Learning Plan 10 Ch 22 Respiratory System Marieb
Learning Plan 10 Ch 22 Respiratory System: Marieb (College Text, 8 th Ed. ): 804 -824, 830 -832, 834, 837, 840 -843 Ch. 13—Respiratory System: Marieb (High School Text, 8 th Ed. ): 425 -452 Michael Aprill Lakeshore Technical College Copyright © 2010 Pearson Education, Inc.
Respiration • Involves both the respiratory and the circulatory systems • Failure of either system has the same effect. • Four processes that supply the body with O 2 and dispose of CO 2 Copyright © 2010 Pearson Education, Inc.
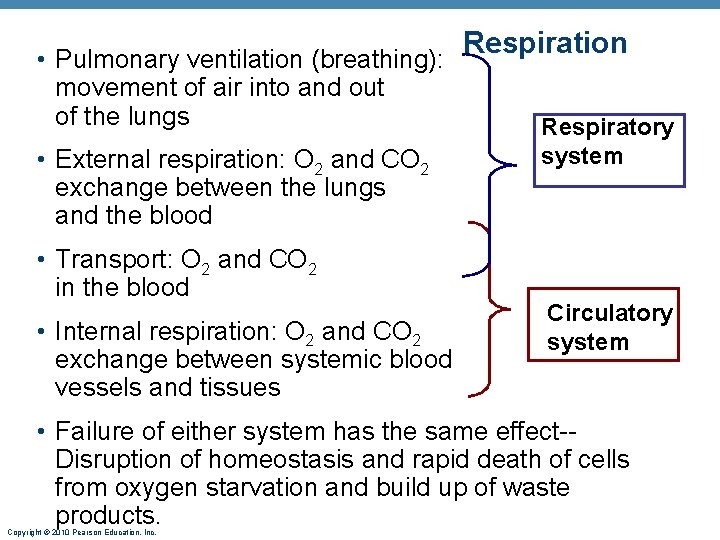
Respiration • Pulmonary ventilation (breathing): movement of air into and out of the lungs • External respiration: O 2 and CO 2 exchange between the lungs and the blood • Transport: O 2 and CO 2 in the blood • Internal respiration: O 2 and CO 2 exchange between systemic blood vessels and tissues Respiratory system Circulatory system • Failure of either system has the same effect-Disruption of homeostasis and rapid death of cells from oxygen starvation and build up of waste products. Copyright © 2010 Pearson Education, Inc.
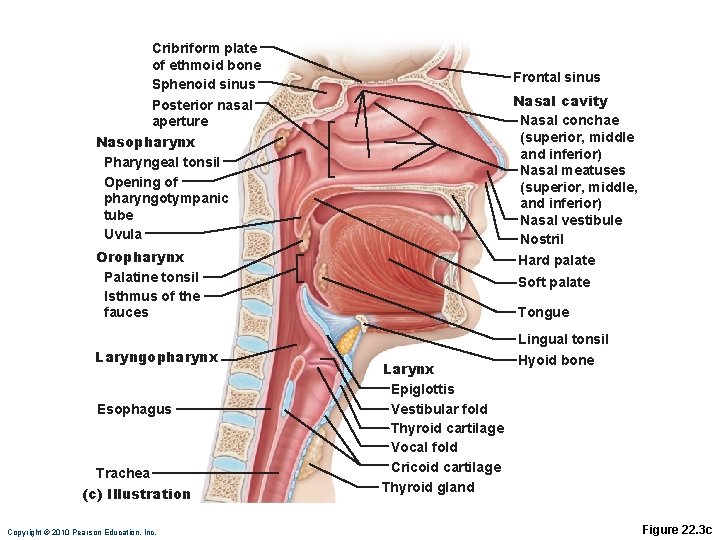
Respiratory System: Functional Anatomy • Major organs • Nose, nasal cavity, and paranasal sinuses • Pharynx (throat) • Larynx (voice box) • Trachea (wind pipe) • Bronchi and their branches (airway) • Lungs and alveoli • Locations of infections: • Upper Respiratory Tract: above the vocal cords • Lower Respiratory Tract: below the vocal cords Copyright © 2010 Pearson Education, Inc.
