Laryngeal Malignancy Dr Vishal Sharma Overview Most common













- Slides: 66

Laryngeal Malignancy Dr. Vishal Sharma
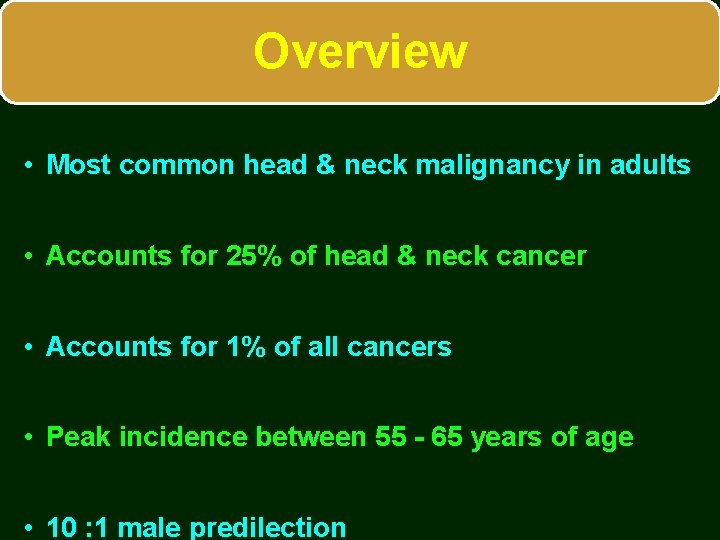
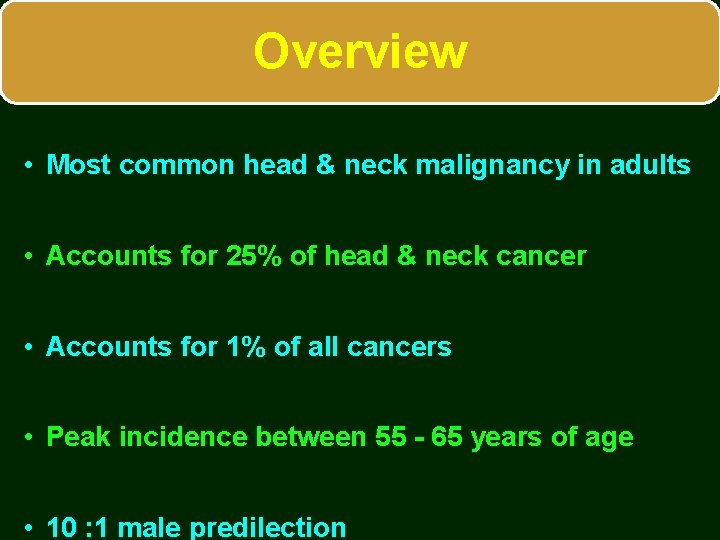
Overview • Most common head & neck malignancy in adults • Accounts for 25% of head & neck cancer • Accounts for 1% of all cancers • Peak incidence between 55 - 65 years of age • 10 : 1 male predilection
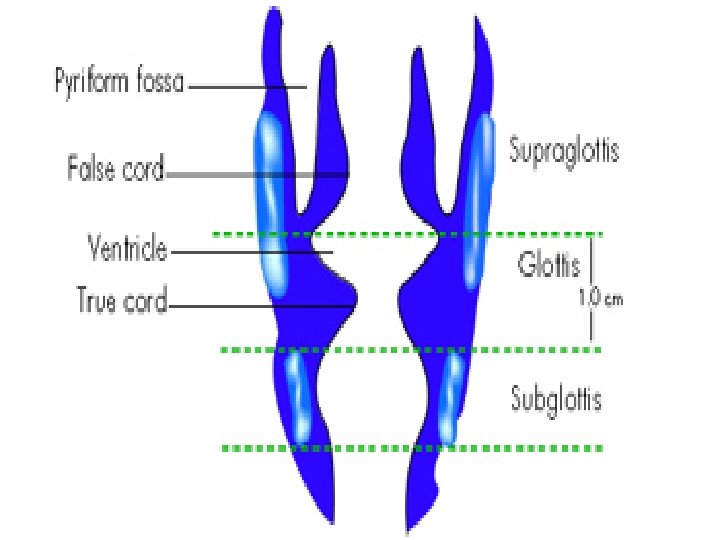

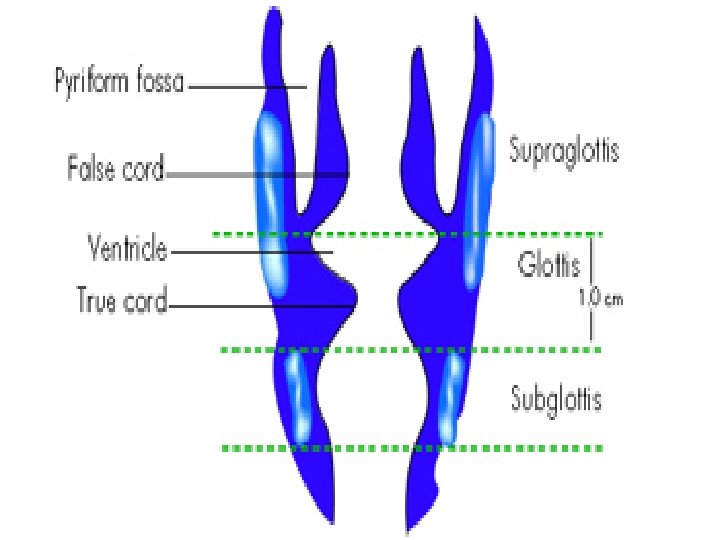
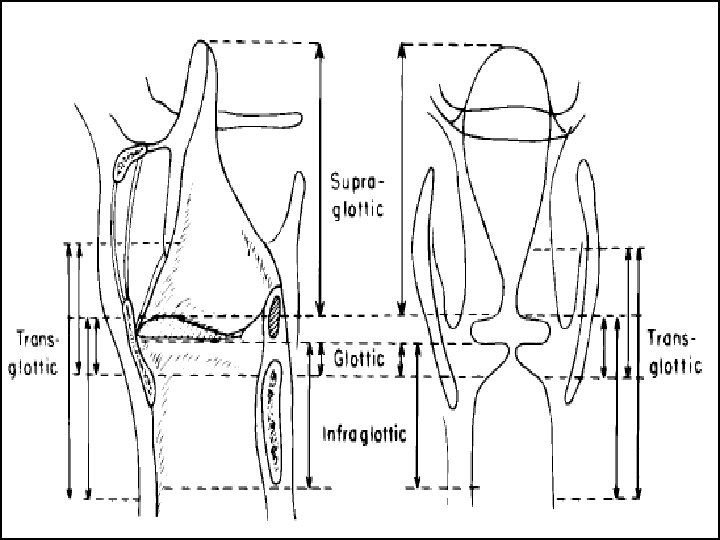
Sites & subsites of larynx Supraglottis • Suprahyoid epiglottis • Aryepiglottic fold • Arytenoid • Infrahyoid epiglottis • Ventricular bands Glottis • Vocal cords • Anterior commissure • Posterior commissure Subglottis
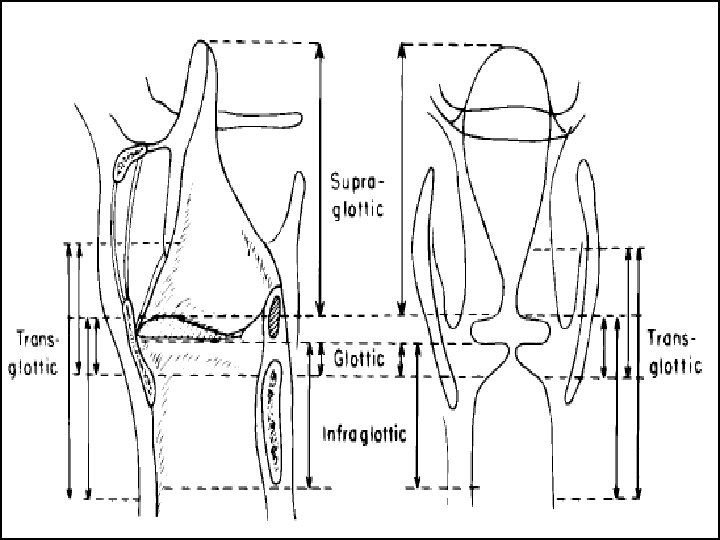
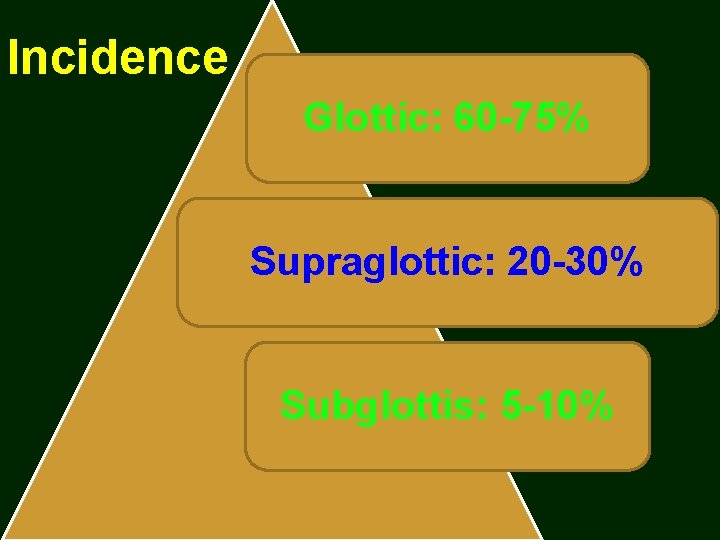
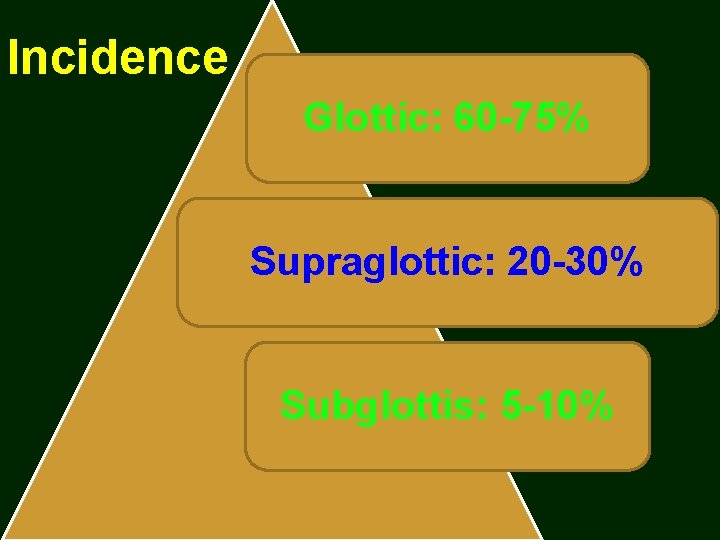
Incidence Glottic: 60 -75% Supraglottic: 20 -30% Subglottis: 5 -10%
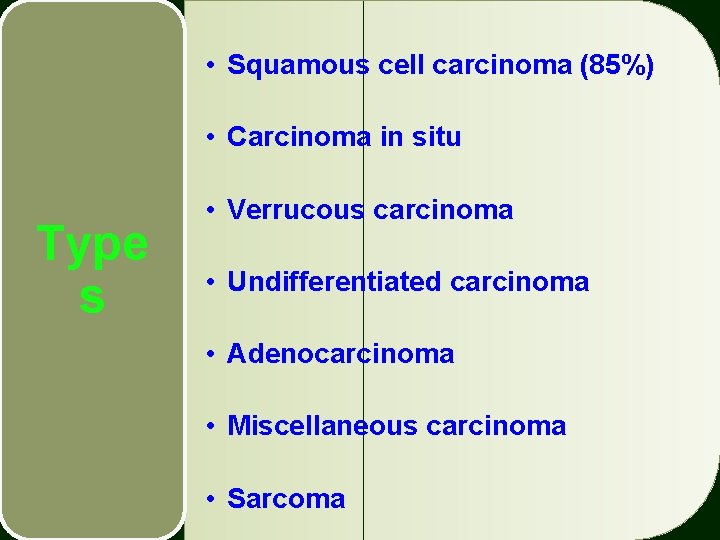
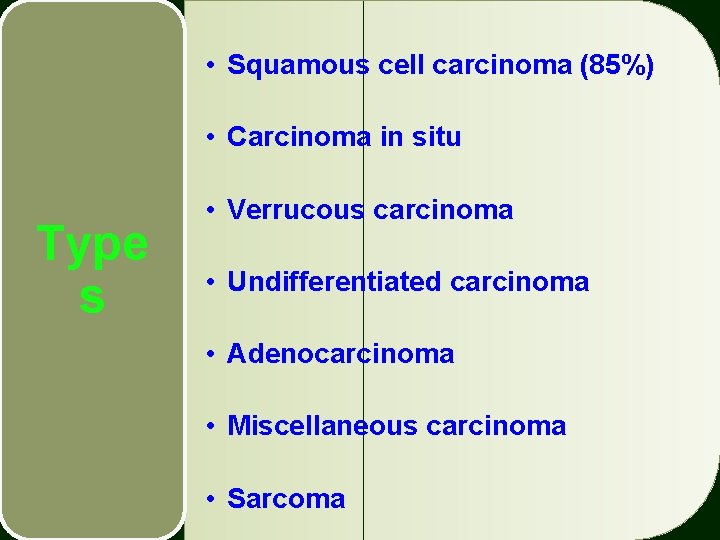
• Squamous cell carcinoma (85%) • Carcinoma in situ Type s • Verrucous carcinoma • Undifferentiated carcinoma • Adenocarcinoma • Miscellaneous carcinoma • Sarcoma
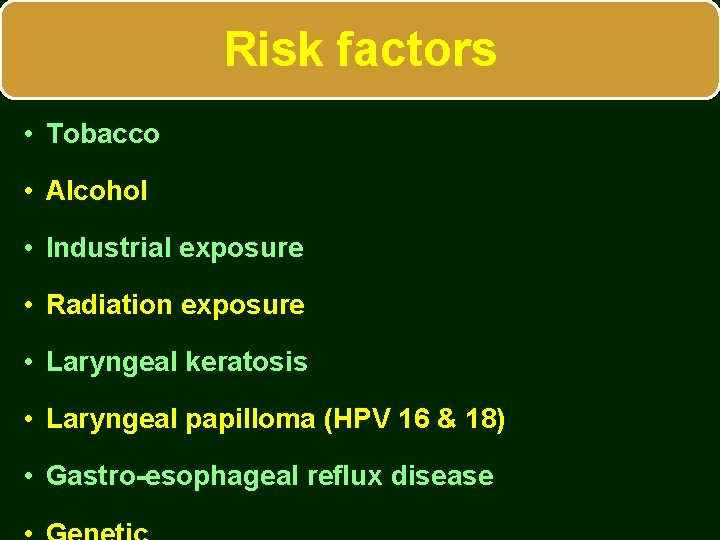
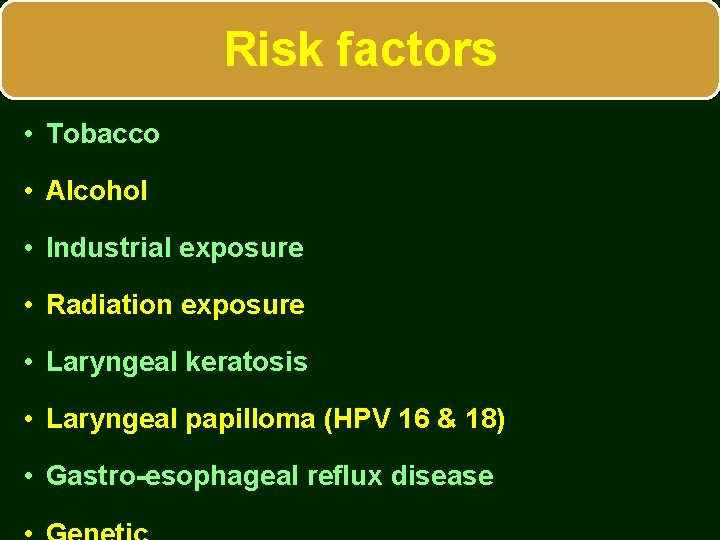
Risk factors • Tobacco • Alcohol • Industrial exposure • Radiation exposure • Laryngeal keratosis • Laryngeal papilloma (HPV 16 & 18) • Gastro-esophageal reflux disease
