LEARNING FROM DISASTERS Focus on Nephrology Experience on


- Slides: 105
LEARNING FROM DISASTERS (Focus on Nephrology Experience on Crush Syndrome) FILOTEO C. FERRER, MD Section of Nephrology Makati Medical Center March 24, 2011
Outline • Lessons from past disasters (Objectives) – Be aware – Understand – Prepare
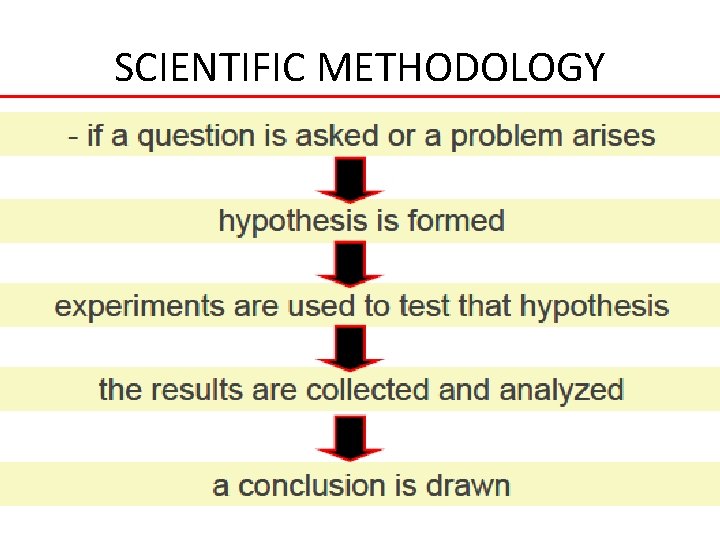
SCIENTIFIC METHODOLOGY
NO EXPERIMENTAL MODEL OF DISASTERS • Only way to collect information and draw conclusions is by: – Retrospective analysis of past disasters – And have a good understanding of these lessons
NO EXPERIMENTAL MODEL OF DISASTERS • Lessons learned from these unfortunate experiences can contribute – Minimize number of mistakes – Implement an effective response – Decrease death toll in future catastrophes
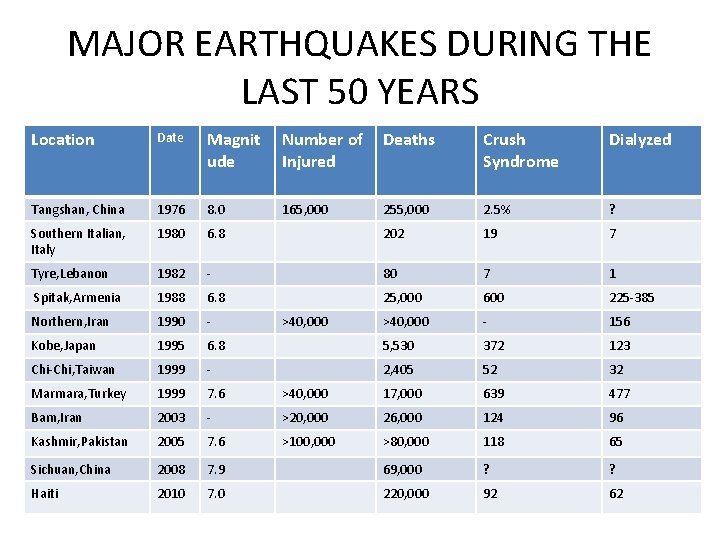
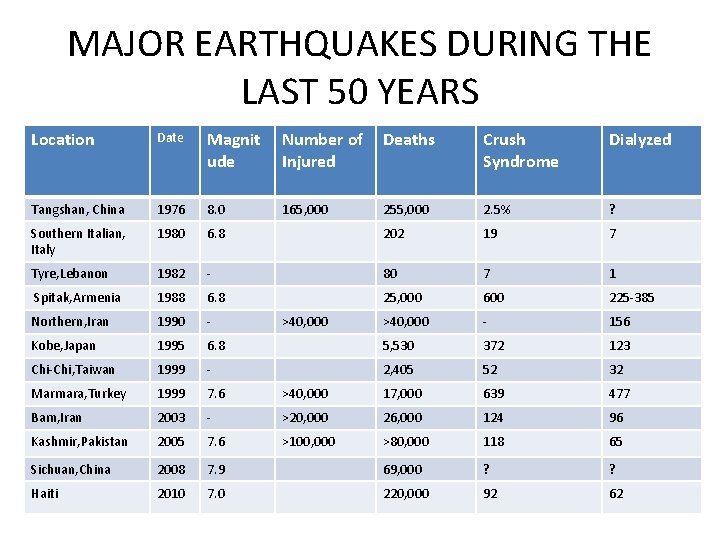
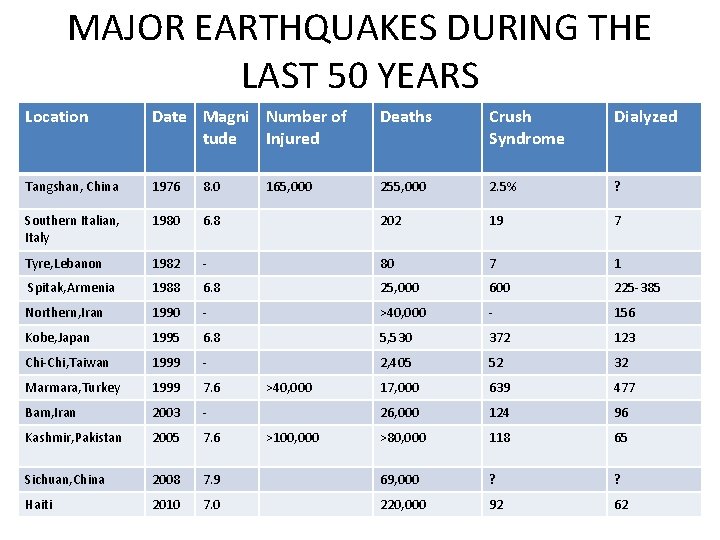
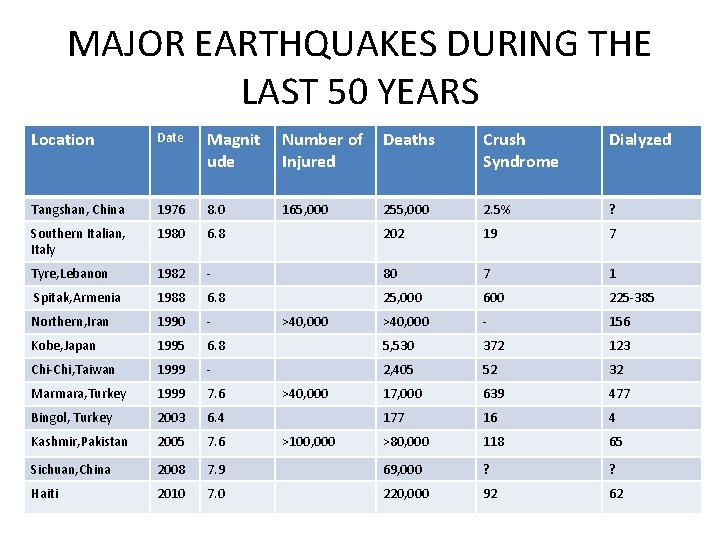
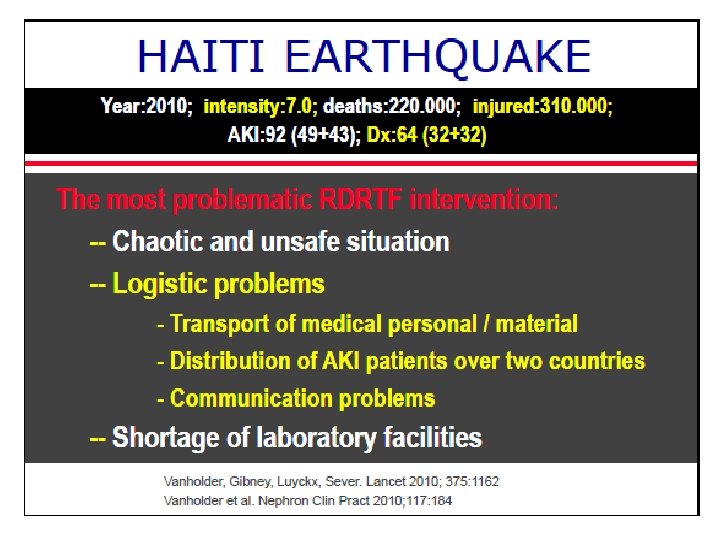
MAJOR EARTHQUAKES DURING THE LAST 50 YEARS Location Date Magnit ude Number of Deaths Injured Crush Syndrome Dialyzed Tangshan, China 1976 8. 0 165, 000 255, 000 2. 5% ? Southern Italian, Italy 1980 6. 8 202 19 7 Tyre, Lebanon 1982 - 80 7 1 Spitak, Armenia 1988 6. 8 25, 000 600 225 -385 Northern, Iran 1990 - >40, 000 - 156 Kobe, Japan 1995 6. 8 5, 530 372 123 Chi-Chi, Taiwan 1999 - 2, 405 52 32 Marmara, Turkey 1999 7. 6 >40, 000 17, 000 639 477 Bam, Iran 2003 - >20, 000 26, 000 124 96 Kashmir, Pakistan 2005 7. 6 >100, 000 >80, 000 118 65 Sichuan, China 2008 7. 9 69, 000 ? ? Haiti 2010 7. 0 220, 000 92 62 >40, 000
INCIDENCE OF CRUSH INJURY AFTER DISASTRERS • • • Intensity of the disaster Population density of the region Structural characteristics of the buildings Timing of disaster Efficacy of rescue
• Crush injury is defined as a direct injury caused by collapsing material and debris resulting in manifest muscle swelling and/or neurological disturbances in the affected parts of the body.
• Crush Syndrome on the other hand is defined as patients with crush injury and systemic manifestation due to muscle cell damage which would include: – – – – – acute kidney injury Sepsis acute respiratory distress syndrome diffuse intravascular coaugulation Bleeding hypovolemic shock cardiac failure arrhythmias electrolyte disturbances.
Crush syndrome • Second most frequent cause of disaster related mortality after earthquakes (after direct trauma) • Incidence may increase up to 2 -5% overall in disaster victims • But according to general perception: • they constitute a relatively minor group requiring a complex labor- intensive therapeutic measures and are rarely included in governmental or local disaster plans (emergency teams concentrate on housing and primary health ) Sever M. S. , et al Renal disaster relief: from theory to practice NDT (2009)
Crush Syndrome (CS) • It takes a lot of effort to extricate victims from the rubble • Hence, it would be deplorable and even counter productive if proper therapeutic possibilities would not be prepared and offered Sever M. S. , et al Renal disaster relief; from theory to practice; NDT (2009)
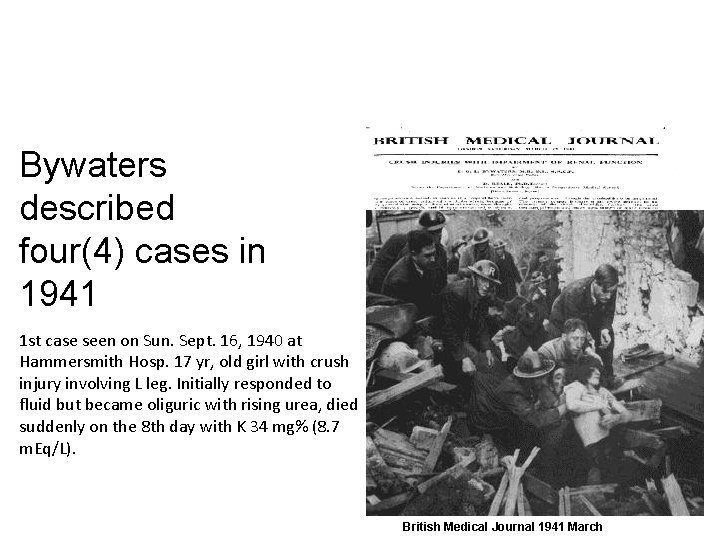
Bywaters described four(4) cases in 1941 1 st case seen on Sun. Sept. 16, 1940 at Hammersmith Hosp. 17 yr, old girl with crush injury involving L leg. Initially responded to fluid but became oliguric with rising urea, died suddenly on the 8 th day with K 34 mg% (8. 7 m. Eq/L). British Medical Journal 1941 March
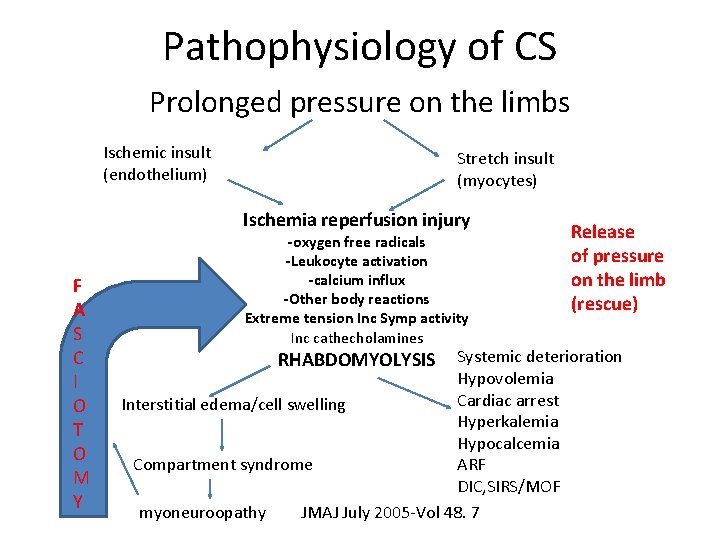
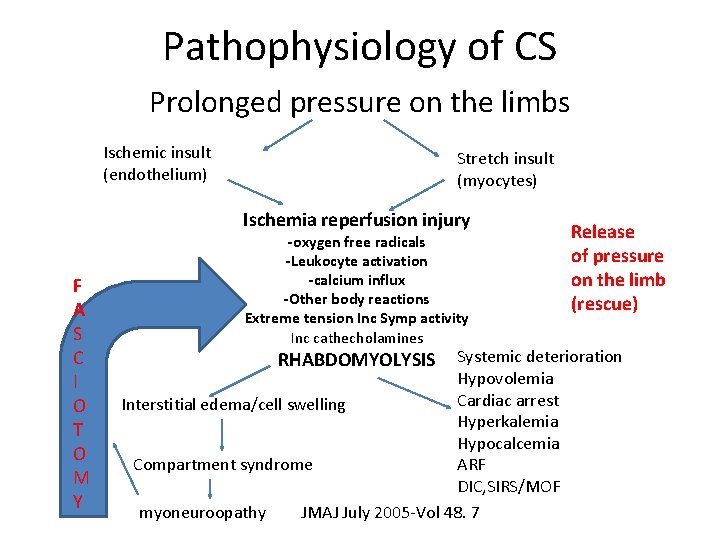
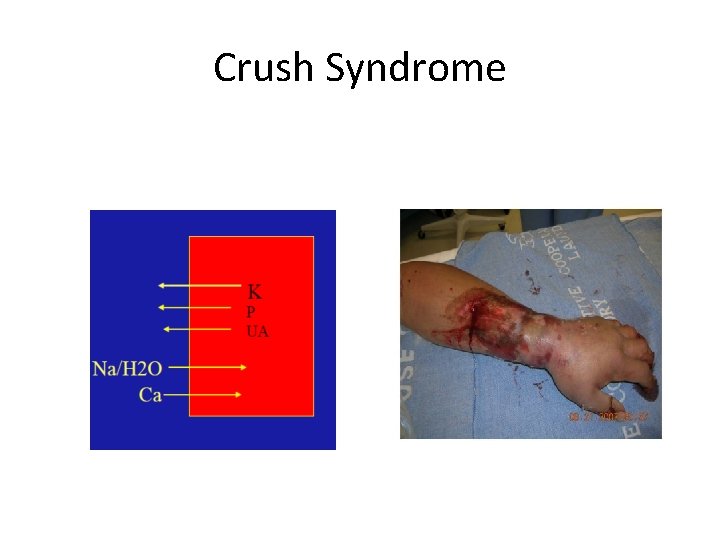
