LAPAROSCOPIC PARTIAL NEPHRECTOMY AS A NEPHRON SPARING SURGERY

- Slides: 31
LAPAROSCOPIC PARTIAL NEPHRECTOMY AS A NEPHRON SPARING SURGERY PROF. DR. METE KİLCİLER DEPARTMENT OF UROLOGY, SCHOOL OF MEDICINE, BAHÇEŞEHİR UNIVERSITY
Introduction �The incidence of small incidental renal tumors is increasing �Nephron-sparing surgery -new trend �NSS - 4 cm or small localized RCC (Novick) �Open partial nephrectomy - gold standard
Introduction �The first LPN was described in 1993 (J. Endourol, 7: 521, 1993) �It is an advanced laparoscopic procedure �Dissection, renal hilum clamping, renal parenchymal hemostasis, pelvicaliceal reconstruction and renorraphy �Steps are essentially duplicating those of open partial nephrectomy
Indications Classical indications: �Small renal tumors �Peripheral location �Superficial �Exophytic As the surgeon’s experience increases: �more complex tumors can be done �tumors invading the parenchyma to the collecting system, or renal sinus �complete intrarenal tumors �tumor in a solitary kidney
Contraindications �Renal vein thrombus �Multiple renal tumors �Locally advanced disease �Bleeding diathesis �Morbid obesity �Prior renal surgery �General C/I to laparoscopic surgery
C/I to lap. surgery Absolute contraindications: �Uncorrectable coagulopathy �Intestinal obstruction �Abdominal wall infection �Massive hemoperitonium �Peritonitis �Suspected malignant ascites
C/I to lap. surgery Relative contraindications: �Morbid obesity �Prior abdominal or pelvic surgery �Pelvic fibrosis �Organomegaly �Ascites �Pregnancy �Hernia �Iliac or aortic aneurysm
