KONJENTAL KALP HASTALIKLARI Yrd Do Dr Cenk Eray















- Slides: 65

KONJENİTAL KALP HASTALIKLARI Yrd. Doç. Dr. Cenk Eray YILDIZ Kalp Ve Damar Cerrahisi A. D. KALP DAMAR CERRAHİSİ ANABİLİM DALI Prof. Dr. Süha KÜÇÜKAKSU Yrd. Doç. Dr. Cenk Eray YILDIZ Yrd. Doç. Dr. Mehmet ERGENOĞLU Dr. Halit YEREBAKAN
Kalp ve Damar Cerrahisine Genel Bakış • İskemik kalp hastalıkları • Kalp kapak hastalıkları • Konjenital kalp hastalıkları preoperatif dönem peroperatif dönem postoperatif dönem
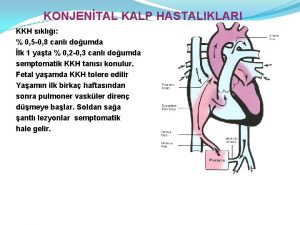
Konjenital kalp hastalıkları (KKH) sınıflaması ve cerrahisi • *SHUNT OLUŞTURANLAR: -Asiyanotik (sol-sağ şant) (Geç siyanotik) -Siyanotik (sağ-sol şant) (erken siyanotik) • *Obstrüktif lezyonlar • *Kompleks malformasyonlar • *Diğer lezyonlar

• • Dikkat: KALP(? ) Morarma Emme güçlüğü İştahsızlık Nefes darlığı Çarpıntı Düşük doğum ağırlığı(DİYABET) Gelişme geriliği Çabuk yorulma
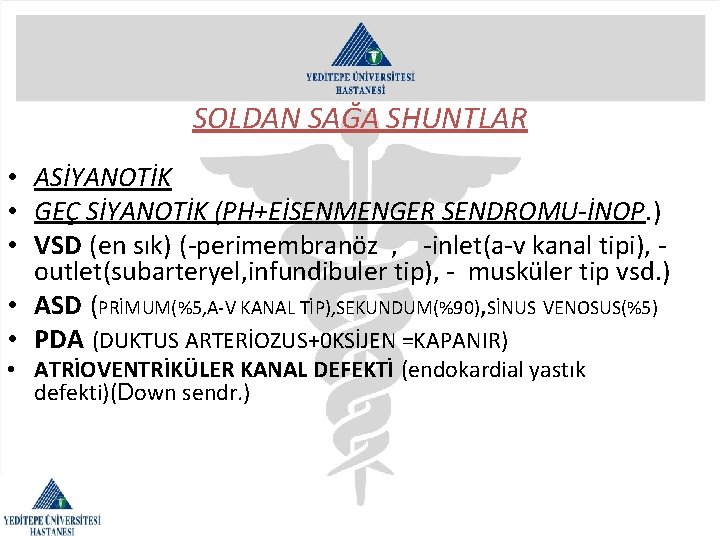
SOLDAN SAĞA SHUNTLAR • ASİYANOTİK • GEÇ SİYANOTİK (PH+EİSENMENGER SENDROMU-İNOP. ) • VSD (en sık) (-perimembranöz , -inlet(a-v kanal tipi), outlet(subarteryel, infundibuler tip), - musküler tip vsd. ) • ASD (PRİMUM(%5, A-V KANAL TİP), SEKUNDUM(%90), SİNUS VENOSUS(%5) • PDA (DUKTUS ARTERİOZUS+0 KSİJEN =KAPANIR) • ATRİOVENTRİKÜLER KANAL DEFEKTİ (endokardial yastık defekti)(Down sendr. )

SAĞDAN SOLA SHUNTLAR (ERKEN SİYANOTİK, MAVİ BEBEK) • FALLOT TETRALOJİSİ(vsd+ata binen aorta+pulm. kapak stenozu+sağ vent. hipertrofisi)+ASD varsa fallot pentalojisi olur. (SABO, TAHTA PABUÇ KALP) • BÜYÜK DAMAR TRANSPOZİSYONU(BAT) • TRUNKUS ARTERİOZUS(acil op. ) • TRİKUSPİD ATREZİ • HİPOPLASTİK SOL KALP SENDROMU. • TOTAL ANORMAL VENÖZ DÖNÜŞ. (KARDAN ADAM KALP) • PULMONER ATREZİ.
Klinik semptomlar Soldan sağa shuntlarda; küçük defektler asemptomatiktir, spontan kapanabilir. Büyük defektler büyüme gerilği, beslenme bozukluğu, çabuk yorulma, enfektif endokardit, akc. infeksiyonu, yüksek shunt oranı ile akc. ye aşırı perfüzyon sonucu pulmoner hipertansiyon(küçük musküler arterlerde medial hipertrofi, intimal hiperplazi ve obstrüksiyon, intimal fibrozis, küçük arter dilatasyonu , kavernöz ve anjiomatoid lezyonlar, nekrotizan arterit. ), eisenmenger sendromu(sağ kalp yetersizliği, siyanoz, ölüm)
Klinik semptomlar • Sağdan sola shuntlarda; doğumdan hemen sonra , bebeklik ya da daha ileri çocukluk döneminde siyanoz atakları(taşipne, dispne, -fallot tetrolojisine karakteristik- çömelme pozisyonu görülür. Kalp yetersizliği, enfektif endokardit(jet akım) riski artar. Hipoksik bebeklerde polisitemi olur. Hct: %65 i aşarsa aşırı vizkozite , paradoksik embolizasyon, sistemik venöz emboli, arteryel emboli, septik emboli, beyin absesine yol açar.
Etyoloji; • 6 -8/1000 sıklıkta, maternal(4 -9 hafta) viral infeks. (rubella), kr. alkol alımı, talidomid vs. , insüline bağlı diabet, fenilketonüri, ikizlerden birinde defekt, kromozom anomalisi. • Turner send. PDA, AO KOARKTASYONU • Kartagener send. -kardiak situs inversus • Fetal alkol send. VSD • SİYANOZ: Arter kanında oksijenlenmemiş Hb konsantrasyonun 5 gr/desilitre yi aşmasıdır.
