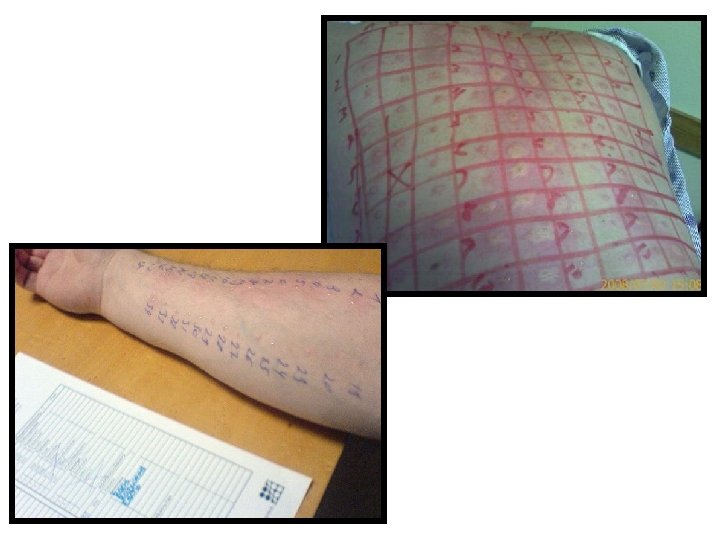
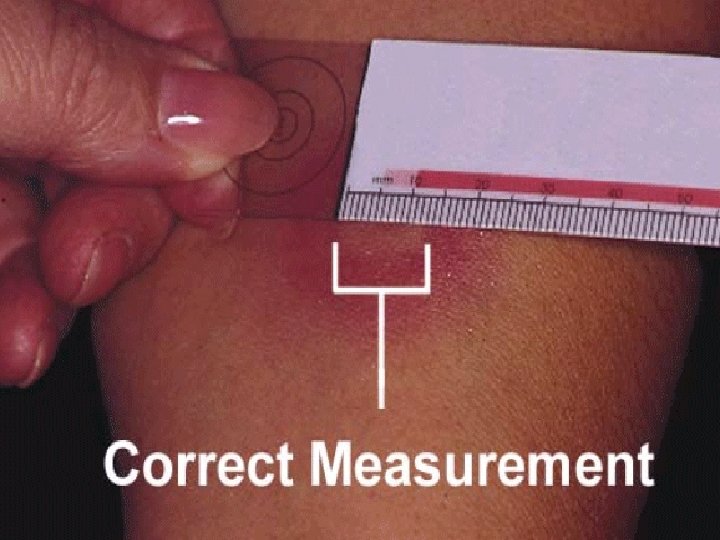
Methods of diagnosis 1) History taking for determining the allergen involved. 2) Skin tests: § Intradermal injection of battery of different allergens; A wheal and flare (erythema) develop at the site of allergen to which the person is allergic. 3) Determination of total serum Ig E level.
Management 1) Avoidance of specific allergen responsible for condition. 2) Hyposensitization: Injection of gradually increasing doses of extract of allergen. 3) Drug Therapy: corticosteroids injection, epinephrine, antihistamines.
Type II hypersensitivity: Cytotoxic or Cytolytic Reactions • An antibody (Ig. G or Ig. M) reacts with antigen fixed on the cell surface. • This antigen may be part of cell membrane or a hapten that attaches to cell membrane.
Mechanism of Cytolysis Cell lysis results due to : • 1)Complement fixation to antigen antibody complex on cell surface. Activated complement proteins (C 5 – C 9) form membrane attack complex Cell lysis. • 2)Activation of Phagocytosis by Ig. G (opsonin) bound to cell antigen. • 3) ADCC.
Clinical Examples of Type II hypersensitivity 1) Blood Transfusion reactions due to ABO incompatibility. 2) Rh-incompatability (Haemolytic disease of the newborn). 3) Autoimmune diseases: e. g. SLE, autoimmune haemolytic anaemia, idiopathic thrombocytopenic purpura. 4) Graft rejection reactions: In hyperacute rejection the recipient has antibody against the graft.
5 - Drug reaction: • Penicillin may attach as a hapten to RBCs and induce antibodies which lead to hemolysis. • Quinine may attach as a hapten to platelets and induce antibodies that cause platelets destruction and thrombocytopenic purpura.