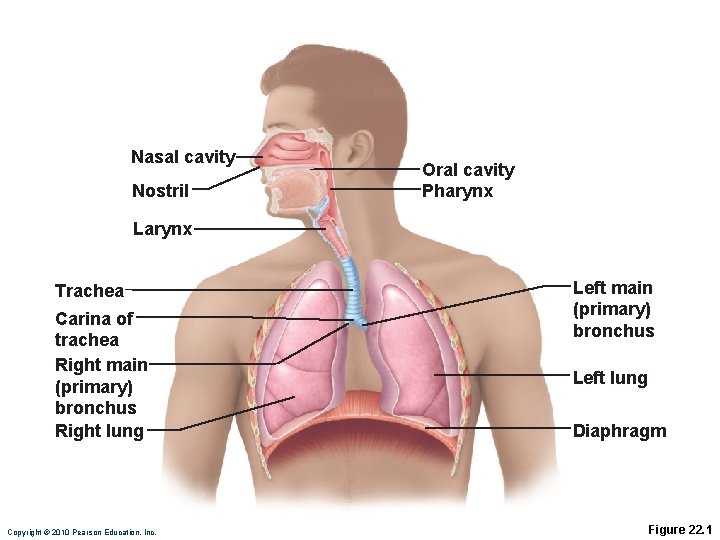
Nasal cavity Nostril Oral cavity Pharynx Larynx Trachea Carina of trachea Right main (primary) bronchus Right lung Copyright © 2010 Pearson Education, Inc. Left main (primary) bronchus Left lung Diaphragm Figure 22. 1
Functional Anatomy • Respiratory zone: site of gas exchange • Microscopic structures: respiratory bronchioles, alveolar ducts, and alveoli • Conducting zone: conduits to gas exchange sites • Includes all other respiratory structures • Respiratory muscles: diaphragm and other muscles that promote ventilation Copyright © 2010 Pearson Education, Inc.
The Nose • Functions • Provides an airway for respiration • Moistens and warms the entering air • Filters and cleans inspired air • Serves as a resonating chamber for speech • Houses olfactory receptors Copyright © 2010 Pearson Education, Inc.
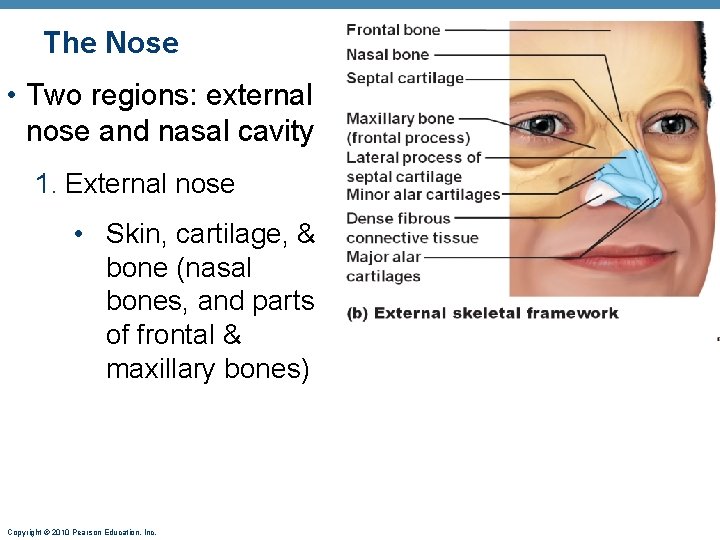
The Nose • Two regions: external nose and nasal cavity 1. External nose • Skin, cartilage, & bone (nasal bones, and parts of frontal & maxillary bones) Copyright © 2010 Pearson Education, Inc.
The Nose 2. Nasal cavity: in and posterior to the external nose • Nostrils (external nares): entrance to the nose • Divided by a midline nasal septum • Posterior nasal apertures (choanae) open into the nasal pharynx (internal nares) Copyright © 2010 Pearson Education, Inc.
Nasal Cavity • Vestibule: nasal cavity superior to the nostrils • Vibrissae filter coarse particles from inspired air • Olfactory mucosa • Lines the superior nasal cavity • Contains smell receptors Copyright © 2010 Pearson Education, Inc.
Cribriform plate of ethmoid bone Sphenoid sinus Posterior nasal aperture Nasopharynx Pharyngeal tonsil Opening of pharyngotympanic tube Uvula Frontal sinus Nasal cavity Nasal conchae (superior, middle and inferior) Nasal meatuses (superior, middle, and inferior) Nasal vestibule Nostril Oropharynx Palatine tonsil Isthmus of the fauces Laryngopharynx Esophagus Trachea (c) Illustration Copyright © 2010 Pearson Education, Inc. Hard palate Soft palate Tongue Lingual tonsil Larynx Epiglottis Vestibular fold Thyroid cartilage Vocal fold Cricoid cartilage Thyroid gland Hyoid bone Figure 22. 3 c
Functions of the Nasal Mucosa and Conchae • During inhalation, the conchae and nasal mucosa • Filter, heat, and moisten air • During exhalation these structures • Reclaim heat and moisture Copyright © 2010 Pearson Education, Inc.
Paranasal Sinuses • In frontal, sphenoid, ethmoid, and maxillary bones • Lighten the skull and help to warm and moisten the air • Communicates with the internal portion of the nose. Copyright © 2010 Pearson Education, Inc.
