KNH 411 1 Intake Measured in kilojoules k










- Slides: 48
KNH 411 1
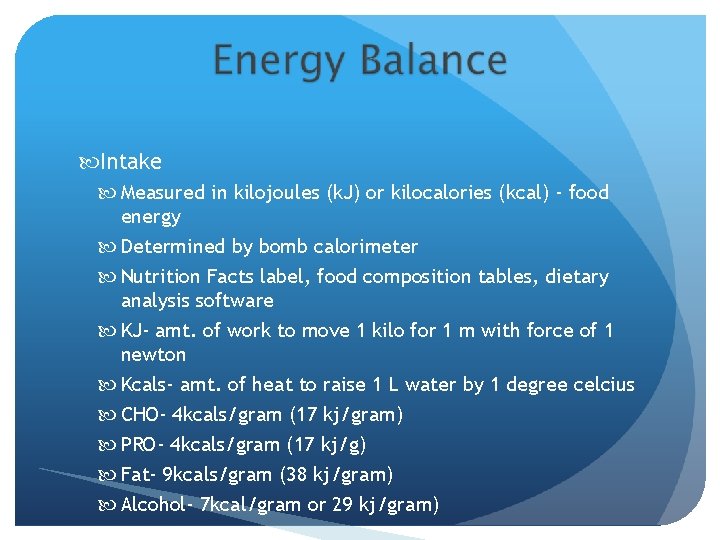
Intake Measured in kilojoules (k. J) or kilocalories (kcal) - food energy Determined by bomb calorimeter Nutrition Facts label, food composition tables, dietary analysis software KJ- amt. of work to move 1 kilo for 1 m with force of 1 newton Kcals- amt. of heat to raise 1 L water by 1 degree celcius CHO- 4 kcals/gram (17 kj/gram) PRO- 4 kcals/gram (17 kj/g) Fat- 9 kcals/gram (38 kj/gram) Alcohol- 7 kcal/gram or 29 kj/gram)

24 -Hour Energy Expenditure (EE) Resting energy expenditure (REE) - 60 to 75% - Amt. of energy needed for heart, lungs, brain, liver and kidneys to function Thermic effect of food Physical activity - Most variable - About 23%
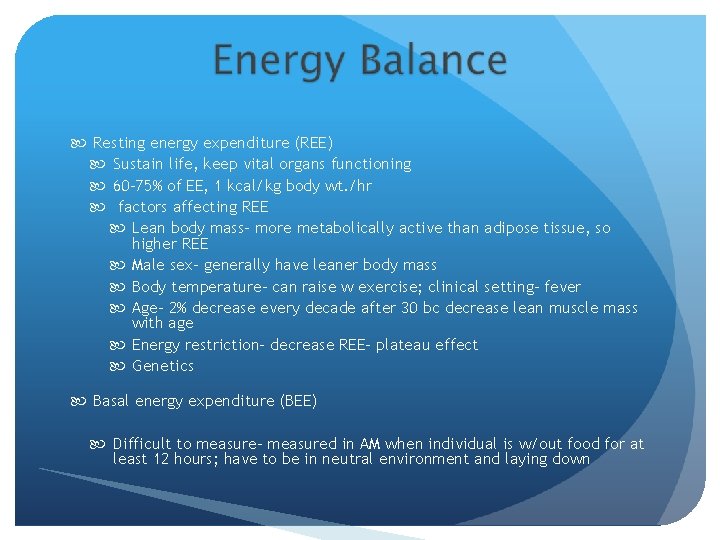
Resting energy expenditure (REE) Sustain life, keep vital organs functioning 60 -75% of EE, 1 kcal/kg body wt. /hr factors affecting REE Lean body mass- more metabolically active than adipose tissue, so higher REE Male sex- generally have leaner body mass Body temperature- can raise w exercise; clinical setting- fever Age- 2% decrease every decade after 30 bc decrease lean muscle mass with age Energy restriction- decrease REE- plateau effect Genetics Basal energy expenditure (BEE) Difficult to measure- measured in AM when individual is w/out food for at least 12 hours; have to be in neutral environment and laying down
