Kingdom Bacteria Phylum Firmicutes Class Bacilli Order Lactobacillales

Kingdom : Bacteria Phylum : Firmicutes Class : Bacilli Order : Lactobacillales Family : Streptococcaceae Genus : Streptococcus
Introduction: v Streptococci are gram positive cocci, arranged in chains. v They are a part of normal flora of humans and animals. Some of them are human pathogens v The most important of them is Streptococcus pyogenes causing pyogenic infection’s with a characteristic tendency to spread. v It is also responsible for non – suppurative lesions, acute rheumatic fever and glomerulonephritis which occur as sequale to infection.
History • Cocci in chains were first seen in erysipelas and wound infection by Billroth (1874). – Streptos meaning twisted or coiled • Ogstain (1881) – Isolated them from acute abscess. – Distinguished them from Streptococci – Established their pathogenicity by animal inoculation. • Rosenbach (1884) – Isolated cocci from human suppurative lesions. – Gave them name Streptococcus pyogenes.
Classification • • O 2 requirement. Hemolysis Nature of carbohydrate antigen on the cell wall. Protein antigen present on cell surface (Griffith typing )
O 2 requirement : – Aerobic and facultative anaerobes. – Obligate anaerobes – peptostreptococci
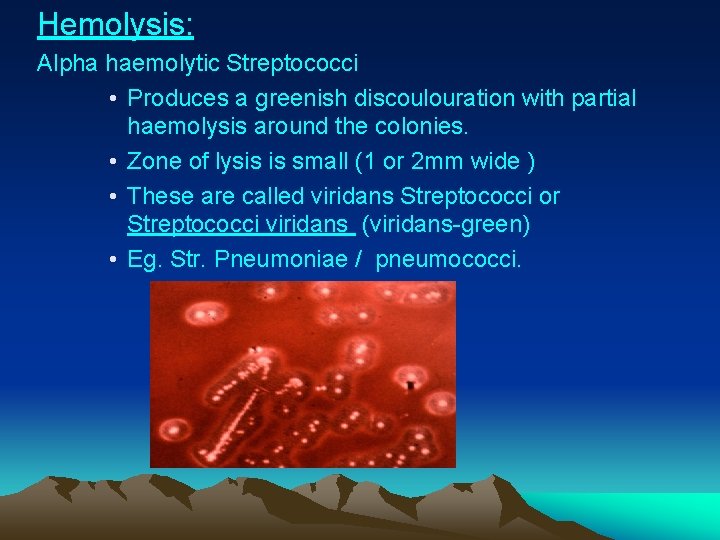
Hemolysis: Alpha haemolytic Streptococci • Produces a greenish discoulouration with partial haemolysis around the colonies. • Zone of lysis is small (1 or 2 mm wide ) • These are called viridans Streptococci or Streptococci viridans (viridans-green) • Eg. Str. Pneumoniae / pneumococci.
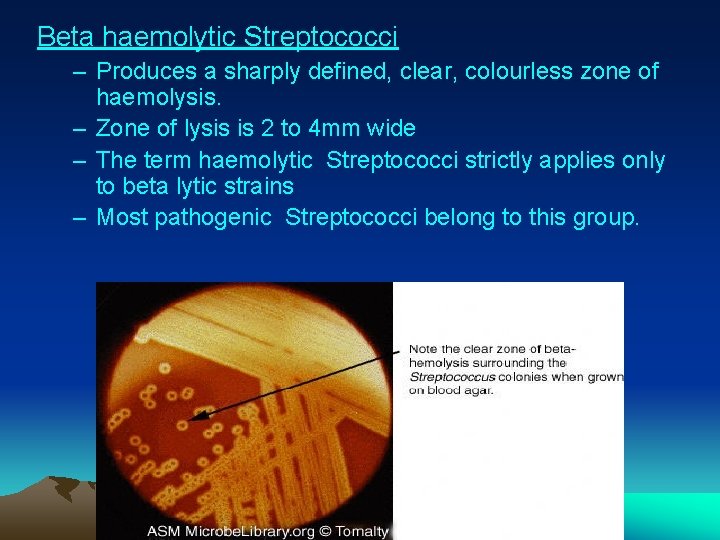
Beta haemolytic Streptococci – Produces a sharply defined, clear, colourless zone of haemolysis. – Zone of lysis is 2 to 4 mm wide – The term haemolytic Streptococci strictly applies only to beta lytic strains – Most pathogenic Streptococci belong to this group.
