Lecture 13 Bone Tissue Objectives Chapter 7 1
Lecture # 13: Bone Tissue Objectives: (Chapter 7) 1 - Describe the gross anatomical features of a typical long bone and a typical short bone. 2 - Discuss the microscopic structure of compact bone and compare it to that of cancellous bone. 3 Define ossification and distinguish between intramembranous and endochondral ossification. 4 - Explain the effects of vitamin D and various hormones on bone physiology and plasma Ca++.
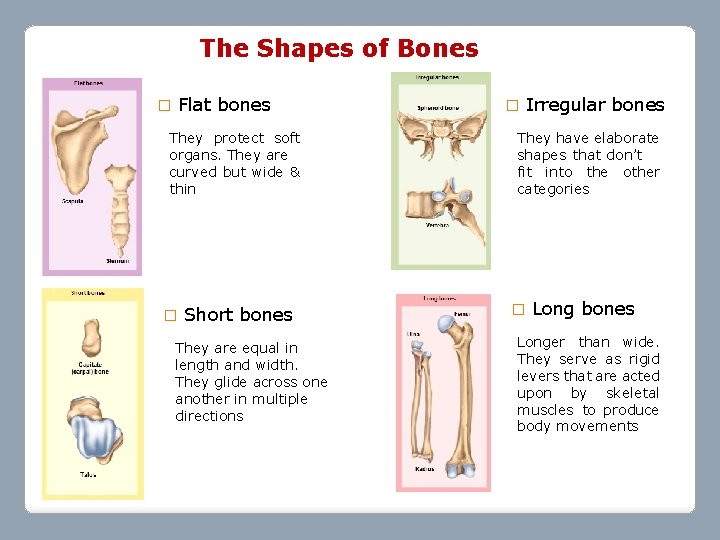
The Shapes of Bones � Flat bones They protect soft organs. They are curved but wide & thin � Short bones They are equal in length and width. They glide across one another in multiple directions � Irregular bones They have elaborate shapes that don’t fit into the other categories � Long bones Longer than wide. They serve as rigid levers that are acted upon by skeletal muscles to produce body movements
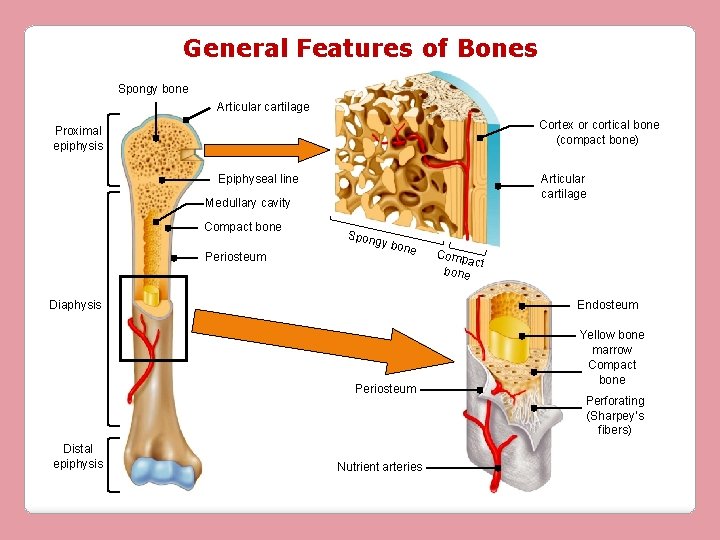