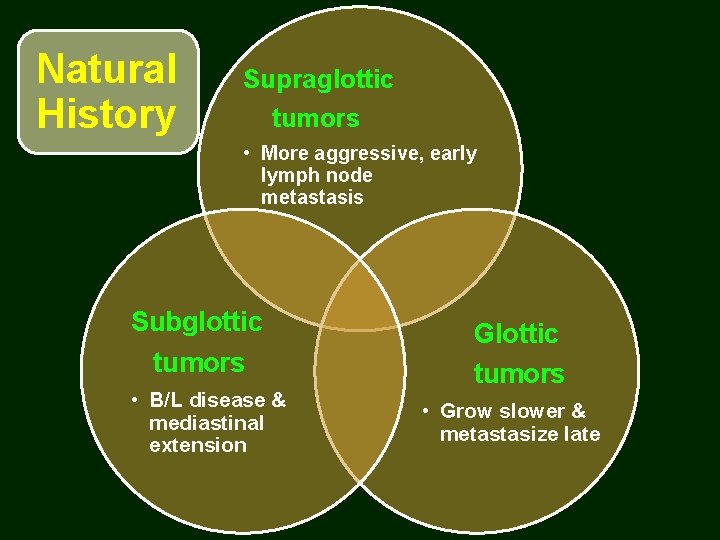
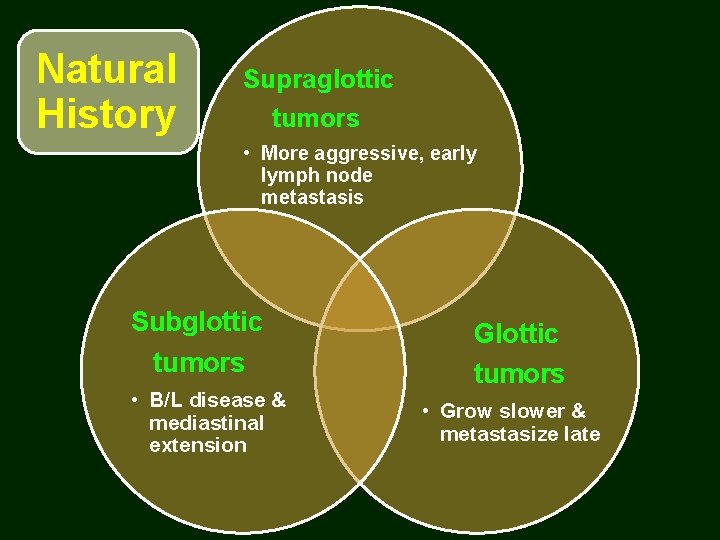
Natural History Supraglottic tumors • More aggressive, early lymph node metastasis Subglottic tumors • B/L disease & mediastinal extension Glottic tumors • Grow slower & metastasize late
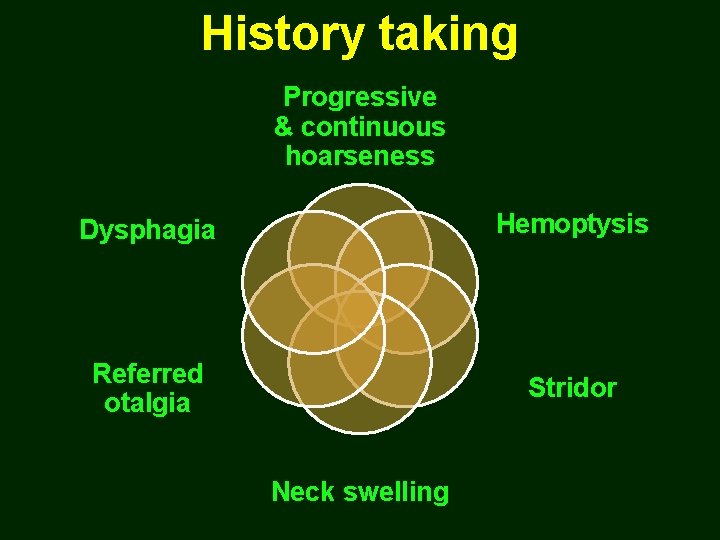
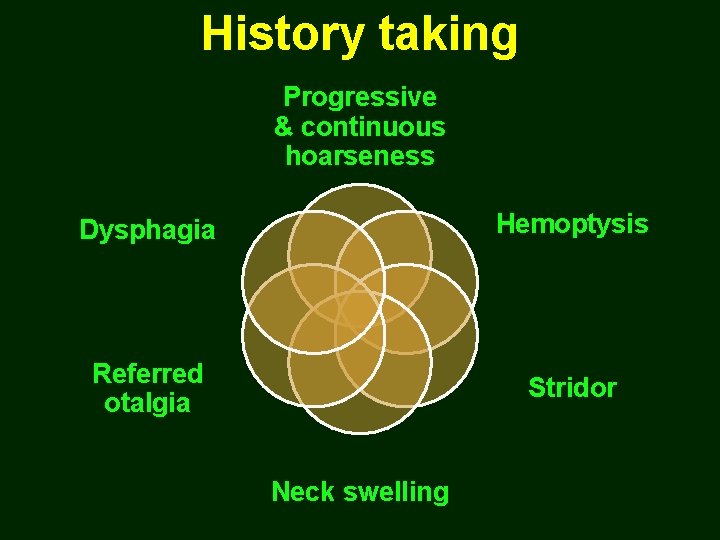
History taking Progressive & continuous hoarseness Dysphagia Hemoptysis Referred otalgia Stridor Neck swelling
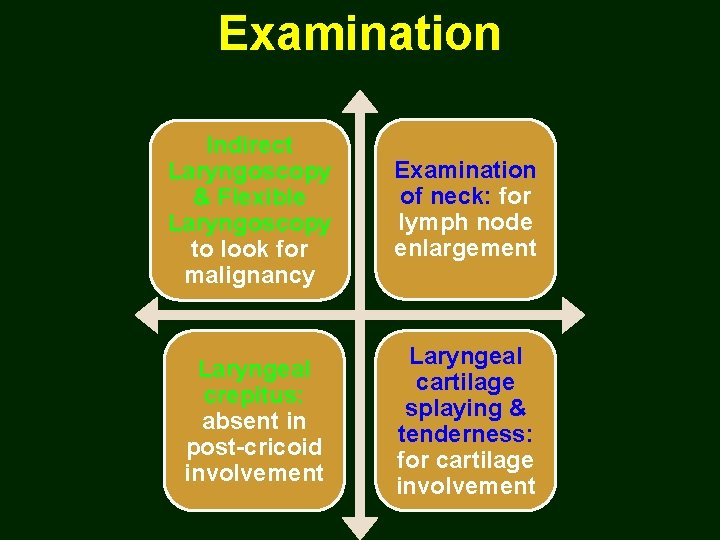
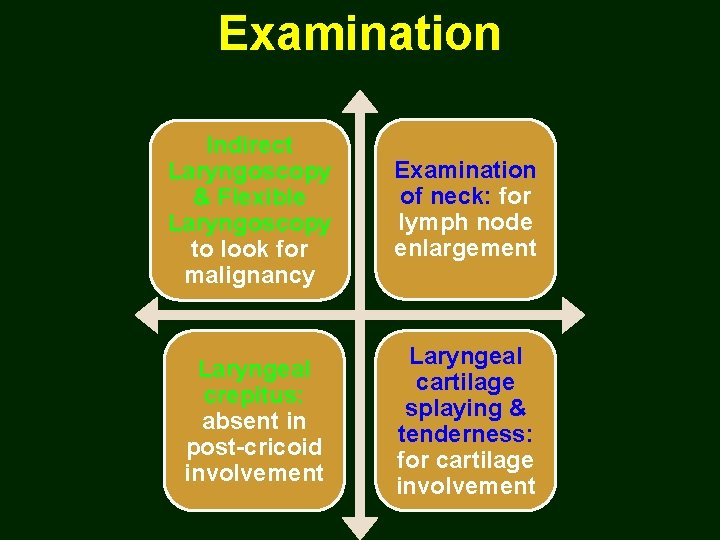
Examination Indirect Laryngoscopy & Flexible Laryngoscopy to look for malignancy Examination of neck: for lymph node enlargement Laryngeal crepitus: absent in post-cricoid involvement Laryngeal cartilage splaying & tenderness: for cartilage involvement
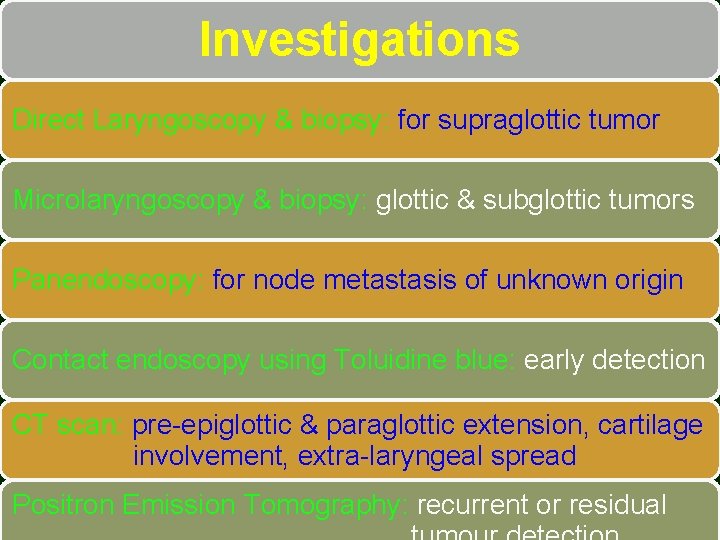
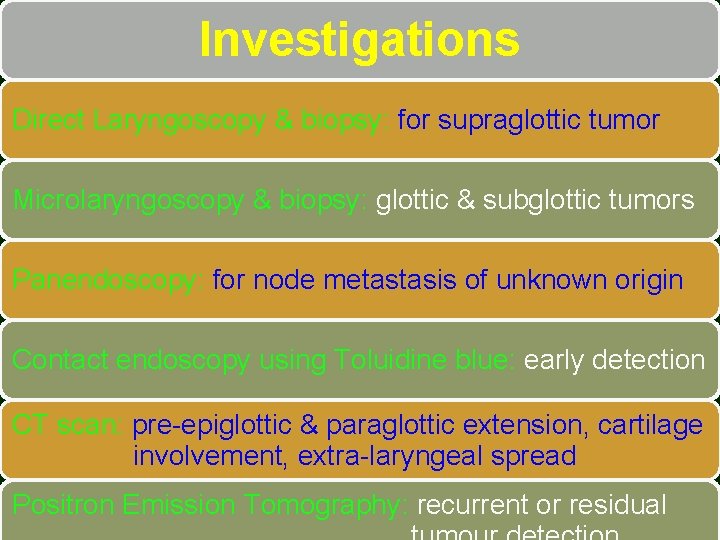
Investigations Direct Laryngoscopy & biopsy: for supraglottic tumor Microlaryngoscopy & biopsy: glottic & subglottic tumors Panendoscopy: for node metastasis of unknown origin Contact endoscopy using Toluidine blue: early detection CT scan: pre-epiglottic & paraglottic extension, cartilage involvement, extra-laryngeal spread Positron Emission Tomography: recurrent or residual
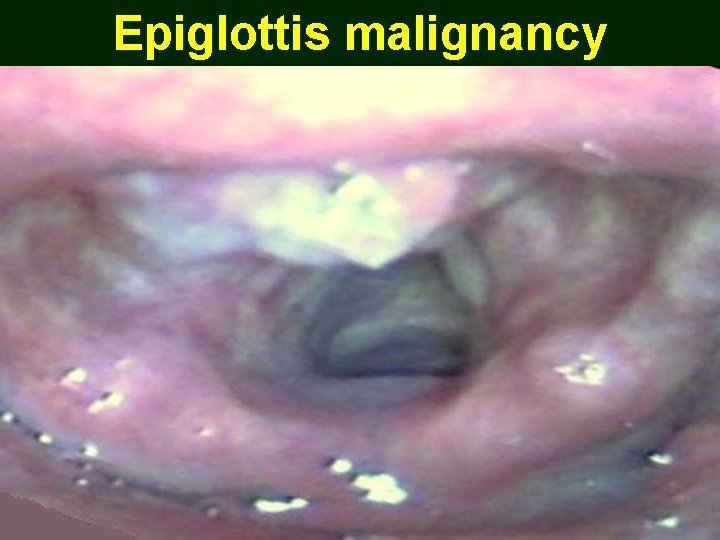
