Layout Key Definitions Executive summary Introduction Part One



- Slides: 29
Layout • Key Definitions • Executive summary • Introduction • Part One: General Preventive Measures • Part Two: EMS Specific Procedures • Annexures
Definitions Emergency Medical Services: a system of care with linked and interdependent components: prehospital care (including transportation) and care at the hospital. All components must work together to make a lasting impact on the health of a population (Kobusingye et al. , 2006). Pre- Hospital Care: It is defined as care provided in the community (at home, school, work or recreation area) until the patient arrives at a formal health-care facility capable of providing definitive care comprising basic strategies with proven effectiveness, such as accessible and rapid transportation and the deployment of personnel with basic life-support skills (Kobusingye et al. , 2006).
Definitions Standard Ambulance care team § Minimum of a trained driver and ambulance assistant. § Ambulance vehicle with separated patient and driver compartments. § Equipped with PPEs – Service provider and Patient. § Diagnostic and patient care equipment, medicines and supplies. § External and internal communication systems. § Linked to medical control.
Definitions Types of Ambulances: • Type A: Provides most basic care. No IV access • Type B: Simple treatment and able to provide IV treatment. • Type C: Advanced Life Support
Executive Summary In December 2019, an outbreak of a highly infectious pneumonia of unknown cause was declared in Wuhan city, China. On the 7 th of January 2020, the causative pathogen was identified as a novel coronavirus (2019 n. Co. V)/COVID-19/SARS-Cov 200. Following rapid global spread and mortality, COVID-19 was declared a global pandemic by WHO. On 18 th March 2020, H. E the President of Uganda declared COVID-19 a national emergency and put in place several measures to control the pandemic. The Ministry of Health has developed the National Prehospital Emergency Medical Services (EMS) Covid 19 Guidelines that provide guidance for EMS preparedness and response to COVID-19 in the prehospital setting in Uganda. These guidelines are aligned with current national and global recommendations and also consideration for the prehospital context in Uganda. Despite the risks and challenges, GOU is committed to not only providing a continuous professional prehospital ambulance service for both COVID-19 and none COVID-19 emergencies, but also ensuring the safety and wellbeing of EMS teams. These guidelines provide information for an organised coordinated and integrated and functionalized EMS system both Regional and National level. The National Prehospital Emergency Medical Services (EMS) Covid-19 Guidelines are intended for frontline EMS personnel providing care of patients in the community and during transportation on ambulances to health facilities. They provide practical guidance to these health workers that ensure safety while providing standard quality pre-hospital care. I would like to extend appreciation to the Korean Foundation for International Healthcare (KOFIH), who provided the funding for the development of these guidelines. Technical input was provided by experts from the Emergency Care Society Uganda, World Health Organization and Association of Ambulance Professionals Uganda. Special mention goes to the Department of Emergency Medical Services-Mo. H who provided guidance throughout the process. Dr. Henry Mwebesa Director General Health Services, MOH
EMS UNIQUE CHALLENGES: a) b) c) d) e) Uncontrolled environment( unlike a healthcare facility) Enclosed space during transport Frequent need for rapid medical decision-making Interventions with limited Information Varying range of patient acuity and healthcare resources
REVIEW OF CDC GUIDANCE FOR EMS • Emergency medical dispatchers(EMDs) should question callers and determine the possibility that this call concerns a person who may have signs, symptoms and risk factors for COVID-19 • EMDs should USE NAS COVID-19 CHECKLIST to screen ALL calls. • And appropriately inform crew and destination COVID-19 treatment facility • That they may be caring for, transporting or receiving a patient who may have COVID-19 infection
CDC GUIDANCE FOR EMS • Patient should then be transported as a person under investigation(PUI) using standard precautions for COVID-19 • Facemask should be worn by the patient for source control • Single pair of appropriate size gloves is appropriate(change when torn or soiled) • N-95 respirator or higher-level respirator or facemask(if respirator is not available) • N-95 respirators or other high level respirators(N-100) OR FFP 2 OR FFP 3(Filtering Face Piece) should be used instead of facemask when performing or present for an aerosol-generating procedure • Aerosol generating procedures(intubation, oropharyngeal & oropharyngeal swabs, O 2 administration etc
CDC GUIDANCE FOR EMS • Eye protection( googles or disposable face shield that fully covers the front and sides of the face ) • Personal eye glasses and eye-contacts are NOT considered adequate eye protection.