General Features of Bones Spongy bone Articular cartilage Cortex or cortical bone (compact bone) Proximal epiphysis Epiphyseal line Articular cartilage Medullary cavity Compact bone Periosteum Spon gy bo ne Endosteum Diaphysis Periosteum Distal epiphysis Comp act bone Nutrient arteries Yellow bone marrow Compact bone Perforating (Sharpey’s fibers)
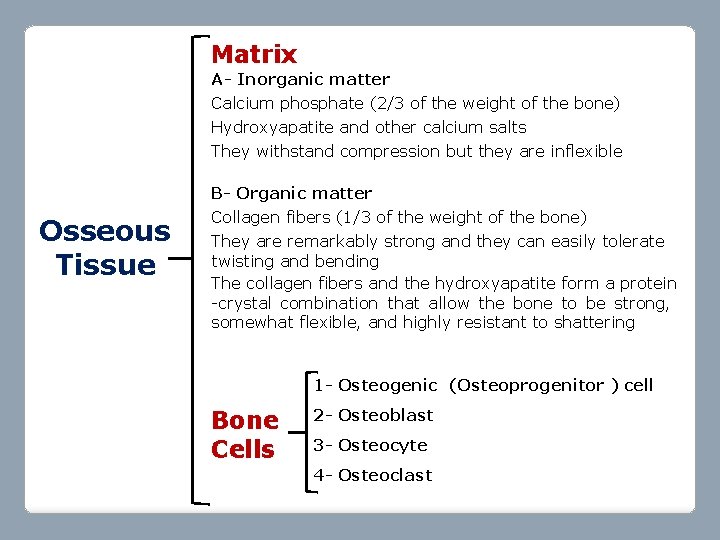
Matrix A- Inorganic matter Calcium phosphate (2/3 of the weight of the bone) Hydroxyapatite and other calcium salts They withstand compression but they are inflexible B- Organic matter Osseous Tissue Collagen fibers (1/3 of the weight of the bone) They are remarkably strong and they can easily tolerate twisting and bending The collagen fibers and the hydroxyapatite form a protein -crystal combination that allow the bone to be strong, somewhat flexible, and highly resistant to shattering 1 - Osteogenic (Osteoprogenitor ) cell Bone Cells 2 - Osteoblast 3 - Osteocyte 4 - Osteoclast
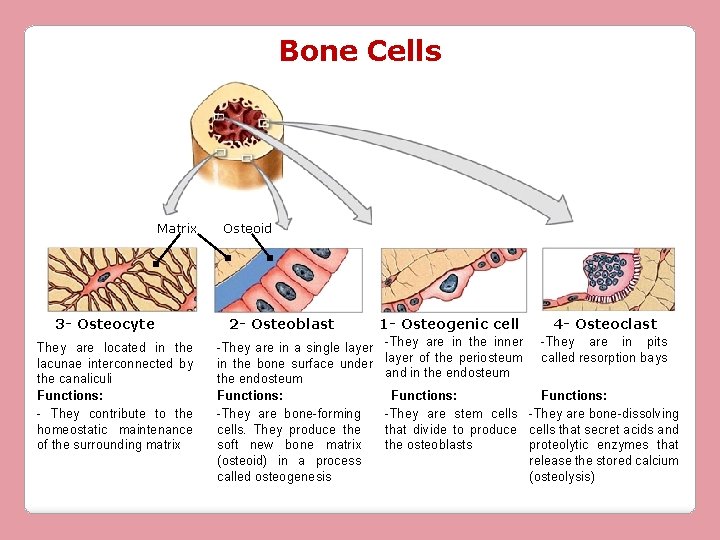
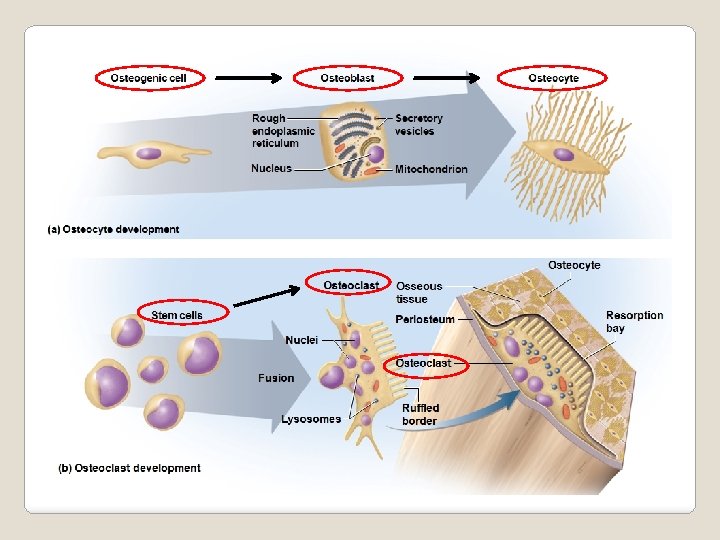
Bone Cells Matrix 3 - Osteocyte They are located in the lacunae interconnected by the canaliculi Functions: - They contribute to the homeostatic maintenance of the surrounding matrix Osteoid 2 - Osteoblast -They are in a single layer