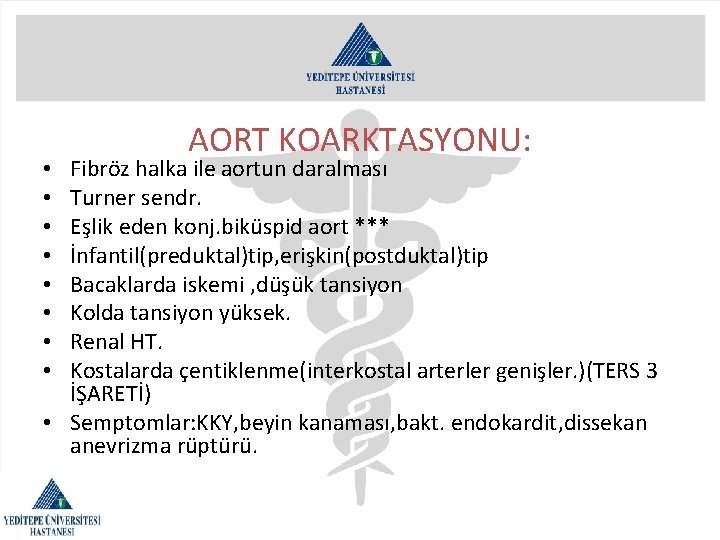
OBSTRÜKTİF LEZYONLAR: • Aort koarktasyonu • Aort stenozu • Pulmoner stenoz
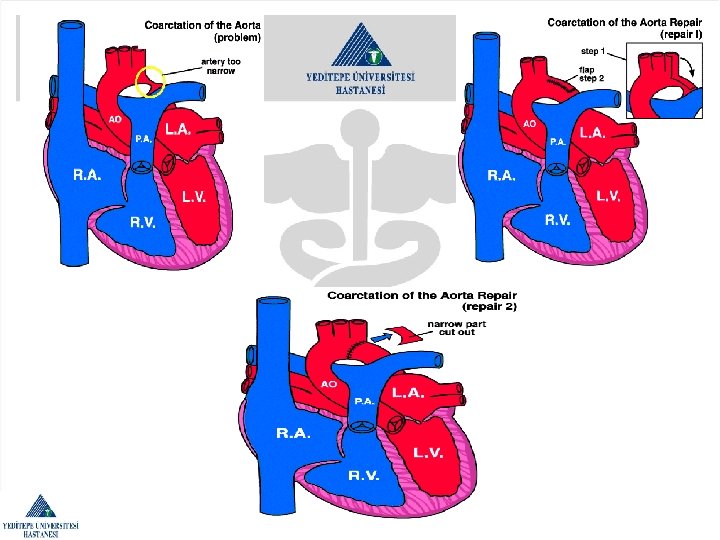
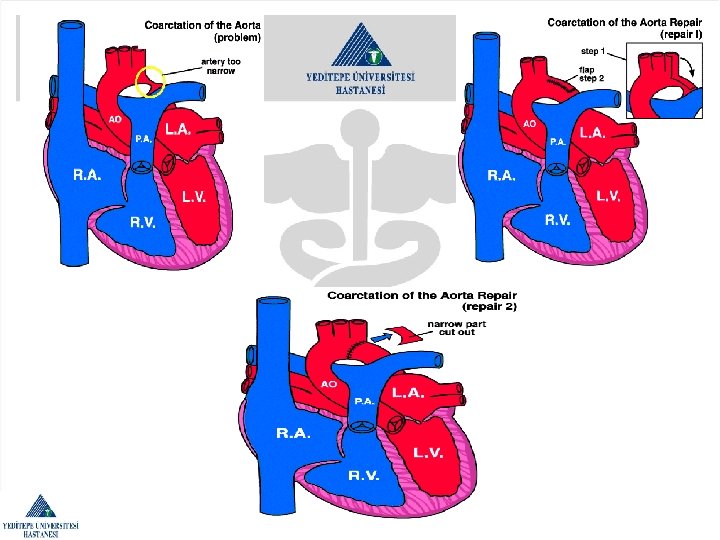
AORT KOARKTASYONU: Fibröz halka ile aortun daralması Turner sendr. Eşlik eden konj. biküspid aort *** İnfantil(preduktal)tip, erişkin(postduktal)tip Bacaklarda iskemi , düşük tansiyon Kolda tansiyon yüksek. Renal HT. Kostalarda çentiklenme(interkostal arterler genişler. )(TERS 3 İŞARETİ) • Semptomlar: KKY, beyin kanaması, bakt. endokardit, dissekan anevrizma rüptürü. • •
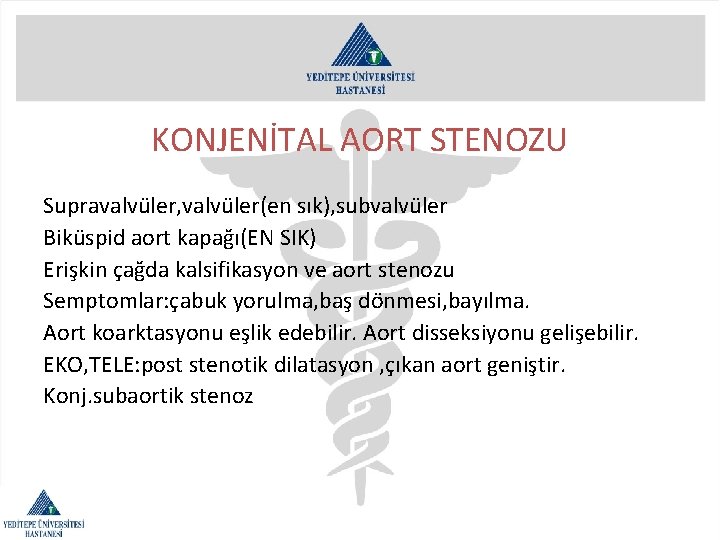
KONJENİTAL AORT STENOZU Supravalvüler, valvüler(en sık), subvalvüler Biküspid aort kapağı(EN SIK) Erişkin çağda kalsifikasyon ve aort stenozu Semptomlar: çabuk yorulma, baş dönmesi, bayılma. Aort koarktasyonu eşlik edebilir. Aort disseksiyonu gelişebilir. EKO, TELE: post stenotik dilatasyon , çıkan aort geniştir. Konj. subaortik stenoz
KONJENİTAL PULMONER STENOZ • Akc. yeterli kan gitmez. sağ vent. engeli aşamaz. • Darlık balon valvuloplasty veya açık kalp cerrahisi(pulm. Valvotomi) ile giderilir.

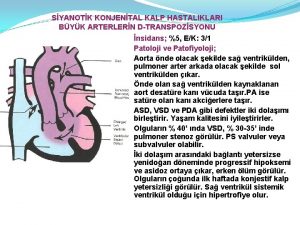
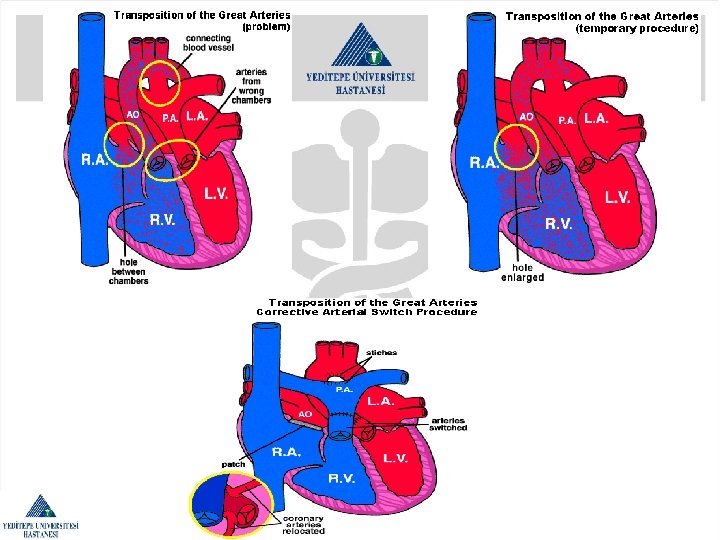
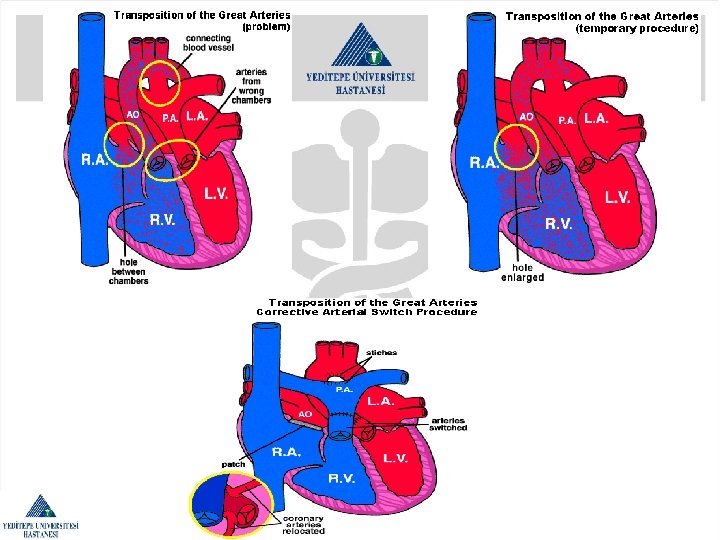
Kompleks malformasyonlar Büyük damarların transpozisyonu(TGA, BAT): 1 yaş altı siyanoz (en sık) Ventrikülo-arteryal discordans Atrioventriküler Kapakçıklar (mitral, triküspit) ventrikülden gelişir. Herzaman bu kapaklar kendi ventrikülünün olduğu taraftadır. Mitral kapak ; morfolojik sol ventrikülde, triküspit kapak ; morfolojik sağ ventriküldedir. • Atrio-ventriküler concordans , aort sağdaki sağ ventrikülden, pulmoner arter soldaki sol ventrikülden çıkar. • Doğumdan hemen sonra tanı konulan hastanın acil opere edilmesi gerekir. Bu durumda pulmoner akım, sistemik akım oranları, pulmoner arter çapları önemlidir. palyatif blalock-tausing shunt veya tam düzeltme ameliyatı= jatene operasyonu(arteryel switch) yapılır. • Blalock-tausing shunt sağ veya sol subclavian arter-pulmoner arter arasında yapılır. pulmoner arterlerin çapı, arkus aortanın yönü önemlidir. • •
KONJENİTAL KORONER ARTER ANOMALİLERİ: • Koroner arter çıkış anomalisi(ALCAPA) • ‘’ ‘’ sonlanış ‘’ • ‘’ ‘’ seyir ‘’ • ‘’ ‘’ anevrizmaları



• • 1 in every 120 births has CHD Mild – resolve by themselves Non life threatening – but require treatment Severe – multiple operations , lifetime medication
What causes congenital heart defects? • • • Present at birth Fetal development An infant's chromosomes (5 to 6 percent ) Single gene defects (3 to 5 percent) Environmental factors (2 percent) There is no identifiable (In 85 to 90 percent of cases) • Multifactorial inheritance
Maternal factors and CHD • • • The first few weeks of pregnancy (49 day) Maternal illnesses and medications Lithium (Anti-depression) Mothers who have phenylketonuria (PKU) Women with insulin-dependent diabetes (particularly if the diabetes is not well-controlled) • Lupus (SLE) • Rubella, MMR vaccine (pregnant)
Family history and CHD • If you have had one child with congenital heart disease, the chance… from 1. 5 to 5 percent. • Two children with CHD, then the risk increases to 5 to 10 percent. • Mother has CHD ranges from 2. 5 to 18 percent (average risk of 6. 7 percent) • Father has CHD from 1. 5 to 3 percent. • Obstructions to blood flow in the left side of the heart have a higher rate of recurrence than other heart defects. • Autosomal-dominant inheritance 50 percent chance with each pregnancy

• Fetal echocardiography can be performed in the second trimester, at about 18 to 20 weeks of pregnancy, to determine the presence of major heart defects in the fetus.