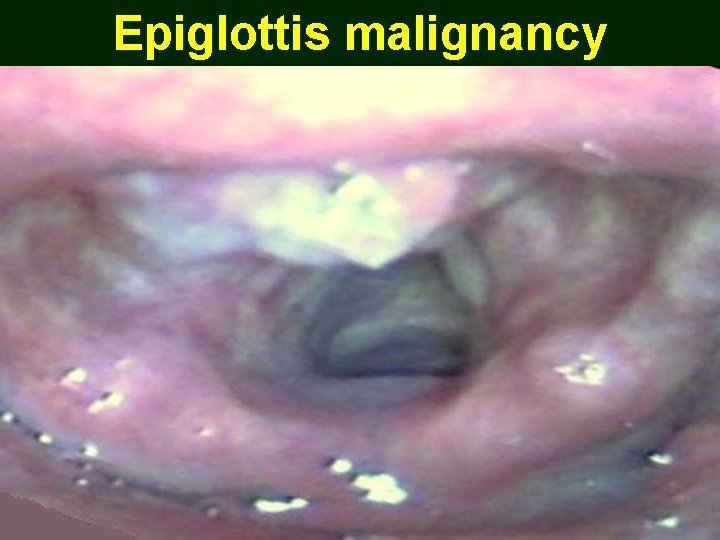
Epiglottis malignancy

Ventricular band malignancy

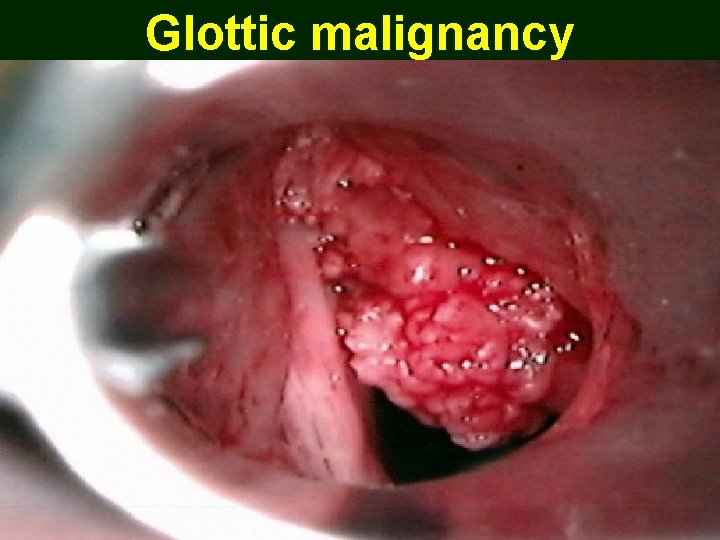
Glottic malignancy
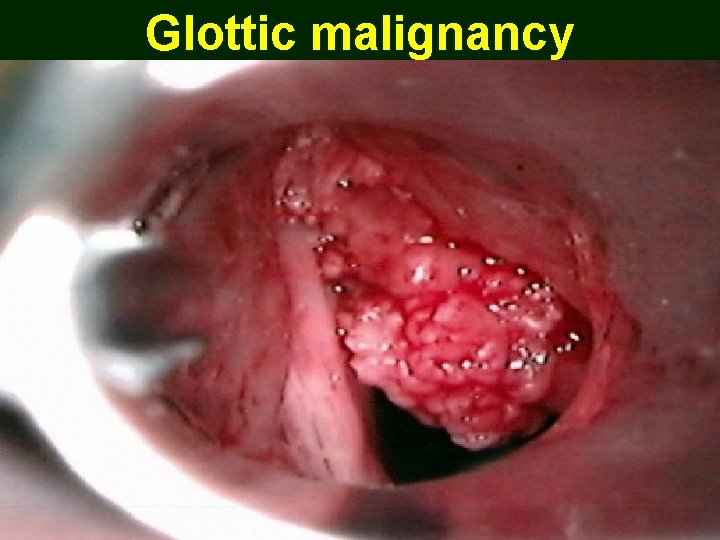
Glottic malignancy

Subglottic malignancy
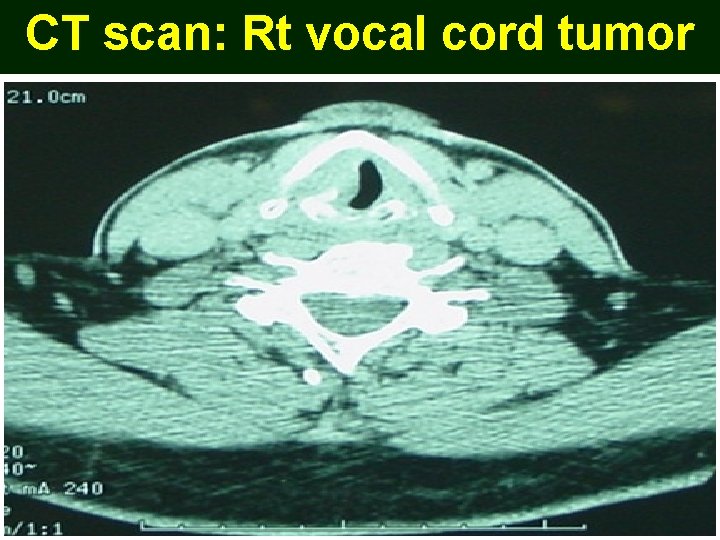
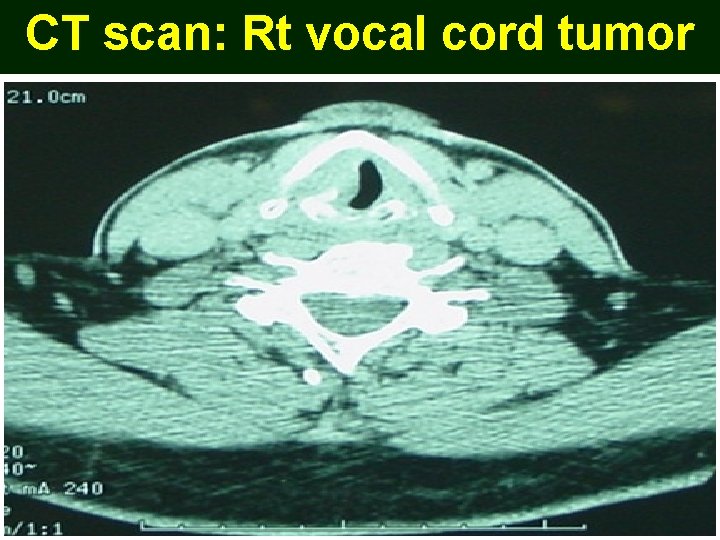
CT scan: Rt vocal cord tumor
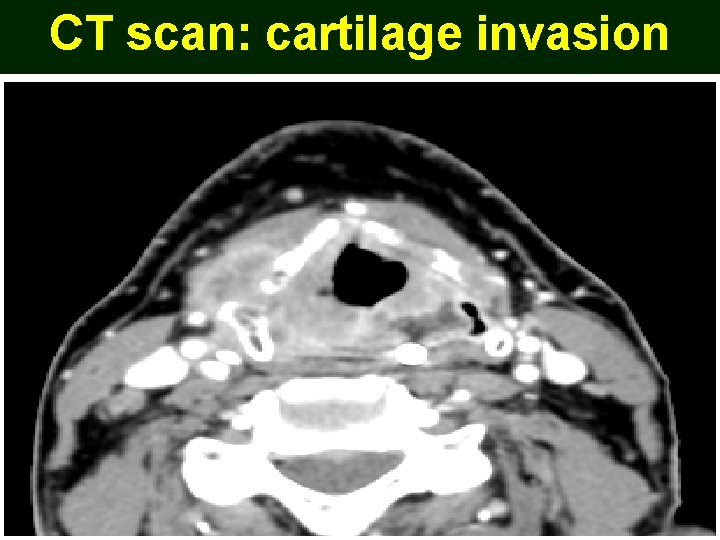
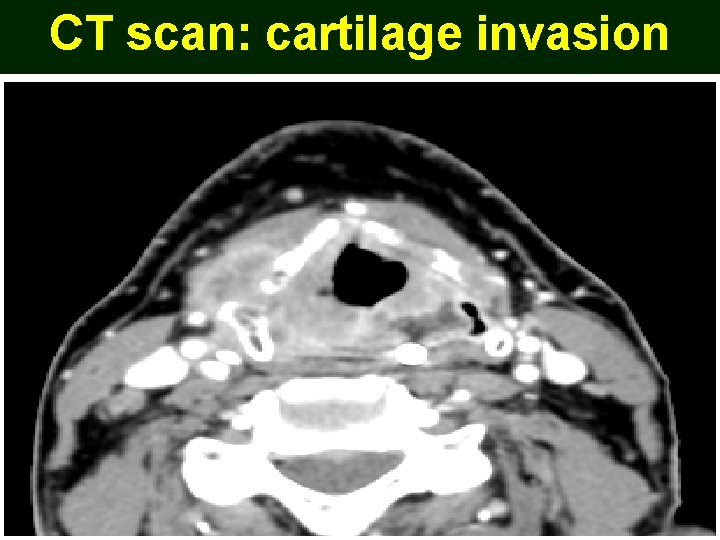
CT scan: cartilage invasion
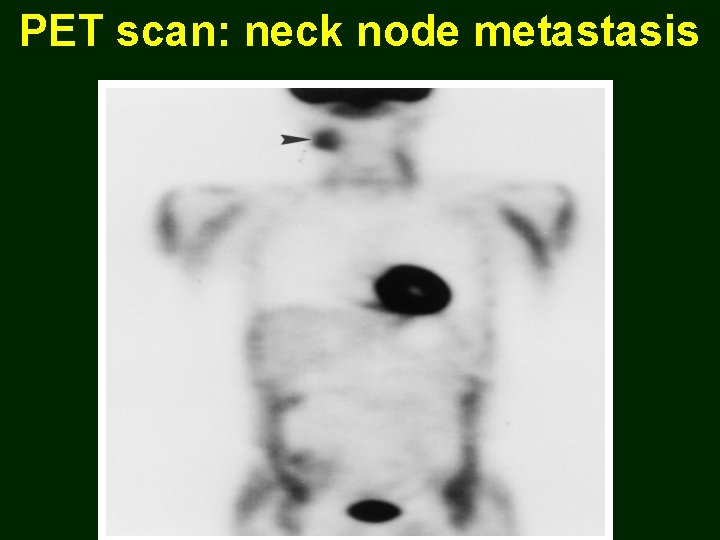
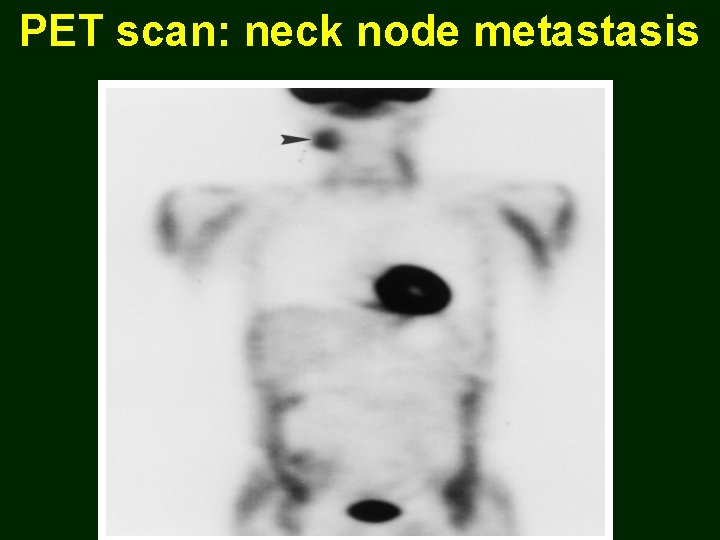
PET scan: neck node metastasis

PET CT scan: laryngeal malignancy
TNM Classification UICC (1997)
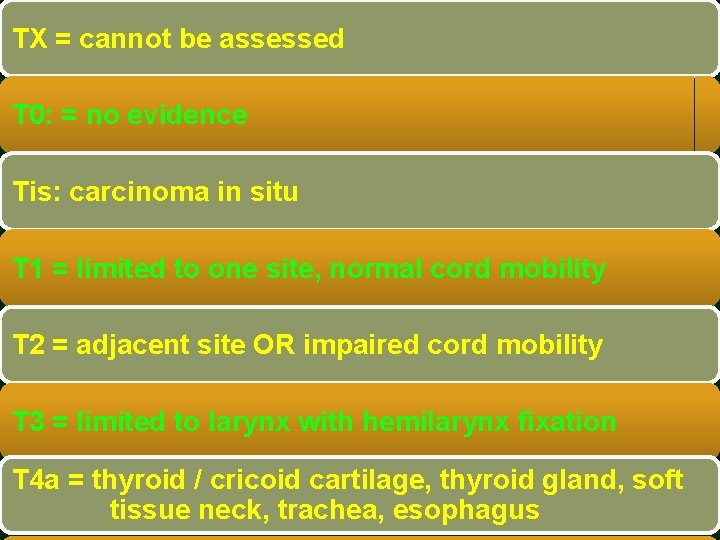
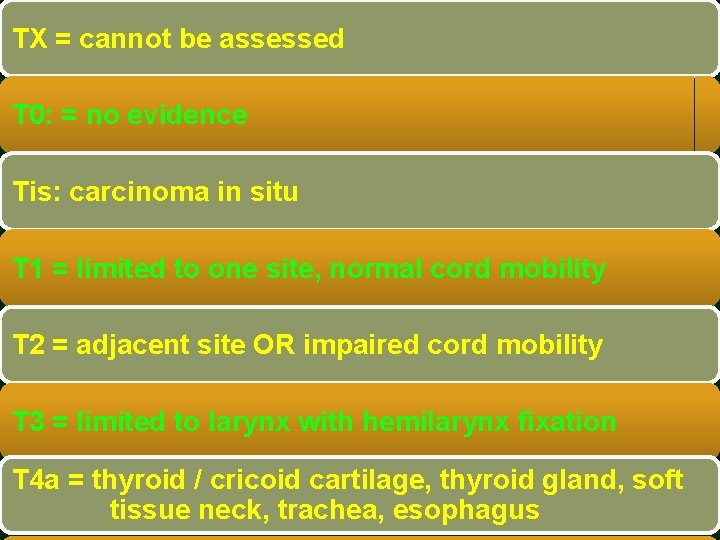
TX = cannot be assessed T 0: = no evidence Tis: carcinoma in situ T 1 = limited to one site, normal cord mobility T 2 = adjacent site OR impaired cord mobility T 3 = limited to larynx with hemilarynx fixation T 4 a = thyroid / cricoid cartilage, thyroid gland, soft tissue neck, trachea, esophagus
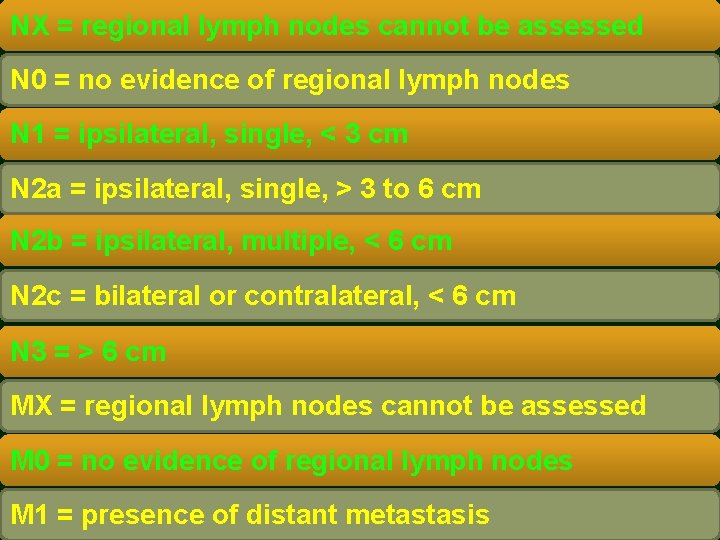
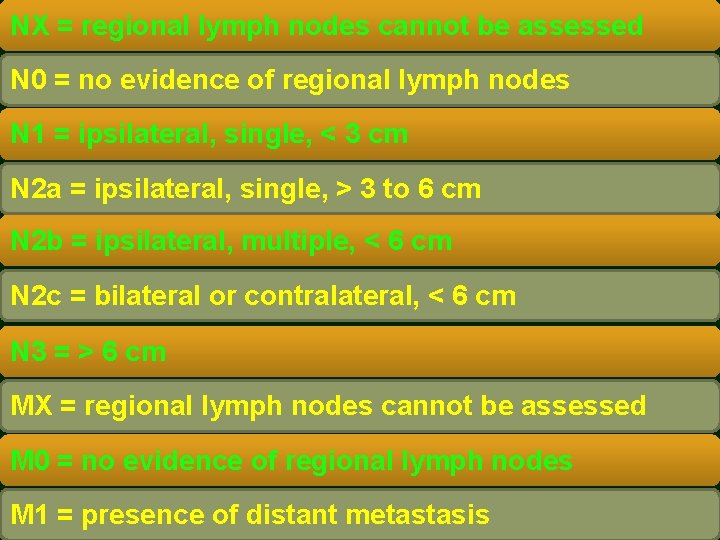
NX = regional lymph nodes cannot be assessed N 0 = no evidence of regional lymph nodes N 1 = ipsilateral, single, < 3 cm N 2 a = ipsilateral, single, > 3 to 6 cm N 2 b = ipsilateral, multiple, < 6 cm N 2 c = bilateral or contralateral, < 6 cm N 3 = > 6 cm MX = regional lymph nodes cannot be assessed M 0 = no evidence of regional lymph nodes M 1 = presence of distant metastasis