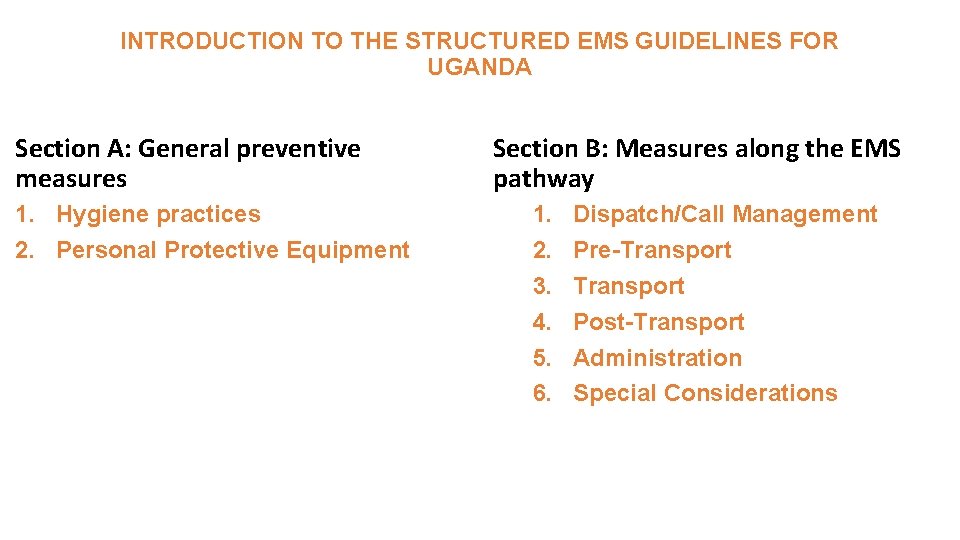
INTRODUCTION TO THE STRUCTURED EMS GUIDELINES FOR UGANDA Section A: General preventive measures 1. Hygiene practices 2. Personal Protective Equipment Section B: Measures along the EMS pathway 1. 2. 3. 4. 5. 6. Dispatch/Call Management Pre-Transport Post-Transport Administration Special Considerations
Part One: General Preventive Measures
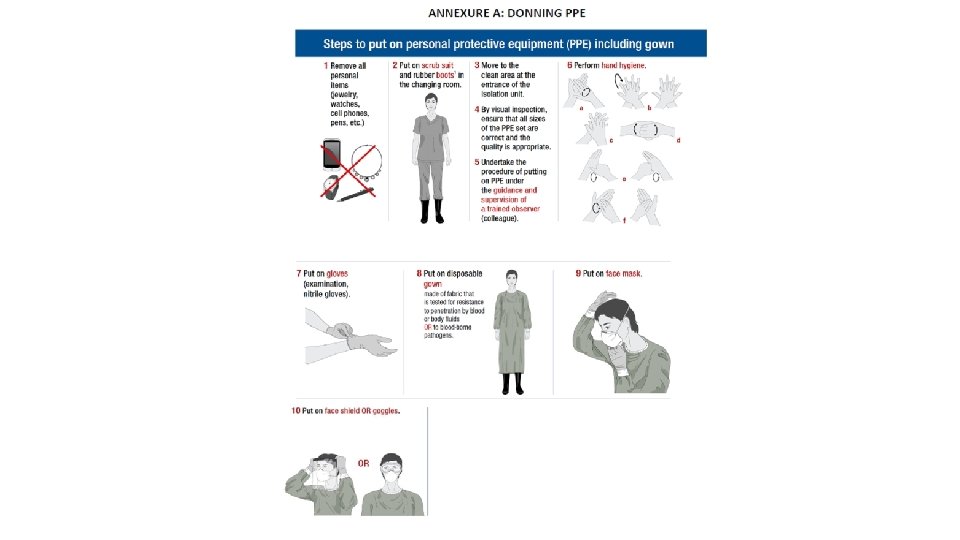
Part One: General Preventive Measures 1. Hygiene Practices 1. 1 Hand Hygiene 1. 2 Coughing And Sneezing 2. Personal Protective Equipment 2. 1 Recommended PPE For Different Risk Categories


Part Two: EMS Specific Procedures
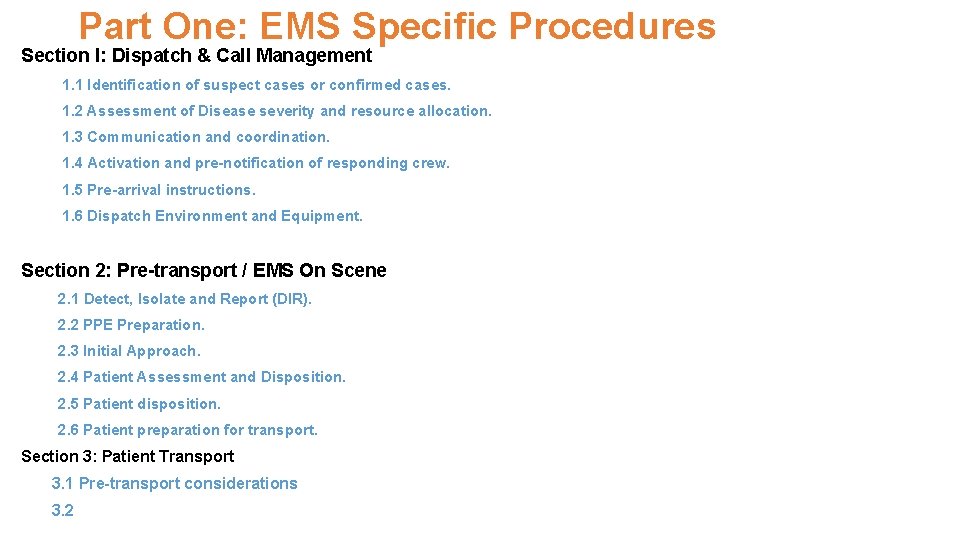
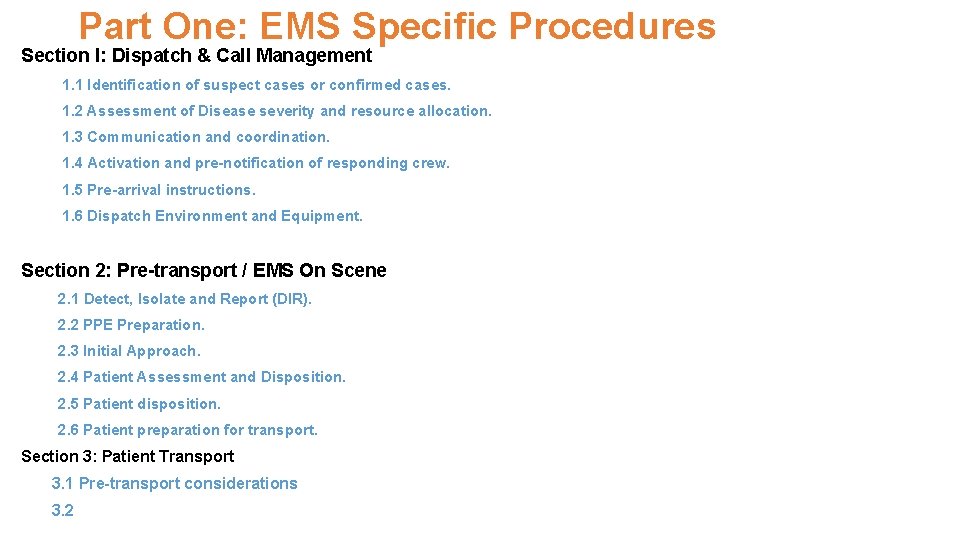
Part One: EMS Specific Procedures Section I: Dispatch & Call Management 1. 1 Identification of suspect cases or confirmed cases. 1. 2 Assessment of Disease severity and resource allocation. 1. 3 Communication and coordination. 1. 4 Activation and pre-notification of responding crew. 1. 5 Pre-arrival instructions. 