LAB DIAGNOSIS OF DIABETES MELLITUS Regarding type 1
LAB DIAGNOSIS OF DIABETES MELLITUS

Regarding type 1 diabetes mellitus, which one statement is correct: a. b. Most commonly develops in old age Type 1 diabetes is an autoimmune disease with pancreatic beta islet cell destruction caused by Tlymphocytes c. Usually not associated with genetic susceptibility d. Type 1 diabetes is an autoimmune disease with pancreatic beta islet cell destruction caused by Blymphocytes
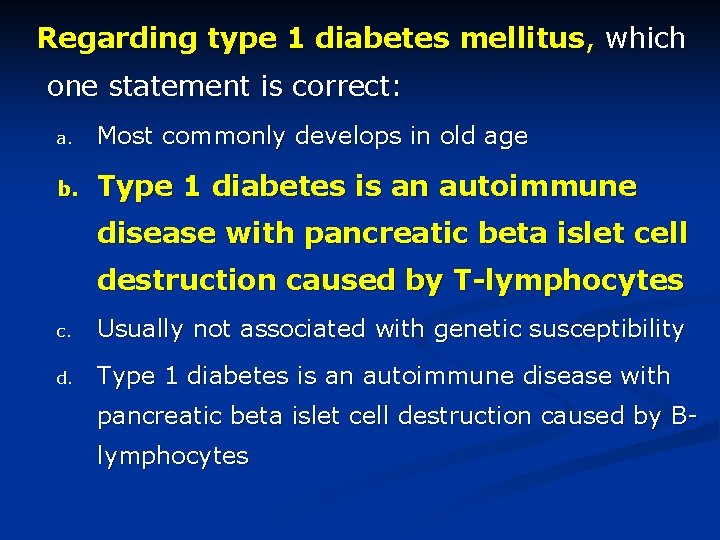
Regarding type 1 diabetes mellitus, which one statement is correct: a. Most commonly develops in old age b. Type 1 diabetes is an autoimmune disease with pancreatic beta islet cell destruction caused by T-lymphocytes c. Usually not associated with genetic susceptibility d. Type 1 diabetes is an autoimmune disease with pancreatic beta islet cell destruction caused by Blymphocytes
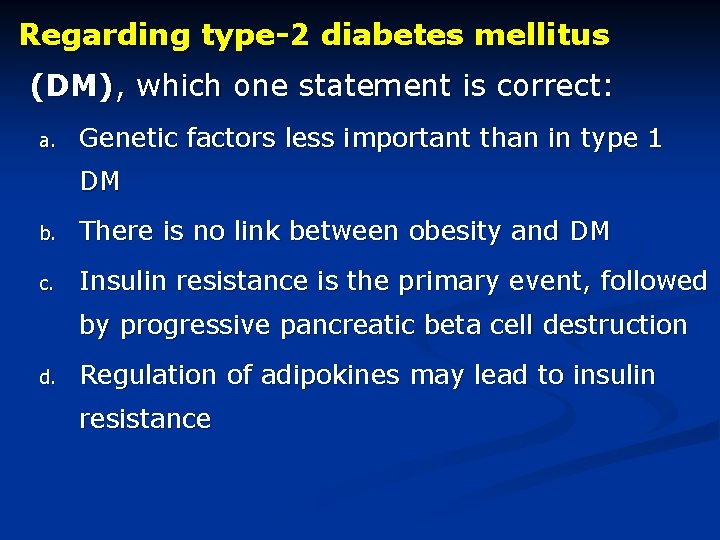
Regarding type-2 diabetes mellitus (DM), which one statement is correct: a. Genetic factors less important than in type 1 DM b. There is no link between obesity and DM c. Insulin resistance is the primary event, followed by progressive pancreatic beta cell destruction d. Regulation of adipokines may lead to insulin resistance
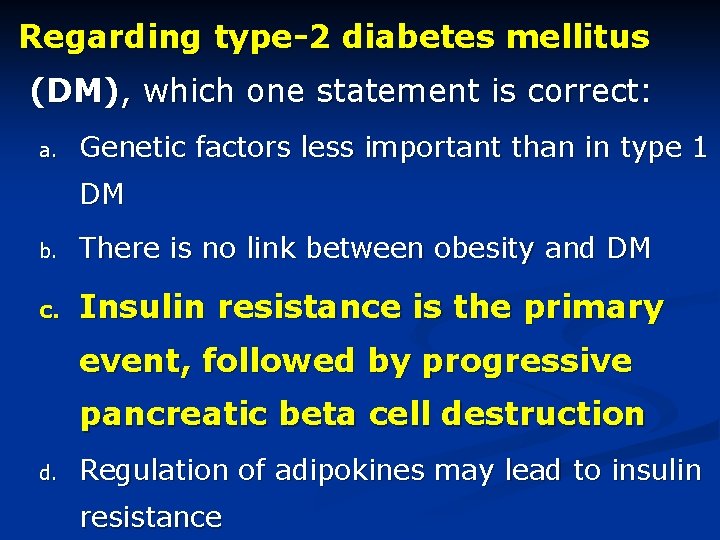
Regarding type-2 diabetes mellitus (DM), which one statement is correct: a. Genetic factors less important than in type 1 DM b. There is no link between obesity and DM c. Insulin resistance is the primary event, followed by progressive pancreatic beta cell destruction d. Regulation of adipokines may lead to insulin resistance
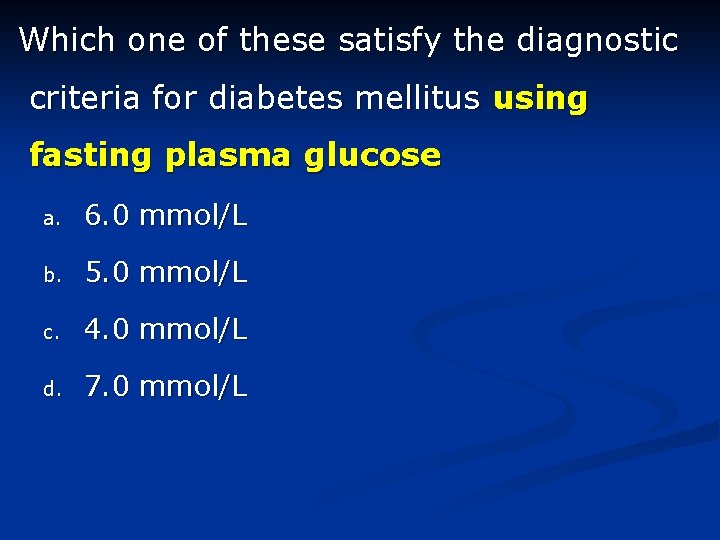
Which one of these satisfy the diagnostic criteria for diabetes mellitus using fasting plasma glucose a. 6. 0 mmol/L b. 5. 0 mmol/L c. 4. 0 mmol/L d. 7. 0 mmol/L
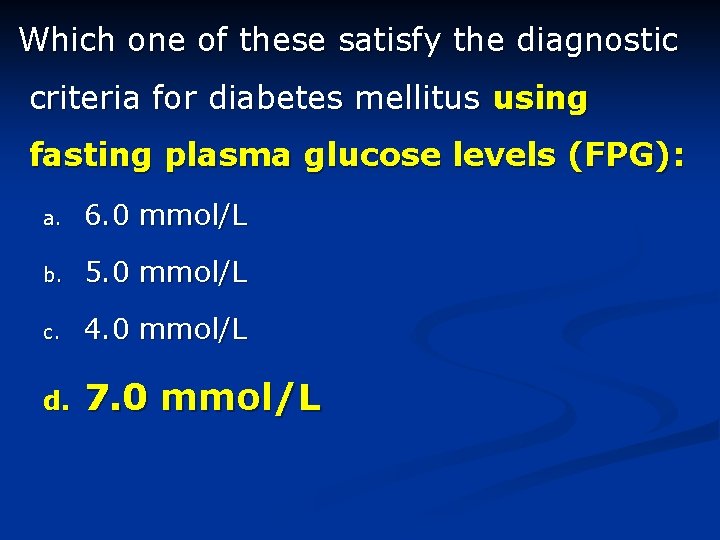
Which one of these satisfy the diagnostic criteria for diabetes mellitus using fasting plasma glucose levels (FPG): a. 6. 0 mmol/L b. 5. 0 mmol/L c. 4. 0 mmol/L d. 7. 0 mmol/L
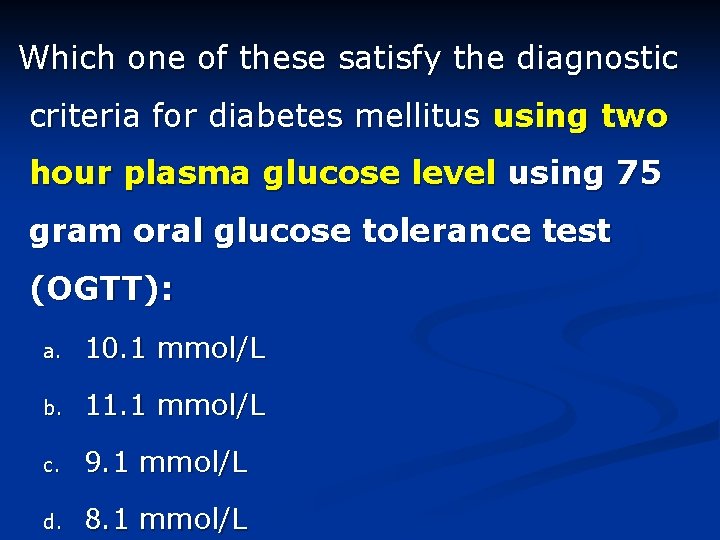
Which one of these satisfy the diagnostic criteria for diabetes mellitus using two hour plasma glucose level using 75 gram oral glucose tolerance test (OGTT): a. 10. 1 mmol/L b. 11. 1 mmol/L c. 9. 1 mmol/L d. 8. 1 mmol/L
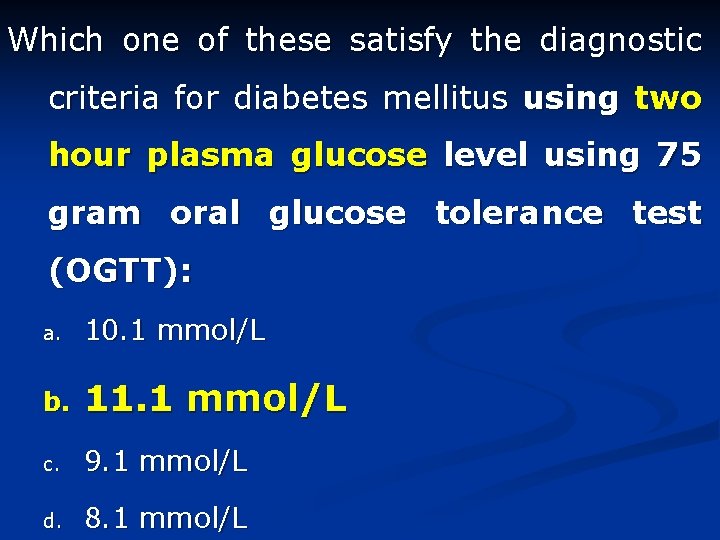
