Lab 8 Routine Urine Analysis Identification of Normal
Lab (8): Routine Urine Analysis Identification of Normal Physical and Chemical Urine Constituents KAU-Faculty of Science- Biochemistry department Clinical biochemistry lab (Bioc 416) 2012 T. A Nouf Alshareef nf. shareef@hotmail. com
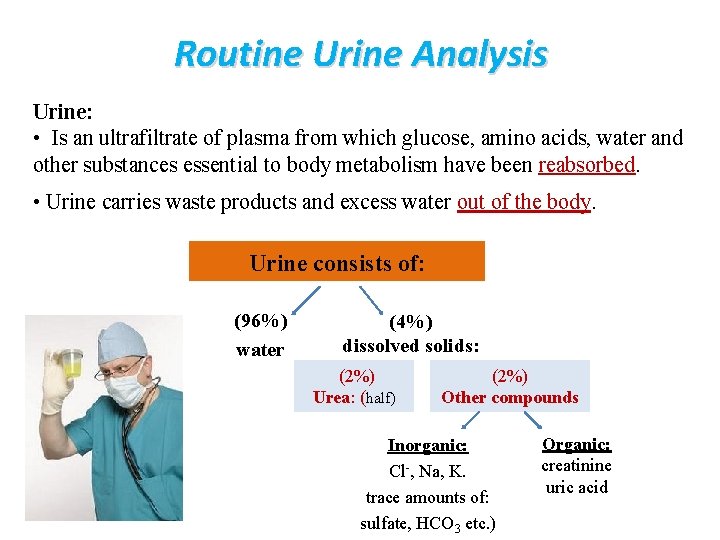
Routine Urine Analysis Urine: • Is an ultrafiltrate of plasma from which glucose, amino acids, water and other substances essential to body metabolism have been reabsorbed. • Urine carries waste products and excess water out of the body. Urine consists of: (96%) water (4%) dissolved solids: (2%) Urea: (half) (2%) Other compounds Inorganic: Cl-, Na, K. trace amounts of: sulfate, HCO 3 etc. ) Organic: creatinine uric acid
Factors affect on urine constituents: • dietary intake, • physical activity, • body metabolism, • endocrine function • others.
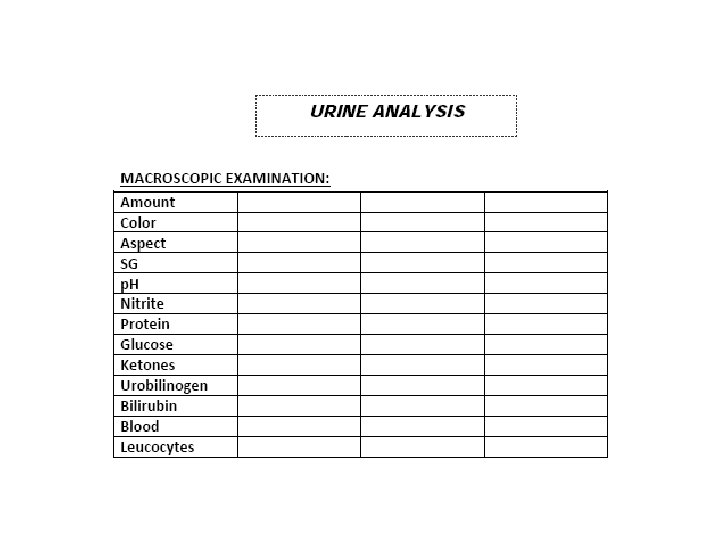
Urine Analysis: Routine Urinalysis (Routine-UA): • It consists of a group of tests performed as part of physical examination. It involves macroscopic and microscopic analysis. Type of analysis: • macroscopic analysis: physical characteristics chemical analysis • microscopic examination: urine sediment is examined under microscope to identify the components of the urinary sediments.
