L 04 A Just Working in an FQHC



- Slides: 43
L 04 A Just Working in an FQHC isn’t enough: Training Residents for Underserved Care Christine Jacobs MD FAAFP Program Director Saint Louis University FMR St Louis MO April 26, 2015
Disclosures • I have no conflict of interest
Objectives On completion of this session, you should be able to: • Assess your residency training program for current activities and outcomes in preparing physicians for underserved care. • Identify and strengthen programmatic areas within the residency that complement ambulatory underserved training. • Describe curricular activities that increase residents’ knowledge, attitudes and skills in underserved care.
Step 1: Assess your Residency • Please complete the residency selfassessment form.
Residency Self Assessment • Outcomes– Knowledge/Attitudes/Skills – Graduate practice choice • Input– Recruiting – Conferences – Experiential learning – Practice – Mentoring
Why Do Physicians Enter Underserved Practice? • Life experiences/background/ community of origin • Social commitment • Residency clinical experiences • Residency curriculum
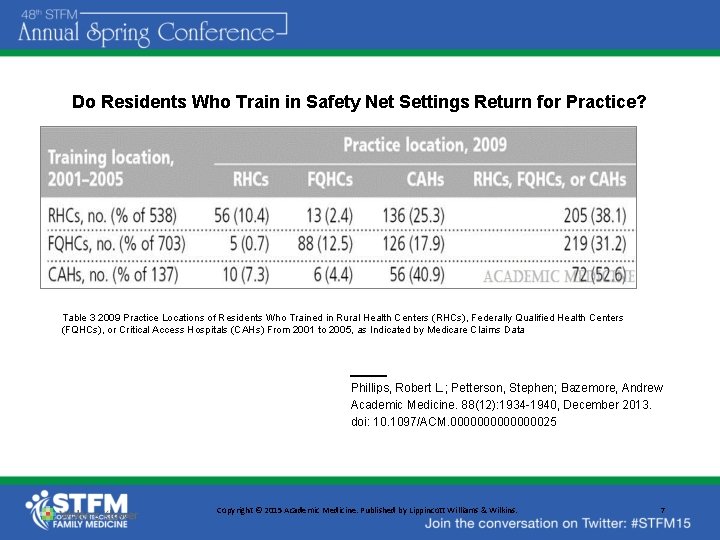
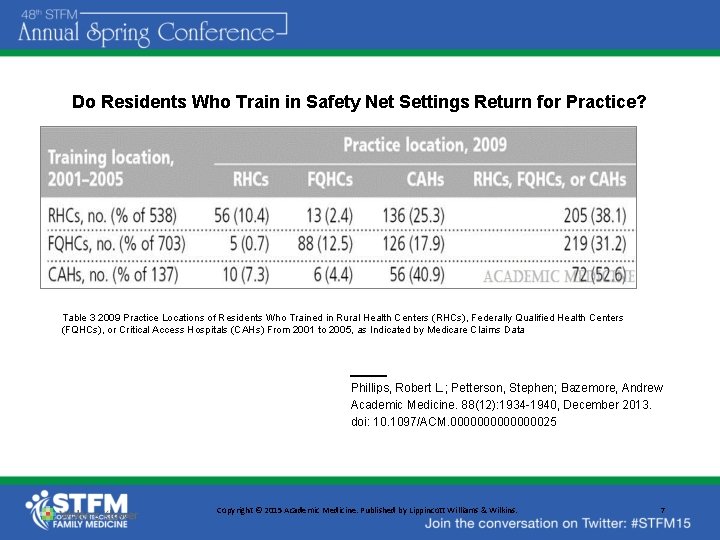
Do Residents Who Train in Safety Net Settings Return for Practice? Table 3 2009 Practice Locations of Residents Who Trained in Rural Health Centers (RHCs), Federally Qualified Health Centers (FQHCs), or Critical Access Hospitals (CAHs) From 2001 to 2005, as Indicated by Medicare Claims Data Phillips, Robert L. ; Petterson, Stephen; Bazemore, Andrew Academic Medicine. 88(12): 1934 -1940, December 2013. doi: 10. 1097/ACM. 000000025 Copyright © 2015 Academic Medicine. Published by Lippincott Williams & Wilkins. 7
What Predicts Preparedness for Cross-Cultural Care? • Mail Survey of 1150 residents (family medicine, internal medicine, pediatrics and OB/gyne) in 2004: • Among the strongest predictors of preparedness were the training characteristics, including having role models, a greater cross-cultural case mix during residency, and receiving more instructional opportunities for learning crosscultural care. • Greer. JA et al. Primary care resident perceived preparedness to deliver cross-cultural care: an examination of training and specialty differences. J Gen Intern Med. 2007 Aug; 22(8): 1107 -13.
