Lateral neck dissection for papillary thyroid cancer Joint
- Slides: 39
Lateral neck dissection for papillary thyroid cancer Joint hospital Surgical Grand Round 19 October 2013 Dr. Dennis CT Lam United Christian Hospital
Outline � � � Introduction Lateral neck dissection (LND) for PTC Indication of LND Extent of LND Morbidity of LND Conclusion
Introduction � � Papillary thyroid cancer (PTC) composed of 77 -85% of thyroid malignancies Strong propensity for regional LN involvement A National Cancer Data Base report on 53, 856 cases of thyroid carcinoma treated in the U. S. , 1985– 1995. Hundahl SA, et al. Cancer 1998.
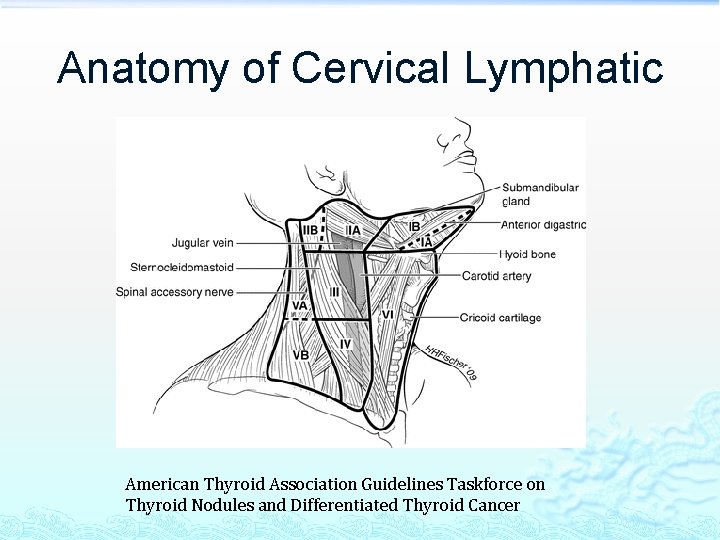
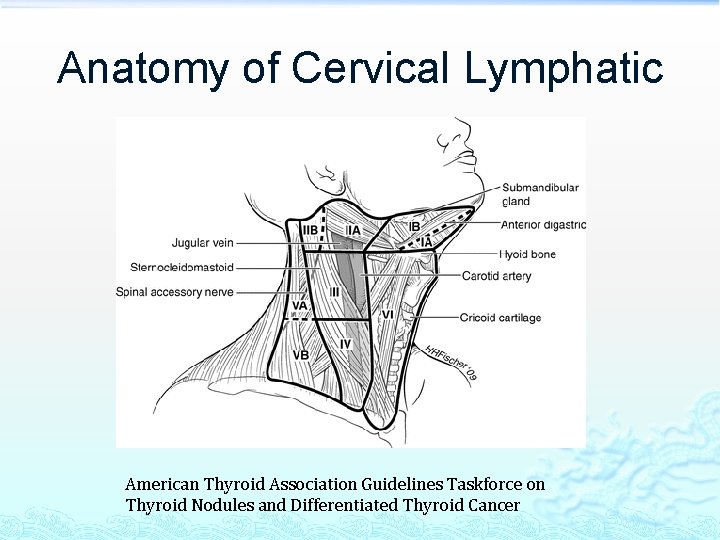
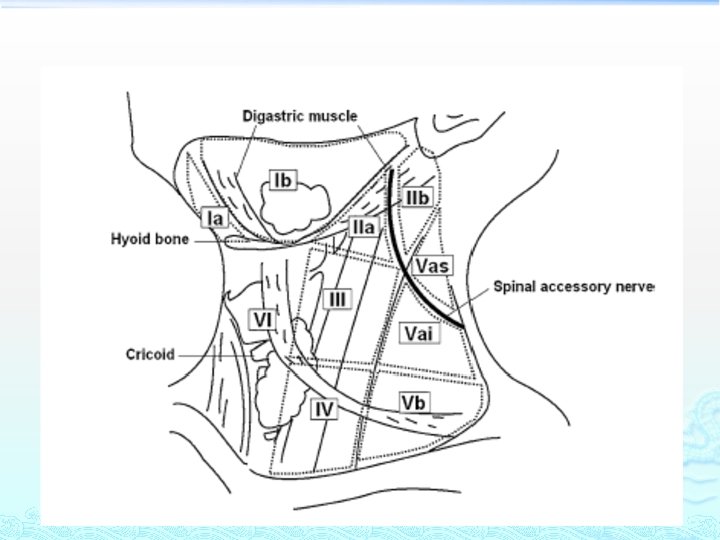
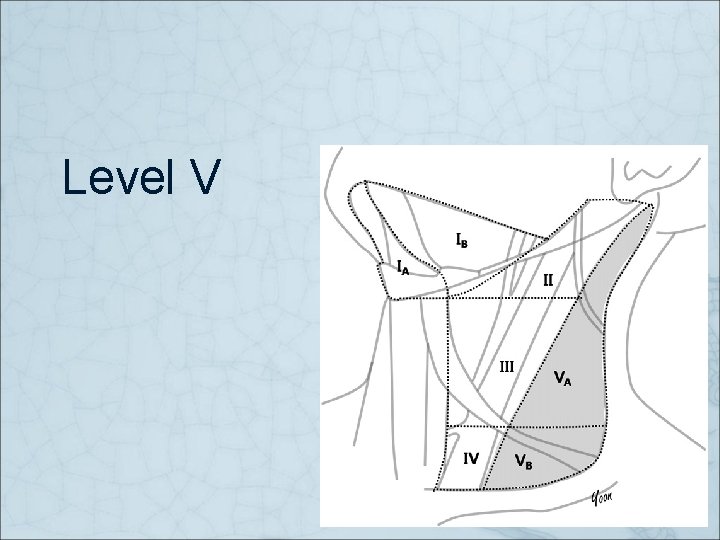
Anatomy of Cervical Lymphatic American Thyroid Association Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer
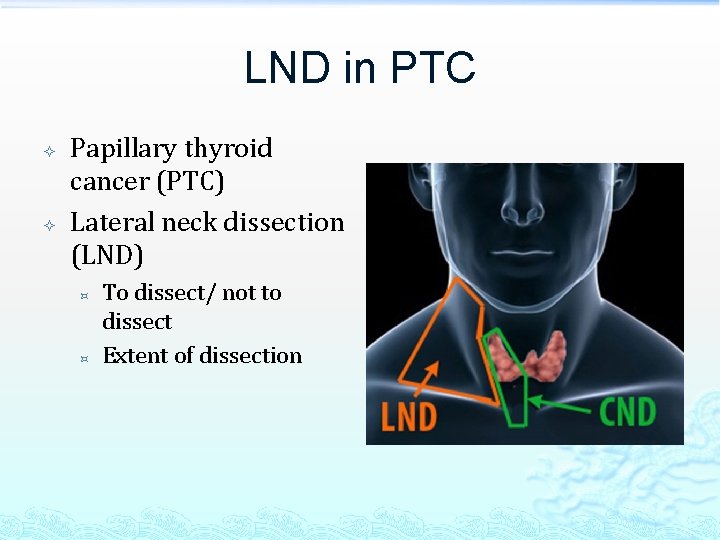
LND in PTC Papillary thyroid cancer (PTC) Lateral neck dissection (LND) ³ ³ To dissect/ not to dissect Extent of dissection
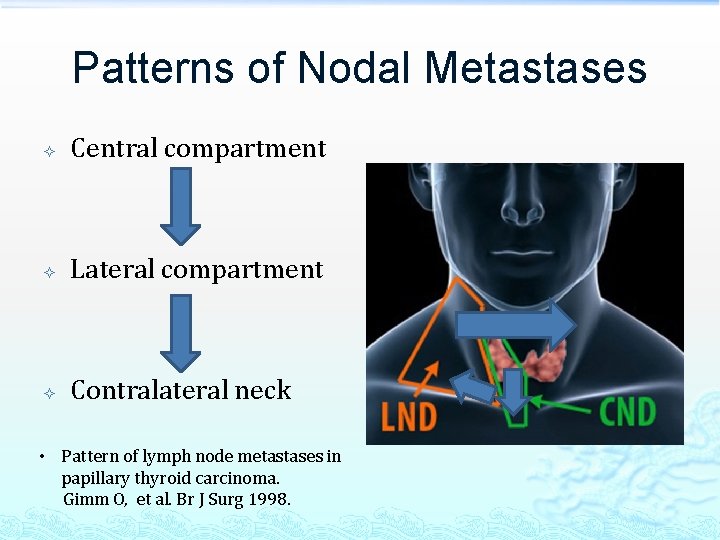
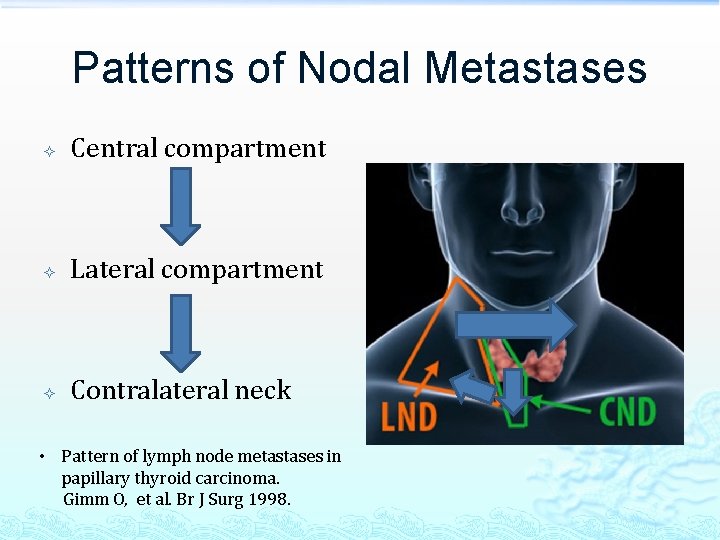
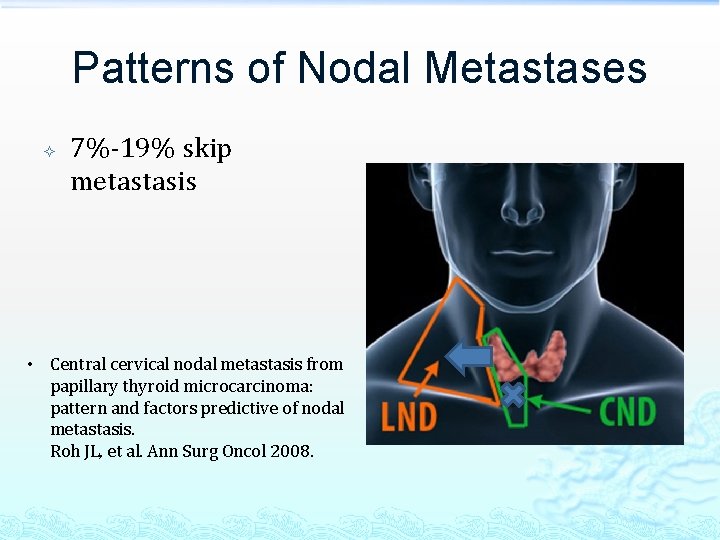
Patterns of Nodal Metastases Central compartment Lateral compartment Contralateral neck • Pattern of lymph node metastases in papillary thyroid carcinoma. Gimm O, et al. Br J Surg 1998.
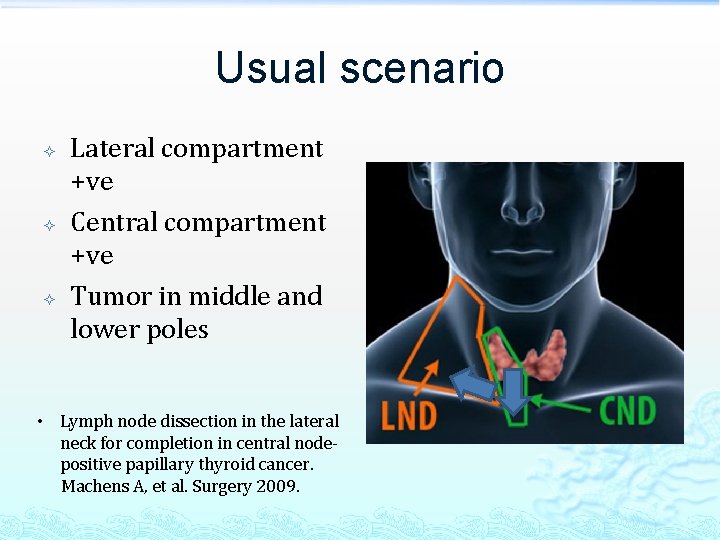
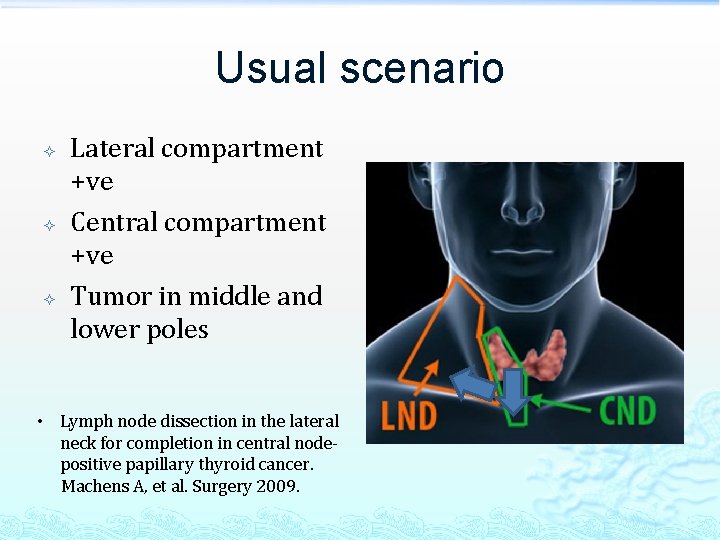
Usual scenario Lateral compartment +ve Central compartment +ve Tumor in middle and lower poles • Lymph node dissection in the lateral neck for completion in central nodepositive papillary thyroid cancer. Machens A, et al. Surgery 2009.