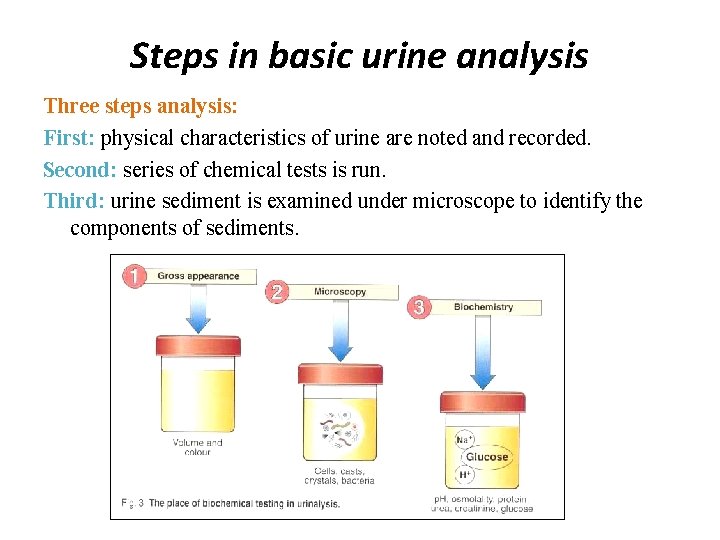
Steps in basic urine analysis Three steps analysis: First: physical characteristics of urine are noted and recorded. Second: series of chemical tests is run. Third: urine sediment is examined under microscope to identify the components of sediments.
Urine Collection: Types of urine specimens: • type of specimen and collection procedure are determined by physician and depend on the tests to be performed. There are basically four types of urine specimens: 1. First morning specimen 2. Random urine specimen 3. Fractional collection 4. Timed collection • Composition and concentration of urine changes during 24 hr • Urine conc. vary according: to water intake and physical activities.
Truly representative sample: • it is necessary to regulate: time of collection, length of collection period, patient's dietary, medical intake and method of collection. • Initial morning sample is preferred (particularly for protein analysis) because they are more concentrated from overnight retention in bladder. • Time of analysis: - must analyzed within 1 h at room temp. or within 8 hr at 2 o. C- 8 o. C - If not assayed within these time limits, several changes will occur. • sample should collected in a clean container. • urine container must be sterile if the urine is to be cultured. • For microscopic examination, the urine must be fresh.
I- Physical Characteristics: • direct visual observation. • Normal fresh urine: Color: pale or dark yellow-amber, clear. • Vol: 750 - 2000 ml/24 hr. • Physical examination involves: 1. Color 2. Transparency 3. Odour 4. Volume 5. p. H 6. Specific gravity
1 - Color: • Color intensity of urine correlates to concentration. • Darker color means more concentrated sample. • Amber yellow Urochrome (derivative of urobilin, produce from bilirubin degradation, is pigment found in normal urine). • Colorless due to reduced concentration. • Silver or milky appearance • Reddish brown • Yellow foam Pus, bacteria or epithelial cells Blood (Hemoglobin). Bile or medications. • Orange, green, blue or red medications.
2 - Transparency: • Is classified as clear or turbid. • In normal urine: the main cause of cloudiness is crystals and epithelial cells. • In pathological urine: it is due to pus, blood and bacteria. • Degree of cloudiness depends on: p. H and dissolved solids Ø Turbidity: may be due to gross bacteriuria, Ø Smoky appearance: is seen in hematouria. Ø Thread-like cloudiness: is seen in sample full of mucus.