in the bone surface under the endosteum Functions: -They are bone-forming cells. They produce the soft new bone matrix (osteoid) in a process called osteogenesis 1 - Osteogenic cell -They are in the inner layer of the periosteum and in the endosteum 4 - Osteoclast -They are in pits called resorption bays Functions: -They are stem cells -They are bone-dissolving that divide to produce cells that secret acids and the osteoblasts proteolytic enzymes that release the stored calcium (osteolysis)
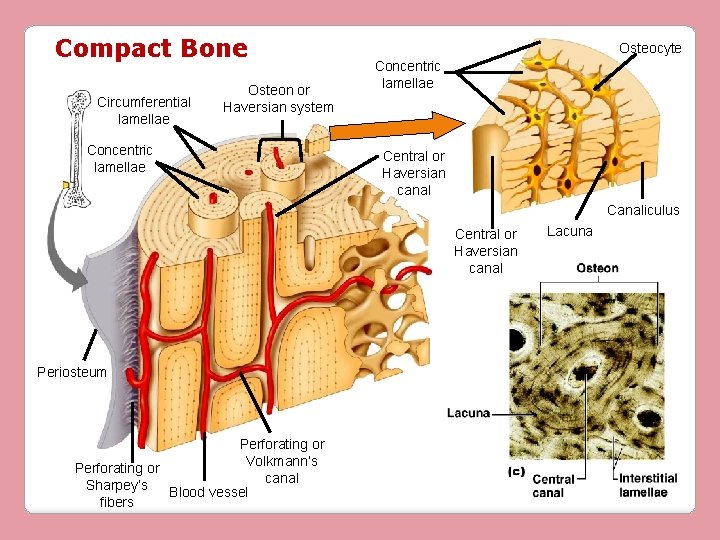
Compact Bone Circumferential lamellae Osteon or Haversian system Concentric lamellae Osteocyte Concentric lamellae Central or Haversian canal Canaliculus Central or Haversian canal Periosteum Perforating or Volkmann’s Perforating or canal Sharpey’s Blood vessel fibers Lacuna
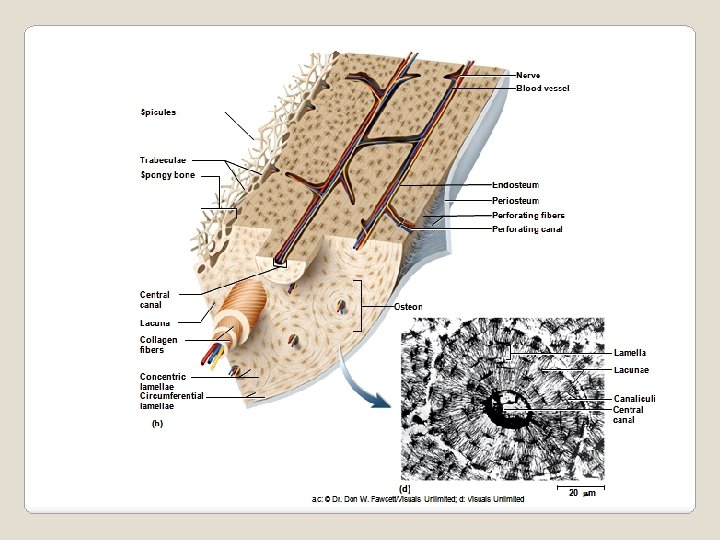
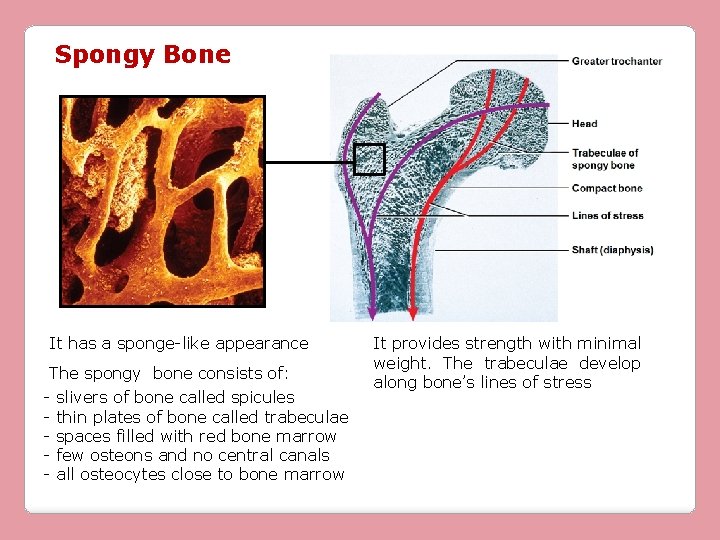
Spongy Bone It has a sponge-like appearance The spongy bone consists of: - slivers of bone called spicules - thin plates of bone called trabeculae - spaces filled with red bone marrow - few osteons and no central canals - all osteocytes close to bone marrow It provides strength with minimal weight. The trabeculae develop along bone’s lines of stress