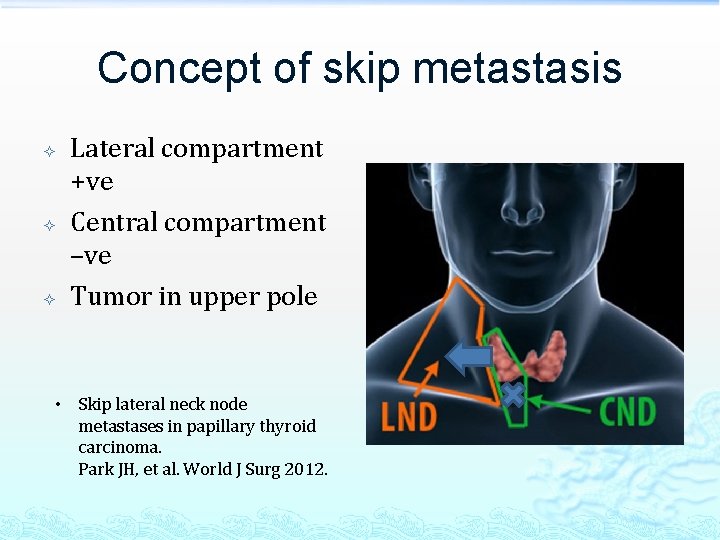
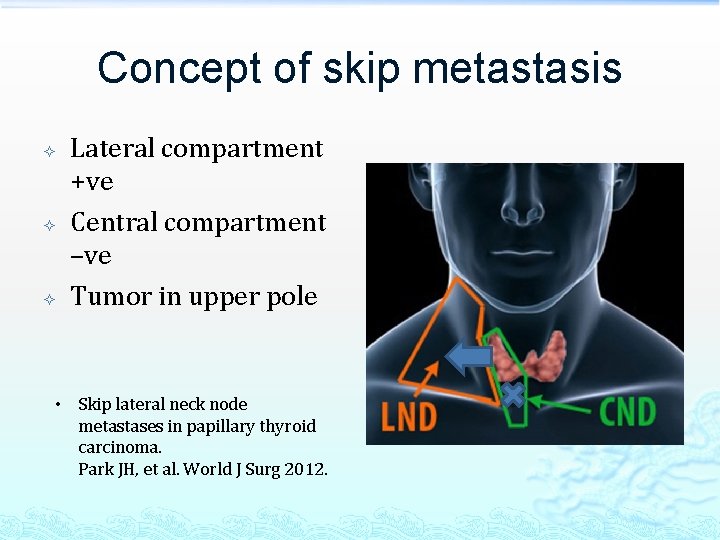
Concept of skip metastasis Lateral compartment +ve Central compartment –ve Tumor in upper pole • Skip lateral neck node metastases in papillary thyroid carcinoma. Park JH, et al. World J Surg 2012.
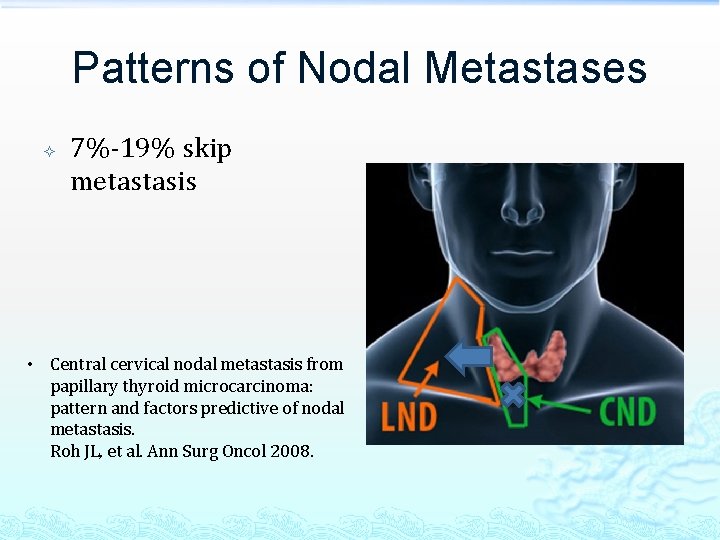
Patterns of Nodal Metastases 7%-19% skip metastasis • Central cervical nodal metastasis from papillary thyroid microcarcinoma: pattern and factors predictive of nodal metastasis. Roh JL, et al. Ann Surg Oncol 2008.
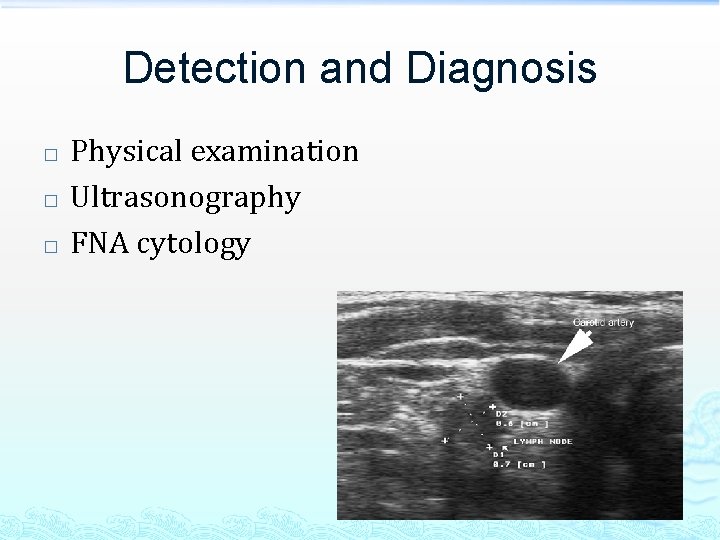
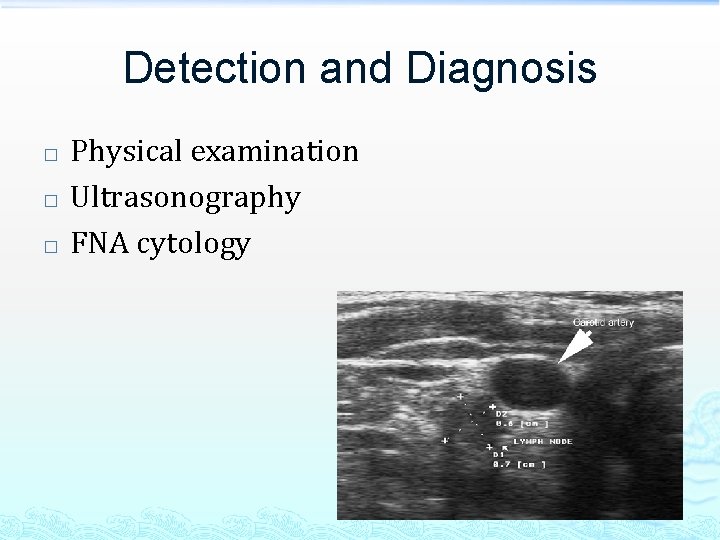
Detection and Diagnosis � � � Physical examination Ultrasonography FNA cytology
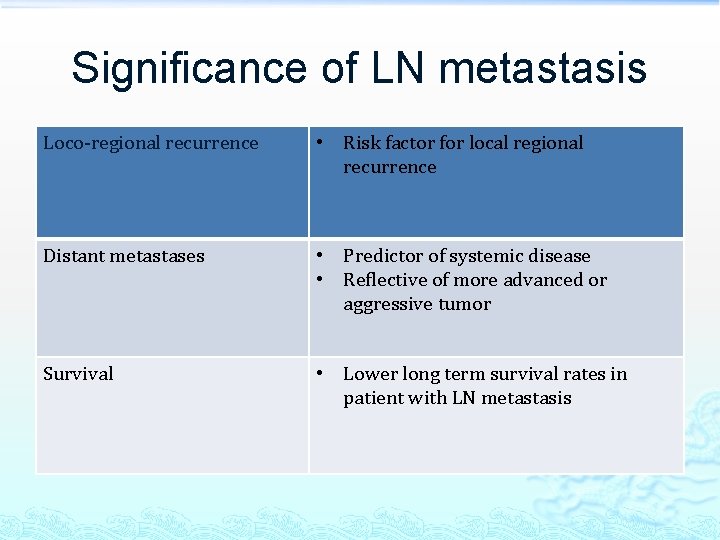
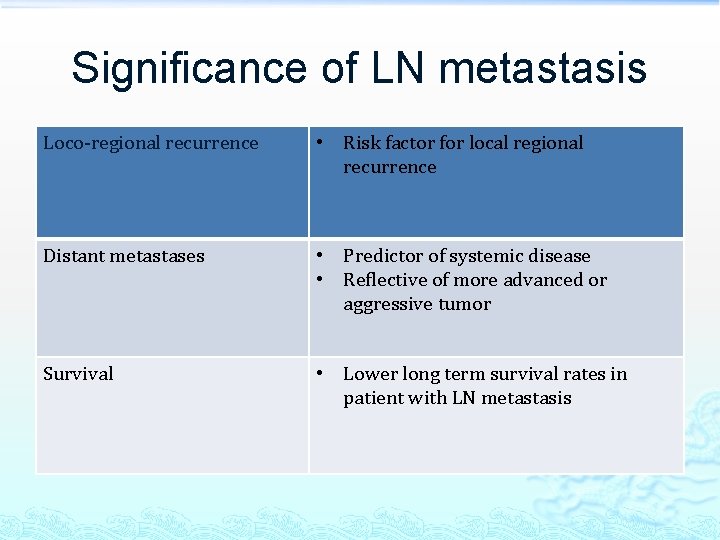
Significance of LN metastasis Loco-regional recurrence • Risk factor for local regional recurrence Distant metastases • Predictor of systemic disease • Reflective of more advanced or aggressive tumor Survival • Lower long term survival rates in patient with LN metastasis
To dissect/ not to dissect?