Pathophysiology of CS Prolonged pressure on the limbs Ischemic insult (endothelium) Stretch insult (myocytes) Ischemia reperfusion injury F A S C I O T O M Y -oxygen free radicals -Leukocyte activation -calcium influx -Other body reactions Extreme tension Inc Symp activity Inc cathecholamines Release of pressure on the limb (rescue) Systemic deterioration Hypovolemia Cardiac arrest Interstitial edema/cell swelling Hyperkalemia Hypocalcemia ARF Compartment syndrome DIC, SIRS/MOF myoneuroopathy JMAJ July 2005 -Vol 48. 7 RHABDOMYOLYSIS
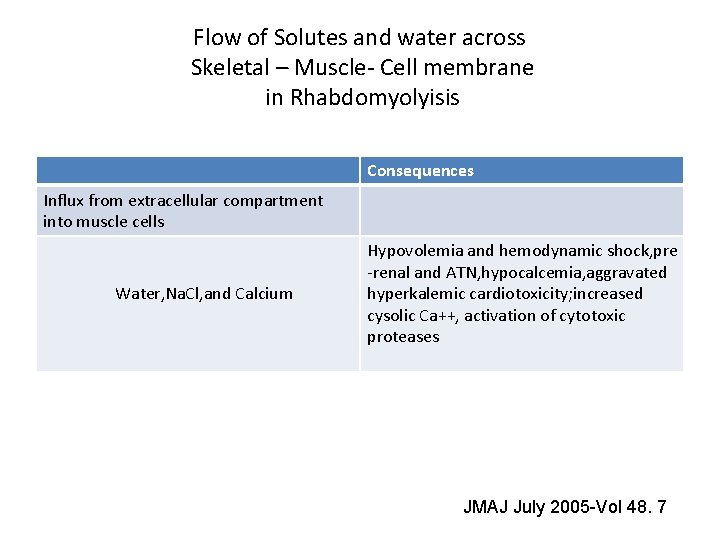
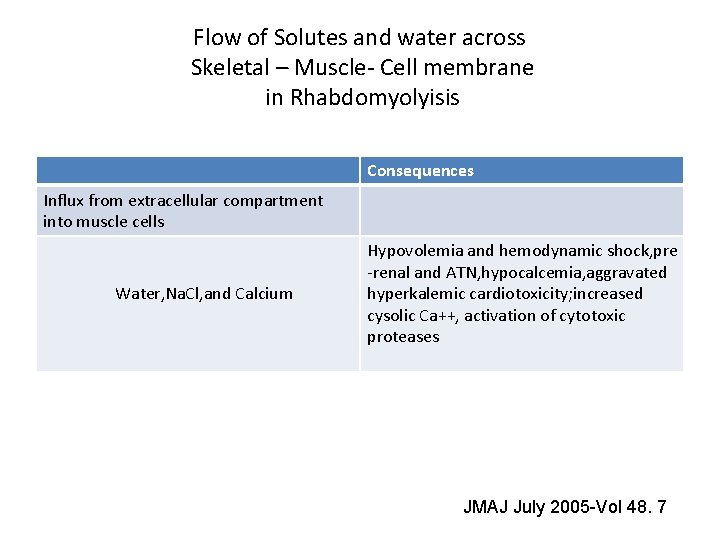
Flow of Solutes and water across Skeletal – Muscle- Cell membrane in Rhabdomyolyisis Consequences Influx from extracellular compartment into muscle cells Water, Na. Cl, and Calcium Hypovolemia and hemodynamic shock, pre -renal and ATN, hypocalcemia, aggravated hyperkalemic cardiotoxicity; increased cysolic Ca++, activation of cytotoxic proteases JMAJ July 2005 -Vol 48. 7
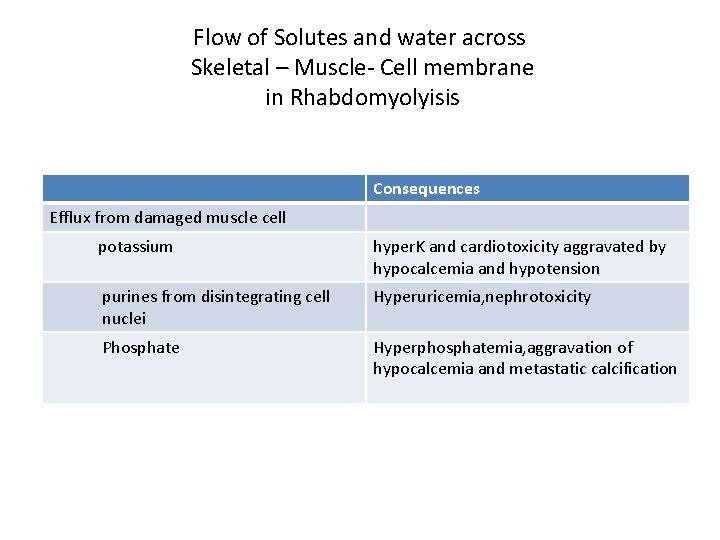
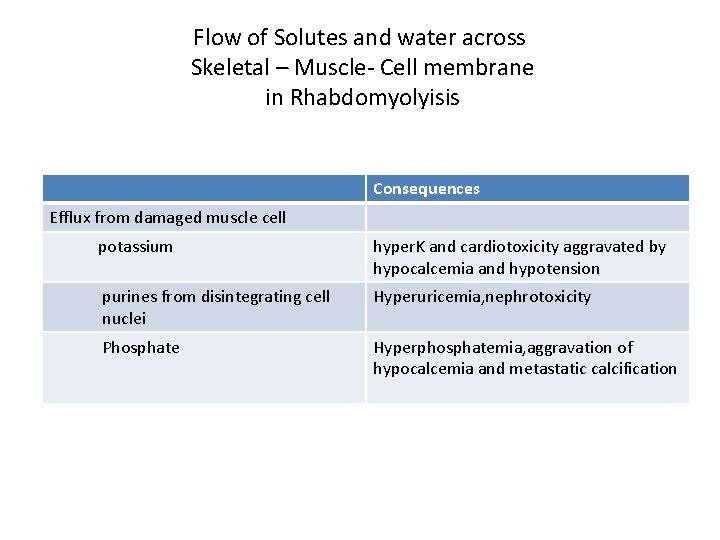
Flow of Solutes and water across Skeletal – Muscle- Cell membrane in Rhabdomyolyisis Consequences Efflux from damaged muscle cell potassium hyper. K and cardiotoxicity aggravated by hypocalcemia and hypotension purines from disintegrating cell Hyperuricemia, nephrotoxicity nuclei Phosphate Hyperphosphatemia, aggravation of hypocalcemia and metastatic calcification
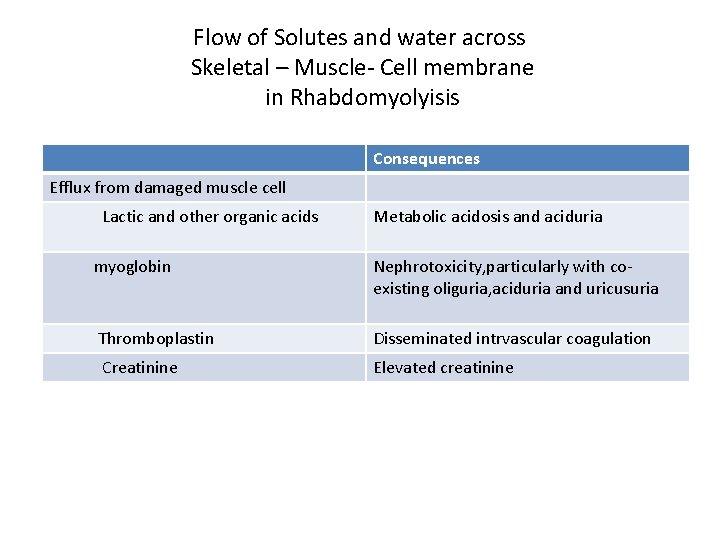
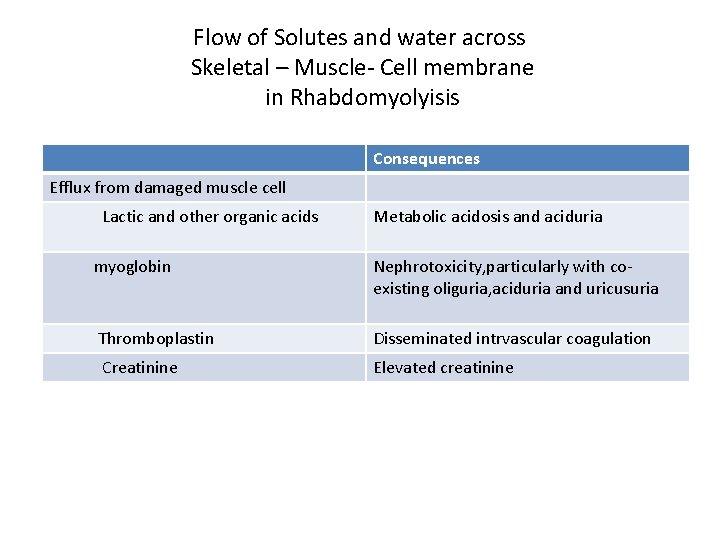
Flow of Solutes and water across Skeletal – Muscle- Cell membrane in Rhabdomyolyisis Consequences Efflux from damaged muscle cell Lactic and other organic acids Metabolic acidosis and aciduria myoglobin Nephrotoxicity, particularly with coexisting oliguria, aciduria and uricusuria Thromboplastin Disseminated intrvascular coagulation Creatinine Elevated creatinine
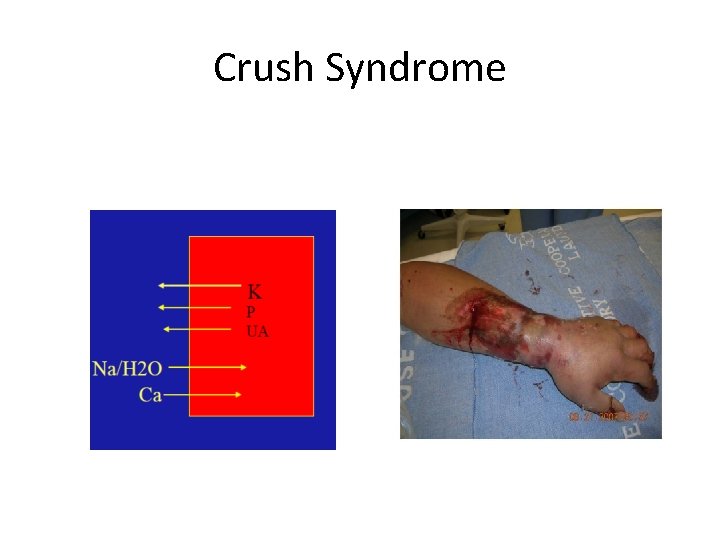
Crush Syndrome
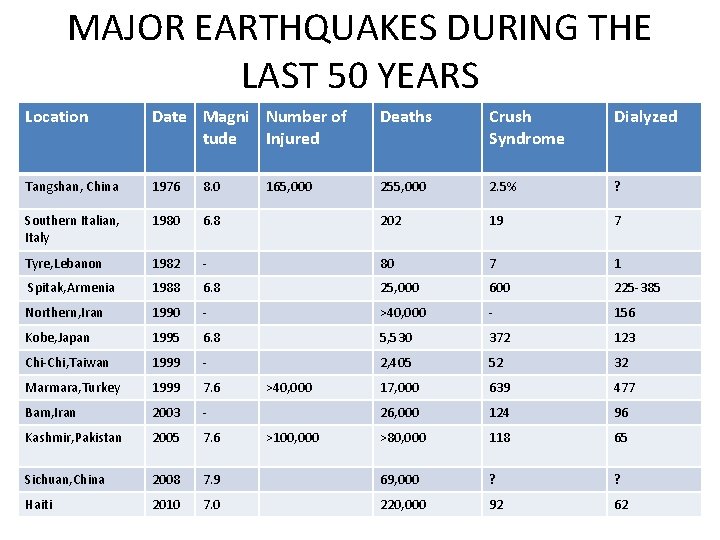
MAJOR EARTHQUAKES DURING THE LAST 50 YEARS Location Date Magni Number of tude Injured Deaths Crush Syndrome Dialyzed Tangshan, China 1976 8. 0 255, 000 2. 5% ? Southern Italian, Italy 1980 6. 8 202 19 7 Tyre, Lebanon 1982 - 80 7 1 Spitak, Armenia 1988 6. 8 25, 000 600 225 -385 Northern, Iran 1990 - >40, 000 - 156 Kobe, Japan 1995 6. 8 5, 530 372 123 Chi-Chi, Taiwan 1999 - 2, 405 52 32 Marmara, Turkey 1999 7. 6 17, 000 639 477 Bam, Iran 2003 - 26, 000 124 96 Kashmir, Pakistan 2005 7. 6 >80, 000 118 65 Sichuan, China 2008 7. 9 69, 000 ? ? Haiti 2010 7. 0 220, 000 92 62 165, 000 >40, 000 >100, 000
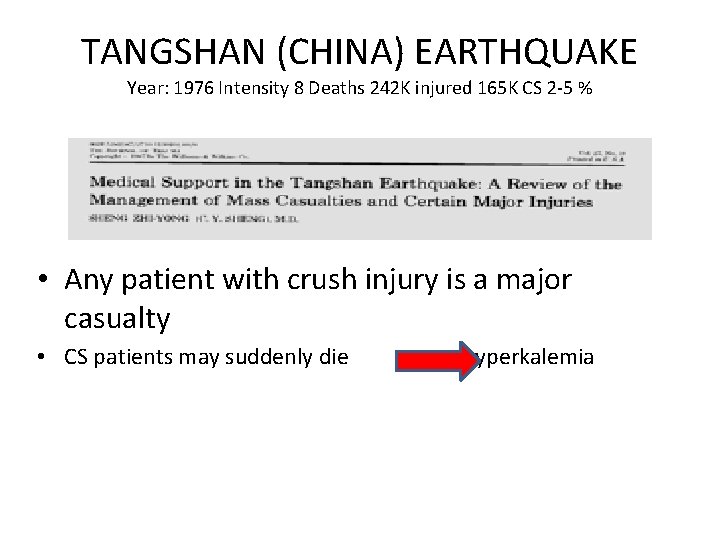
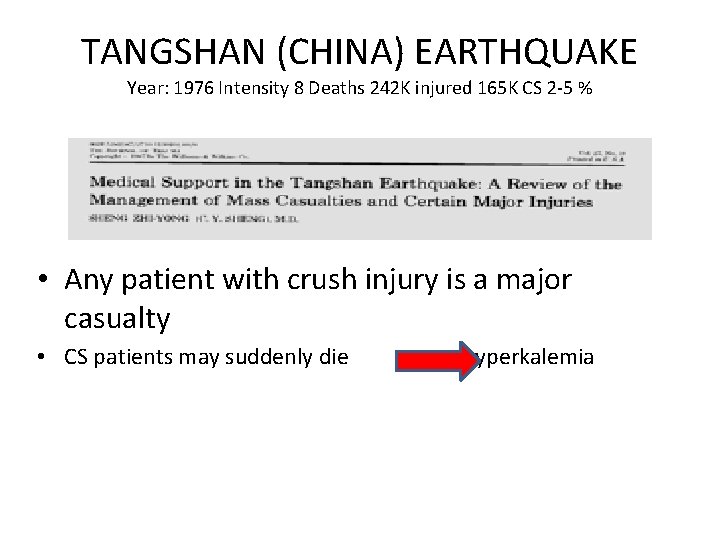
TANGSHAN (CHINA) EARTHQUAKE Year: 1976 Intensity 8 Deaths 242 K injured 165 K CS 2 -5 % • Any patient with crush injury is a major casualty • CS patients may suddenly die hyperkalemia
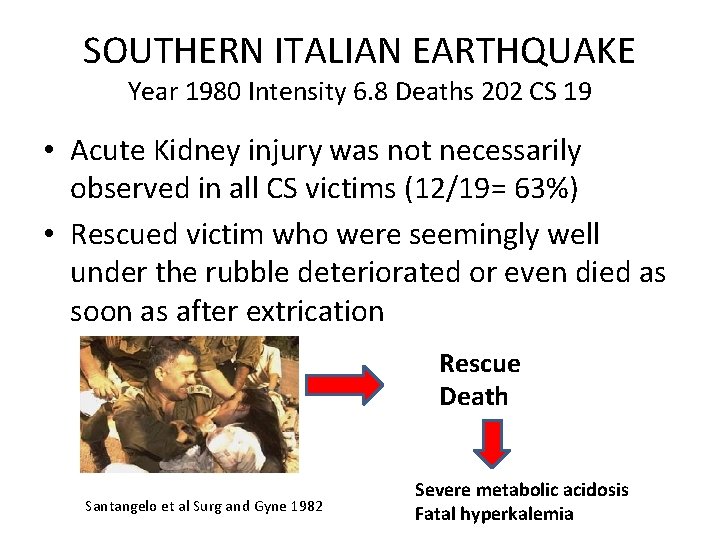
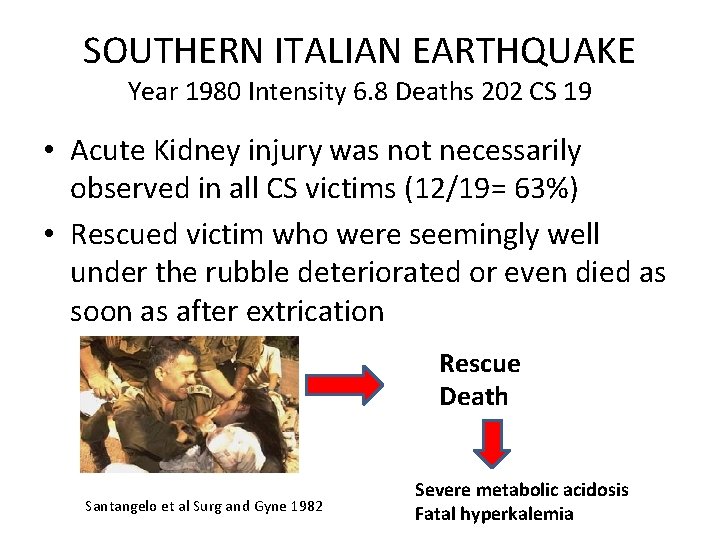
SOUTHERN ITALIAN EARTHQUAKE Year 1980 Intensity 6. 8 Deaths 202 CS 19 • Acute Kidney injury was not necessarily observed in all CS victims (12/19= 63%) • Rescued victim who were seemingly well under the rubble deteriorated or even died as soon as after extrication Rescue Death Santangelo et al Surg and Gyne 1982 Severe metabolic acidosis Fatal hyperkalemia
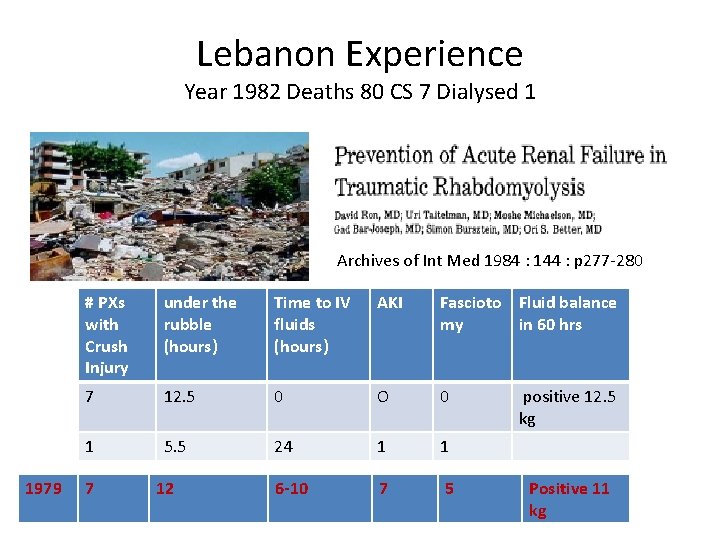
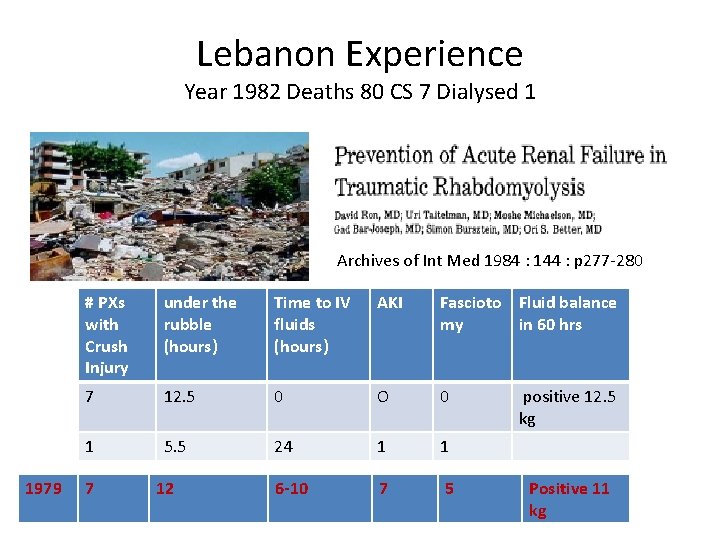
Lebanon Experience Year 1982 Deaths 80 CS 7 Dialysed 1 Archives of Int Med 1984 : 144 : p 277 -280 1979 # PXs with Crush Injury under the rubble (hours) Time to IV fluids (hours) AKI Fascioto Fluid balance my in 60 hrs 7 12. 5 0 O 0 positive 12. 5 kg 1 5. 5 24 1 1 6 -10 7 5 7 12 Positive 11 kg