Which one of these satisfy the diagnostic criteria for diabetes mellitus using two hour plasma glucose level using 75 gram oral glucose tolerance test (OGTT): a. 10. 1 mmol/L b. 11. 1 mmol/L c. 9. 1 mmol/L d. 8. 1 mmol/L
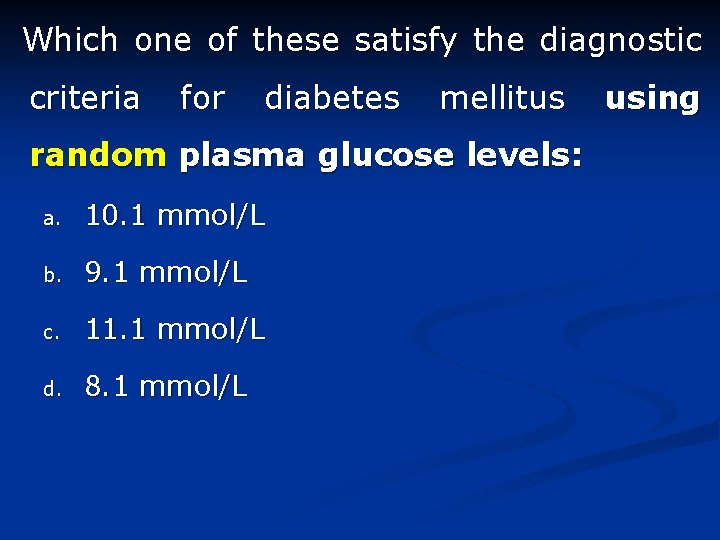
Which one of these satisfy the diagnostic criteria for diabetes mellitus random plasma glucose levels: a. 10. 1 mmol/L b. 9. 1 mmol/L c. 11. 1 mmol/L d. 8. 1 mmol/L using
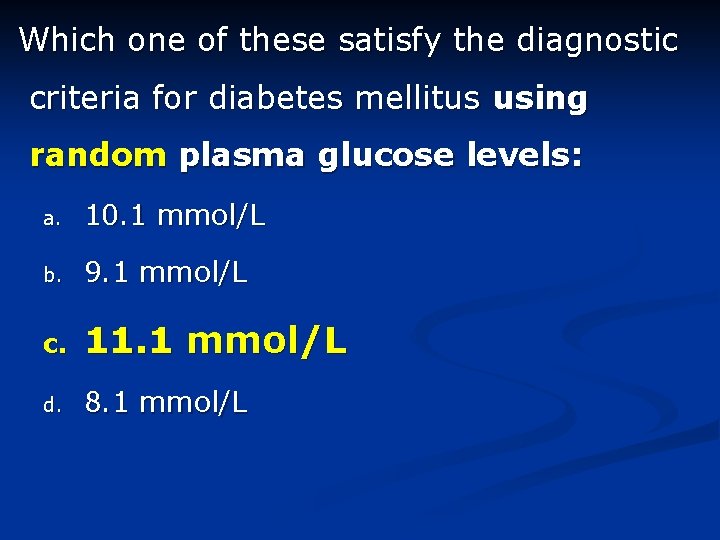
Which one of these satisfy the diagnostic criteria for diabetes mellitus using random plasma glucose levels: a. 10. 1 mmol/L b. 9. 1 mmol/L c. 11. 1 mmol/L d. 8. 1 mmol/L
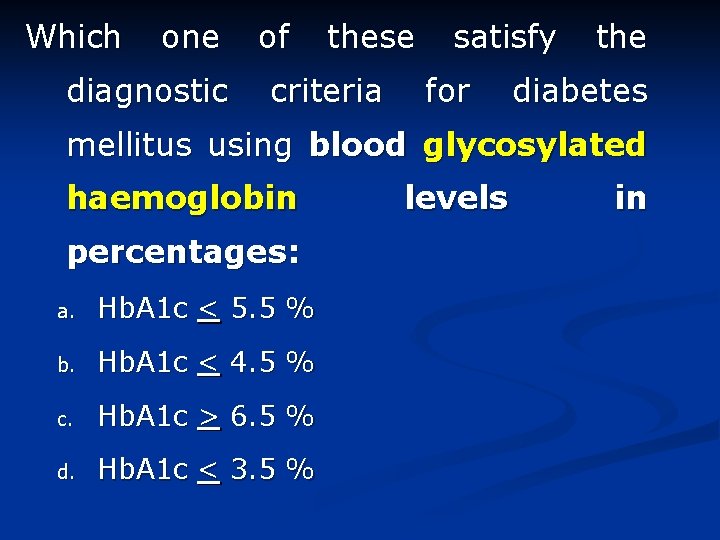
Which one diagnostic of these criteria satisfy for the diabetes mellitus using blood glycosylated haemoglobin percentages: a. Hb. A 1 c < 5. 5 % b. Hb. A 1 c < 4. 5 % c. Hb. A 1 c > 6. 5 % d. Hb. A 1 c < 3. 5 % levels in
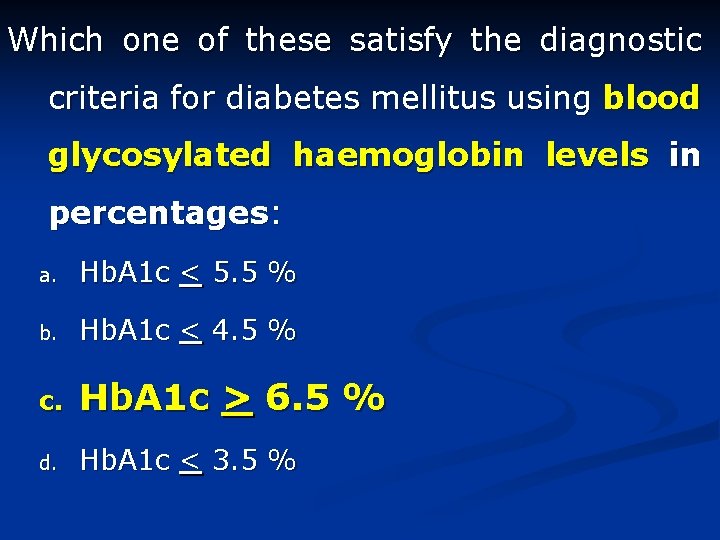
Which one of these satisfy the diagnostic criteria for diabetes mellitus using blood glycosylated haemoglobin levels in percentages: a. Hb. A 1 c < 5. 5 % b. Hb. A 1 c < 4. 5 % c. Hb. A 1 c > 6. 5 % d. Hb. A 1 c < 3. 5 %
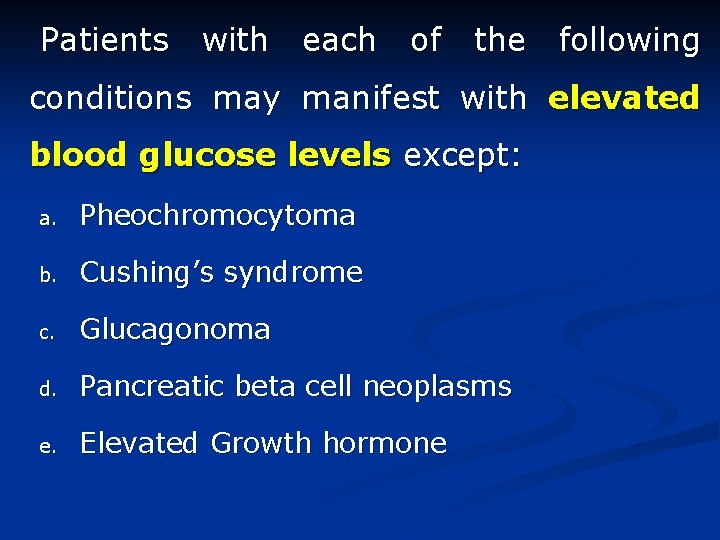
Patients with each of the following conditions may manifest with elevated blood glucose levels except: a. Pheochromocytoma b. Cushing’s syndrome c. Glucagonoma d. Pancreatic beta cell neoplasms e. Elevated Growth hormone
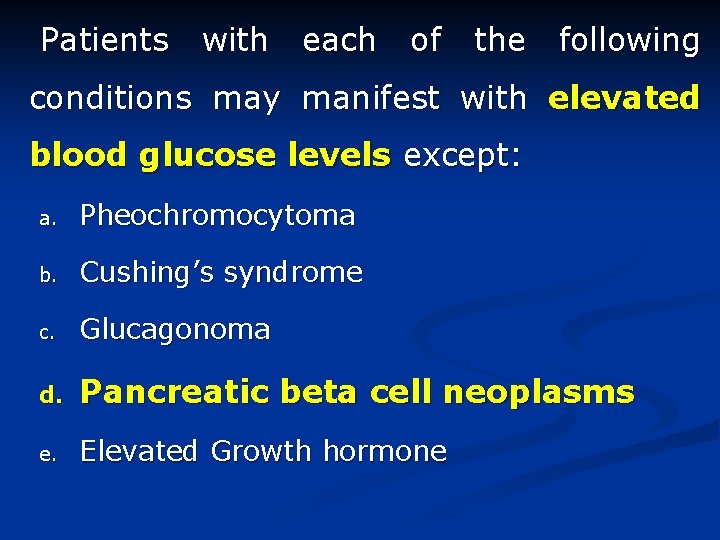
Patients with each of the following conditions may manifest with elevated blood glucose levels except: a. Pheochromocytoma b. Cushing’s syndrome c. Glucagonoma d. Pancreatic beta cell neoplasms e. Elevated Growth hormone
Complication of diabetes mellitus (D. M) Brig Rizwan Hashim Pathology dept Army Medical College

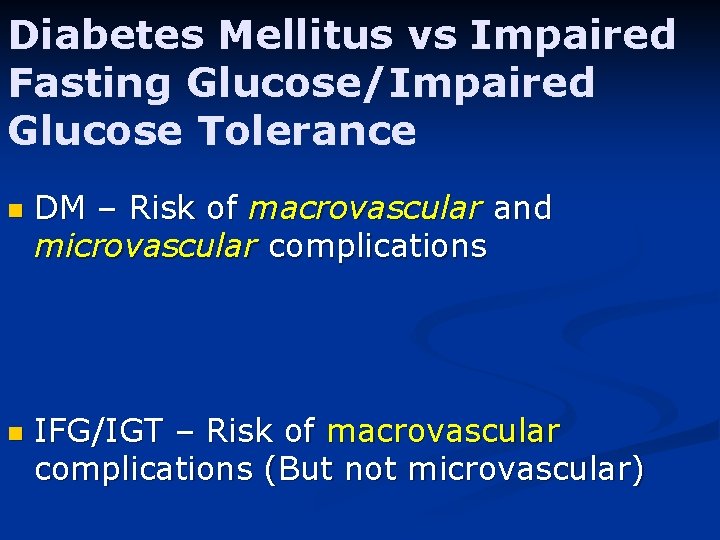
Diabetes Mellitus vs Impaired Fasting Glucose/Impaired Glucose Tolerance n n DM – Risk of macrovascular and microvascular complications IFG/IGT – Risk of macrovascular complications (But not microvascular)
D. M Complications n Short term Complications: (metabolic) n Hypoglycemia n Diabetic Ketoacidosis n Non Ketotic hyperosmolar diabetic coma n Lactic acidosis
Patho-physiology of DKA n Relative or absolute insulin deficiency in the presence of catabolic counterregulatory stress hormones (particularly glucagon and catecholamines, but also growth hormone and cortisol) leads to hepatic overproduction of glucose and ketones.
