Lecture 10 HEPATIC CLEARANCE Outline Hepatic Blood Flow
Lecture #10 HEPATIC CLEARANCE
Outline • • Hepatic Blood Flow (QH) Liver Factors that Effect Hepatic Elimination Intrinsic Clearance Biliary Clearance Extraction Ratio Hepatic Clearance
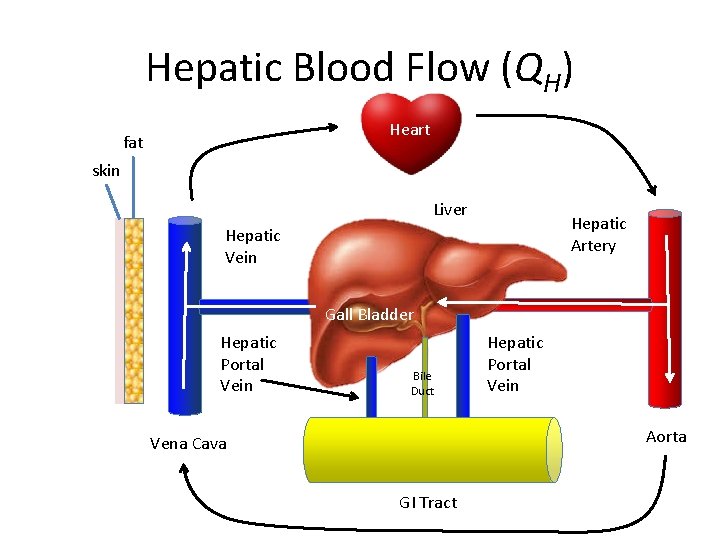
Hepatic Blood Flow (QH) Heart fat skin Liver Hepatic Artery Hepatic Vein Gall Bladder Hepatic Portal Vein Bile Duct Hepatic Portal Vein Aorta Vena Cava GI Tract
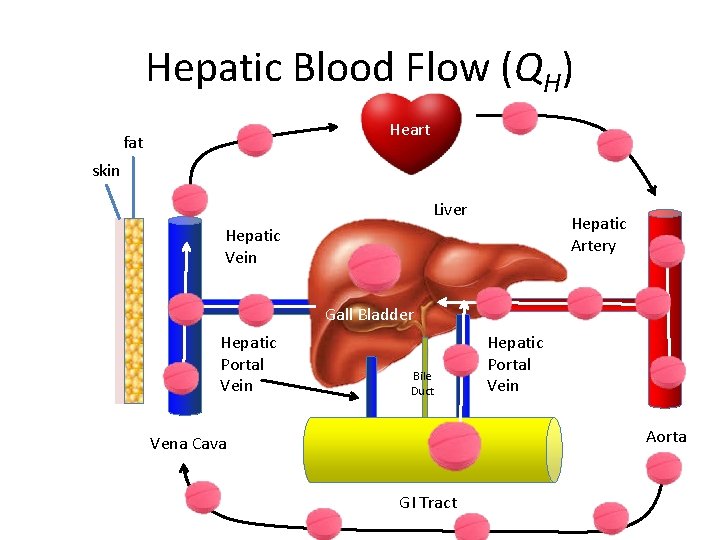
Hepatic Blood Flow (QH) Heart fat skin Liver Hepatic Artery Hepatic Vein Gall Bladder Hepatic Portal Vein Bile Duct Hepatic Portal Vein Aorta Vena Cava GI Tract