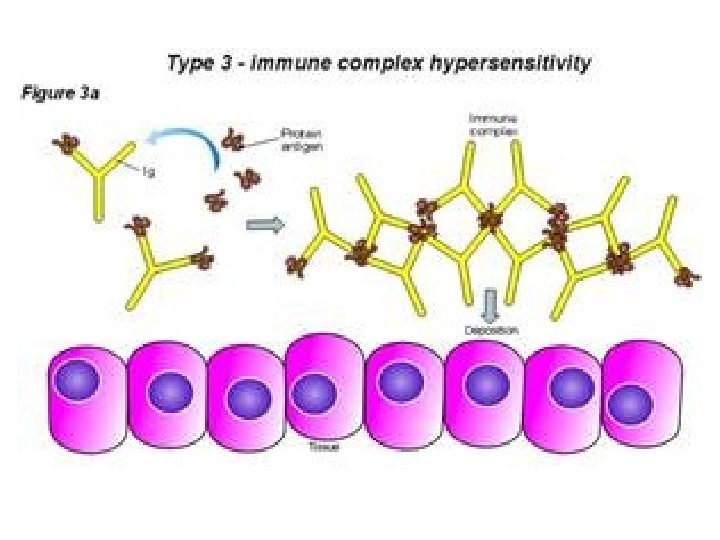
Type III: Immune Complex Mediated Reaction • When antibodies (Ig G or Ig M) and antigen coexist immune complexes are formed. • *Immune complexes are removed by reticuloendothelial system. • *Some immune complexes escape phagocytosis. • *Immune complexes deposited in tissues on the basement membrane of blood vessels and cause tissue injury.
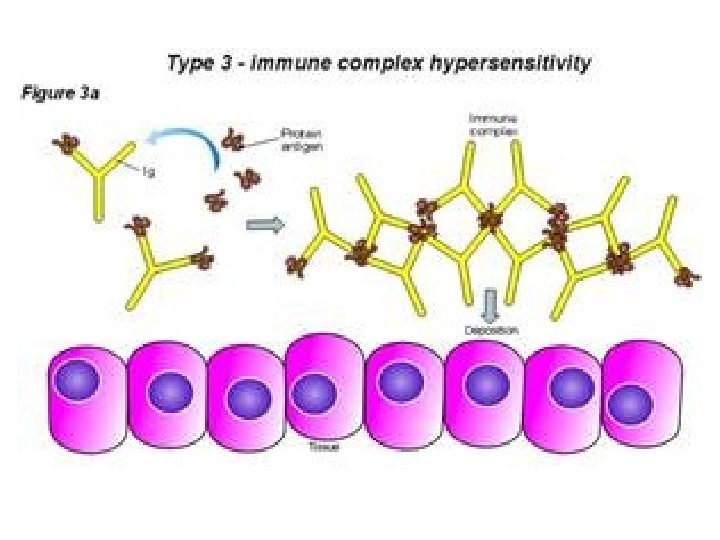
Mechanism Of Tissue Injury • Immune complexes trigger inflammatory processes: 1)Immune complexes activate the complement release anaphylatoxins C 3 a, C 5 a; stimulate degranulation of basophiles and mast cells release histamine. • Histamine increase vascular permeability and help deposition of immune complexes.
2) Neutrophils are attracted to the site by immune complexes and release lysosomal enzymes which damage tissues and intensify the inflammatory Process. 3) Platelets are aggregated with two consequences: a- release of histamine. b- form of microthrombi which lead to ischemia.

Clinical conditions of Type III Hypersensitivity • Diseases produced by immune complexes are those in which antigens persists without being eliminated as: • a- Repeated exposure to extrinsic antigen. • b- injection of large amounts of antigens. • c- Persistent infections. • d- Autoimmunity to self components.
1 - Arthus Reaction • This is a local immune complex deposition phenomenon e. g. diabetic patients receiving insulin subcutaneously. edema • Local reactions in the form of erythema necrosis • Immune complexes deposited in small blood vessels. • leading to; vasculitis, microthrombi formation, vascular occlusion, necrosis.