Pre-op. Preparation �Same as for open surgery �Basic blood count �Accurate staging �Three dimensional CT scan
Pre-op. Preparation �Informed consent (for lap and open) �Bowel prep (empty bowel) �Foley catheter (empty bladder) �NG or OG tube (empty stomach) �DVT prophylaxis (sequential compression stockings) �+/- Antibiotics �Shave prep
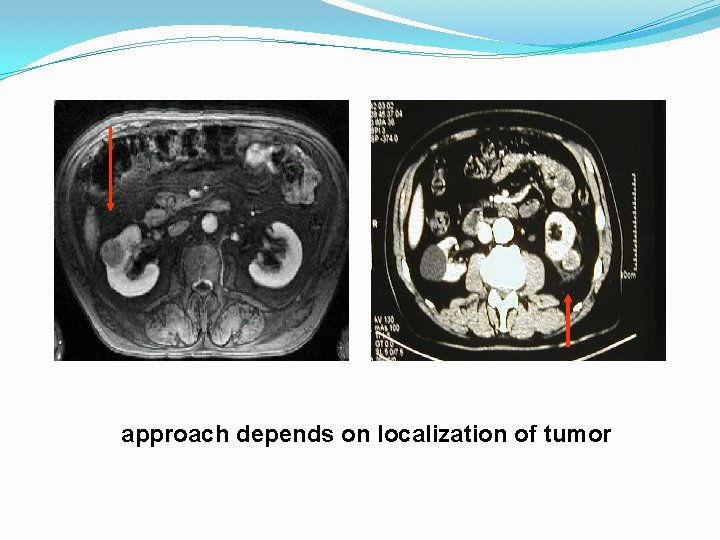
Surgical technique Transperitoneal • anterior • antero-lateral • upper pole-apical Retroperitoneal • posterior • posterolateral • Lower pole
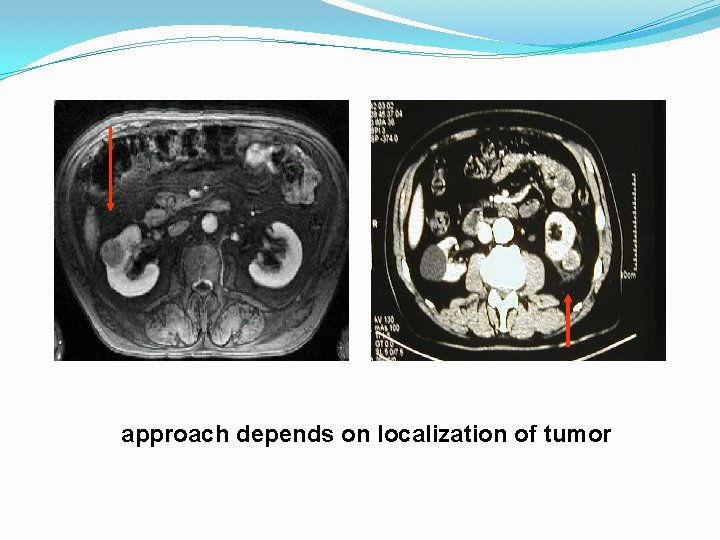
approach depends on localization of tumor
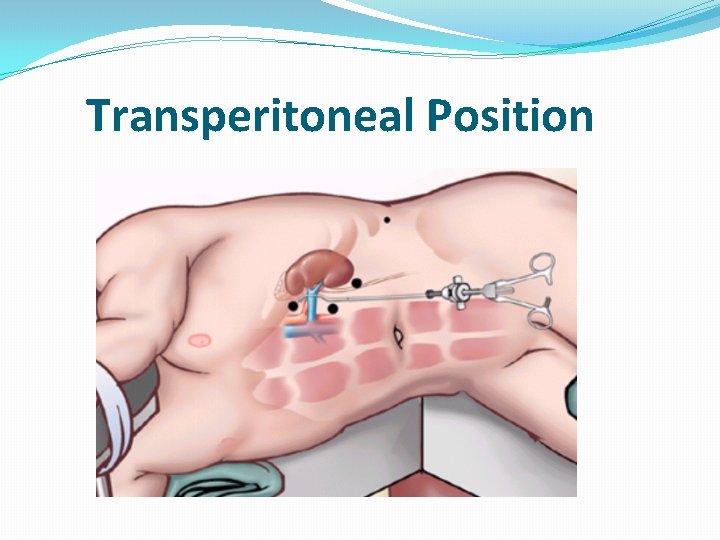
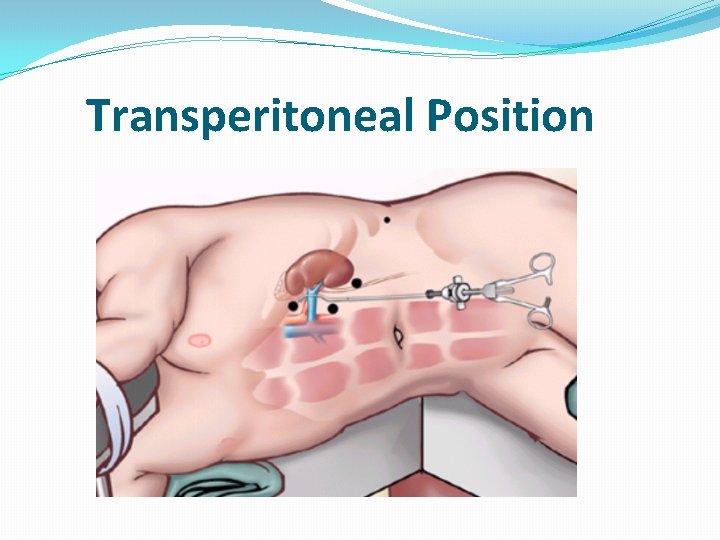
Transperitoneal Position
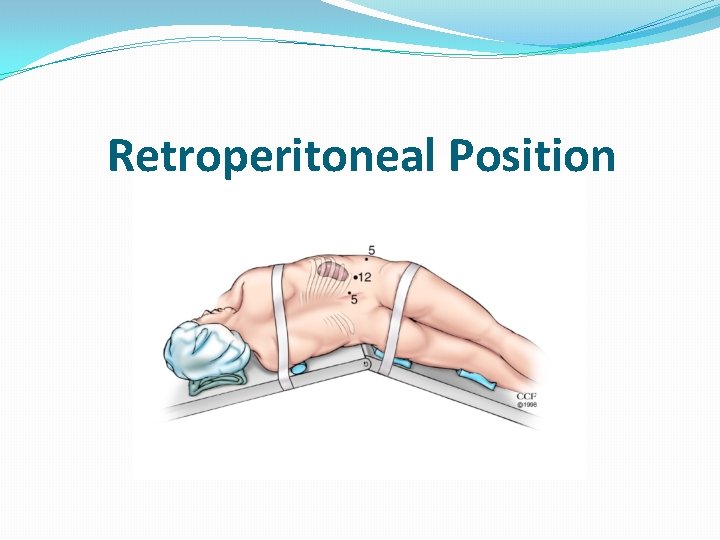