Gamma haemolytic Streptococci – Produces no change in medium and so are sometimes referred to as indifferent Streptococci – They include fecal Streptococci ( str. faecalis and enterococci ) – They are called the Enterococcus group
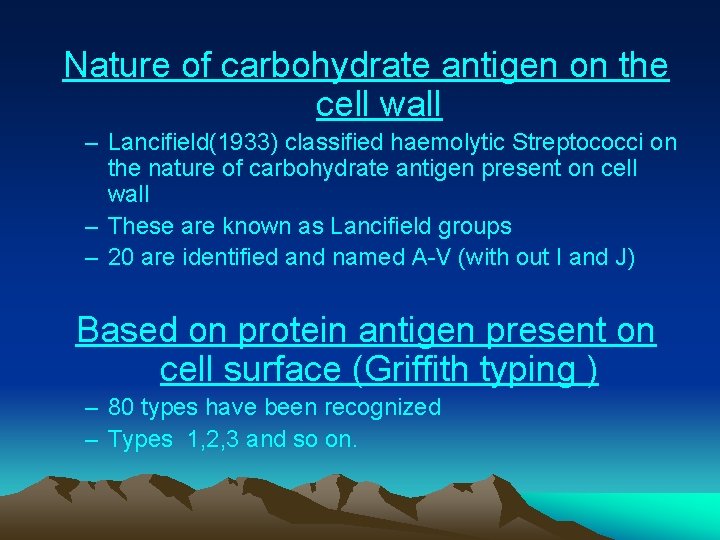
Nature of carbohydrate antigen on the cell wall – Lancifield(1933) classified haemolytic Streptococci on the nature of carbohydrate antigen present on cell wall – These are known as Lancifield groups – 20 are identified and named A-V (with out I and J) Based on protein antigen present on cell surface (Griffith typing ) – 80 types have been recognized – Types 1, 2, 3 and so on.
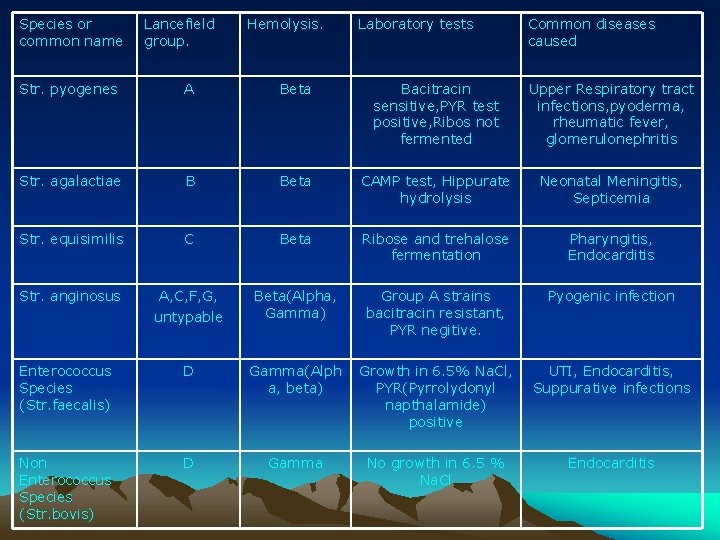
Species or common name Lancefield group. Hemolysis. Laboratory tests Common diseases caused Str. pyogenes A Beta Bacitracin sensitive, PYR test positive, Ribos not fermented Upper Respiratory tract infections, pyoderma, rheumatic fever, glomerulonephritis Str. agalactiae B Beta CAMP test, Hippurate hydrolysis Neonatal Meningitis, Septicemia Str. equisimilis C Beta Ribose and trehalose fermentation Pharyngitis, Endocarditis Str. anginosus A, C, F, G, untypable Beta(Alpha, Gamma) Group A strains bacitracin resistant, PYR negitive. Pyogenic infection Enterococcus Species (Str. faecalis) D Gamma(Alph a, beta) Growth in 6. 5% Na. Cl, PYR(Pyrrolydonyl napthalamide) positive UTI, Endocarditis, Suppurative infections Non Enterococcus Species (Str. bovis) D Gamma No growth in 6. 5 % Na. Cl Endocarditis