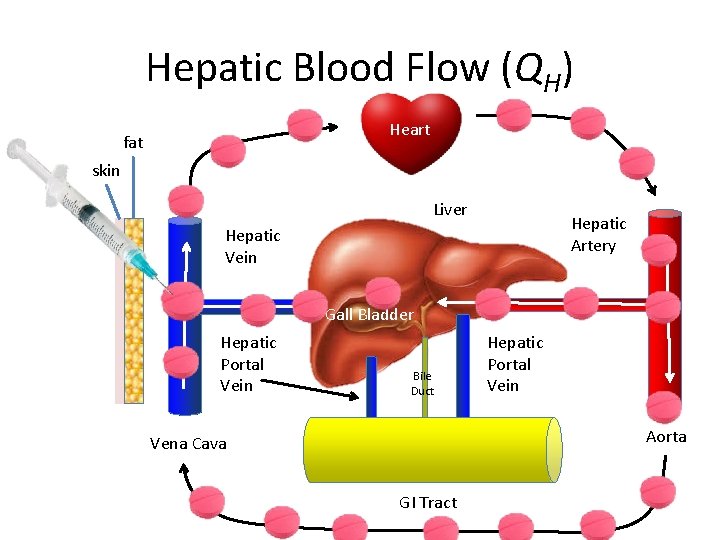
Hepatic Blood Flow (QH) Heart fat skin Liver Hepatic Artery Hepatic Vein Gall Bladder Hepatic Portal Vein Bile Duct Hepatic Portal Vein Aorta Vena Cava GI Tract
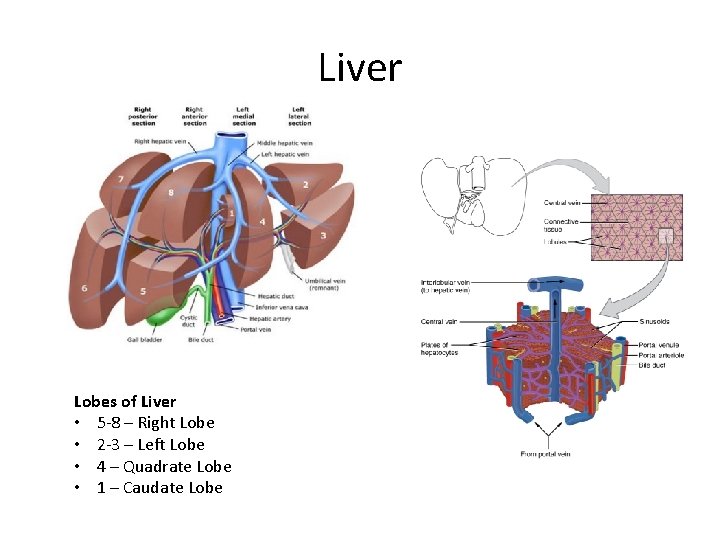
Liver Lobes of Liver • 5 -8 – Right Lobe • 2 -3 – Left Lobe • 4 – Quadrate Lobe • 1 – Caudate Lobe
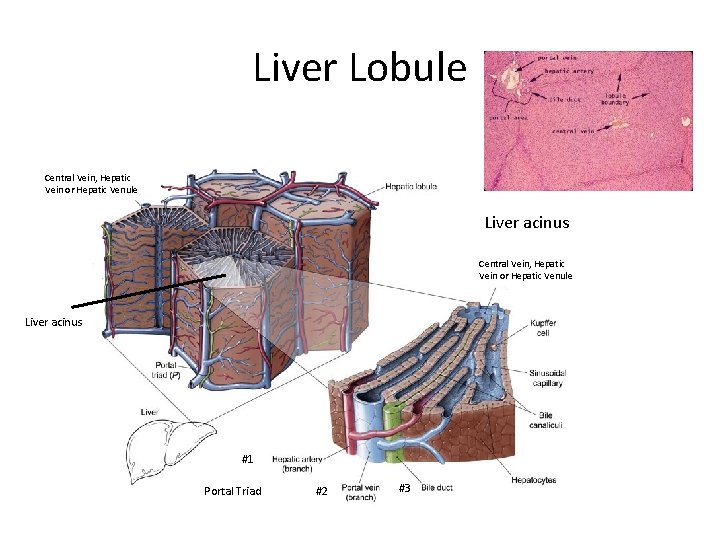
Liver Lobule Central Vein, Hepatic Vein or Hepatic Venule Liver acinus #1 Portal Triad #2 #3
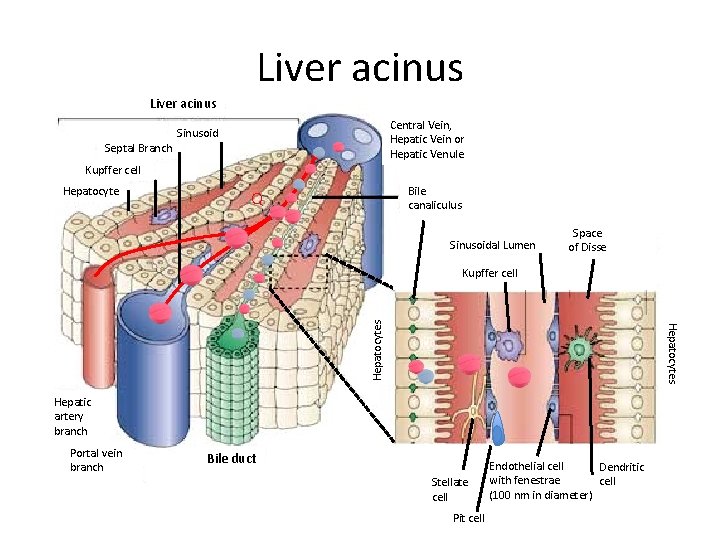
Liver acinus Septal Branch Central Vein, Hepatic Vein or Hepatic Venule Sinusoid Kupffer cell Hepatocyte Bile canaliculus Q