Lebanon Experience Year 1982 Deaths 80 CS 7 Dialysed 1 • Immediate fluid resuscitation is of vital importance to prevent crush syndrome complications
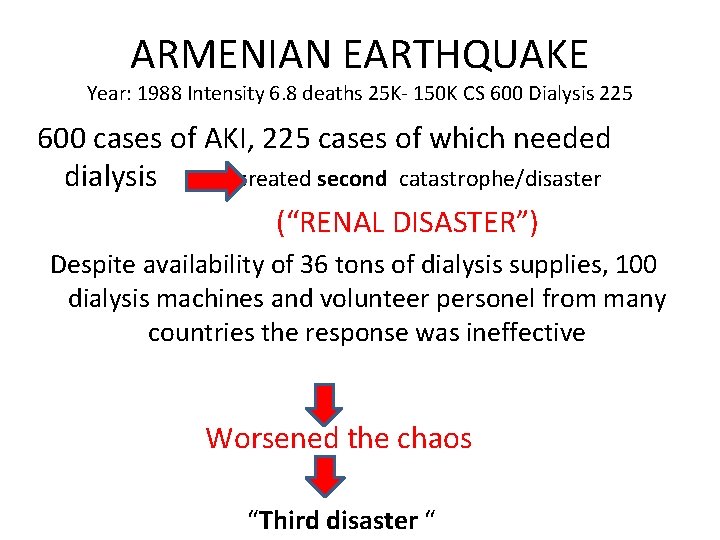
ARMENIAN EARTHQUAKE Year: 1988 Intensity 6. 8 deaths 25 K- 150 K CS 600 Dialysis 225 600 cases of AKI, 225 cases of which needed dialysis created second catastrophe/disaster (“RENAL DISASTER”) Despite availability of 36 tons of dialysis supplies, 100 dialysis machines and volunteer personel from many countries the response was ineffective Worsened the chaos “Third disaster “
ARMENIAN EARTHQUAKE Year: 1988 Intensity 6. 8 deaths 25 K- 150 K CS 600 Dialysis 225 • “Disaster within in a disaster” – No organized international structure with appropriate training and deployment strategies Disappointing experience
• International Society of Nephrology • Logistic organization to avoid similar problems in the future disasters • Headquarters are informed immediately of all disasters • Logistic support from NGOs such as Medicins Sans Frontieres (MSF) • Since the organization, it had intervened in several disasters (Marmara, Bam, Kashmir, Kobe)
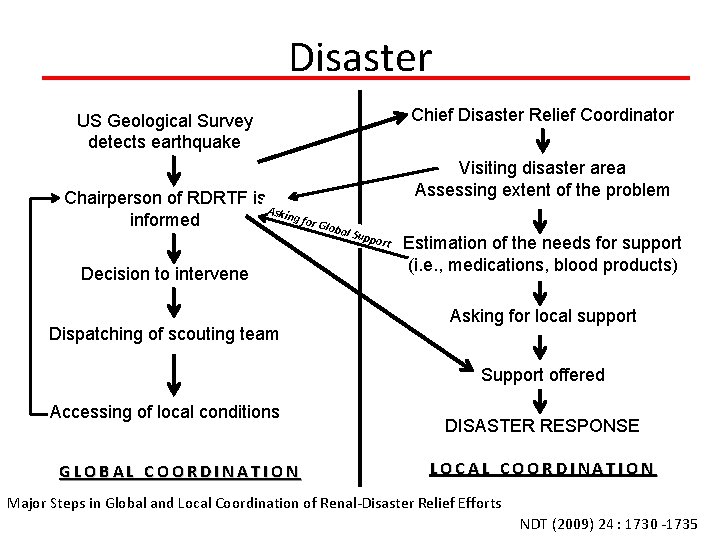
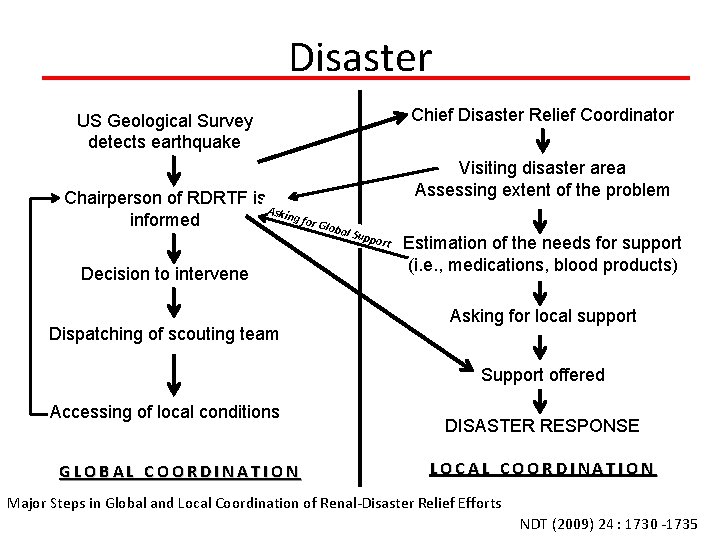
Disaster Chief Disaster Relief Coordinator US Geological Survey detects earthquake Chairperson of RDRTF is Askin g for informed Glob a Decision to intervene Dispatching of scouting team Visiting disaster area Assessing extent of the problem l Sup port Estimation of the needs for support (i. e. , medications, blood products) Asking for local support Support offered Accessing of local conditions GLOBAL COORDINATION DISASTER RESPONSE LOCAL COORDINATION Major Steps in Global and Local Coordination of Renal-Disaster Relief Efforts NDT (2009) 24 : 1730 -1735
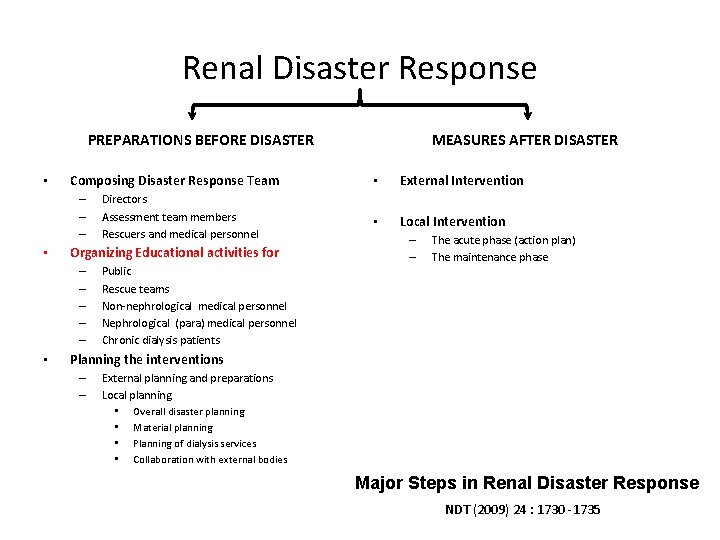
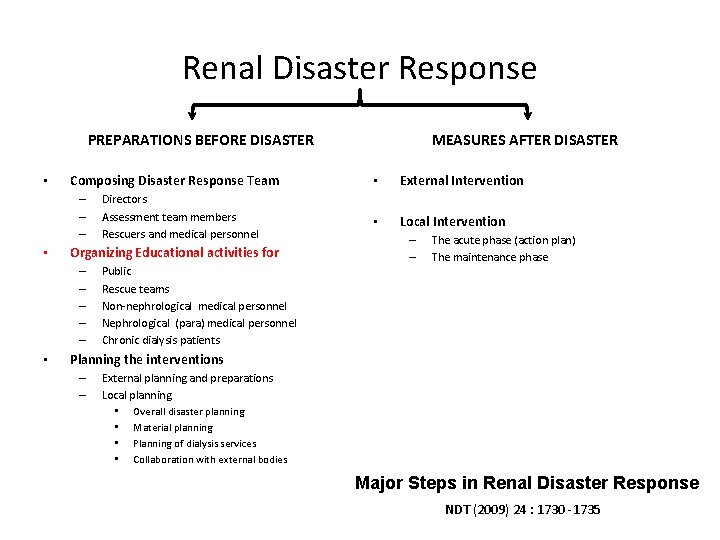
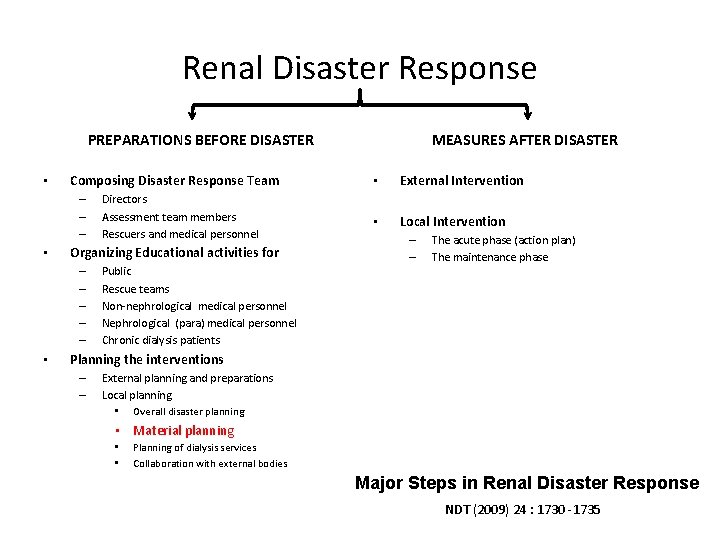
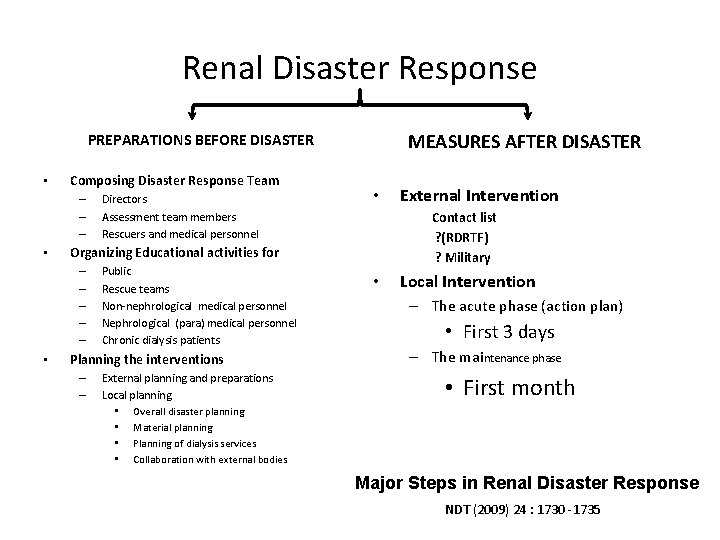
Renal Disaster Response PREPARATIONS BEFORE DISASTER • Composing Disaster Response Team – – – • Organizing Educational activities for – – – • Directors Assessment team members Rescuers and medical personnel Public Rescue teams Non-nephrological medical personnel Nephrological (para) medical personnel Chronic dialysis patients MEASURES AFTER DISASTER • External Intervention • Local Intervention – – The acute phase (action plan) The maintenance phase Planning the interventions – – External planning and preparations Local planning • Overall disaster planning • Material planning • Planning of dialysis services • Collaboration with external bodies Major Steps in Renal Disaster Response NDT (2009) 24 : 1730 -1735
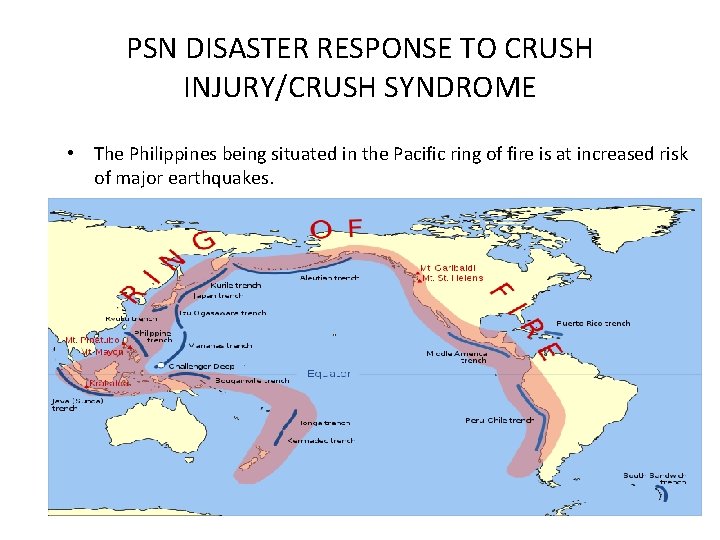
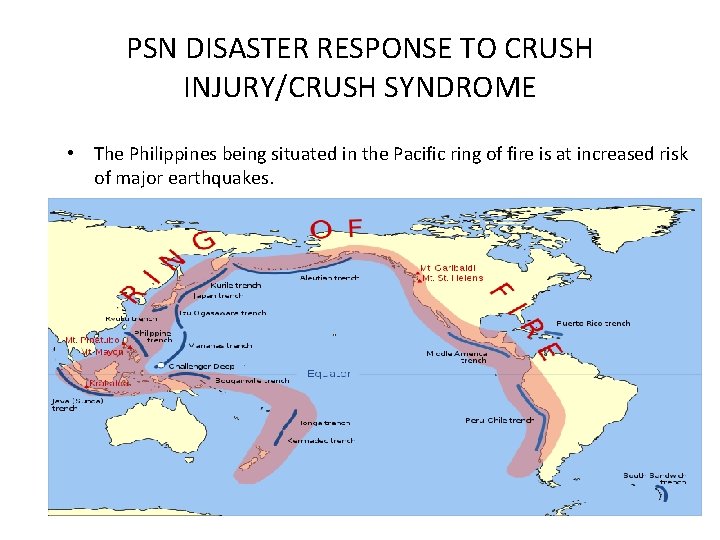
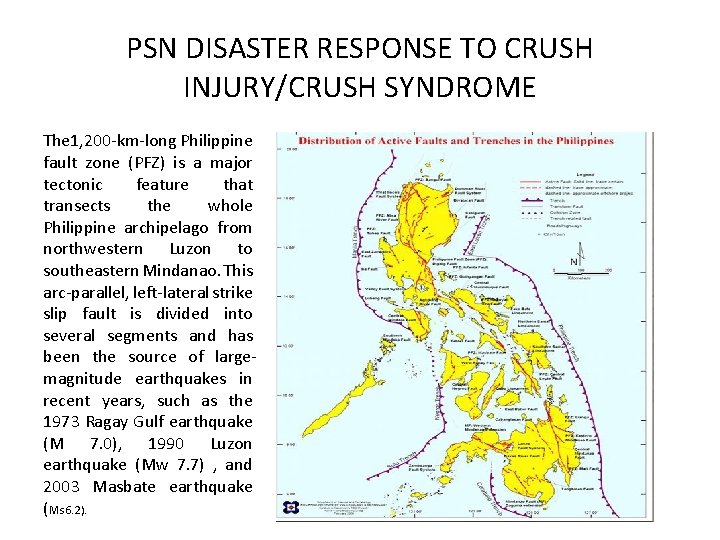
PSN DISASTER RESPONSE TO CRUSH INJURY/CRUSH SYNDROME • The Philippines being situated in the Pacific ring of fire is at increased risk of major earthquakes. • Situated in a geotectonically active region
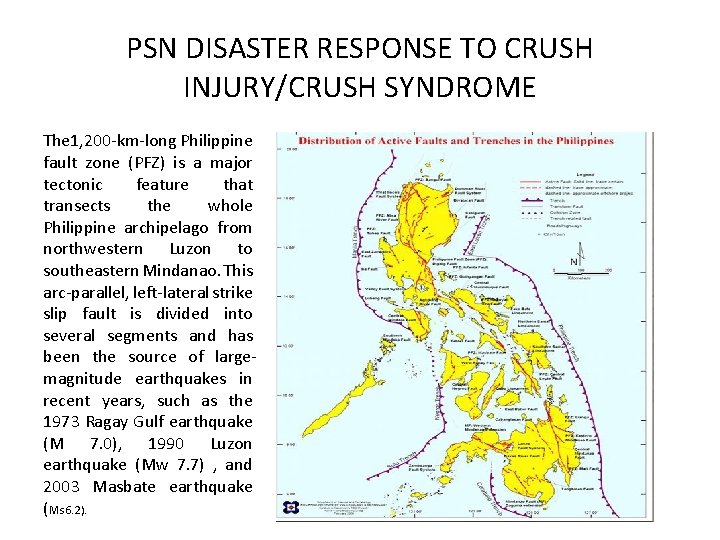
PSN DISASTER RESPONSE TO CRUSH INJURY/CRUSH SYNDROME The 1, 200 -km-long Philippine fault zone (PFZ) is a major tectonic feature that transects the whole Philippine archipelago from northwestern Luzon to southeastern Mindanao. This arc-parallel, left-lateral strike slip fault is divided into several segments and has been the source of largemagnitude earthquakes in recent years, such as the 1973 Ragay Gulf earthquake (M 7. 0), 1990 Luzon earthquake (Mw 7. 7) , and 2003 Masbate earthquake (Ms 6. 2).