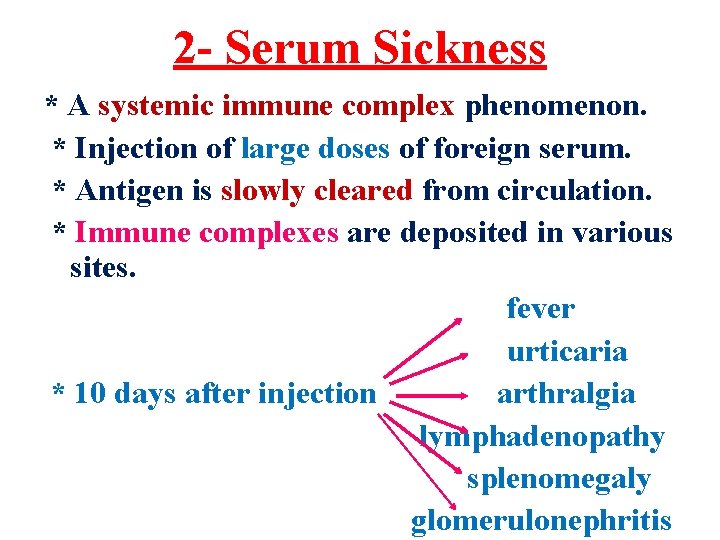
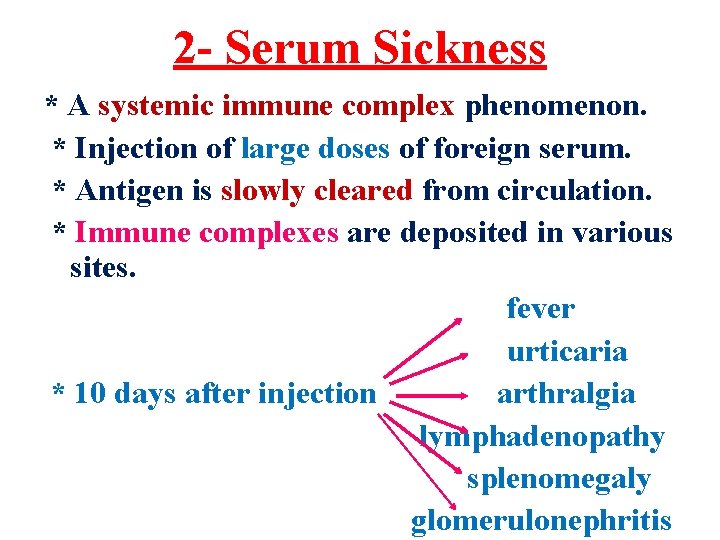
2 - Serum Sickness * A systemic immune complex phenomenon. * Injection of large doses of foreign serum. * Antigen is slowly cleared from circulation. * Immune complexes are deposited in various sites. fever urticaria * 10 days after injection arthralgia lymphadenopathy splenomegaly glomerulonephritis
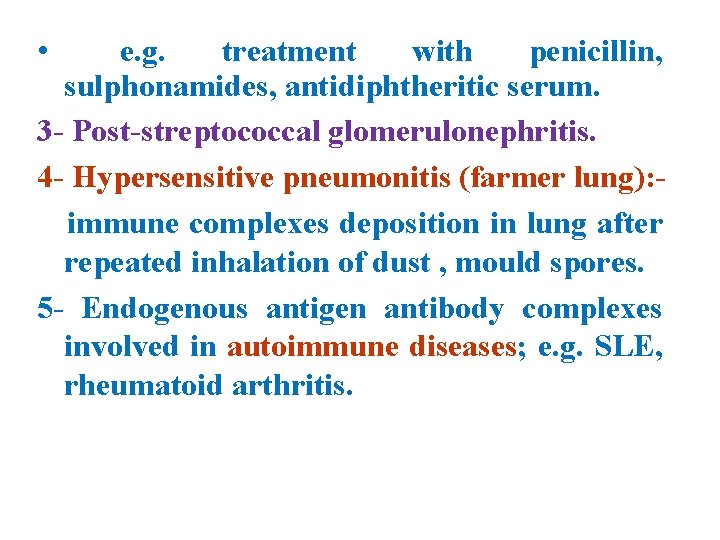
• e. g. treatment with penicillin, sulphonamides, antidiphtheritic serum. 3 - Post-streptococcal glomerulonephritis. 4 - Hypersensitive pneumonitis (farmer lung): immune complexes deposition in lung after repeated inhalation of dust , mould spores. 5 - Endogenous antigen antibody complexes involved in autoimmune diseases; e. g. SLE, rheumatoid arthritis.