Sinusoidal Lumen Space of Disse Hepatocytes Kupffer cell Hepatic artery branch Portal vein branch Bile duct Stellate cell Pit cell Endothelial cell Dendritic with fenestrae cell (100 nm in diameter)
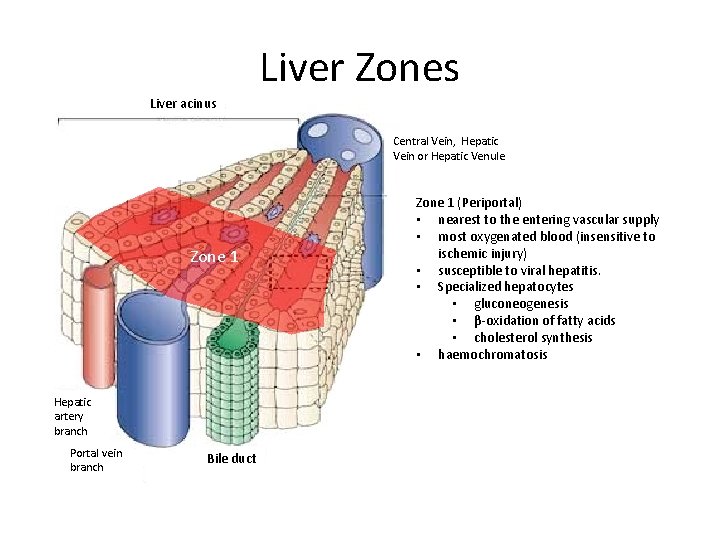
Liver Zones Liver acinus Central Vein, Hepatic Vein or Hepatic Venule Zone 1 Hepatic artery branch Portal vein branch Bile duct Zone 1 (Periportal) • nearest to the entering vascular supply • most oxygenated blood (insensitive to ischemic injury) • susceptible to viral hepatitis. • Specialized hepatocytes • gluconeogenesis • β-oxidation of fatty acids • cholesterol synthesis • haemochromatosis