Patho-physiology of DKA n Lack of insulin combined with excess stress hormones promotes lipolysis, with the release of non-esterified fatty acids (NEFAs) from adipose tissue into the circulation.
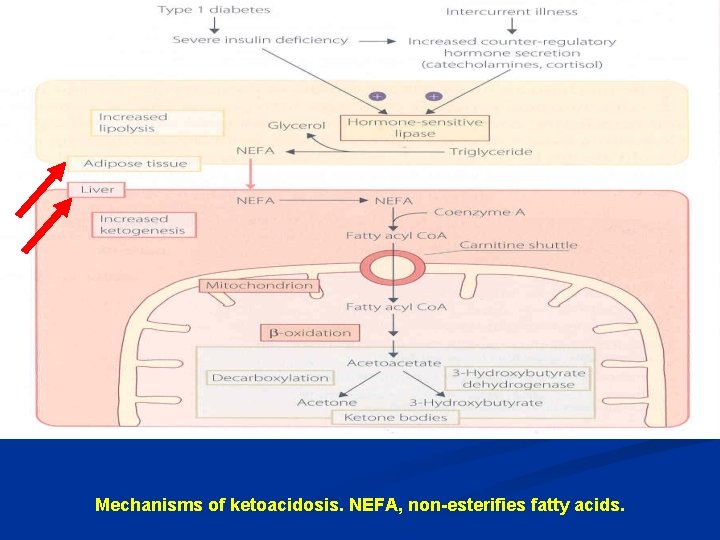
Mechanisms of ketoacidosis. NEFA, non-esterifies fatty acids.
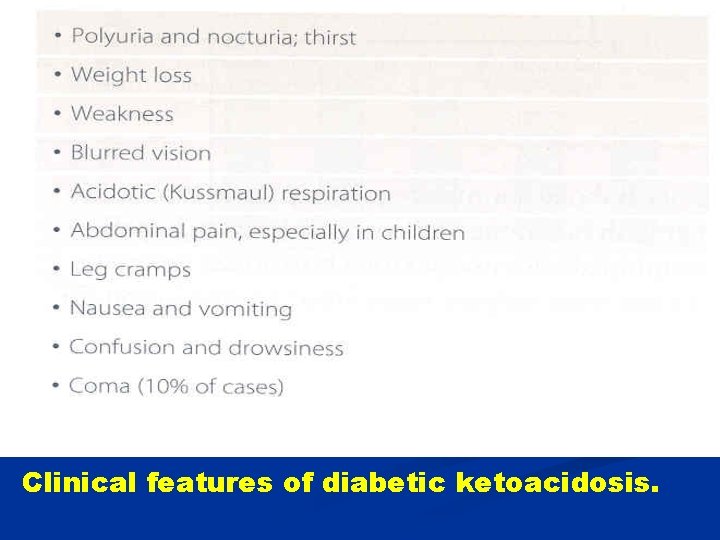
Clinical features of diabetic ketoacidosis.
Complications Long term complications: (microangiopathy) n Angiopathy, n Retinopathy, n Nephropathy, n Neuropathy
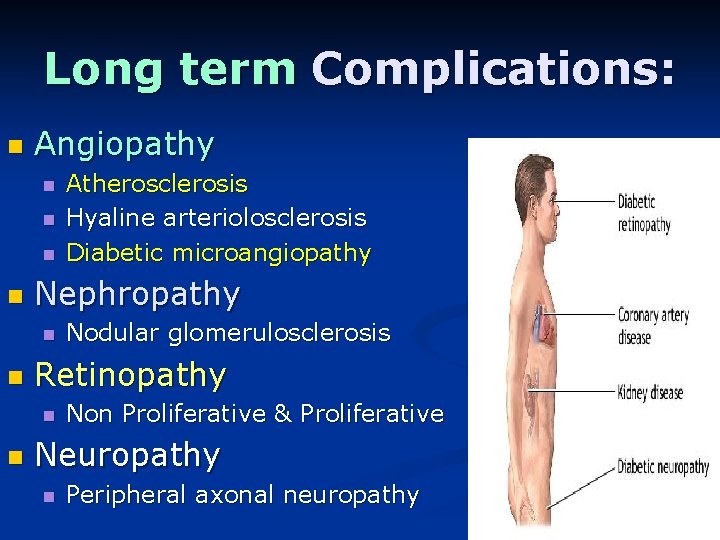
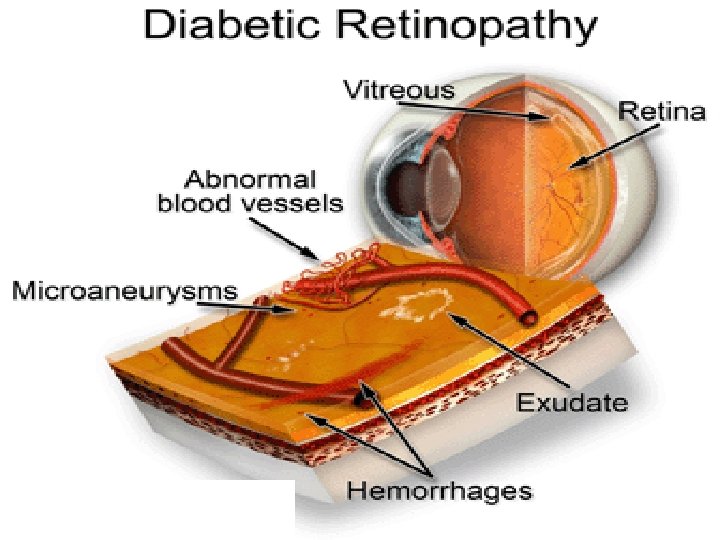
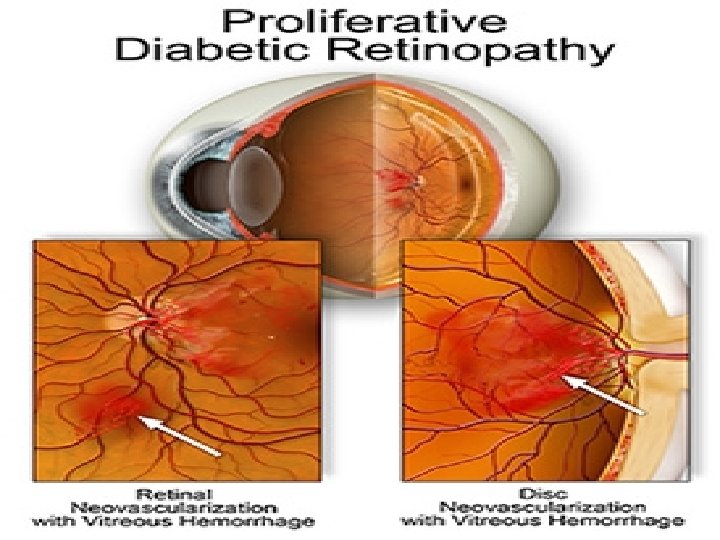
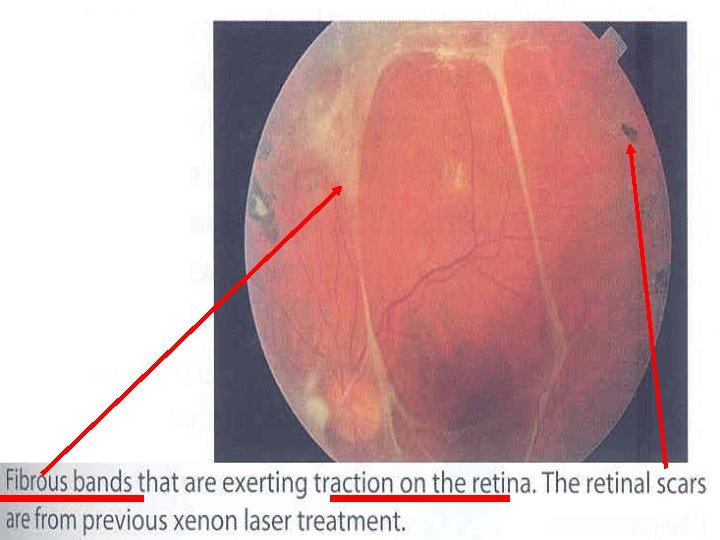
Long term Complications: n Angiopathy n n Nephropathy n n Nodular glomerulosclerosis Retinopathy n n Atherosclerosis Hyaline arteriolosclerosis Diabetic microangiopathy Non Proliferative & Proliferative Neuropathy n Peripheral axonal neuropathy
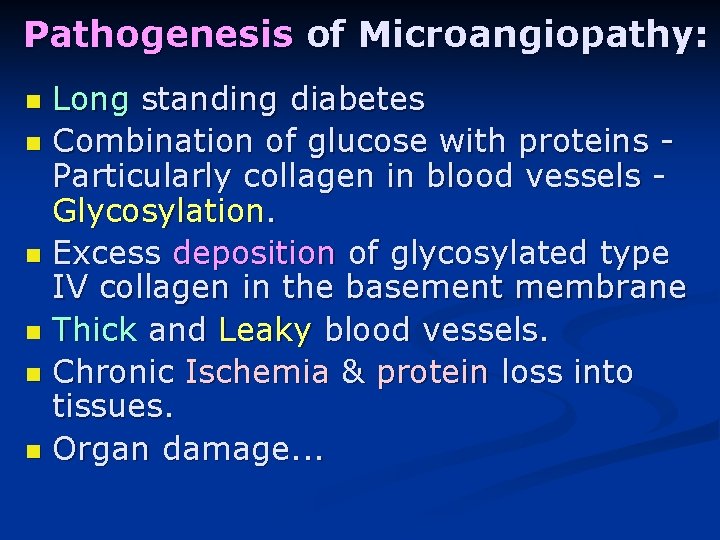
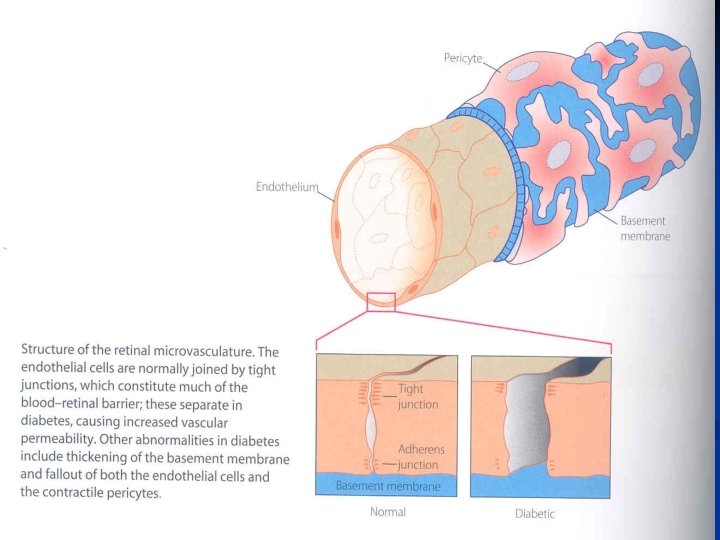