Thermic effect of food (TEF) Measured for several hours postprandial Digest, absorb, metabolize, store, and eliminate nutrients 10% of EE Specific action of food another name for TEF Large amt. of food raises TEF Fat has lowest, PRO highest Peaks 1 hr after food and can last 4 to 6 hours
Physical Activity EE Most variable 20 -25% of EE Influenced by body weight, number of muscle groups used, intensity, duration and frequency of activity
Methods Equations- should account for gender, age, weight, stature, and PA Indirect calorimetry- more accurate, used in ICU setting w/ critically ill patients Doubly-labeled water: research facilities Direct calorimetry
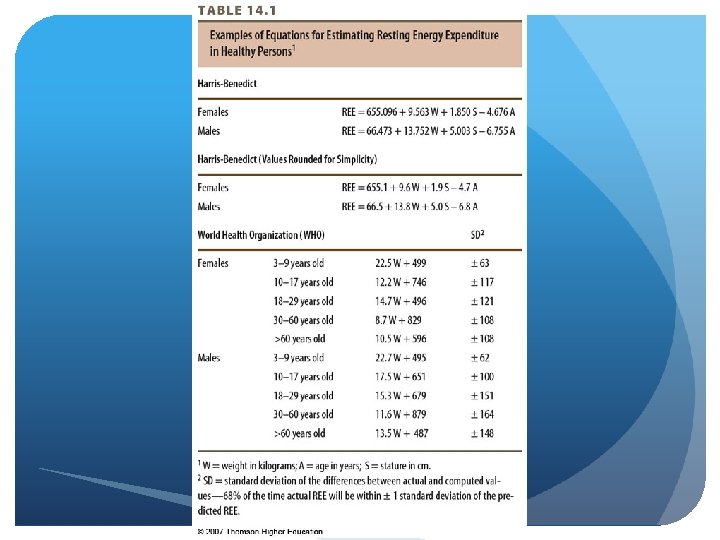
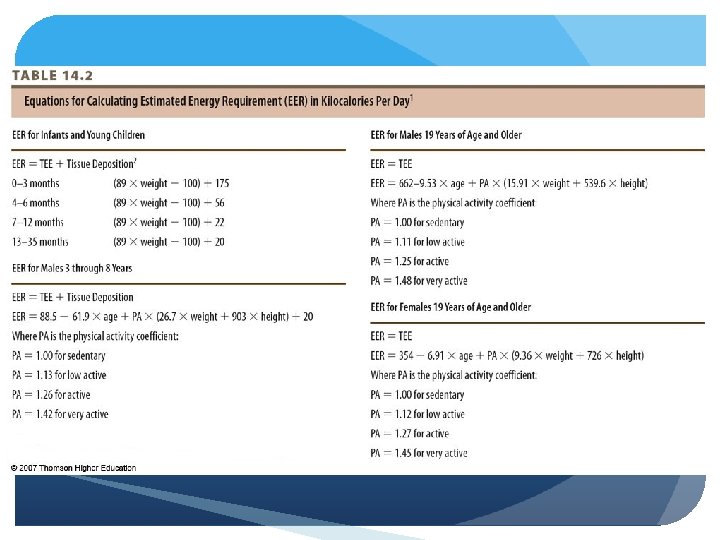
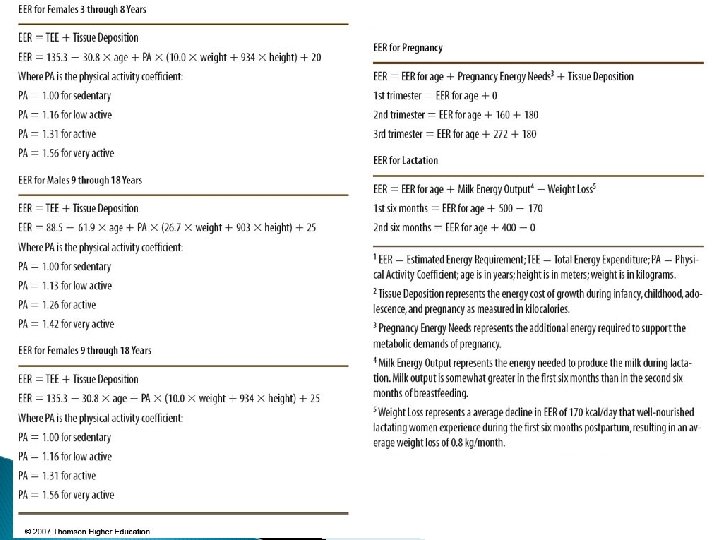
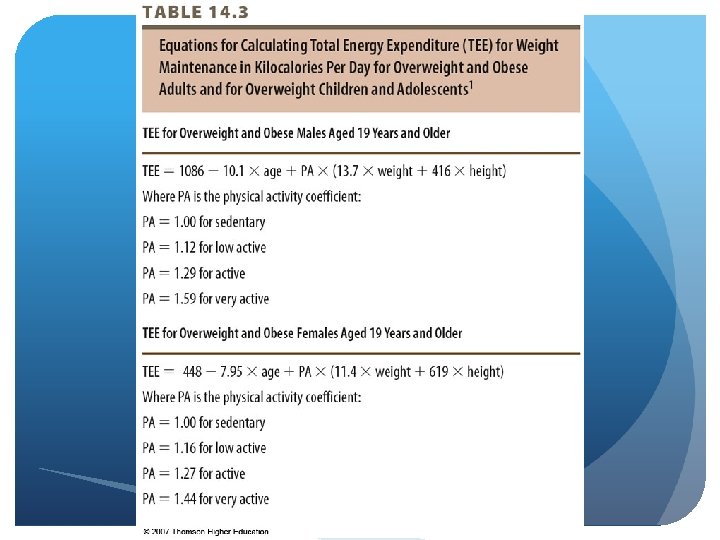
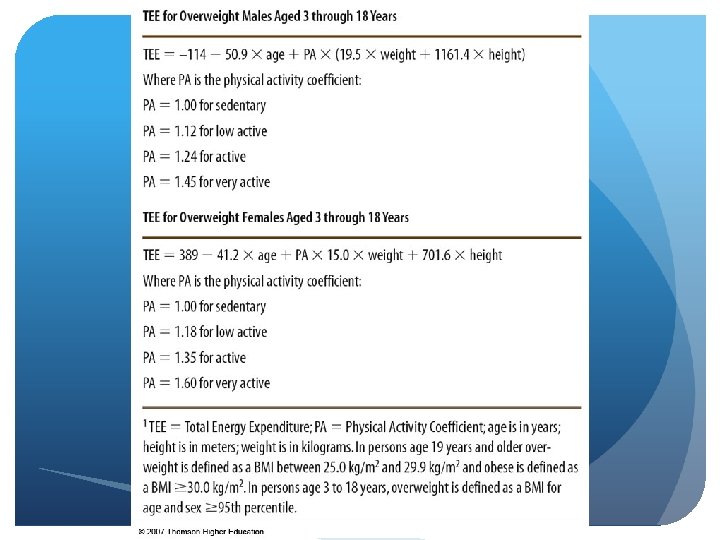
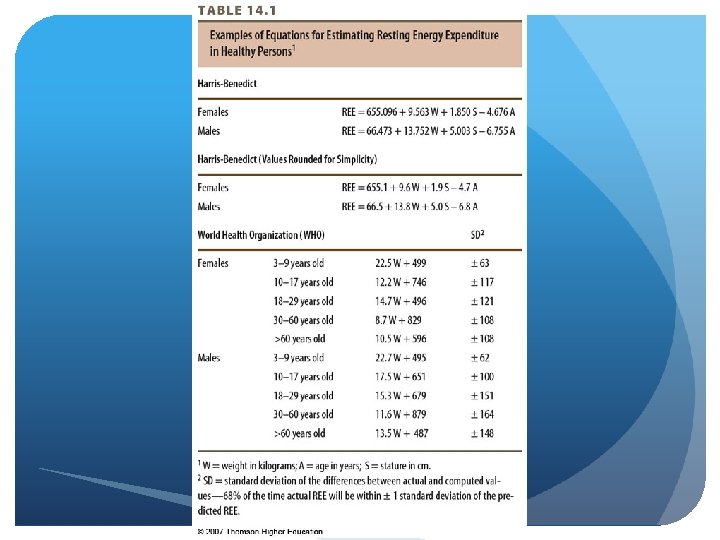
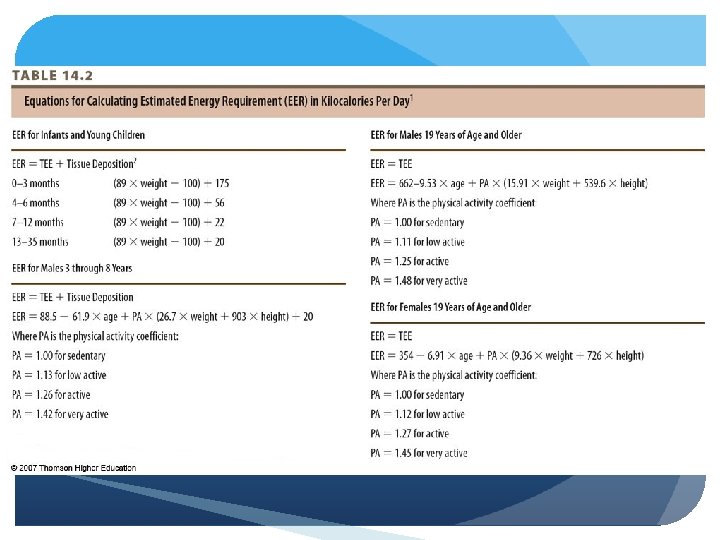
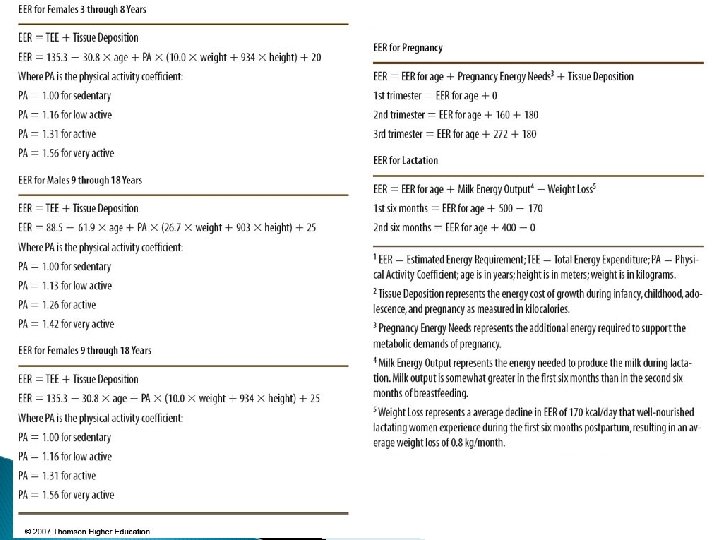
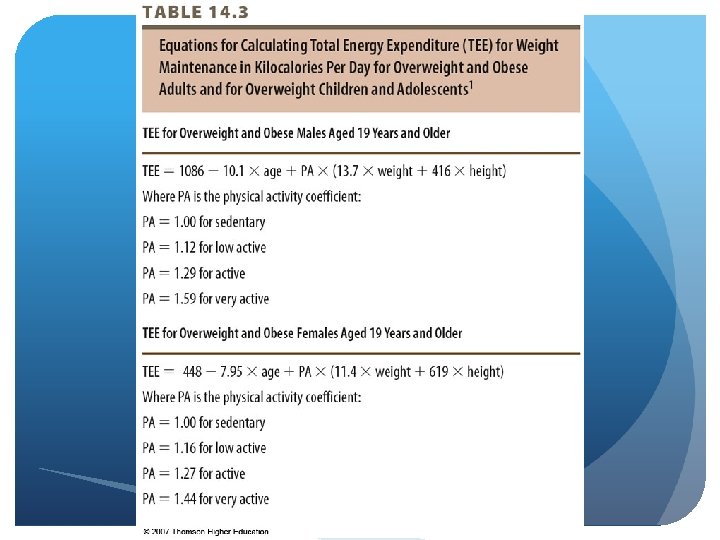
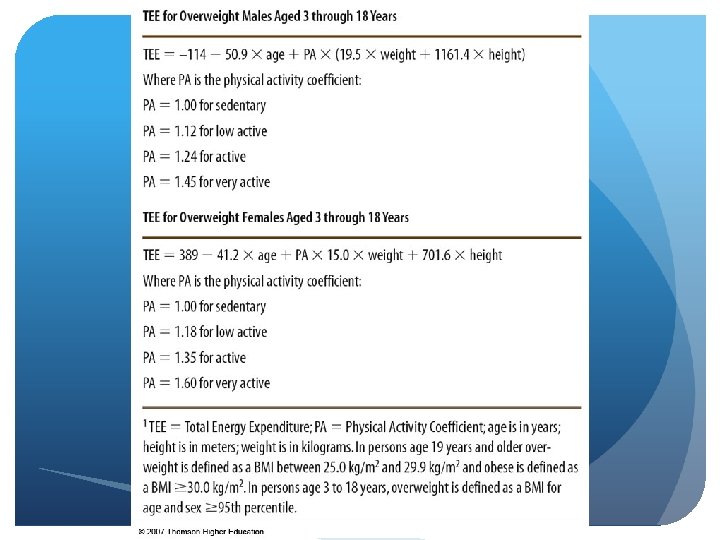
Equations for estimating EE Harris-Benedict- indirect cal. WHO- 1980 s, not stature addressed IOM DRI – estimated energy requirement (EER) Includes physical activity (PA) coefficient Separate calculations for overweight adults and overweight children and adolescents – based on BMI
© 2007 Thomson - Wadsworth
© 2007 Thomson - Wadsworth
© 2007 Thomson - Wadsworth
© 2007 Thomson - Wadsworth