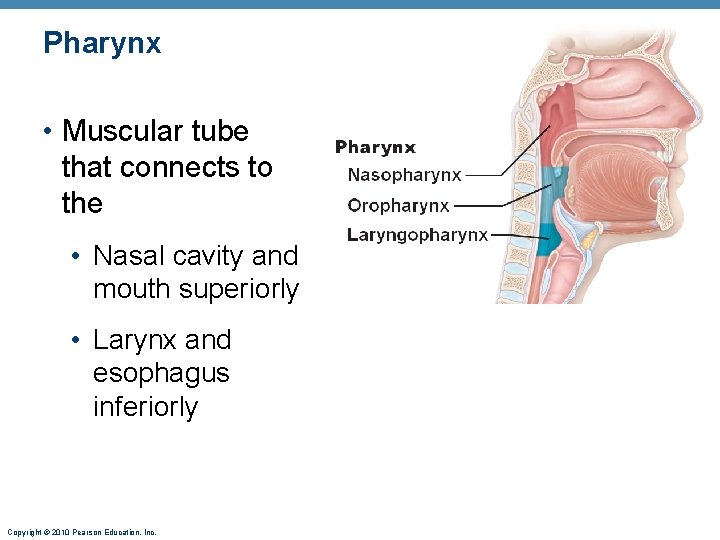
Pharynx • Muscular tube that connects to the • Nasal cavity and mouth superiorly • Larynx and esophagus inferiorly Copyright © 2010 Pearson Education, Inc.
Nasopharynx • Air passageway posterior to the nasal cavity • Soft palate and uvula close nasopharynx during swallowing Copyright © 2010 Pearson Education, Inc.
Oropharynx • Passageway for food and air from the level of the soft palate to the epiglottis • Fauces: opening to the oral cavity Copyright © 2010 Pearson Education, Inc.
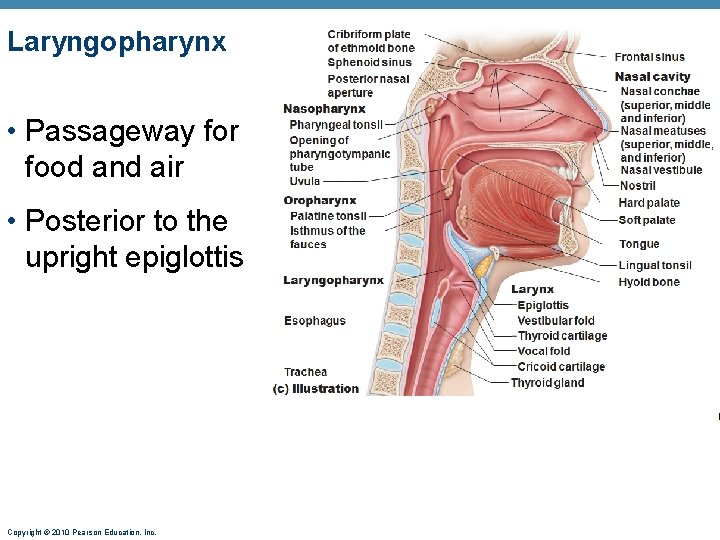
Laryngopharynx • Passageway for food and air • Posterior to the upright epiglottis Copyright © 2010 Pearson Education, Inc.
Larynx • Attaches to the hyoid bone and opens into the laryngopharynx • Functions 1. Provides a patent airway 2. Routes air and food into proper channels 3. Voice production Copyright © 2010 Pearson Education, Inc.
Larynx • Cartilages of the larynx • Hyaline cartilage: • Thyroid cartilage with laryngeal prominence (Adam’s apple) • Ring-shaped cricoid cartilage • Paired arytenoid, cuneiform, and corniculate cartilages • Epiglottis: elastic cartilage; covers the laryngeal inlet during swallowing Copyright © 2010 Pearson Education, Inc.
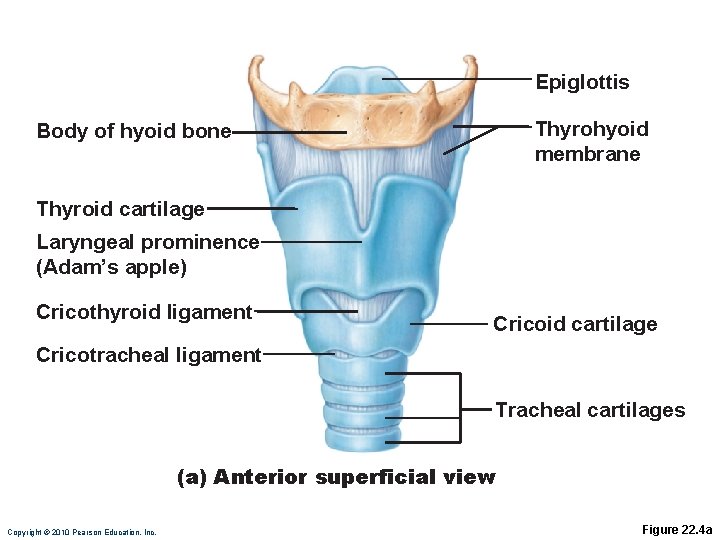
Epiglottis Thyrohyoid membrane Body of hyoid bone Thyroid cartilage Laryngeal prominence (Adam’s apple) Cricothyroid ligament Cricoid cartilage Cricotracheal ligament Tracheal cartilages (a) Anterior superficial view Copyright © 2010 Pearson Education, Inc. Figure 22. 4 a
Larynx • Vocal ligaments • Form core of vocal folds (true vocal cords) • Opening between them is the glottis • Folds vibrate to produce sound as air rushes up from the lungs • Vestibular folds (false vocal cords) • Superior to the vocal folds • No part in sound production • Help to close the glottis during swallowing Copyright © 2010 Pearson Education, Inc.