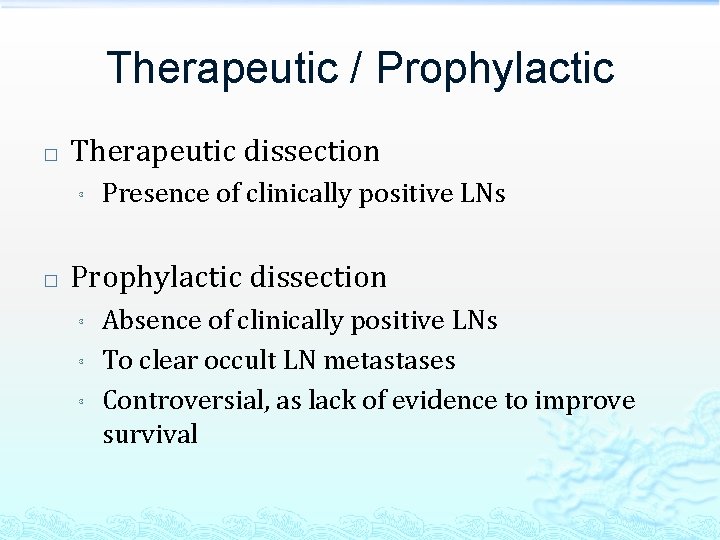
Therapeutic / Prophylactic � Therapeutic dissection ³ � Presence of clinically positive LNs Prophylactic dissection ³ ³ ³ Absence of clinically positive LNs To clear occult LN metastases Controversial, as lack of evidence to improve survival
Prophylactic dissection � � Primary tumor located in the upper pole Extensive involvement of the ipsilateral central compartment Surgical management of the lateral neck compartment for metastatic thyroid cancer. Dralle H, et al. Current Opinion in Oncology. 25(1): 20 -6, 2013 Jan.
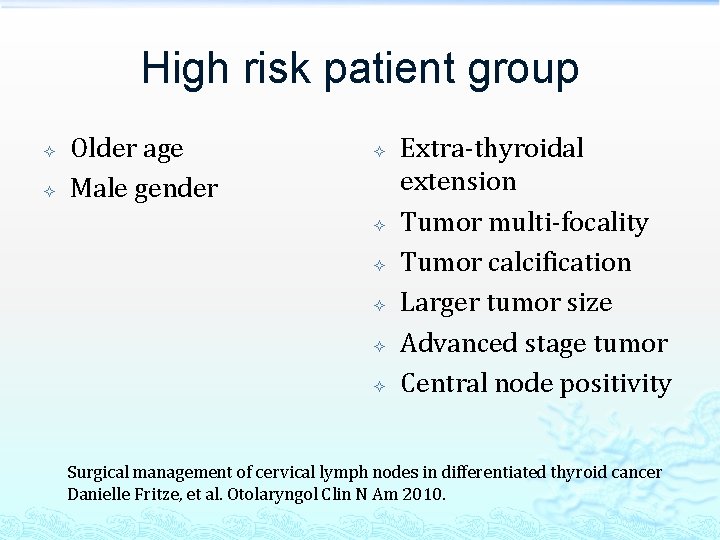
High risk patient group Older age Male gender Extra-thyroidal extension Tumor multi-focality Tumor calcification Larger tumor size Advanced stage tumor Central node positivity Surgical management of cervical lymph nodes in differentiated thyroid cancer Danielle Fritze, et al. Otolaryngol Clin N Am 2010.
Extent of lateral neck dissection
Extent of lateral neck dissection � Selective ‘berry picking’ is associated with higher rates of loco-regional recurrence and has been largely abandoned Greater local recurrence occurs with ‘berry picking’ than neck dissection in thyroid cancer. Musacchio MJ, et al. Am Surg 2003; 69: 191– 196.
Supra-hyoid dissection (Level I) � � Less than 5% of patients had supra-hyoid involvement in patients with lateral cervical metastases Not routinely included in lymph node dissections unless there is macroscopic involvement Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Roh JL, et al. Ann Surg Oncol 2008; 15(4): 1177– 82.