Chromosome abnormalities and CHD • 5 to 8 percent of all babies with CHD have a chromosome abnormality. • Down syndrome • trisomy 18 and trisomy 13 • Turner's syndrome • Cri du chat syndrome • Wolf-Hirshhorn syndrome • Velo-cardio-facial syndrome and/or Di. George sequence • William’s syndrome
Single gene defects • There an estimated 70, 000 genes contained on the 46 chromosomes in each cell of the body. • Marfan syndrome • Smith-Lemli-Opitz syndrome • Ellis-van Creveld • Holt-Oram syndrome • Noonan syndrome • Mucopolysaccharidoses
The others; • Goldenhar syndrome (hemifacial microsomia) • William's syndrome, • VACTERL association (tracheal and esophageal malformations associated with vertebral, anorectal, cardiac, renal, radial, and limb abnormalities make up the VACTERL syndrome).

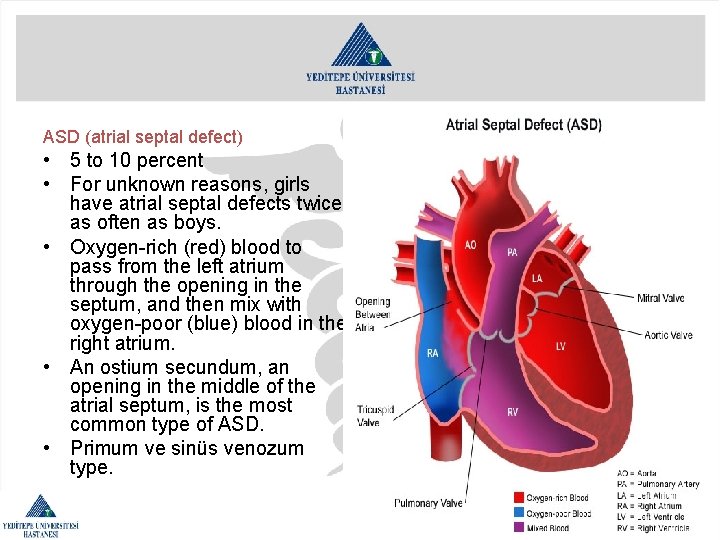
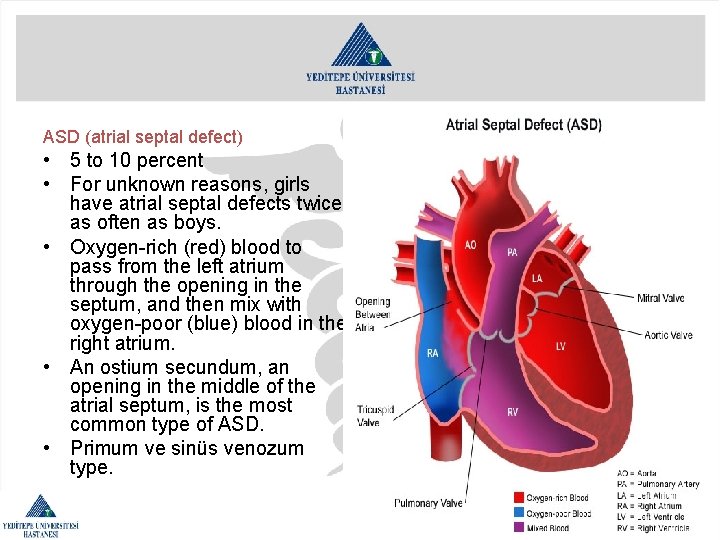
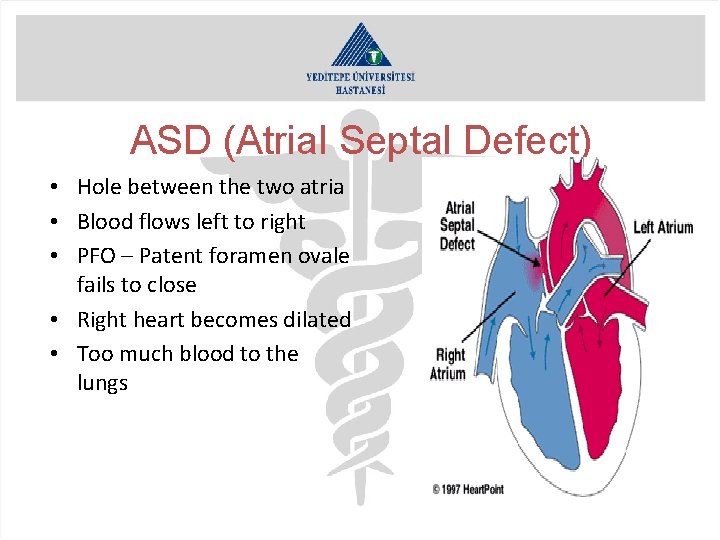
ASD (atrial septal defect) • 5 to 10 percent • For unknown reasons, girls have atrial septal defects twice as often as boys. • Oxygen-rich (red) blood to pass from the left atrium through the opening in the septum, and then mix with oxygen-poor (blue) blood in the right atrium. • An ostium secundum, an opening in the middle of the atrial septum, is the most common type of ASD. • Primum ve sinüs venozum type.