Bone Development Ossification or Osteogenesis is the formation of bone During ossification, deposit of calcium salts occurs (calcification), but calcification occurs also in other tissues. When calcification occurs in tissues other than bones, the result is calcified tissue that does not resemble bone. Ossification occurs during the whole life 1 - Embryo: Formation of bonny skeleton 2 - Until early adulthood: Bone growth 3 - Adulthood: Remodeling and repair
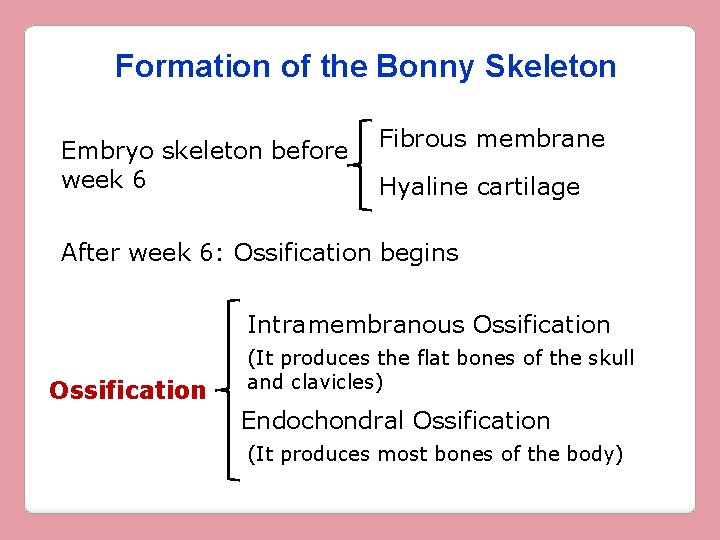
Formation of the Bonny Skeleton Embryo skeleton before week 6 Fibrous membrane Hyaline cartilage After week 6: Ossification begins Intramembranous Ossification (It produces the flat bones of the skull and clavicles) Endochondral Ossification (It produces most bones of the body)
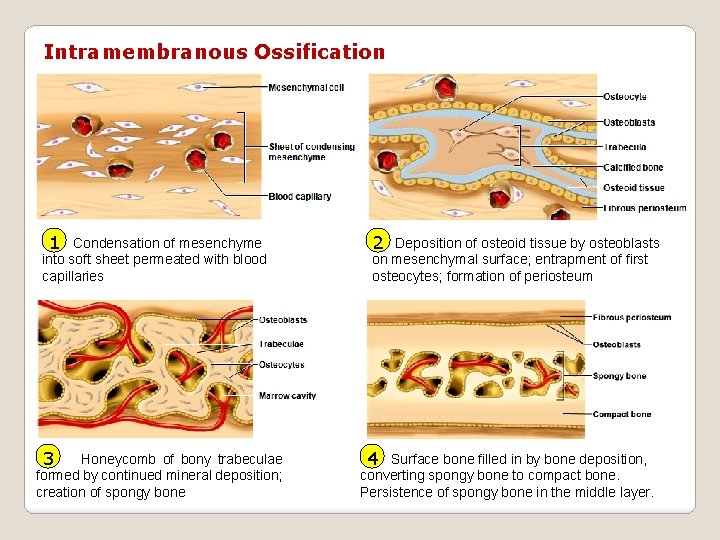
Intramembranous Ossification 1 Condensation of mesenchyme into soft sheet permeated with blood capillaries 3 Honeycomb of bony trabeculae formed by continued mineral deposition; creation