What Barriers To Underserved Practice Do Family Medicine Residents Encounter? Knowledge • Lack of education about health disparities • Lack of confidence in preparedness for complex medicine Attitude • Workload burnout in residency • Faculty/role model unhappiness • Salary Skills • Lack of mastery of challenging patient interactions
How Do We… • Give resident physicians the skills and cultural competence to care for underserved patients? • Train family physicians who want to care for underserved patients? (while keeping residents from becoming overwhelmed or burned out in that process)
Our Answer: Longitudinal Underserved Community Curriculum Comprehensive Curriculum started concurrently with the residency in 2011
Saint Louis University Family Medicine Residency • 12 residents, increasing to 18 • University-FQHC-Hospital Partnership – Saint Louis University – Family Care Health Centers – SSM St. Mary’s Health Center

Family Care Health Center • Federally Qualified Health Center founded 1969 • Family Medicine, IM, OB, Psych • Eye, dental, pharmacy • Integrated Behavioral Health
Longitudinal Underserved Community Curriculum • Early orientation to the community • 12 PGY 2 Community Health Seminars • 18 month repeating Community-Focused lectures • Recruiting of diverse residents • Career counseling • Physician mentoring
Orientation Month • • • Clinic orientation Windshield survey Poverty simulation Domestic violence simulation Community nurse visits- newborns & elders • Personal & Professional Identity Sessions
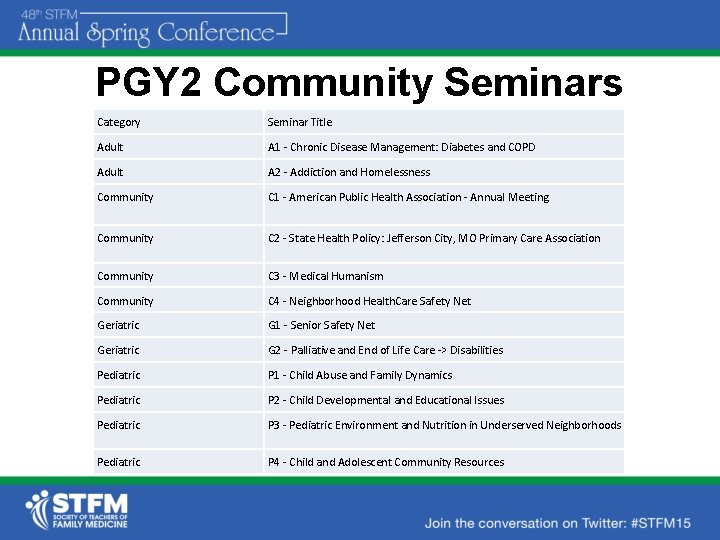
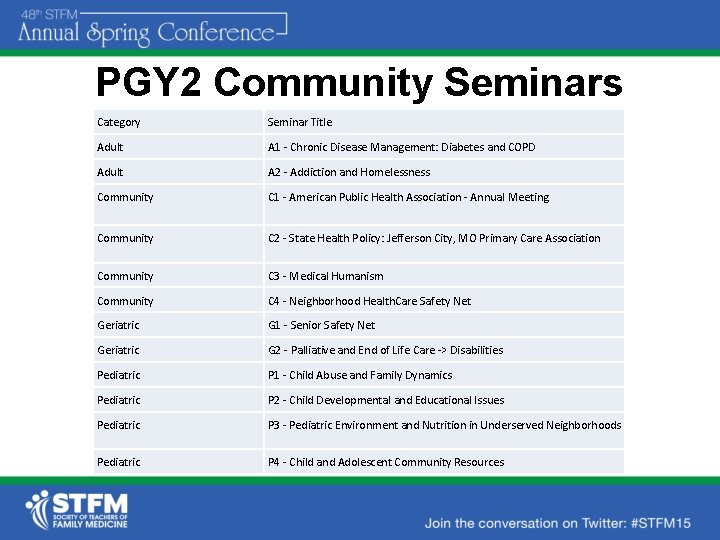
PGY 2 Community Seminars Category Seminar Title Adult A 1 - Chronic Disease Management: Diabetes and COPD Adult A 2 - Addiction and Homelessness Community C 1 - American Public Health Association - Annual Meeting Community C 2 - State Health Policy: Jefferson City, MO Primary Care Association Community C 3 - Medical Humanism Community C 4 - Neighborhood Health. Care Safety Net Geriatric G 1 - Senior Safety Net Geriatric G 2 - Palliative and End of Life Care -> Disabilities Pediatric P 1 - Child Abuse and Family Dynamics Pediatric P 2 - Child Developmental and Educational Issues Pediatric P 3 - Pediatric Environment and Nutrition in Underserved Neighborhoods Pediatric P 4 - Child and Adolescent Community Resources
Adult 1 - Chronic Disease • • • Conversation with COPD patient Half day diabetes/half day COPD Guideline reviews Hands-on spirometry/ inhaler training Management discussions EHR template review
Adult 2 - Homelessness and Addiction • Agency visit: provider of housing, employment and health opportunities for people who are homeless or at risk of becoming homeless • Detox medication learning session • Immunizing homeless clients