1. 6 Dispatch Environment and Equipment. Section 2: Pre-transport / EMS On Scene 2. 1 Detect, Isolate and Report (DIR). 2. 2 PPE Preparation. 2. 3 Initial Approach. 2. 4 Patient Assessment and Disposition. 2. 5 Patient disposition. 2. 6 Patient preparation for transport. Section 3: Patient Transport 3. 1 Pre-transport considerations 3. 2
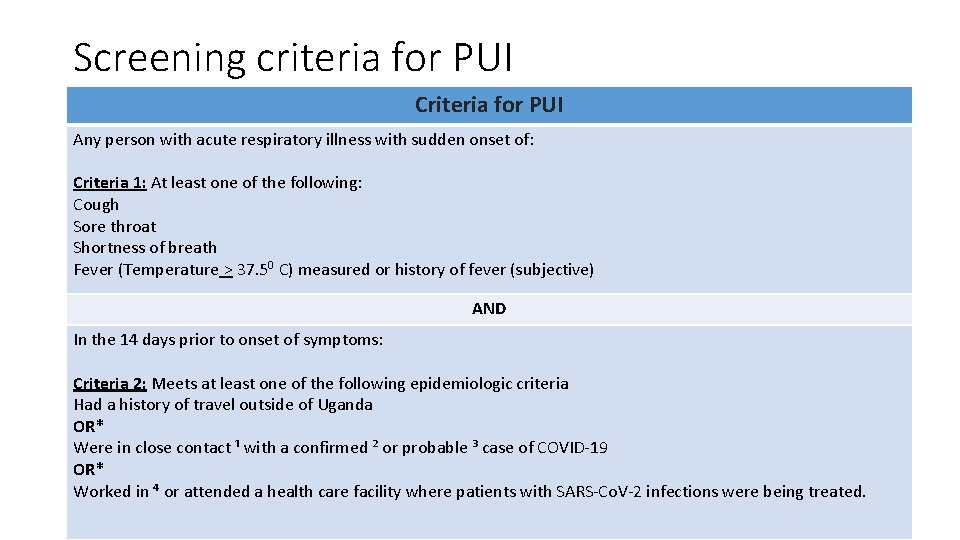
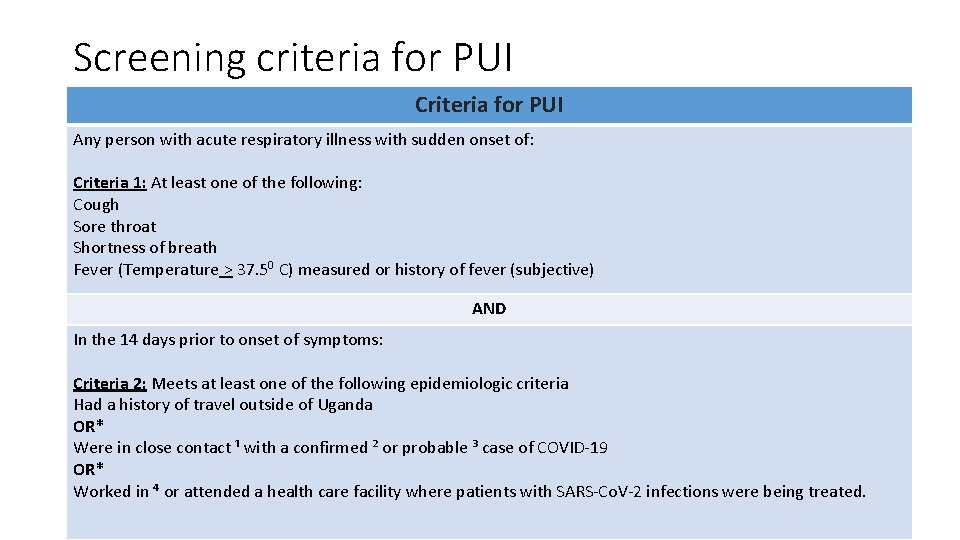
Screening criteria for PUI Criteria for PUI Any person with acute respiratory illness with sudden onset of: Criteria 1: At least one of the following: Cough Sore throat Shortness of breath Fever (Temperature > 37. 50 C) measured or history of fever (subjective) AND In the 14 days prior to onset of symptoms: Criteria 2: Meets at least one of the following epidemiologic criteria Had a history of travel outside of Uganda OR* Were in close contact ¹ with a confirmed ² or probable ³ case of COVID-19 OR* Worked in ⁴ or attended a health care facility where patients with SARS-Co. V-2 infections were being treated.