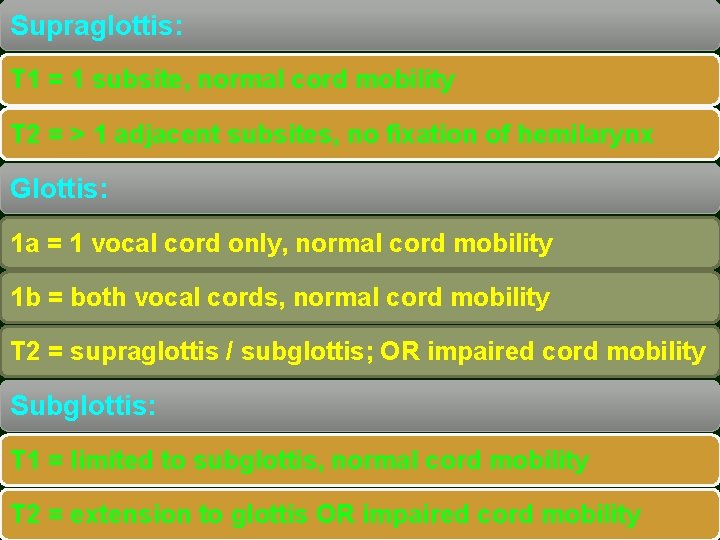
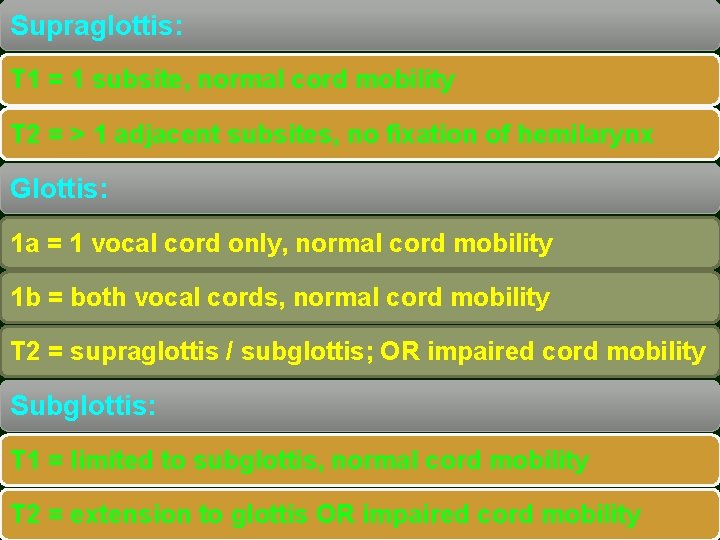
Supraglottis: T 1 = 1 subsite, normal cord mobility T 2 = > 1 adjacent subsites, no fixation of hemilarynx Glottis: 1 a = 1 vocal cord only, normal cord mobility 1 b = both vocal cords, normal cord mobility T 2 = supraglottis / subglottis; OR impaired cord mobility Subglottis: T 1 = limited to subglottis, normal cord mobility T 2 = extension to glottis OR impaired cord mobility
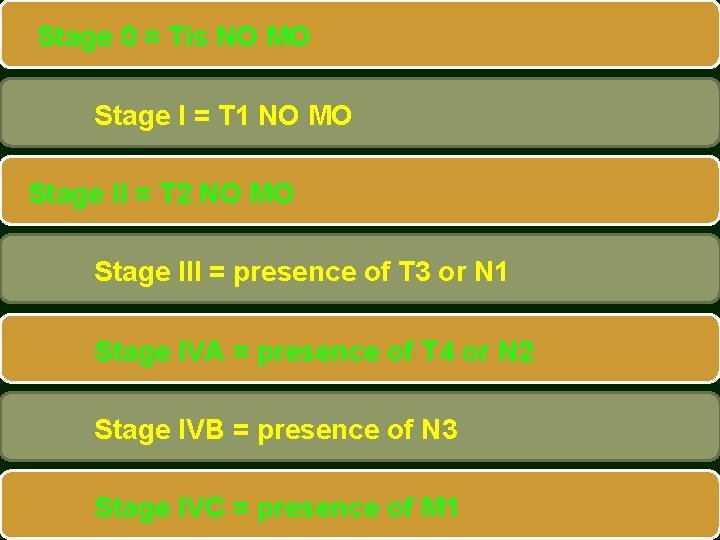
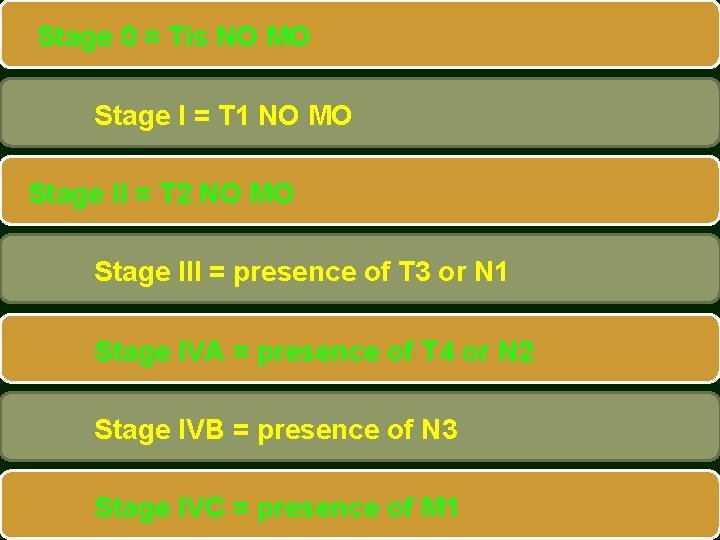
Stage 0 = Tis NO MO Stage I = T 1 NO MO Stage II = T 2 NO MO Stage III = presence of T 3 or N 1 Stage IVA = presence of T 4 or N 2 Stage IVB = presence of N 3 Stage IVC = presence of M 1

Treatment of Laryngeal Malignancy
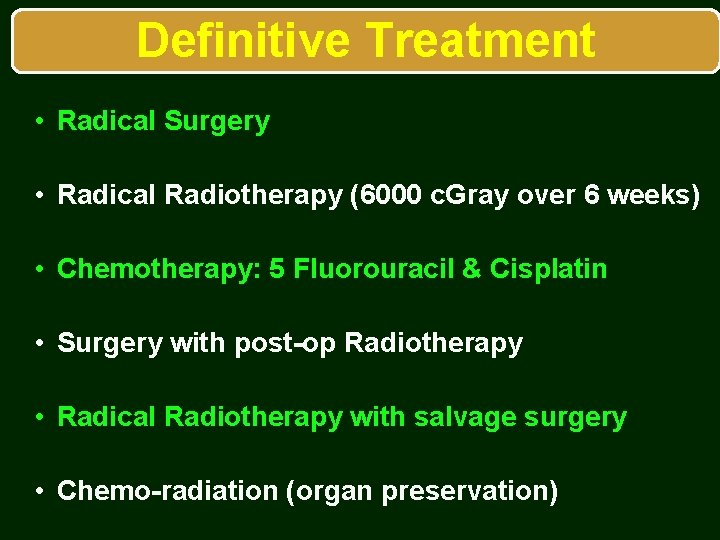
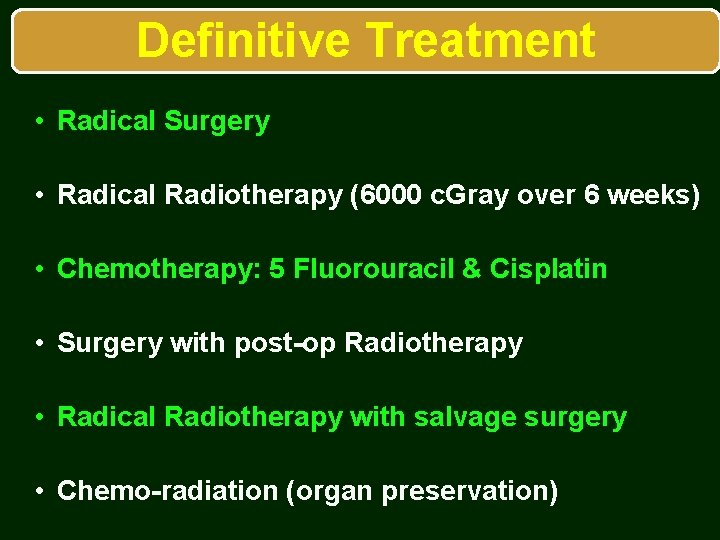
Definitive Treatment • Radical Surgery • Radical Radiotherapy (6000 c. Gray over 6 weeks) • Chemotherapy: 5 Fluorouracil & Cisplatin • Surgery with post-op Radiotherapy • Radical Radiotherapy with salvage surgery • Chemo-radiation (organ preservation)

Surgical Treatment
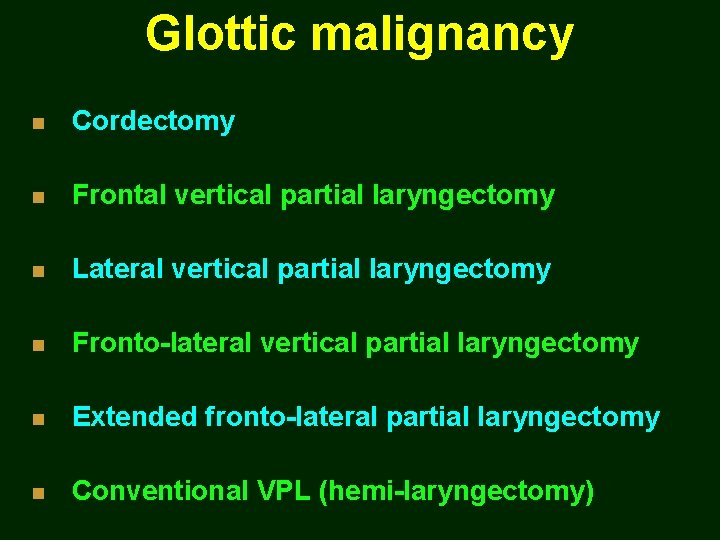
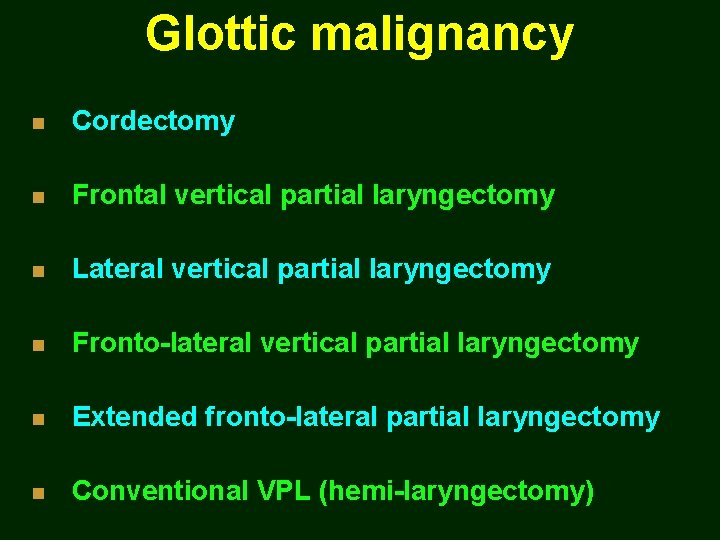
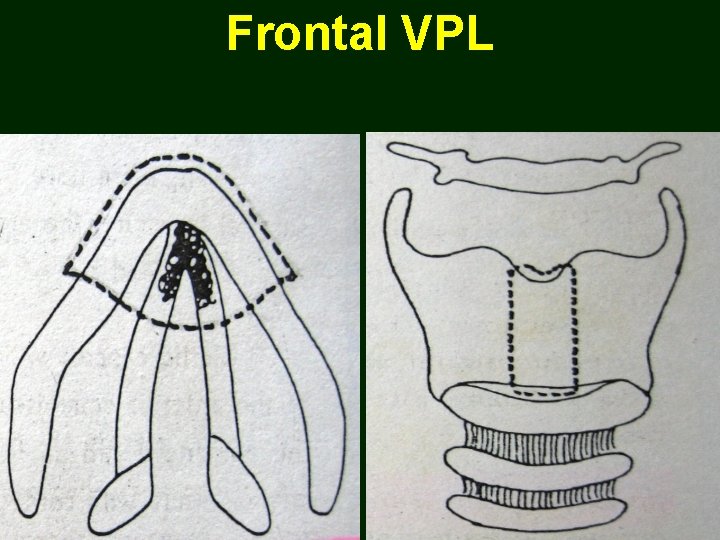