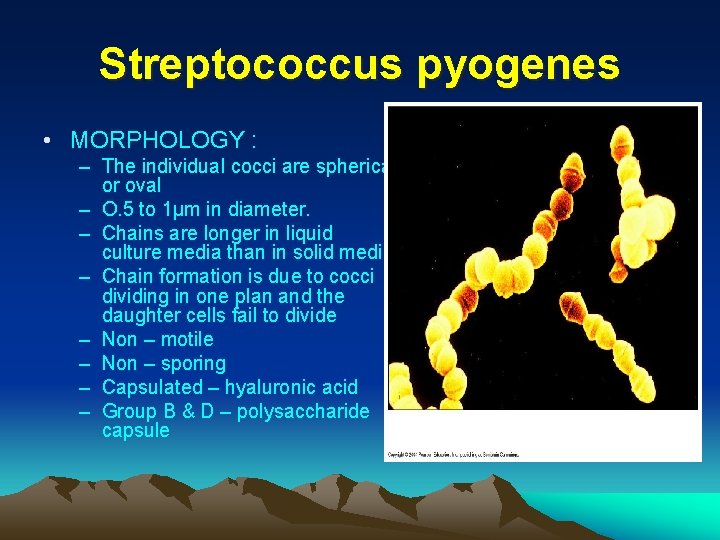
Streptococcus pyogenes • MORPHOLOGY : – The individual cocci are spherical or oval – O. 5 to 1μm in diameter. – Chains are longer in liquid culture media than in solid media. – Chain formation is due to cocci dividing in one plan and the daughter cells fail to divide – Non – motile – Non – sporing – Capsulated – hyaluronic acid – Group B & D – polysaccharide capsule
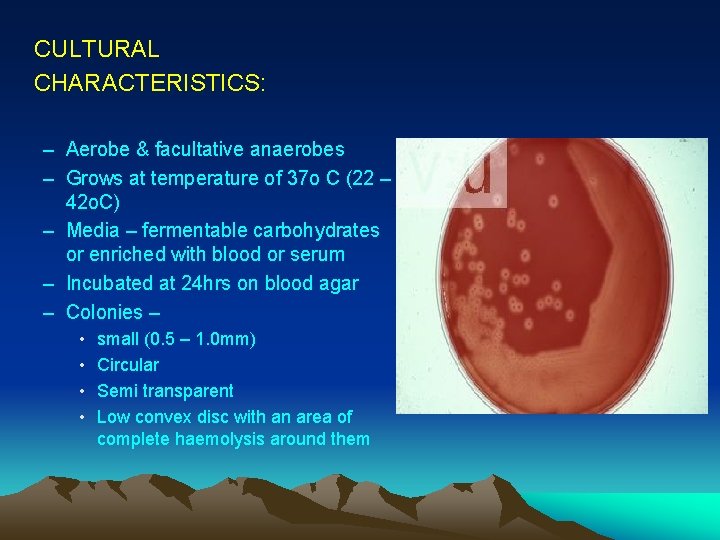
CULTURAL CHARACTERISTICS: – Aerobe & facultative anaerobes – Grows at temperature of 37 o C (22 – 42 o. C) – Media – fermentable carbohydrates or enriched with blood or serum – Incubated at 24 hrs on blood agar – Colonies – • • small (0. 5 – 1. 0 mm) Circular Semi transparent Low convex disc with an area of complete haemolysis around them
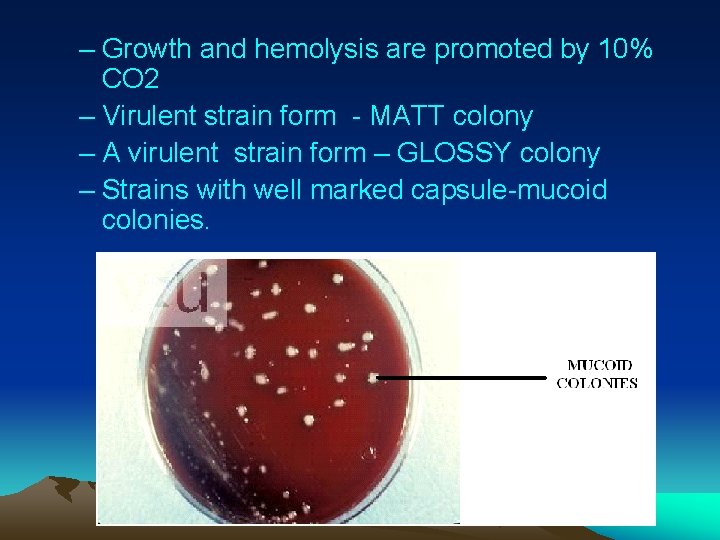
– Growth and hemolysis are promoted by 10% CO 2 – Virulent strain form - MATT colony – A virulent strain form – GLOSSY colony – Strains with well marked capsule-mucoid colonies.
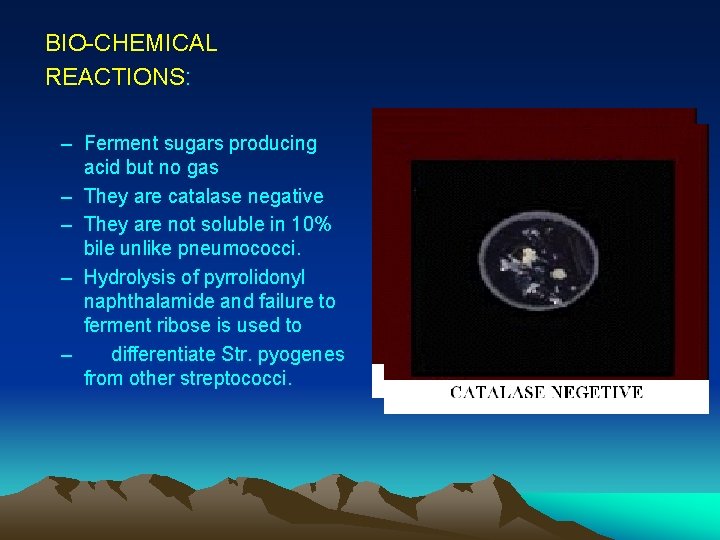
BIO-CHEMICAL REACTIONS: – Ferment sugars producing acid but no gas – They are catalase negative – They are not soluble in 10% bile unlike pneumococci. – Hydrolysis of pyrrolidonyl naphthalamide and failure to ferment ribose is used to – differentiate Str. pyogenes from other streptococci.