Pediatric 1 – Child Abuse and Family Dynamics • Speaker – Lead ER Social Worker: Child abuse statistics, myths, risk factors, red flags, and state laws. • Learning Session – Evaluation and management of child sexual abuse • Speaker – Author of first-hand account of child abuse (required reading for session)
Pediatric 2 - Child Developmental and Educational Issues • Speaker from area independent school • Simulation- dyslexia and other learning disabilities • Immigrant parent discussing experiences
Pediatric 3 - Pediatric Environment and Nutrition • Learning session – Childhood obesity, nutrition recommendations, WIC program, obesity prevention, co-morbidities • Experiential learning – Residents tasked with purchasing a healthy lunch in neighborhood; evaluated by dietitian • Guest speaker – Health Education Specialist and Health Coach
Pediatric 4 - Child and Adolescent Community Resources • Speaker- local agency providing evidencebased programming and resources for disadvantaged teens • Speaker- Coalition on Human Trafficking: Red flags, the role of the provider, and resources • Agency Tour- emergency maternity shelter, supporting young women through a healthy pregnancy
Geriatric 1 - Senior Safety Net • Learning session – Medicare, Medicaid, SSI, SSDI • Alzheimer’s Association presentation • Community visits – Adult day care – Adult drop-in/ meal center – Senior housing – Speech and hearing agency
Geriatric 2 - Palliative Care and End-of-Life • Learning session – Introduction to Hospice and Palliative Care • Hospice interdisciplinary team meeting • Conversation with hospice physician • Half-day learning session with cases: – Pain – Symptom relief at end of life
Community 1 - Conference • National Association of Community Health Centers • American Public Health Association
Community 2 - State Health Policy • Preparatory lecture re. current legislative issues • Trip to State Capitol • Meeting with Primary Care Association leaders and lobbyists • Conversations with legislators
Community 3 - Medical Humanism • • Yoga Personal/professional identity follow up Reflective writing & optional sharing Discussions of: – Meaningful Scut Work – Verghese TED talk – Facing Our Mistakes • Reflective writing
Community 4 - Neighborhood Healthcare Safety Net • Visit to another Federally Qualified Health Center • Settlement house with neighborhood projects

New Seminars • Disability/Implicit Bias exchanged for Hospice and Palliative Care • International experience including citizenship swearing in and cultural conversations.