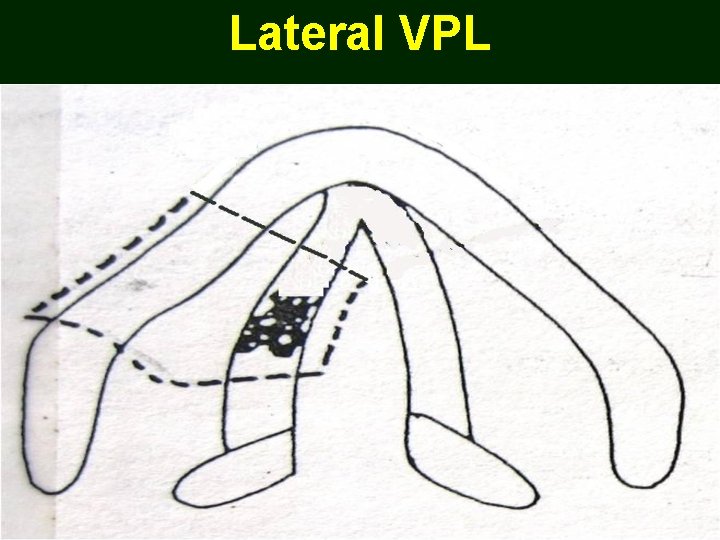
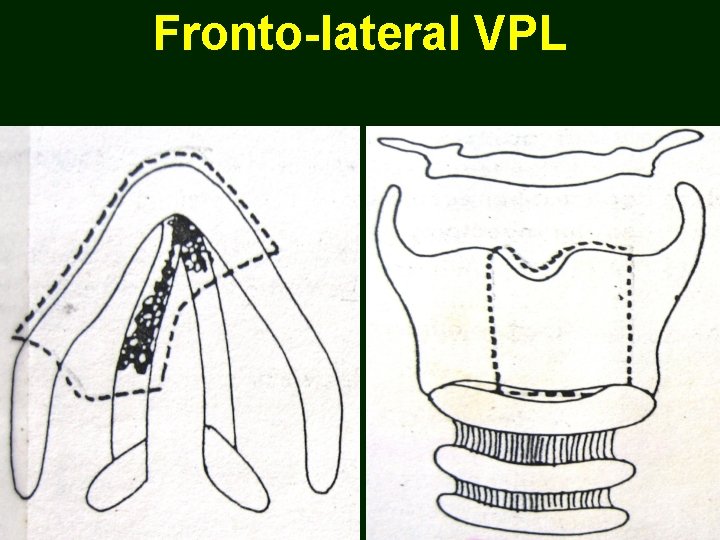
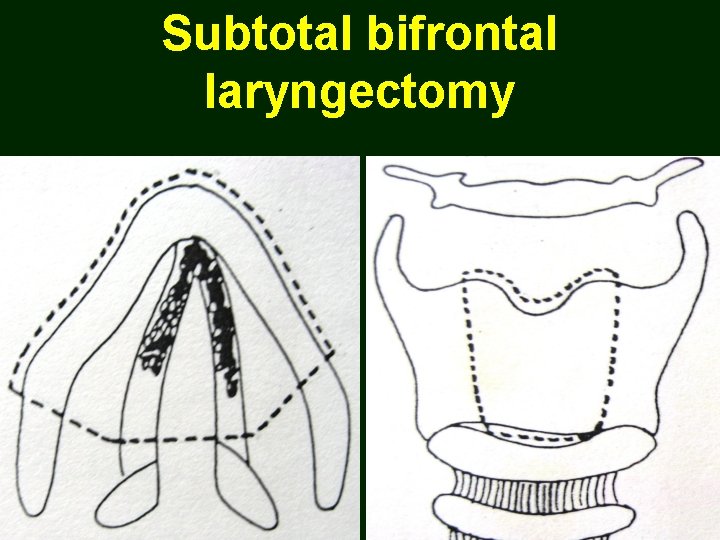
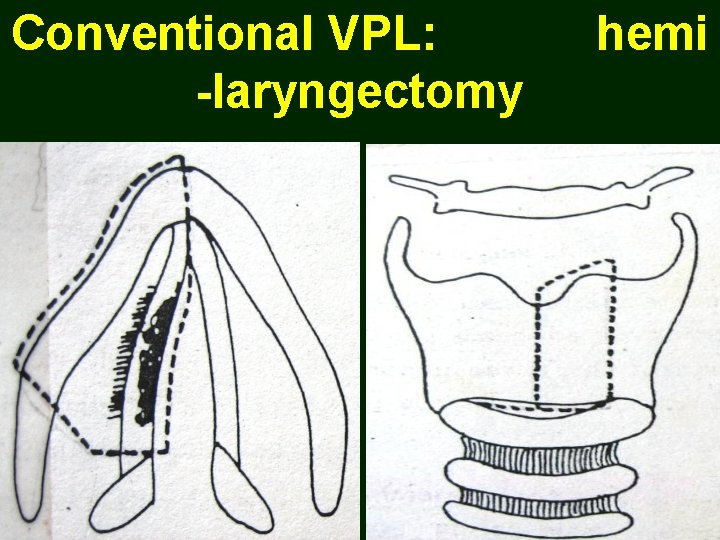
Glottic malignancy n Cordectomy n Frontal vertical partial laryngectomy n Lateral vertical partial laryngectomy n Fronto-lateral vertical partial laryngectomy n Extended fronto-lateral partial laryngectomy n Conventional VPL (hemi-laryngectomy)
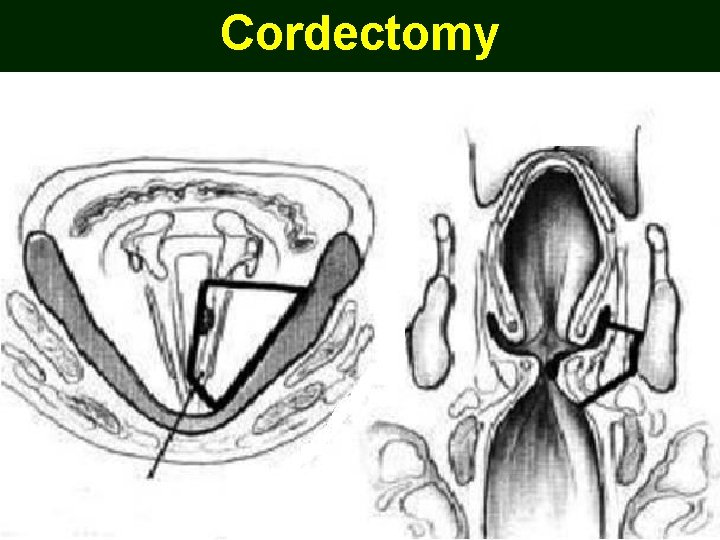
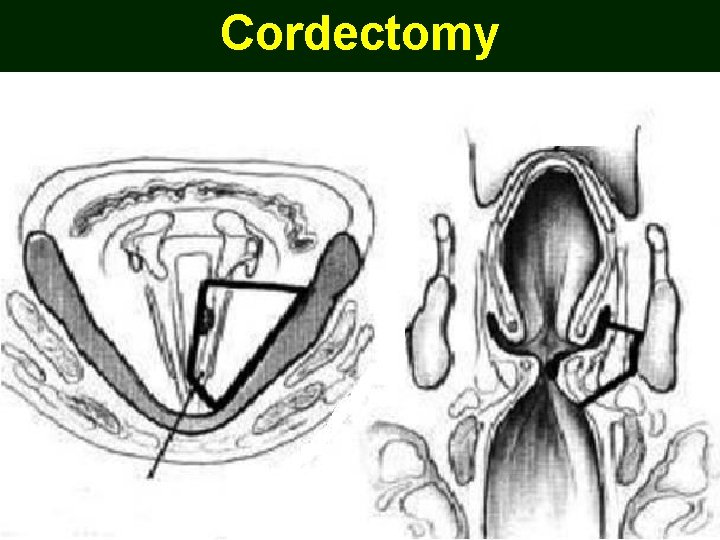
Cordectomy
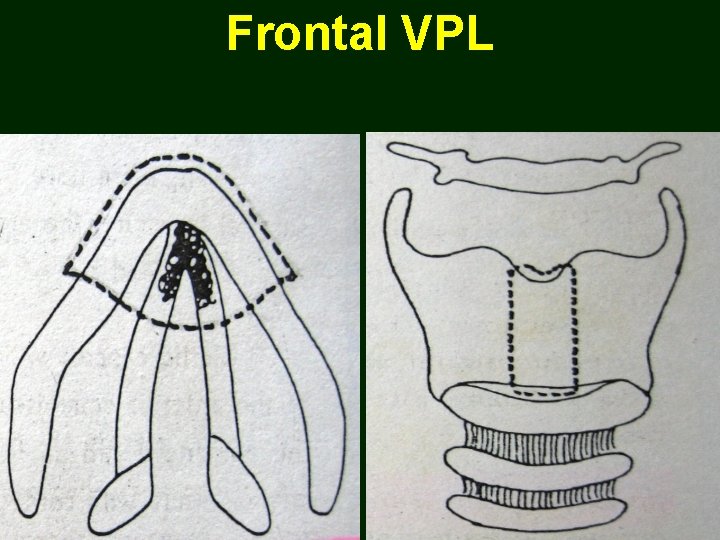
Frontal VPL
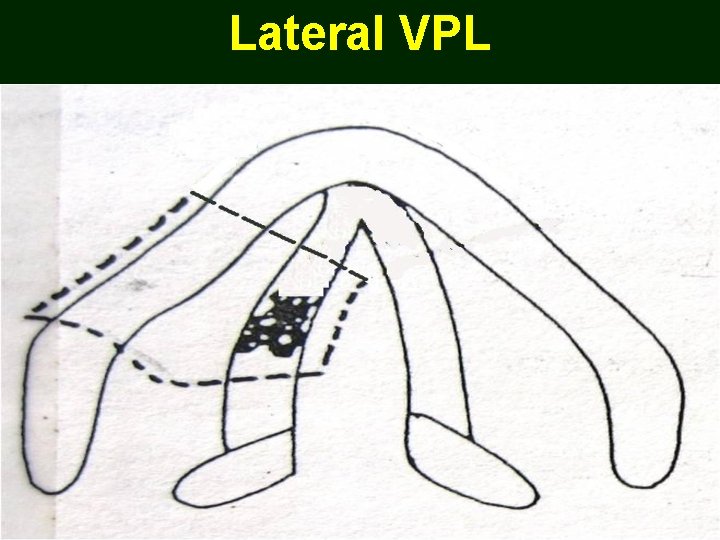
Lateral VPL
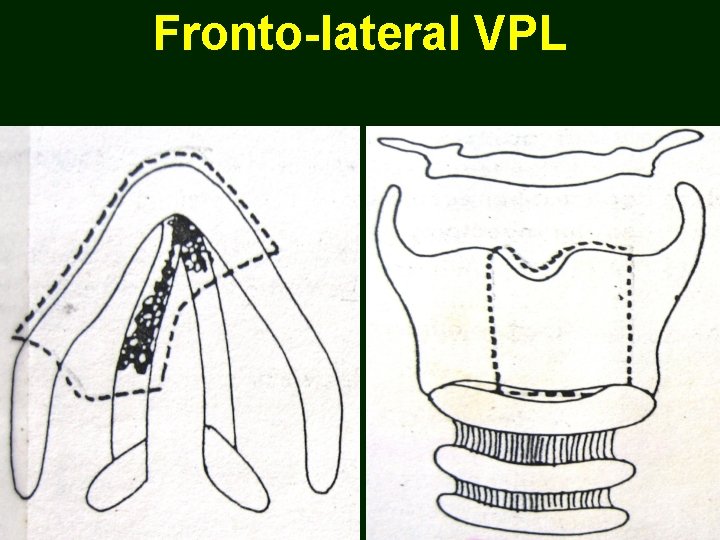
Fronto-lateral VPL
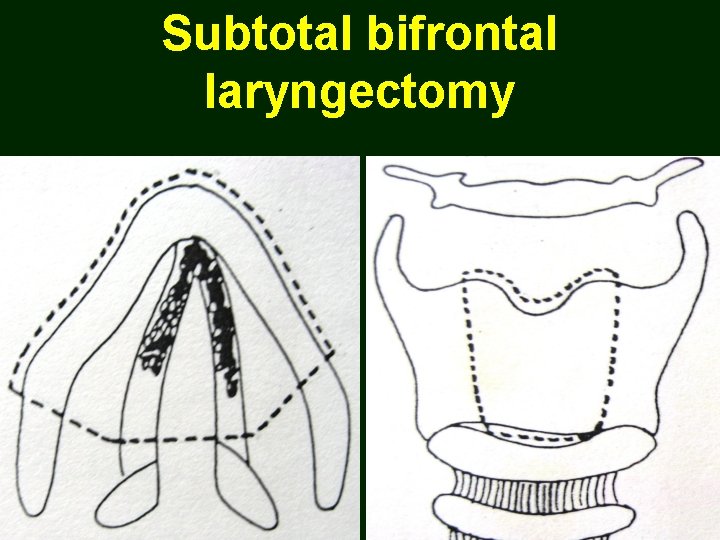
Subtotal bifrontal laryngectomy
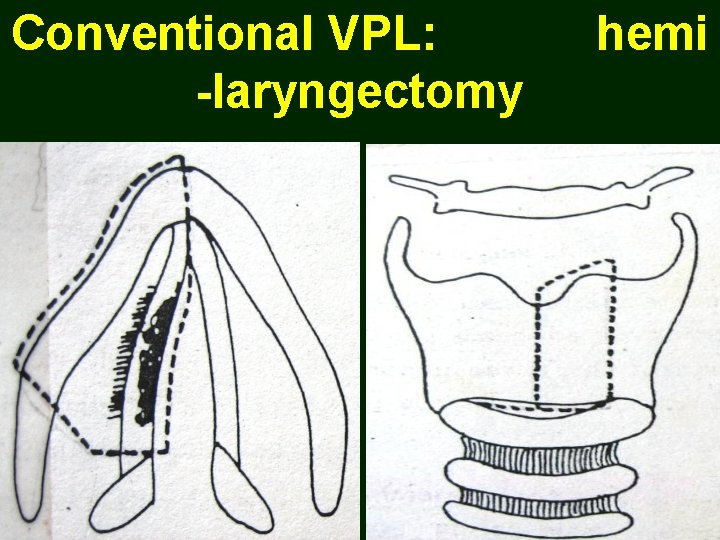
Conventional VPL: hemi -laryngectomy
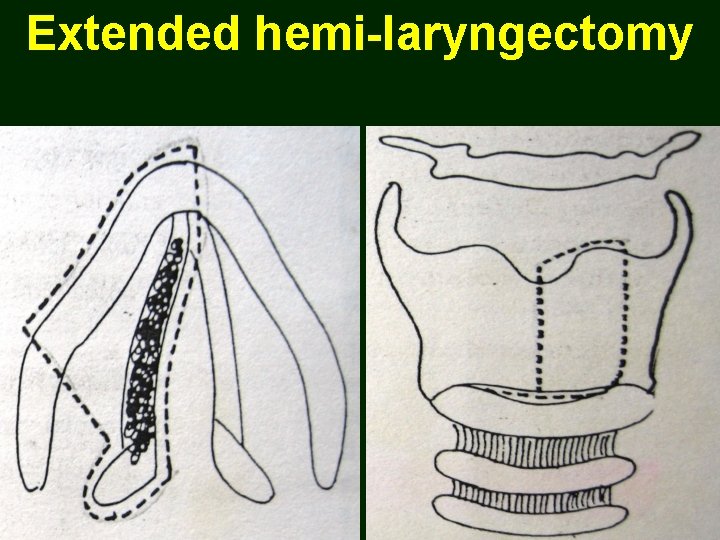
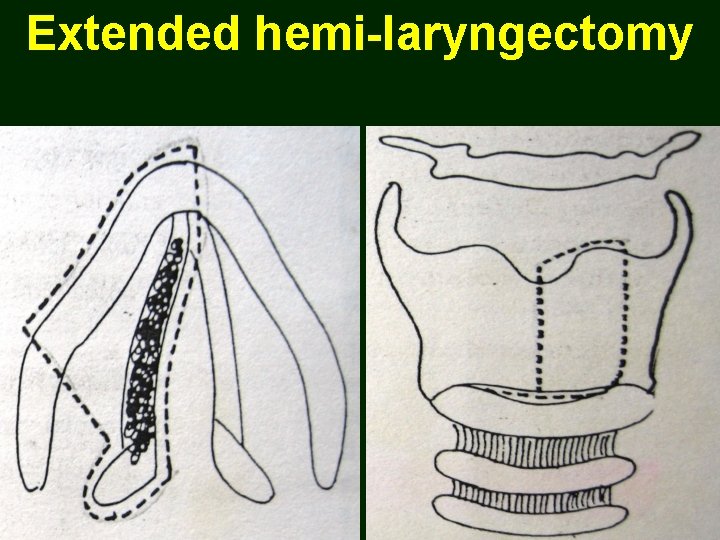
Extended hemi-laryngectomy
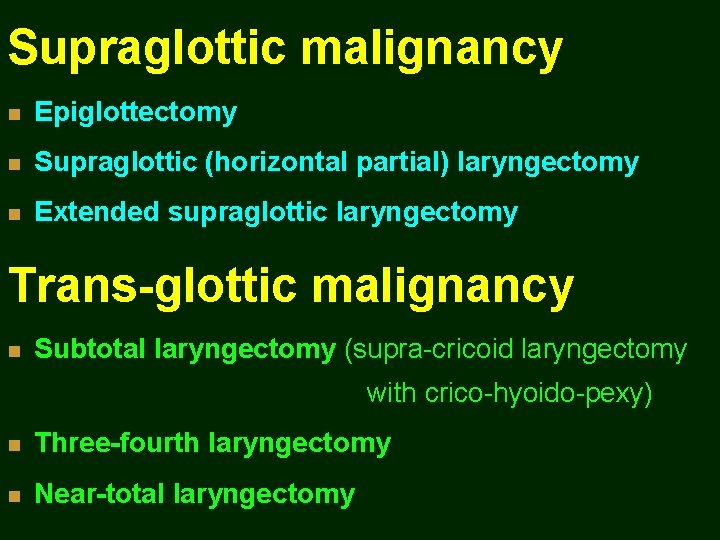
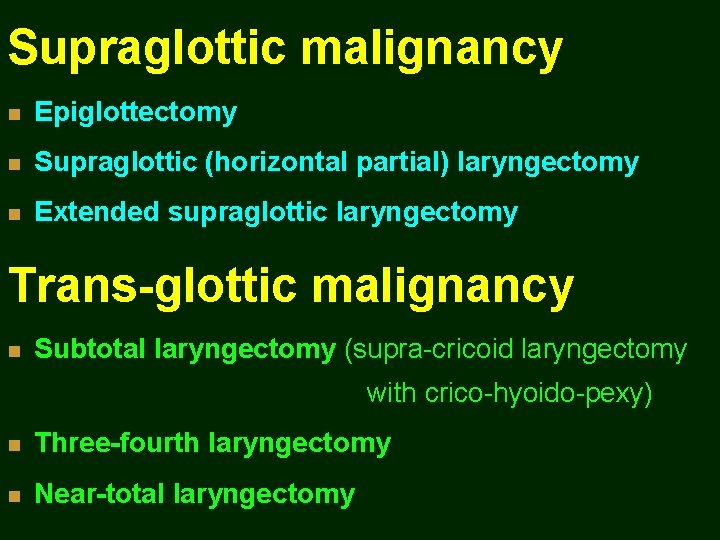
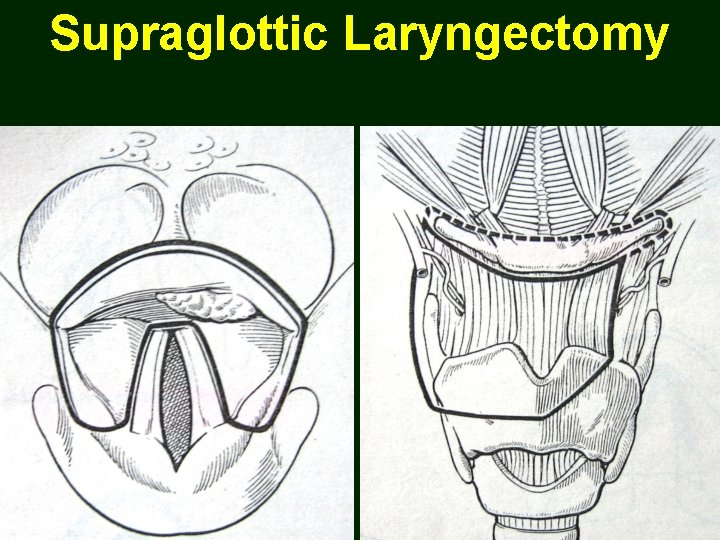
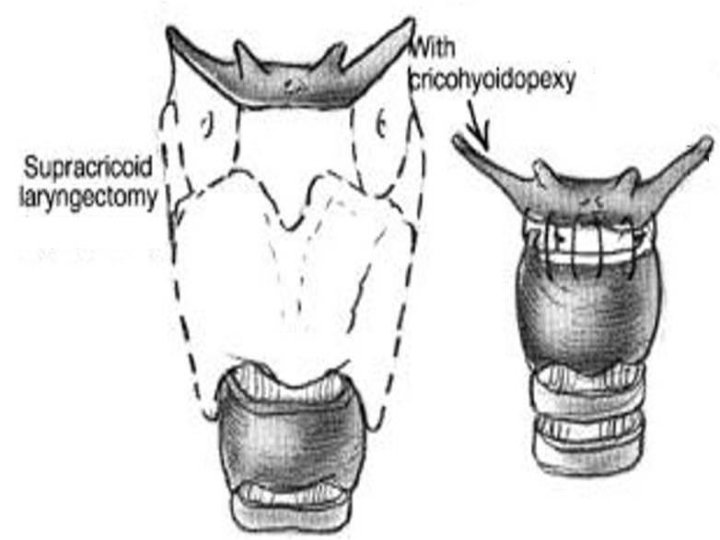
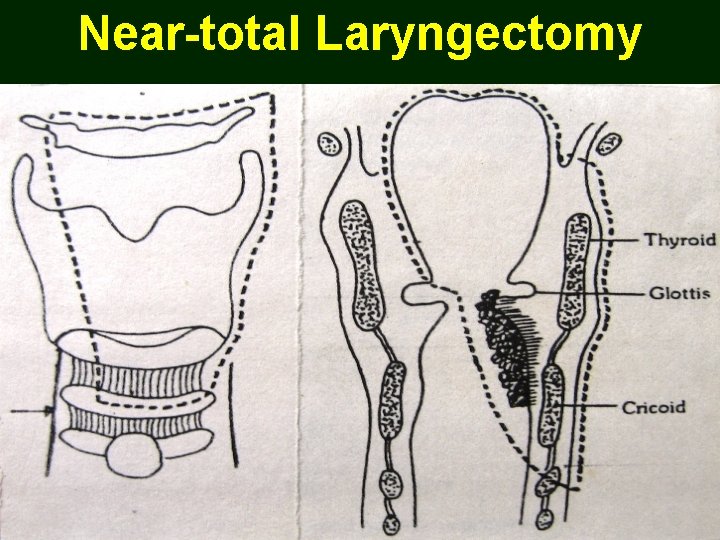
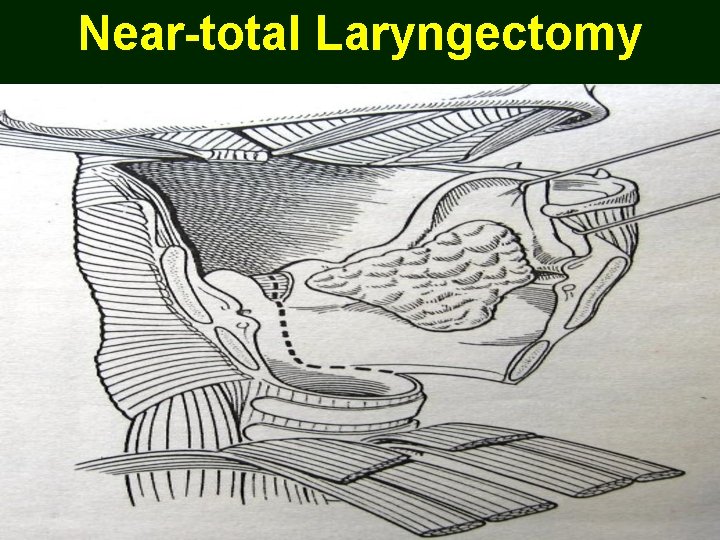
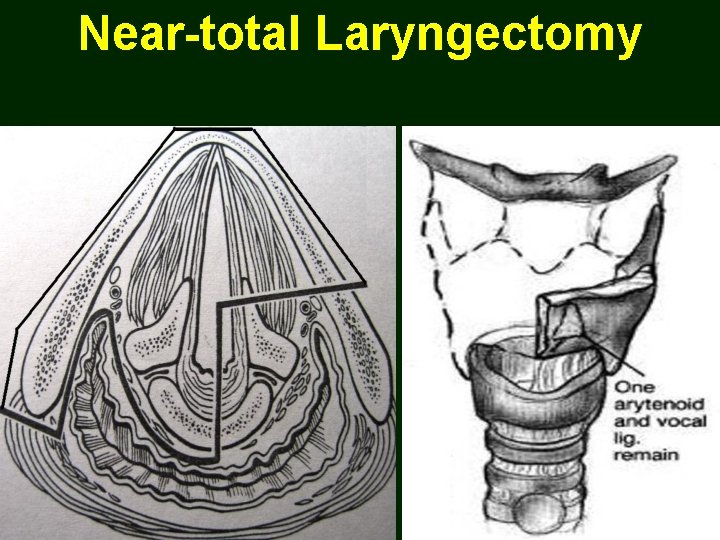
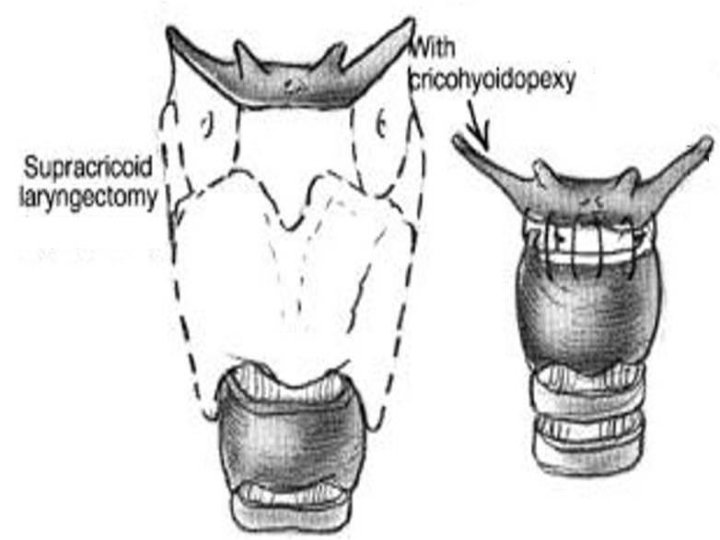