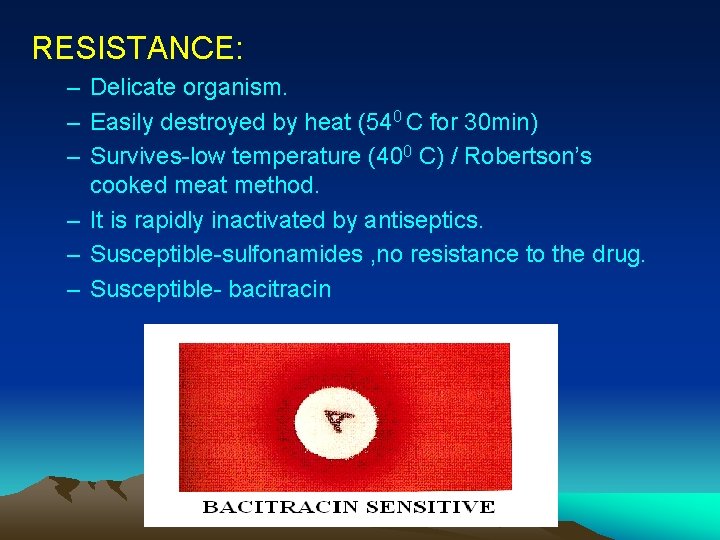
RESISTANCE: – Delicate organism. – Easily destroyed by heat (540 C for 30 min) – Survives-low temperature (400 C) / Robertson’s cooked meat method. – It is rapidly inactivated by antiseptics. – Susceptible-sulfonamides , no resistance to the drug. – Susceptible- bacitracin
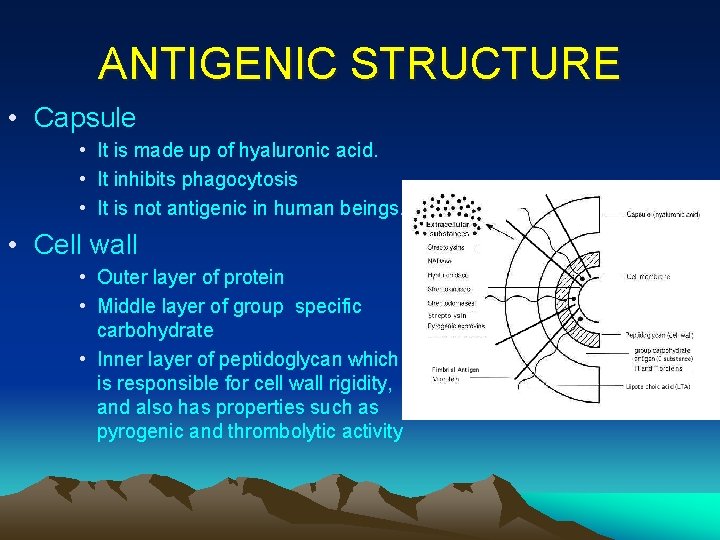
ANTIGENIC STRUCTURE • Capsule • It is made up of hyaluronic acid. • It inhibits phagocytosis • It is not antigenic in human beings. • Cell wall • Outer layer of protein • Middle layer of group specific carbohydrate • Inner layer of peptidoglycan which is responsible for cell wall rigidity, and also has properties such as pyrogenic and thrombolytic activity
PATHOGENESIS • Several protein antigens are identified on the outer part of cell wall • Surface protein M, T & R • The ‘M’ protein – It is the most important protein – It acts as a virulent factor by inhibiting phagocytosis – It is antigenic – Its antibody promotes phagocytosis of the coccus and is therefore protective – The ‘M’ protein is heat and acid stable but susceptible to tryptic digestion. – Associated with pathogenesis of acute rheumatic fever
• The ‘T’ protein – This is acid labile, trypsin resistant antigen – It may be specific but many different ‘M’ types posses the same ‘T’ antigen – Demonstrated by – slide agglutination test, using trypsin with Streptococci • The ‘R’ protein – Some types of Str. pyogenes (types 2, 3, 28 & 48) & some strains of group B, C & G contain a third antigen the ‘R’ protein • The ‘T’ & ‘R’ protein have no relation to virulence • Lipotechoic acid (L T A) – Facilitates attachment of Streptococci to fibronectin by a two way process – Antigenic but does not confer immunity
CYTOLYTIC TOXINS AND OTHER EXOENZYMES • Hemolysins – Streptolysin O • • • O 2 labile Damages mammalian cells by releasing lysosomal enzymes Cardiotoxic and leucotoxic activity It is also heat labile Contributes to virulence In its biological activity Streptolysin O resembles the O 2 labile haemolysins of cl. perfringens, cl. tetani and the pneumococcus • ASO titre - serological procedure for a retrospective diagnosis of infection with str. pyogenes • Inhibited by cholesterol.