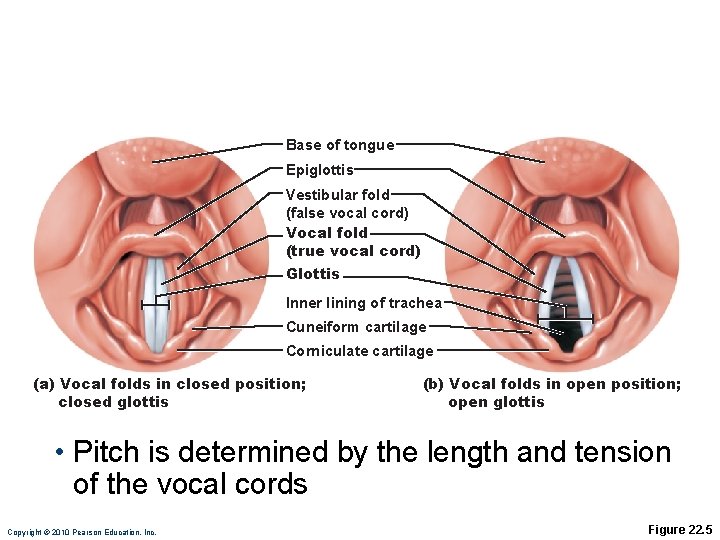
Base of tongue Epiglottis Vestibular fold (false vocal cord) Vocal fold (true vocal cord) Glottis Inner lining of trachea Cuneiform cartilage Corniculate cartilage (a) Vocal folds in closed position; closed glottis (b) Vocal folds in open position; open glottis • Pitch is determined by the length and tension of the vocal cords Copyright © 2010 Pearson Education, Inc. Figure 22. 5
Laryngitis • Inflammation of the larynx that is usually caused by respiratory infection or irritants. Cancer of the larynx is almost exclusively found in smokers. Copyright © 2010 Pearson Education, Inc.
Trachea • Windpipe: from the larynx into the mediastinum • Wall composed of three layers 1. Mucosa: ciliated pseudostratified epithelium with goblet cells (sweep debris up) 2. Submucosa: connective tissue with seromucous glands 3. Adventitia: C-shaped rings of hyaline cartilage Copyright © 2010 Pearson Education, Inc.
Tracheostomy and Intubation • Reestablishing airflow past an airway obstruction • crushing injury to larynx or chest • swelling that closes airway • vomit or foreign object • Tracheostomy is incision in trachea below cricoid cartilage if larynx is obstructed • Intubation is passing a tube from mouth or nose through larynx and trachea Copyright © 2010 Pearson Education, Inc.
Bronchi and Subdivisions • Air passages undergo 23 orders of branching • Branching pattern called the bronchial (respiratory) tree Copyright © 2010 Pearson Education, Inc.
Conducting Zone Structures • Trachea right and left main (primary) bronchi • Each main bronchus branches into lobar (secondary) bronchi (three right, two left) • Each lobar bronchus supplies one lobe (supplying the lung) • Each lobar bronchus branches into segmental (tertiary) bronchi—divide repeatedly • Terminal bronchioles are the smallest in diameter. Copyright © 2010 Pearson Education, Inc.