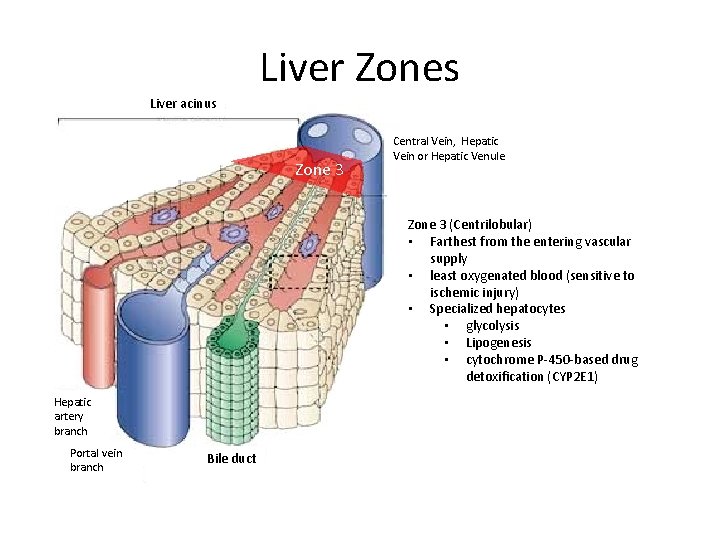
Liver Zones Liver acinus Zone 3 Central Vein, Hepatic Vein or Hepatic Venule Zone 3 (Centrilobular) • Farthest from the entering vascular supply • least oxygenated blood (sensitive to ischemic injury) • Specialized hepatocytes • glycolysis • Lipogenesis • cytochrome P-450 -based drug detoxification (CYP 2 E 1) Hepatic artery branch Portal vein branch Bile duct
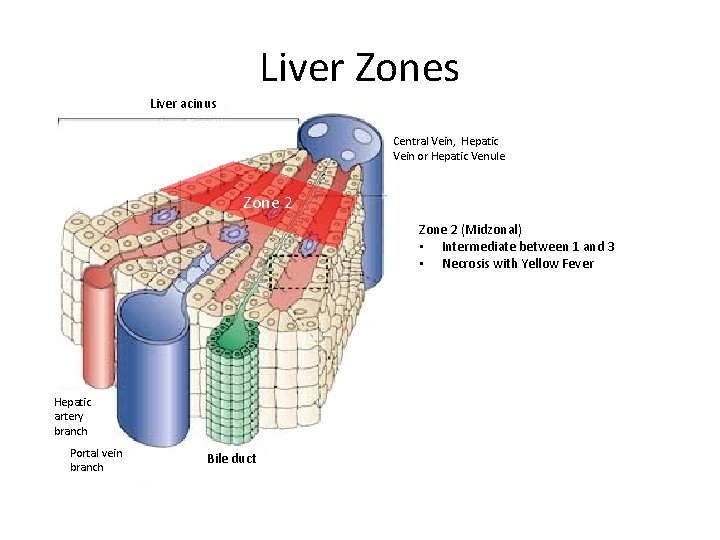
Liver Zones Liver acinus Central Vein, Hepatic Vein or Hepatic Venule Zone 2 (Midzonal) • Intermediate between 1 and 3 • Necrosis with Yellow Fever Hepatic artery branch Portal vein branch Bile duct