CYTOLYTIC TOXINS AND OTHER EXOENZYMES • Streptolysin S – O 2 stable – Responsible for hemolysis seen around phosphatase, estarase, amylase, N acetyl glucosamidase, neuraminidase and other toxins or enzymes.
Pyrogenic exotoxin : (Erythrogenic Dick, Scarlatinal toxin) Intradermal injection susceptible individuals Erythematous reaction
– so named ‘erythrogenic’ – this was used to identify children susceptible to scarlet fever, a type of acute pharyngitis with extensive erythematous rash caused by the str. pyogenes strains producing this toxin • blanching of rash on local infection of covalescent serum was used as a diagnostic test for scarlet fever (Schultz Charlton reaction-1918) • streptococcal pyrogenic exotoxin (SPE) are ‘superantigens’ • ‘T’ cell mitogens which induce massive release of inflammatory cytokines causing fever, shock & tissue damage.

SCARLET FEVER
Streptokinase (Fibrinolysin): – This toxin promotes the lysis of human fibrin clots by activating a plasma precursor(plasminogen). – Biological role in breaking down the fibrin barrier around the lesions & facilitating spread of infection. – IV - Myocardial Infarction & other thromboembolic disorder.
Strepdornases DNAses: • Helps to liquefy thick pus and responsible for thin serous character of streptococcal exudates. • There are 4 antigenically distinct DNAses A, B, C & D. • B is most antigenic in human beings. Hyaluronidase: • It breaks down hyaluronic acid of the tissue. • It posses a hyaluronic acid capsule, hyaluronidase a self destructive process. • This enzyme is antigenic.
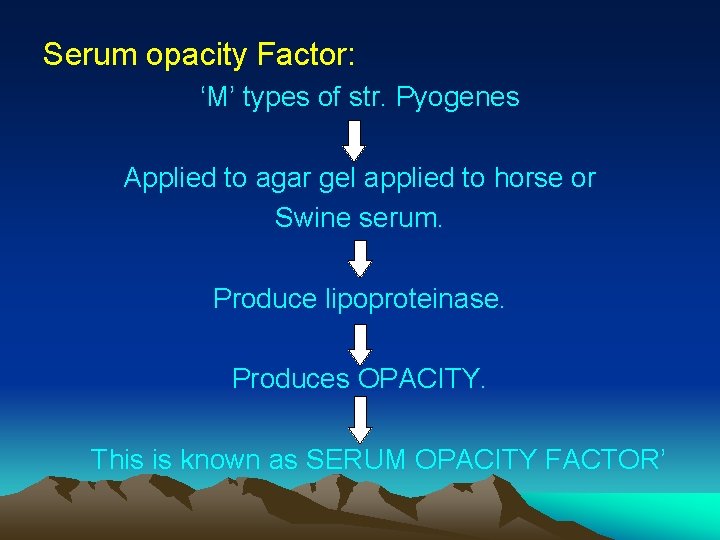