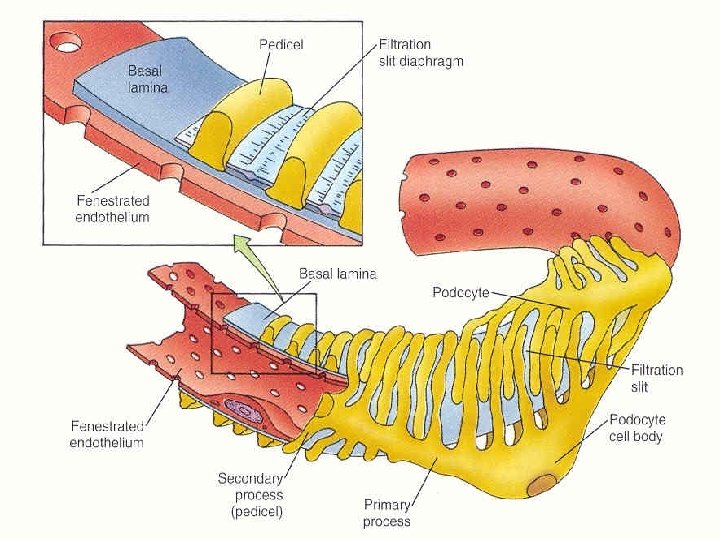
Pathogenesis of Microangiopathy: Long standing diabetes n Combination of glucose with proteins Particularly collagen in blood vessels Glycosylation. n Excess deposition of glycosylated type IV collagen in the basement membrane n Thick and Leaky blood vessels. n Chronic Ischemia & protein loss into tissues. n Organ damage. . . n
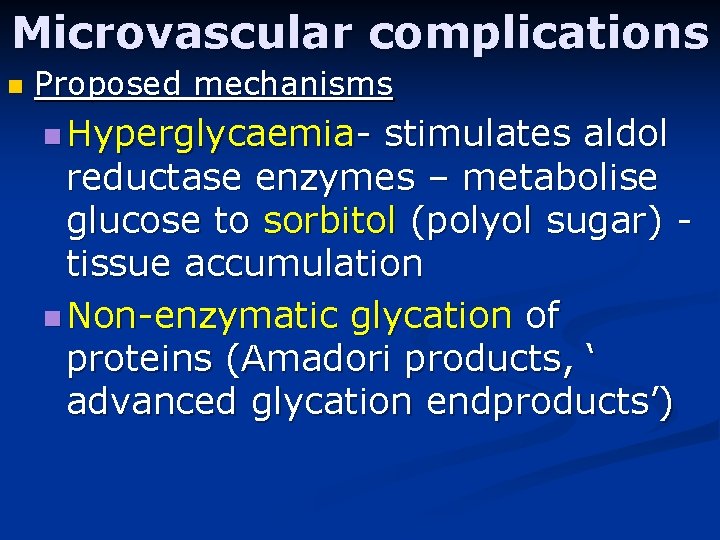
Microvascular complications n Proposed mechanisms n Hyperglycaemia- stimulates aldol reductase enzymes – metabolise glucose to sorbitol (polyol sugar) tissue accumulation n Non-enzymatic glycation of proteins (Amadori products, ‘ advanced glycation endproducts’)
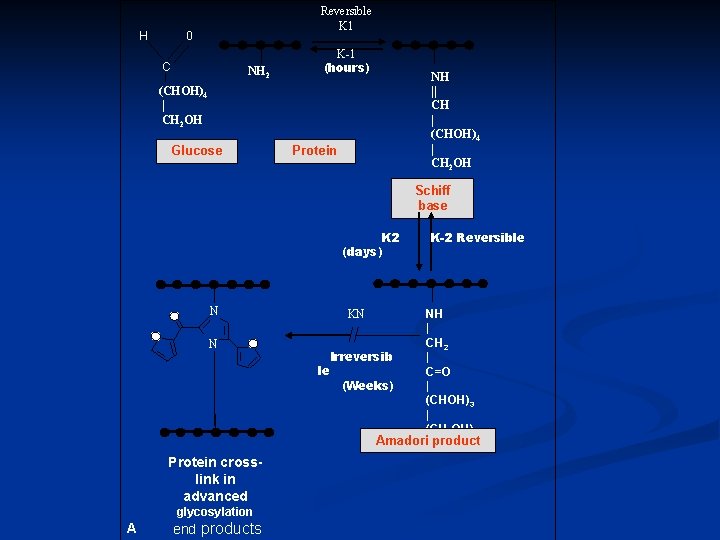
H Reversible K 1 0 C NH 2 K-1 (hours) NH || CH | (CHOH)4 | CH 2 OH Glucose Protein Schiff base K 2 (days) N KN N le Irreversib (Weeks) K-2 Reversible NH | CH 2 | C=O | (CHOH)3 | (CH 2 OH) Amadori product Protein crosslink in advanced glycosylation A end products
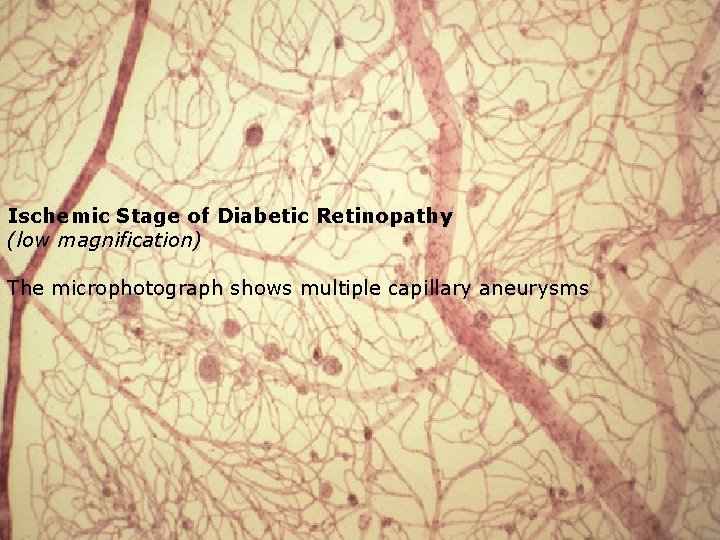