Indirect Calorimetry Metabolic research or critically ill patients Measures inspired and expired air by minute ventilation EE proportional to oxygen consumption and carbon dioxide production Most commonly used method for ICU settings - More accurate than formulas Harris-benefit/mifflin st. jeor - Measured body energy expenditure
Doubly Labeled Water “Gold standard” 2 stable isotope forms of water Rate at which isotopes disappear is measured in urine over 2 -week period More difficult/complex Used in research Accurate within 1 to 2%
Direct Calorimetry Chamber which measures heat expired through evaporation, convection, and radiation Rarely available, even more complex
Interaction of nervous and endocrine systems Orexigenic- stimulates appetite, assoc. with anti-psych drugs Anorexigenic- stimuli that’s stressed related; anti-anxiety; causes weight loss (adderall) Adaptive thermogenesis- TEF, anything regulating response to change temp. of diet
Appetite stimulated by hypothalamus Secretions of pancreatic and GI hormones Increase and decrease appetite and food intake Pradar-Willi syndrome
Hormones affecting appetite & food intake Insulin- high levels mean decreased appetite Glucagon- during fasting beta cells this is released Amylin- decreases appetite Cholecystokinin (CCK)- hormone decreasing appetite Glucagon like peptide-1 - “ “ “ Peptide YY- “ “ “ Ghrelin- stimulates appetite; preytor willi