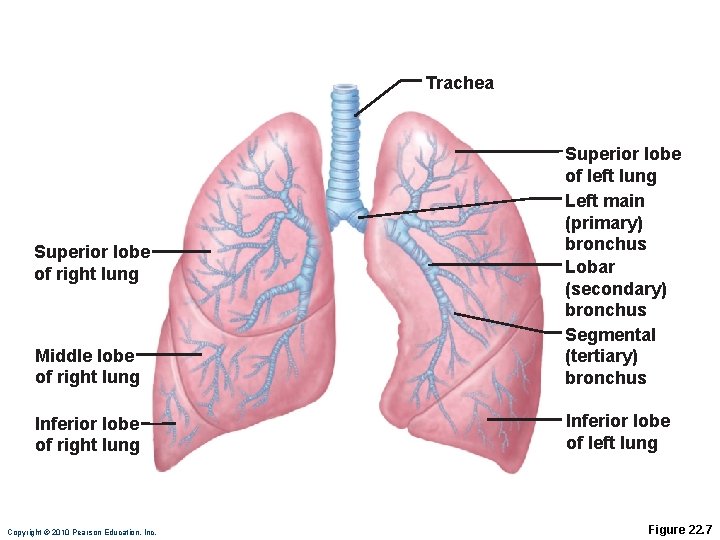
Trachea Middle lobe of right lung Superior lobe of left lung Left main (primary) bronchus Lobar (secondary) bronchus Segmental (tertiary) bronchus Inferior lobe of right lung Inferior lobe of left lung Superior lobe of right lung Copyright © 2010 Pearson Education, Inc. Figure 22. 7
Conducting Zone Structures • From bronchi through bronchioles, structural changes occur • Trachea & bronchi contain cartilage rings give way to plates; cartilage is absent from bronchioles • Gradually changes over to smooth muscle-wall of bronchioles contain smooth muscle. Copyright © 2010 Pearson Education, Inc.
Respiratory Zone • Respiratory bronchioles, alveolar ducts, alveolar sacs (clusters of alveoli) • ~300 million alveoli account for most of the lungs’ volume and are the main site for gas exchange Copyright © 2010 Pearson Education, Inc.
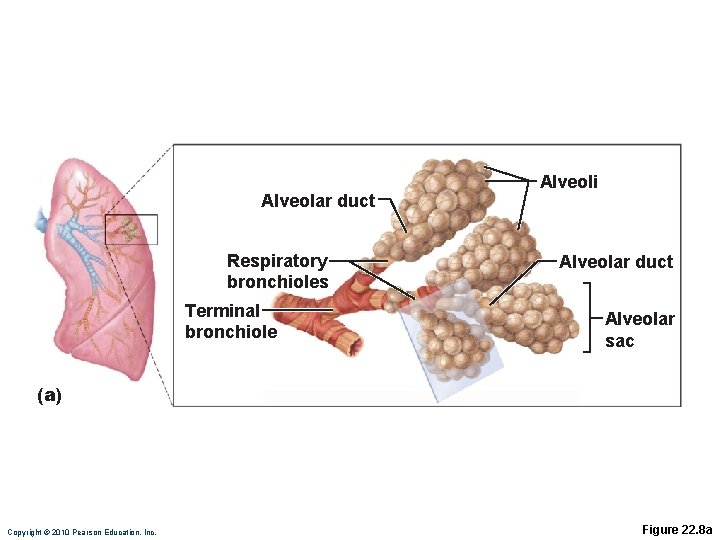
Alveolar duct Respiratory bronchioles Terminal bronchiole Alveoli Alveolar duct Alveolar sac (a) Copyright © 2010 Pearson Education, Inc. Figure 22. 8 a
Respiratory Membrane • Alveolar walls • Single layer of squamous epithelium (type I cells) • Scattered type II cuboidal cells secrete surfactant and antimicrobial proteins Copyright © 2010 Pearson Education, Inc.
Alveolar Surface Tension • Surfactant • Detergent-like lipid and protein complex produced by type II alveolar cells • Reduces surface tension of alveolar fluid and discourages alveolar collapse • Insufficient quantity in premature infants causes infant respiratory distress syndrome • Nebulization, a procedure for administering medication as small droplets suspended in air into the respiratory tract, is used to treat many different types of respiratory disorders. Copyright © 2010 Pearson Education, Inc.