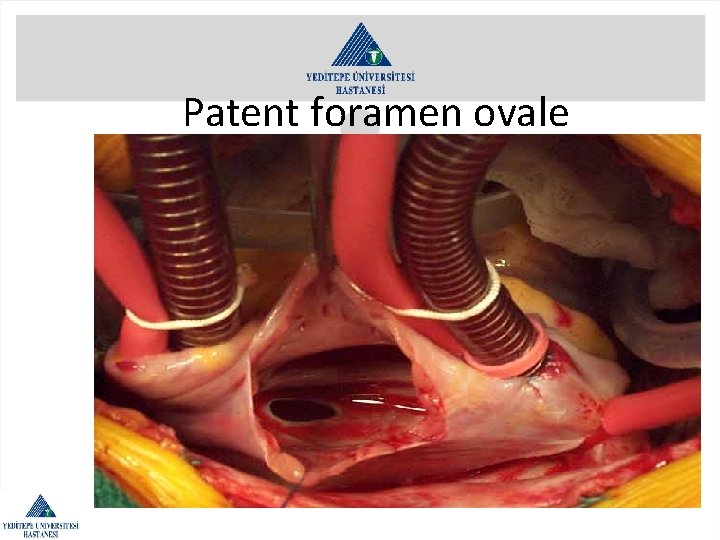
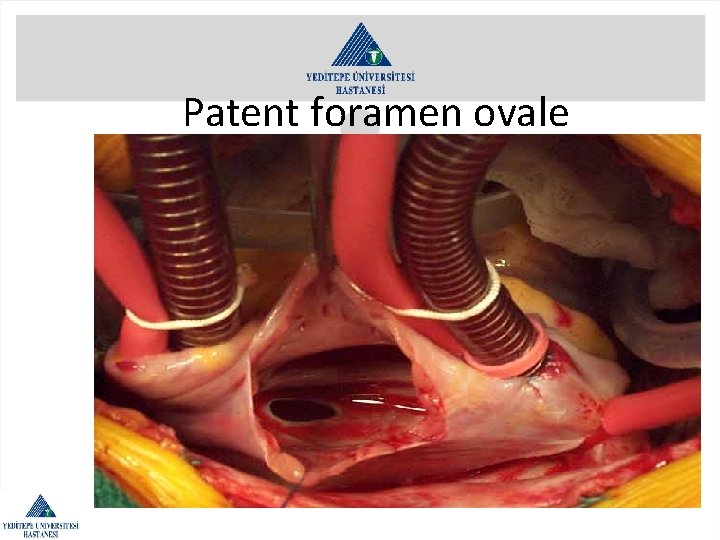
Patent foramen ovale
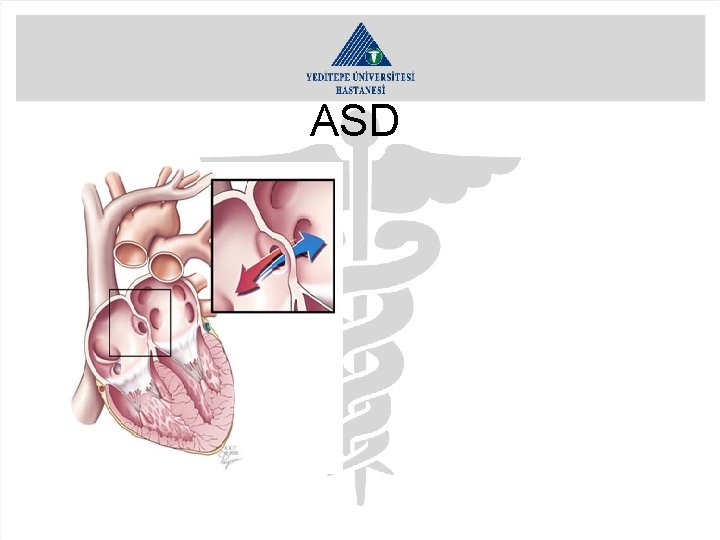
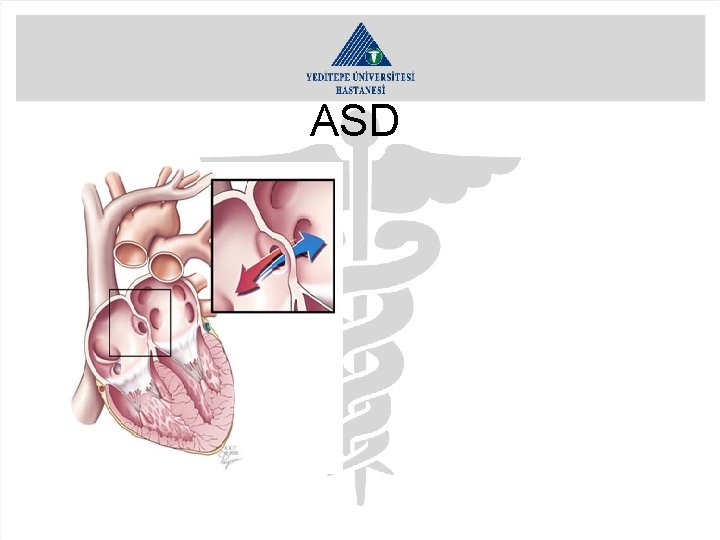
ASD
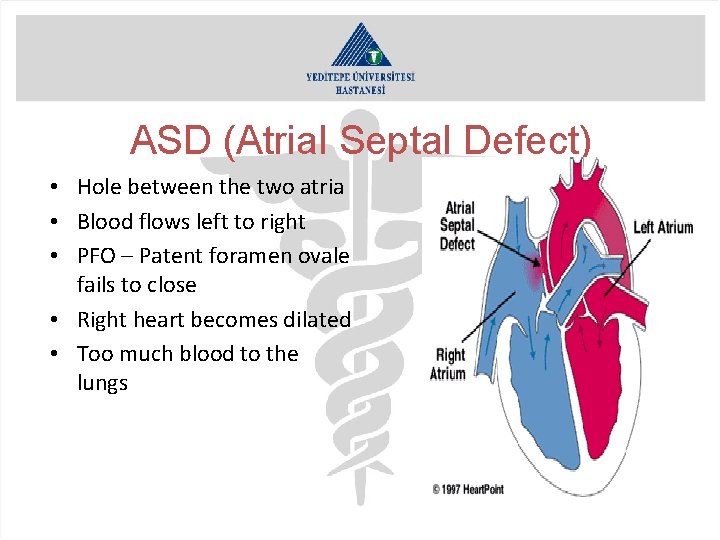
ASD (Atrial Septal Defect) • Hole between the two atria • Blood flows left to right • PFO – Patent foramen ovale fails to close • Right heart becomes dilated • Too much blood to the lungs
ASD (Atrial Septal Defect) • • Primum ASD Secundum ASD Sinus venosus AVSD – Atrio ventricular septal defect
ASD (Atrial Septal Defect) • Secundum – closure in cath lab if suitable • Surgery – patch or stitch – CP bypass • Smaller defects – allow time to close - ? Stroke in later life
What are the symptoms of an atrial septal defect? • child tires easily when playing • fatigue • sweating • rapid breathing • shortness of breath • poor growth • frequent respiratory infections
How is an atrial septal defect diagnosed? • • • Chest X-ray Electrocardiogram (ECG or EKG) Echocardiogram (echo) Cardiac Catheterization Cardiac Magnetic Resonance Imaging (MRI)

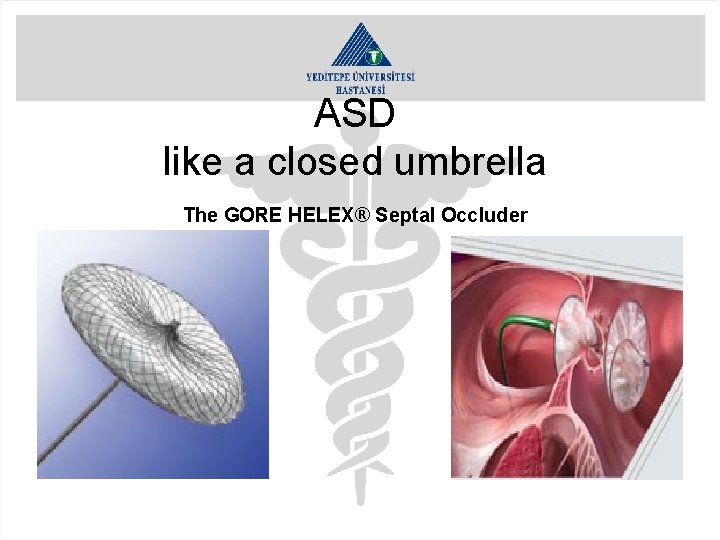
What are the treatments for atrial septal defect? • Medical Management; Digoxin Diuretics • Infection Control • Cardiac Catheterization; A patch shaped like an umbrella is closed (like a closed umbrella) • Surgical Repair (Primer or pericardial patch)
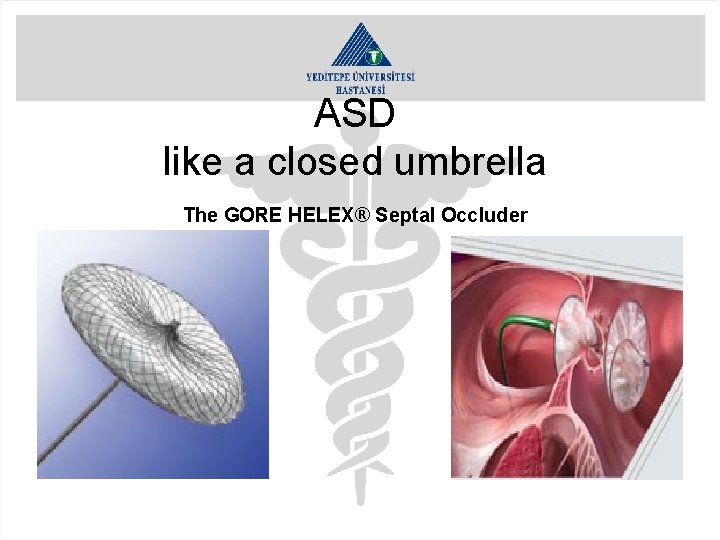
ASD like a closed umbrella The GORE HELEX® Septal Occluder
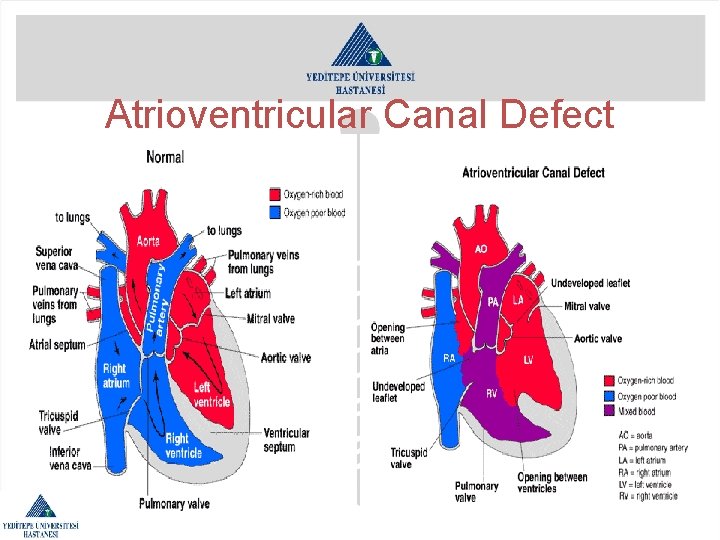
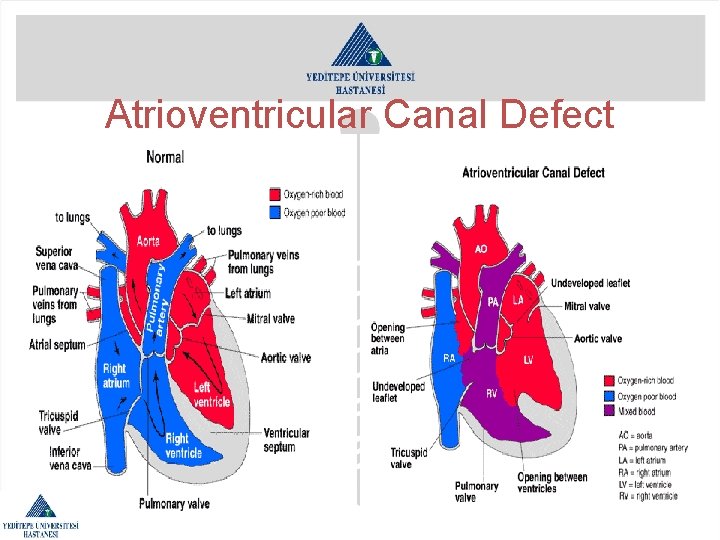
Atrioventricular Canal Defect
Atrioventricular Canal Defect • An atrial septal defect • A ventricular septal defect • Abnormalities of the mitral or tricuspid valves • First eight weeks of fetal development • one-third of all children born with AV canal also have Down syndrome.

Atrioventricular Canal Defect Symptoms may include: • fatigue • sweating • pale skin • cool skin • rapid breathing • heavy breathing • rapid heart rate • congested breathing • disinterest in feeding, or tiring while feeding • poor weight gain