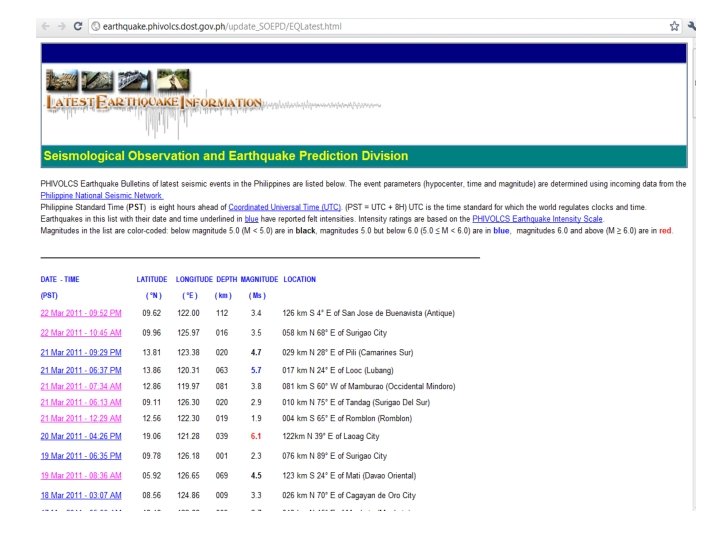
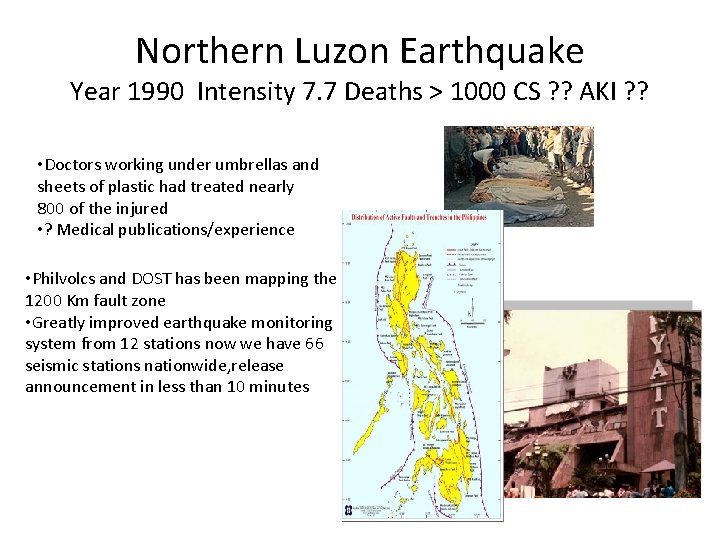
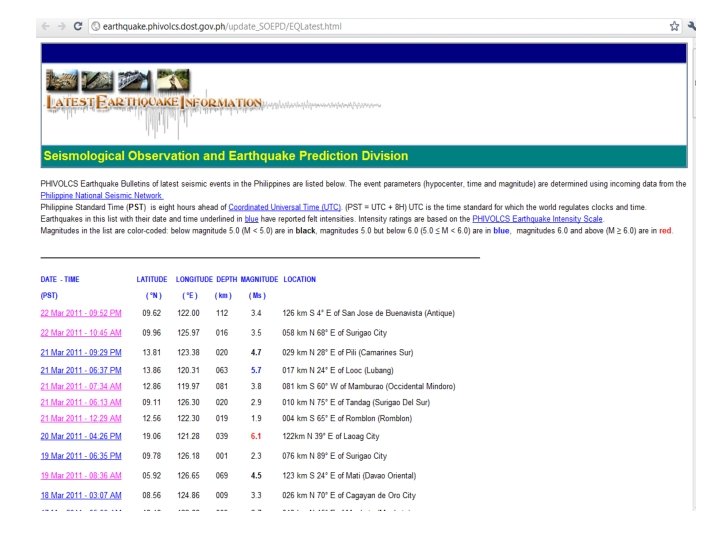
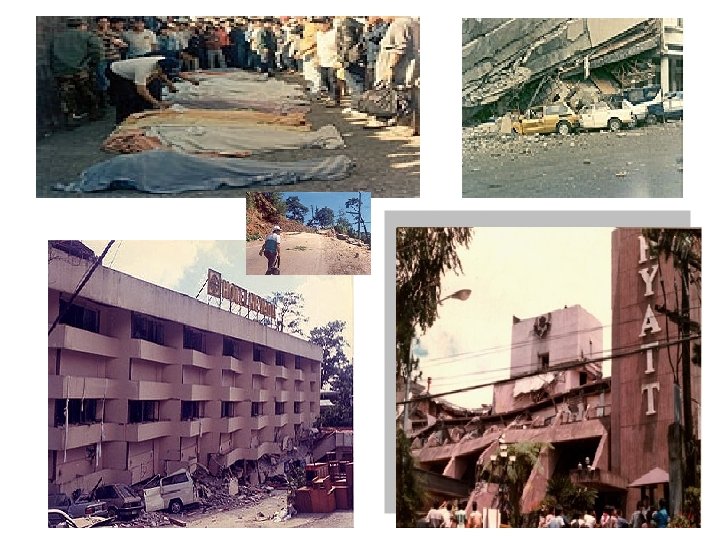
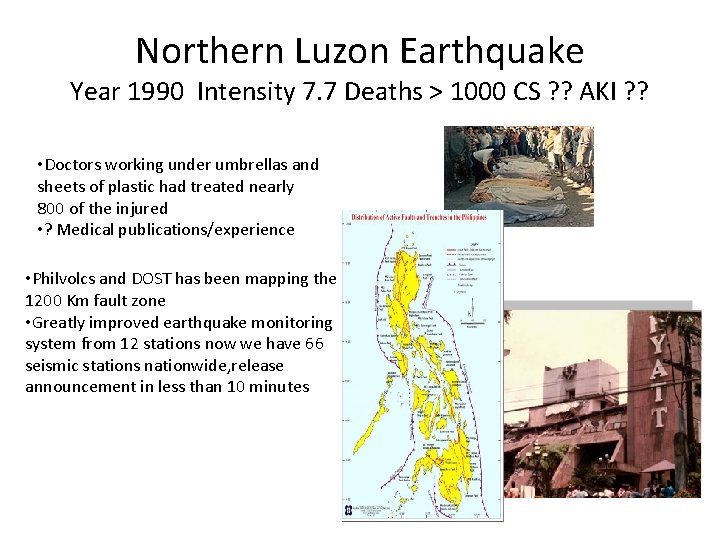
Northern Luzon Earthquake Year 1990 Intensity 7. 7 Deaths > 1000 CS ? ? AKI ? ? • Doctors working under umbrellas and sheets of plastic had treated nearly 800 of the injured • ? Medical publications/experience • Philvolcs and DOST has been mapping the 1200 Km fault zone • Greatly improved earthquake monitoring system from 12 stations now we have 66 seismic stations nationwide, release announcement in less than 10 minutes
PSN DISASTER RESPONSE TO CRUSH INJURY/CRUSH SYNDROME • Most doctors and even nephrologists have no regular experience with CS • Thus, there is a need for guidance • “recommendations only” due to lack of evidence
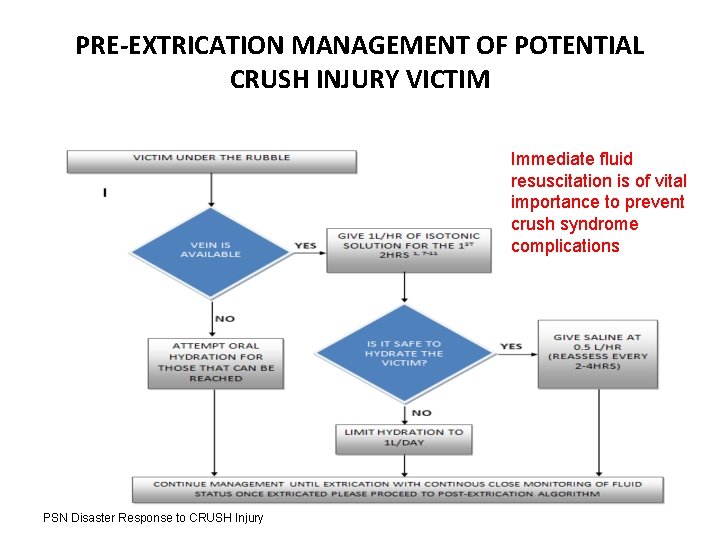
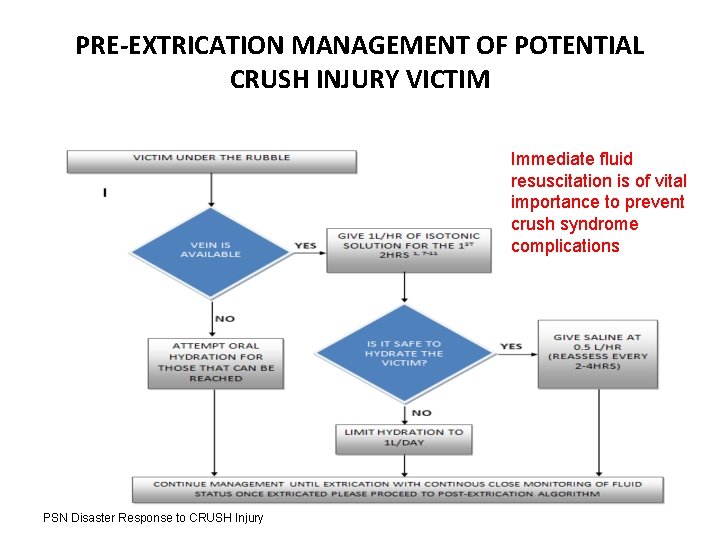
PRE-EXTRICATION MANAGEMENT OF POTENTIAL CRUSH INJURY VICTIM Immediate fluid resuscitation is of vital importance to prevent crush syndrome complications PSN Disaster Response to CRUSH Injury
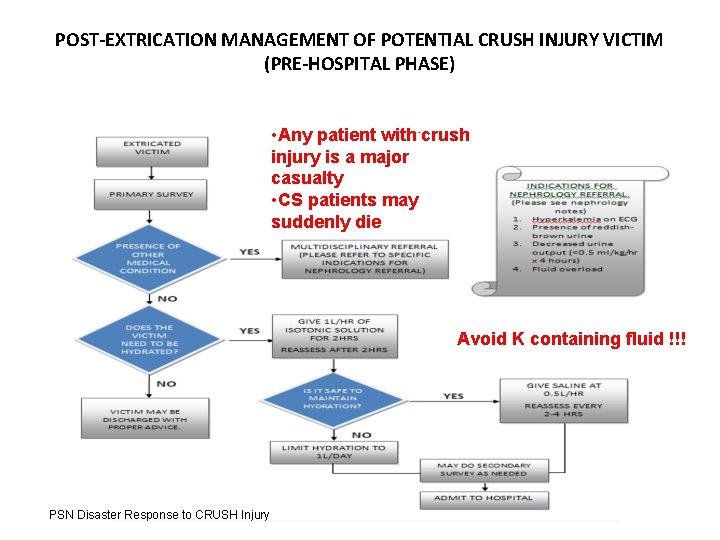
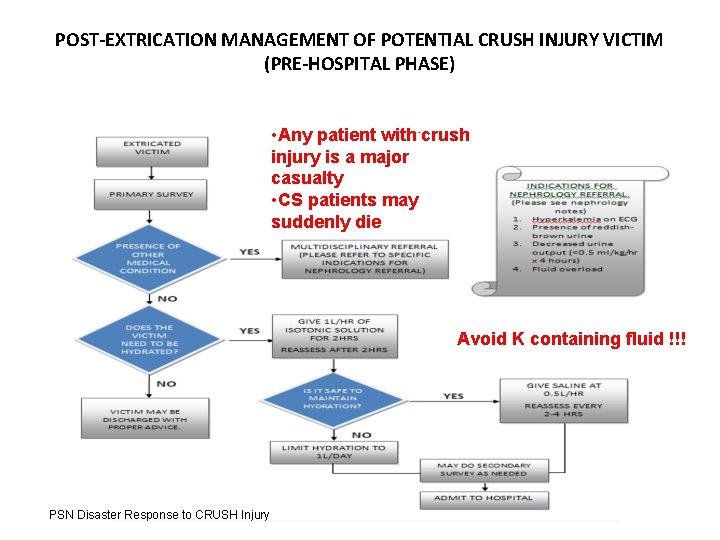
POST-EXTRICATION MANAGEMENT OF POTENTIAL CRUSH INJURY VICTIM (PRE-HOSPITAL PHASE) • Any patient with crush injury is a major casualty • CS patients may suddenly die Avoid K containing fluid !!! PSN Disaster Response to CRUSH Injury
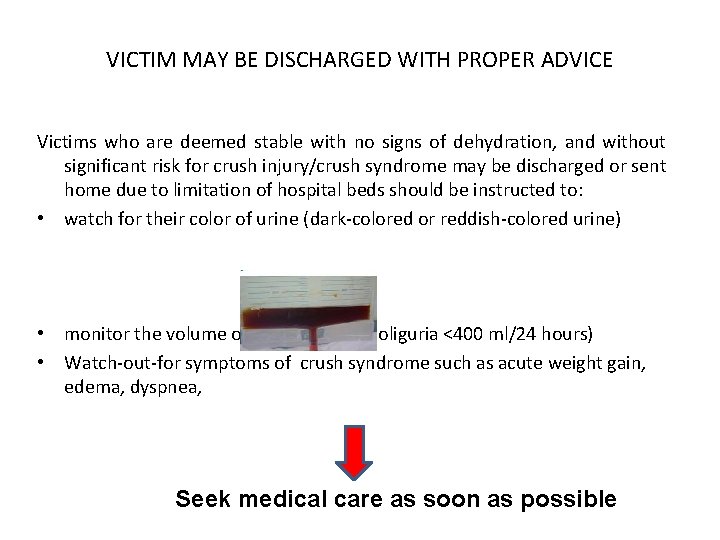
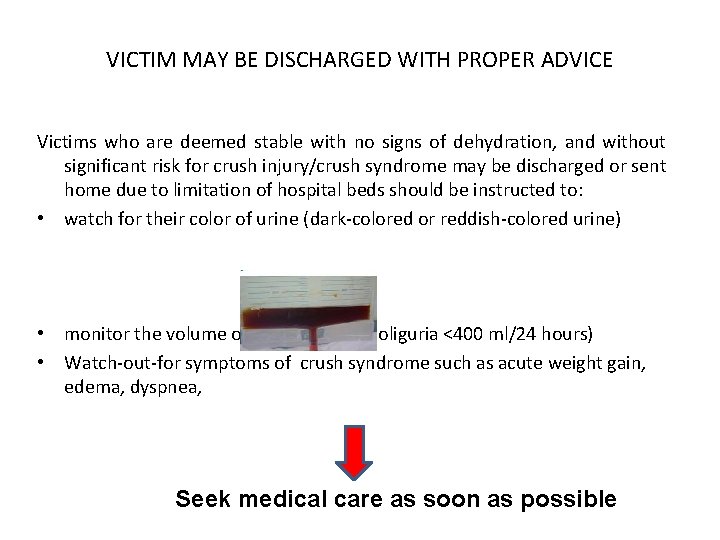
VICTIM MAY BE DISCHARGED WITH PROPER ADVICE Victims who are deemed stable with no signs of dehydration, and without significant risk for crush injury/crush syndrome may be discharged or sent home due to limitation of hospital beds should be instructed to: • watch for their color of urine (dark-colored or reddish-colored urine) • monitor the volume of urine (Note for oliguria <400 ml/24 hours) • Watch-out-for symptoms of crush syndrome such as acute weight gain, edema, dyspnea, Seek medical care as soon as possible
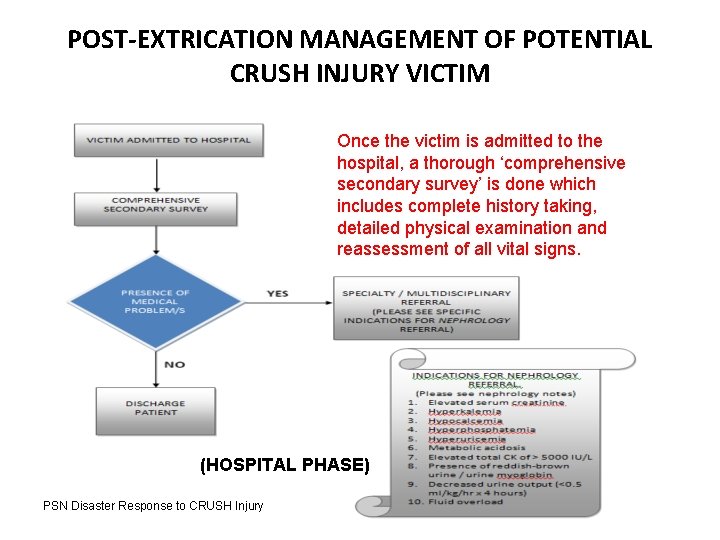
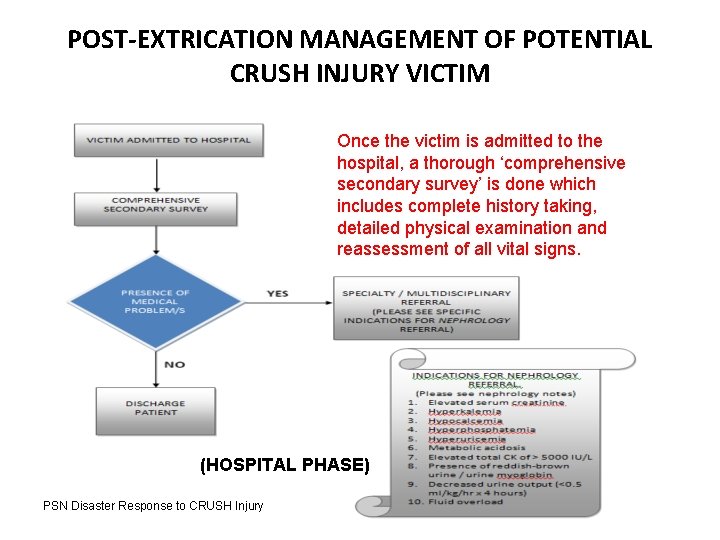
POST-EXTRICATION MANAGEMENT OF POTENTIAL CRUSH INJURY VICTIM Once the victim is admitted to the hospital, a thorough ‘comprehensive secondary survey’ is done which includes complete history taking, detailed physical examination and reassessment of all vital signs. (HOSPITAL PHASE) PSN Disaster Response to CRUSH Injury
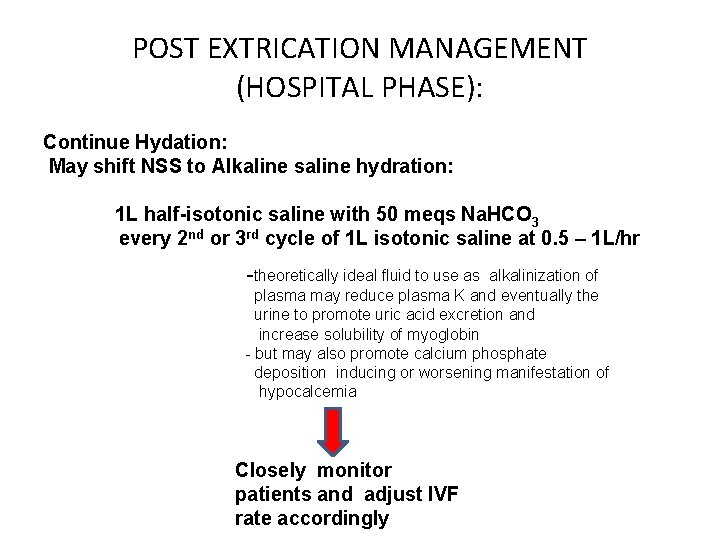
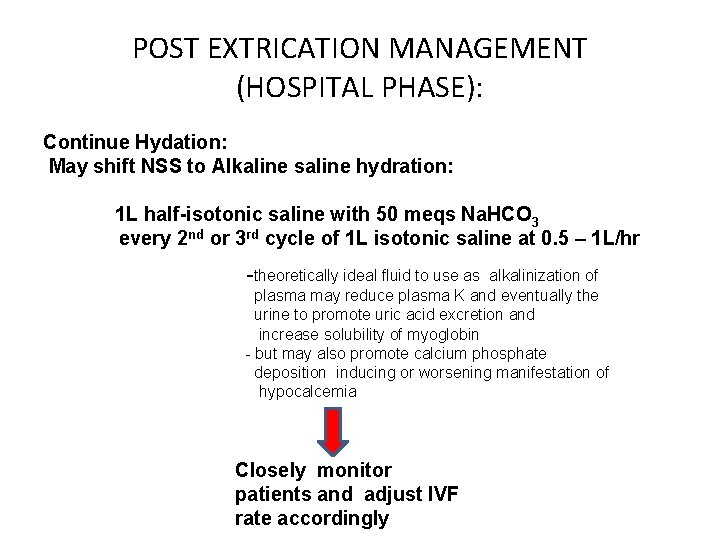
POST EXTRICATION MANAGEMENT (HOSPITAL PHASE): Continue Hydation: May shift NSS to Alkaline saline hydration: 1 L half-isotonic saline with 50 meqs Na. HCO 3 every 2 nd or 3 rd cycle of 1 L isotonic saline at 0. 5 – 1 L/hr -theoretically ideal fluid to use as alkalinization of plasma may reduce plasma K and eventually the urine to promote uric acid excretion and increase solubility of myoglobin - but may also promote calcium phosphate deposition inducing or worsening manifestation of hypocalcemia Closely monitor patients and adjust IVF rate accordingly
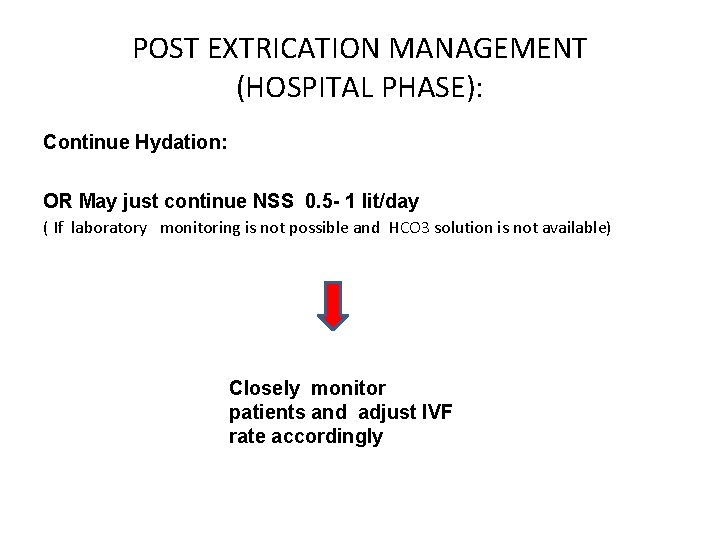
POST EXTRICATION MANAGEMENT (HOSPITAL PHASE): Continue Hydation: OR May just continue NSS 0. 5 - 1 lit/day ( If laboratory monitoring is not possible and HCO 3 solution is not available) Closely monitor patients and adjust IVF rate accordingly
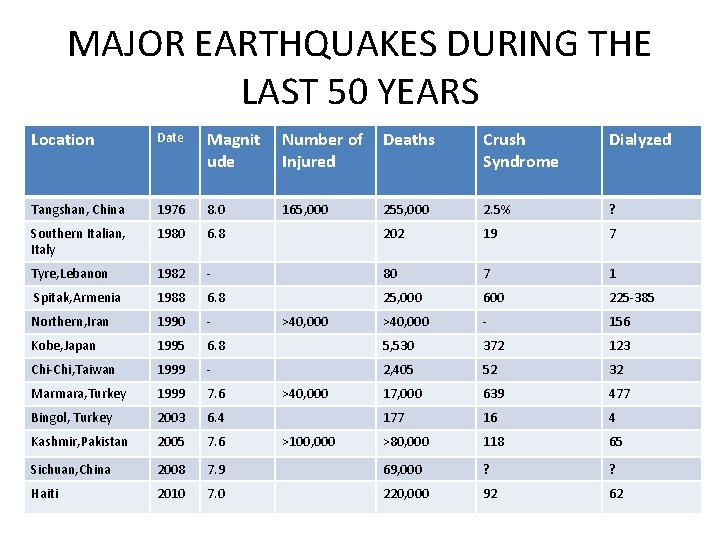