Serum opacity Factor: ‘M’ types of str. Pyogenes Applied to agar gel applied to horse or Swine serum. Produce lipoproteinase. Produces OPACITY. This is known as SERUM OPACITY FACTOR’
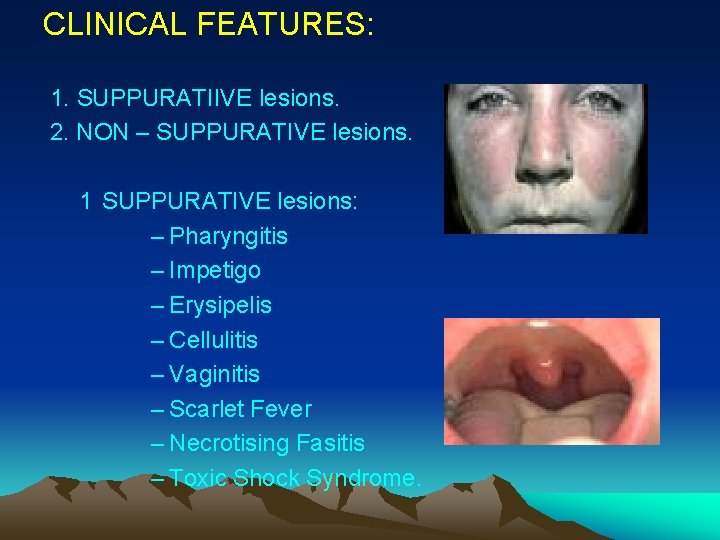
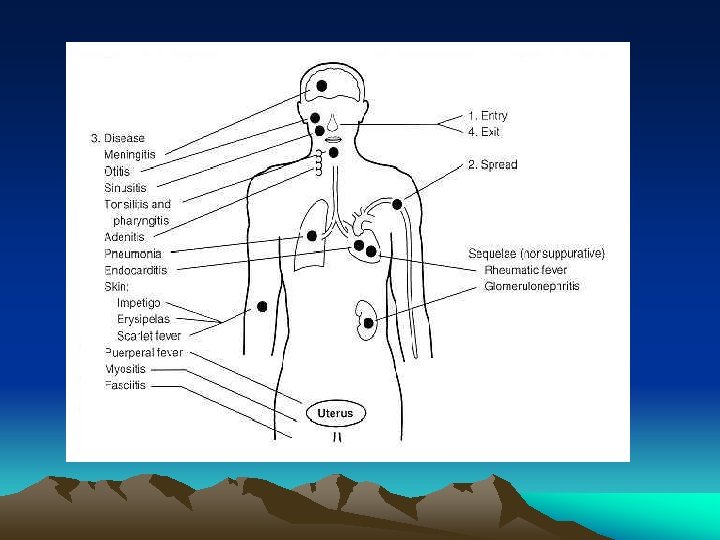
CLINICAL FEATURES: 1. SUPPURATIIVE lesions. 2. NON – SUPPURATIVE lesions. 1 SUPPURATIVE lesions: – Pharyngitis – Impetigo – Erysipelis – Cellulitis – Vaginitis – Scarlet Fever – Necrotising Fasitis – Toxic Shock Syndrome.
2 NON- SUPPURATIVE lesions: – Acute Rheumatic Fever – Acute Post Streptococcal Glomerulonephritis.
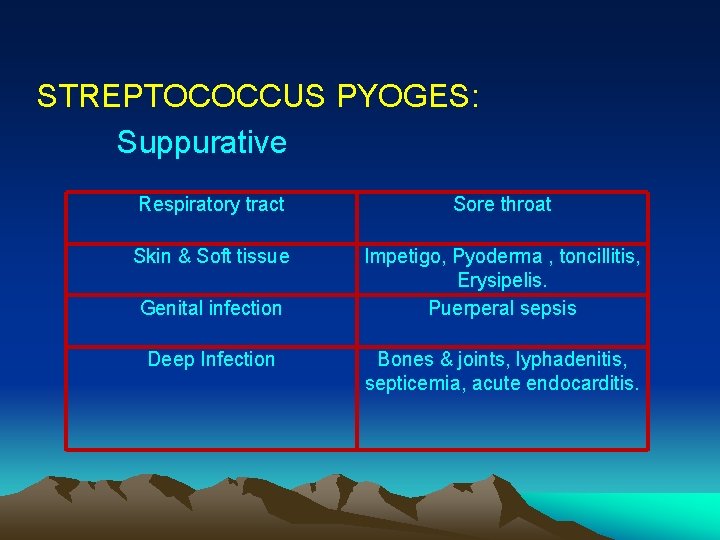
STREPTOCOCCUS PYOGES: Suppurative Respiratory tract Sore throat Skin & Soft tissue Impetigo, Pyoderma , toncillitis, Erysipelis. Puerperal sepsis Genital infection Deep Infection Bones & joints, lyphadenitis, septicemia, acute endocarditis.
Non – Suppurative: The two non – suppurative complications are; 1. Acute Rheumatic Fever. 2. Acute Post streptococcal Glomerulonephritis.
Acute Rheumatic Fever: • The essential lesion in rheumatic fever is carditis including connective tissue degeneration of heart valves & inflammation myocardial lesions characterized by Aschoff nodules. • Rheumatic fever follows persistant or repeated str. throat infection with a strong antibody response. • Lesions are believed to be result of hypersensitivity to some str. components.
LABORATORY DIAGNOSIS: A. Acute Suppurative Infection: 1. Smear: Examination of Gram Stained films from pus & CSF. • Presence of Gram Positive cocci in chains is indicative of str. infection.