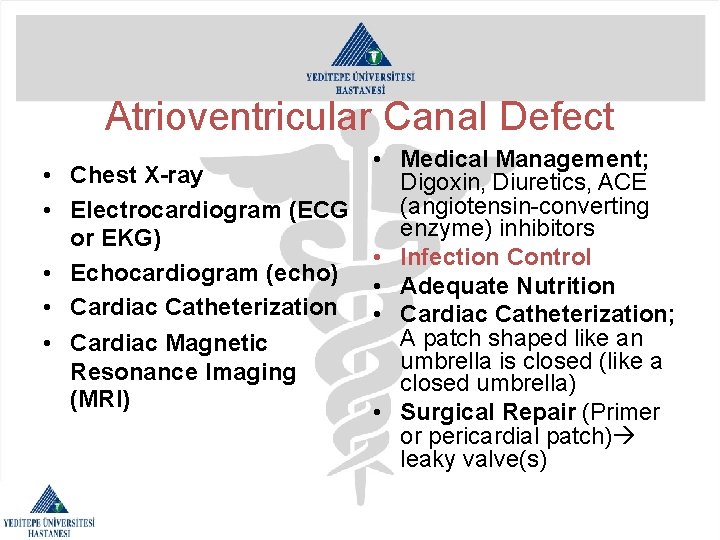
Atrioventricular Canal Defect • • • Medical Management; Chest X-ray Digoxin, Diuretics, ACE (angiotensin-converting Electrocardiogram (ECG enzyme) inhibitors or EKG) • Infection Control Echocardiogram (echo) • Adequate Nutrition Cardiac Catheterization • Cardiac Catheterization; A patch shaped like an Cardiac Magnetic umbrella is closed (like a Resonance Imaging closed umbrella) (MRI) • Surgical Repair (Primer or pericardial patch) leaky valve(s)
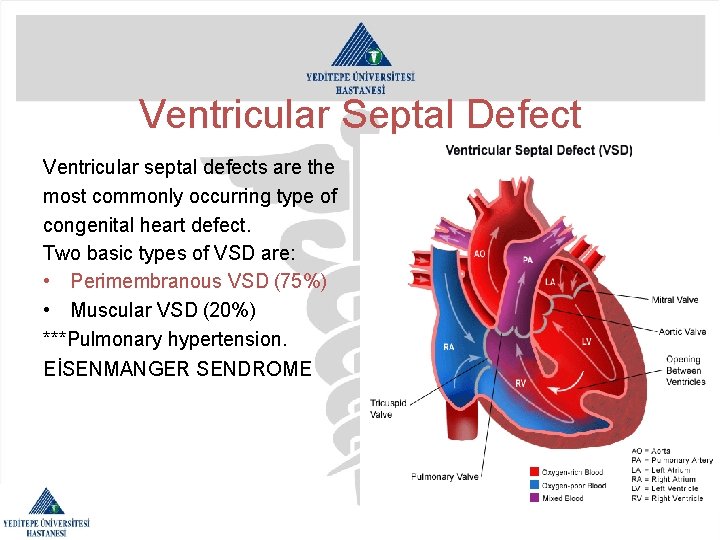
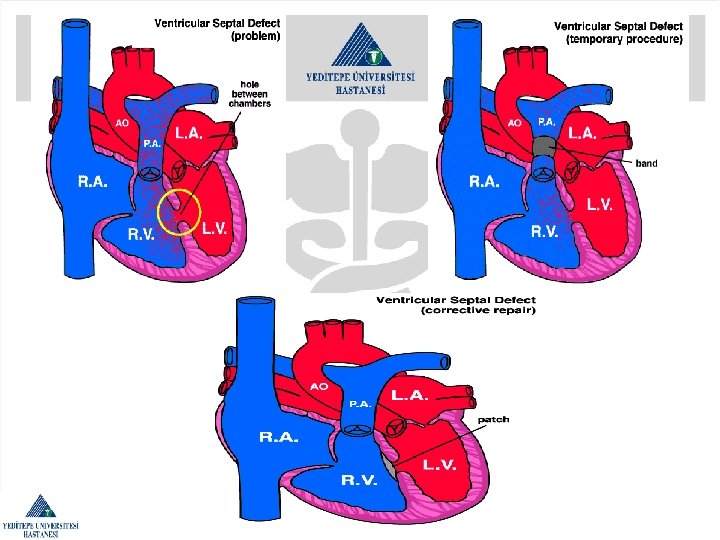
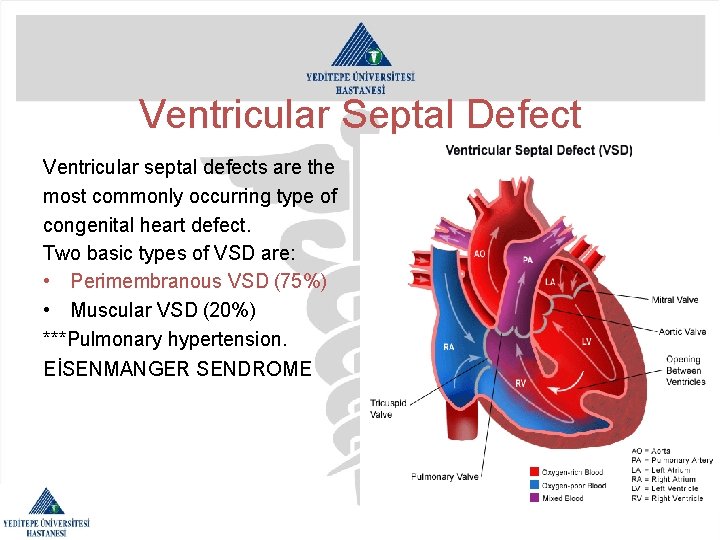
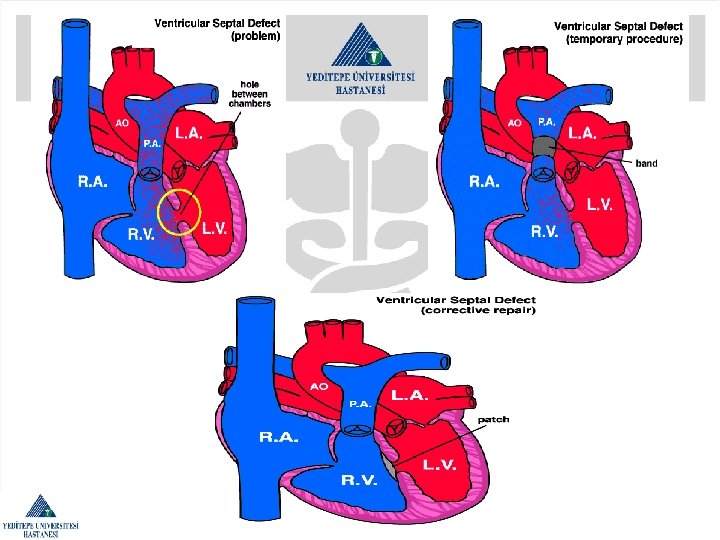
Ventricular Septal Defect Ventricular septal defects are the most commonly occurring type of congenital heart defect. Two basic types of VSD are: • Perimembranous VSD (75%) • Muscular VSD (20%) ***Pulmonary hypertension. EİSENMANGER SENDROME
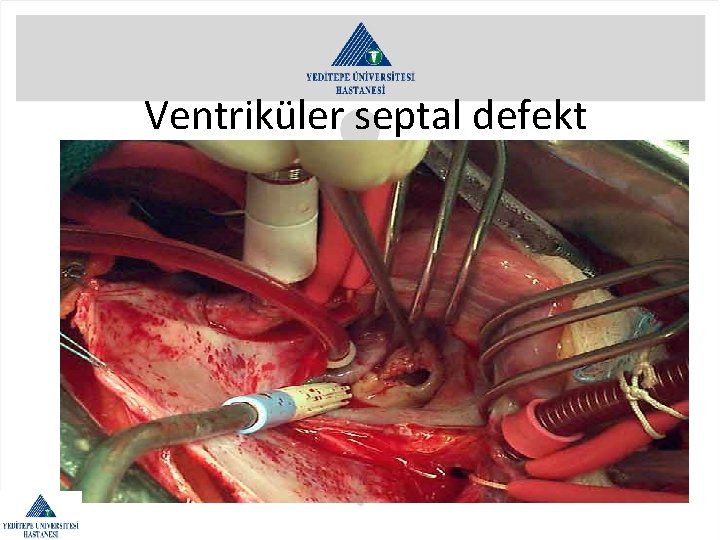
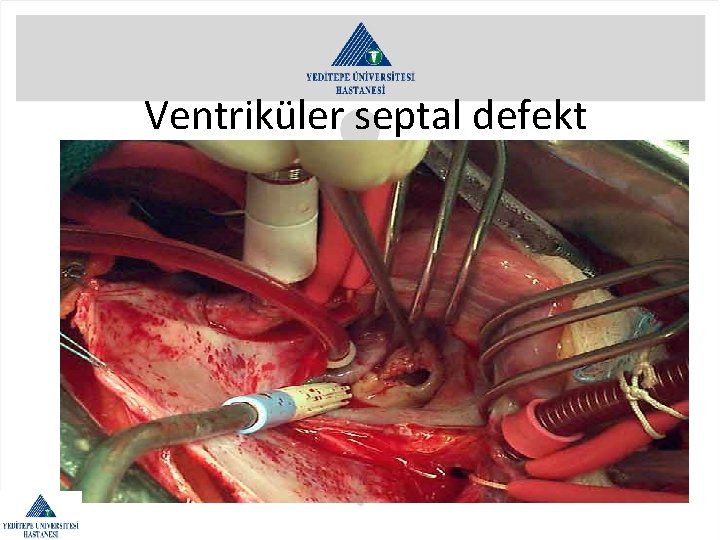
Ventriküler septal defekt
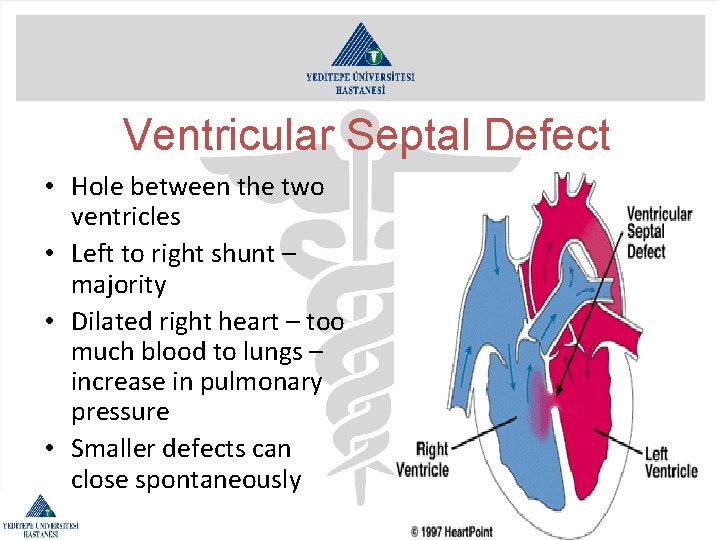
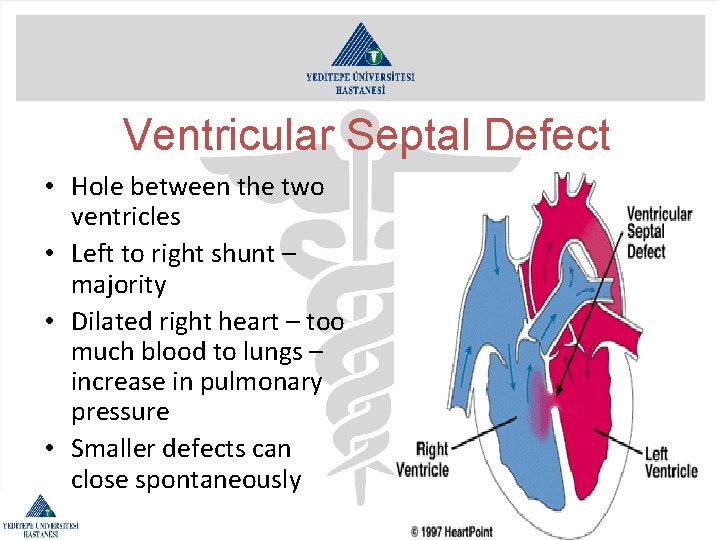
Ventricular Septal Defect • Hole between the two ventricles • Left to right shunt – majority • Dilated right heart – too much blood to lungs – increase in pulmonary pressure • Smaller defects can close spontaneously
Ventricular Septal Defect • • Perimembranous VSD – most common Muscular VSD – can be multiple Apical VSD – usually small Variable in size
Ventricular Septal Defect • Surgical – CP bypass • Catheter lab – Amplatzer if suitable • Residual defects
Ventricular Septal Defect Symptoms may include: • fatigue • sweating • rapid breathing • heavy breathing • congested breathing • disinterest in feeding, or tiring while feeding • poor weight gain