MAJOR EARTHQUAKES DURING THE LAST 50 YEARS Location Date Magnit ude Number of Deaths Injured Crush Syndrome Dialyzed Tangshan, China 1976 8. 0 165, 000 255, 000 2. 5% ? Southern Italian, Italy 1980 6. 8 202 19 7 Tyre, Lebanon 1982 - 80 7 1 Spitak, Armenia 1988 6. 8 25, 000 600 225 -385 Northern, Iran 1990 - >40, 000 - 156 Kobe, Japan 1995 6. 8 5, 530 372 123 Chi-Chi, Taiwan 1999 - 2, 405 52 32 Marmara, Turkey 1999 7. 6 17, 000 639 477 Bingol, Turkey 2003 6. 4 177 16 4 Kashmir, Pakistan 2005 7. 6 >80, 000 118 65 Sichuan, China 2008 7. 9 69, 000 ? ? Haiti 2010 7. 0 220, 000 92 62 >40, 000 >100, 000
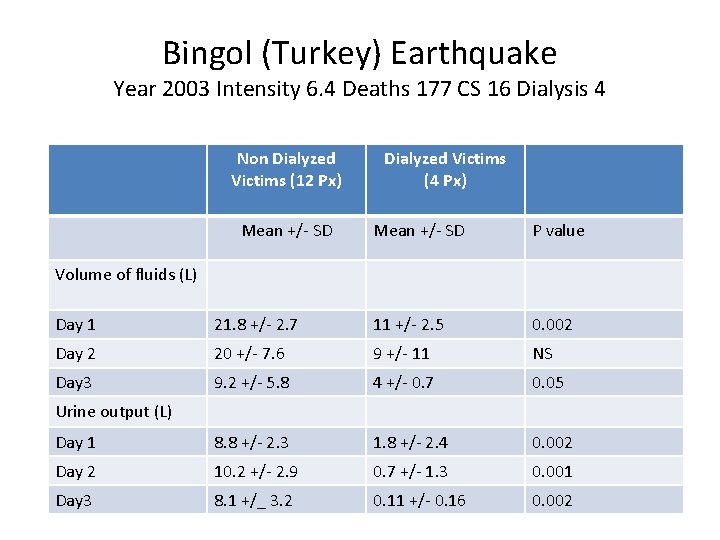
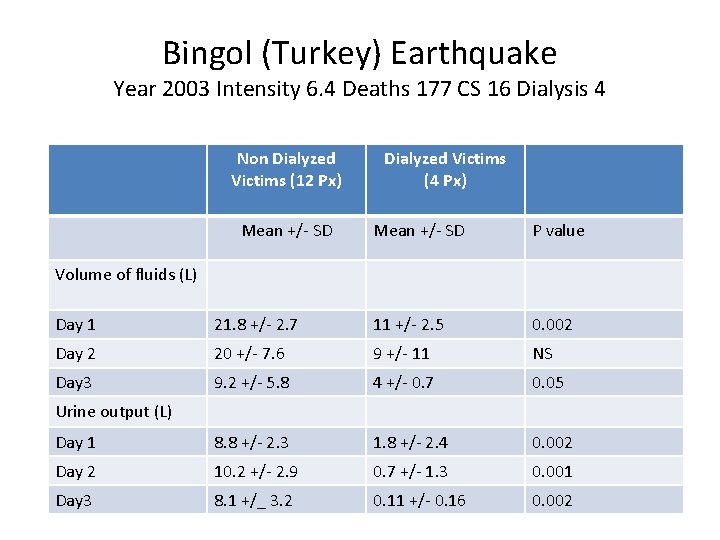
Bingol (Turkey) Earthquake Year 2003 Intensity 6. 4 Deaths 177 CS 16 Dialysis 4 Non Dialyzed Victims (12 Px) Mean +/- SD Dialyzed Victims (4 Px) Mean +/- SD P value Volume of fluids (L) Day 1 21. 8 +/- 2. 7 11 +/- 2. 5 0. 002 Day 2 20 +/- 7. 6 9 +/- 11 NS Day 3 9. 2 +/- 5. 8 4 +/- 0. 7 0. 05 Day 1 8. 8 +/- 2. 3 1. 8 +/- 2. 4 0. 002 Day 2 10. 2 +/- 2. 9 0. 7 +/- 1. 3 0. 001 Day 3 8. 1 +/_ 3. 2 0. 11 +/- 0. 16 0. 002 Urine output (L)
Bingol (Turkey) Earthquake Year 2003 Intensity 6. 4 Deaths 177 CS 16 Dialysis 4 • Early adequate fluid administration helps prevent dialysis
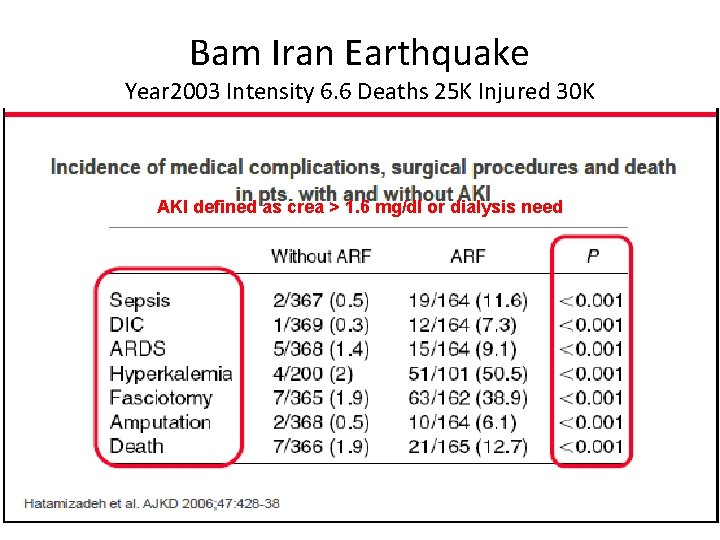
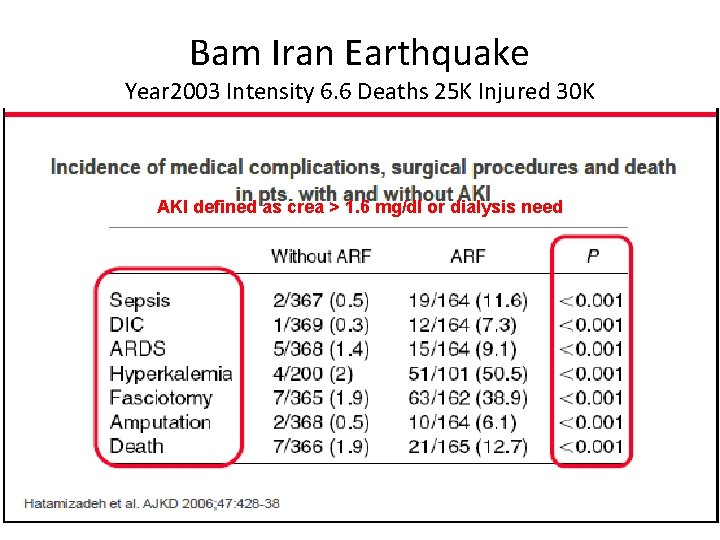
Bam Iran Earthquake Year 2003 Intensity 6. 6 Deaths 25 K Injured 30 K AKI defined as crea > 1. 6 mg/dl or dialysis need
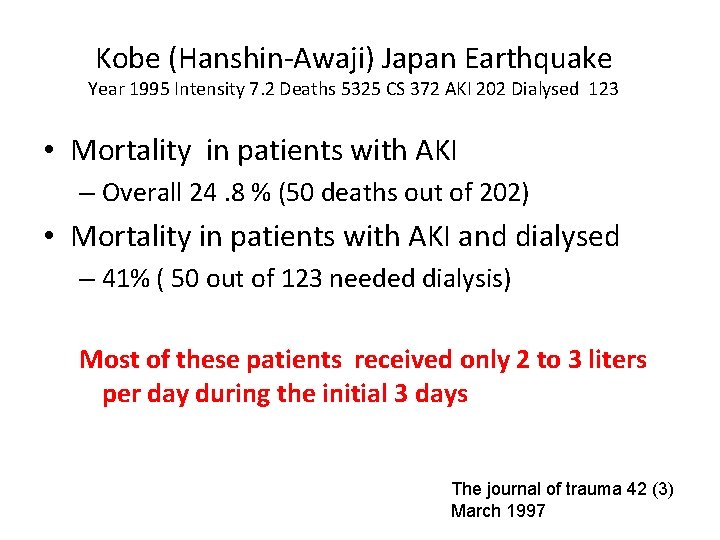
Kobe (Hanshin-Awaji) Japan Earthquake Year 1995 Intensity 7. 2 Deaths 5325 CS 372 AKI 202 Dialysed 123 • Mortality in patients with AKI – Overall 24. 8 % (50 deaths out of 202) • Mortality in patients with AKI and dialysed – 41% ( 50 out of 123 needed dialysis) Most of these patients received only 2 to 3 liters per day during the initial 3 days The journal of trauma 42 (3) March 1997
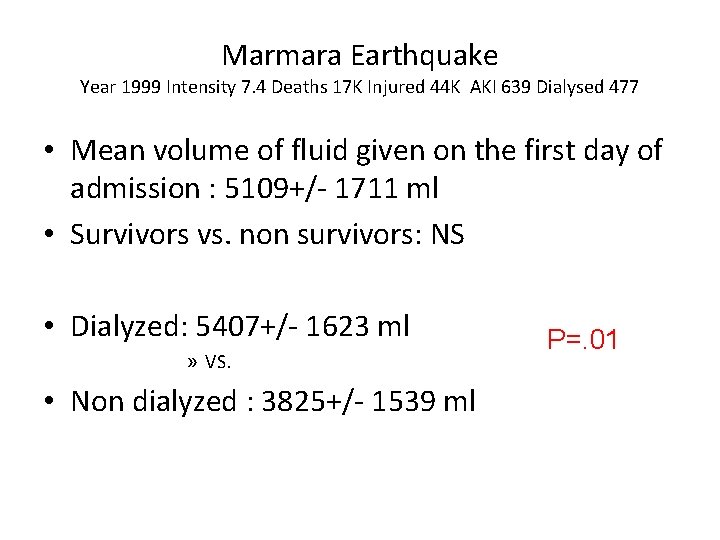
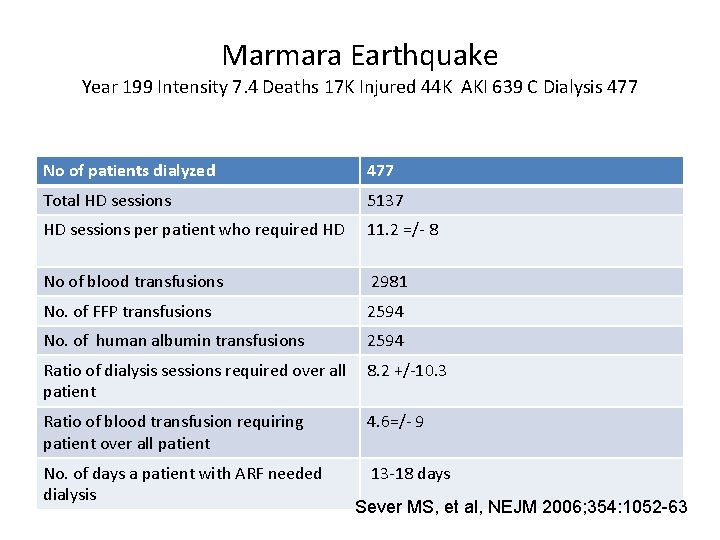
Marmara Earthquake Year 1999 Intensity 7. 4 Deaths 17 K Injured 44 K AKI 639 Dialysed 477 • Mean volume of fluid given on the first day of admission : 5109+/- 1711 ml • Survivors vs. non survivors: NS • Dialyzed: 5407+/- 1623 ml » VS. • Non dialyzed : 3825+/- 1539 ml P=. 01
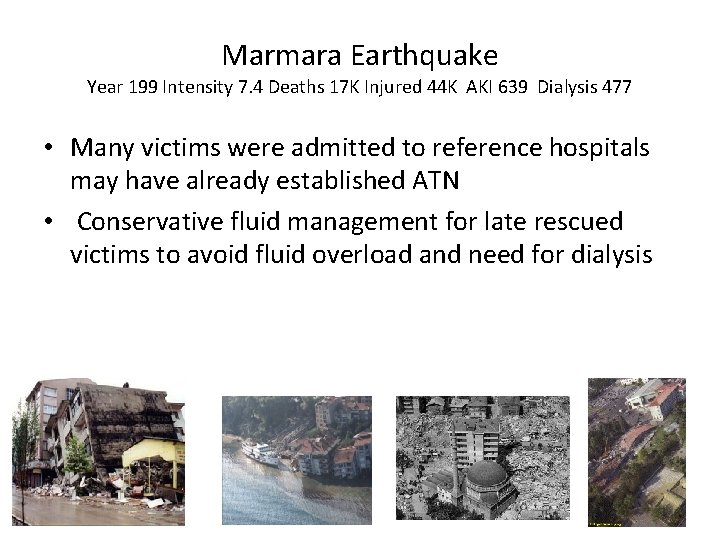
Marmara Earthquake Year 199 Intensity 7. 4 Deaths 17 K Injured 44 K AKI 639 Dialysis 477 • Many victims were admitted to reference hospitals may have already established ATN • Conservative fluid management for late rescued victims to avoid fluid overload and need for dialysis
POST EXTRICATION MANAGEMENT (HOSPITAL PHASE): Conservative Hydration: if close monitoring is impossible late rescued victims as ATN have developed already
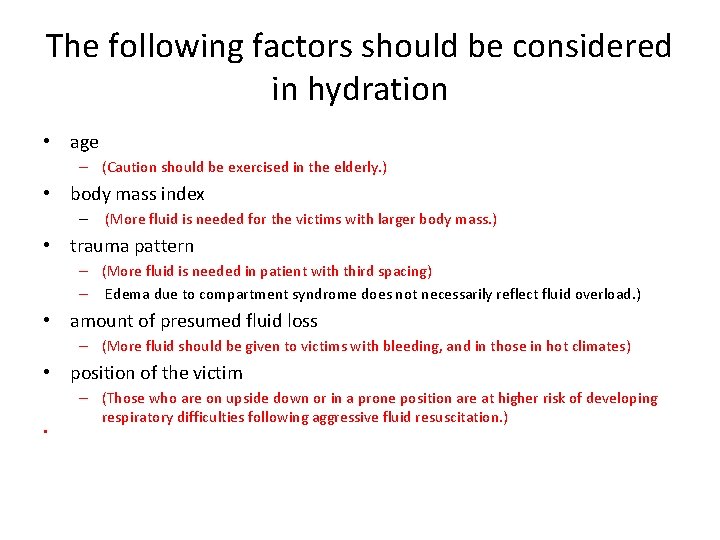
The following factors should be considered in hydration • age – (Caution should be exercised in the elderly. ) • body mass index – (More fluid is needed for the victims with larger body mass. ) • trauma pattern – (More fluid is needed in patient with third spacing) – Edema due to compartment syndrome does not necessarily reflect fluid overload. ) • amount of presumed fluid loss – (More fluid should be given to victims with bleeding, and in those in hot climates) • position of the victim • – (Those who are on upside down or in a prone position are at higher risk of developing respiratory difficulties following aggressive fluid resuscitation. )
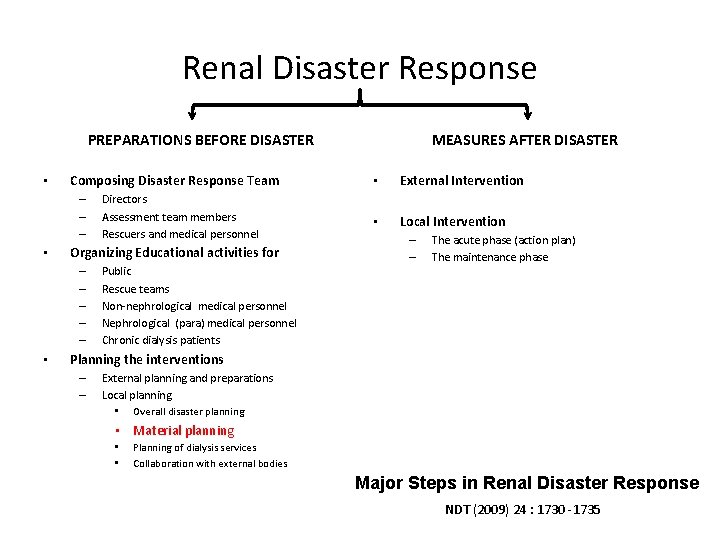