Supraglottic malignancy n Epiglottectomy n Supraglottic (horizontal partial) laryngectomy n Extended supraglottic laryngectomy Trans-glottic malignancy n Subtotal laryngectomy (supra-cricoid laryngectomy with crico-hyoido-pexy) n Three-fourth laryngectomy n Near-total laryngectomy
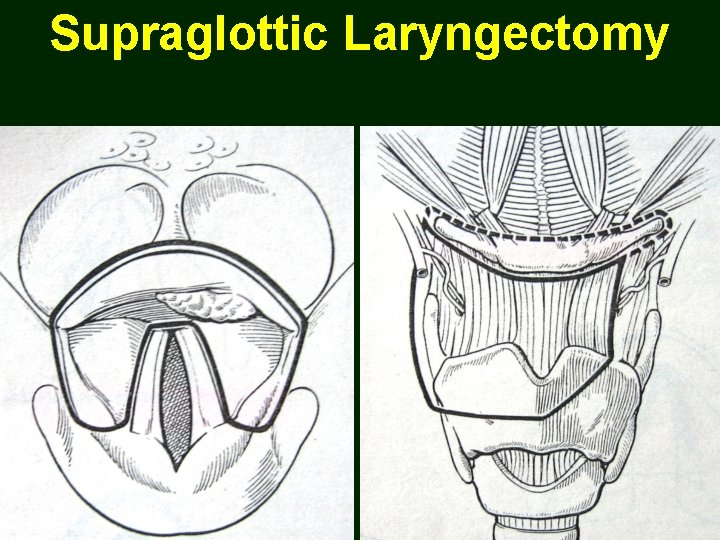
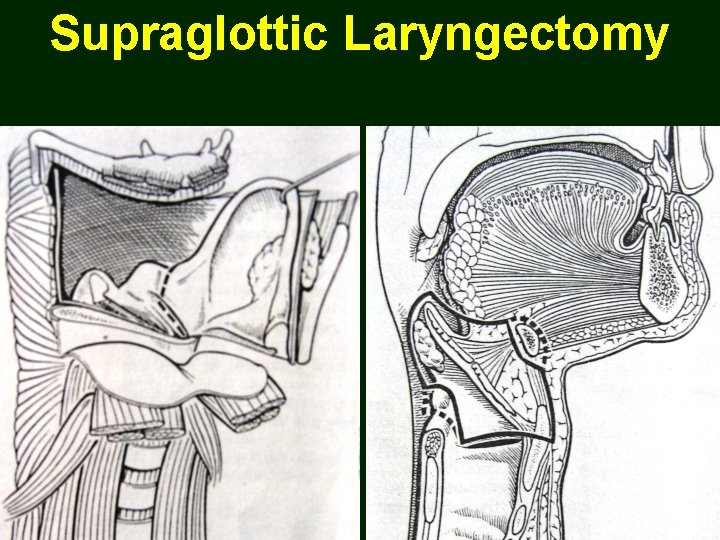
Supraglottic Laryngectomy
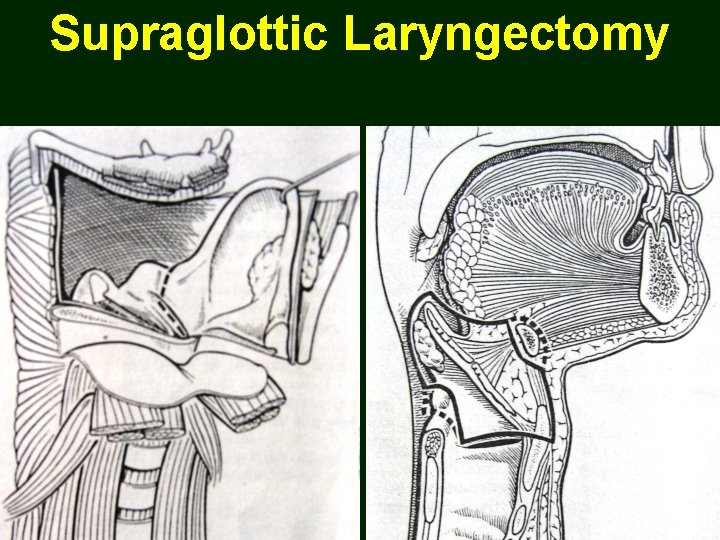
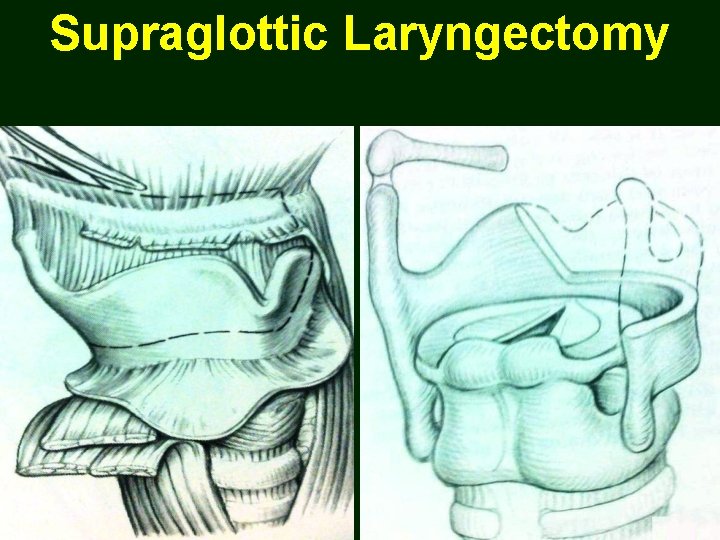
Supraglottic Laryngectomy
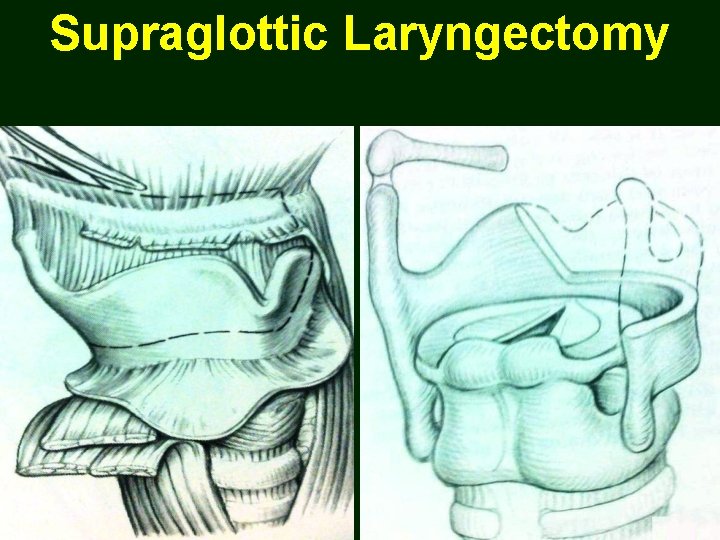
Supraglottic Laryngectomy

Three-fourth Laryngectomy
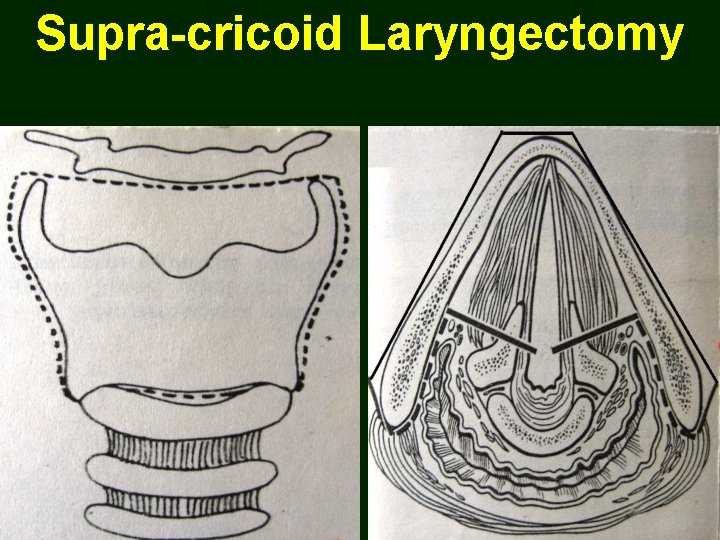
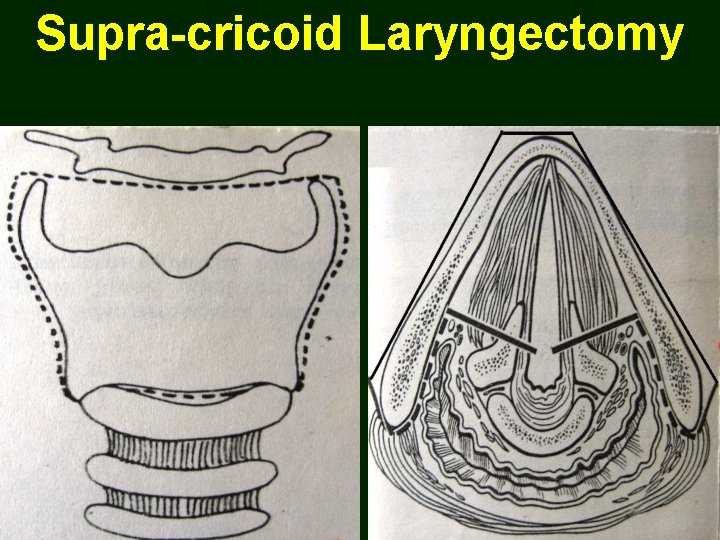
Supra-cricoid Laryngectomy
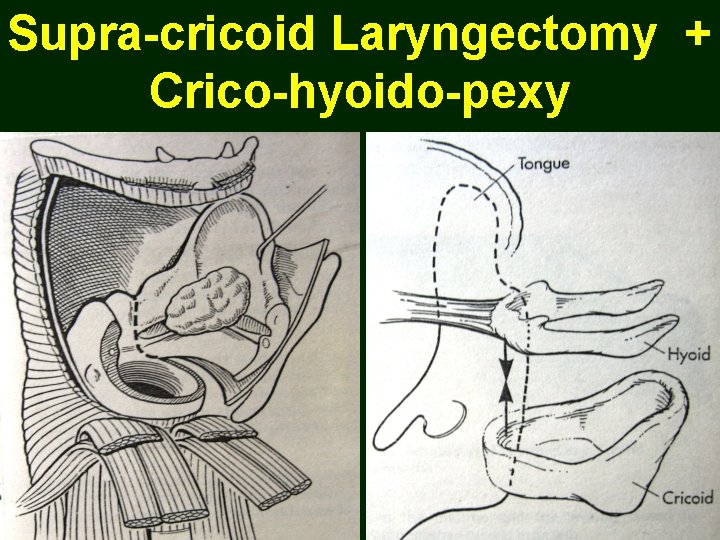
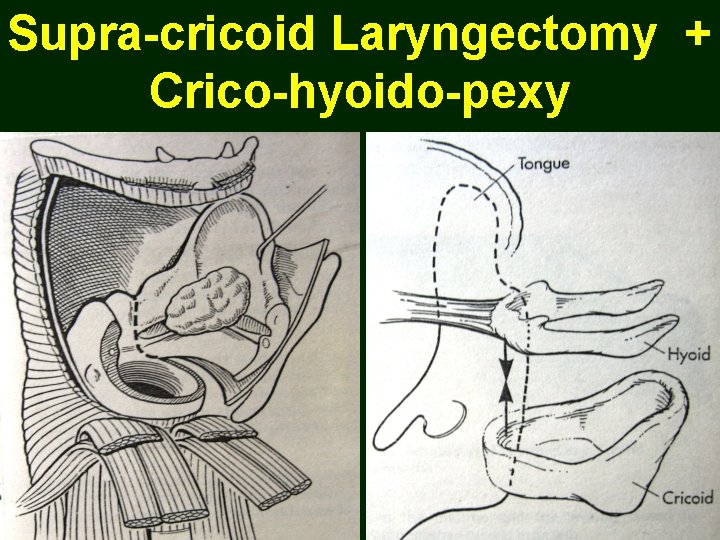
Supra-cricoid Laryngectomy + Crico-hyoido-pexy
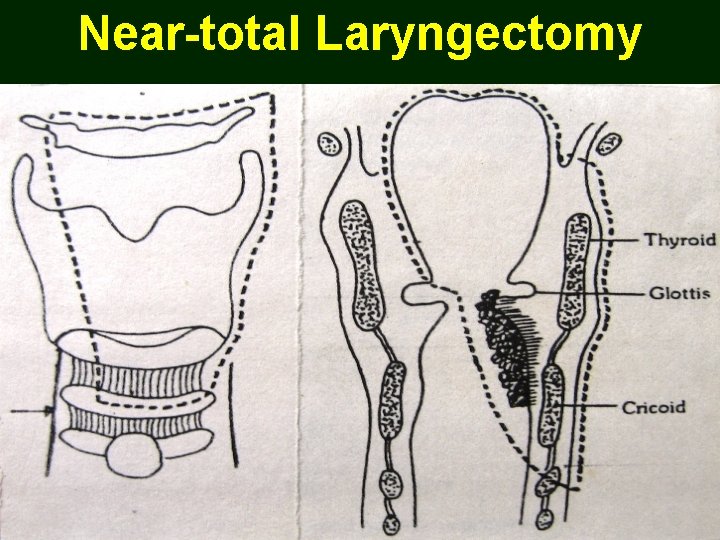
Near-total Laryngectomy
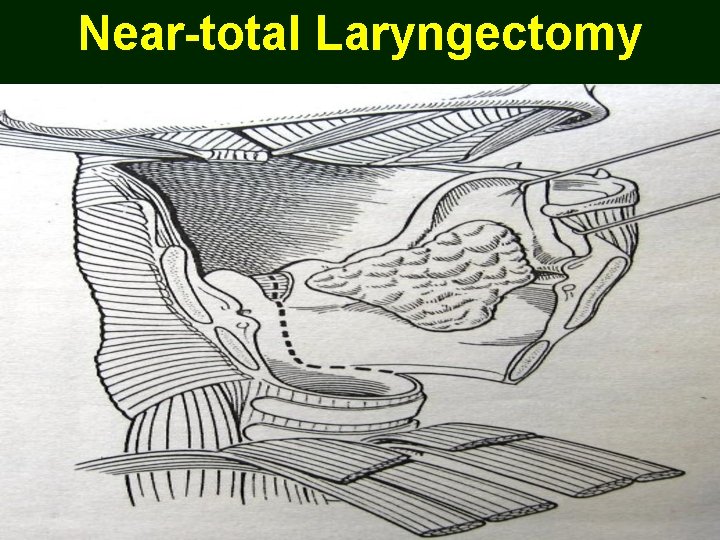
Near-total Laryngectomy
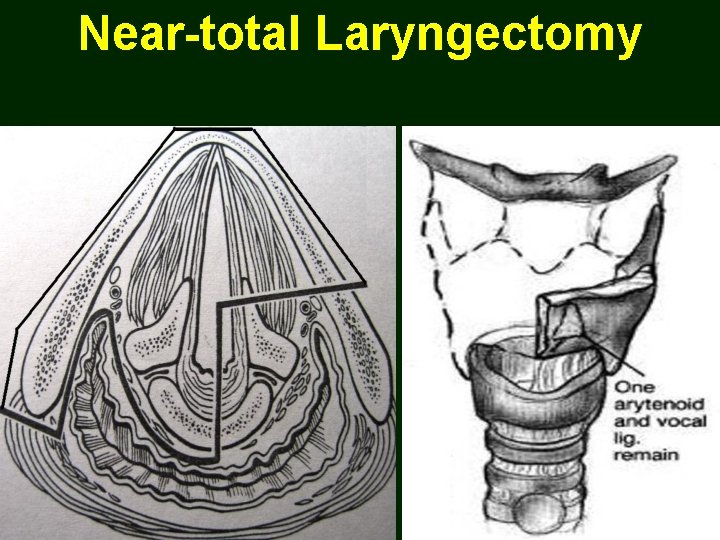
Near-total Laryngectomy
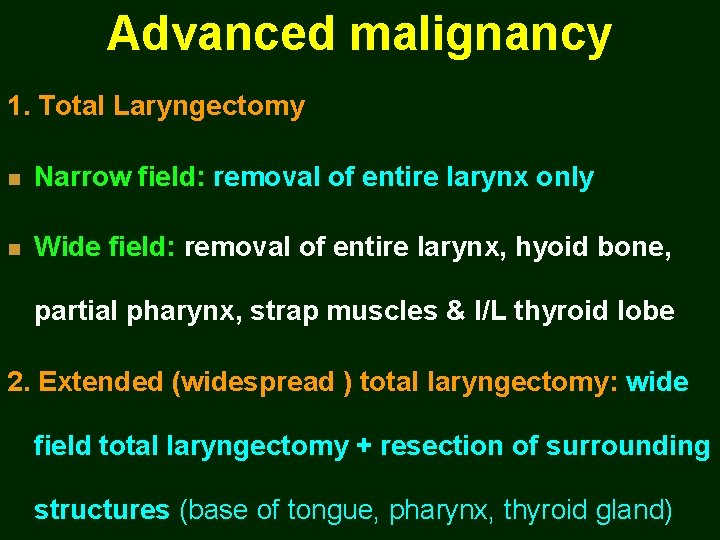
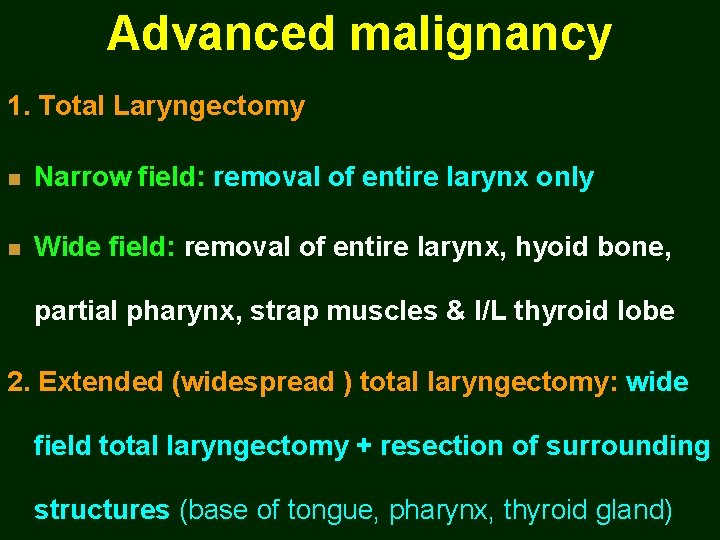
Advanced malignancy 1. Total Laryngectomy n Narrow field: removal of entire larynx only n Wide field: removal of entire larynx, hyoid bone, partial pharynx, strap muscles & I/L thyroid lobe 2. Extended (widespread ) total laryngectomy: wide field total laryngectomy + resection of surrounding structures (base of tongue, pharynx, thyroid gland)
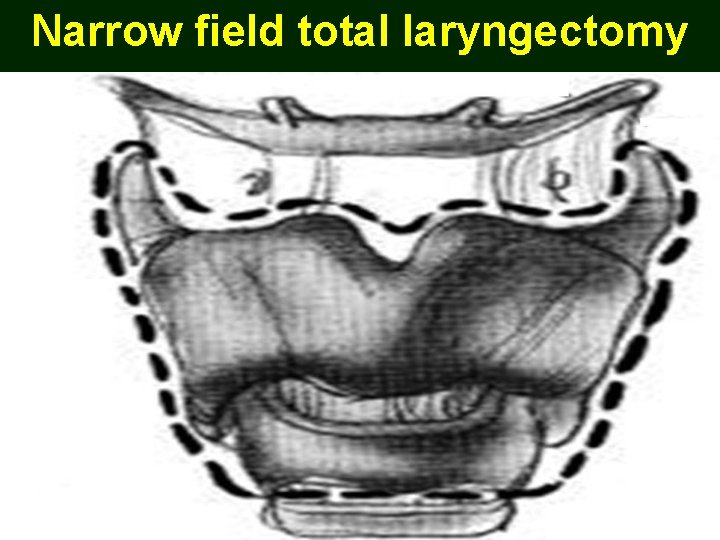