Ventricular Septal Defect • Chest X-ray • Electrocardiogram (ECG or EKG) • Echocardiogram (echo) • Cardiac Catheterization • Cardiac Magnetic Resonance Imaging (MRI) • Medical Management; Digoxin, Diuretics, ACE (angiotensin-converting enzyme) inhibitors • Infection Control • Adequate Nutrition • Cardiac Catheterization(septal occluder closes) • Surgical Repair (usually through the right atrium, patch of Dacron cloth or a patch of thin leather-like material called pericardium)
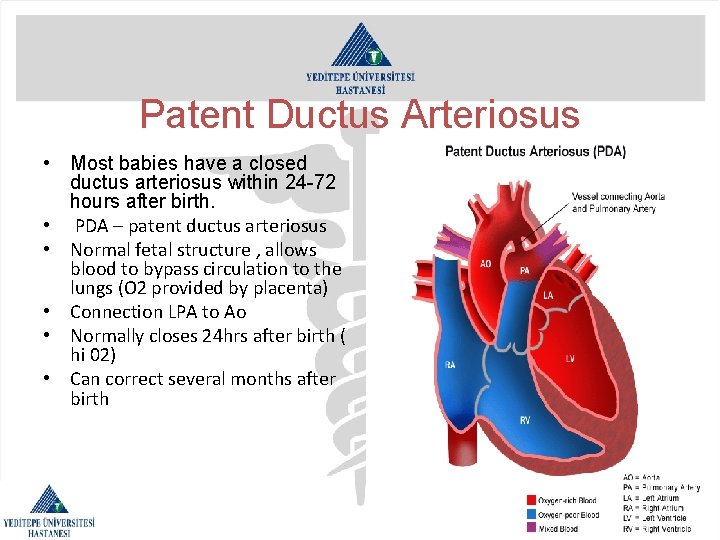
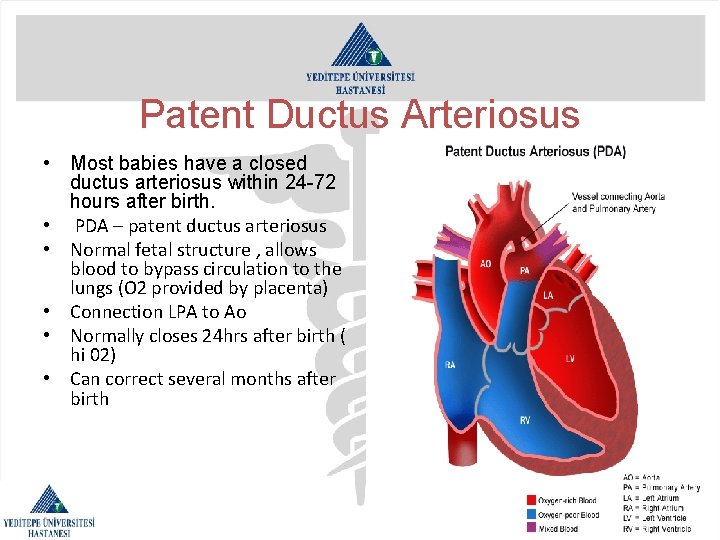
Patent Ductus Arteriosus • Most babies have a closed ductus arteriosus within 24 -72 hours after birth. • PDA – patent ductus arteriosus • Normal fetal structure , allows blood to bypass circulation to the lungs (O 2 provided by placenta) • Connection LPA to Ao • Normally closes 24 hrs after birth ( hi 02) • Can correct several months after birth
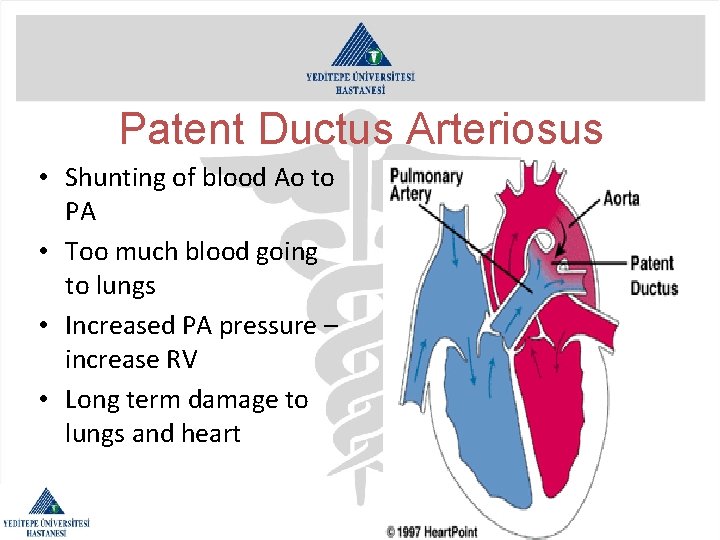
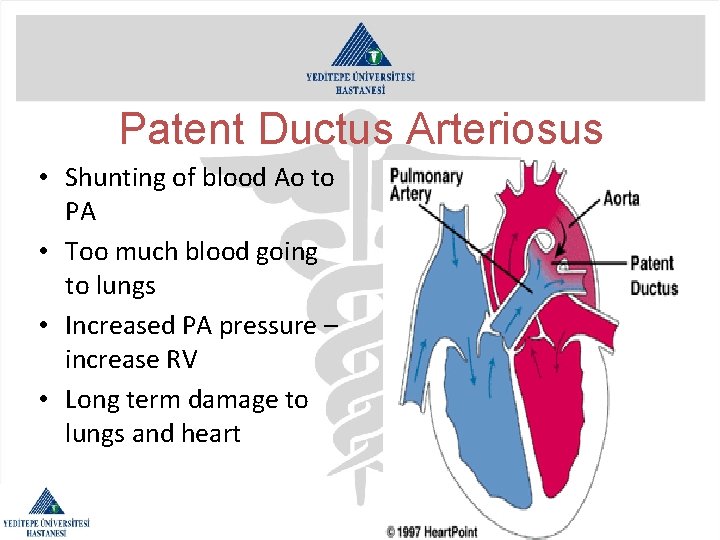
Patent Ductus Arteriosus • Shunting of blood Ao to PA • Too much blood going to lungs • Increased PA pressure – increase RV • Long term damage to lungs and heart
Patent Ductus Arteriosus • • Drug treatment to induce closure Cath lab – amplatzer or coil Surgery – ligation With associated severe CHD beneficial to remain patent
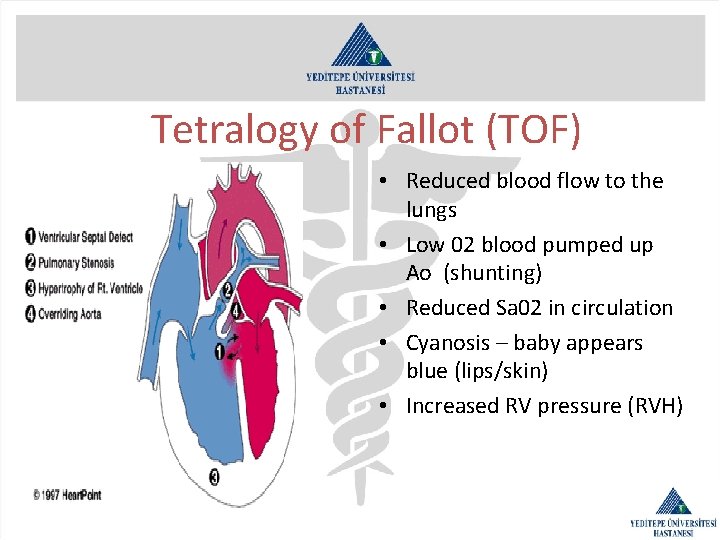
Tetralogy of Fallot (TOF) • • • Four related defects: Pulmonary stenosis ( obstuction PV/RVOT) VSD Overriding Aorta ( large AV ) Right ventricular hypertrophy (RVH) Secondary – asd /
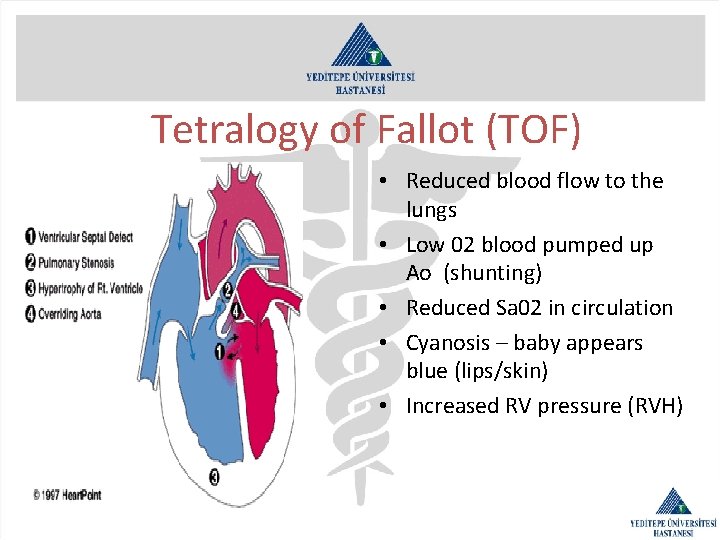
Tetralogy of Fallot (TOF) • Reduced blood flow to the lungs • Low 02 blood pumped up Ao (shunting) • Reduced Sa 02 in circulation • Cyanosis – baby appears blue (lips/skin) • Increased RV pressure (RVH)

Tetralogy of Fallot (TOF) • Diagnosed in first few weeks of life – loud murmur/cyanosis • PDA closes – symptons increase • Rapid breathing • Tet spell – sudden increase in pulm resistance /decrease Sa 02 /more blue/squat • Increasing 02 breathed – little effect • Echo ? Cath –assess PA’s