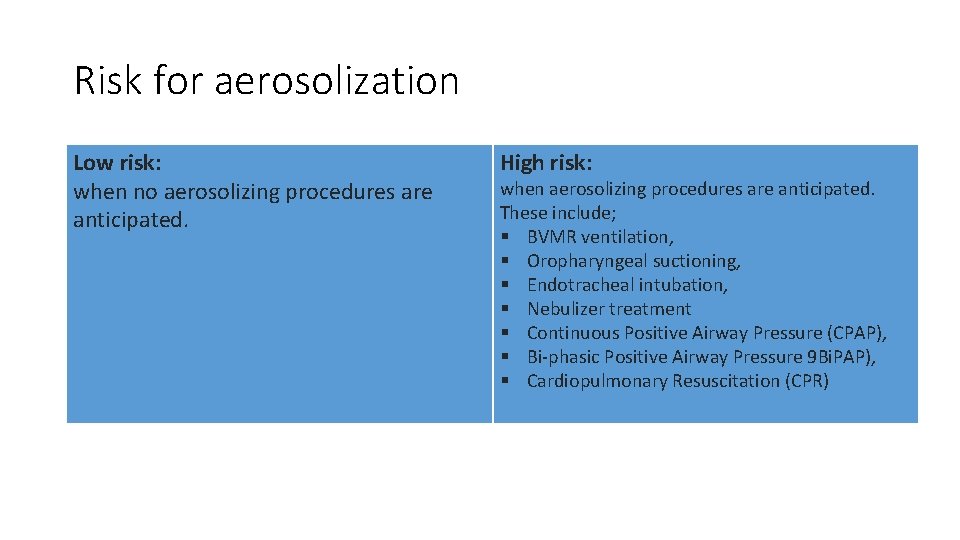
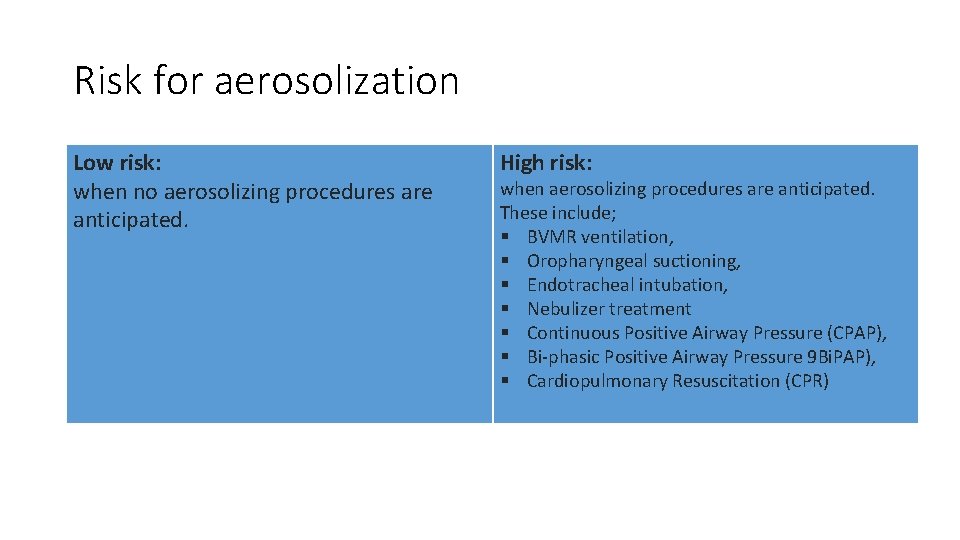
Risk for aerosolization Low risk: when no aerosolizing procedures are anticipated. High risk: when aerosolizing procedures are anticipated. These include; § BVMR ventilation, § Oropharyngeal suctioning, § Endotracheal intubation, § Nebulizer treatment § Continuous Positive Airway Pressure (CPAP), § Bi-phasic Positive Airway Pressure 9 Bi. PAP), § Cardiopulmonary Resuscitation (CPR)
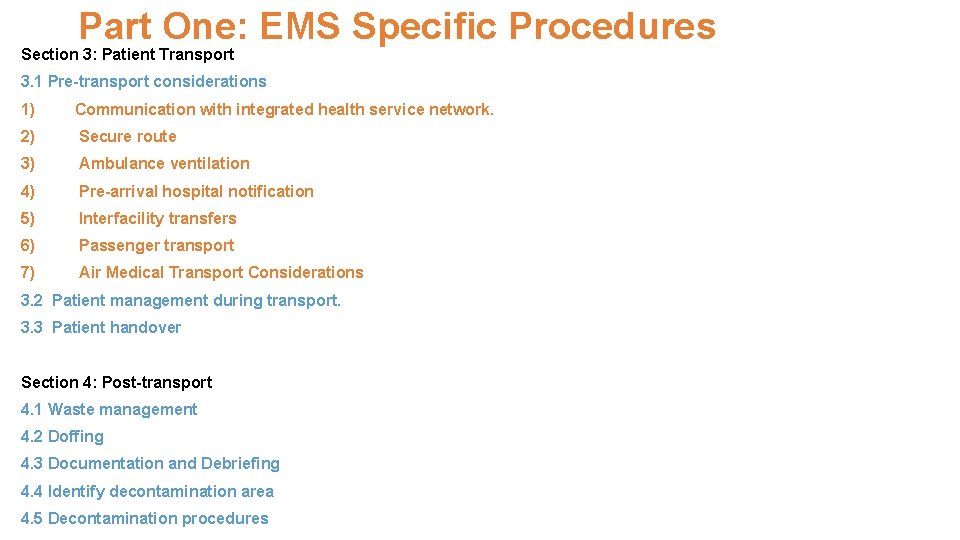
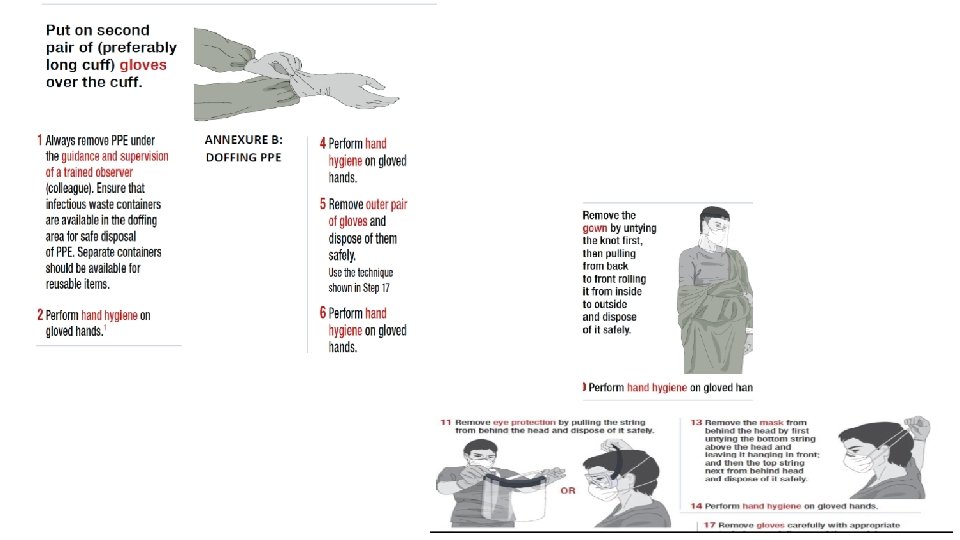
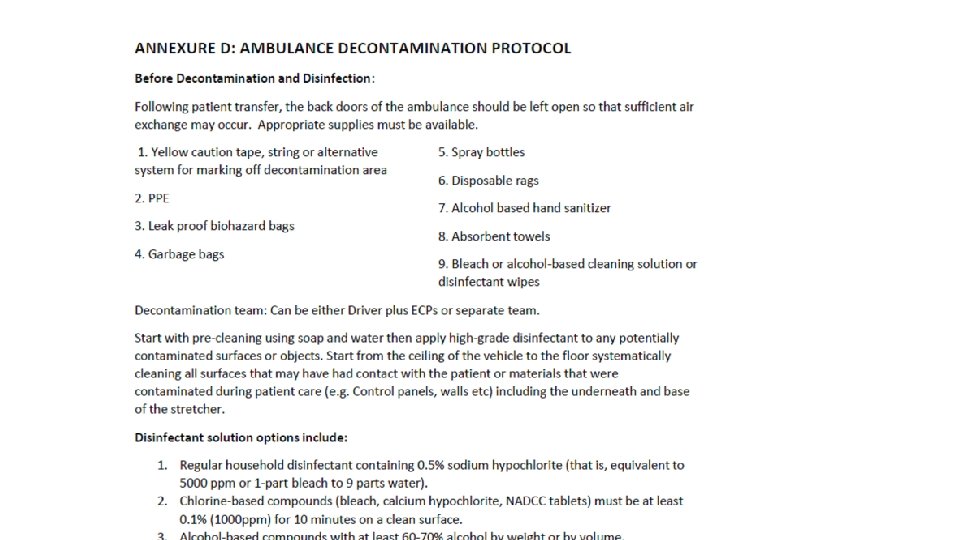