of spongy bone 2 Deposition of osteoid tissue by osteoblasts on mesenchymal surface; entrapment of first osteocytes; formation of periosteum 4 Surface bone filled in by bone deposition, converting spongy bone to compact bone. Persistence of spongy bone in the middle layer.
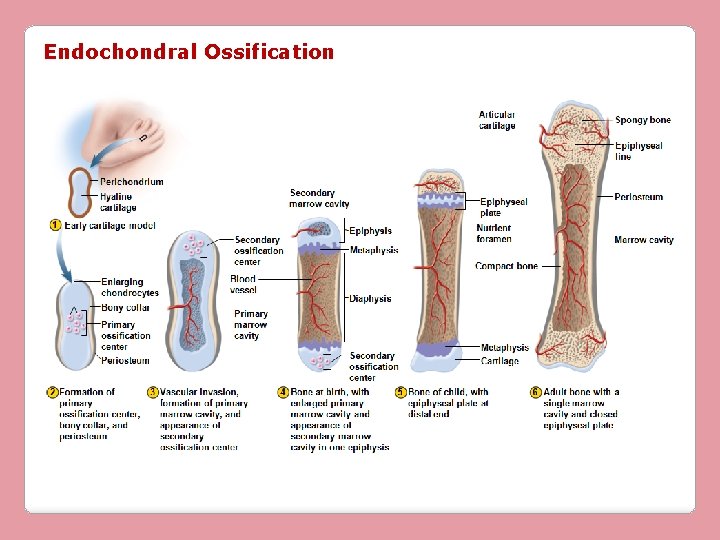
Endochondral Ossification
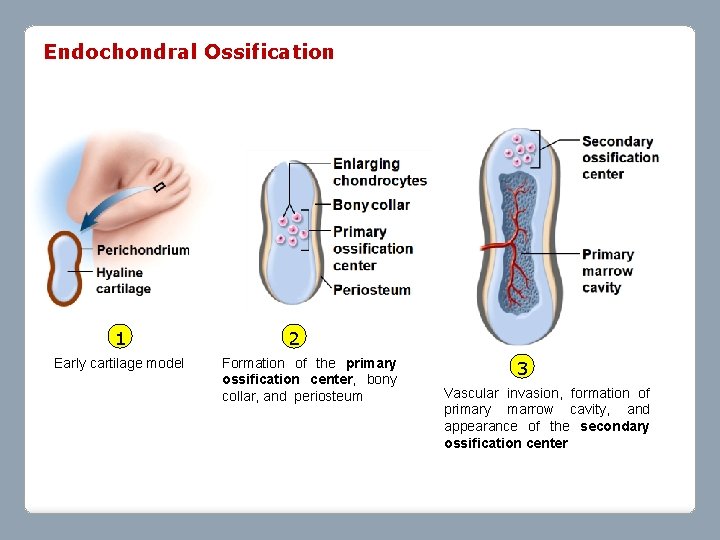
Endochondral Ossification 1 Early cartilage model 2 Formation of the primary ossification center, bony collar, and periosteum 3 Vascular invasion, formation of primary marrow cavity, and appearance of the secondary ossification center
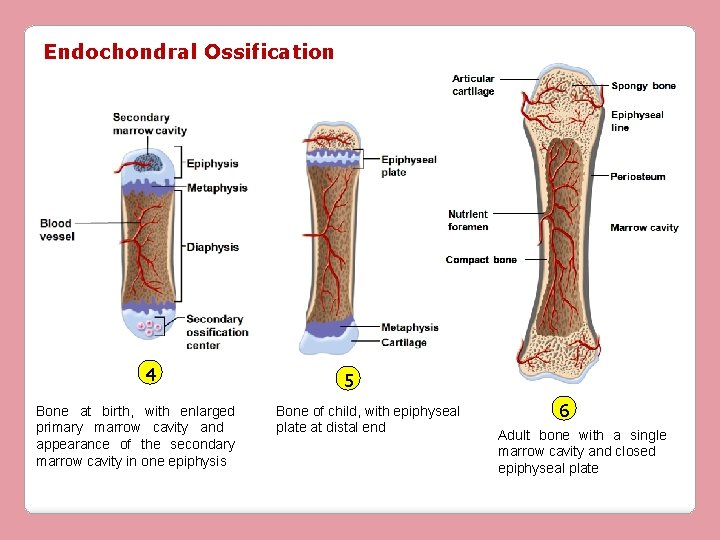
Endochondral Ossification 4 Bone at birth, with enlarged primary marrow cavity and appearance of the secondary marrow cavity in one epiphysis 5 Bone of child, with epiphyseal plate at distal end 6 Adult bone with a single marrow cavity and closed epiphyseal plate
Endochondral Ossification All bones of the skeleton below the base of the skull, except the clavicles Intramembranous Ossification Cranial bones of the skull, mandible, and clavicles
