Lean Belt Certification Pathway for Student Resident and
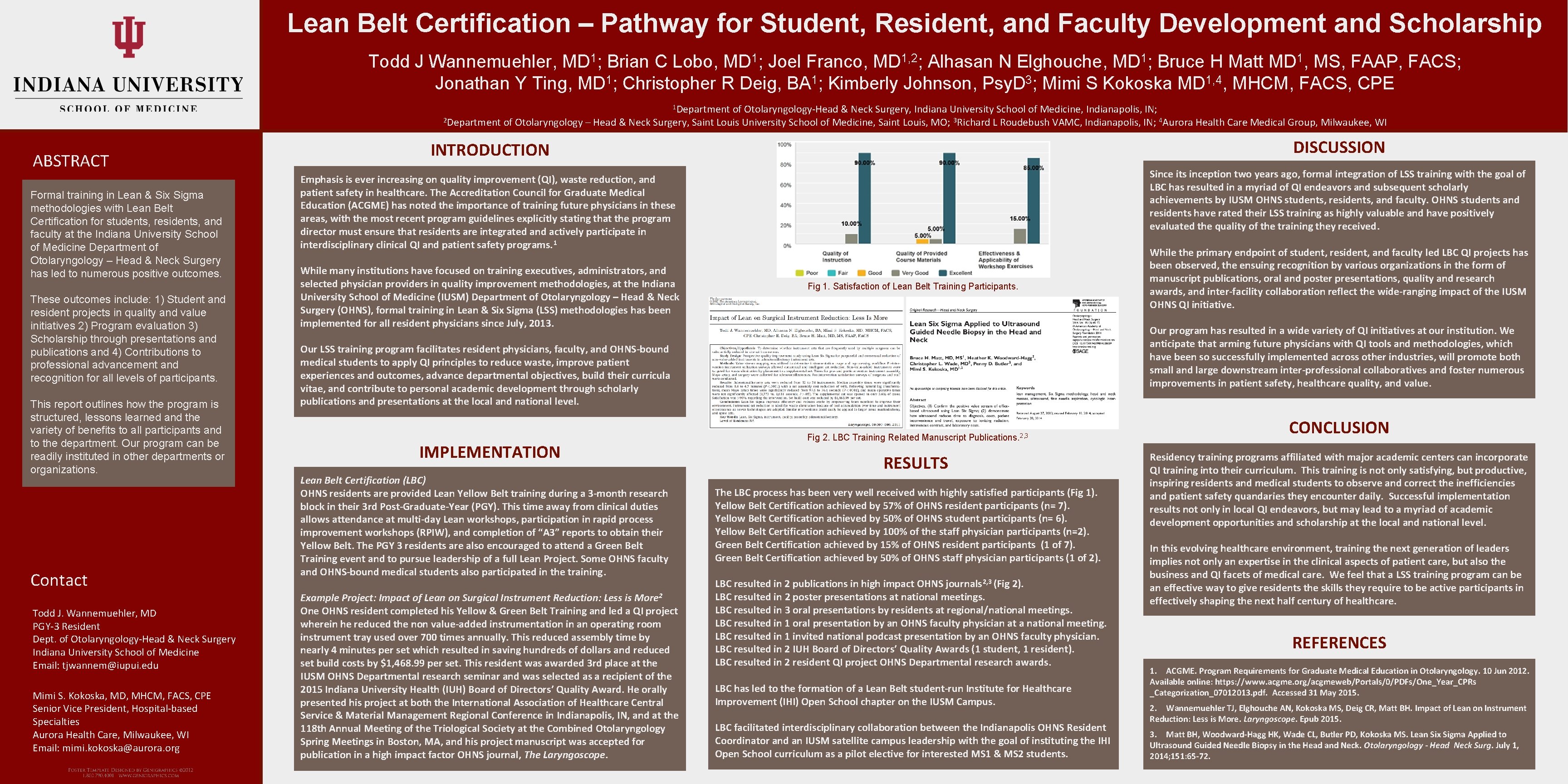
Lean Belt Certification – Pathway for Student, Resident, and Faculty Development and Scholarship Todd J Wannemuehler, MD 1; Brian C Lobo, MD 1; Joel Franco, MD 1, 2; Alhasan N Elghouche, MD 1; Bruce H Matt MD 1, MS, FAAP, FACS; Jonathan Y Ting, MD 1; Christopher R Deig, BA 1; Kimberly Johnson, Psy. D 3; Mimi S Kokoska MD 1, 4, MHCM, FACS, CPE 1 Department of Otolaryngology-Head & Neck Surgery, Indiana University School of Medicine, Indianapolis, IN; 2 Department of Otolaryngology – Head & Neck Surgery, Saint Louis University School of Medicine, Saint Louis, MO; 3 Richard L Roudebush VAMC, Indianapolis, IN; 4 Aurora Health Care Medical Group, Milwaukee, WI ABSTRACT Formal training in Lean & Six Sigma methodologies with Lean Belt Certification for students, residents, and faculty at the Indiana University School of Medicine Department of Otolaryngology – Head & Neck Surgery has led to numerous positive outcomes. These outcomes include: 1) Student and resident projects in quality and value initiatives 2) Program evaluation 3) Scholarship through presentations and publications and 4) Contributions to professional advancement and recognition for all levels of participants. This report outlines how the program is structured, lessons learned and the variety of benefits to all participants and to the department. Our program can be readily instituted in other departments or organizations. Contact Todd J. Wannemuehler, MD PGY-3 Resident Dept. of Otolaryngology-Head & Neck Surgery Indiana University School of Medicine Email: tjwannem@iupui. edu Mimi S. Kokoska, MD, MHCM, FACS, CPE Senior Vice President, Hospital-based Specialties Aurora Health Care, Milwaukee, WI Email: mimi. kokoska@aurora. org INTRODUCTION DISCUSSION Emphasis is ever increasing on quality improvement (QI), waste reduction, and patient safety in healthcare. The Accreditation Council for Graduate Medical Education (ACGME) has noted the importance of training future physicians in these areas, with the most recent program guidelines explicitly stating that the program director must ensure that residents are integrated and actively participate in interdisciplinary clinical QI and patient safety programs. 1 Since its inception two years ago, formal integration of LSS training with the goal of LBC has resulted in a myriad of QI endeavors and subsequent scholarly achievements by IUSM OHNS students, residents, and faculty. OHNS students and residents have rated their LSS training as highly valuable and have positively evaluated the quality of the training they received. While many institutions have focused on training executives, administrators, and selected physician providers in quality improvement methodologies, at the Indiana University School of Medicine (IUSM) Department of Otolaryngology – Head & Neck Surgery (OHNS), formal training in