Community- Focused Lectures • Cultural Competency (Bosnian, Albanian, Somali, and Hispanic populations; Use of interpreters; Citizenship and naturalization) • Health Disparities (Understanding Poverty, Health Outcomes in the Region, LGBT, health literacy) • Behavioral (addictions, adolescent risky behavior, SBIRT) • Violence (intimate partner violence, human trafficking) • Policy (State healthcare policy, Affordable Care Act)
Continuity Practice • Precepting and clinical experience with the seminar faculty • Tools learned in seminars integrated into practice
Career Counseling • Orientation- intro to practice models by Primary Care Association • Annual meetings with PCA representative • Exposure to family physicians in Community Health Center practices
Resident Recruiting • Underrepresented minorities • Liaison with school • Lectures at local medical schools about the resident experience of healthcare in community health centers • Integrated behavioral health • Clarity of priorities
Faculty Mentoring • Seminars allow residents to experience faculty in more intimate setting • Out-of-the-Box experiences
LUCC Evaluation • Knowledge/Attitudes: Pre- and postsurveys for all seminars and lectures: Knowledge and attitudes showed consistent improvement. Annual resident survey documents increasing comfort with cultural and community issues • Skills: Progress on milestones
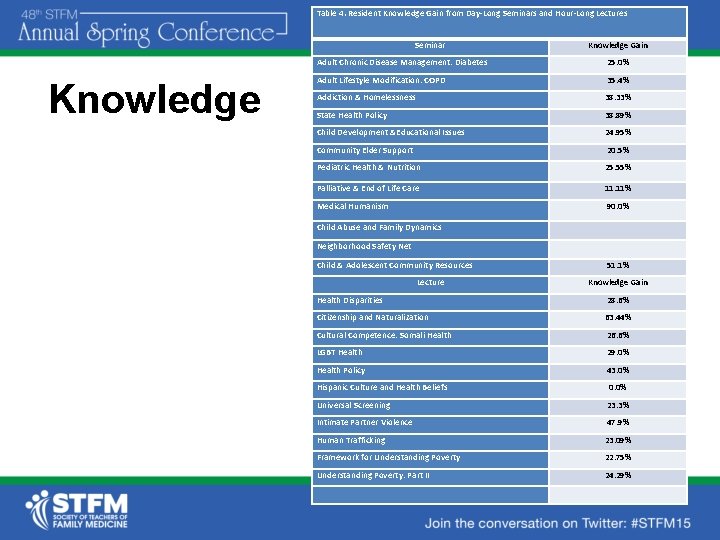
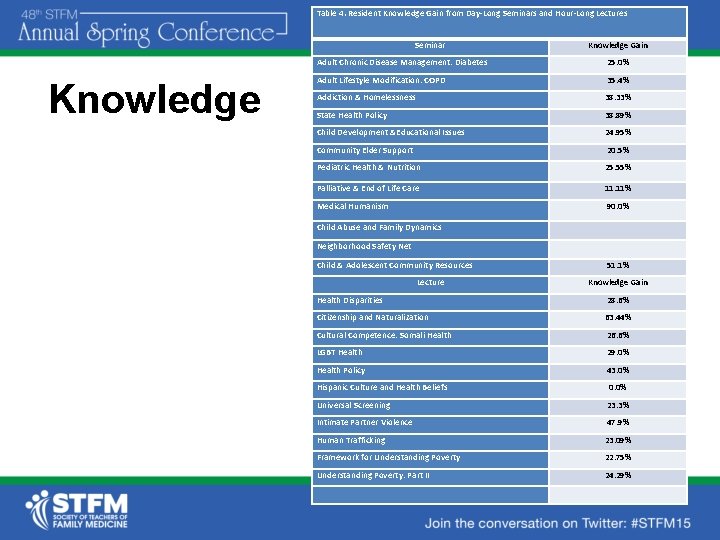
Table 4. Resident Knowledge Gain from Day-Long Seminars and Hour-Long Lectures Seminar Knowledge Gain Adult Chronic Disease Management: Diabetes 25. 0% Adult Lifestyle Modification: COPD 35. 4% Addiction & Homelessness 38. 33% State Health Policy 38. 89% Child Development &Educational Issues 24. 95% Community Elder Support 20. 5% Pediatric Health & Nutrition 25. 55% Palliative & End of Life Care 11. 11% Medical Humanism 90. 0% Child Abuse and Family Dynamics Neighborhood Safety Net Child & Adolescent Community Resources Lecture 51. 1% Knowledge Gain Health Disparities 28. 6% Citizenship and Naturalization 63. 44% Cultural Competence: Somali Health 26. 6% LGBT Health 29. 0% Health Policy 43. 0% Hispanic Culture and Health Beliefs 0. 0% Universal Screening 23. 3% Intimate Partner Violence 47. 9% Human Trafficking 23. 09% Framework for Understanding Poverty 22. 75% Understanding Poverty: Part II 24. 29%
