Leah Thornhill NU 522 PICOT EBP PROJECT Effectiveness
Leah Thornhill NU 522 PICOT -EBP PROJECT Effectiveness of the Use of Continuous Bedside Pressure Monitoring for Prevention of Pressure Ulcers as Compared to Standard Techniques
Table of Contents Introduction PICOT Question Literature Review Summary Conclusion Pertaining to the PICOT Question Recommendations for Incorporation of the Evidence into Practice General Conclusion References
INTRODUCTION Impaired skin integrity is a serious problem that fully or partially immobile patients suffer from. Pressure ulcer is the most wide-spread type of impaired skin integrity nowadays. There are more than 2. 5 million cases of pressure ulcer registered in US hospitals annually. Although pressure ulcer is the subject matter of numerous studies, its effective prevention remains largely under researched.
PICOT QUESTION According to Melnyk & Fineout-Overholt (2010), PICOT consists of such elements as: P – population/disease I – intervention or variable of interest C – comparison O – outcome T - time
PICOT QUESTION OF THE PROJECT P: patients that remain immobile for a prolonged period of time, especially senior patients staying at intensive care units; I: use of continuous bedside pressure monitoring; C: use of standard pressure ulcer prevention methods, in particular repositioning; O: a risk of developing pressure ulcers during the hospital stay; T: the period of observation should last at least six months for making credible conclusions on the effectiveness of intervention as compared to the standard procedure.
PICOT QUESTION OF THE PROJECT Meaning of the PICOT question: For immobile patients (P) does the use of continuous bedside pressure monitoring (I) reduce the future risk of pressure ulcer development (C) as compared with the use of standard procedures like repositioning (O) during the hospital stay? (T) time period of observation?
LITERATURE REVIEW SUMMARY Sources relating to the economic aspect of pressure ulcers; Sources relating to definition and typology of pressure ulcers; Sources relating to development and detection of pressure ulcers; Sources relating to prevention and treatment of pressure ulcers.
Sources relating to the economic aspect of pressure ulcers Pressure ulcers are costly both for patients and hospitals. In 2001, the cost of pressure ulcer treatment was from $20, 000 to $50, 000 (Vermette et al. , 2012). Other figures show costs from $5, 000 to $50, 000 (Cooper, 2013). Today, the figure has doubled and amounts in total to more than $2. 4 billion per annum (Siddiqui et al. , 2013). Pressure ulcers are not covered by Medicare and Medicaid.
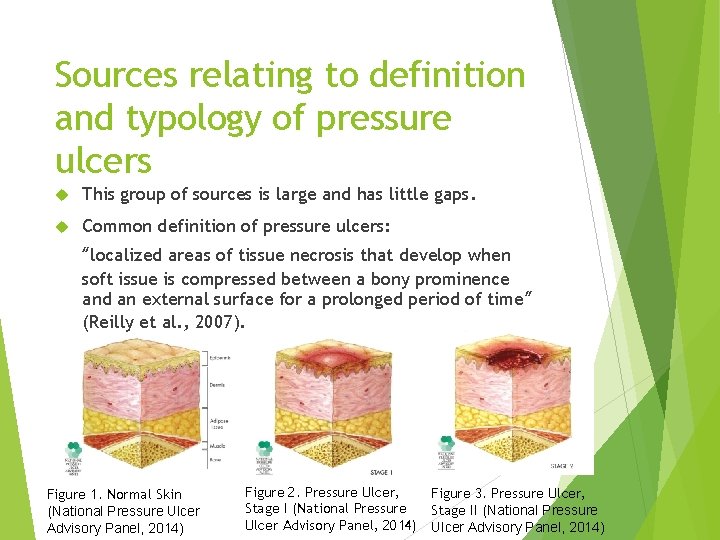
Sources relating to definition and typology of pressure ulcers This group of sources is large and has little gaps. Common definition of pressure ulcers: “localized areas of tissue necrosis that develop when soft issue is compressed between a bony prominence and an external surface for a prolonged period of time” (Reilly et al. , 2007). Figure 1. Normal Skin (National Pressure Ulcer Advisory Panel, 2014) Figure 2. Pressure Ulcer, Figure 3. Pressure Ulcer, Stage I (National Pressure Stage II (National Pressure Ulcer Advisory Panel, 2014)
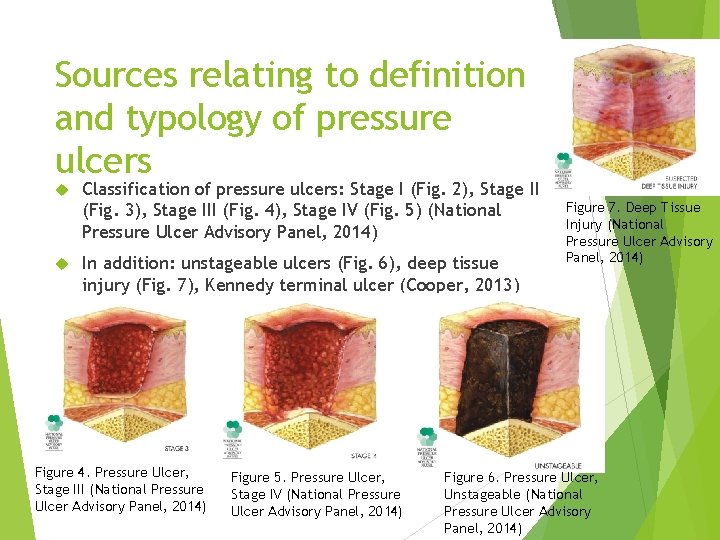