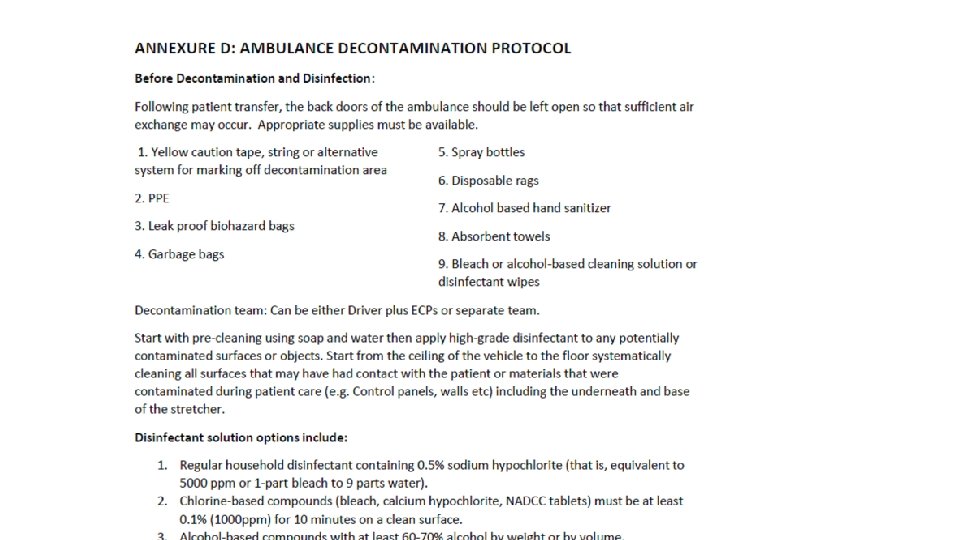
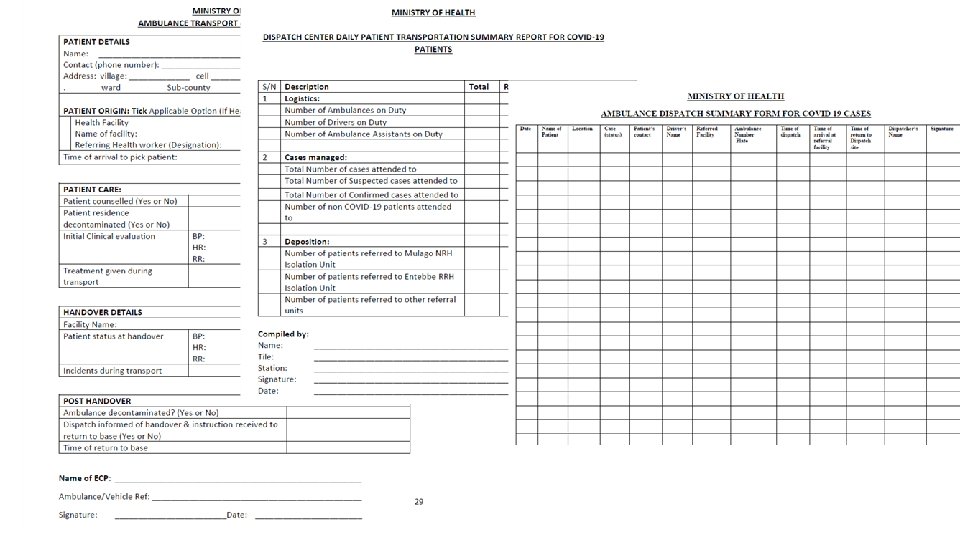
Part One: EMS Specific Procedures Section 3: Patient Transport 3. 1 Pre-transport considerations 1) Communication with integrated health service network. 2) Secure route 3) Ambulance ventilation 4) Pre-arrival hospital notification 5) Interfacility transfers 6) Passenger transport 7) Air Medical Transport Considerations 3. 2 Patient management during transport. 3. 3 Patient handover Section 4: Post-transport 4. 1 Waste management 4. 2 Doffing 4. 3 Documentation and Debriefing 4. 4 Identify decontamination area 4. 5 Decontamination procedures