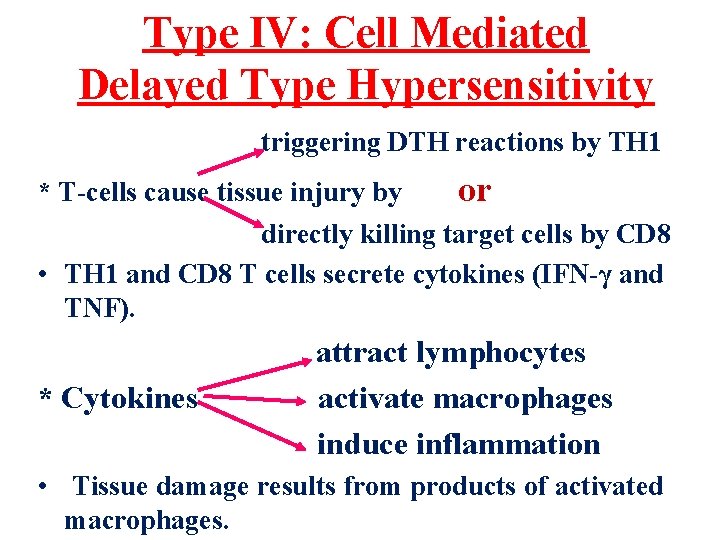
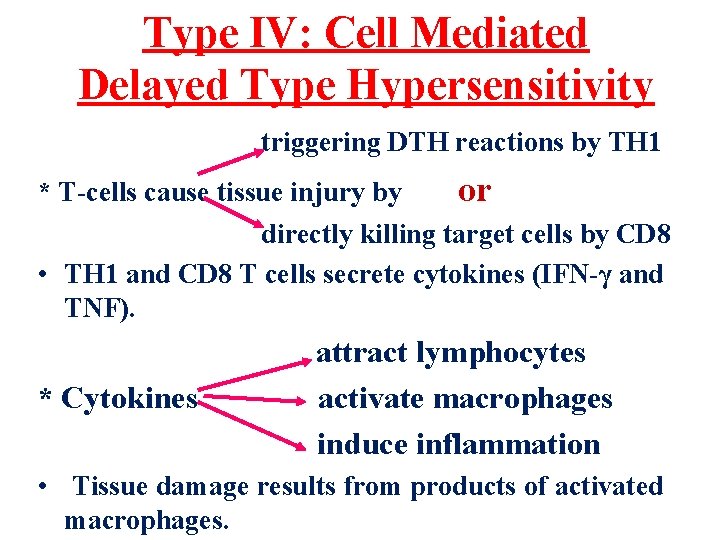
Type IV: Cell Mediated Delayed Type Hypersensitivity triggering DTH reactions by TH 1 * T-cells cause tissue injury by or directly killing target cells by CD 8 • TH 1 and CD 8 T cells secrete cytokines (IFN-γ and TNF). * Cytokines attract lymphocytes activate macrophages induce inflammation • Tissue damage results from products of activated macrophages.