Sources relating to definition and typology of pressure ulcers Classification of pressure ulcers: Stage I (Fig. 2), Stage II (Fig. 3), Stage III (Fig. 4), Stage IV (Fig. 5) (National Pressure Ulcer Advisory Panel, 2014) In addition: unstageable ulcers (Fig. 6), deep tissue injury (Fig. 7), Kennedy terminal ulcer (Cooper, 2013) Figure 4. Pressure Ulcer, Stage III (National Pressure Ulcer Advisory Panel, 2014) Figure 5. Pressure Ulcer, Stage IV (National Pressure Ulcer Advisory Panel, 2014) Figure 7. Deep Tissue Injury (National Pressure Ulcer Advisory Panel, 2014) Figure 6. Pressure Ulcer, Unstageable (National Pressure Ulcer Advisory Panel, 2014)
Sources relating to development and detection of pressure ulcers Pressure ulcers develop because of the impact of body weight on skin, shear, pressure, and friction in fully or partially immobile patients. Risk factors: aging; moisture; pressure; malnutrition; incontinence; neurologic diseases; tissue ischemia (Stojadinovic et al. , 2013) Pressure ulcers can develop only after 2 hours of immobility. Aging skin is at higher risk due to a decrease in NLRP 3 inflammasome proteins (Stojadinovic et al. , 2013). Because of molecular composition and decreased collagen levels of aging skin, sometimes it cannot be prevented.
Sources relating to detection and development of pressure ulcers Sources on detection focus on manual detection and use of equipment and laboratory tests. Manual detection occurs during repositioning. Some studies suppose that laboratory tests can help with detection, e. g. through levels of Ca++ and elevated levels of CK (Gefen et al. , 2013). Ultrasound equipment is promising for detection of pressure ulcers, especially of deep tissue injury.
Sources relating to prevention and treatment of pressure ulcers Prevention is more important than intervention. Special wheelchair cushions and matrasses are more effective than standard bed matrasses and segmented foam cushions (Brienza et al. , 2010). Pressure redistribution matrasses and low-air-loss matrasses in ICUs (Cooper, 2013). HSF matrasses with “strategically designed foam segments and select indentation force deflection” (Vermette et al. , 2012). A lower number of incontinence pads and linens on lowair-loss surfaces decrease chances of pressure ulcer development (Williamson et al. , 2013).
Sources relating to prevention and treatment of pressure ulcers Prevention and treatment require risk assessment instruments. The Braden Scale is the most prevalent instrument in the USA (Reilly et al. , 2007). Other popular instruments include Norton Scale, Cornell Ulcer Risk Score, and Jackson/Cubbin Scale (Reilly et al. , 2007). Standard recommendation of the National Pressure Ulcer Advisory Panel: repositioning or turning of fully or partially immobile patients every two hours.
Continuous Bedside Pressure Monitoring Systems CBPM systems are today the most innovative and effective prevention technique (Hand, 2013). One of such systems is called MAP by Wellsense and costs $80, 000 per 20 UCI beds (Hand, 2013). Nurses report 90% satisfaction with MAP CBPM system. Other CBPM system trial results are remarkable: 1 patient with pressure ulcer (0. 3%) in CBPM group versus 16 patients with pressure ulcer (5%) over the trial period (Siddiqui et al. , 2013). CBPM systems give real-time feedback to medical practitioners on repositioning and body parts at risk of pressure ulcer development.