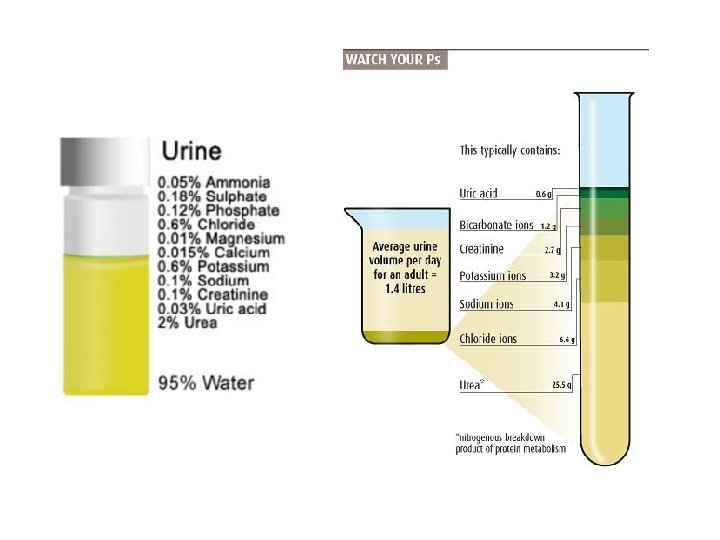
3 - Odour: Odour has little diagnostic significance. 1. Aromatic odour------> Normal urine due to aromatic acids. 2. Ammonia odour------> On standing due to decomposition of urea. 3. Fruity odour----> Diabetes due to the presence of ketones. 4 - Volume: • Is important part of assessment for fluid balance and kidney functions. • Adults produce from 750 ml-2500 ml / 24 h, with the average of about 1. 5 L person. • For RUA, a 10 ml-12 ml of sample is optimal for accurate of analysis
5 - p. H: • p. H measure acidicity or alkalinity (basic) of urine • Normal urine p. H: 4. 5 -8. • Increased acidity in urine: due to diabetes or medications. • Urine sample must be fresh (why? ) (on standing urine become alkaline as a result of ammonia liberation due to urea decomposition). 6 - Specific Gravity (SG): • measures the amount of substances dissolved in urine. • also indicates how well kidneys are able to adjust amount of water in urine. • higher SG: more solid material is dissolved in urine
Normal Chemical Constituents of Urine: Organic: urea, uric acid, creatinine Inorganic: Cl-, PO 4 -3, HBO 3, NH 4, SO 4 -2 1 - Urea: 1 ml urine + 3 ml Na. OCL (sodium hypochlorite) ==>Evolution of N 2 gas. 2 - Uric acid UA: 1 ml urine + 0. 5 ml 10% Na. OH +1 ml Folins reagent ===> Blue color. 3 - Creatinine: - 1 ml urine + drops Picric acid + drops Na. OH ====> red color ppt. Note: if reaction is acidified with HCL, the color changes to yellow.
4 - Chloride: - 1 ml urine + drops HNO 3 +1 ml Ag. NO 3===> white ppt of Ag. CL 5 - Phosphate: 1 ml urine + 1 ml conc. HNO 3 + 1 ml NH 4 -molybdate===>Yellow color. 6 - Carbonate: 1 ml urine + drops conc. HCL ==> Na 2 CO 3 + 2 HCL ==> H 2 O + 2 Na. CL + CO 2 (effervescence) 7 - Ammonia: - Make urine alkaline with Na. OH. Close the tube with a cork containing another side tube dipped in Nessler's reagent. Heat the urine and then notice the evolving of NH 3 in Nessler's reagent - Detect NH 3 by its odour. - 1 ml urine + 1 ml phenol + 1 ml Na. Br =======> Blue color. 8 - Sulphates: - 1 ml urine + 2 drops conc. HCL + few drops Ba. CL 2 ===> White ppt of Ba. SO 4 + Ba. CL 2 =====> Ba. SO 4 + 2 CL-
Lab Practices: • Collect urine in a clean container. • Run routine UA on the sample by using both urine strip and the method described before for chemical analysis. • Record the results in the lab report of UA.
http: //human-physiology---ashley-vg. wikispaces. com/Urology http: //nursingcrib. com/medical-laboratory-diagnostic-test/nursing-considerations-for-routine-urinalysis/ http: //ahdc. vet. cornell. edu/clinpath/modules/ua-rout. htm
- Slides: 19