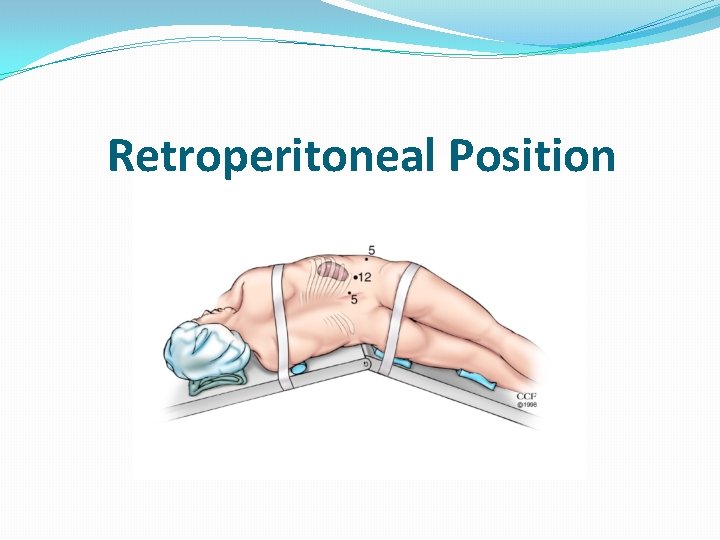
Retroperitoneal Position
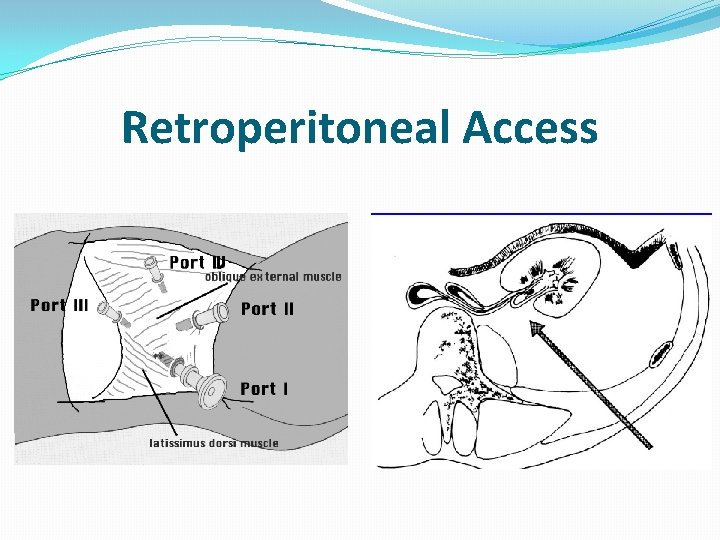
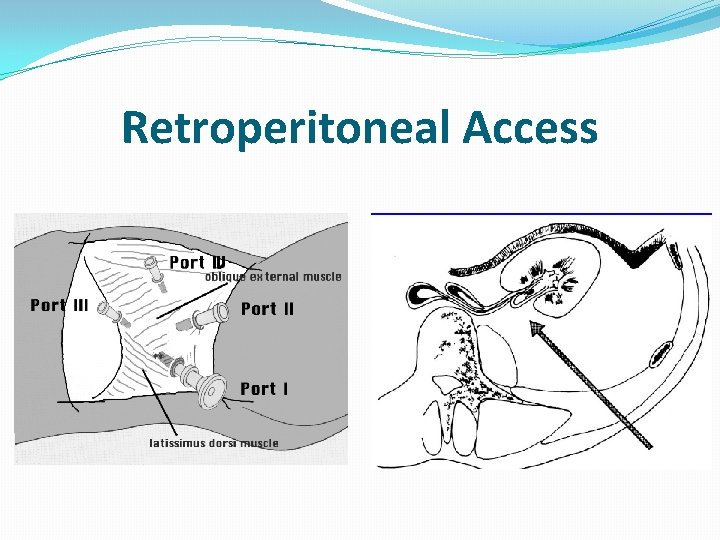
Retroperitoneal Access
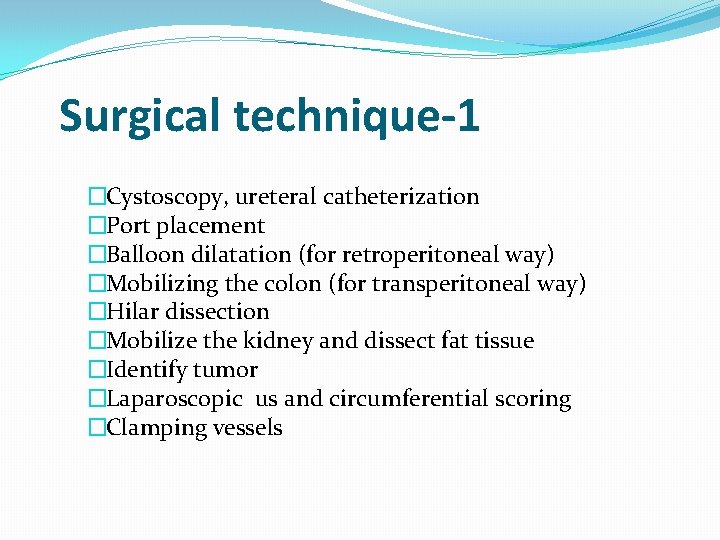
Surgical technique-1 �Cystoscopy, ureteral catheterization �Port placement �Balloon dilatation (for retroperitoneal way) �Mobilizing the colon (for transperitoneal way) �Hilar dissection �Mobilize the kidney and dissect fat tissue �Identify tumor �Laparoscopic us and circumferential scoring �Clamping vessels
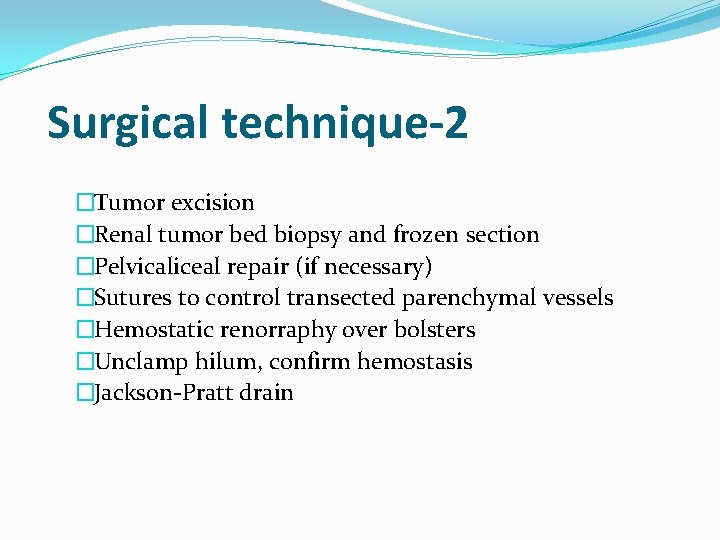
Surgical technique-2 �Tumor excision �Renal tumor bed biopsy and frozen section �Pelvicaliceal repair (if necessary) �Sutures to control transected parenchymal vessels �Hemostatic renorraphy over bolsters �Unclamp hilum, confirm hemostasis �Jackson-Pratt drain