CONCLUSION PERTAINING TO THE PICOT QUESTION As mentioned before, the PICOT question of the current project is: For immobile patients (P) does the use of continuous bedside pressure monitoring (I) reduce the future risk of pressure ulcer development (C) as compared with the use of standard procedures like repositioning (O) during the hospital stay? Answer is as follows: Yes, the use of continuous bedside pressure monitoring reduces the future risk of pressure ulcer development as compared with the use of standard procedures like repositioning during the hospital stay.
RECOMMENDATIONS FOR INCORPORATION OF THE EVIDENCE INTO PRACTICE To consider the CBPM system as the best practice currently available in terms of pressure ulcer prevention; To install CBPM systems in hospitals and especially in intensive care units Figure 8. MAP CBPM System (American Israeli Medical Association, 2014)
RECOMMENDATIONS FOR INCORPORATION OF THE EVIDENCE INTO PRACTICE However, implementation of the CBPM system is only a part of the solution. Human factor is essential. Implementation of such systems does not mean that hospitals should abandon all other available pressure ulcer prevention instruments like specialized matrasses, wheelchair cushions. Further trials are necessary to prove efficiency and effectiveness of the CBPM system. Training of nurses is required for smooth functioning of implemented systems
GENERAL CONCLUSION Impaired skin integrity is a serious problem for patients bound to bed and wheelchair. Prevention seems to be a better choice than treatment as it is less costly and damaging for the patient. The CBMP system may be deemed the best currently existing solution for prevention of pressure ulcers. Additional studies of the system are required to prove its efficiency and supposedly improve its functional capabilities.
References American Israeli Medical Association. (2014). Israeli technology helps patients with pressure ulcers. Blog. Retrieved from http: //www. aima 4 u. com/israelitechnology-helps-patients-with-pressure-ulcers/ Brienza, D. , Kelsey, S. , Karg, P. , Allegretti, A. , Olson, M. , Schmeler, M. , Zanca, J. , Geyer, M. J. , Kusturiss, M. , & Holm, M. (2010). A randomized clinical trial on preventing pressure ulcers with wheelchair seat cushions. Journal of the American Geriatrics Society, 58 (12), 2308– 2314. Cooper, K. L. (2012, December). Evidence-based prevention of pressure ulcers in the intensive care unit. Critical Care Nurse, 33 (6), 57– 66.
References Gefen, A. , Farid, K. J. , & Shaywitz, I. (2013, February). A review of deep tissue injury development, detection, and prevention: Shear savvy. Ostomy Wound Management, 59 (2), 26– 35. Hand, L. (2013, December 19). Pressure-monitoring tool may decrease pressure ulcers in ICU. Medscape. Retrieved from http: //www. medscape. com/viewarticle/818104#vp_1 Melnyk B. , & Fineout-Overholt E. (2010). Evidence-based practice in nursing & healthcare. New York: Lippincott Williams & Wilkins.
References National Pressure Ulcer Advisory Panel. (2014). NPUAP pressure ulcer stages/categories. Educational and Clinical Resources. Retrieved from http: //www. npuap. org/resources/educational-andclinical-resources/npuap-pressure-ulcerstagescategories/ Reilly, E. F. , Karakousis, G. C. , Schrag, S. P. , & Stawicki, S. P. (2007). Pressure ulcers in the intensive care unit: The ‘forgotten’ enemy. Scientist, 1 (2), 17– 30. Siddiqui, A. , Behrendt, R, Lafluer, M. , & Craft, S. (2013). A continuous bedside pressure mapping system for prevention of pressure ulcer development in the medical ICU: A retrospective analysis. Wounds, 25 (12), 333– 339.
References Stojadinovic, O. , Minkiewicz, J. , Sawaya, A. , Bourne, J. W. , Torzilli, P. , de Rivero Vaccari, J. P. , Dietrich, W. D. , Keane, R. W. , & Tomic-Canic, M. (2013). Deep tissue injury in development of pressure ulcers: A decrease of inflammasome activation and changes in human skin morphology in response to aging and mechanical load. PLo. S ONE, 8 (8), e 69223. Vermette, S. , Reeves, I. , & Lemaire, J. (2012). Cost effectiveness of an air-inflated static overlay for pressure ulcer prevention: A randomized, controlled trial. Wounds, 24 (8), 207– 214. Williamson, R. , Lachenbruch, C. , & Van. Gilder, C. (2013). A laboratory study examining the impact of linen use on low-air-loss support surface heat and water vapor transmission rates. Ostomy Wound Management, 59 (8), 32– 41.
- Slides: 23