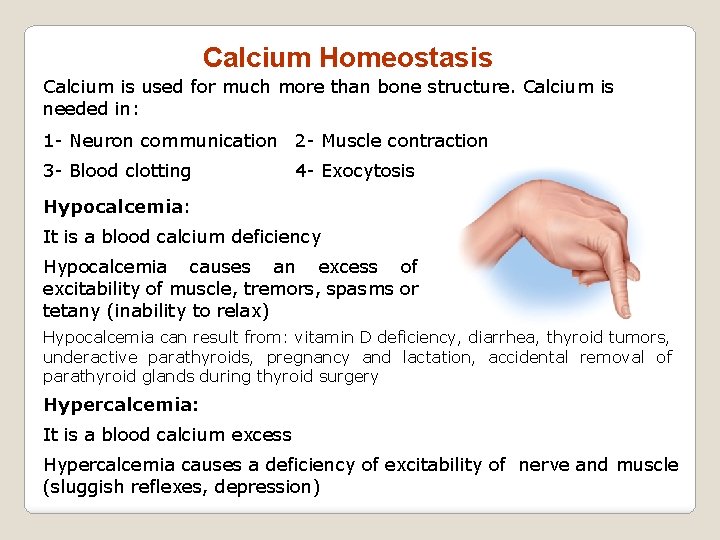
Calcium Homeostasis Calcium is used for much more than bone structure. Calcium is needed in: 1 - Neuron communication 2 - Muscle contraction 3 - Blood clotting 4 - Exocytosis Hypocalcemia: It is a blood calcium deficiency Hypocalcemia causes an excess of excitability of muscle, tremors, spasms or tetany (inability to relax) Hypocalcemia can result from: vitamin D deficiency, diarrhea, thyroid tumors, underactive parathyroids, pregnancy and lactation, accidental removal of parathyroid glands during thyroid surgery Hypercalcemia: It is a blood calcium excess Hypercalcemia causes a deficiency of excitability of nerve and muscle (sluggish reflexes, depression)
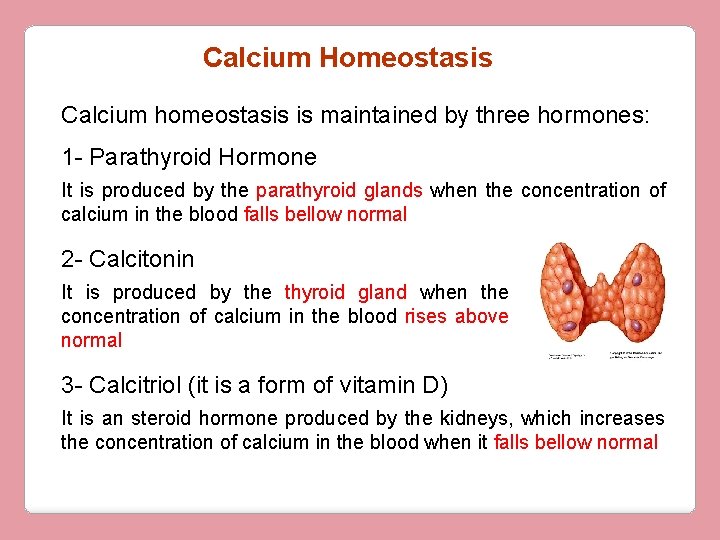
Calcium Homeostasis Calcium homeostasis is maintained by three hormones: 1 - Parathyroid Hormone It is produced by the parathyroid glands when the concentration of calcium in the blood falls bellow normal 2 - Calcitonin It is produced by the thyroid gland when the concentration of calcium in the blood rises above normal 3 - Calcitriol (it is a form of vitamin D) It is an steroid hormone produced by the kidneys, which increases the concentration of calcium in the blood when it falls bellow normal