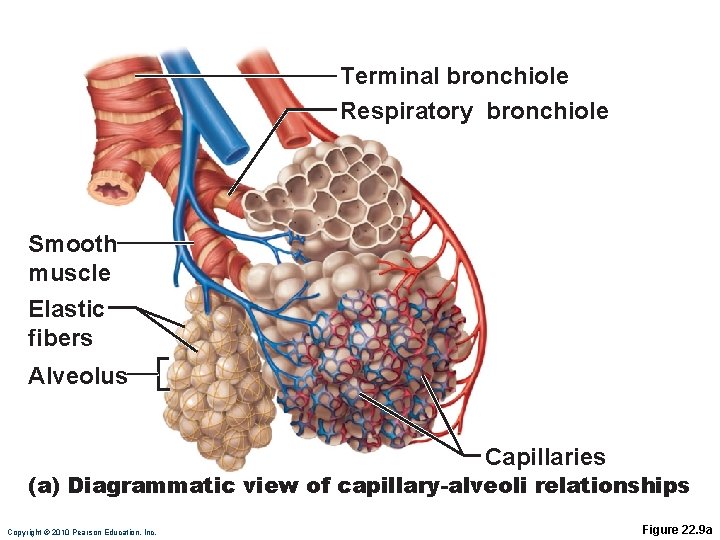
Terminal bronchiole Respiratory bronchiole Smooth muscle Elastic fibers Alveolus Capillaries (a) Diagrammatic view of capillary-alveoli relationships Copyright © 2010 Pearson Education, Inc. Figure 22. 9 a
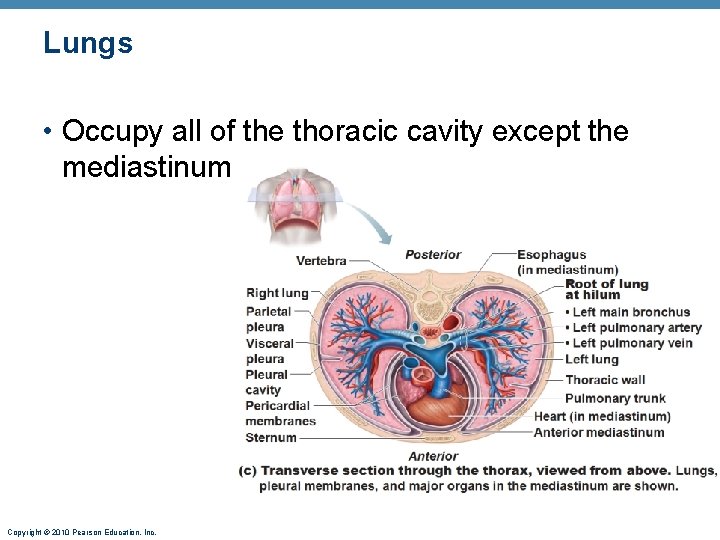
Lungs • Occupy all of the thoracic cavity except the mediastinum Copyright © 2010 Pearson Education, Inc.
Lungs • Left lung is smaller, separated into two lobes. • Right lung has three lobes. • Bronchopulmonary segments (10 right, 8– 9 left) • Broken into compartments called lobules are the smallest subdivisions; served by bronchioles and their branches • Lobules contain lymphatics, arterioles, venules, terminal bronchioles, respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli. Copyright © 2010 Pearson Education, Inc.
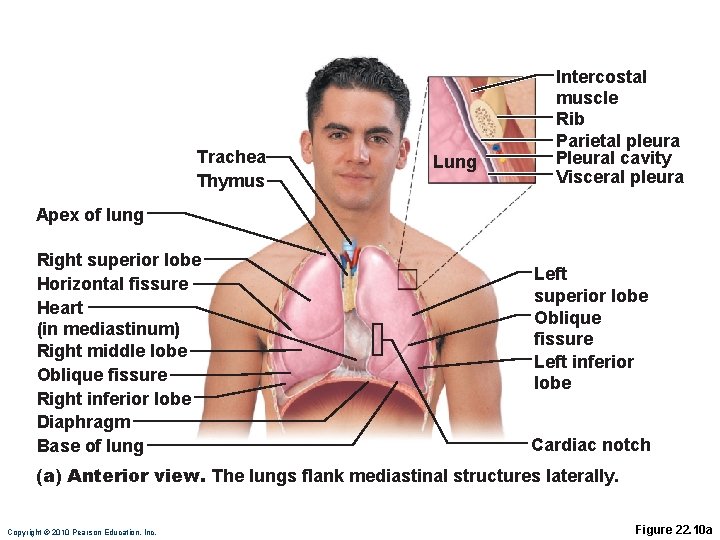
Trachea Thymus Lung Intercostal muscle Rib Parietal pleura Pleural cavity Visceral pleura Apex of lung Right superior lobe Horizontal fissure Heart (in mediastinum) Right middle lobe Oblique fissure Right inferior lobe Diaphragm Base of lung Left superior lobe Oblique fissure Left inferior lobe Cardiac notch (a) Anterior view. The lungs flank mediastinal structures laterally. Copyright © 2010 Pearson Education, Inc. Figure 22. 10 a
Double Blood Supply • Pulmonary circulation • Pulmonary arteries deliver systemic venous blood • Branch profusely, along with bronchi • Feed into the pulmonary capillary networks • Pulmonary veins carry oxygenated blood from respiratory zones to the heart Copyright © 2010 Pearson Education, Inc.
Double Blood Supply • Systemic circulation • Bronchial arteries provide oxygenated blood to lung tissue • Arise from aorta and enter the lungs at the hilum • Supply all lung tissue except the alveoli • Bronchial veins anastomose with pulmonary veins • Pulmonary veins carry most venous blood back to the heart Copyright © 2010 Pearson Education, Inc.