Hemostatic techniques �Argon beam coagulator �Electrocautery �Harmonic scalpel �Fibrin glue �Gelatin sponges �Ultrasonic surgical aspirator �Laser �Microwave tissue coagulator
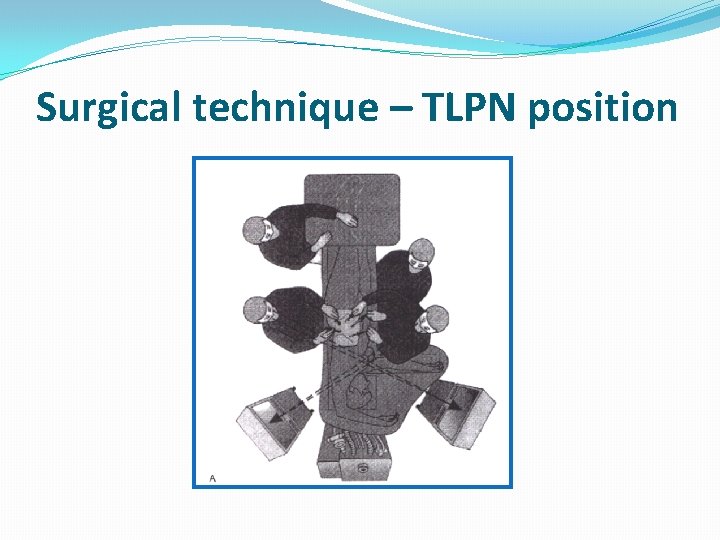
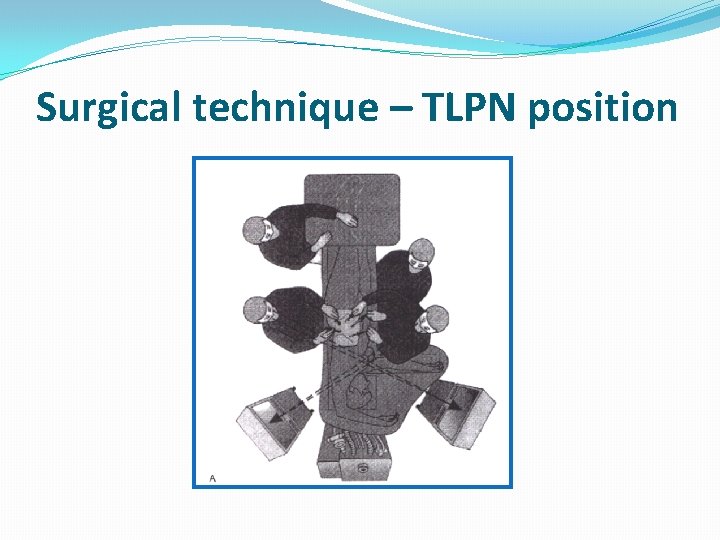
Surgical technique – TLPN position
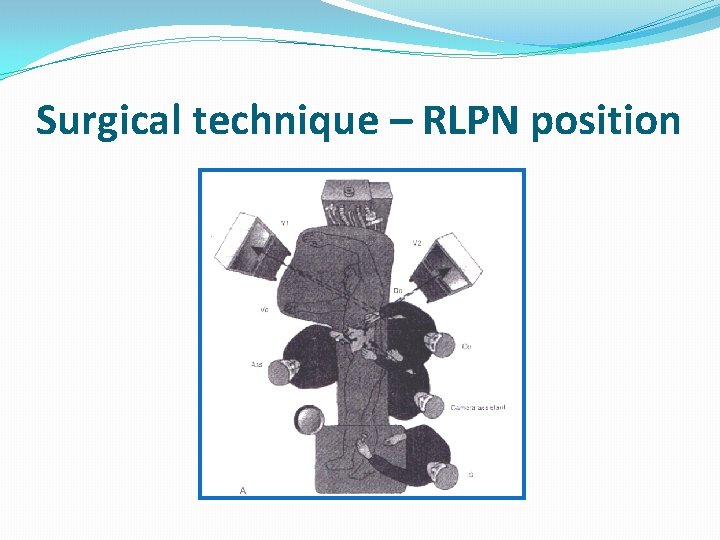
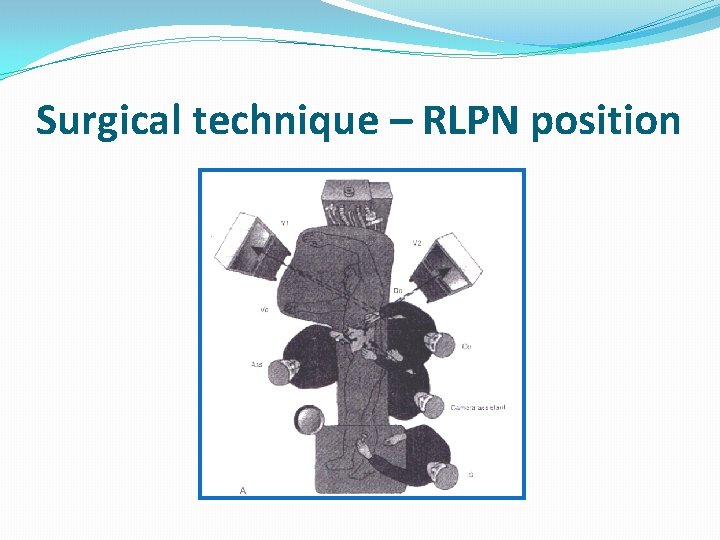
Surgical technique – RLPN position
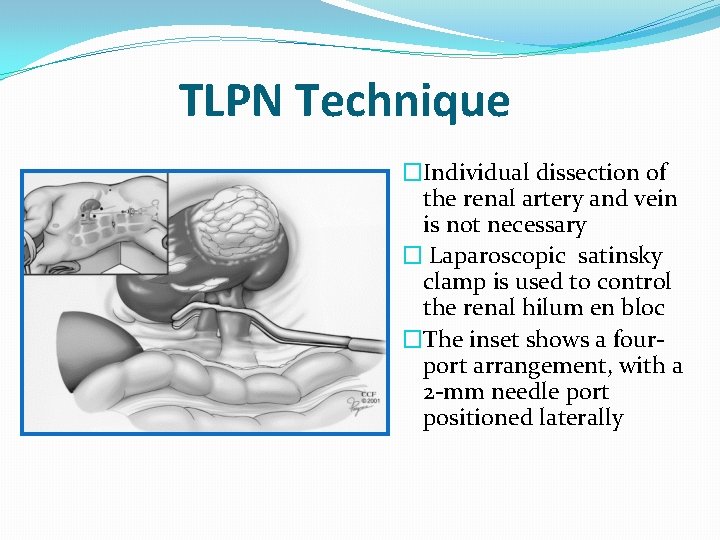
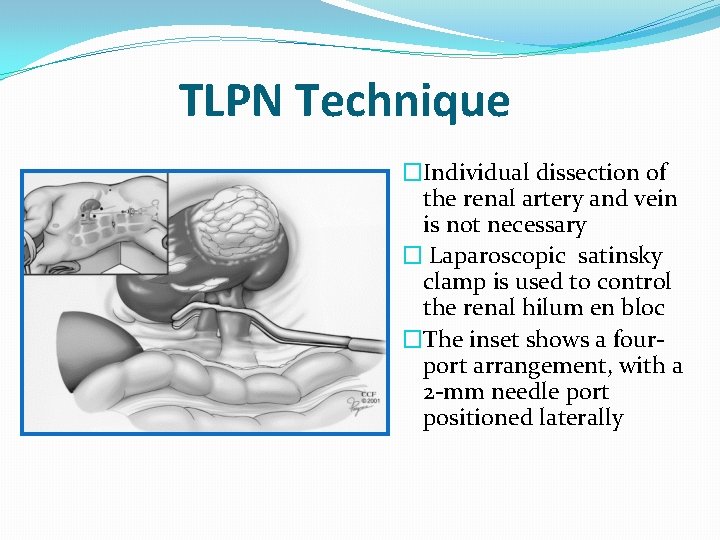
TLPN Technique �Individual dissection of the renal artery and vein is not necessary � Laparoscopic satinsky clamp is used to control the renal hilum en bloc �The inset shows a fourport arrangement, with a 2 -mm needle port positioned laterally