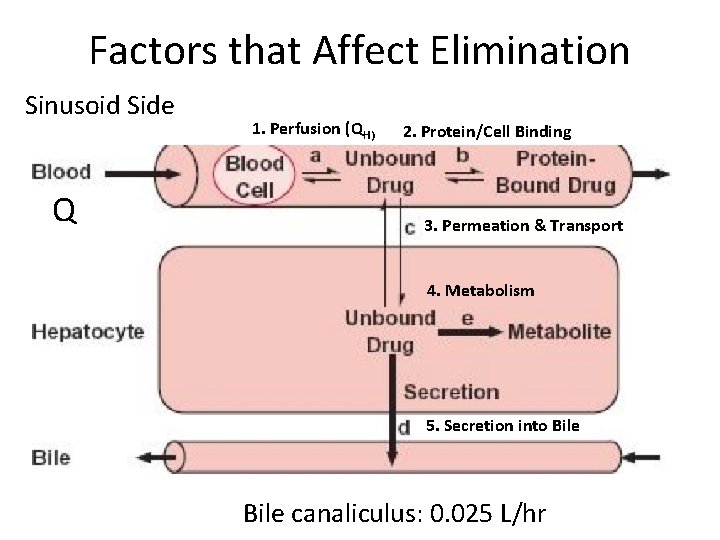
Factors that Affect Elimination Sinusoid Side Q 1. Perfusion (QH) 2. Protein/Cell Binding 3. Permeation & Transport 4. Metabolism 5. Secretion into Bile canaliculus: 0. 025 L/hr
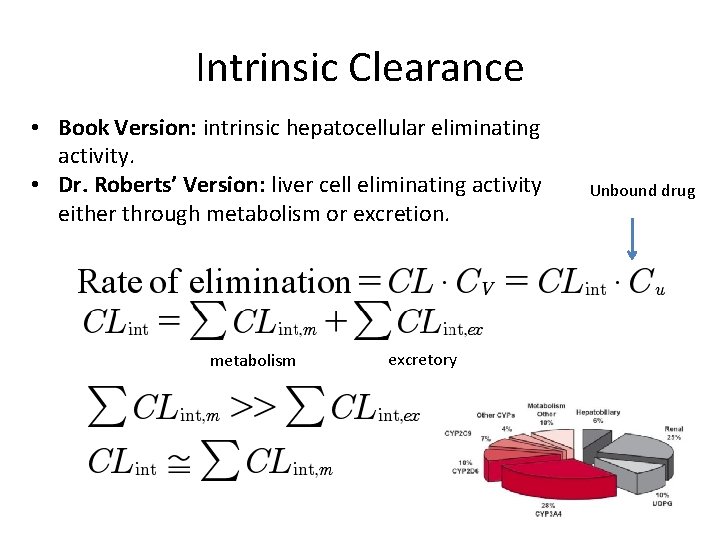
Intrinsic Clearance • Book Version: intrinsic hepatocellular eliminating activity. • Dr. Roberts’ Version: liver cell eliminating activity either through metabolism or excretion. metabolism excretory Unbound drug
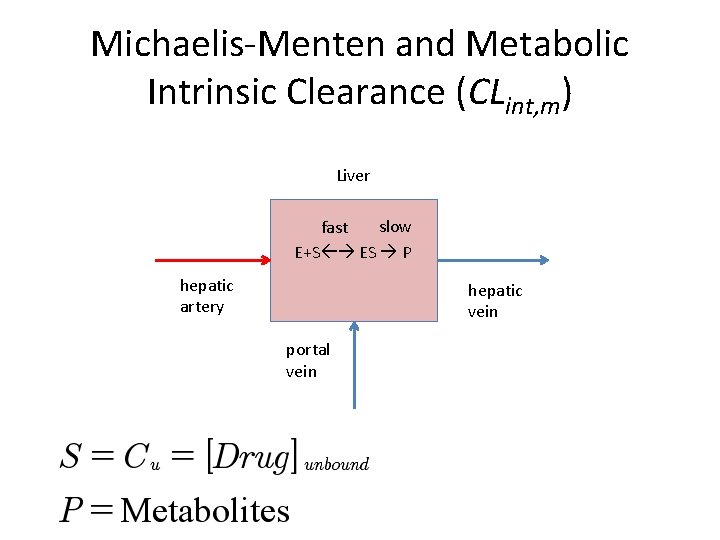
Michaelis-Menten and Metabolic Intrinsic Clearance (CLint, m) Liver slow fast E+S ES P hepatic artery hepatic vein portal vein