Adipocyte – fat cell; mostly TG Storage site - 90% energy reserves is TG Other functions- infants: maintaining body temp White fat (WAT) storage of TG from diet fat, synthesized from CHO and Fat vs. brown fat (BAT), found in the fetus, infants and children= 6%, body temp/insulation; decreases with age and will convert to white fat Lipogenesis- need to store excessive energy

© 2007 Thomson - Wadsworth

Adiponectin- stimulate/signals body to store fat Leptin- signaling ample fat and body doesn’t need to store more Hypertrophy- occurs when someone is overweight and adipose tissue mass that increases and accumulates more TG; energy intake exceeds expenditure hyperplasia of cells- adipose cells increase in number of cells can no longer these cells, can only shrink them; occurs w/ extreme obesity “Adiposity rebound” - From ages 1 to 6, there was a change in body % fat to leaner muscle mass, but now we are seeing that % body fat is beginning to increase at this age up to 8
“Two compartment model” – fat vs. fat-free mass Adipose vs. lean tissue Different ways to measure: 1. skin-fold measurements, 2. underwater weighing, 3. biochemical impendents Use of height and weight – BMI commonly used to assess obesity Does not directly measure fatness Clinical judgment should be used
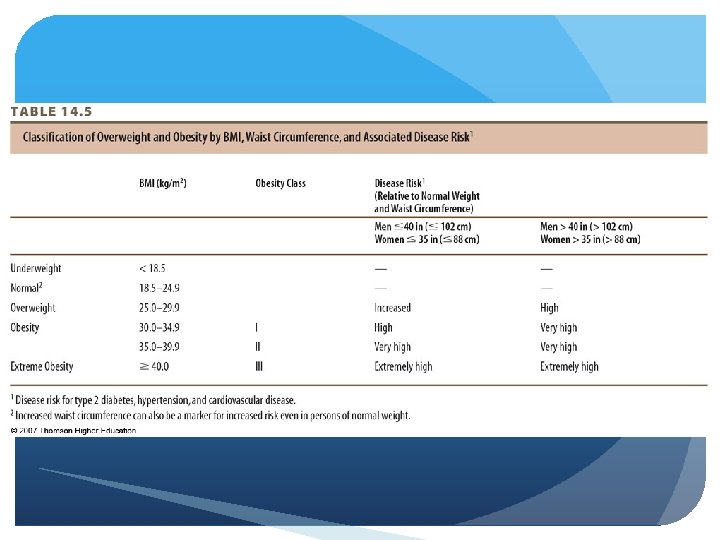
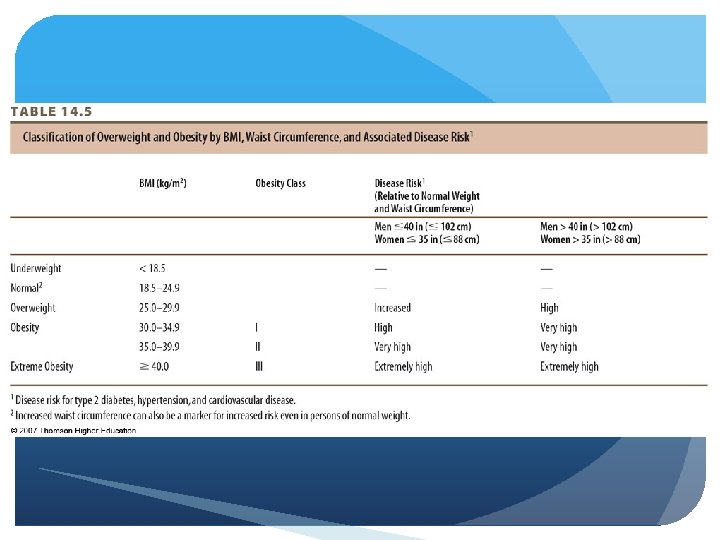
Body Mass Index (BMI) Obese ≥ 30 calculation and classifications BMI percentiles CDC growth charts Pediatric population ≥ 95%th percentile = obesity ≥ 85%th percentile = overweight