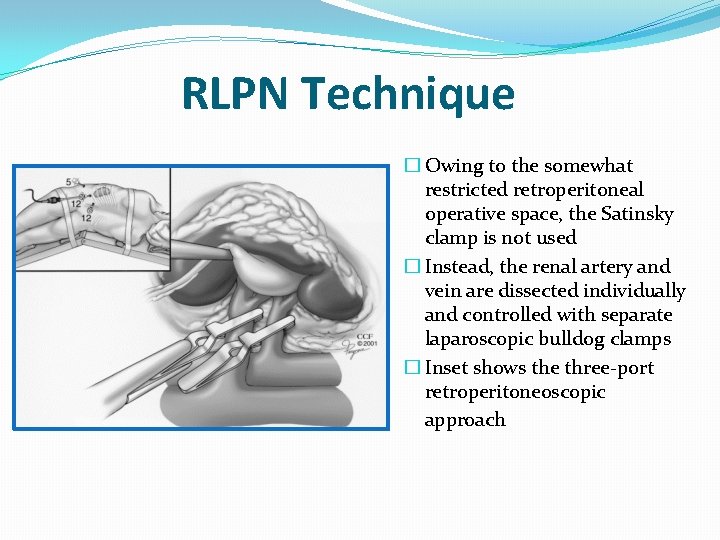
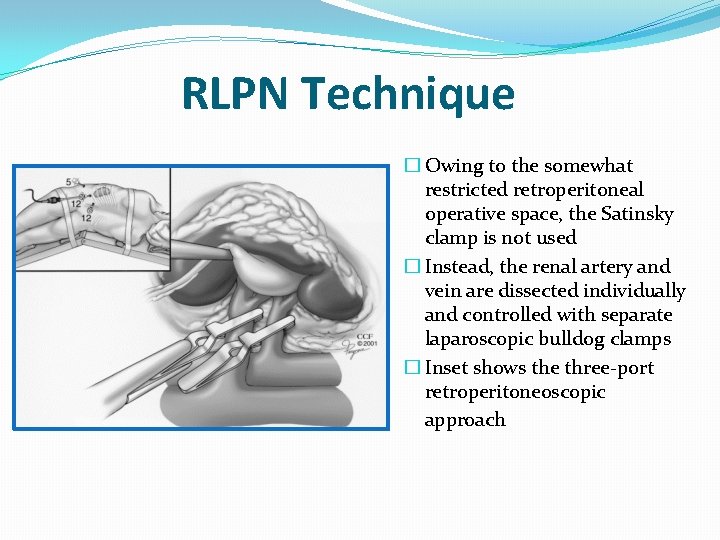
RLPN Technique � Owing to the somewhat restricted retroperitoneal operative space, the Satinsky clamp is not used � Instead, the renal artery and vein are dissected individually and controlled with separate laparoscopic bulldog clamps � Inset shows the three-port retroperitoneoscopic approach
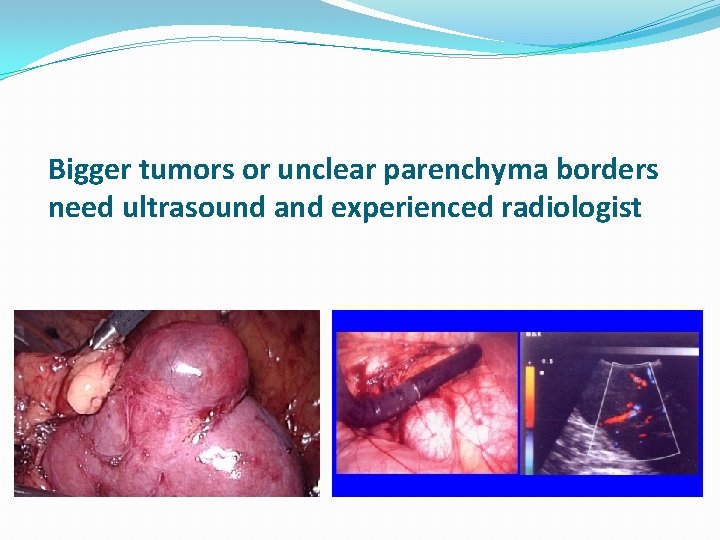
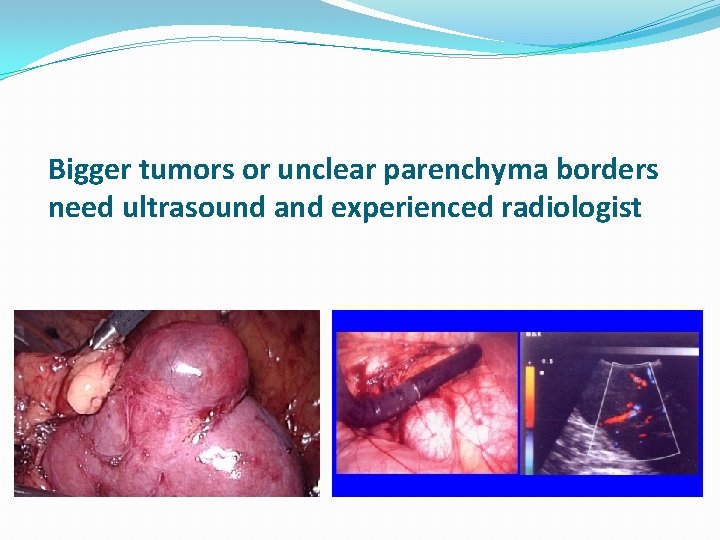
Bigger tumors or unclear parenchyma borders need ultrasound and experienced radiologist
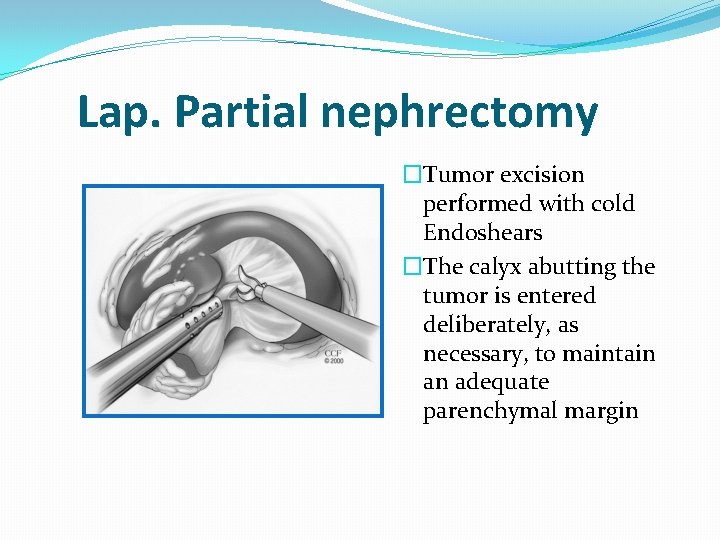
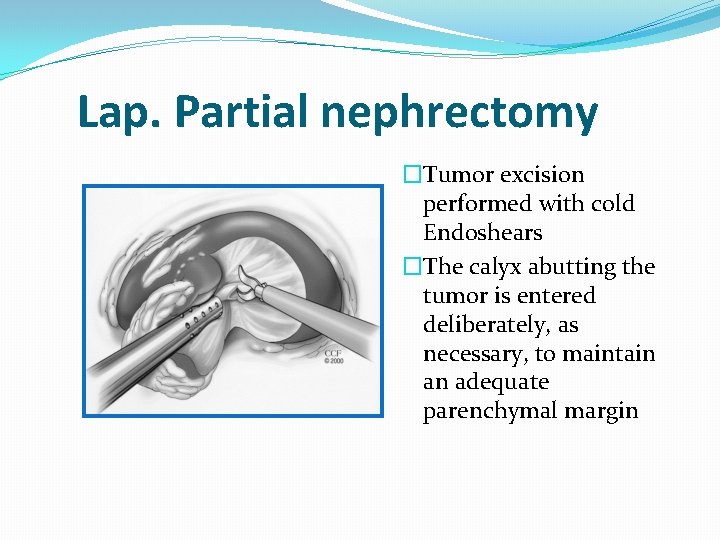
Lap. Partial nephrectomy �Tumor excision performed with cold Endoshears �The calyx abutting the tumor is entered deliberately, as necessary, to maintain an adequate parenchymal margin