Renal Disaster Response PREPARATIONS BEFORE DISASTER • Composing Disaster Response Team – – – • Organizing Educational activities for – – – • Directors Assessment team members Rescuers and medical personnel Public Rescue teams Non-nephrological medical personnel Nephrological (para) medical personnel Chronic dialysis patients MEASURES AFTER DISASTER • External Intervention • Local Intervention – – The acute phase (action plan) The maintenance phase Planning the interventions – – External planning and preparations Local planning • Overall disaster planning • Material planning • • Planning of dialysis services Collaboration with external bodies Major Steps in Renal Disaster Response NDT (2009) 24 : 1730 -1735
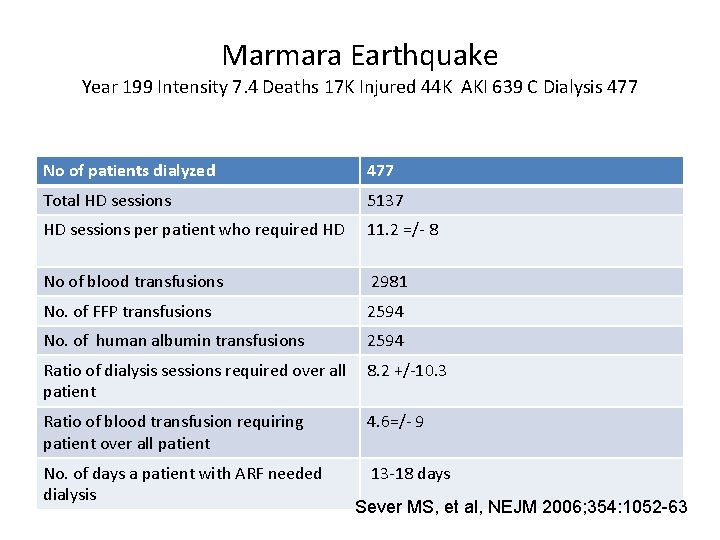
Marmara Earthquake Year 199 Intensity 7. 4 Deaths 17 K Injured 44 K AKI 639 C Dialysis 477 No of patients dialyzed 477 Total HD sessions 5137 HD sessions per patient who required HD 11. 2 =/- 8 No of blood transfusions 2981 No. of FFP transfusions 2594 No. of human albumin transfusions 2594 Ratio of dialysis sessions required over all 8. 2 +/-10. 3 patient Ratio of blood transfusion requiring patient over all patient 4. 6=/- 9 No. of days a patient with ARF needed dialysis 13 -18 days Sever MS, et al, NEJM 2006; 354: 1052 -63
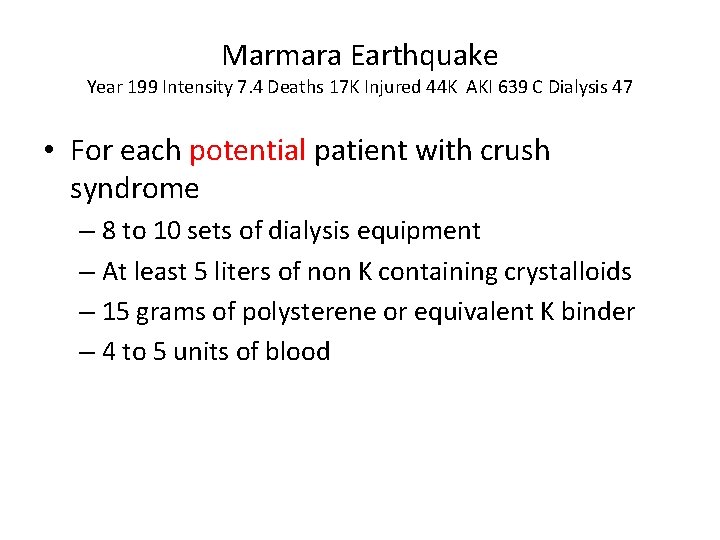
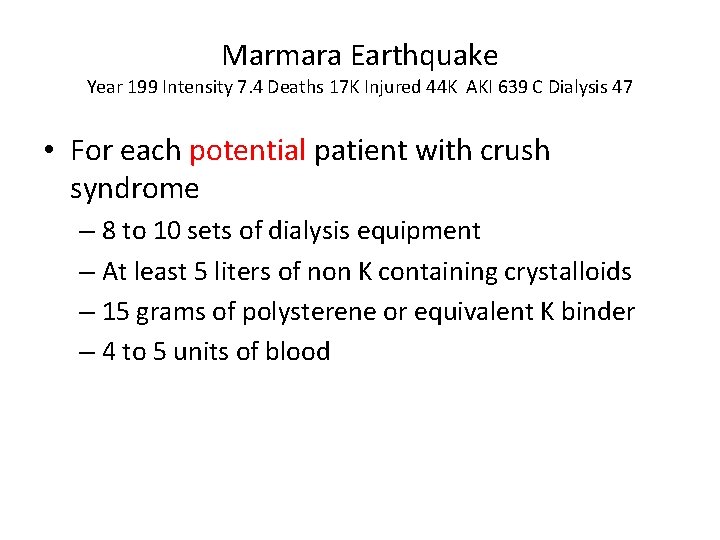
Marmara Earthquake Year 199 Intensity 7. 4 Deaths 17 K Injured 44 K AKI 639 C Dialysis 47 • For each potential patient with crush syndrome – 8 to 10 sets of dialysis equipment – At least 5 liters of non K containing crystalloids – 15 grams of polysterene or equivalent K binder – 4 to 5 units of blood
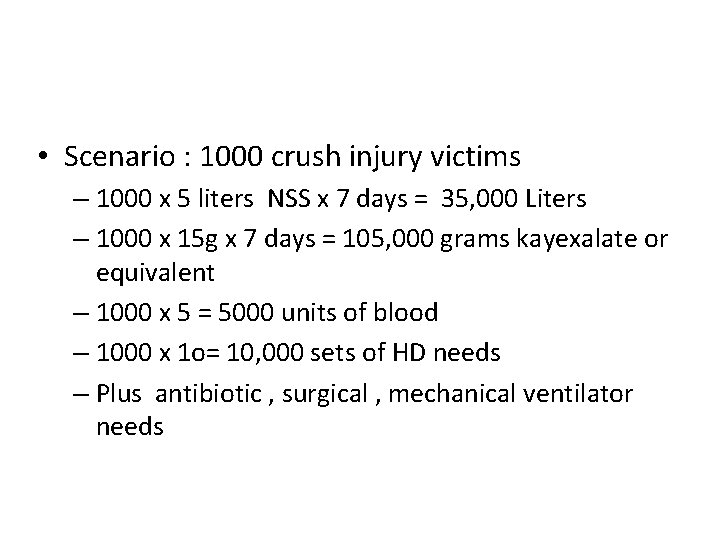
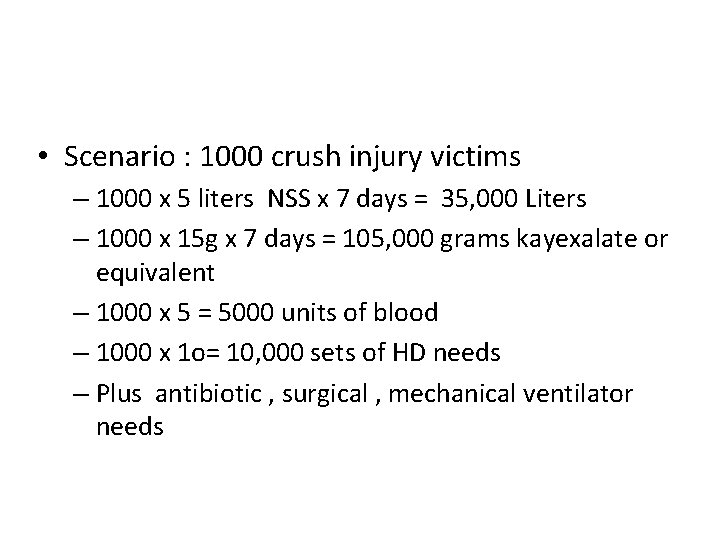
• Scenario : 1000 crush injury victims – 1000 x 5 liters NSS x 7 days = 35, 000 Liters – 1000 x 15 g x 7 days = 105, 000 grams kayexalate or equivalent – 1000 x 5 = 5000 units of blood – 1000 x 1 o= 10, 000 sets of HD needs – Plus antibiotic , surgical , mechanical ventilator needs
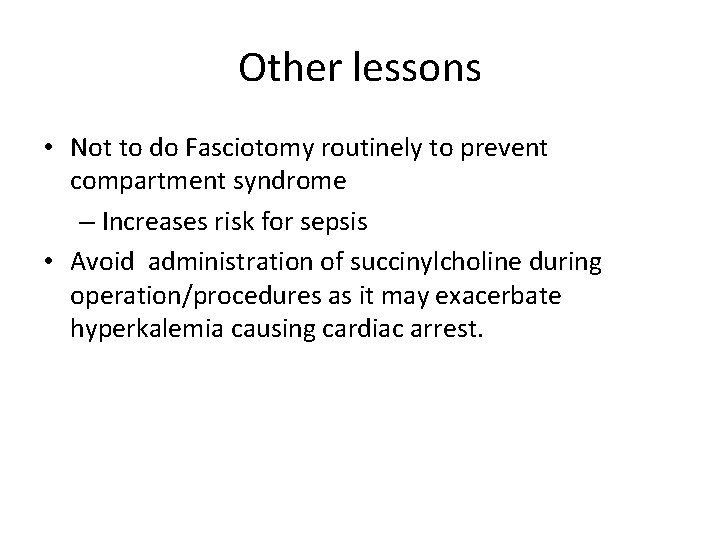
Other lessons • Not to do Fasciotomy routinely to prevent compartment syndrome – Increases risk for sepsis • Avoid administration of succinylcholine during operation/procedures as it may exacerbate hyperkalemia causing cardiac arrest.
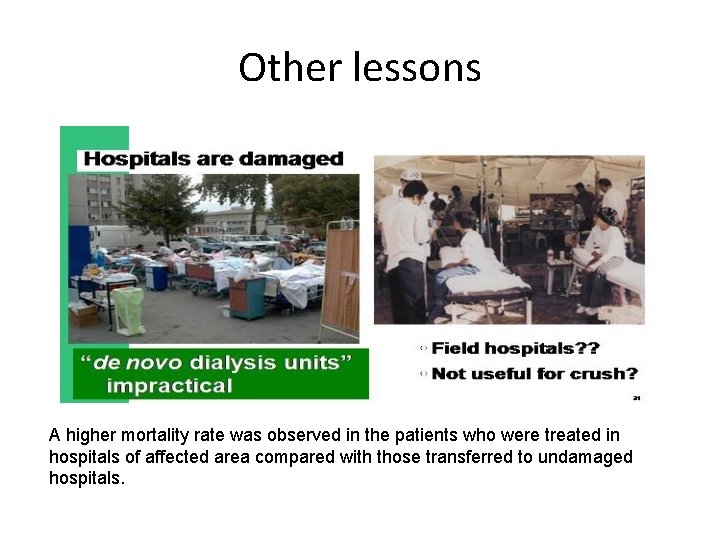
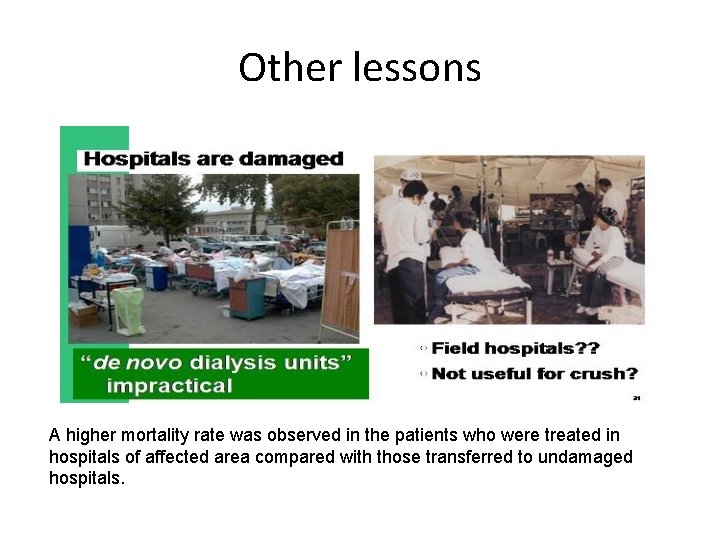
Other lessons A higher mortality rate was observed in the patients who were treated in hospitals of affected area compared with those transferred to undamaged hospitals.
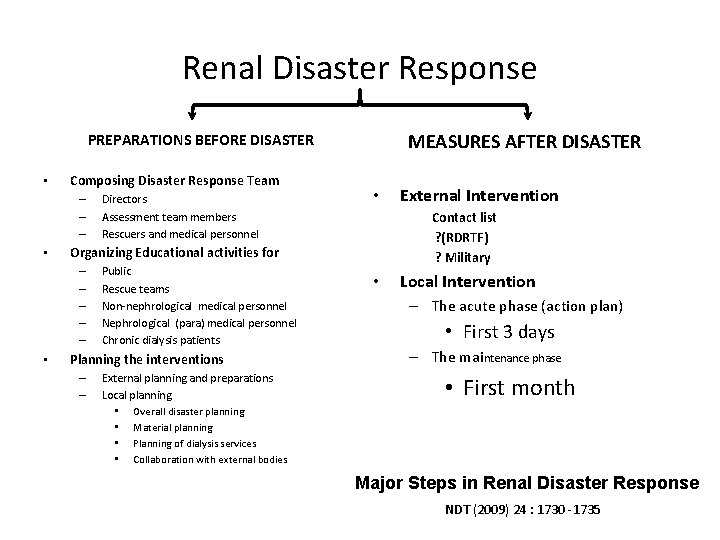
Renal Disaster Response MEASURES AFTER DISASTER PREPARATIONS BEFORE DISASTER • Composing Disaster Response Team – – – • • Public Rescue teams Non-nephrological medical personnel Nephrological (para) medical personnel Chronic dialysis patients Planning the interventions – – External planning and preparations Local planning • Overall disaster planning • Material planning • Planning of dialysis services • Collaboration with external bodies External Intervention Contact list ? (RDRTF) ? Military Organizing Educational activities for – – – • Directors Assessment team members Rescuers and medical personnel • Local Intervention – The acute phase (action plan) • First 3 days – The maintenance phase • First month Major Steps in Renal Disaster Response NDT (2009) 24 : 1730 -1735
There is no substitute for public awareness and preparedness as Diasaters can rarely be anticipated, much less prevented.
the Filipino value of communal effort “The Children of Adam are limbs of each other Having been created of one essence. When the calamity of time afflicts one limb The other limbs cannot remain at rest. If thou hast no sympathy for the troubles of others Thou art unworthy to be called by the name of a man” Saadi ( Persian poet) In times of disaster it is a universal instinct of a man to be of help.