Important predictor of health status Abdominal/central body fat Apple, android- associated with obesity risk and other health concerns related to diabetes and CVD Lower body fat Hips and thighs, pear, gynoid Measured by waist circumference and waist-to-hip ratio Anything greater than 1 is of concern b/c related to being unhealthy
Waist circumference Increased risk of type 2 DM, htn. , dyslipidemia, CHD, metabolic syndrome > 40 in. males, > 35 in. females – “high risk”
Waist-to-hip ratio (WHR) Waist circumference/hip circumference Disease risk increases with WHR > 0. 95 in males and >0. 8 in females Key concept: fat deep within abdomen and around intestines and liver increases disease risk
“Globesity, ” “epidemic”- concern of the decade according to WHO In the U. S. - NHANES data Significant increases Canada - 36% obese - 23% overweight Europe - 45% to 80% of population By race, ethnicity, SES, age - African american females (50% obese), African American males 30% obese

“The age of caloric anxiety” Type 2 diabetes- 2 x more prevalent in obese population High blood pressure- 3 x more prevalent in obese pop. CHD- 2 to 3 x more likely if obese Cancer- esophagus, colon, rectum, pancreas, liver, prostate Mortality- doubled with increased body weight
Chronic energy intake exceeding energy expenditure Key contributors: Medical disorders and treatment: ex- hyperthyroidism Genetics- small component Obesigenic environment- #1 contributor
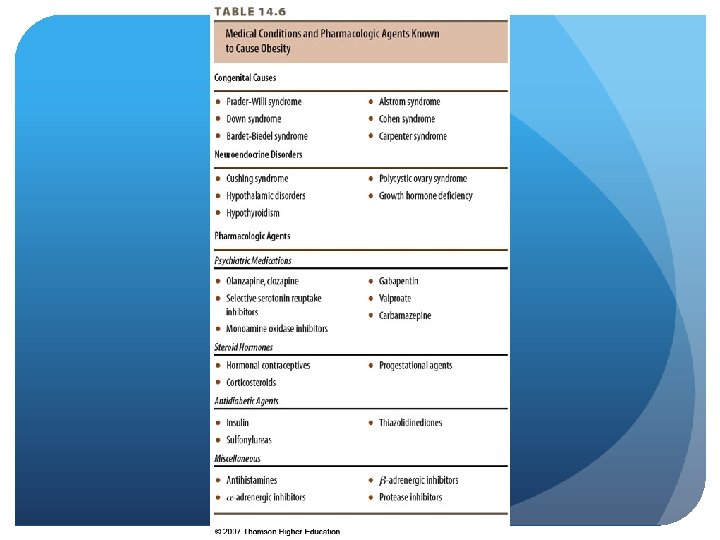
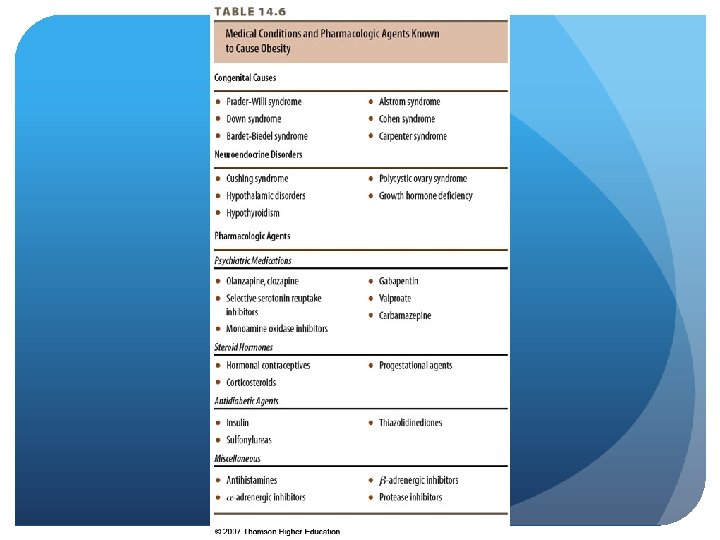