2. Culture: Specimen is inoculated immediately • Transport media is Pikes transport media – Blood Agar containing 1 in 1, 000 crystal violet & 1 in 16, 000 Sodium azine. • Specimen is plated on blood agar & incubated at 37 o. C anaerobically (haemolysis develops better in 5 – 10 % CO 2 ) • Sheep blood agar is used for primary isolation as it inhibits haemophylus haemolyticus. • Detection is done by agar plate test using paper discs impregnated with bacitracin (1 unit/ ml). • A wide zone of inhibition is seen with str. pyogenes but not with other streptococci.
3. Antigen detection test: Test kits of ELISA & Agglutination test Demonstrate group A str. antigen. 75 -80% sensitive Throat swabs are used Commercial test kit of a nucleic acid probe based test for direct detection of Group A streptococci in throat swabs is available.
GLOMERULAR DISEASE • Glomerulus is a modified capillary network that delivers an ultra filtrate of plasma to bowman’s space • In health glomerular endothelium is also antithrombotic & antiadhesive for leucocytes & platelets, thereby preventing inappropriate vascular thrombosis & inflammation during the filtration process. • Glomerular injury results in impairment in glomerular filtration & /inappropriate appearance of plasma protein & blood cells in urine.
Pathogenicity : • Exposure of host to foreign antibodies has been implicated as the trigger for generation of nephritogenic autoantibodies – glomerulonephritis • Mechanisms: 1. A foreign antigen whose structure resembles that of a host glomerular antigen Stimulates production of autoantibodies.
Cross react with intrinsic glomerular antigen . MOLECULAR MIMICRY. • 2. Foreign antigen expression of MHC class II molecules on glomerular cells Present autoantigens to T lymphocytes Generate Autoimmune response
• 3. Triggers polyclonal activation of B lymphocytes, which generates nephritogenic antibodies. Clinical features: Ø Common in children between 3 -7 years. Ø Fever , malaise, headache, hematuria, oliguria, oedema , hypertention. On examination: fluid overload , puffinessof face, hypertention(diastolic pressure-110 mm. HG or higher.
• Investigations: – Urine - cloudy – GFR - low – ESR - high – ASO titre - high – Serum complement – low.
RHEUMATIC FEVER • Pathogenesis: • Direct infection by group A str, • Toxic effect of str. extracellular products on host tissue • Abnormal or dysfuntional immune response. • Clinical features: ü Jones criteria- major & minor criteria are as follows v. Major-Fever - Polyarthritis/Polyarthralgia - Carditis - Chorea - Subcutaneous nodules - Erythema marginatum v. Minor-Epistaxis, pneumonitis, weakness, erythemanodosum
• Laboratory-Diagnosis: § § ASO titre- increases Streptozyme test Antiheart antibodies detected Throat culture • Treatment: • 1. 2 millions – Benzathine penicillin (every 4 weeks. ) • 250 mg BD – penicillin. • 1 g daily - sulfadiazine.
B. Non – Suppurative complications: ü In rheumatic fever & glomerulonephritis could be diagnosed by demonstrating high levels of str. toxins ü Usual test is antistreptolysin O (ASO) titration. ASO titre > 200 = prior str. infection High level = rheumatic fever. Low level = glomerulonepritis ü Antideoxyribonuclease B (anti- DNAse) estimation is also common and titres > 300 is significant. ü Anti DNAase B and antihyaluronidase tests are very useful for retrospective diagnosis of streptococcus pyoderma , for which ASO- less value
• The streptozyme test – a passive slide haemagglutination test using erythrocytes sensitized with a crude preparation of extra cellular antigen of streptococci is a convenient , sensitive and specific screening test. PROPHYLAXIS : • Indication - prevention of rheumatic fever - administration of penicillin in children, with signs of rheumatic fever. • Antibiotic prophylaxis is not useful for glomerulonephritis – this complication follows a single str. infections and re infections do not occur
TREATMENT: – β-haemolytic group A streptococci are sensitive to penicillin G –sensitive to erythromycin – Patients allergic to penicillin –erythromycin or cephalexin used. – Strains resistant to erythromycin are present. – Tetracyclins and sulfonamides are not recommended – Antimicrobial drugs have effect on established glomerulonephritis and rheumatic fever.