Tetralogy of Fallot (TOF) Drugs – increase pulm blood flow/Sa 02 Surgical repair dependant on Pt condition Complete repair at 6 months. Elective Palliative op – BT shunt. LSCA to PA VSD dacron patch. PS cut away obstuction and patch RVOT • Very successful op – pulm problems in later life. ? Residual VSD. • • •
Transposition of the Great Vessels Pulmonary arteries supplied by left ventricle Aorta by right ventricle Not compatable with life Immediate survival dependant on shunt from left heart to right heart • 25% have VSD. 33% abnormal coronaries • •

Transposition of the Great Vessels • Diagnosed in first few days of life • Cyanosis. Low sa 02. Rapid breathing. • PDA closes. Symptons worsen. • 02 treatment does not improve pt
Transposition of the Great Vessels Drug (prostin) maintain PDA Cath lab/echo for atrial septostomy(palliative) Requires surgery within weeks Mustard/Senning – ventricular failure/arrythmias • Switch operation • •
Transposition of the Great Vessels • Division of Ao and PA just above heart • Reconnect to correct ventricle • Coronaries disconnected and reimplanted onto new Ao (difficult) • Close ASD and VSD if present • Excellent results – PA problems in later life

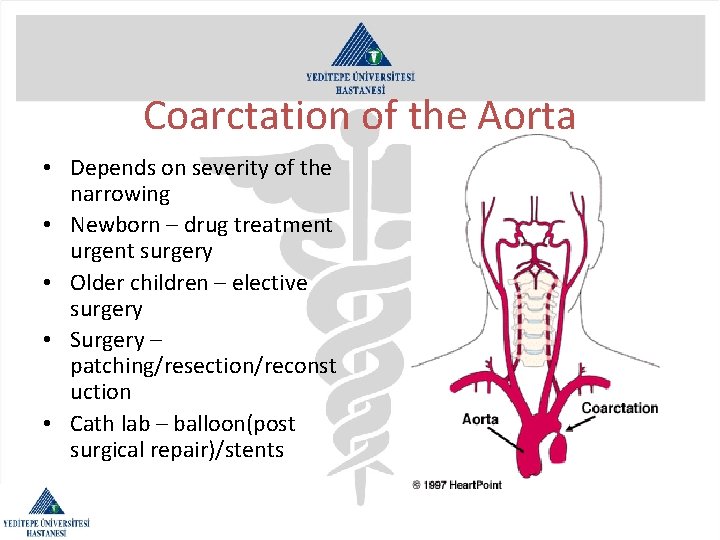
Coarctation of the Aorta • Narrowing of the Dao – juxta ductal • Often associated with other CHD-e. g. bicusp AV, VSD • LVH /congestive heart failure • Severe coarct require immediate treatment • Weak femoral pulses – reduced blood flow to lower limbs
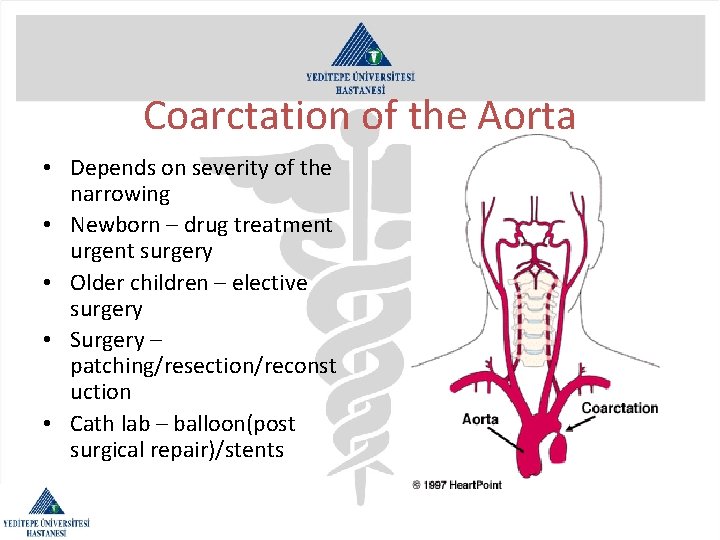
Coarctation of the Aorta • Depends on severity of the narrowing • Newborn – drug treatment urgent surgery • Older children – elective surgery • Surgery – patching/resection/reconst uction • Cath lab – balloon(post surgical repair)/stents
Coarctation of the Aorta • • Damage to lower organs during surgery Recoarctation – highest risk in newborn Hypertension – even post repair Importance of cardiology follow up especially if AV bicusp
 Structural variation
Structural variation Eray sevingil bilici
Eray sevingil bilici Oktay eray
Oktay eray Eray çil
Eray çil Dromotrop nedir
Dromotrop nedir Dr oktay eray