Ischemic Stage of Diabetic Retinopathy (low magnification) The microphotograph shows multiple capillary aneurysms
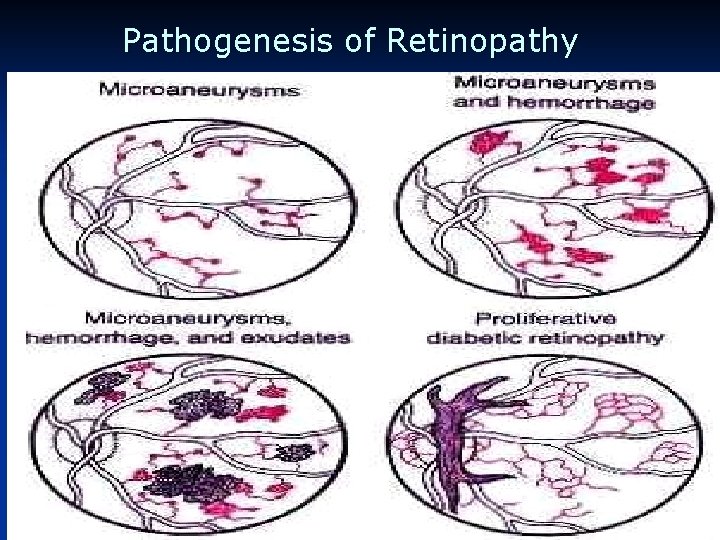
Pathogenesis of Retinopathy
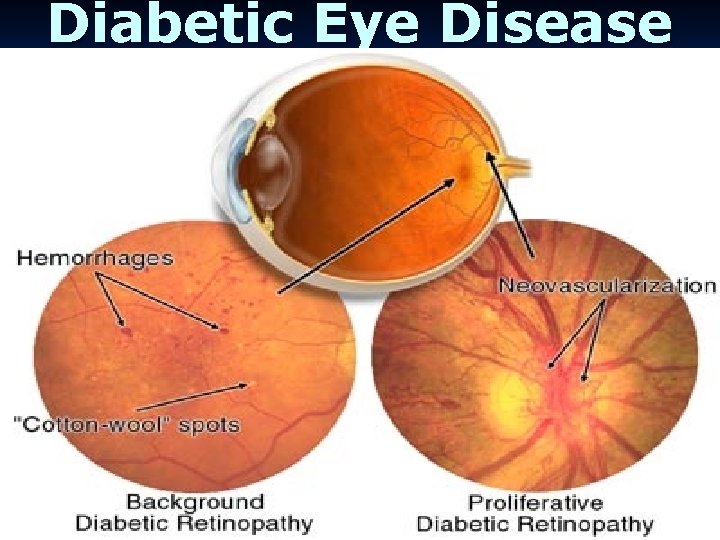
Diabetic Eye Disease
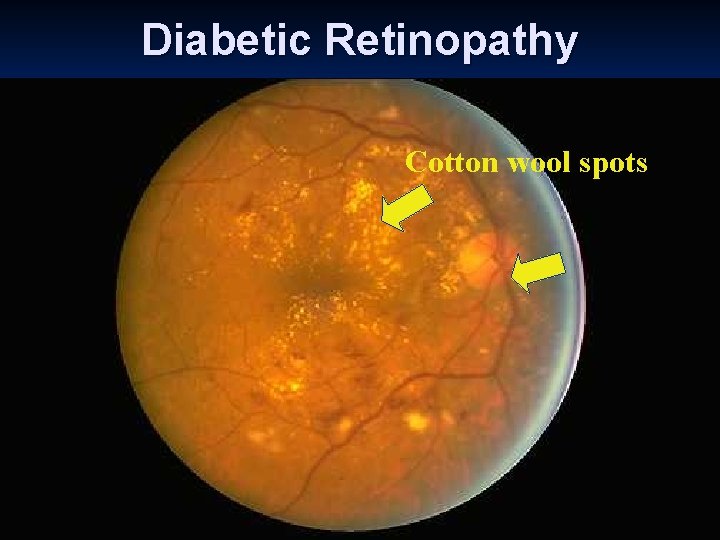
Diabetic Retinopathy Cotton wool spots
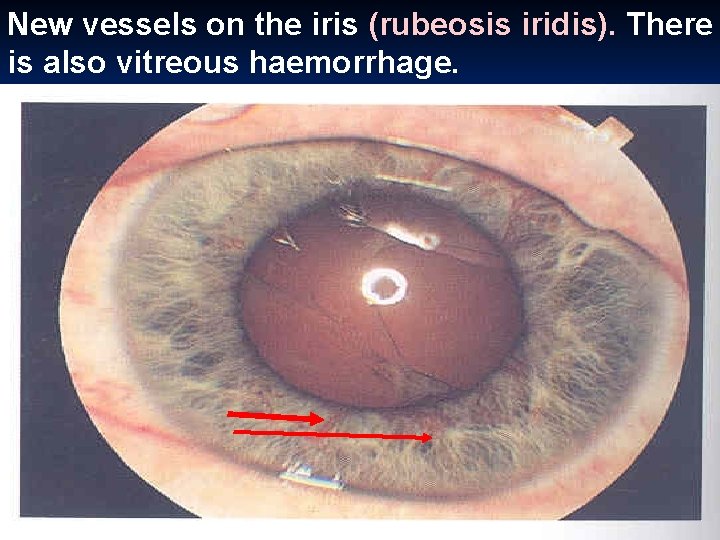
New vessels on the iris (rubeosis iridis). There is also vitreous haemorrhage.
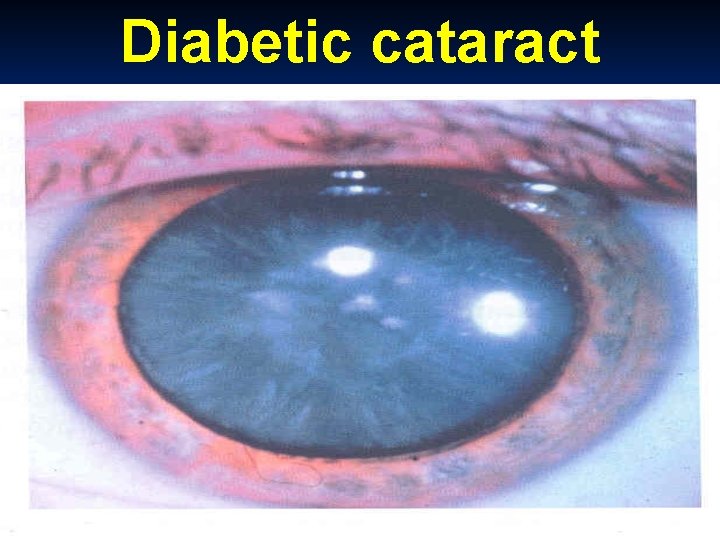
Diabetic cataract
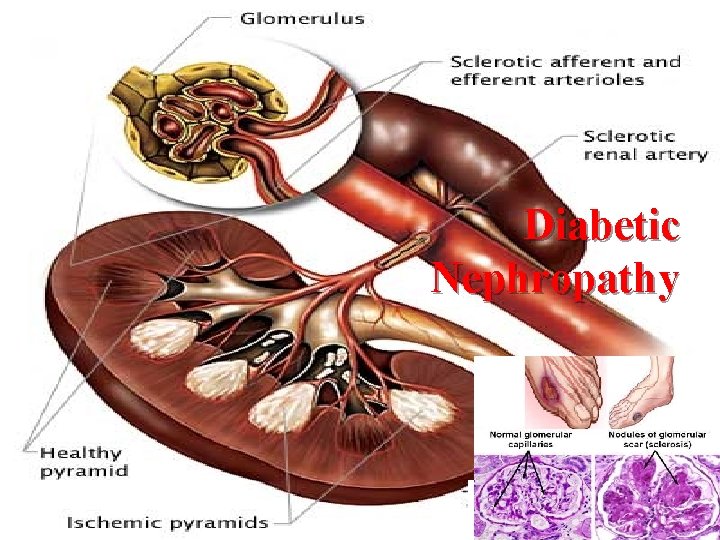
Diabetic Nephropathy
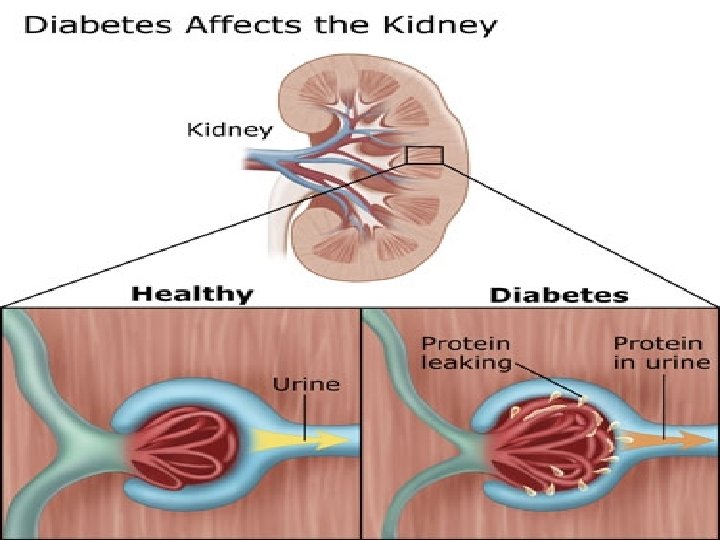
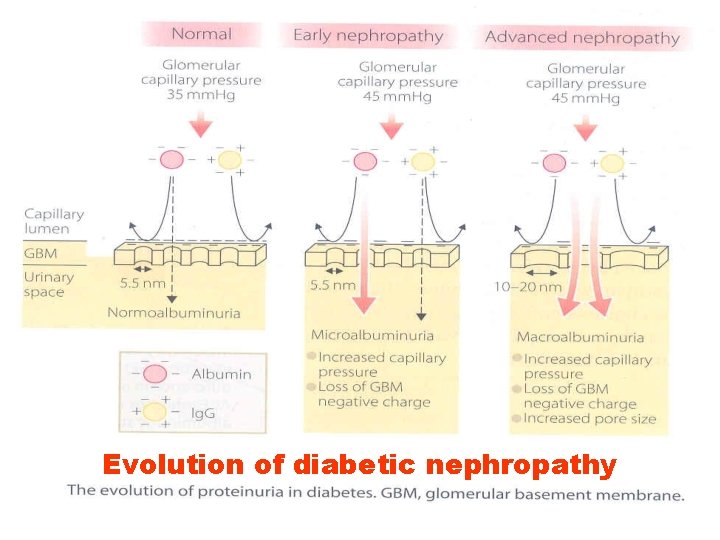
Evolution of diabetic nephropathy
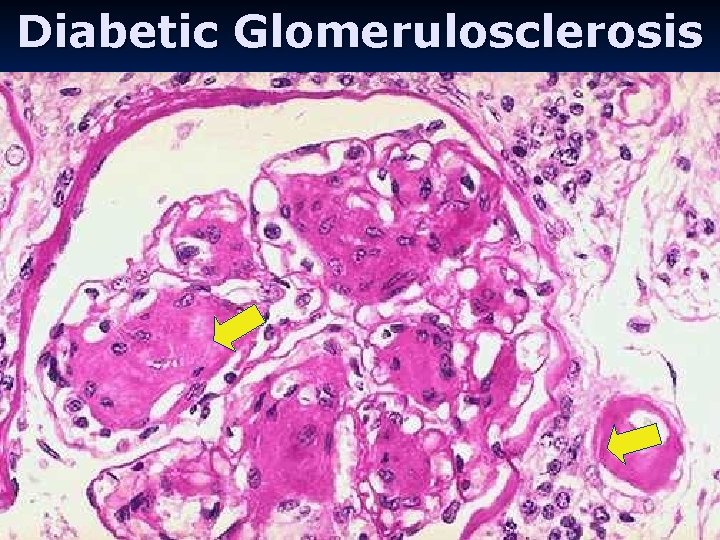
Diabetic Glomerulosclerosis
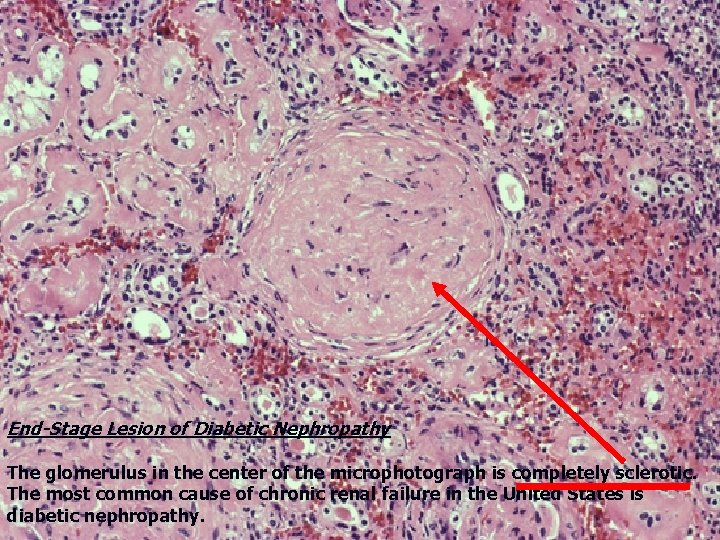
End-Stage Lesion of Diabetic Nephropathy The glomerulus in the center of the microphotograph is completely sclerotic. The most common cause of chronic renal failure in the United States is diabetic nephropathy.