Lean & Six Sigma (LSS) methodologies has been implemented for all resident physicians since July, 2013. Fig 1. Satisfaction of Lean Belt Training Participants. Our program has resulted in a wide variety of QI initiatives at our institution. We anticipate that arming future physicians with QI tools and methodologies, which have been so successfully implemented across other industries, will promote both small and large downstream inter-professional collaboratives and foster numerous improvements in patient safety, healthcare quality, and value. Our LSS training program facilitates resident physicians, faculty, and OHNS-bound medical students to apply QI principles to reduce waste, improve patient experiences and outcomes, advance departmental objectives, build their curricula vitae, and contribute to personal academic development through scholarly publications and presentations at the local and national level. IMPLEMENTATION Lean Belt Certification (LBC) OHNS residents are provided Lean Yellow Belt training during a 3 -month research block in their 3 rd Post-Graduate-Year (PGY). This time away from clinical duties allows attendance at multi-day Lean workshops, participation in rapid process improvement workshops (RPIW), and completion of “A 3” reports to obtain their Yellow Belt. The PGY 3 residents are also encouraged to attend a Green Belt Training event and to pursue leadership of a full Lean Project. Some OHNS faculty and OHNS-bound medical students also participated in the training. Example Project: Impact of Lean on Surgical Instrument Reduction: Less is More 2 One OHNS resident completed his Yellow & Green Belt Training and led a QI project wherein he reduced the non value-added instrumentation in an operating room instrument tray used over 700 times annually. This reduced assembly time by nearly 4 minutes per set which resulted in saving hundreds of dollars and reduced set build costs by $1, 468. 99 per set. This resident was awarded 3 rd place at the IUSM OHNS Departmental research seminar and was selected as a recipient of the 2015 Indiana University Health (IUH) Board of Directors’ Quality Award. He orally presented his project at both the International Association of Healthcare Central Service & Material Management Regional Conference in Indianapolis, IN, and at the 118 th Annual Meeting of the Triological Society at the Combined Otolaryngology Spring Meetings in Boston, MA, and his project manuscript was accepted for publication in a high impact factor OHNS journal, The Laryngoscope. While the primary endpoint of student, resident, and faculty led LBC QI projects has been observed, the ensuing recognition by various organizations in the form of manuscript publications, oral and poster presentations, quality and research awards, and inter-facility collaboration reflect the wide-ranging impact of the IUSM OHNS QI initiative. Fig 2. LBC Training Related Manuscript Publications. 