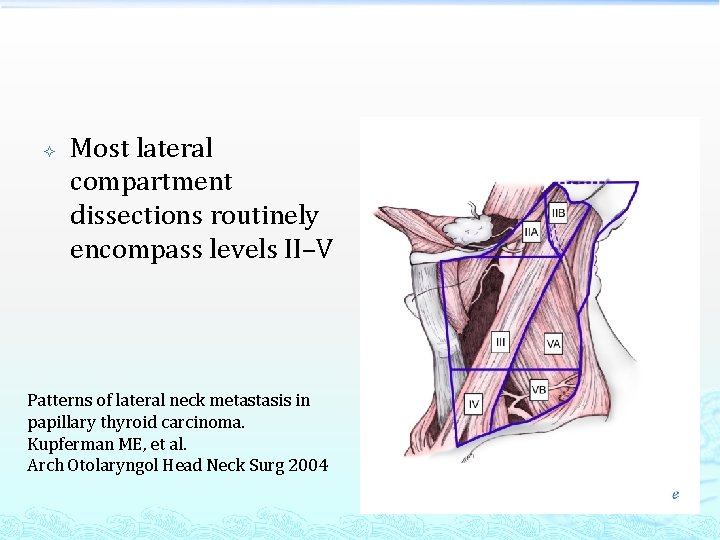
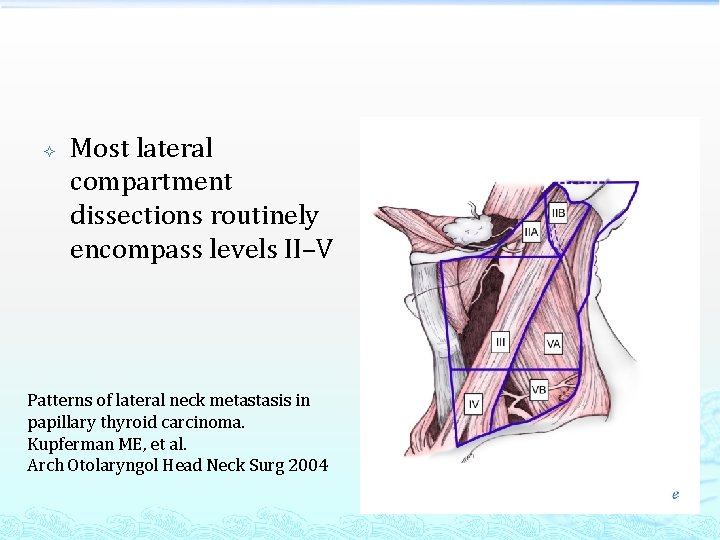
Most lateral compartment dissections routinely encompass levels II–V Patterns of lateral neck metastasis in papillary thyroid carcinoma. Kupferman ME, et al. Arch Otolaryngol Head Neck Surg 2004
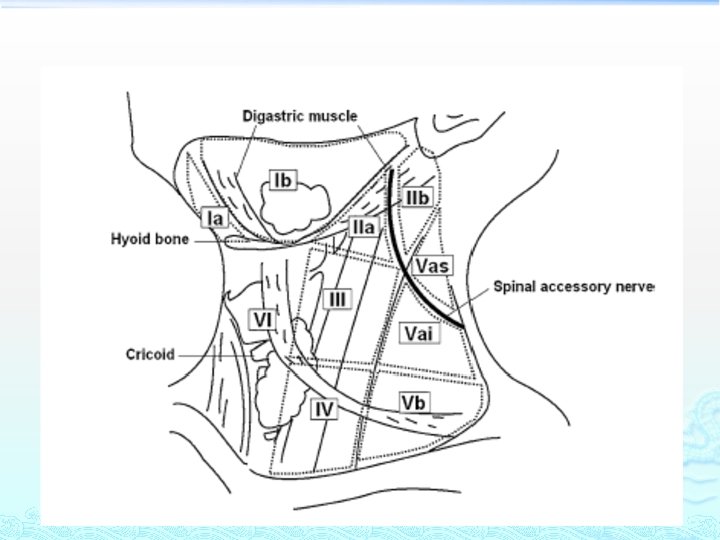
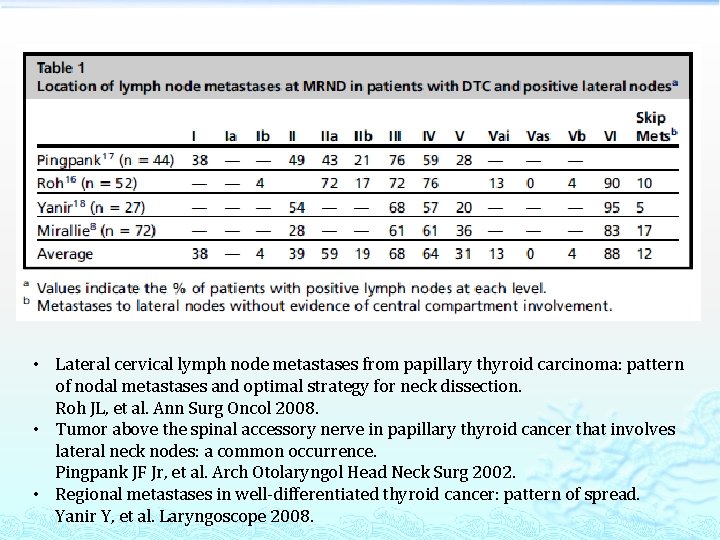
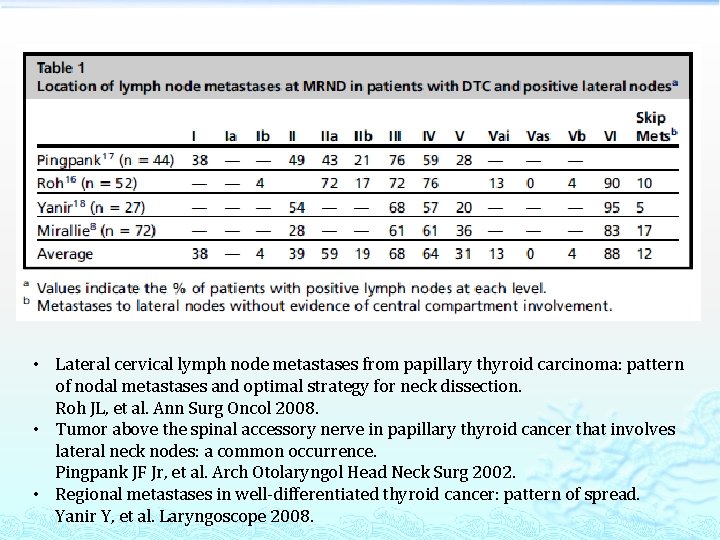
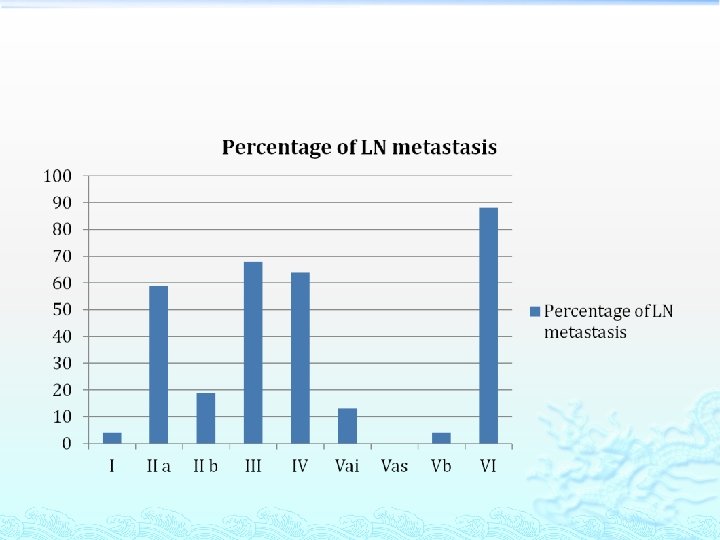
• Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Roh JL, et al. Ann Surg Oncol 2008. • Tumor above the spinal accessory nerve in papillary thyroid cancer that involves lateral neck nodes: a common occurrence. Pingpank JF Jr, et al. Arch Otolaryngol Head Neck Surg 2002. • Regional metastases in well-differentiated thyroid cancer: pattern of spread. Yanir Y, et al. Laryngoscope 2008.