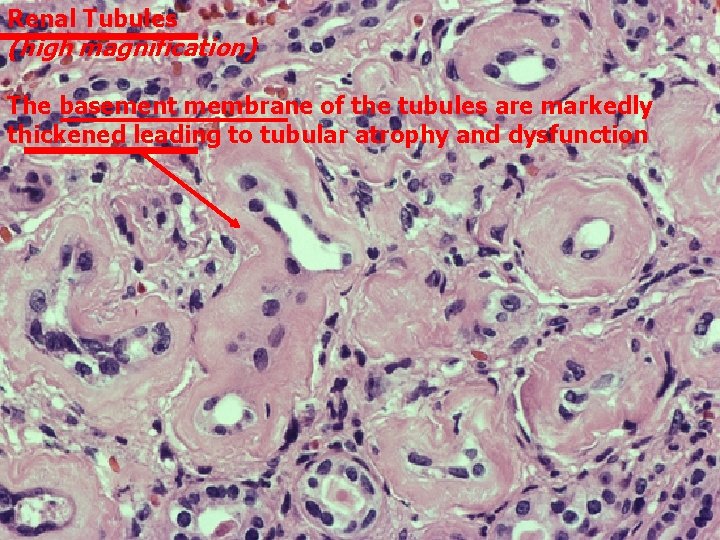
Renal Tubules (high magnification) The basement membrane of the tubules are markedly thickened leading to tubular atrophy and dysfunction
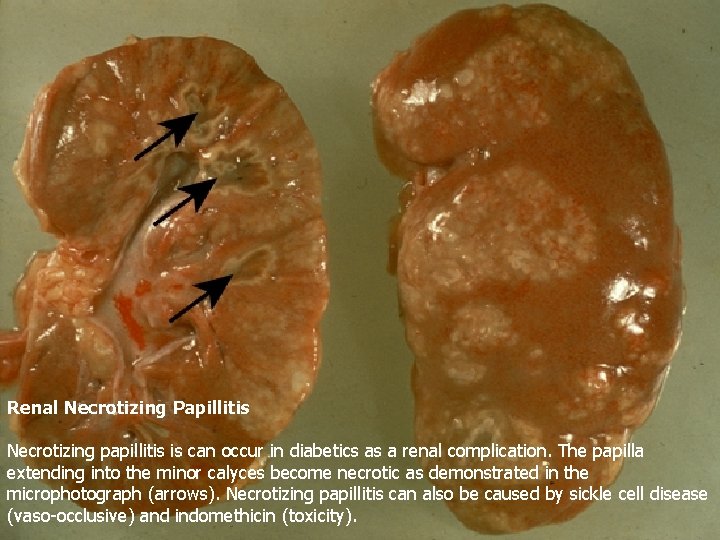
Renal Necrotizing Papillitis Necrotizing papillitis is can occur in diabetics as a renal complication. The papilla extending into the minor calyces become necrotic as demonstrated in the microphotograph (arrows). Necrotizing papillitis can also be caused by sickle cell disease (vaso-occlusive) and indomethicin (toxicity).
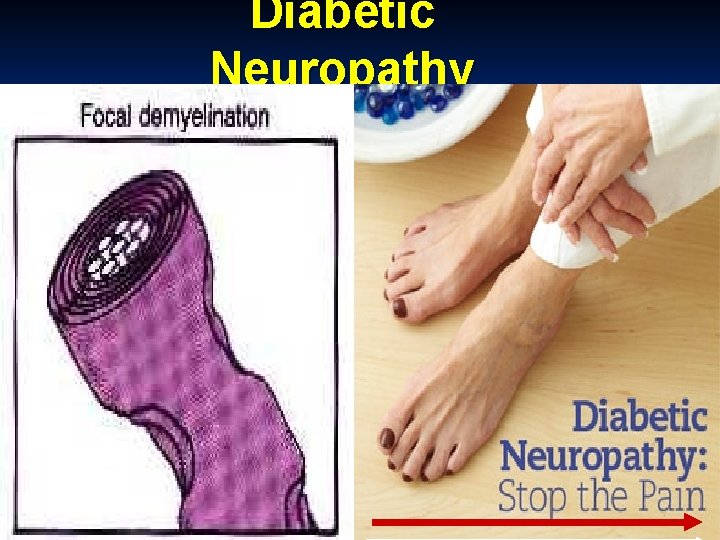
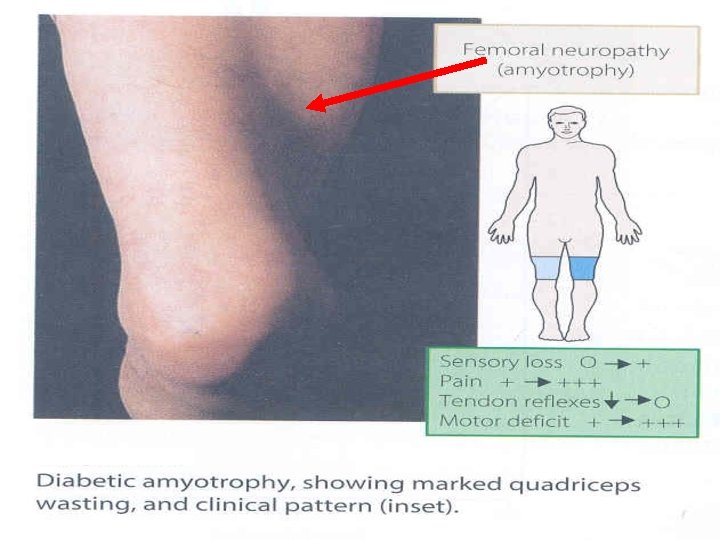
Diabetic Neuropathy

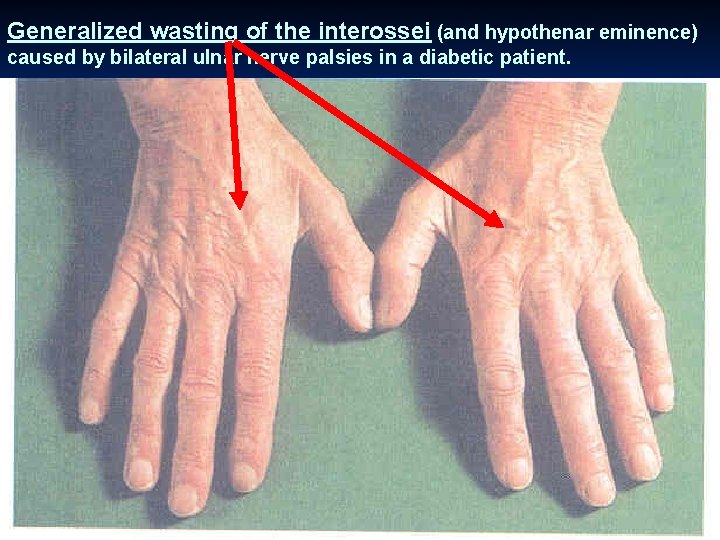
Generalized wasting of the interossei (and hypothenar eminence) caused by bilateral ulnar nerve palsies in a diabetic patient.
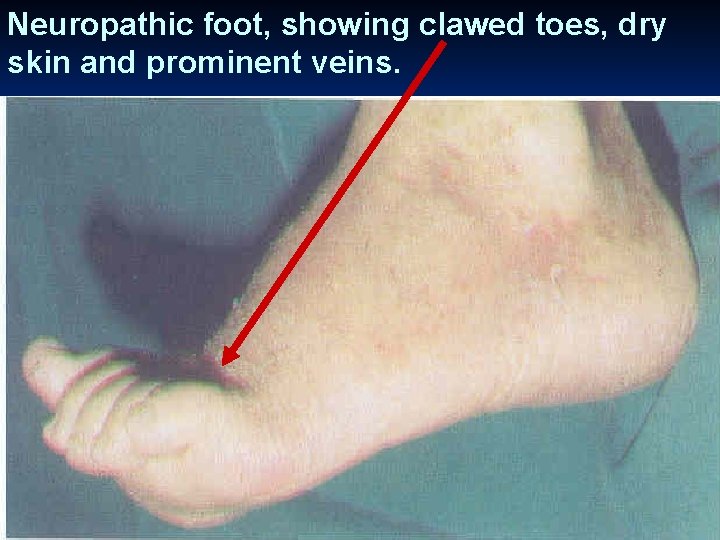
Neuropathic foot, showing clawed toes, dry skin and prominent veins.