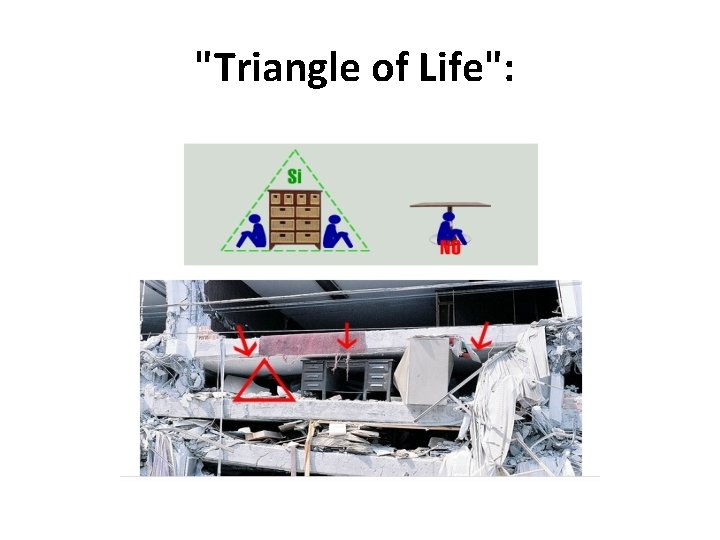
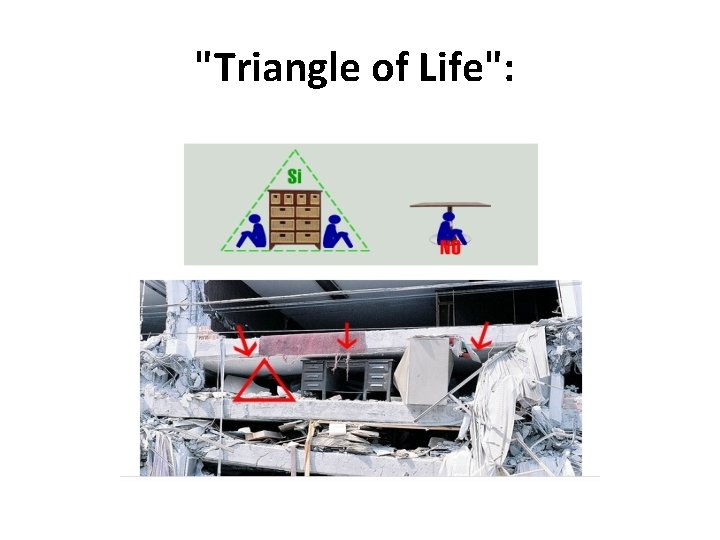
"Triangle of Life":
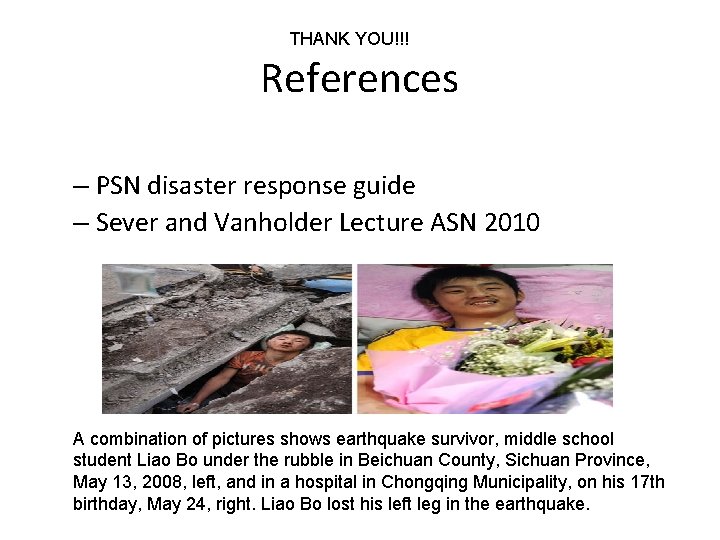
THANK YOU!!! References – PSN disaster response guide – Sever and Vanholder Lecture ASN 2010 A combination of pictures shows earthquake survivor, middle school student Liao Bo under the rubble in Beichuan County, Sichuan Province, May 13, 2008, left, and in a hospital in Chongqing Municipality, on his 17 th birthday, May 24, right. Liao Bo lost his left leg in the earthquake.

EMERGENCY PREPAREDNESS AND TRANSPORT OF THE SICK AND INJURED (Patient/ Casualty Handling) by: Bernardo C. Cueto, MD ( Emergency Preparedness Officer)
PURPOSE The purpose of this lecture is to orient MMC medical personel how to prepare for possible emergencies that may occur in the hospital. It also intends to inform the participants how to properly transport patients
OBJECTIVES At the end of this module, participants will be able to • Describe the Hospital Emergency Preparedness Committee Structure • Enumerate the Hospital Emergency Codes • Enumerate the Hospital Evacuation Code
OBJECTIVES • Define Emergency Rescue and Transfer • Demonstrate technique of Emergency Transfer • Describe the hospital plan for the different possible disasters
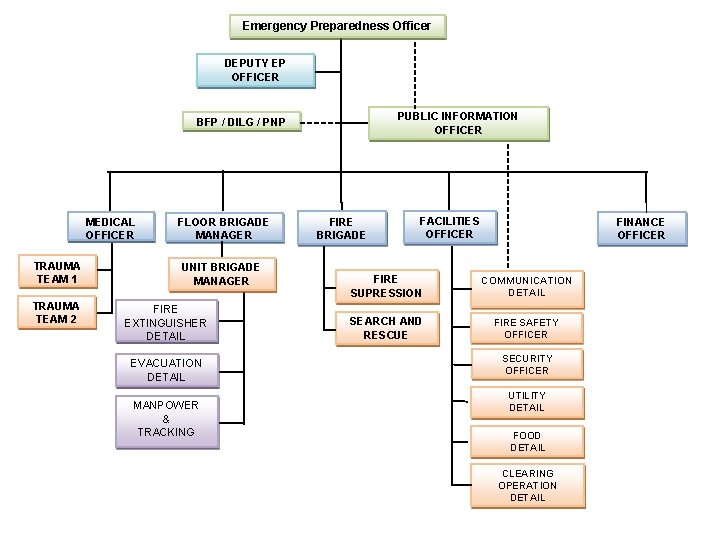
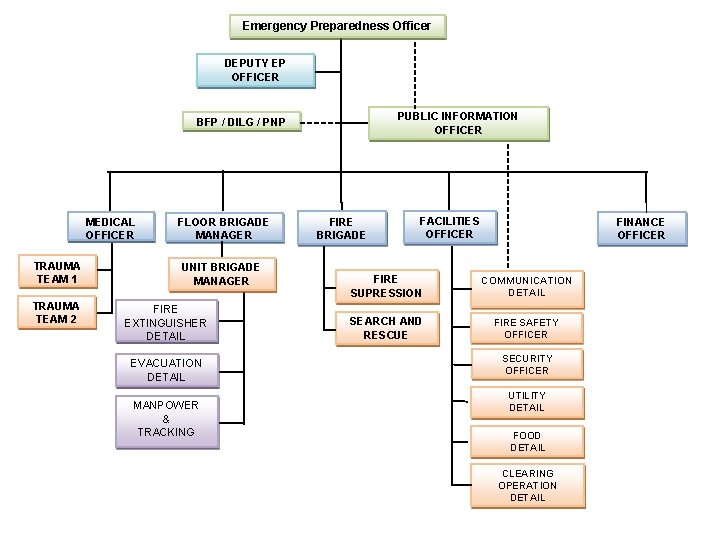
Emergency Preparedness Officer DEPUTY EP OFFICER PUBLIC INFORMATION OFFICER BFP / DILG / PNP MEDICAL OFFICER TRAUMA TEAM 1 TRAUMA TEAM 2 FLOOR BRIGADE MANAGER UNIT BRIGADE MANAGER FIRE EXTINGUISHER DETAIL EVACUATION DETAIL MANPOWER & TRACKING FIRE BRIGADE FACILITIES OFFICER FINANCE OFFICER FIRE SUPRESSION COMMUNICATION DETAIL SEARCH AND RESCUE FIRE SAFETY OFFICER SECURITY OFFICER UTILITY DETAIL FOOD DETAIL CLEARING OPERATION DETAIL
FLOOR BRIGADE MANAGER Organizes and coordinates emergency response in their area of responsibility. DUTIES AND RESPONSIBILITIES: 1. Responsible for matters relative to Emergency Preparedness in his/her floor. 2. Responsible for the enforcement of safety rules and regulations in his/her floor 3. Organizes Floor Brigade in his/her floor composed of unit brigades in the different areas of the front rectangular , rear rectangular, wing and circular. ( The new building will have a different set of Floor Brigade Manager)
FLOOR BRIGADE MANAGER 4. Acts as incident commander in his area of responsibility when an Emergency Incident arises. a) Directs fire fighting and if necessary direct initial evacuation b) Assures and calms down and assists patients and visitors in her floor to avoid panic c) Supervises the evacuation of his/her floor when so ordered and return his/her evacuees in accordance with the established procedure. 5. Communicates and updates Emergency Incident Commander during an incident.
FLOOR BRIGADE MANAGER 6. Informs the EPO, any situation likely to abate the effectiveness and readiness of the operation of the Emergency Preparedness Committee. 7. Carries out other responsibilities that may be assigned upon him/her by the Emergency Incident Commander as to aspect of emergency response.
UNIT BRIGADE MANAGER Organizes and directs emergency operations in the unit level DUTIES AND RESPONSIBILITIES: 1. Responsible for enforcing safety rules and regulations in his/her unit. 2. Ensures that fire fighting equipments in his/her area of responsibility are in proper condition. 3. Ensures that the telephone operators are informed when there is an emergency in his/her area of responsibility.
UNIT BRIGADE MANAGER 4. In case of actual Emergency Incident, a) Directs fire fighting and if necessary direct initial evacuation b) Assures, calms down and assists patients and visitors in his/her unit to avoid panic c) Supervises the evacuation of his/her floor when so ordered return his/her evacuees in accordance with the established procedure. d) Oversees accounting of evacuated patients
UNIT BRIGADE MANAGER 5. Informs the Floor Brigade Manager of any situation likely to abate the effectiveness and readiness of the operation of the Emergency Preparedness Committee 6. Carries out other responsibilities that may be assigned to him/her in aspect of emergency response.
COMPOSITION OF THE UNIT BRIGADE 1. Fire extinguisher detail 2. Evacuation detail A. Personnel evacuation detail B. Property evacuation detail 3. Manpower and tracking
GUIDELINES IN EMERGENCY RESPONSE 1. PLAN 2. GATHER NEEDED MATERIALS 3. FOLLOW THE FOLLOWING INITIAL ACTION A – ASK FOR HELP I – INTERVENE D – DO NOT ADD INJURIES
Patient Assessment
GUIDELINES IN EMERGENCY RESPONSE SCENE ASSESSMENT ELEMENTS OF SCENE ASSESSMENT 1. CHECK FOR SAFETY ? 2. WHAT HAPPENED ? 3. HOW MANY ARE INJURED/SICK ? 4. ARE THERE PEOPLE WHO CAN HELP ? 5. WHAT IS THE MODE OF INJURY/ILLNESS
GUIDELINES IN EMERGENCY RESPONSE SCENE ASSESSMENT 1. Safety of the rescuer/ responder 2. Safety of the By Stander 3. Safety of the patient CALL FOR HELP 1. Local Emergency Number : Loc 1000 2. Direct Emergency Number: 888 89 00 3. Makati C 3 Number 168
GUIDELINES IN EMERGENCY RESPONSE HOSPITAL EMERGENCY CODE 1. Doctor Red 2. Doctor Blue 3. Doctor Pink 4. Doctor Orange 5. Maxicart
GUIDELINES IN EMERGENCY RESPONSE INITIAL ASSESSMENT – Check for Immediate threats to life R – Responsiveness A – Airway B – Breathing C - Circulation
GUIDELINES IN EMERGENCY RESPONSE SECONDARY ASSESSMENT – Check for possible threats to life 1. Check Vital Signs 2. Get Patient History 3. Do head to toe assessment (for trauma patient)
EVACUATION The process of moving a persons or things from a place to another, as a dangerous place or disaster area, for reason of safety or protection
TWO TYPES OF EVACUATION BASED ON AREA OF RELOCATION HORIZONTAL EVACUATION-means moving away from the area of danger to a safe place on the same floor where the individual is, at the time of the alarm or emergency. In this case, the individual should move away from the area of eminent danger.
TWO TYPES OF EVACUATION BASED ON AREA OF RELOCATION VERTICAL EVACUATION - using a stairway is the preferred method to exit a building. All exit passageways are marked with "EXIT" signs. Stairways can be used by those who are able to evacuate with or without assistance.
TWO HOSPITAL EVACAUATON CODE E 1 - is a partial vertical evacuation where the affected area is evacuated to the Emergency room while the adjacent floors evacuates horizontally away from the area of eminent danger. Other floors are on stand by alert.
TWO HOSPITAL EVACAUATON CODE E 2 - is a complete evacuation of the entire hospital (both towers) and the primary evacuation area is Ayala parking. Another evacuation area may be assigned if the primary evacuation area is found not to be safe.
EMERGENCY RESCUE AND TRANSFER Emergency Rescue – it is the moving of a sick or injured person from unsafe place to a place of safety Transfer – it is the moving of a sick or injured person after giving treatment
SELECTION OF TRANSFER METHOD WILL DEPEND ON THE FOLLOWING: 1. 2. 3. 4. Nature and severity of the injury. Size of the victim. Physical capabilities of the responder. Number of personnel and equipment available. 5. Nature of evacuation route. 6. Distance to be covered. 7. Gender of the victim (Last Consideration).
THINGS TO OBSERVED WHILE CARRYING THINGS TO OBSERVED WHILE CARRYIN 1. 2. 3. 4. 5. Victim’s airway must be maintained open. Hemorrhage is controlled. Victim is safely maintained in the correct position. Regular check of the victim’s condition is made. Supporting bandages and dressing remain effectively applied 6. The method of transfer is safe, comfortable and as speedy as circumstances permit.
THINGS TO OBSERVED WHILE CARRYING 6. The patient’s body is moved as one unit. 7. The taller first aiders stay at the head side of the victim. 8. First Aiders/bearers must observed ergonomics in lifting and moving of patient.