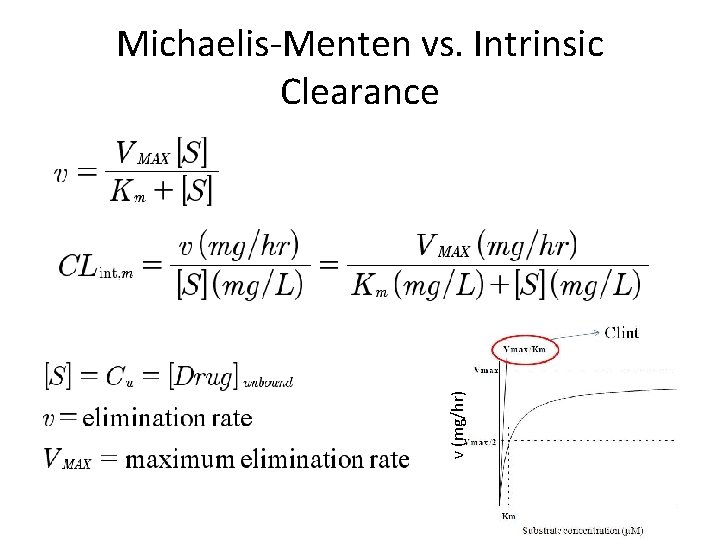
v (mg/hr) Michaelis-Menten vs. Intrinsic Clearance
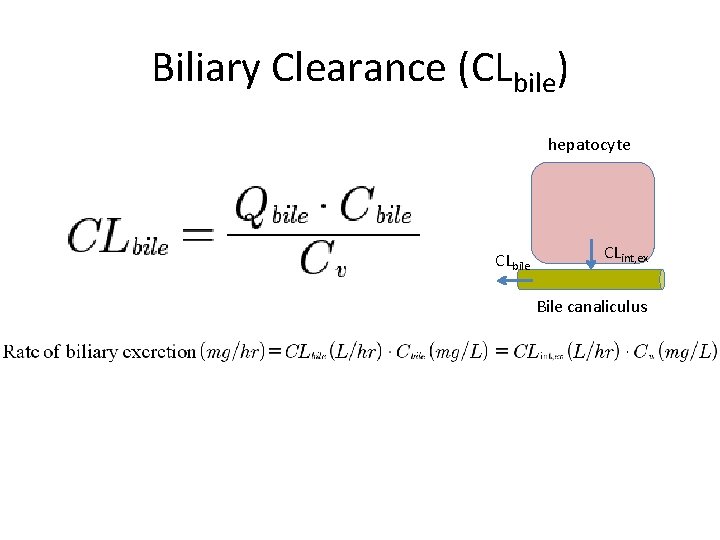
Biliary Clearance (CLbile) hepatocyte CLbile CLint, ex Bile canaliculus
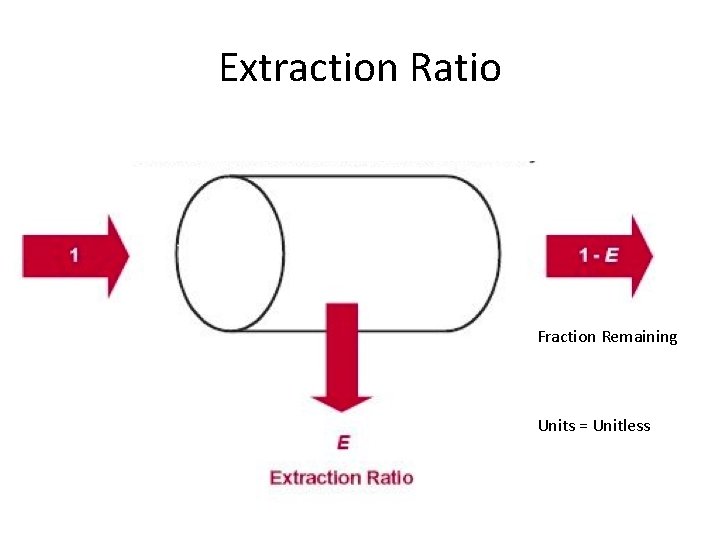
Extraction Ratio Fraction Remaining Units = Unitless
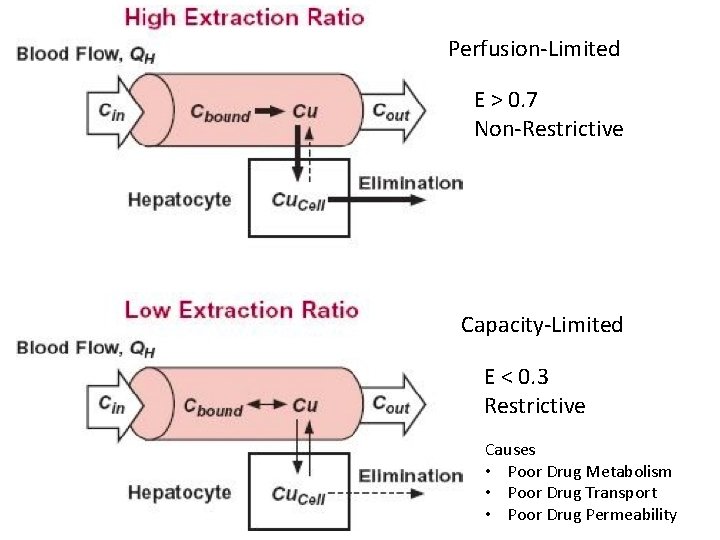
Perfusion-Limited E > 0. 7 Non-Restrictive Capacity-Limited E < 0. 3 Restrictive Causes • Poor Drug Metabolism • Poor Drug Transport • Poor Drug Permeability
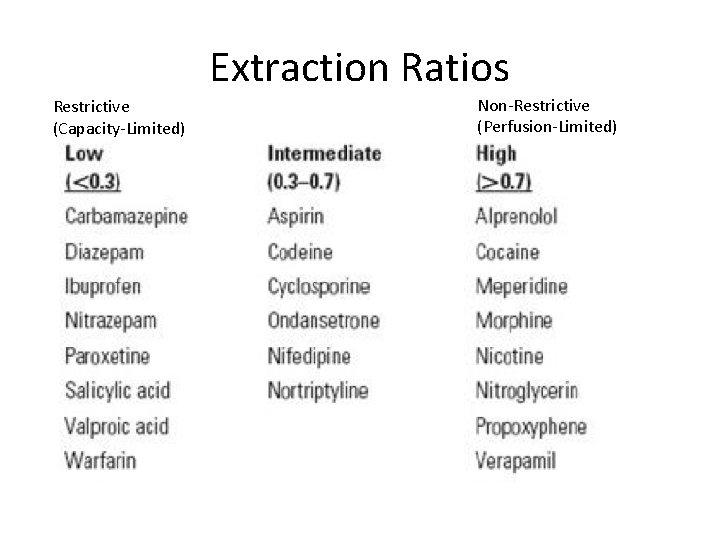
Extraction Ratios Restrictive (Capacity-Limited) Non-Restrictive (Perfusion-Limited)
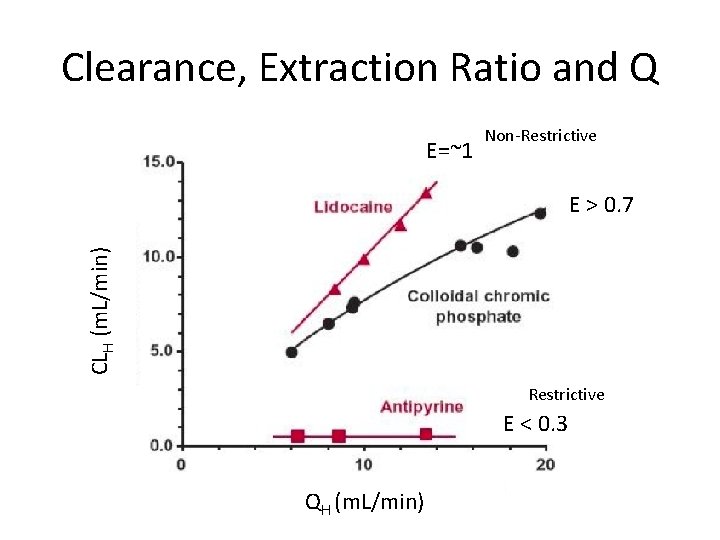