Medical disorders and treatment Cushings syndrome, hypothyroidism, Prader-Willi Pharmacological agents Smoking cessation- 20 to 30 pounds weight gain over decades Night eating syndrome- 25% calories eaten at night without even knowing it Binge eating- 10 to 25% calories eaten in one sitting
Genetics 40 -50% of BMI explained by genetics Influences taste, appetite, intake, expenditure, NEAT, storage “Set-point” theory- reasons why people may gain weight quickly Multiple genes- may cause increase intake significantly Predictive in families – parents & twins 80% of offspring with 2 obese parents 40% of offspring with 1 obese parent MZ twins more likely than DZ twins - Adopted twins: BMI correlated strongly with real parents and not adopted parents
Obesigenic environment “Toxic food environment” – convenient availability of lowcost, tasty, energy-dense foods in large portions Evidence supports low-energy-dense foods for satiety Soups, fruits, vegetables, cooked whole grains Barriers – cost and convenience


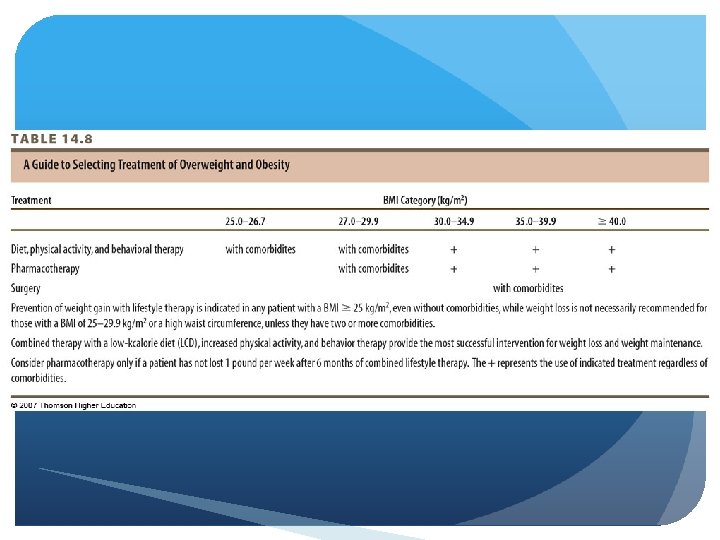
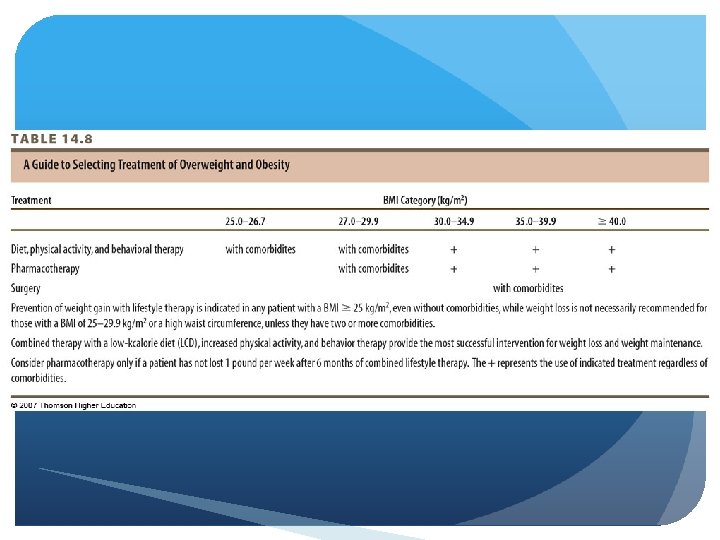
Two-step process to treat weight Assessment - BMI, waist measurements, waste-hip ratios Management NIH algorithm for treatment

© 2007 Thomson - Wadsworth

Assessment BMI & waist circumference Current chronic diseases Diet and physical activity habits Patient’s readiness to lose weight Identify and address barriers, coping skills, self-efficacy Behavioral assessment – what led them to seek weight loss