Dr oktay eray Adrenal kriz acilci
Adrenal kriz acilci Oktay aktolun
Oktay aktolun Mhrs bursa
Mhrs bursa Tidal volüm
Tidal volüm Birikimsel zedelenme hastalıkları
Birikimsel zedelenme hastalıkları Tr reticulospinalis
Tr reticulospinalis Primer beslenme hastalıkları
Primer beslenme hastalıkları Bademde zamklanma
Bademde zamklanma Frontotemporal
Frontotemporal Bistopeni
Bistopeni Dinamik mutasyon hastalıkları
Dinamik mutasyon hastalıkları Meslek hastalıkları
Meslek hastalıkları Kimyasal kaynaklı meslek hastalıkları
Kimyasal kaynaklı meslek hastalıkları çimento yanığı
çimento yanığı Substansia grisea
Substansia grisea Yeni yaşam okulu formatör
Yeni yaşam okulu formatör Niyazi cenk sayın
Niyazi cenk sayın Cenk uygur pronunciation
Cenk uygur pronunciation Cenk adıgüzel
Cenk adıgüzel Cenk canal
Cenk canal Avolüsyon
Avolüsyon Prof dr cenk akbostancı
Prof dr cenk akbostancı Ekg yerleştirme
Ekg yerleştirme Kalp atımlarının atardamara yaptığı basınç
Kalp atımlarının atardamara yaptığı basınç Santral periferik siyanoz
Santral periferik siyanoz Karotis manevrası yapmak
Karotis manevrası yapmak Platolu aksiyon potansiyeli nedir
Platolu aksiyon potansiyeli nedir Pulmoner trunkus genişlemesi
Pulmoner trunkus genişlemesi Opqrst değerlendirme
Opqrst değerlendirme Kalp dinleme odakları
Kalp dinleme odakları Miyokardit troponin
Miyokardit troponin Gördü ki bir avcı dam kurmuş
Gördü ki bir avcı dam kurmuş Ilk yardım abc si
Ilk yardım abc si Kalp
Kalp Skmen
Skmen Raller sesi
Raller sesi S
S Midklavikular
Midklavikular Sinus coronarius nereye dökülür
Sinus coronarius nereye dökülür Yaşa göre nabız değerleri tablosu pdf
Yaşa göre nabız değerleri tablosu pdf Beck triadi
Beck triadi Kalp masajı nasıl yapılır
Kalp masajı nasıl yapılır Kalp oskültasyon odakları
Kalp oskültasyon odakları Kalp nerededir resimli
Kalp nerededir resimli Menderes kıldıran
Menderes kıldıran Kalp atımlarının atardamara yaptığı basınç
Kalp atımlarının atardamara yaptığı basınç Mezokardiyak odak
Mezokardiyak odak