2, 3 RESULTS The LBC process has been very well received with highly satisfied participants (Fig 1). Yellow Belt Certification achieved by 57% of OHNS resident participants (n= 7). Yellow Belt Certification achieved by 50% of OHNS student participants (n= 6). Yellow Belt Certification achieved by 100% of the staff physician participants (n=2). Green Belt Certification achieved by 15% of OHNS resident participants (1 of 7). Green Belt Certification achieved by 50% of OHNS staff physician participants (1 of 2). LBC resulted in 2 publications in high impact OHNS journals 2, 3 (Fig 2). LBC resulted in 2 poster presentations at national meetings. LBC resulted in 3 oral presentations by residents at regional/national meetings. LBC resulted in 1 oral presentation by an OHNS faculty physician at a national meeting. LBC resulted in 1 invited national podcast presentation by an OHNS faculty physician. LBC resulted in 2 IUH Board of Directors’ Quality Awards (1 student, 1 resident). LBC resulted in 2 resident QI project OHNS Departmental research awards. LBC has led to the formation of a Lean Belt student-run Institute for Healthcare Improvement (IHI) Open School chapter on the IUSM Campus. LBC facilitated interdisciplinary collaboration between the Indianapolis OHNS Resident Coordinator and an IUSM satellite campus leadership with the goal of instituting the IHI Open School curriculum as a pilot elective for interested MS 1 & MS 2 students. CONCLUSION Residency training programs affiliated with major academic centers can incorporate QI training into their curriculum. This training is not only satisfying, but productive, inspiring residents and medical students to observe and correct the inefficiencies and patient safety quandaries they encounter daily. Successful implementation results not only in local QI endeavors, but may lead to a myriad of academic development opportunities and scholarship at the local and national level. In this evolving healthcare environment, training the next generation of leaders implies not only an expertise in the clinical aspects of patient care, but also the business and QI facets of medical care. We feel that a LSS training program can be an effective way to give residents the skills they require to be active participants in effectively shaping the next half century of healthcare. REFERENCES 1. ACGME. Program Requirements for Graduate Medical Education in Otolaryngology. 10 Jun 2012. Available online: https: //www. acgme. org/acgmeweb/Portals/0/PDFs/One_Year_CPRs _Categorization_07012013. pdf. Accessed 31 May 2015. 2. Wannemuehler TJ, Elghouche AN, Kokoska MS, Deig CR, Matt BH. Impact of Lean on Instrument Reduction: Less is More. Laryngoscope. Epub 2015. 3. Matt BH, Woodward-Hagg HK, Wade CL, Butler PD, Kokoska MS. Lean Six Sigma Applied to Ultrasound Guided Needle Biopsy in the Head and Neck. Otolaryngology - Head Neck Surg. July 1, 2014; 151: 65 -72.
- Slides: 1