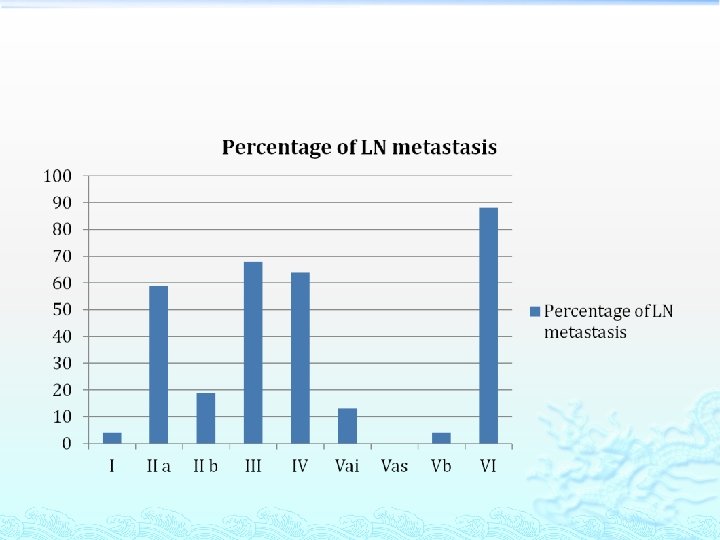
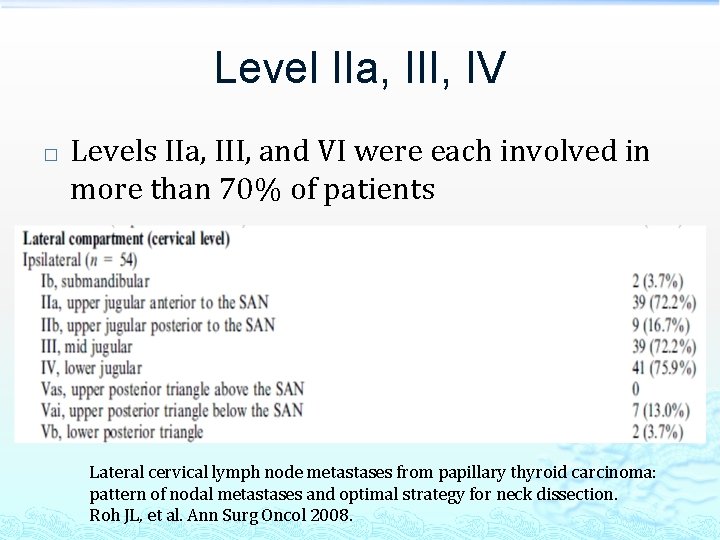
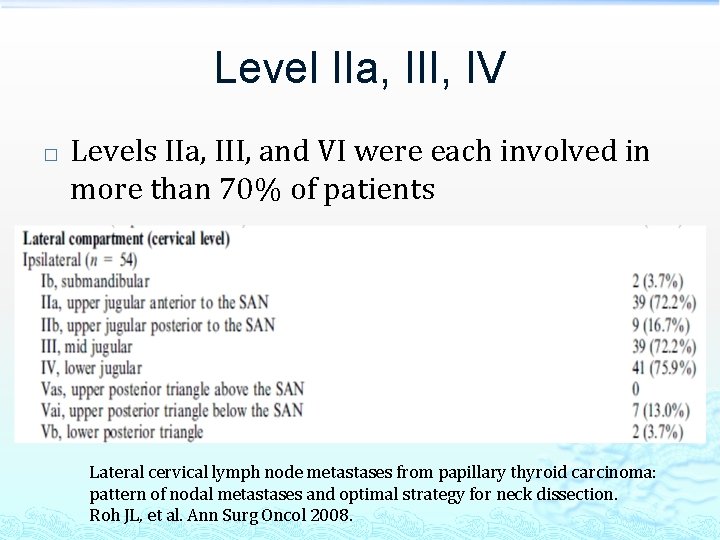
Level IIa, III, IV � Levels IIa, III, and VI were each involved in more than 70% of patients Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Roh JL, et al. Ann Surg Oncol 2008.
� Cervical lateral neck metastases in PTC occur in a predictable pattern, with levels III, IIa, and IV most commonly involved Is routine dissection of level II-B and V-A necessary in patients with papillary thyroid cancer undergoing lateral neck dissection for FNA-confirmed metastases in other levels. Farrag T, et al. World Journal of Surgery. 33(8): 1680 -3, 2009 Aug.
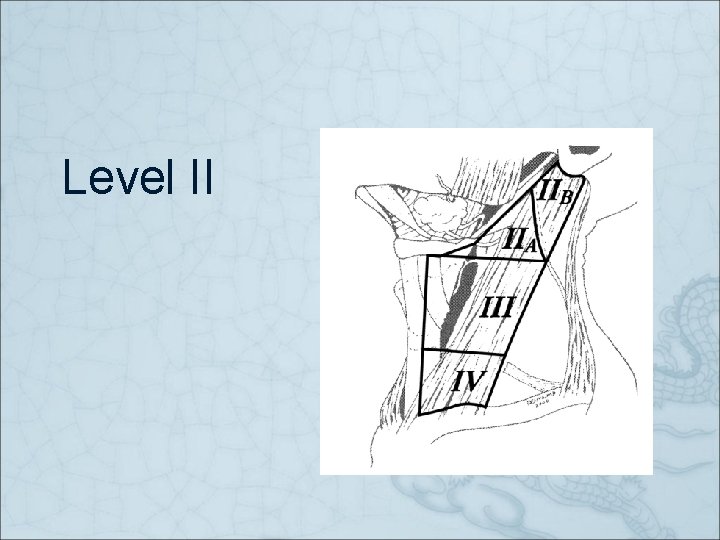
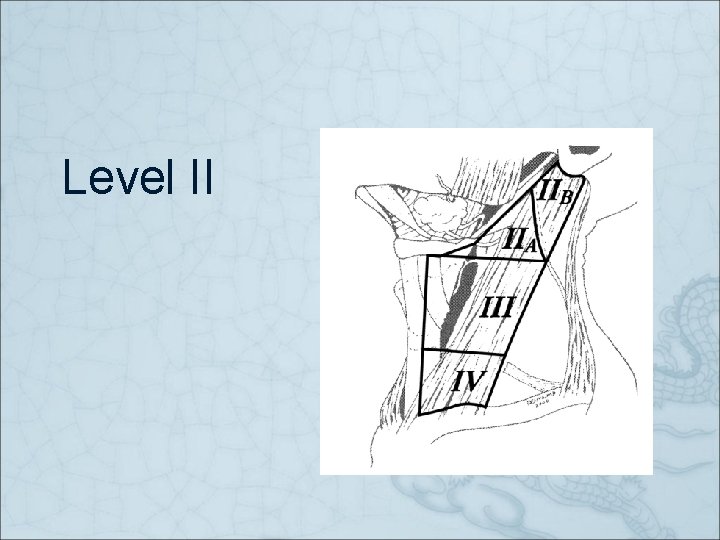
Level II
Level IIb � � Only 16. 7% of patients had positive nodes at level IIb Involvement was associated with multilevel disease in all cases Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Roh JL, et al. Ann Surg Oncol 2008; 15(4): 1177– 82.
Level IIb � ‘’…. the incidence of LN metastases at level IIb was 2. 1%. . . the results of the present study suggested that LN metastases in level IIb are rare in patients with PTC undergoing neck dissection’’ Level IIb lymph node metastasis in thyroid papillary carcinoma. Vayisoglu Y, et al. European Archives of Oto-Rhino-Laryngology 2010.
Level IIb � ‘’…level IIb was positive in 8. 5%…elective dissection of level IIb only when level IIa is involved, based on FNA confirmation, or when it is grossly involved on intraoperative evaluation’’ Is routine dissection of level II-B and V-A necessary in patients with papillary thyroid cancer undergoing lateral neck dissection for FNA-confirmed metastases in other levels. Farrag T, et al. World Journal of Surgery. 33(8): 1680 -3, 2009 Aug.