Management Use of recommended therapies Control of factors known to increase risk of morbidity Therapies include – diet, physical activity, behavioral therapy, bariatric surgery, pharmacologic treatment Lose 10% in 6 mo. (~1 to 2 pounds/week)
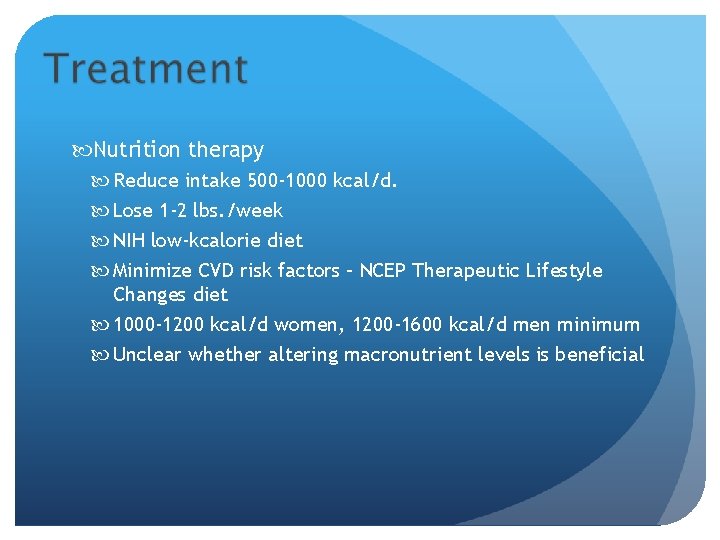
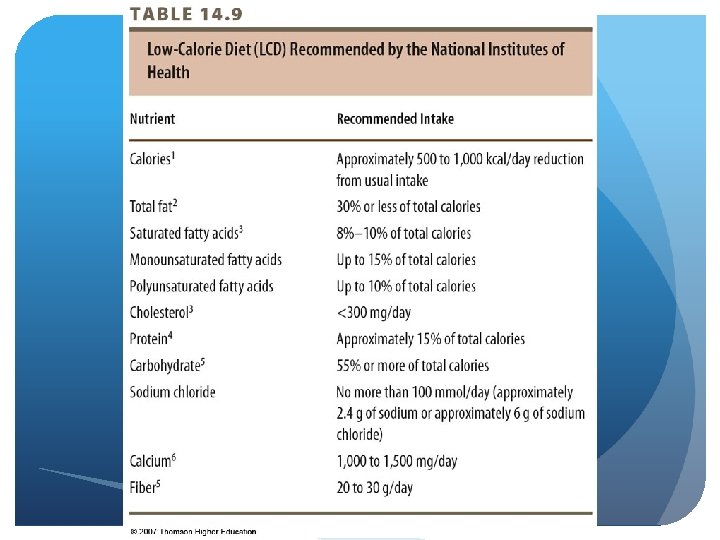
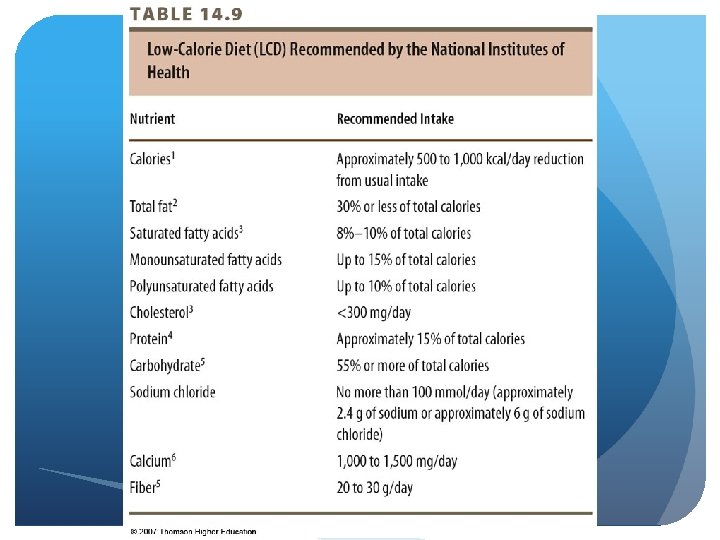
Nutrition therapy Reduce intake 500 -1000 kcal/d. Lose 1 -2 lbs. /week NIH low-kcalorie diet Minimize CVD risk factors – NCEP Therapeutic Lifestyle Changes diet 1000 -1200 kcal/d women, 1200 -1600 kcal/d men minimum Unclear whether altering macronutrient levels is beneficial
© 2007 Thomson - Wadsworth
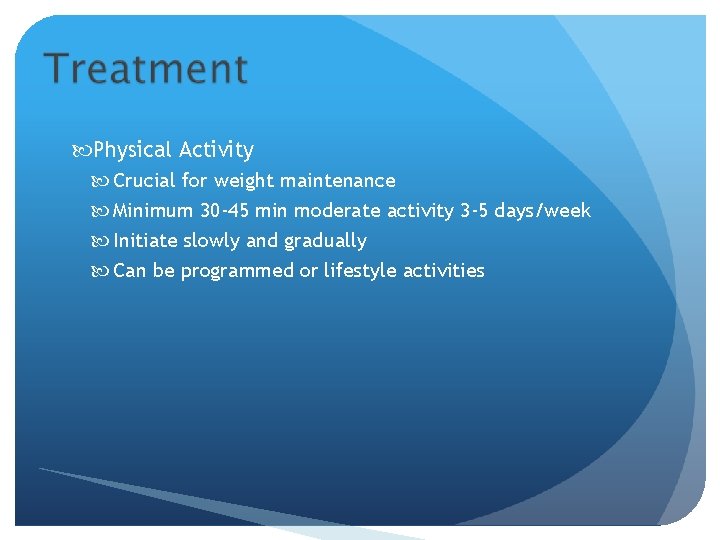
Physical Activity Crucial for weight maintenance Minimum 30 -45 min moderate activity 3 -5 days/week Initiate slowly and gradually Can be programmed or lifestyle activities

Behavior Therapy Techniques for identifying and overcoming barriers Self-monitoring Stimulus control Rewards
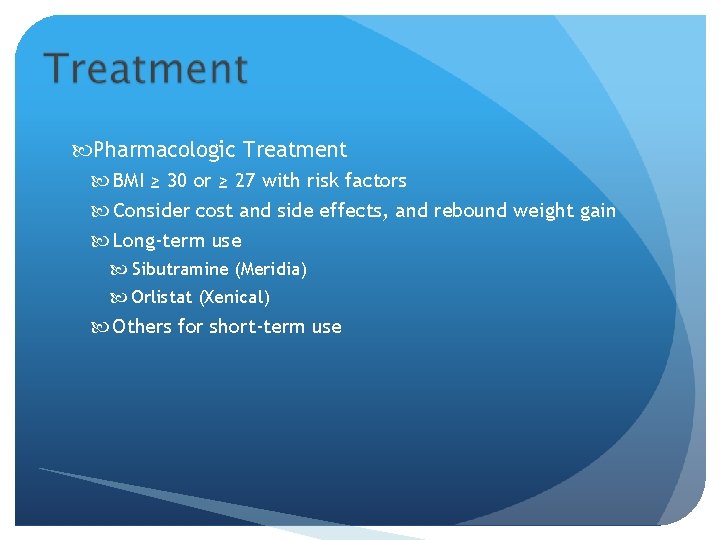
Pharmacologic Treatment BMI ≥ 30 or ≥ 27 with risk factors Consider cost and side effects, and rebound weight gain Long-term use Sibutramine (Meridia) Orlistat (Xenical) Others for short-term use
Surgery Bariatric surgery – BMI ≥ 40 or ≥ 35 with risk factors Roux-en Y gastric bypass, vertical banded gastroplasty, adjustable band gastroplasty Assess benefits vs. risks Preoperative screening & education important

 Knh