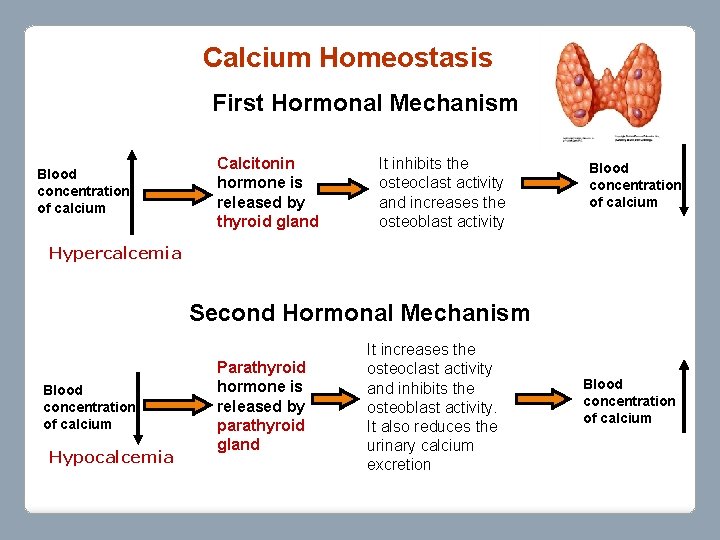
Calcium Homeostasis First Hormonal Mechanism Blood concentration of calcium Calcitonin hormone is released by thyroid gland It inhibits the osteoclast activity and increases the osteoblast activity Blood concentration of calcium Hypercalcemia Second Hormonal Mechanism Blood concentration of calcium Hypocalcemia Parathyroid hormone is released by parathyroid gland It increases the osteoclast activity and inhibits the osteoblast activity. It also reduces the urinary calcium excretion Blood concentration of calcium
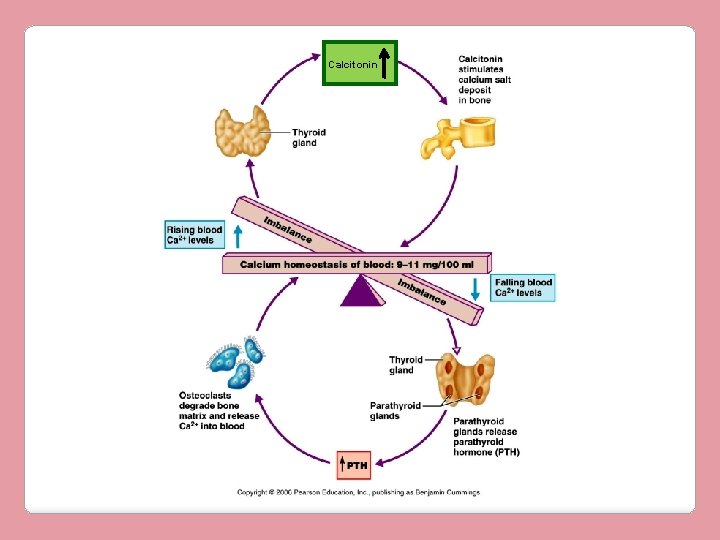
Calcitonin
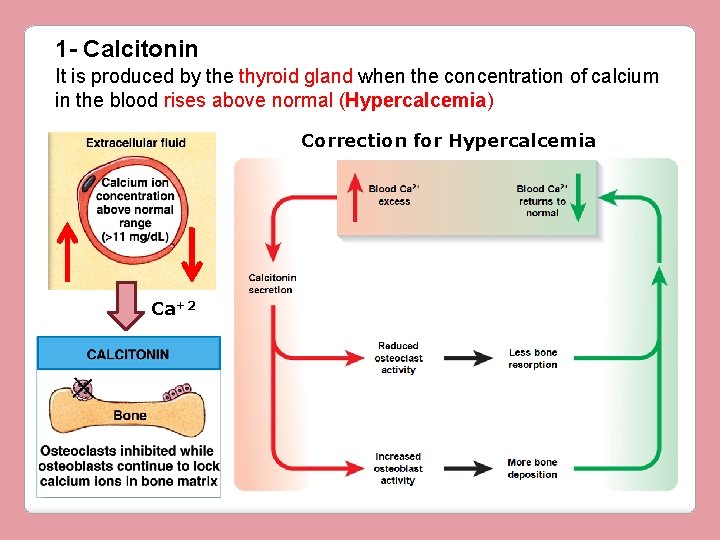
1 - Calcitonin It is produced by the thyroid gland when the concentration of calcium in the blood rises above normal (Hypercalcemia) Correction for Hypercalcemia Ca+2
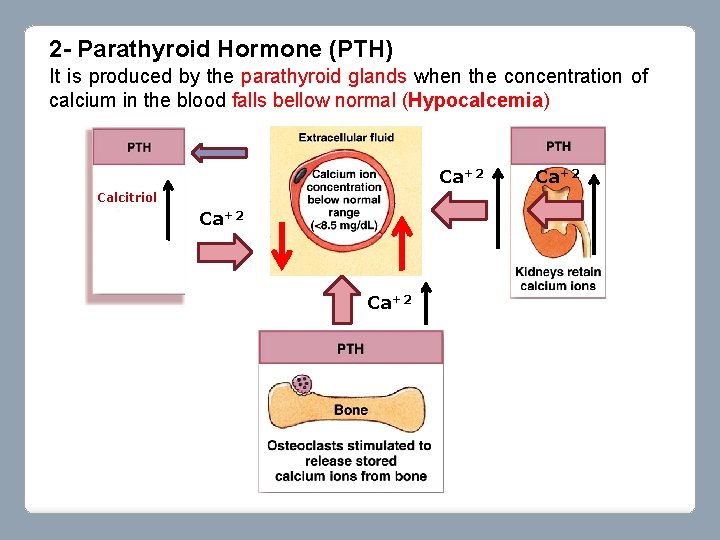
2 - Parathyroid Hormone (PTH) It is produced by the parathyroid glands when the concentration of calcium in the blood falls bellow normal (Hypocalcemia) Ca+2 Calcitriol Ca+2