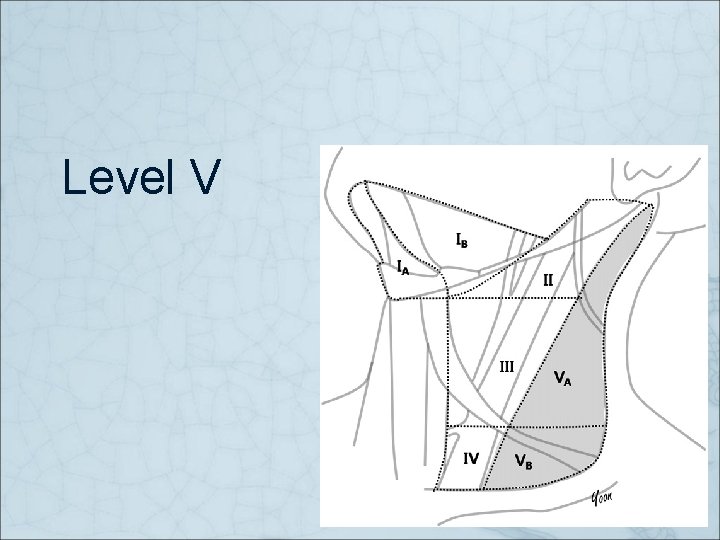
Level V
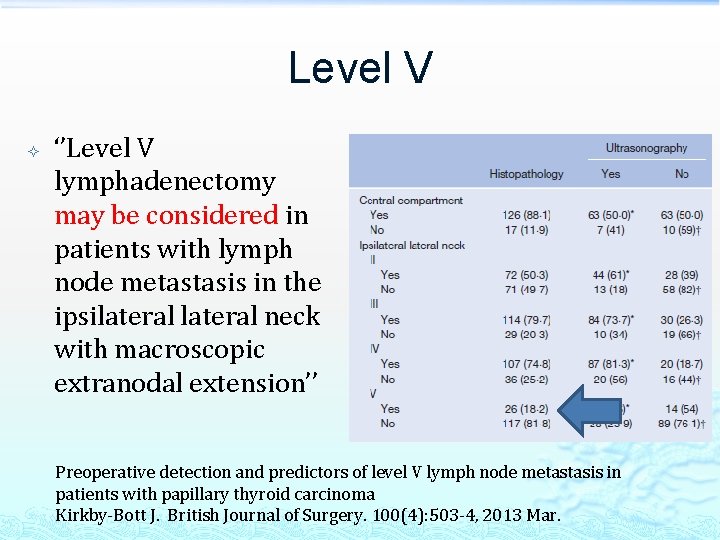
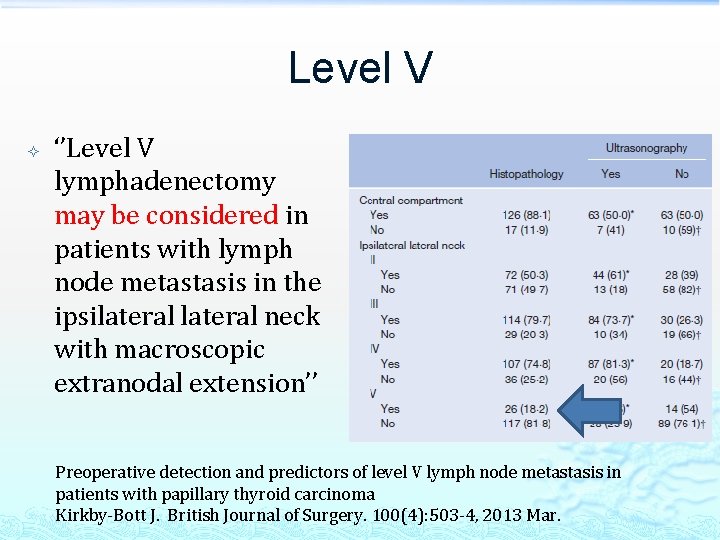
Level V ‘’Level V lymphadenectomy may be considered in patients with lymph node metastasis in the ipsilateral neck with macroscopic extranodal extension’’ Preoperative detection and predictors of level V lymph node metastasis in patients with papillary thyroid carcinoma Kirkby-Bott J. British Journal of Surgery. 100(4): 503 -4, 2013 Mar.
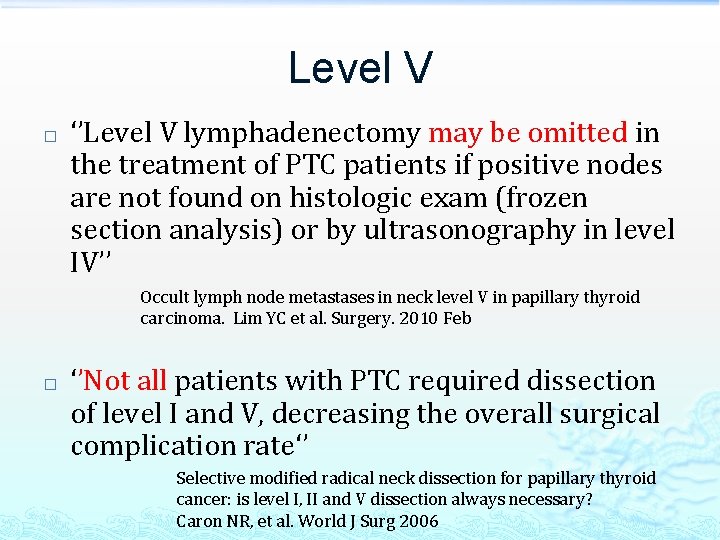
Level V � ‘’Level V lymphadenectomy may be omitted in the treatment of PTC patients if positive nodes are not found on histologic exam (frozen section analysis) or by ultrasonography in level IV’’ Occult lymph node metastases in neck level V in papillary thyroid carcinoma. Lim YC et al. Surgery. 2010 Feb � ‘’Not all patients with PTC required dissection of level I and V, decreasing the overall surgical complication rate‘’ Selective modified radical neck dissection for papillary thyroid cancer: is level I, II and V dissection always necessary? Caron NR, et al. World J Surg 2006
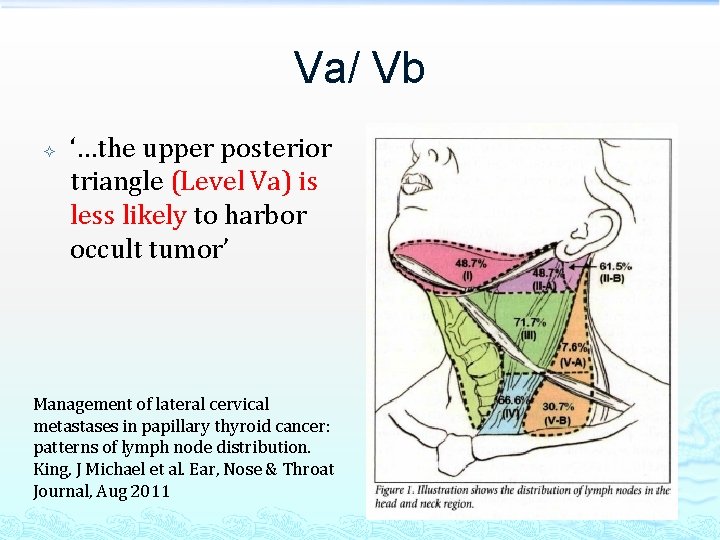
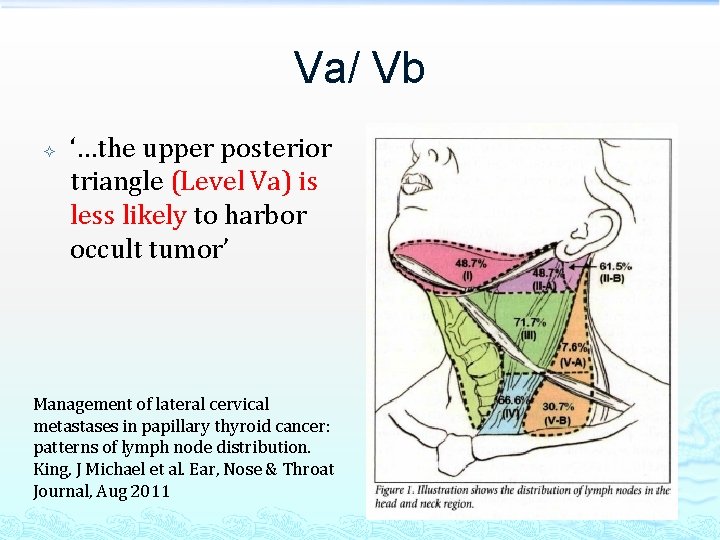
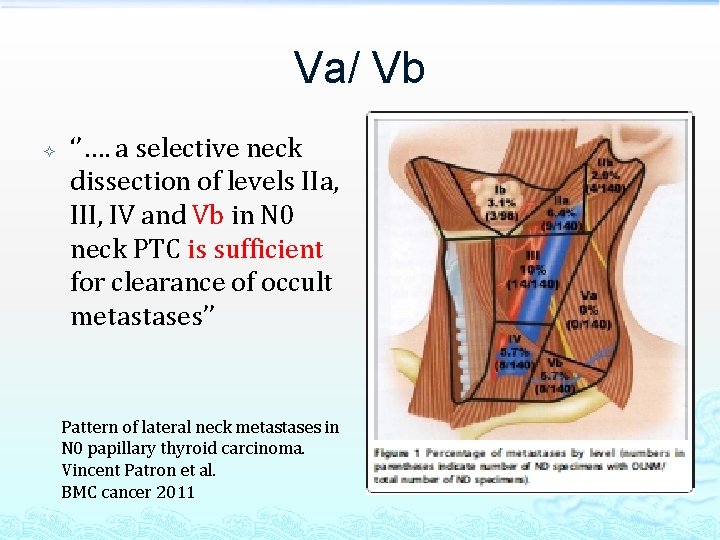
Va/ Vb ‘…the upper posterior triangle (Level Va) is less likely to harbor occult tumor’ Management of lateral cervical metastases in papillary thyroid cancer: patterns of lymph node distribution. King, J Michael et al. Ear, Nose & Throat Journal, Aug 2011
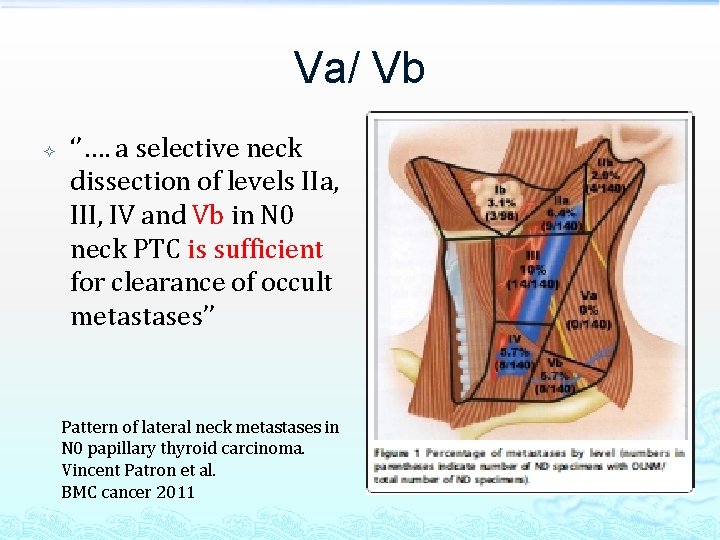