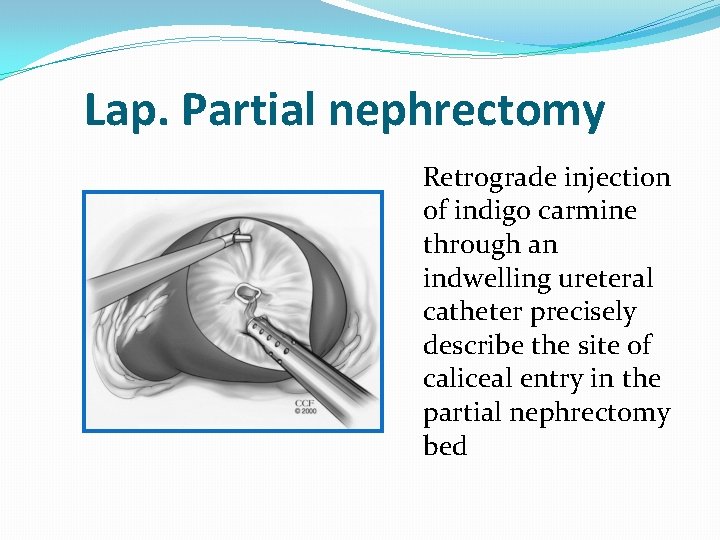
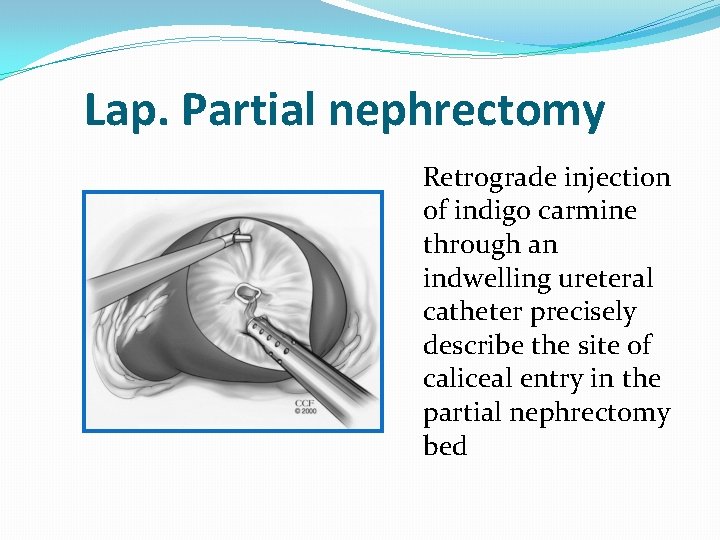
Lap. Partial nephrectomy Retrograde injection of indigo carmine through an indwelling ureteral catheter precisely describe the site of caliceal entry in the partial nephrectomy bed
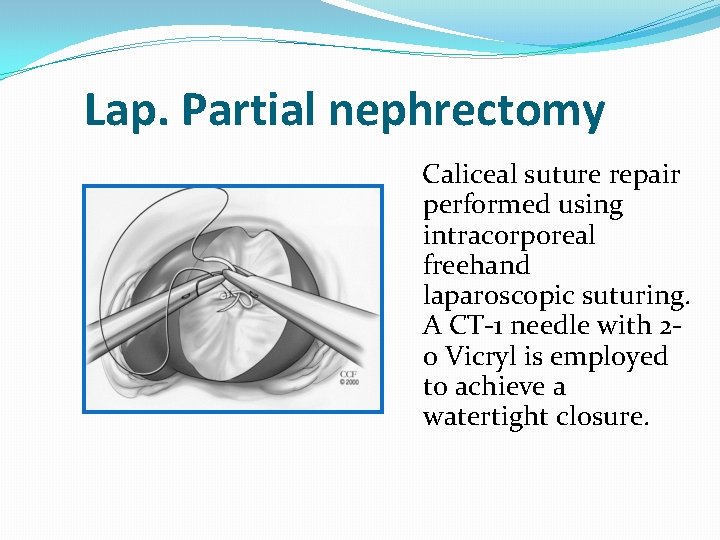
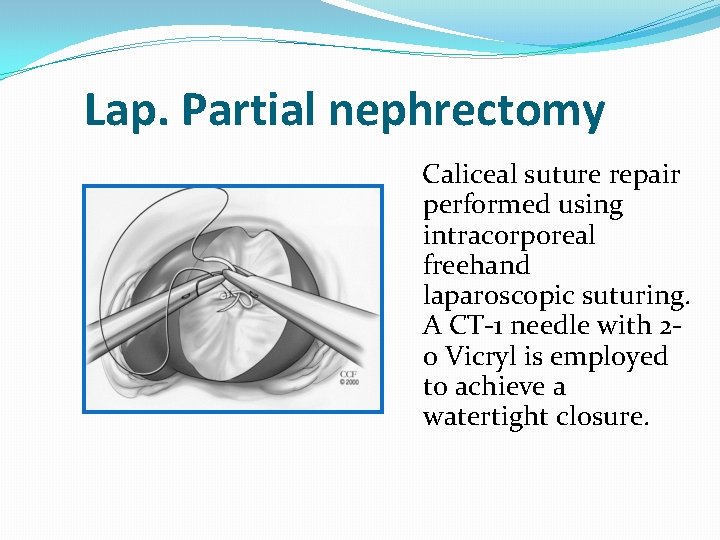
Lap. Partial nephrectomy Caliceal suture repair performed using intracorporeal freehand laparoscopic suturing. A CT-1 needle with 20 Vicryl is employed to achieve a watertight closure.

Lap. Partial nephrectomy �Renal parenchymal reconstruction �A GS-25 needle with 0 Vicryl is employed to place wide parenchymal sutures �Typically, three to four sutures are needed.