Attitudes • “Be more on the lookout for ways to address clinic and community level public health issues. ” • “It helped me to see that the work we do as physicians is important and can impact the lives of our patients. …in general I will make it a priority to continue to treat each patient with the same standards despite ethnicity and give the best care I can in the most objective and compassionate manner. ” • “More awareness of the challenges my homeless patients face and resources to help them. ” • “Now I know more resources and referrals to provide to patients. ”
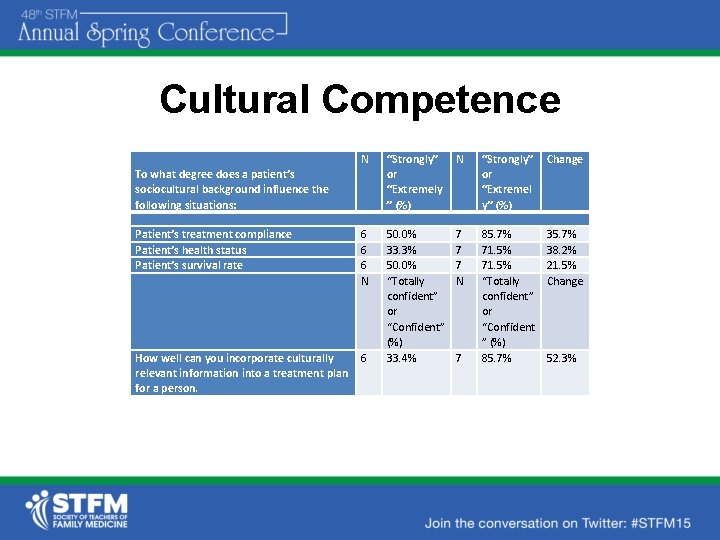
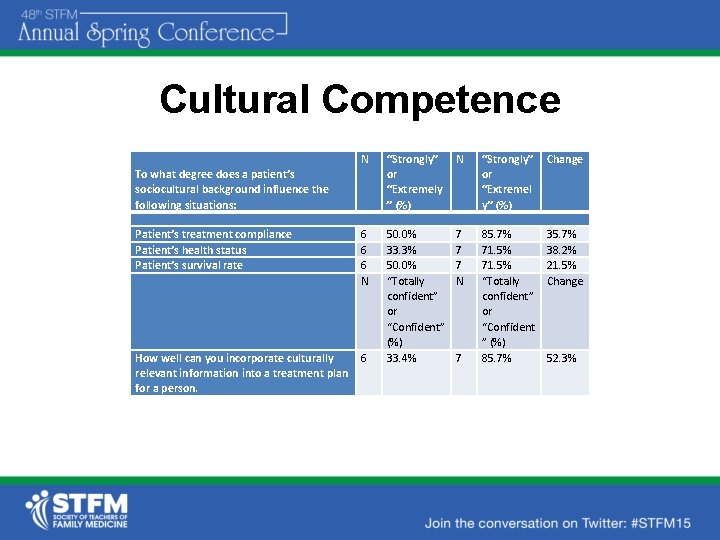
Cultural Competence N “Strongly” or “Extremely ” (%) N “Strongly” or “Extremel y” (%) Change Patient’s treatment compliance Patient’s health status Patient’s survival rate 6 6 6 N 7 7 7 N 6 85. 7% 71. 5% “Totally confident” or “Confident ” (%) 85. 7% 38. 2% 21. 5% Change How well can you incorporate culturally relevant information into a treatment plan for a person. 50. 0% 33. 3% 50. 0% “Totally confident” or “Confident” (%) 33. 4% To what degree does a patient’s sociocultural background influence the following situations: 7 52. 3%
Conclusion • A multi-faceted longitudinal curriculum in underserved care can provide residents with tools and comfort in caring for patients with health disparities. • We believe this training will increase resident affinity and success in caring for underserved communities.
References • Phillips RL, Petterson S, Bazemore A. Do Residents Who Train in Safety Net Settings Return for Practice? Acad Med 2013. 88(12): 1934 -1940. • Greer. JA et al. Primary care resident perceived preparedness to deliver cross-cultural care: an examination of training and specialty differences. J Gen Intern Med. 2007 Aug; 22(8): 1107 -13.
Resources • Assessing Change: Evaluating Cultural Competence Education and Training. AAMC 2015. • Hasnain M, Massengale L, Dykens A, Figueroa E. Health Disparities Training in Residency Programs in the United States. Fam Med 2014; 46(3): 186 -91. • Response in Fam Med 2014; 46(10): 809 -810. • U. S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. Washington, DC. Available at [http: //www. healthypeople. gov/2020/].
• This project is supported by the Health Resources and Services Administration (HRSA) of the U. S. Department of Health and Human Services (HHS) under grant number D 58 HP 23229, Residency Training in Primary Care, total award amount: $652, 421. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U. S. Government.
Please evaluate this session at: stfm. org/sessionevaluation