Va/ Vb ‘’…. a selective neck dissection of levels IIa, III, IV and Vb in N 0 neck PTC is sufficient for clearance of occult metastases’’ Pattern of lateral neck metastases in N 0 papillary thyroid carcinoma. Vincent Patron et al. BMC cancer 2011
Morbidity of lateral neck dissection
Morbidity � � Chyle leakage Spinal assessory nerve damage Carotid artery rupture Nerve injury
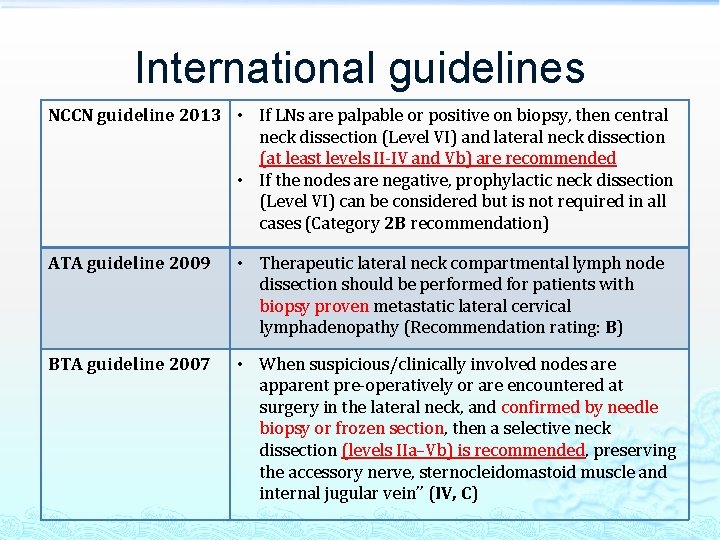
International guidelines
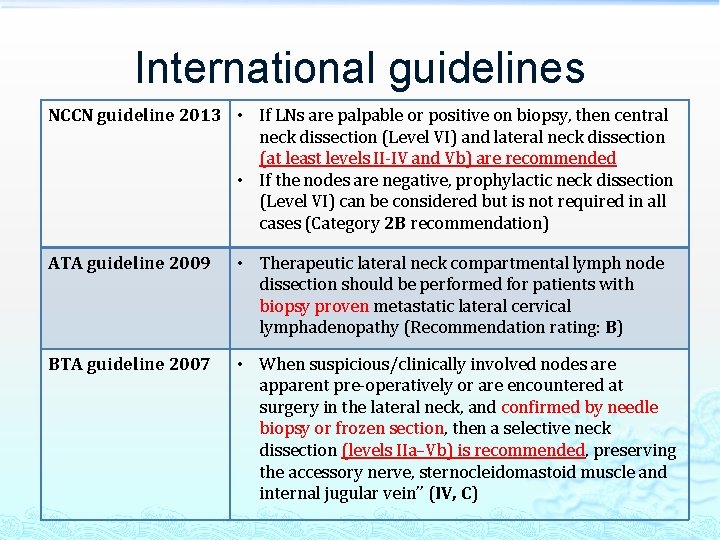
International guidelines NCCN guideline 2013 • If LNs are palpable or positive on biopsy, then central neck dissection (Level VI) and lateral neck dissection (at least levels II-IV and Vb) are recommended • If the nodes are negative, prophylactic neck dissection (Level VI) can be considered but is not required in all cases (Category 2 B recommendation) ATA guideline 2009 • Therapeutic lateral neck compartmental lymph node dissection should be performed for patients with biopsy proven metastatic lateral cervical lymphadenopathy (Recommendation rating: B) BTA guideline 2007 • When suspicious/clinically involved nodes are apparent pre-operatively or are encountered at surgery in the lateral neck, and confirmed by needle biopsy or frozen section, then a selective neck dissection (levels IIa–Vb) is recommended, preserving the accessory nerve, sternocleidomastoid muscle and internal jugular vein’’ (IV, C)
Conclusion � � Skip metastasis may occur in PTC Prophylactic LND is controversial Therapeutic LND includes Level II to V as gold standard It’s important to strike a balance between oncological benefit and surgical risk in the extent of selective neck dissection
The End