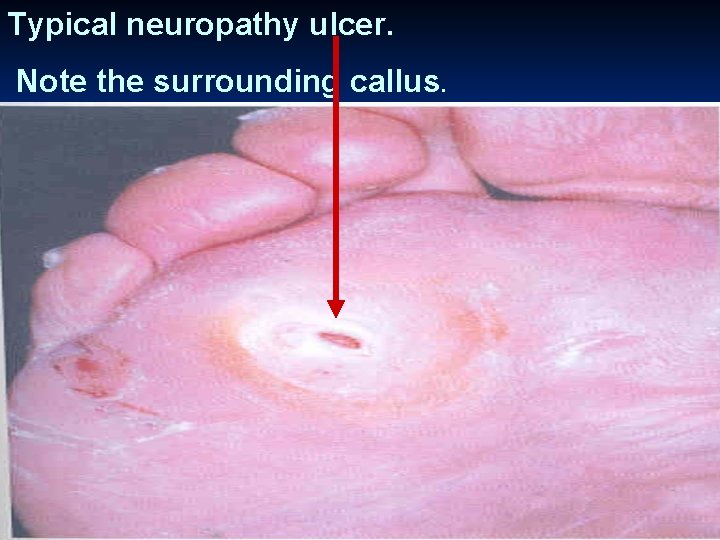
Typical neuropathy ulcer. Note the surrounding callus.
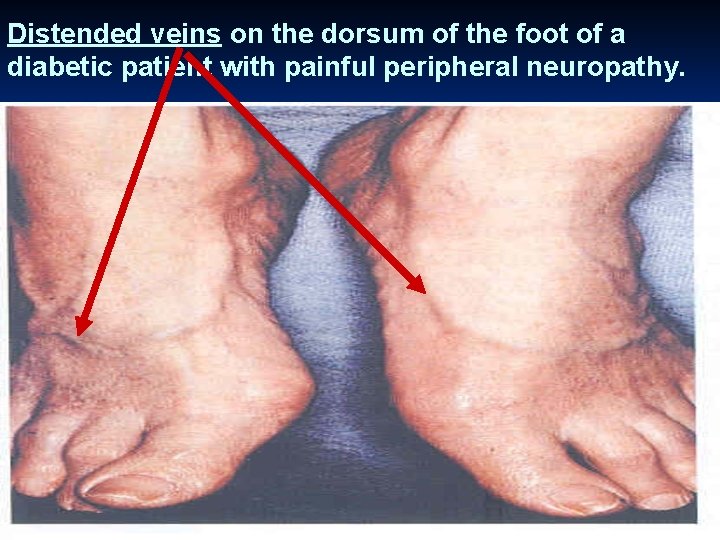
Distended veins on the dorsum of the foot of a diabetic patient with painful peripheral neuropathy.
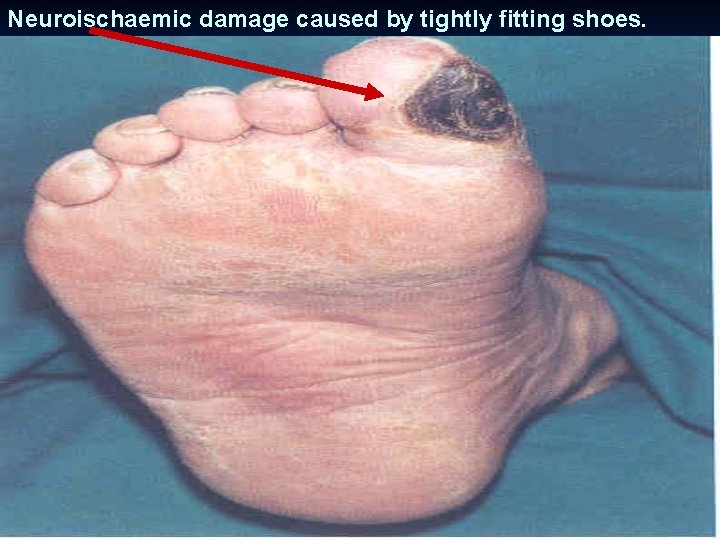
Neuroischaemic damage caused by tightly fitting shoes.
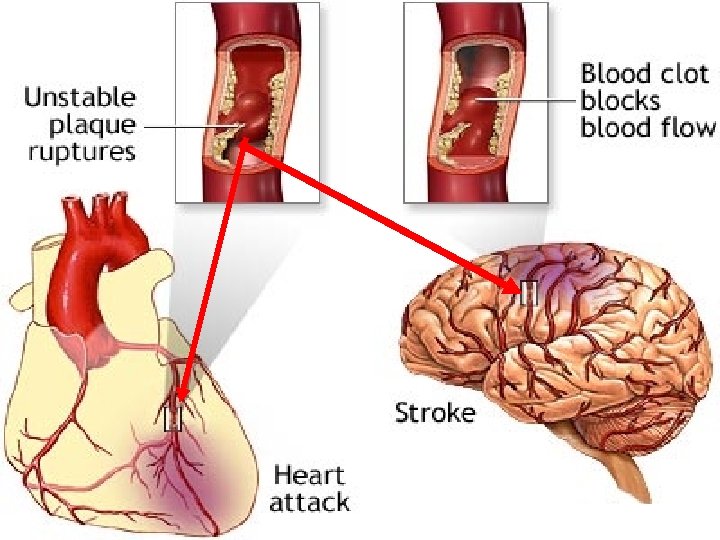
Macrovascular Diseases in Diabetes
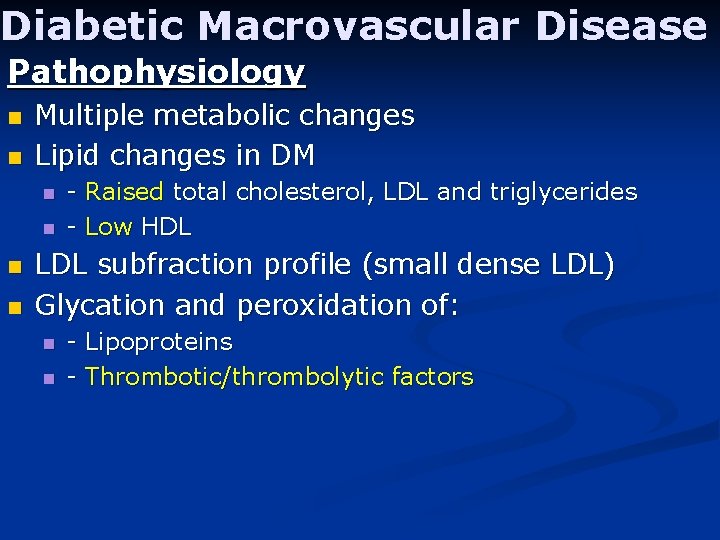
Diabetic Macrovascular Disease Pathophysiology n n Multiple metabolic changes Lipid changes in DM n n - Raised total cholesterol, LDL and triglycerides - Low HDL LDL subfraction profile (small dense LDL) Glycation and peroxidation of: n n - Lipoproteins - Thrombotic/thrombolytic factors
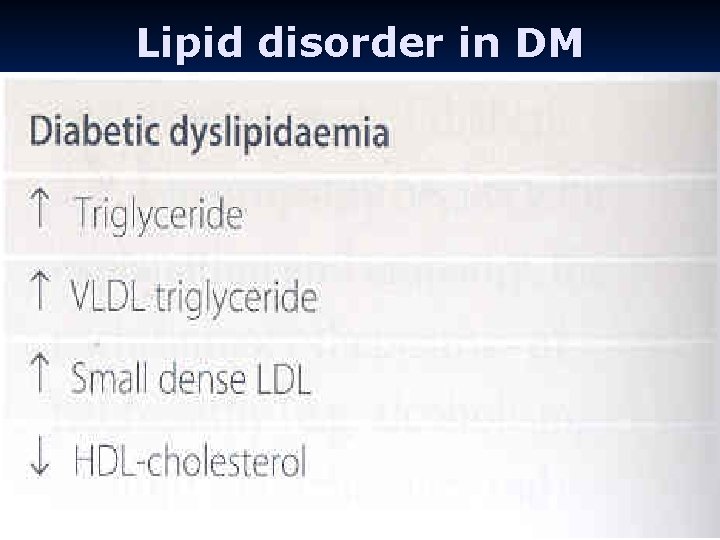
Lipid disorder in DM
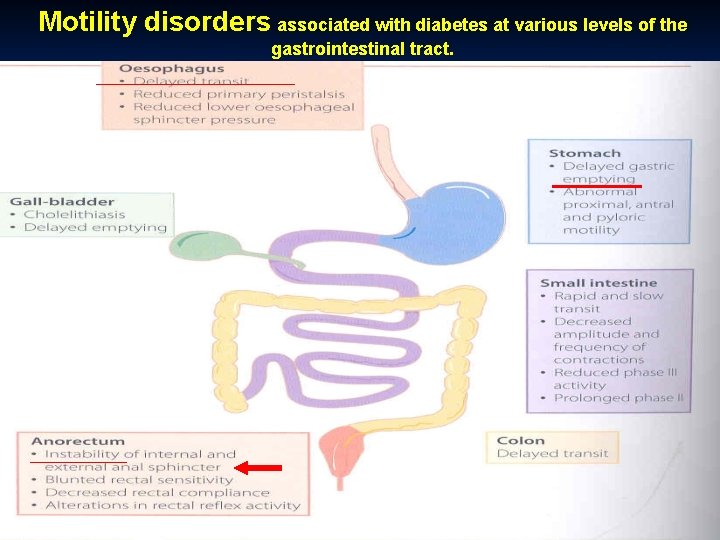
Motility disorders associated with diabetes at various levels of the gastrointestinal tract.