Clearance, Extraction Ratio and Q E=~1 Non-Restrictive CLH (m. L/min) E > 0. 7 Restrictive E < 0. 3 QH (m. L/min)
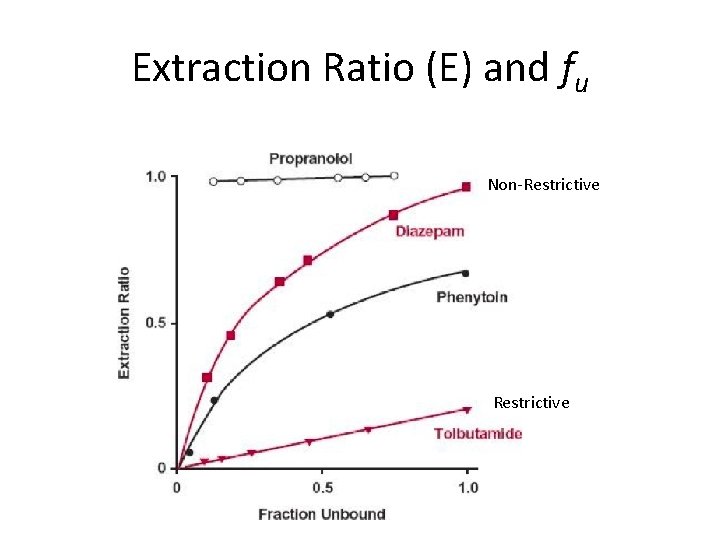
Extraction Ratio (E) and fu Non-Restrictive
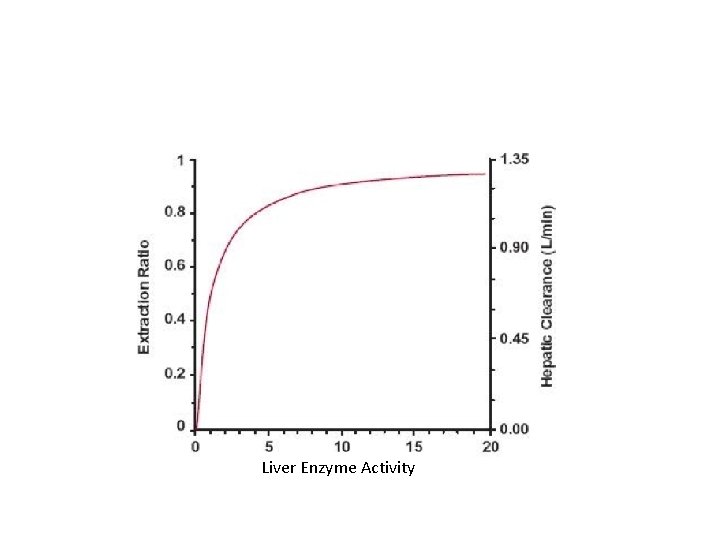
Liver Enzyme Activity
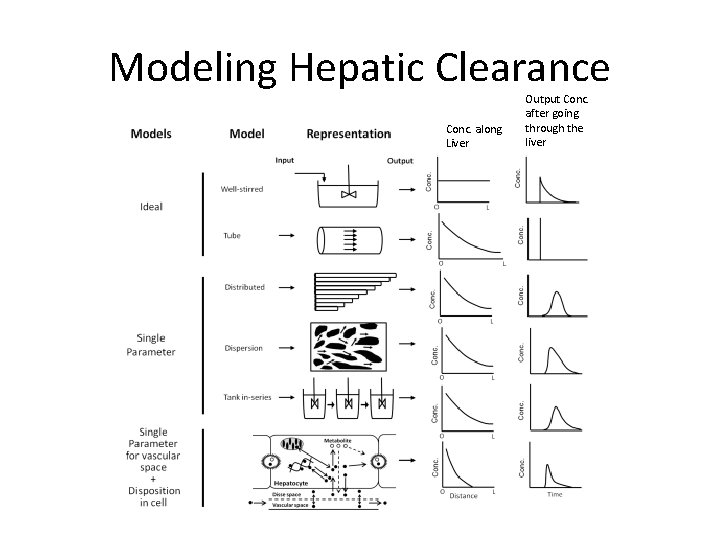
Modeling Hepatic Clearance Conc. along Liver Output Conc. after going through the liver
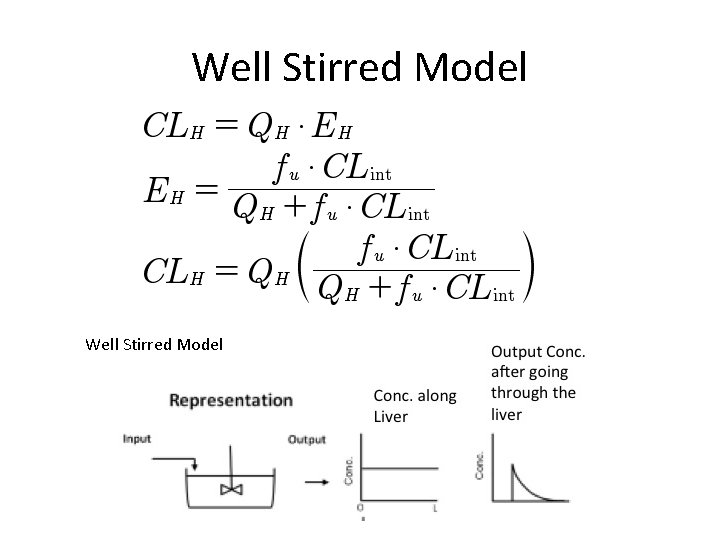
Well Stirred Model
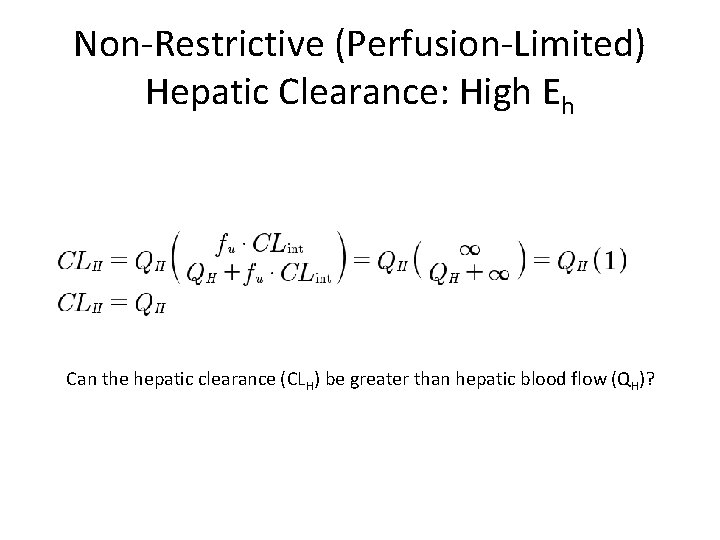
Non-Restrictive (Perfusion-Limited) Hepatic Clearance: High Eh Can the hepatic clearance (CLH) be greater than hepatic blood flow (QH)?