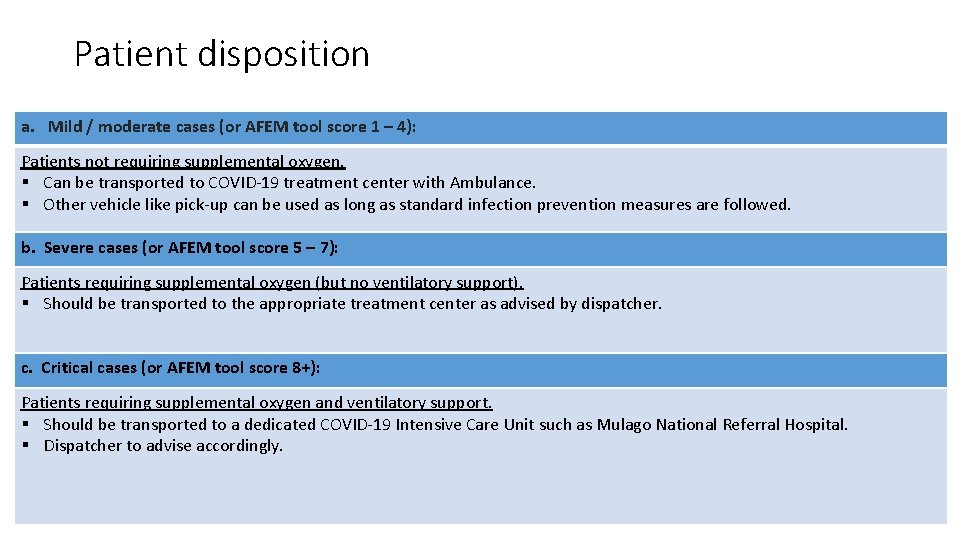
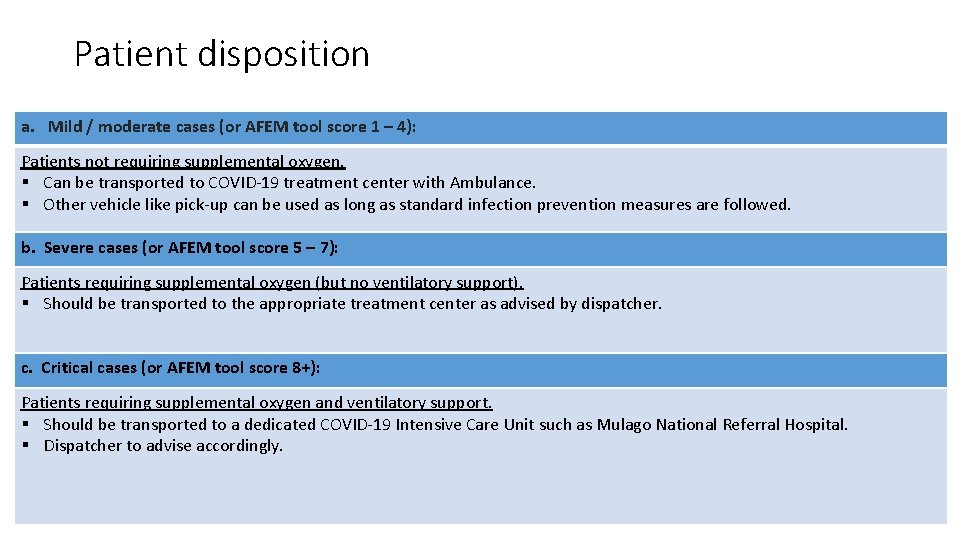
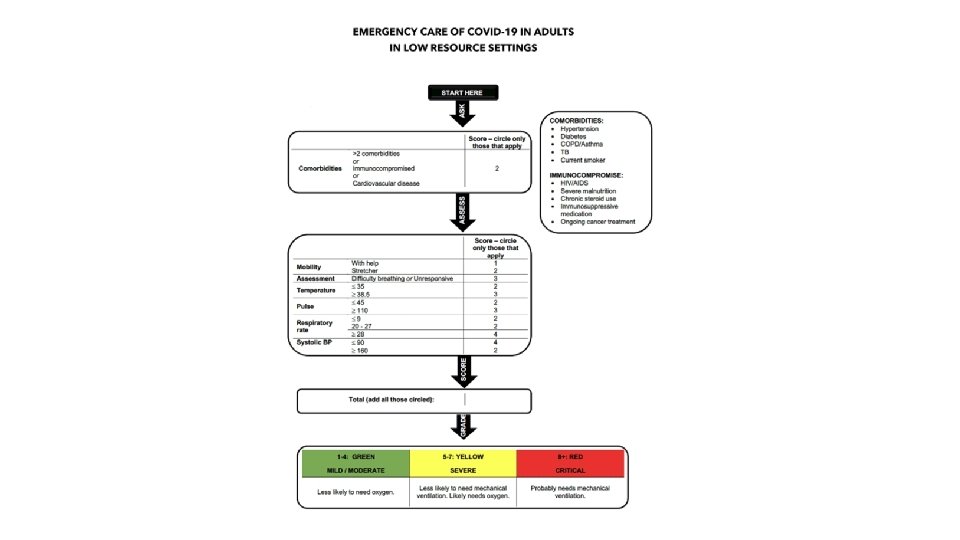
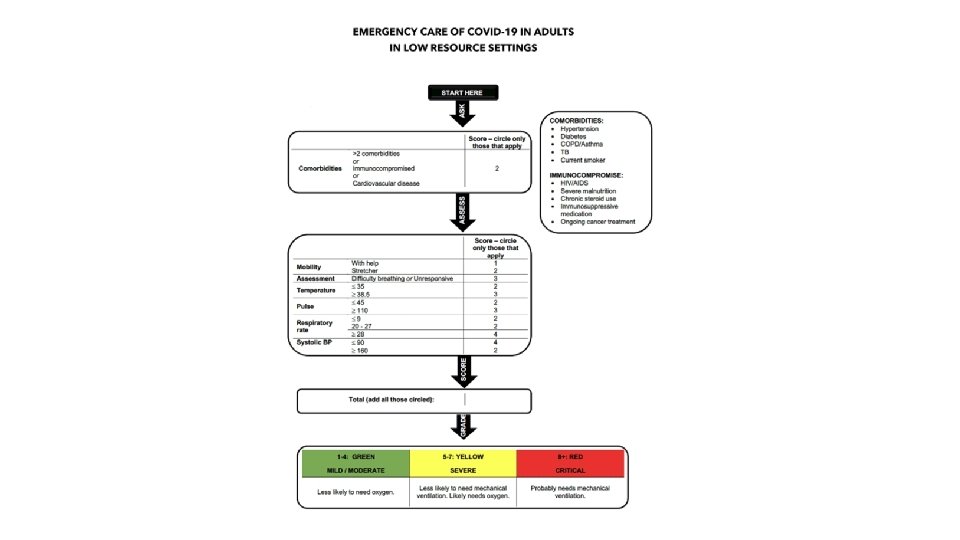
Patient disposition a. Mild / moderate cases (or AFEM tool score 1 – 4): Patients not requiring supplemental oxygen. § Can be transported to COVID-19 treatment center with Ambulance. § Other vehicle like pick-up can be used as long as standard infection prevention measures are followed. b. Severe cases (or AFEM tool score 5 – 7): Patients requiring supplemental