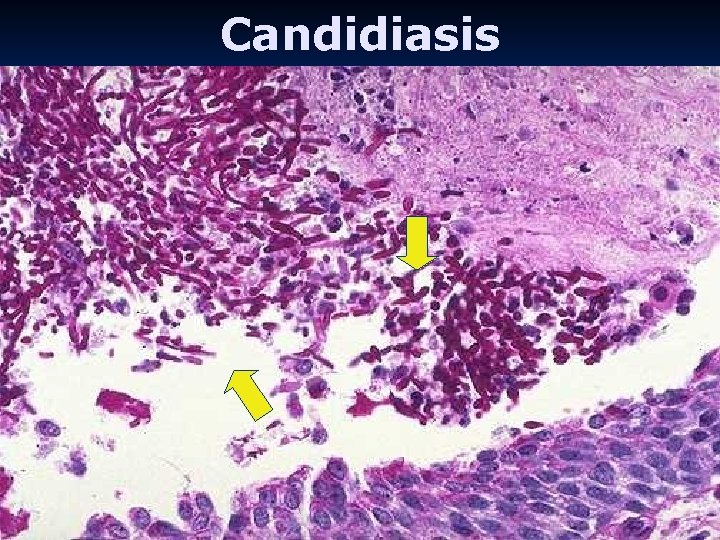
Candidiasis
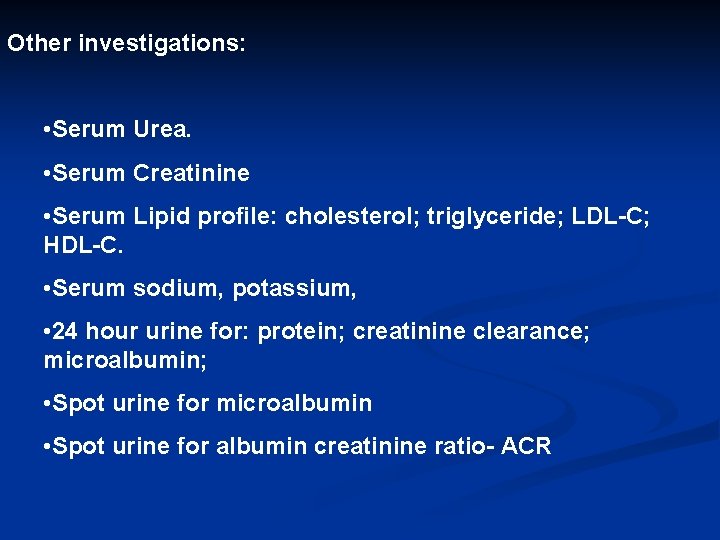
Other investigations: • Serum Urea. • Serum Creatinine • Serum Lipid profile: cholesterol; triglyceride; LDL-C; HDL-C. • Serum sodium, potassium, • 24 hour urine for: protein; creatinine clearance; microalbumin; • Spot urine for microalbumin • Spot urine for albumin creatinine ratio- ACR
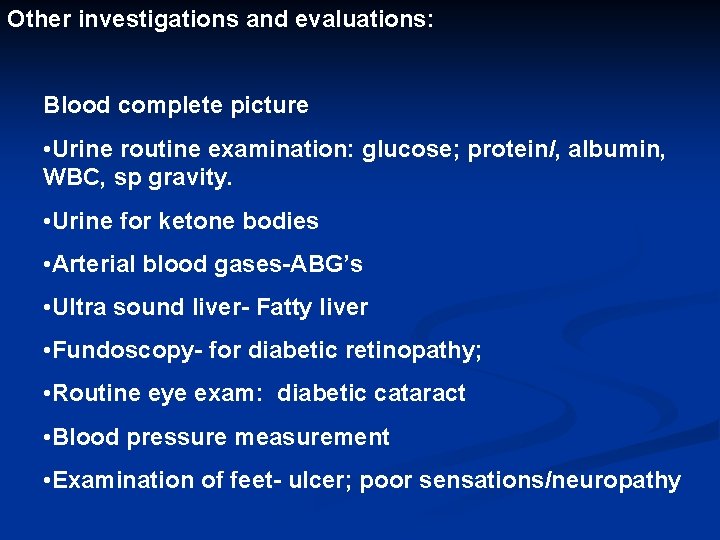
Other investigations and evaluations: Blood complete picture • Urine routine examination: glucose; protein/, albumin, WBC, sp gravity. • Urine for ketone bodies • Arterial blood gases-ABG’s • Ultra sound liver- Fatty liver • Fundoscopy- for diabetic retinopathy; • Routine eye exam: diabetic cataract • Blood pressure measurement • Examination of feet- ulcer; poor sensations/neuropathy
Management Insulin pens

Monitoring
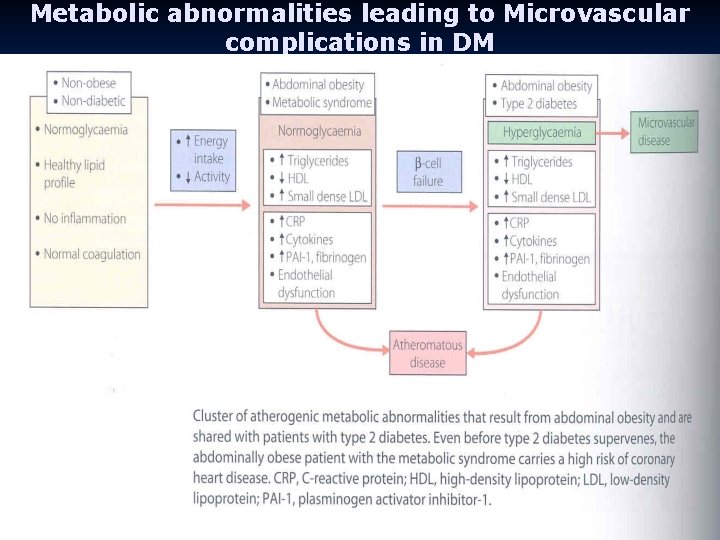
Metabolic abnormalities leading to Microvascular complications in DM
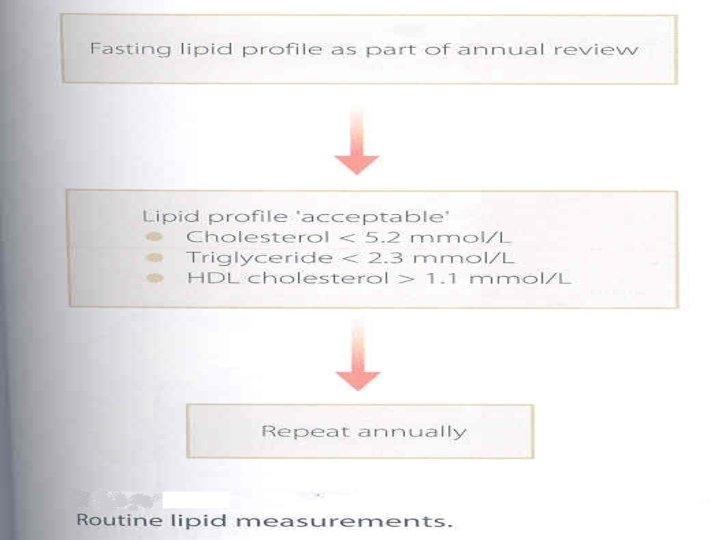
Figure 18. 4
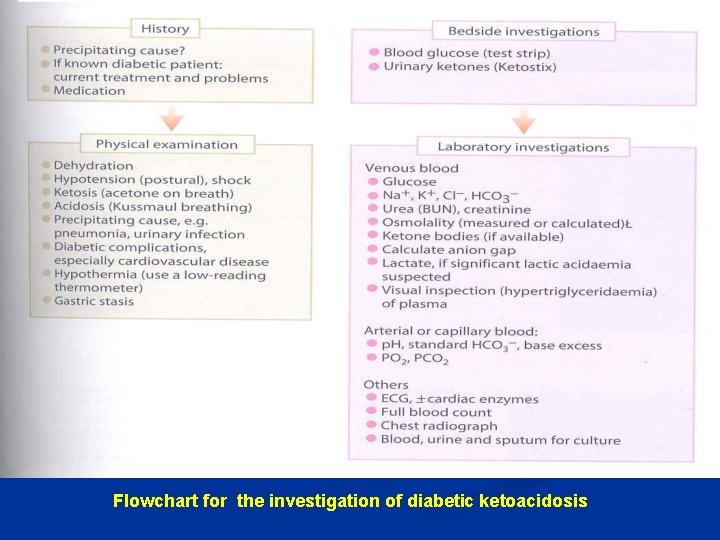
Flowchart for the investigation of diabetic ketoacidosis
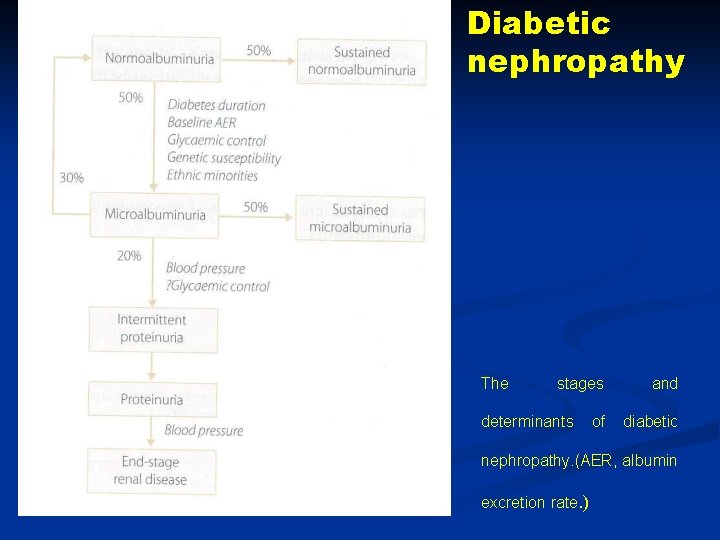
Diabetic nephropathy The stages determinants of and diabetic nephropathy. (AER, albumin excretion rate. )
- Slides: 68