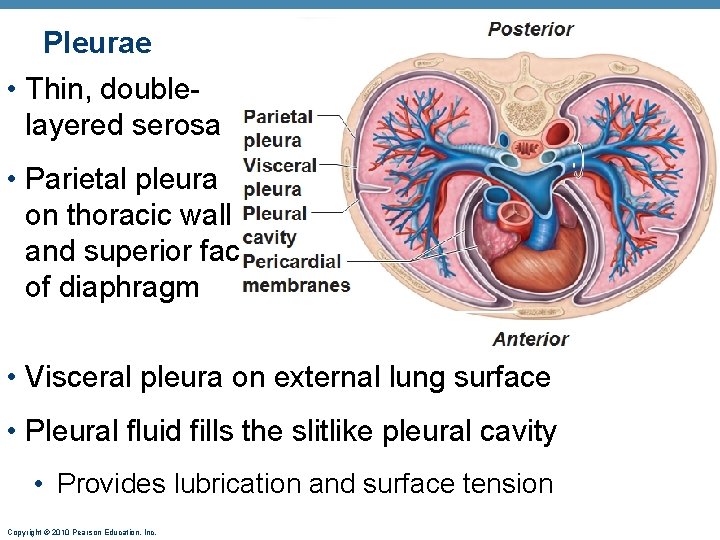
Pleurae • Thin, doublelayered serosa • Parietal pleura on thoracic wall and superior face of diaphragm • Visceral pleura on external lung surface • Pleural fluid fills the slitlike pleural cavity • Provides lubrication and surface tension Copyright © 2010 Pearson Education, Inc.
Homeostatic Imbalance • Atelectasis (lung collapse) is due to • Plugged bronchioles collapse of alveoli • Wound that admits air into pleural cavity (pneumothorax) Copyright © 2010 Pearson Education, Inc.
Pulmonary Ventilation • Inspiration and expiration • Mechanical processes that depend on volume changes in the thoracic cavity • Volume changes pressure changes • Pressure changes gases flow to equalize pressure Copyright © 2010 Pearson Education, Inc.
Inspiration & Expiration • Inspiration: an active process • Inspiratory muscles contract • Thoracic volume increases • Quiet expiration is normally a passive process • Inspiratory muscles relax • Thoracic cavity volume decreases Copyright © 2010 Pearson Education, Inc.
O 2 Transport • Molecular O 2 is carried in the blood • 1. 5% dissolved in plasma • 98. 5% loosely bound to each Fe of hemoglobin (Hb) in RBCs • 4 O 2 per Hb Copyright © 2010 Pearson Education, Inc.
O 2 and Hemoglobin • Loading and unloading of O 2 is facilitated by change in shape of Hb • As O 2 binds, Hb affinity for O 2 increases • As O 2 is released, Hb affinity for O 2 decreases • Fully (100%) saturated if all four heme groups carry O 2 • Partially saturated when one to three hemes carry O 2 Copyright © 2010 Pearson Education, Inc.
O 2 and Hemoglobin • Rate of loading and unloading of O 2 is regulated by • Po 2 • Temperature • Blood p. H • Pco 2 • Medulla Respiratory Centers • The greater the Po 2, the more O 2 will combine with Hb. Copyright © 2010 Pearson Education, Inc.
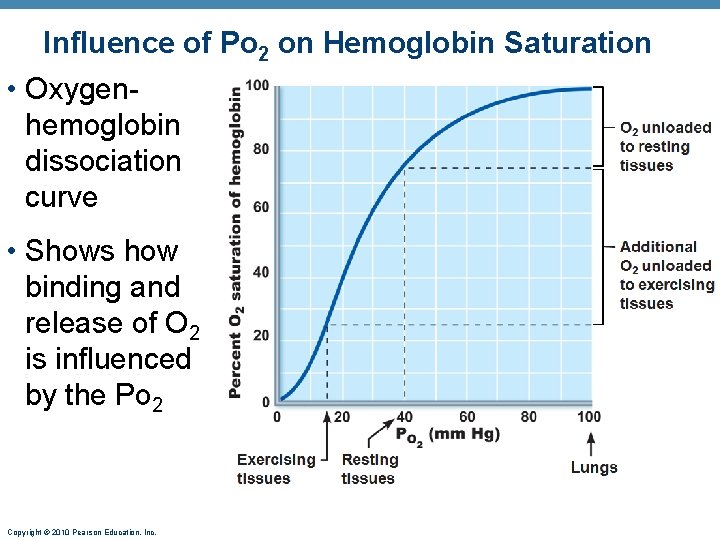
Influence of Po 2 on Hemoglobin Saturation • Oxygenhemoglobin dissociation curve • Shows how binding and release of O 2 is influenced by the Po 2 Copyright © 2010 Pearson Education, Inc.