oxygen (but no ventilatory support). § Should be transported to the appropriate treatment center as advised by dispatcher. c. Critical cases (or AFEM tool score 8+): Patients requiring supplemental oxygen and ventilatory support. § Should be transported to a dedicated COVID-19 Intensive Care Unit such as Mulago National Referral Hospital. § Dispatcher to advise accordingly.
Part One: EMS Specific Procedures Section 5: Administration 5. 1 Setting up a Call & Dispatch centre 5. 2 Call centre maintenance and hygiene 5. 3 Protocols and training 5. 4 Communication among providers 5. 5 Safety/security and environment 5. 6 Public communication 5. 7 Ambulance supplies and procedures 5. 8 Follow-up and/or reporting measures Section 6: Special Considerations 6. 1 Paediatric Considerations. 6. 2 Geriatric Considerations 6. 3 Considerations for Persons Living with Disability 6. 4 Dead body management
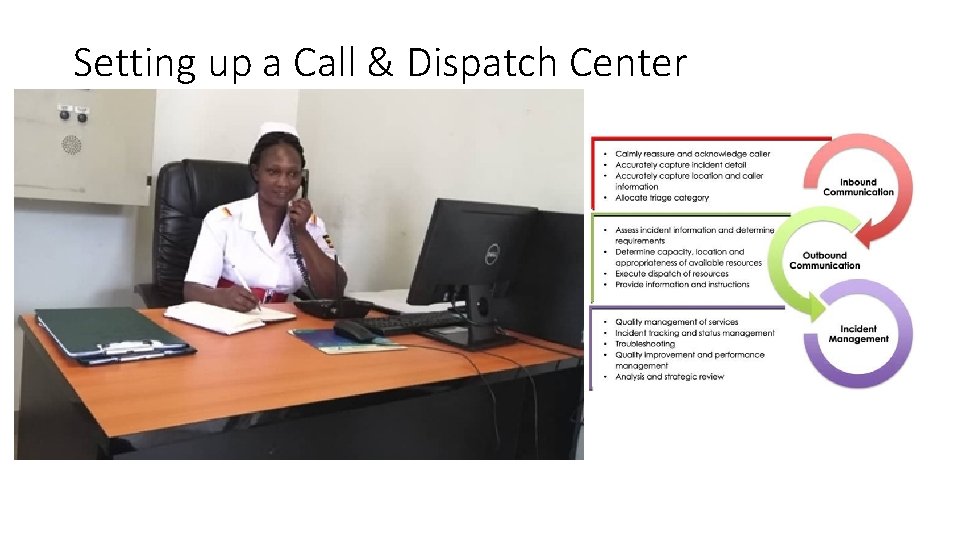
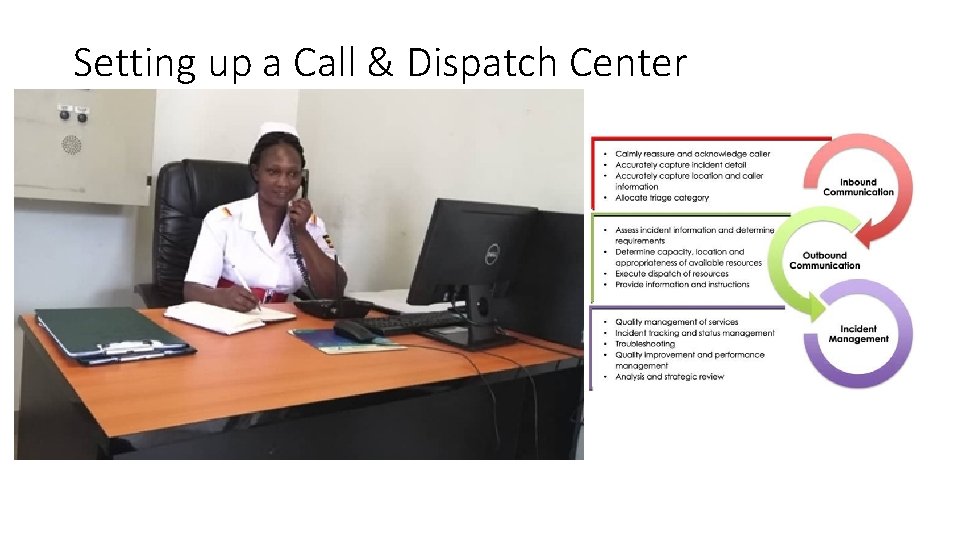
Setting up a Call & Dispatch Center

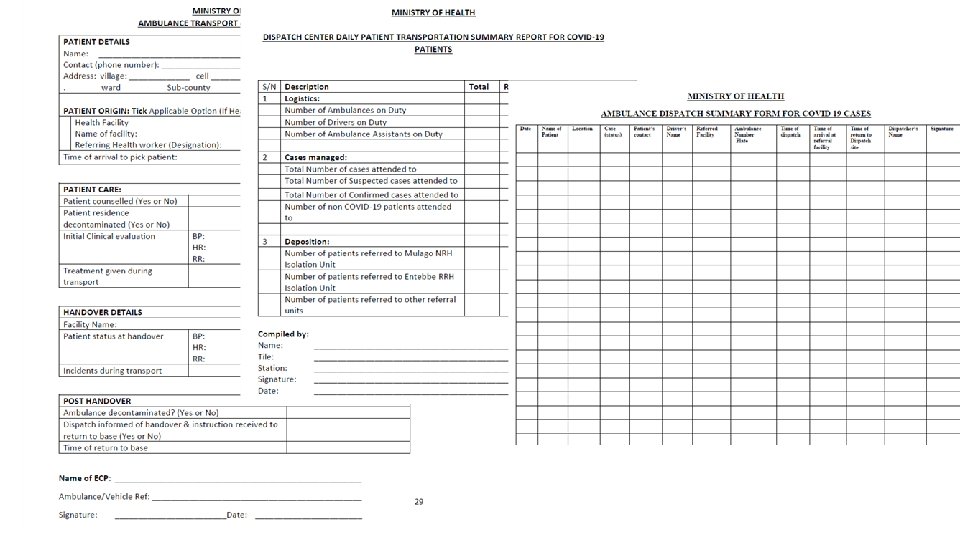
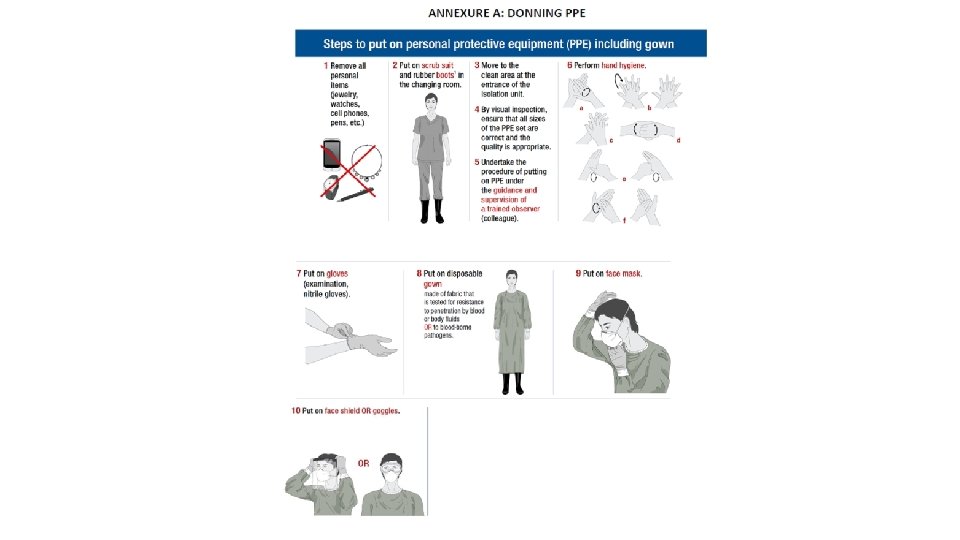
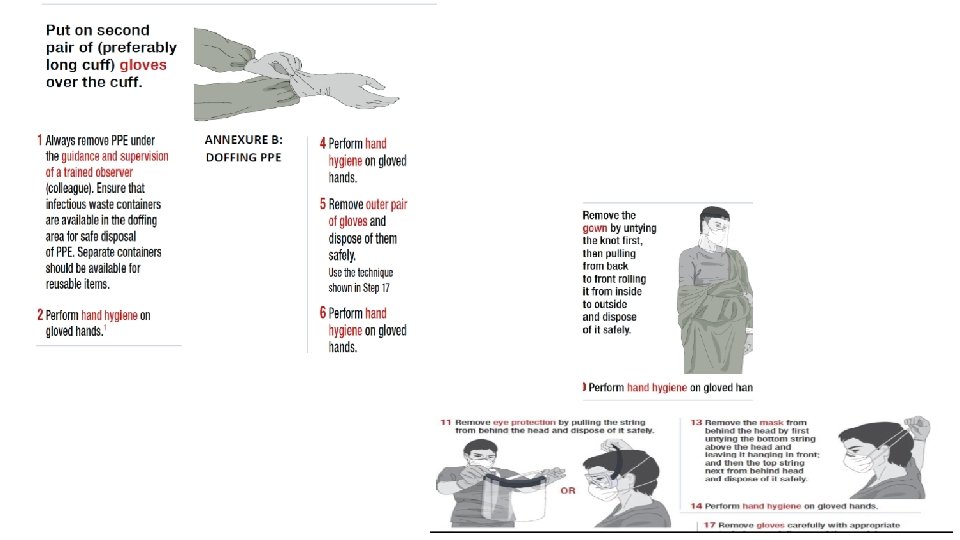
ANNEXURES
Thank you….