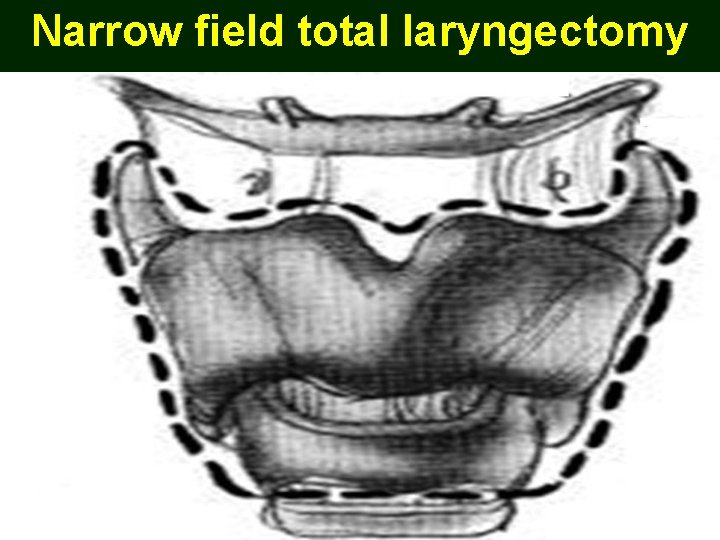
Narrow field total laryngectomy
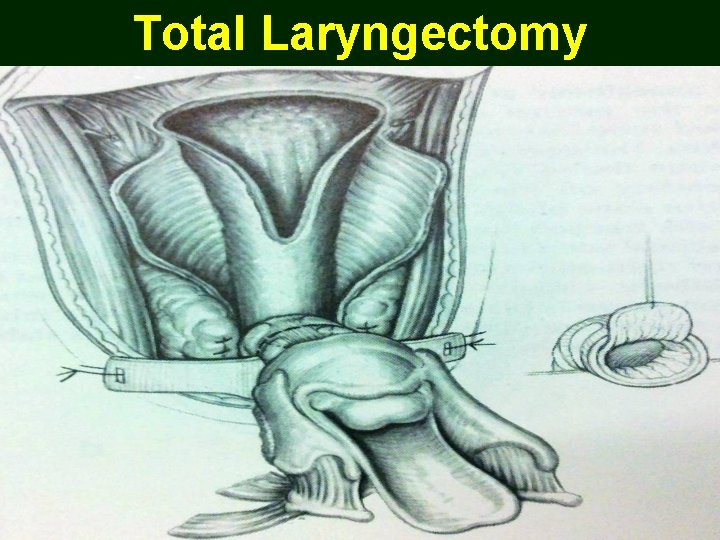
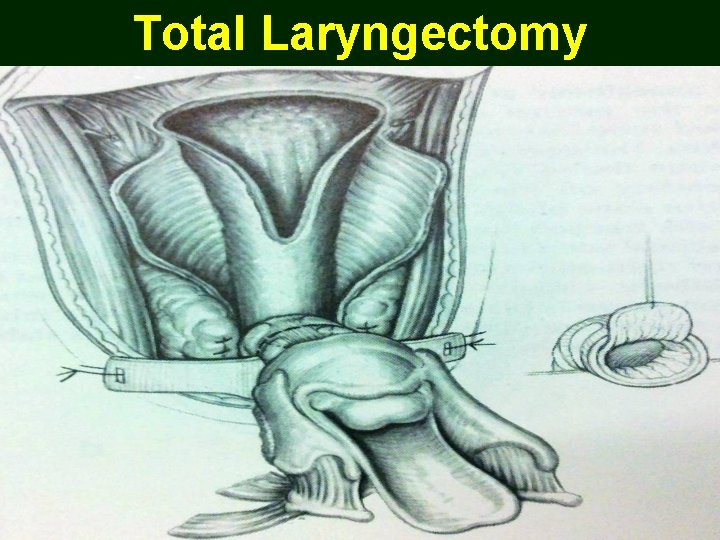
Total Laryngectomy
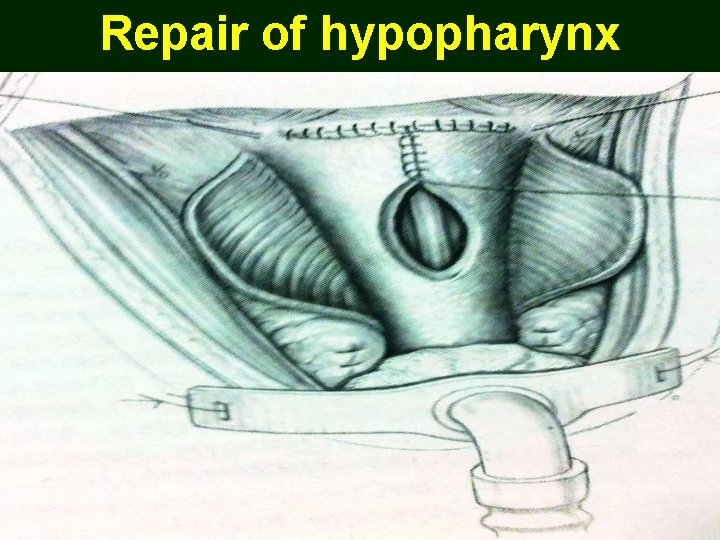
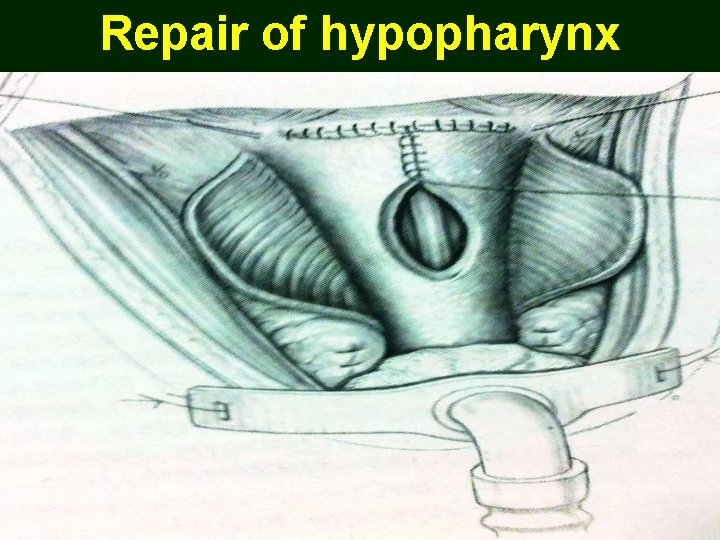
Repair of hypopharynx
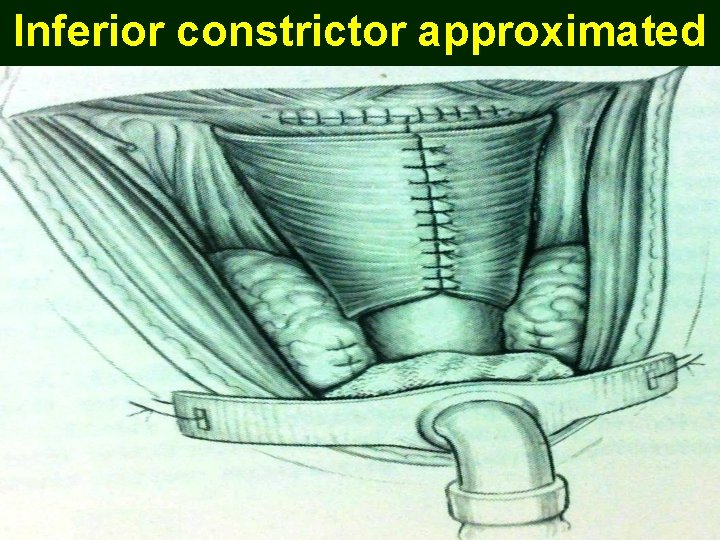
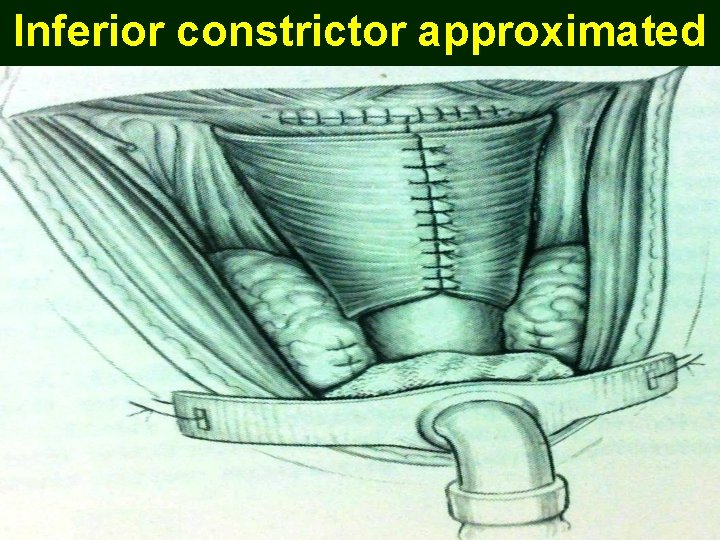
Inferior constrictor approximated
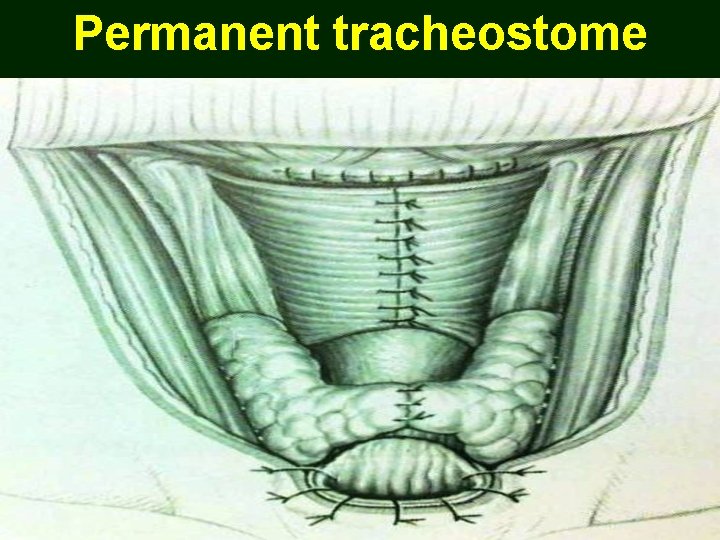
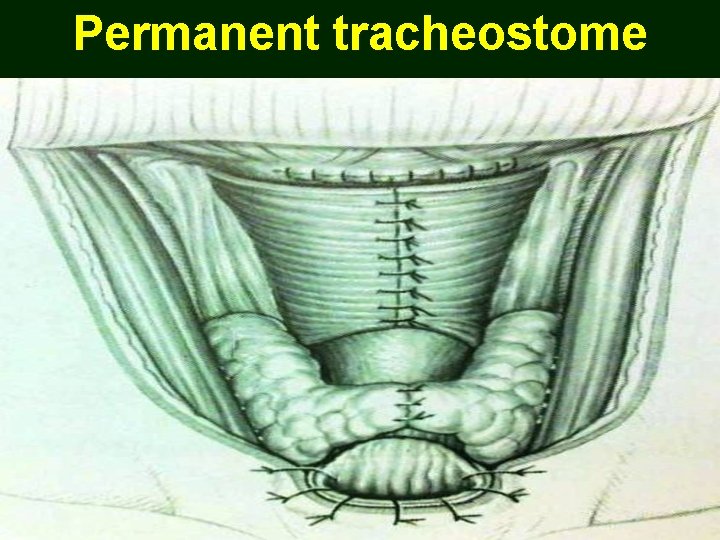
Permanent tracheostome

Laryngectomy specimens

Treatment planning
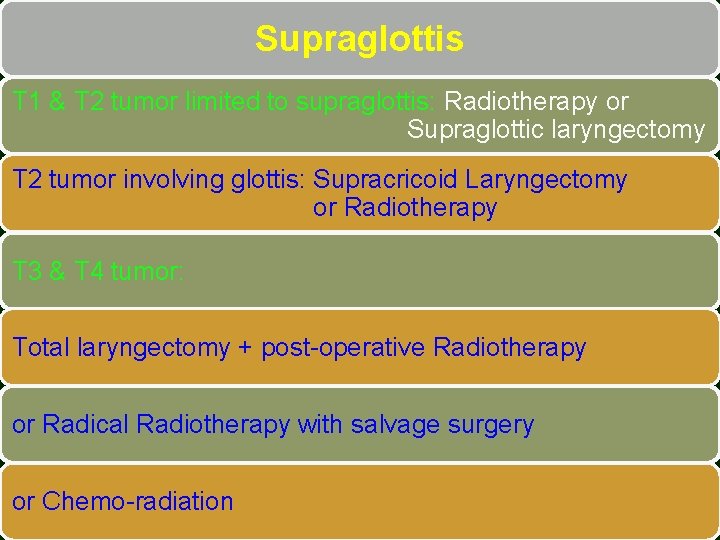
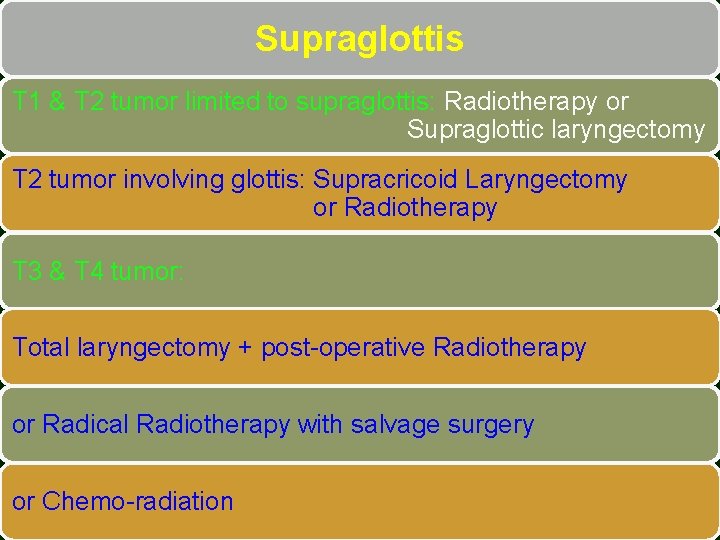
Supraglottis T 1 & T 2 tumor limited to supraglottis: Radiotherapy or Supraglottic laryngectomy T 2 tumor involving glottis: Supracricoid Laryngectomy or Radiotherapy T 3 & T 4 tumor: Total laryngectomy + post-operative Radiotherapy or Radical Radiotherapy with salvage surgery or Chemo-radiation
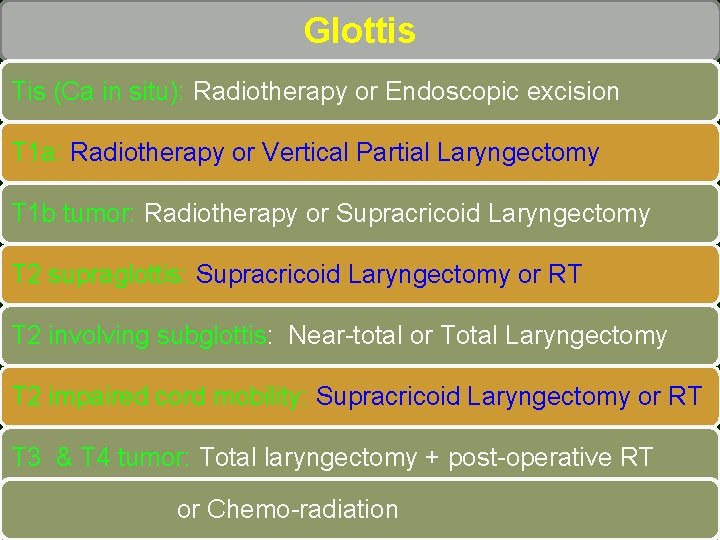
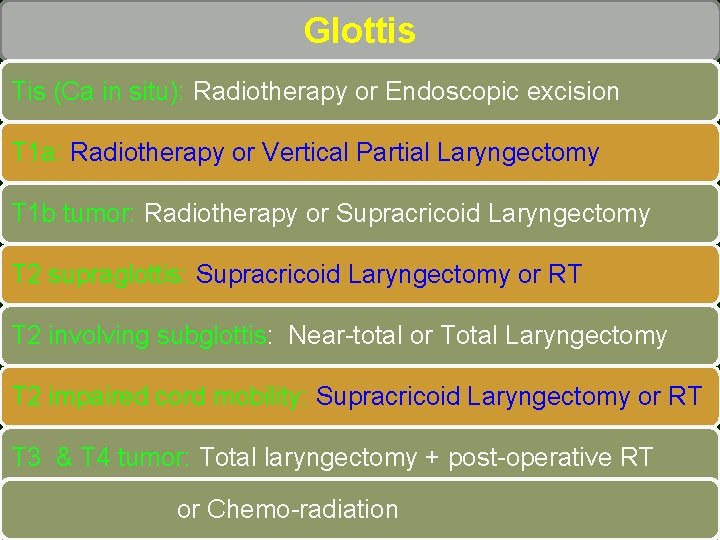
Glottis Tis (Ca in situ): Radiotherapy or Endoscopic excision T 1 a: Radiotherapy or Vertical Partial Laryngectomy T 1 b tumor: Radiotherapy or Supracricoid Laryngectomy T 2 supraglottis: Supracricoid Laryngectomy or RT T 2 involving subglottis: Near-total or Total Laryngectomy T 2 impaired cord mobility: Supracricoid Laryngectomy or RT T 3 & T 4 tumor: Total laryngectomy + post-operative RT or Chemo-radiation or Radical Radiotherapy with salvage surgery