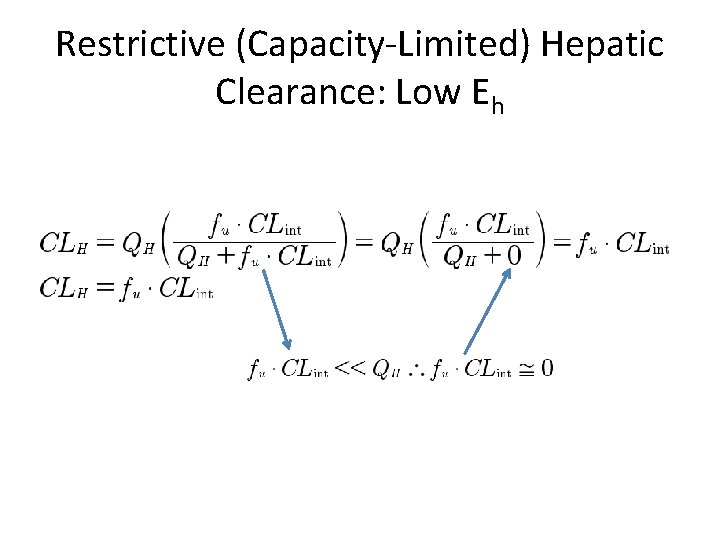
Restrictive (Capacity-Limited) Hepatic Clearance: Low Eh
Complexities • Permeability • Location/Distribution of Transporters • Enterohepatic (Cycle) Circulation
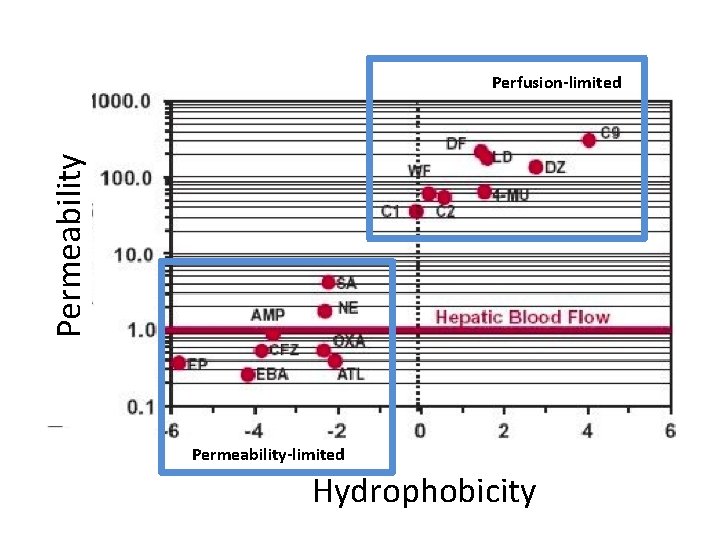
Permeability Perfusion-limited Permeability-limited Hydrophobicity
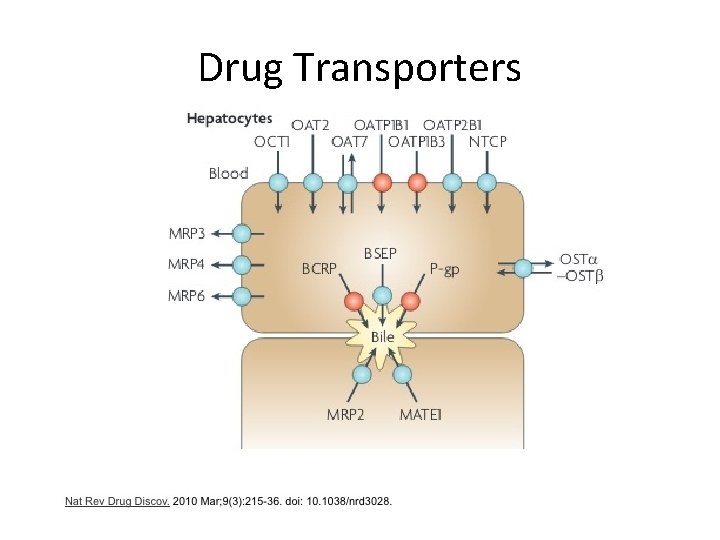
Drug Transporters
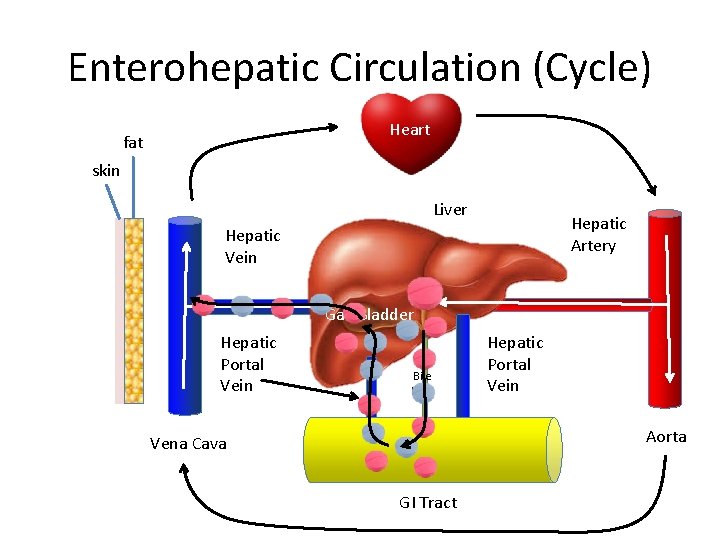
Enterohepatic Circulation (Cycle) Heart fat skin Liver Hepatic Artery Hepatic Vein Gall Bladder Hepatic Portal Vein Bile Duct Hepatic Portal Vein Aorta Vena Cava GI Tract
- Slides: 30