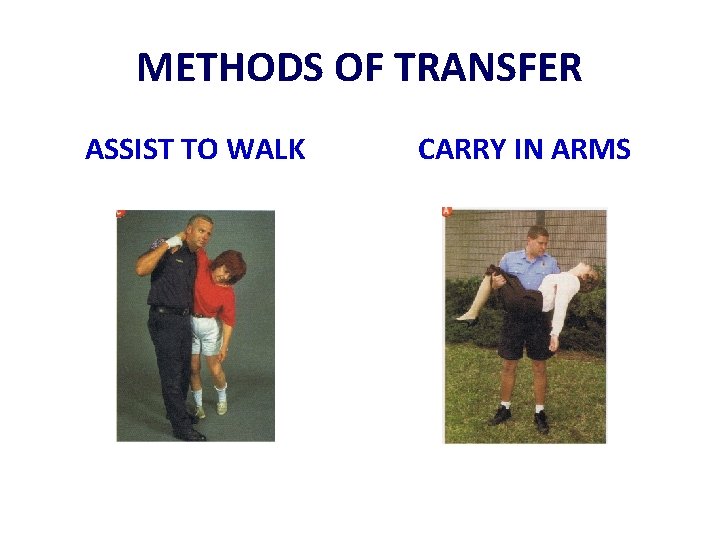
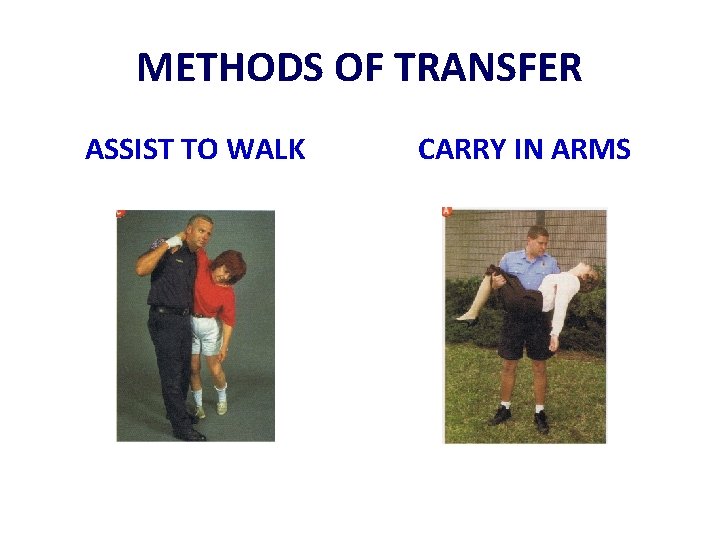
METHODS OF TRANSFER ASSIST TO WALK CARRY IN ARMS
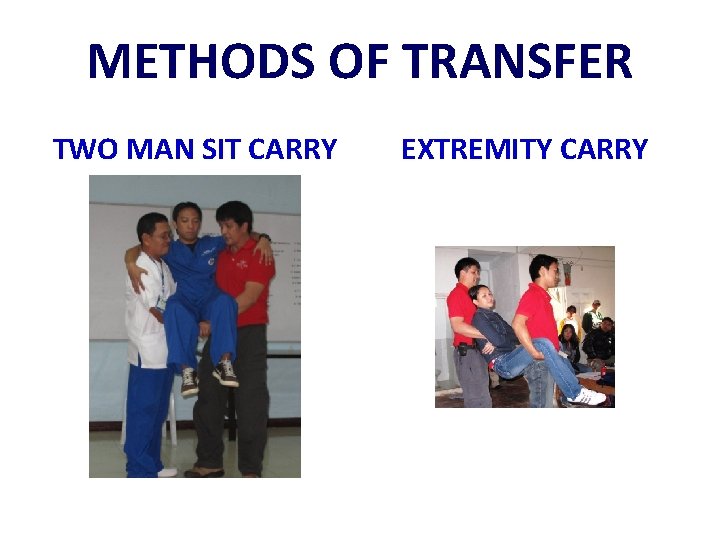
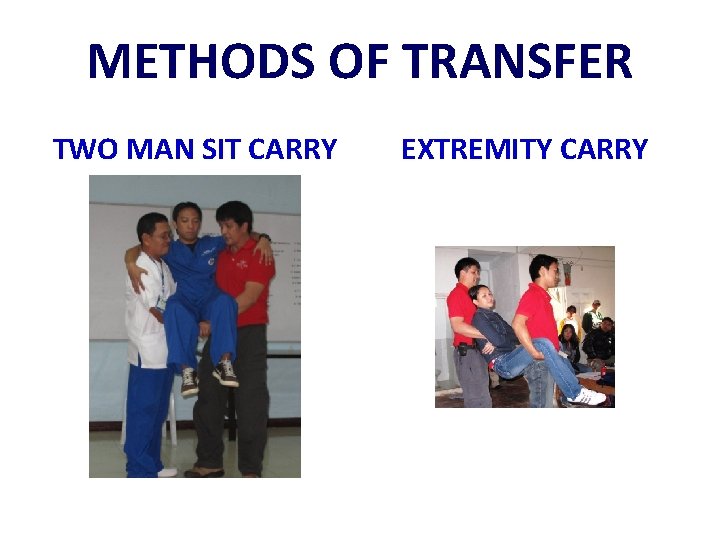
METHODS OF TRANSFER TWO MAN SIT CARRY EXTREMITY CARRY
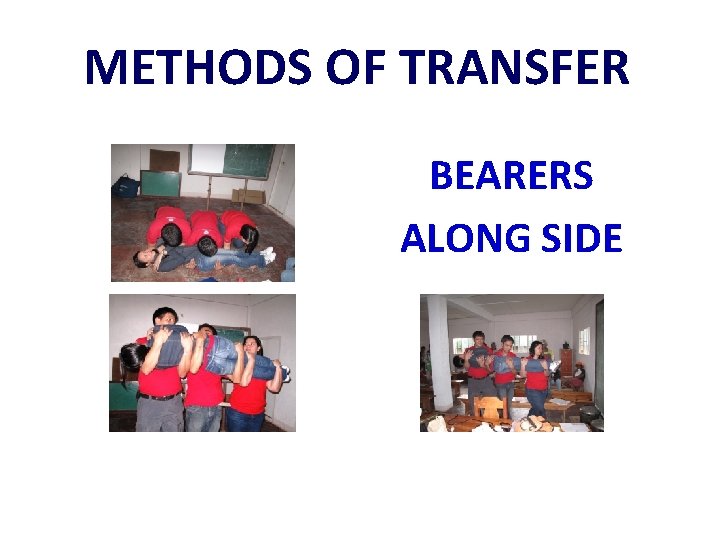
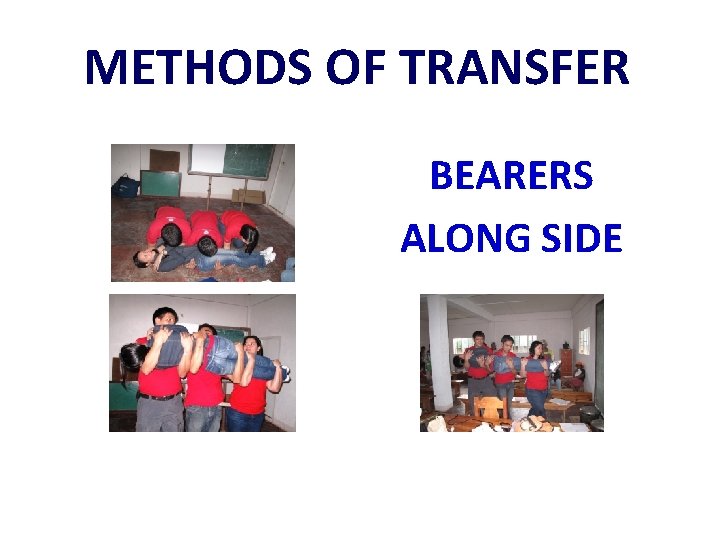
METHODS OF TRANSFER BEARERS ALONG SIDE
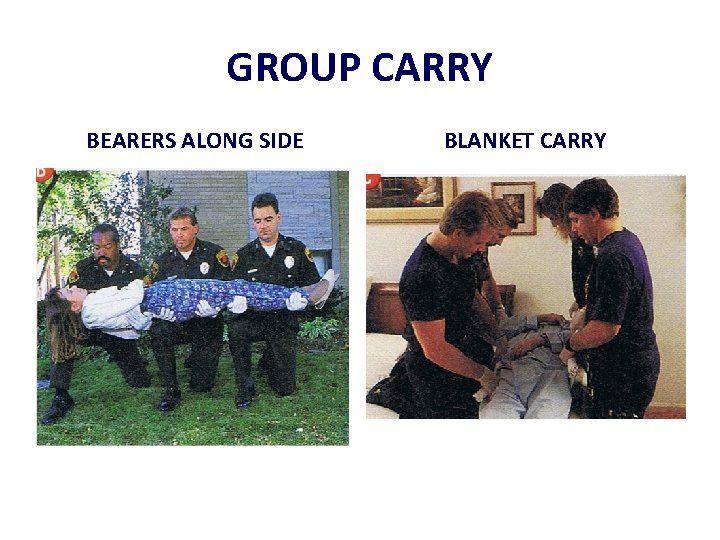
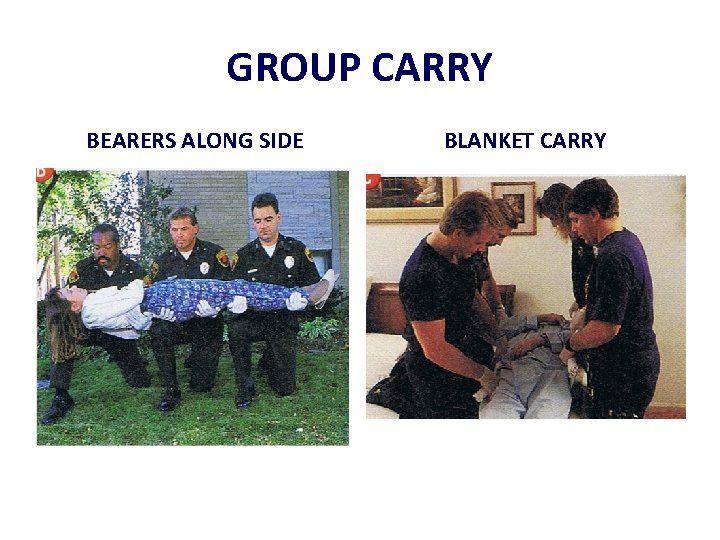
GROUP CARRY BEARERS ALONG SIDE BLANKET CARRY
DISASTER It is an event resulting in great loss and misfortune. TWO TYPES INTERNAL DISASTER- Is an uncontrollable crisis that originated in the facility. EXTERNAL DISASTER – Is an uncontrollable crisis that happened outside the facility and the hospital is tapped as an emergency facility.
HOW DO WE IDENTIFY HAZARD VULNERABILITY ASSESSMENT A process of identifying all hazards and identifying which one should be given priority in the preparedness planning. It is has three categories namely: 1. Natural Event 2. Human Event 3. Technological event
DRILLS 1. To acquaint/refresh the hospital personnel on the correct courses of action under different emergency situation. 2. To achieve an orderly and safe evacuation under proper discipline. 3. To prevent panic, confusion, injury, and loss of life in case of emergency. 4. To monitor the time for evacuation and fire response. 5. To identify training and emergency plan strengths and weaknesses. 6. To test the effectiveness of the alarm system, communication system, and the fire fighting apparatus and other safety equipment.
MAKATI MED DRILLS 1. 2. 3. 4. Fire Drill(announced or unannounced) Earthquake Drill( announced or unannounced) Hazardous Material Drill (announced or unannounced) Personnel Evacuation and rescue Drill (partial or general)
BEFORE EARTHQUAKE 1. CHECK FOR HAZARDS IN THE WORK PLACE 2. BE AWARE OF THE DIFFERENT EXITS IN YOUR AREA 3. IDENTIFY SAFE PLACES INDOOR AND OUTDOOR 4. EDUCATE YOURSELF AND YOUR CO – WORKERS 5. PREPARE DISASTER SUPPLIES a) First Aid Kit b) Flashlight and Whistle c) Drinking water d) Ready to eat food
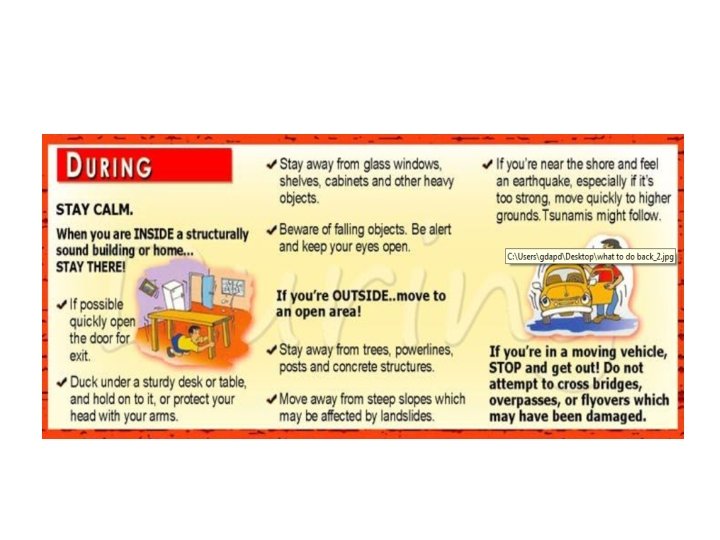
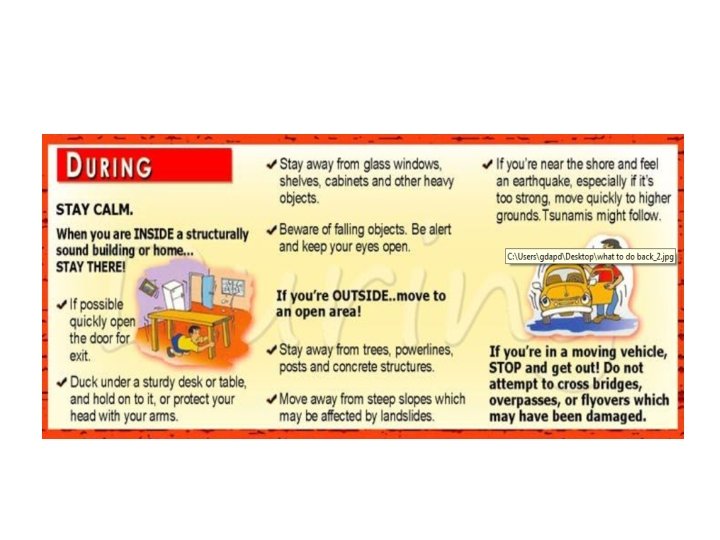
DURING EARTHQUAKE 1. 2. 3. 4. 5. DROP to the ground, take COVER and HOLD on until the shaking stops Stay away from glass, windows, outside doors and walls, and anything that could fall, such as lighting fixtures or furniture. Use a doorway for shelter only if it is in close proximity to you and if you know it is a strongly supported, loadbearing doorway. Stay inside until shaking stops and it is safe to go outside. Research has shown that most injuries occur when people inside buildings attempt to move to a different location inside the building or try to leave. DO NOT use the elevators.
AFTER EARTHQUAKE 1. Check evacuation route if safe 2. Evacuate and proceed to primary evacuation site for complete evacuation (wait for evacuation order) 3. Stay away from debris and objects that may fall 4. Keep a safe distance away from the building 5. Don’t return to area unless ALL CLEAR has been announced and return to work area has been ordered
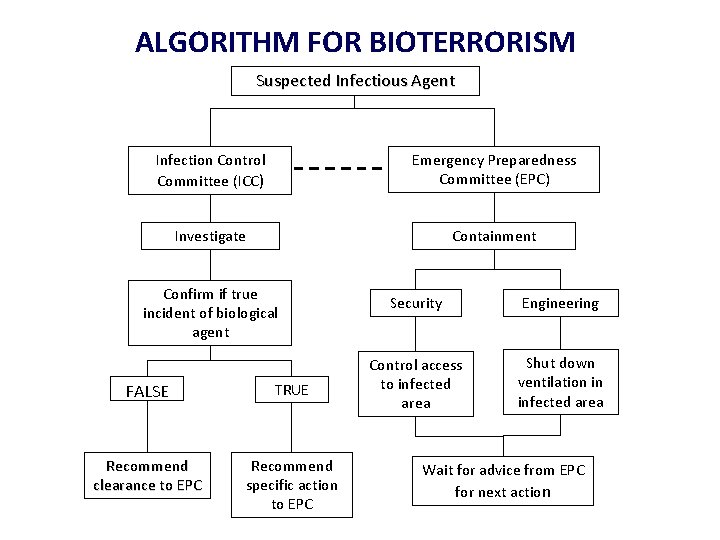
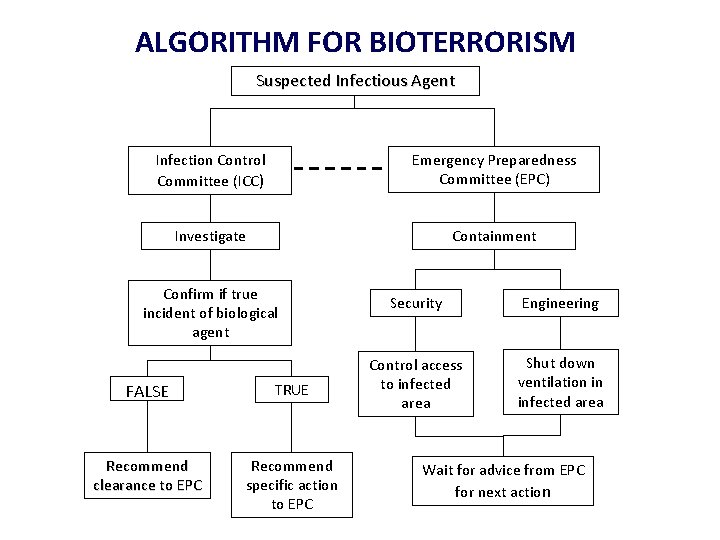
ALGORITHM FOR BIOTERRORISM Suspected Infectious Agent Infection Control Committee (ICC) Emergency Preparedness Committee (EPC) Investigate Containment Confirm if true incident of biological agent FALSE TRUE Recommend clearance to EPC Recommend specific action to EPC Security Engineering Control access to infected area Shut down ventilation in infected area Wait for advice from EPC for next action
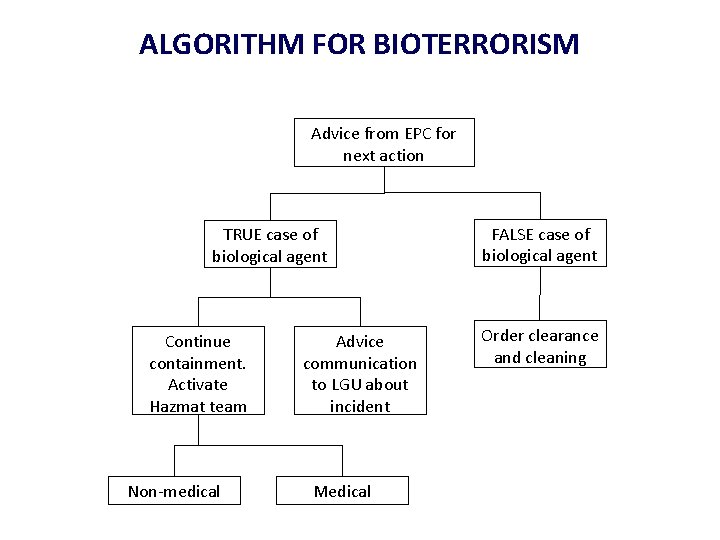
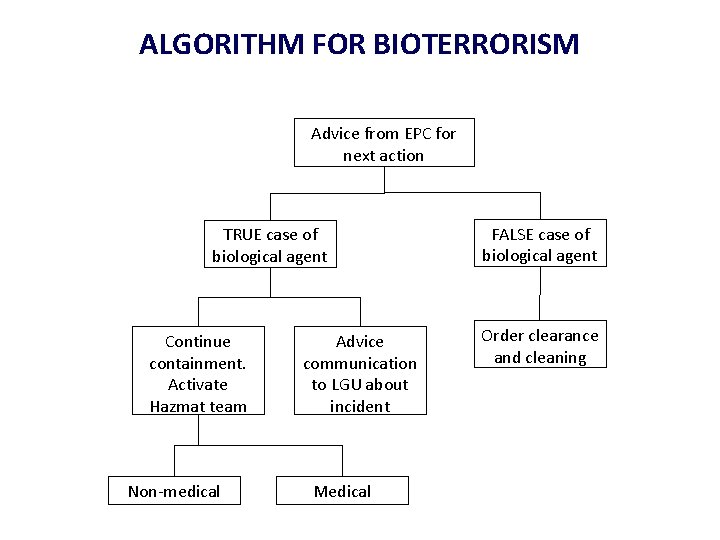
ALGORITHM FOR BIOTERRORISM Advice from EPC for next action TRUE case of biological agent Continue containment. Activate Hazmat team Non-medical Advice communication to LGU about incident Medical FALSE case of biological agent Order clearance and cleaning

BE SAFE GOOD DAY !!!