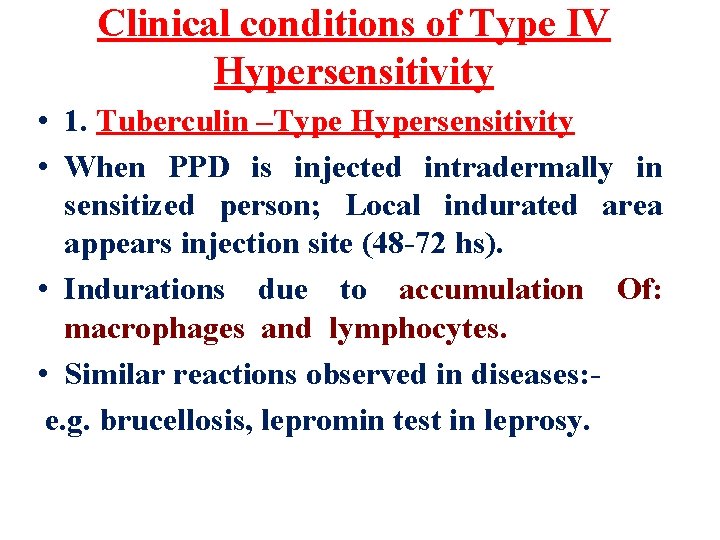
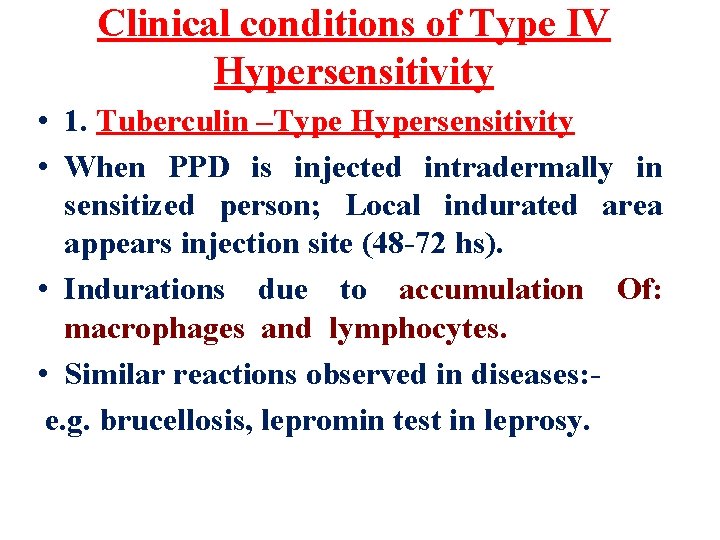
Clinical conditions of Type IV Hypersensitivity • 1. Tuberculin –Type Hypersensitivity • When PPD is injected intradermally in sensitized person; Local indurated area appears injection site (48 -72 hs). • Indurations due to accumulation Of: macrophages and lymphocytes. • Similar reactions observed in diseases: e. g. brucellosis, lepromin test in leprosy.
2. Granulomatous lesions * In chronic diseases : T. B. , Leprosy, schistosomiases. * Intracellular organisms resist destruction by macrophages. * Persistent antigen in tissues stimulate local DTH reaction. * Continuous release of cytokines leads to accumulation of macrophages which give rise to epitheloidal and giant cell granuloma.
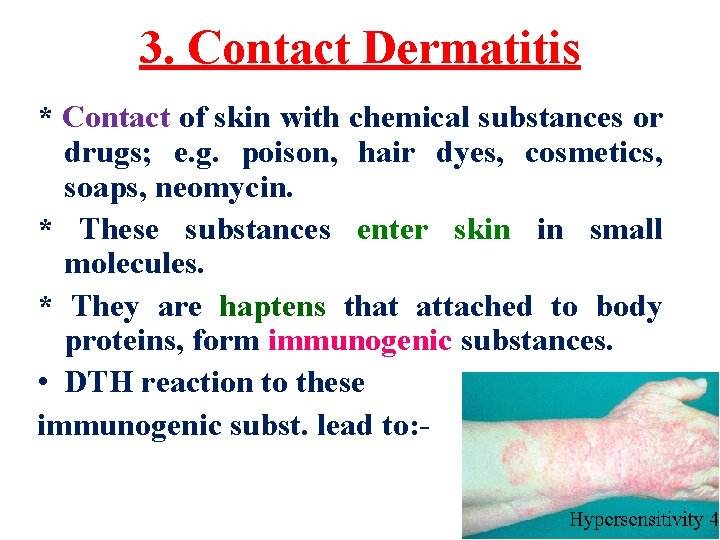
3. Contact Dermatitis * Contact of skin with chemical substances or drugs; e. g. poison, hair dyes, cosmetics, soaps, neomycin. * These substances enter skin in small molecules. * They are haptens that attached to body proteins, form immunogenic substances. • DTH reaction to these immunogenic subst. lead to: -
eczema • inflammatory reaction of skin rash vesicular eruption • 4) Auto immune diseases and graft rejection • 5) Insulin dependant diabetes mellitus: - Tcells invade the pancreatic islets and specifically destroy insulin secreting beta cells.