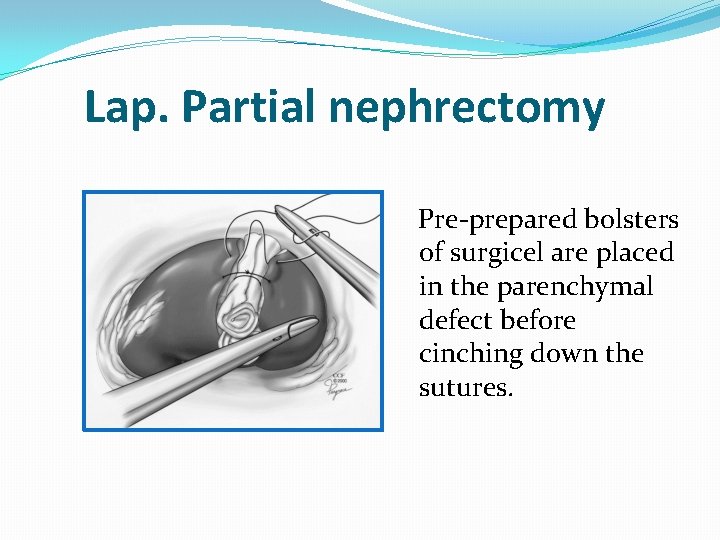
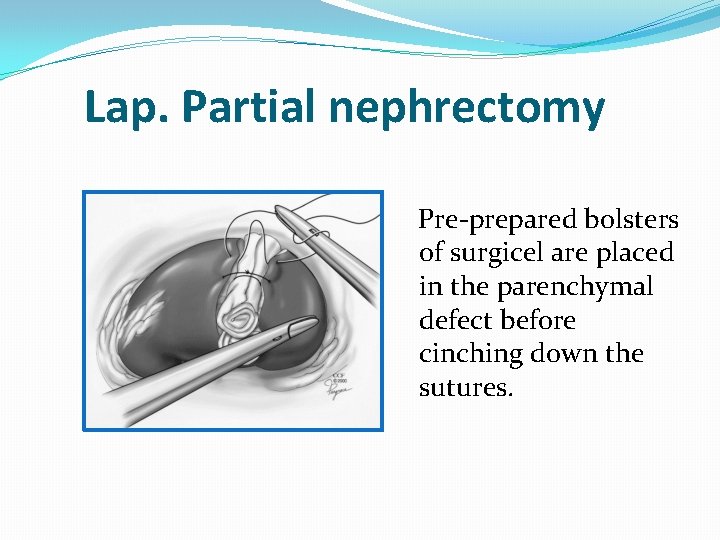
Lap. Partial nephrectomy Pre-prepared bolsters of surgicel are placed in the parenchymal defect before cinching down the sutures.
Warm ischemia time < 30 min • Tumor excision • Suturing collecting system • Suturing parenchyma
Complications of Laparoscopic Partial Nephrectomy • • • Urinoma Total nephrectomy Trocar site infection Pneumothorax Pulmonary edema Tumor fragmentation Transfusion Pneumonia Renal insufficiency
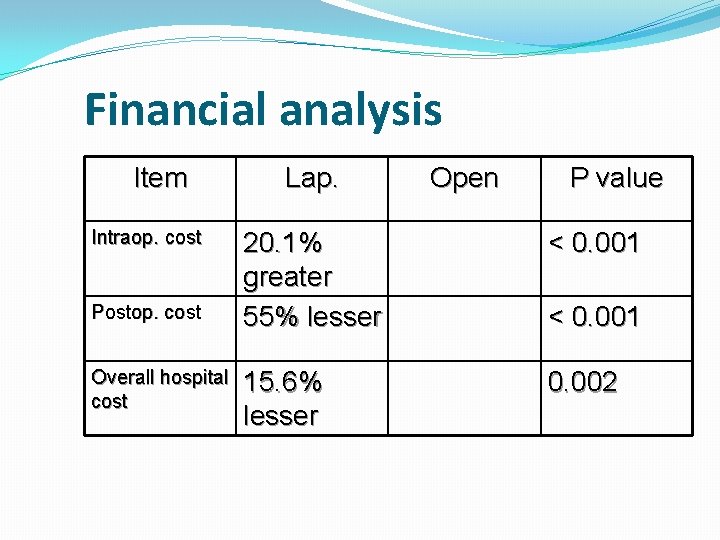
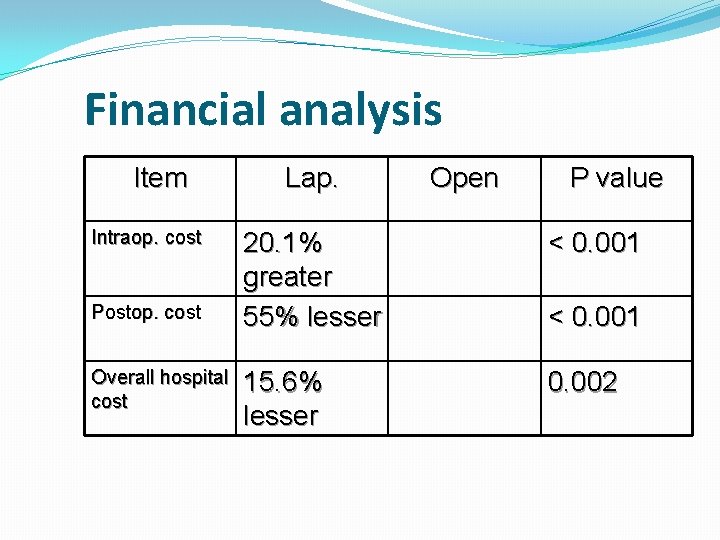
Financial analysis Item Intraop. cost Postop. cost Overall hospital cost Lap. Open P value 20. 1% greater 55% lesser < 0. 001 15. 6% lesser 0. 002 < 0. 001
Conclusions �LPN is an advanced procedure �Carries higher intraop. /postop. complications �As surgeon experience increases, the rate of complications decreases, and the indications for more complex cases increases �Emerging as a viable and efficient treatment option in the minimally invasive armamentarium