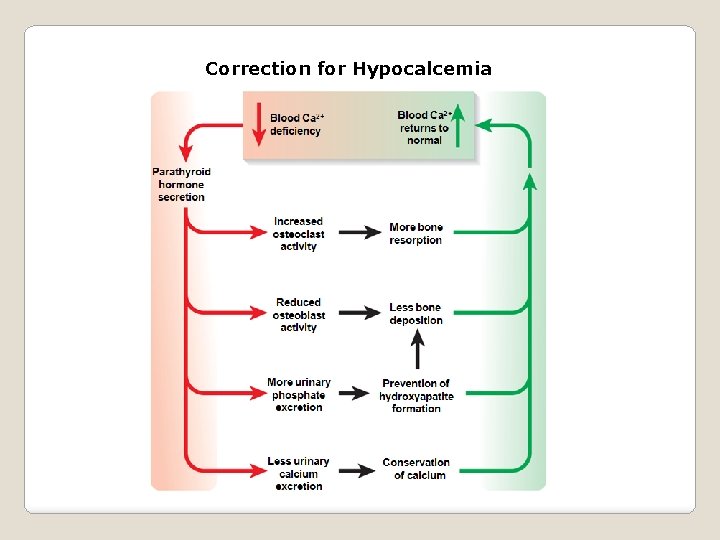
Correction for Hypocalcemia
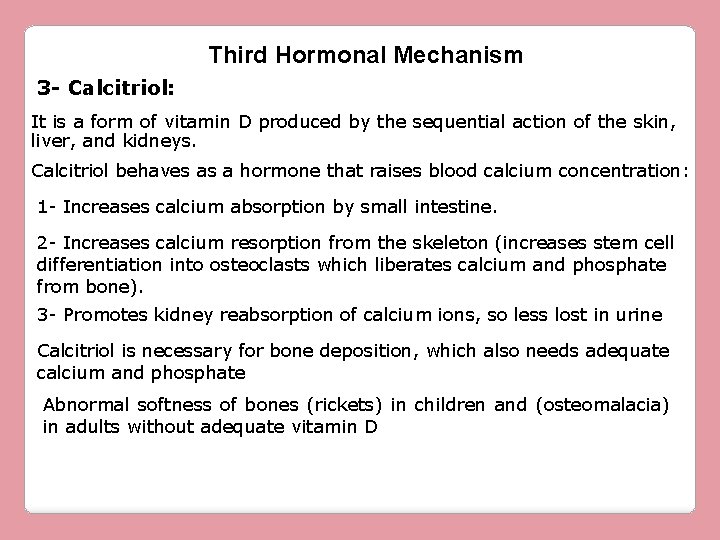
Third Hormonal Mechanism 3 - Calcitriol: It is a form of vitamin D produced by the sequential action of the skin, liver, and kidneys. Calcitriol behaves as a hormone that raises blood calcium concentration: 1 - Increases calcium absorption by small intestine. 2 - Increases calcium resorption from the skeleton (increases stem cell differentiation into osteoclasts which liberates calcium and phosphate from bone). 3 - Promotes kidney reabsorption of calcium ions, so less lost in urine Calcitriol is necessary for bone deposition, which also needs adequate calcium and phosphate Abnormal softness of bones (rickets) in children and (osteomalacia) in adults without adequate vitamin D
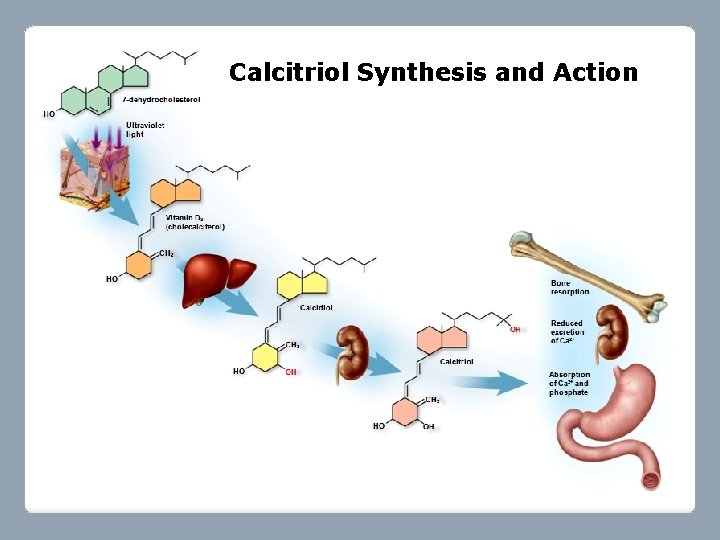
Calcitriol Synthesis and Action
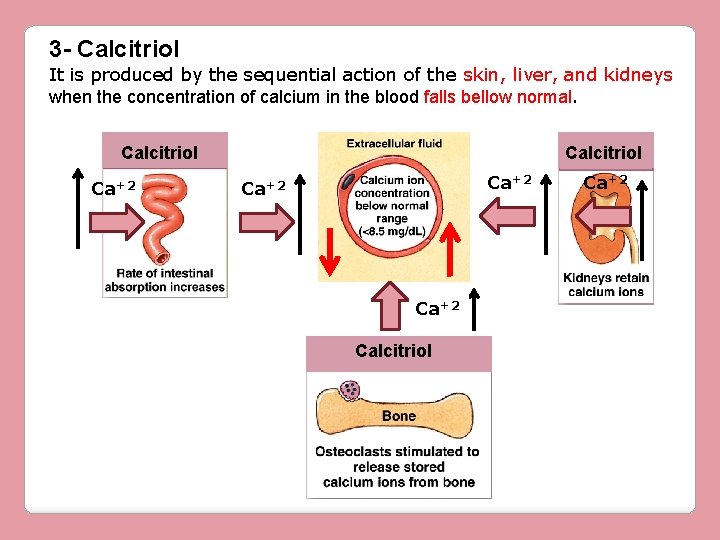
3 - Calcitriol It is produced by the sequential action of the skin, liver, and kidneys when the concentration of calcium in the blood falls bellow normal. Calcitriol Ca+2 Calcitriol Ca+2
- Slides: 26