Knh How the respiratory system maintains homeostasis
How the respiratory system maintains homeostasis Knh
Knh Spanish numbers
Spanish numbers Dog breed 411
Dog breed 411 Comp
Comp Csc 411
Csc 411 Csce 411 tamu
Csce 411 tamu Ece 411
Ece 411 411 database
411 database Csce 411
Csce 411 Party 411
Party 411 Nutrition diagnosis domains
Nutrition diagnosis domains Gacollege 411
Gacollege 411 účet 411
účet 411 Csce 411
Csce 411 411 disability disclosure
411 disability disclosure Csce 411
Csce 411 Cpsc 411
Cpsc 411 411 database
411 database Csci 411
Csci 411 Csce 411
Csce 411 Ada 411
Ada 411 Nutrition 411
Nutrition 411 Cpsc 411
Cpsc 411 Rule 411
Rule 411 Cpsc 411
Cpsc 411 Opwekking 411 tekst
Opwekking 411 tekst Comp 411
Comp 411 Csce 411
Csce 411 Comp 411 unc
Comp 411 unc Unc comp 411
Unc comp 411 Seo931
Seo931 Ist 411
Ist 411 Mgt 411
Mgt 411 Csce 411
Csce 411 Ist 411
Ist 411 Ist 411
Ist 411 Cmsc submit server
Cmsc submit server Actuary roadmap
Actuary roadmap How are latitude and longitude measured
How are latitude and longitude measured Property that can be observed or measured.
Property that can be observed or measured. Current is measured in
Current is measured in What is valume
What is valume Quotes about measurement and improvement
Quotes about measurement and improvement Film the boy in the striped pyjamas
Film the boy in the striped pyjamas Physical quantity measured by thermometer
Physical quantity measured by thermometer Vertical angles
Vertical angles What is mass
What is mass