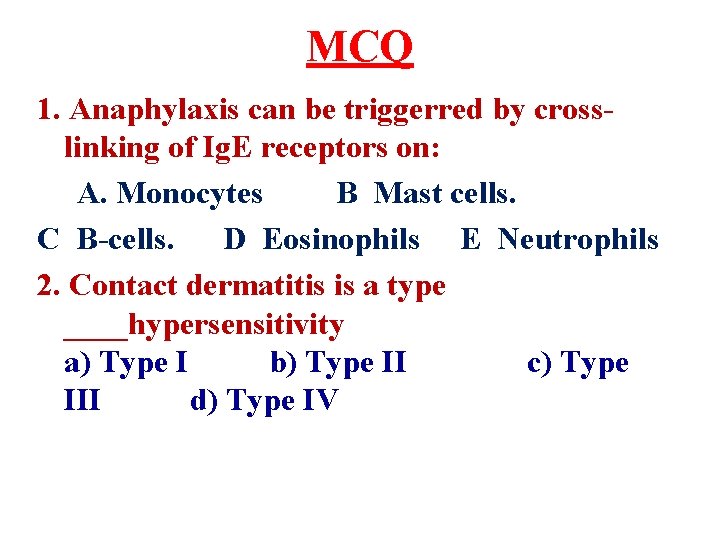
MCQ 1. Anaphylaxis can be triggerred by crosslinking of Ig. E receptors on: A. Monocytes B Mast cells. C B-cells. D Eosinophils E Neutrophils 2. Contact dermatitis is a type ____hypersensitivity a) Type I b) Type II c) Type III d) Type IV
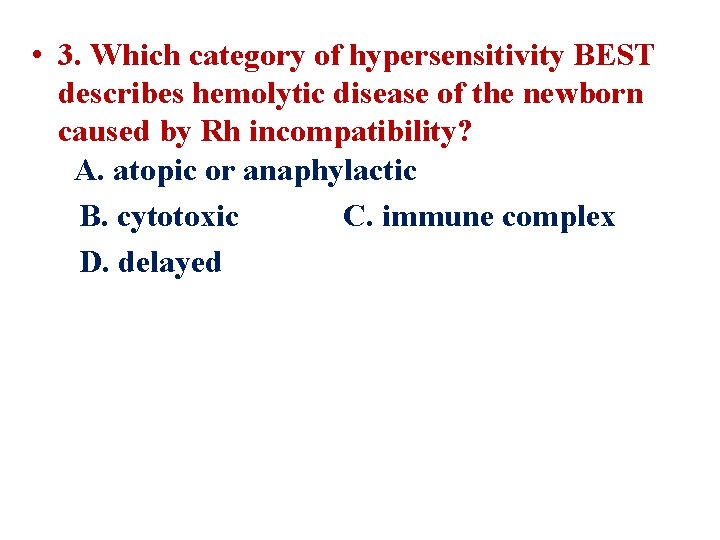
• 3. Which category of hypersensitivity BEST describes hemolytic disease of the newborn caused by Rh incompatibility? A. atopic or anaphylactic B. cytotoxic C. immune complex D. delayed
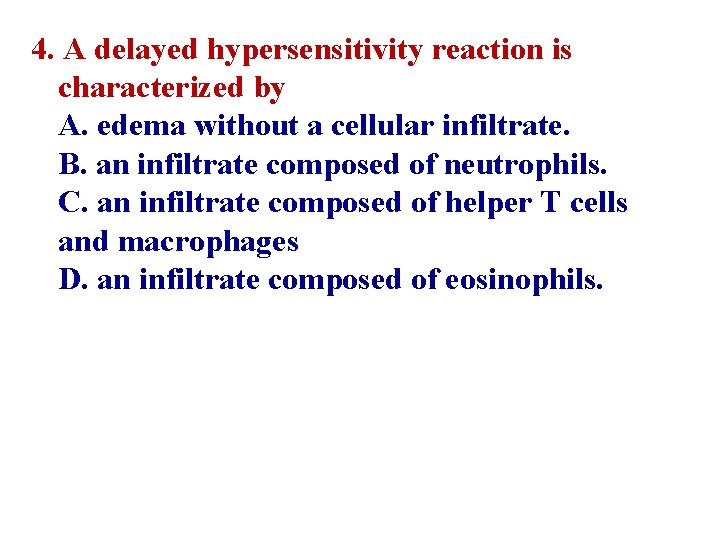
4. A delayed hypersensitivity reaction is characterized by A. edema without a cellular infiltrate. B. an infiltrate composed of neutrophils. C. an infiltrate composed of helper T cells and macrophages D. an infiltrate composed of eosinophils.