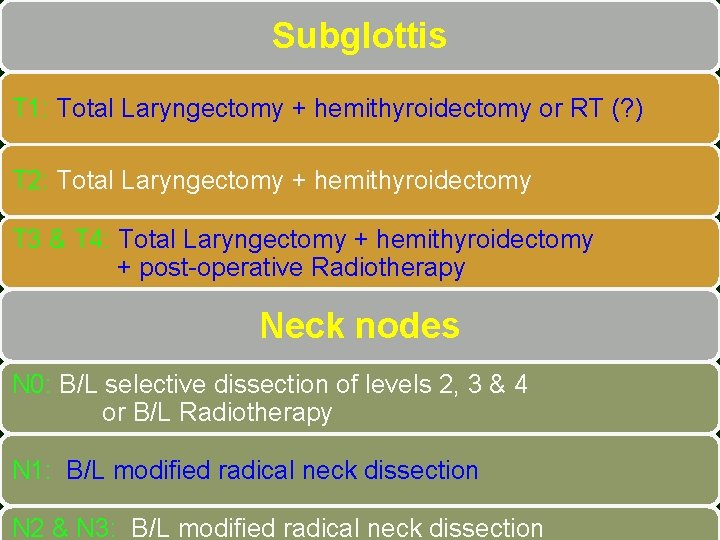
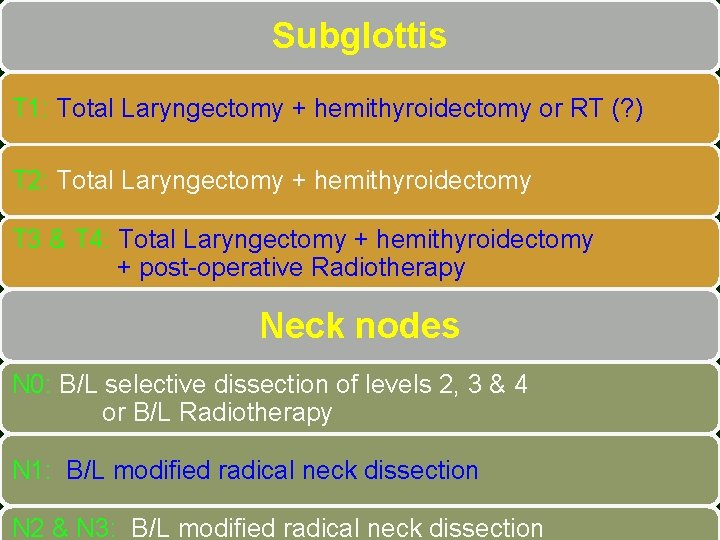
Subglottis T 1: Total Laryngectomy + hemithyroidectomy or RT (? ) T 2: Total Laryngectomy + hemithyroidectomy T 3 & T 4: Total Laryngectomy + hemithyroidectomy + post-operative Radiotherapy Neck nodes N 0: B/L selective dissection of levels 2, 3 & 4 or B/L Radiotherapy N 1: B/L modified radical neck dissection N 2 & N 3: B/L modified radical neck dissection

Voice Rehabilitation
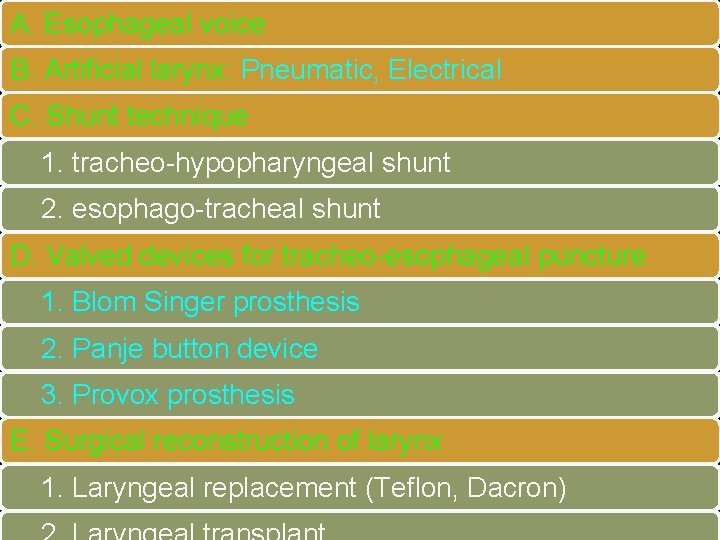
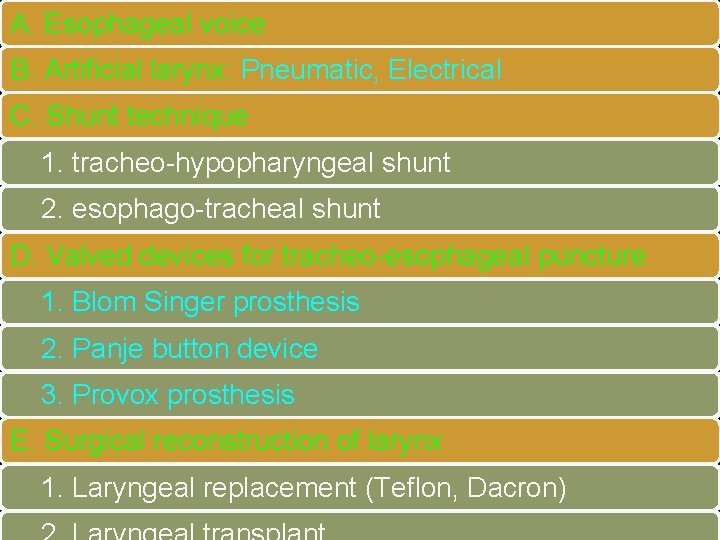
A. Esophageal voice B. Artificial larynx: Pneumatic, Electrical C. Shunt technique 1. tracheo-hypopharyngeal shunt 2. esophago-tracheal shunt D. Valved devices for tracheo-esophageal puncture 1. Blom Singer prosthesis 2. Panje button device 3. Provox prosthesis E. Surgical reconstruction of larynx 1. Laryngeal replacement (Teflon, Dacron)
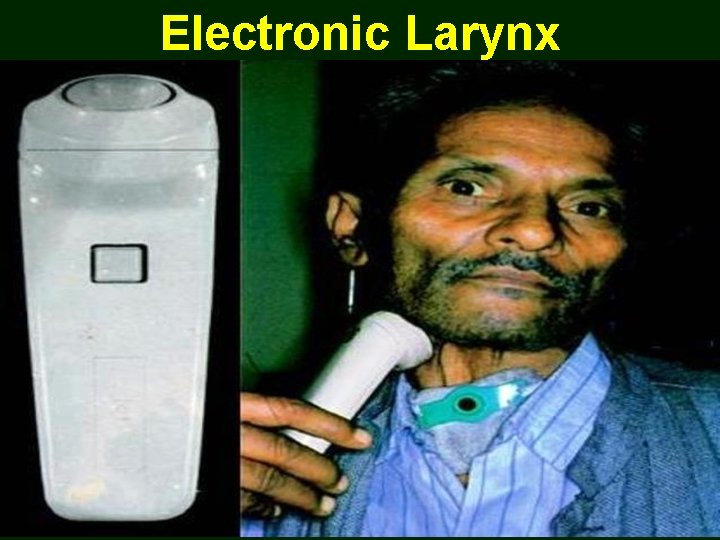
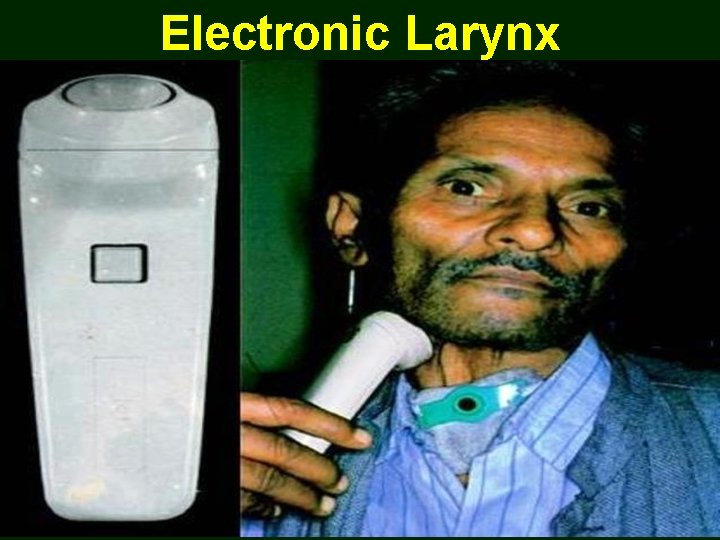
Electronic Larynx
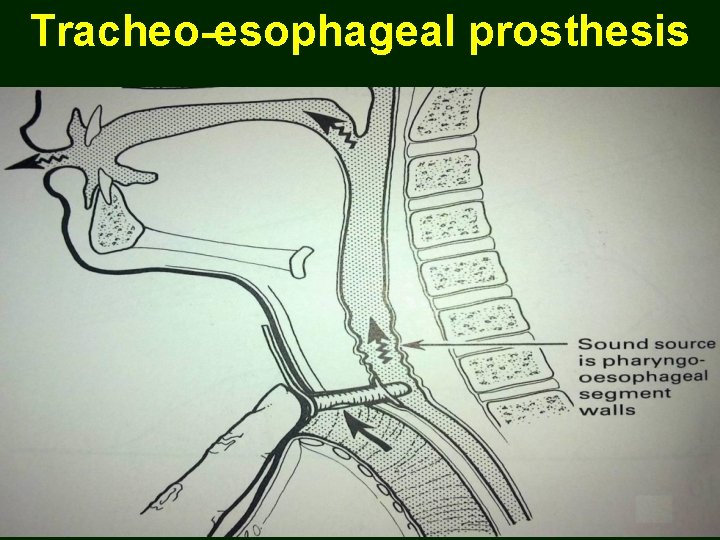
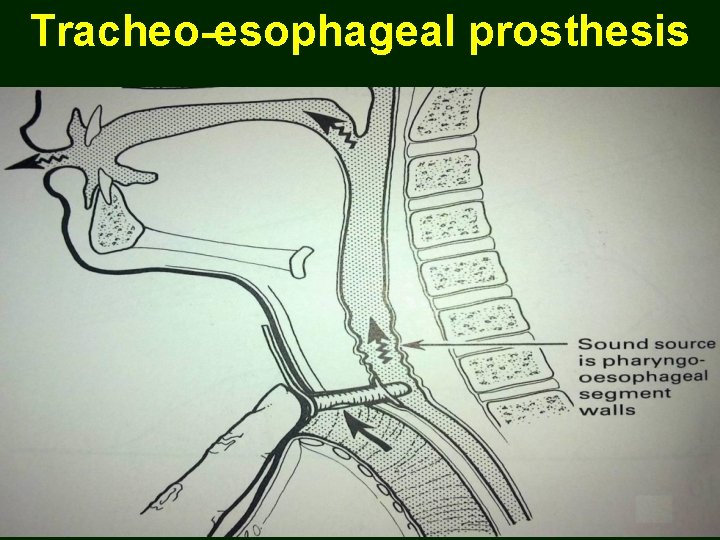
Tracheo-esophageal prosthesis
Palliative Care Used in later stages to ameliorate symptoms 1. Debulking surgery (Laser-assisted) 2. Radiotherapy (short-course) 3. Chemotherapy 4. Tracheostomy 5. Counseling

Thank You