GROUP – B STREPTOCOCCI • These are important pathogens of cattle producing bovine mastitis (str. agalactiae) • It is the most common cause of neonatal meningitis in the neonates. • Other diseases – Arthritis , conjunctivitis , respiratory infection , peritonitis. • In adult –puerperal infection. • Identification –ability to hydrolyse CAMP(Christie, Atkins & Munch – Peterson). PYR - Negative
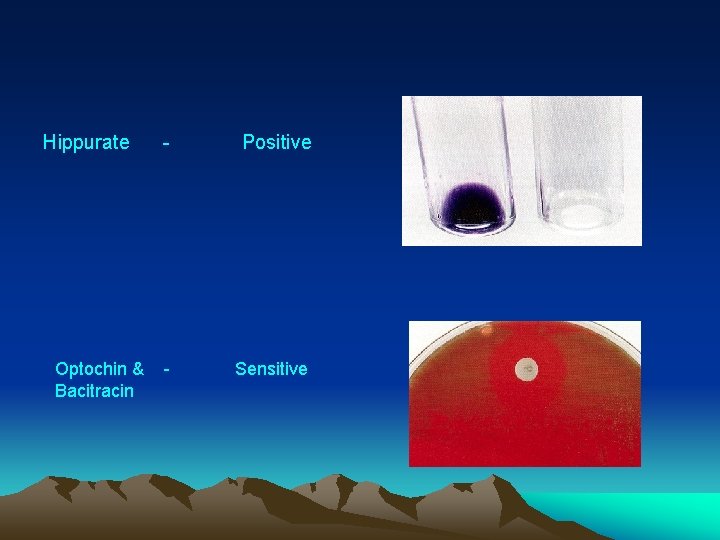
Hippurate - Positive Optochin & - Sensitive Bacitracin
• Human pathogenic Group B strains possess a polysaccharide capsule which appears to confer virulence. • GROUP ‘C’ – Predominantly animal pathogens. • GROUP ‘H’ & ‘K’ – Infective endocarditis.
ENTEROCOCCAL / NON – ENTEROCOCCAL GROUP ‘D’ STREPTOCOCCI They are again grouped into two groups: 1) The enterococcus group – classified – saperate genus called enterococcus – different species Eg. . E. Faecalis, E. faecium & E. durans. 2) The Non – enterococcal group, Eg. . Str. bovis, Str. equines.
CHARECTERISTICS : Enterococcus group: – Appereance – pairs of oval cocci. – Arrangement – in pairs, rt. angles to each others – They grow in presence of 40% bile, 6. 5% Na. Cl at PH of 9. 6 at 450 C & in 0. 1% Methylene blue milk – Mac – Conkeys medium – deep pink colonies. – Heat resistant – surviving 600 C for 30 min. – Non – hemolytic though some may show α & β hemolysis. – E. faecalis identified – biological grounds – ferments mannitol, sucrose, sorbitol. – Tellurite blood agar – black colonies.
Non – Enterococcal group: • It includes Str. bovis & Str. equisinus. • Susceptible to penicillin – penicillin is a choice of drug for Str. bovis infection. • Inhibited by 6. 5% Na. Cl / bile.
CLINICAL FEATURES: Enterococcal infection : • Enterococci - intestinal tract and saliva. • Elderly & debilitated / in whom mucosal or epithelial barrier have been distrupted. • Patients with antibiotic treatment or undergone instrumentation of urinary tract – urinary tract infections are common. • Patients with intravascular catheters – nosocomial bacteraemia. • Bacterial endocarditis – on native & prosthetic Valves. • Also cause infection of biliary tract, septicemia & intra alveolar abscess. “This group is resistant to Penicillin”
Non – Enterococcal infection : • Str. bovis endocarditis is often associated with neoplasms of G. I. T. most frequently a colon carcinoma or a polyp “This group is susceptible to Penicillin”
TREATMENT: • Not reliably killed by penicillin or ampicillin alone. Combined theraphy for enterococcal endocarditis & meningitis. • The regimen is penicillin = 3 – 4 million units every 4 hours. Ampicillin = 2 g every 4 hours. Gentamycin = 1 mg /Kg every 8 hours for patient with normal renal function • Some enterococci are vancomycin resistant
Vancomycin resistant enterococci : • First reported – late 1980’s. • Three major vancomycin resistant phenotypes – Van ‘A’, Van ‘B’ & Van ‘C’. • Van ‘A’ – high level of resistance to vancomycin & to teicoplanin (related glycopeptide antibiotic) • Van ‘B’ & ‘C’ – Resistant to vancomycin but susceptible to teicoplanin although teicoplanin resistance – during treatment in van ‘B’ strains.
Regimen : Ciprofloxacin + rifampin + gentamicin Ampicillin + vancomycin & cloramphenicol / tetracycline Newer agents are – quinupristin / dalfopristin & linezolid. .
QUESTIONS • Main Question: Classify str. & describe pathogenesis & lab diag of RF. • Short Note: 1. 2. 3. 4. 5. Str. viridans. Non-suppurative complications of str. pyogenes. Hemolysis. Post str. sequale. Lab diagnosis of RF. • Short Ans: 1. ASO test. 2. Camp test 3. Enzyme produced by str. 4. Two Non-Suppurative post str. sequale
REFERENCES • ANANTHANARAYAN & PANIKER’S. • LIPPINCOTS • HARRISON • INTERNET

Thank U…….
- Slides: 60