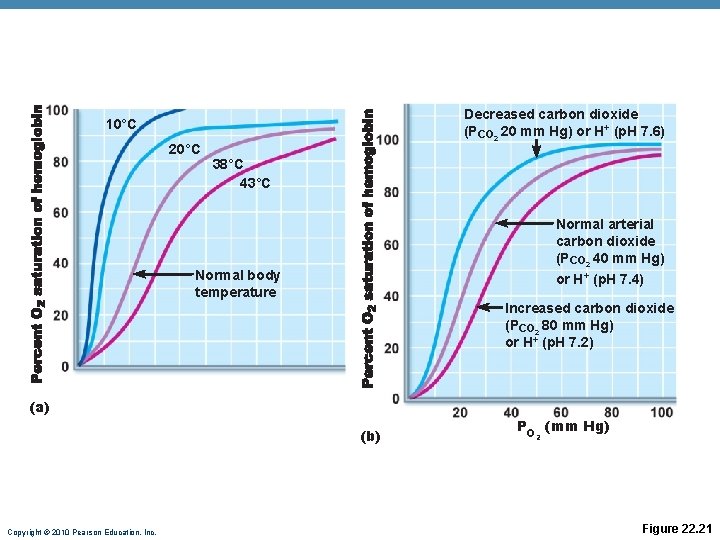
Decreased carbon dioxide (PCO 2 20 mm Hg) or H+ (p. H 7. 6) 10°C 20°C 38°C 43°C Normal arterial carbon dioxide (PCO 2 40 mm Hg) or H+ (p. H 7. 4) Normal body temperature Increased carbon dioxide (PCO 2 80 mm Hg) or H+ (p. H 7. 2) (a) (b) Copyright © 2010 Pearson Education, Inc. PO (mm Hg) 2 Figure 22. 21
CO 2 Transport • CO 2 is transported in the blood in three forms • 7 to 10% dissolved in plasma • 20% bound to globin of hemoglobin (carbaminohemoglobin) • 70% transported as bicarbonate ions (HCO 3–) in plasma Copyright © 2010 Pearson Education, Inc.
Transport and Exchange of CO 2 • CO 2 combines with water to form carbonic acid (H 2 CO 3), which quickly dissociates: CO 2 + Carbon dioxide Copyright © 2010 Pearson Education, Inc. H 2 O Water H 2 CO 3 Carbonic acid H+ Hydrogen ion + HCO 3– Bicarbonate ion
Haldane Effect • At the tissues, as more carbon dioxide enters the blood • More oxygen dissociates from hemoglobin (Bohr effect) • As Hb. O 2 releases O 2, it more readily forms bonds with CO 2 to form carbaminohemoglobin Copyright © 2010 Pearson Education, Inc.
Medullary Respiratory Centers • Sets eupnea (12– 15 breaths/minute) Copyright © 2010 Pearson Education, Inc.
Depth and Rate of Breathing • Hyperventilation: increased depth and rate of breathing that exceeds the body’s need to remove CO 2 • Apnea: period of breathing cessation that occurs when Pco 2 is abnormally low Copyright © 2010 Pearson Education, Inc.
Homeostatic Imbalance • Hypoxia • Inadequate O 2 delivery to tissues • Due to a variety of causes • Too few RBCs • Abnormal or too little Hb • Blocked circulation • Metabolic poisons • Pulmonary disease • Carbon monoxide Copyright © 2010 Pearson Education, Inc.
Homeostatic Imbalances • Chronic obstructive pulmonary disease (COPD) • Exemplified by chronic bronchitis and emphysema • Irreversible decrease in the ability to force air out of the lungs • Asthma • Characterized by coughing, dyspnea, wheezing, and chest tightness • Active inflammation of the airways precedes bronchospasms Copyright © 2010 Pearson Education, Inc.
Homeostatic Imbalances • Tuberculosis • Infectious disease caused by the bacterium Mycobacterium tuberculosis • Symptoms include fever, night sweats, weight loss, a racking cough, and spitting up blood • Treatment entails a 12 -month course of antibiotics Copyright © 2010 Pearson Education, Inc.
Homeostatic Imbalances • Lung cancer • Leading cause of cancer deaths in North America • 90% of all cases are the result of smoking • Pneumonia is an acute infection of the alveoli. The most common cause is the pneumococcal bacteria but other microbes may be involved. Treatment involves antibiotics, bronchodilators, oxygen therapy, and chest physiotherapy. • Coryza (common cold) is caused by viruses and usually is not accompanied by a fever, whereas influenza (flu) is usually accompanied by a fever greater than 101 o. F. Copyright © 2010 Pearson Education, Inc.
DISORDERS: HOMEOSTATIC IMBALANCES • Pulmonary edema refers to an abnormal accumulation of interstitial fluid in the interstitial spaces and alveoli of the lungs. It may be pulmonary or cardiac in origin. • Cystic fibrosis is an inherited disease of secretory epithelia that affects the respiratory passageways, pancreas, salivary glands, and sweat glands. • Asbestos related diseases develop as a result of inhaling asbestos particles. Diseases such as asbestosis, diffuse pleural thickening, and mesothelioma may result. • Sudden infant death syndrome (SIDS) is the sudden unexpected death of an apparently healthy infant. Peak incidence is ages two to four months. The exact cause is unknown. • Severe acute respiratory syndrome (SARS) is an emerging infectious disease. Copyright © 2010 Pearson Education, Inc.
- Slides: 58