Kick Start Your Quality Improvement Project Learn how




















- Slides: 93

‘Kick Start Your Quality Improvement Project’ Learn how to undertake and deliver quality improvement projects Training for Registrars Wednesday 9 th December 2015 & Wednesday 9 th March 2016 1
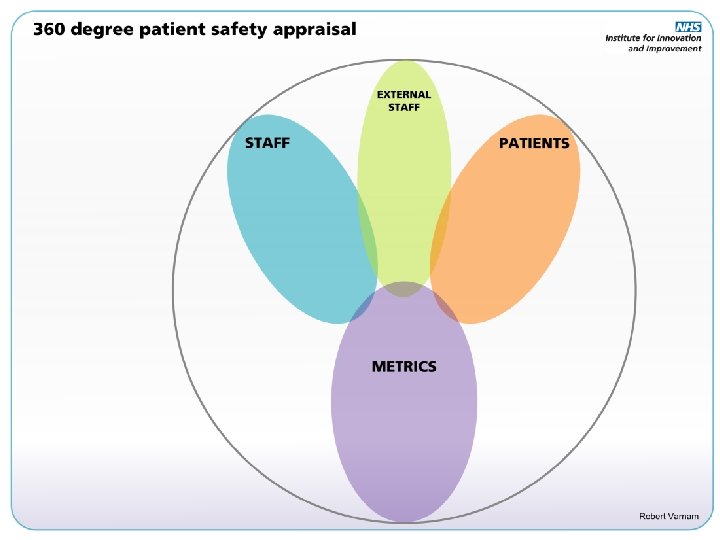
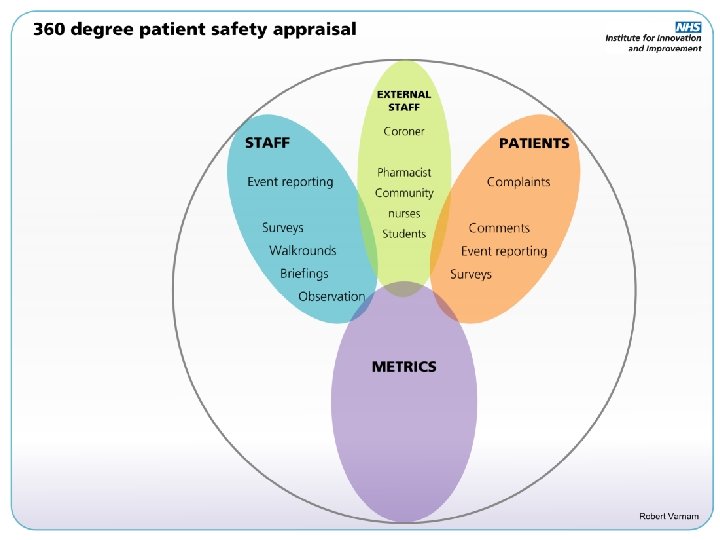
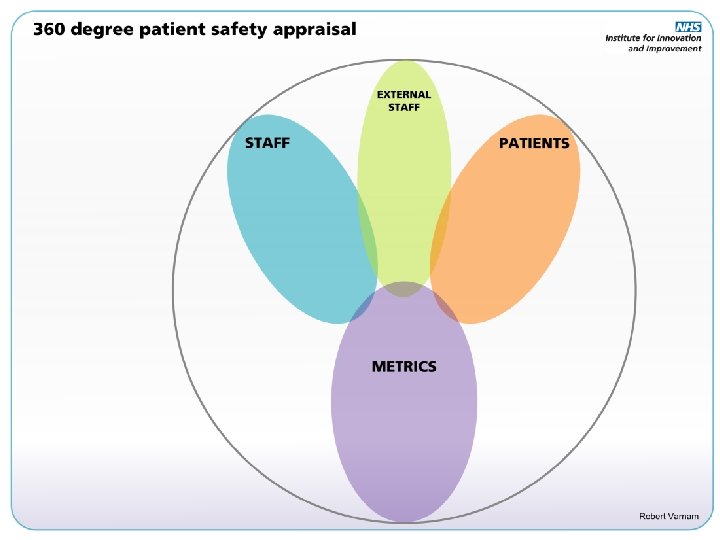
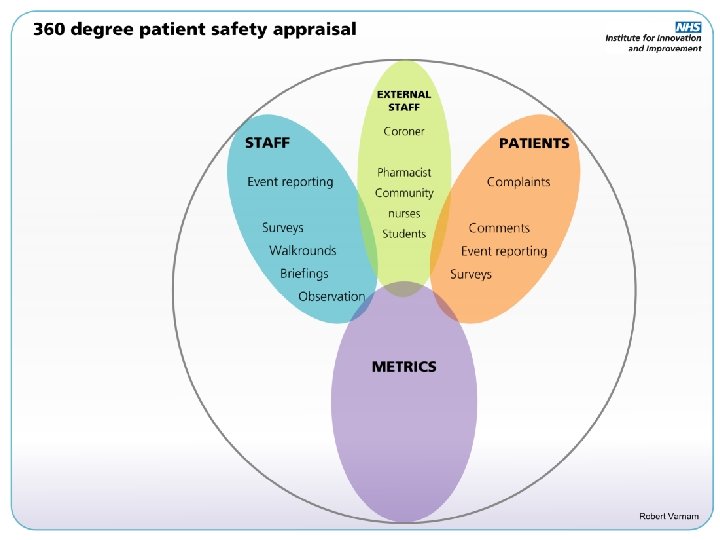
Programme this morning 1. What is Quality Care? 2. Problem Hunting i. 360 Patient Safety Appraisal ii. Process Mapping 3. What to change? i. Driver Diagrams 4. How to change things? i. PDSA cycle 5. Measurement for change 6. QI Resources 2

What is Quality Care? Safe Timely Effective Efficient Equitable Patient - Centered
Problem Hunting….
What Needs Improving? • Write you own niggle list, but be careful • Or analyse one aspect of patient care Ø Safe – where are patients being harmed? Ø Timely – how are we wasting time? Ø Effective – what are we doing that does not work? Ø Efficient – how are we wasting NHS resources? Ø Equitable – what’s not fair? Ø Patient-focused – where are patients being forgotten?
Example 1 – Analysing Safety









Example 2 – Analysing Processes
Process Mapping • Process Mapping is the visual representation of a Patient journey • What ACTUALLY happens, not what should be happening, or you think is happening. • Any process should be possible to map
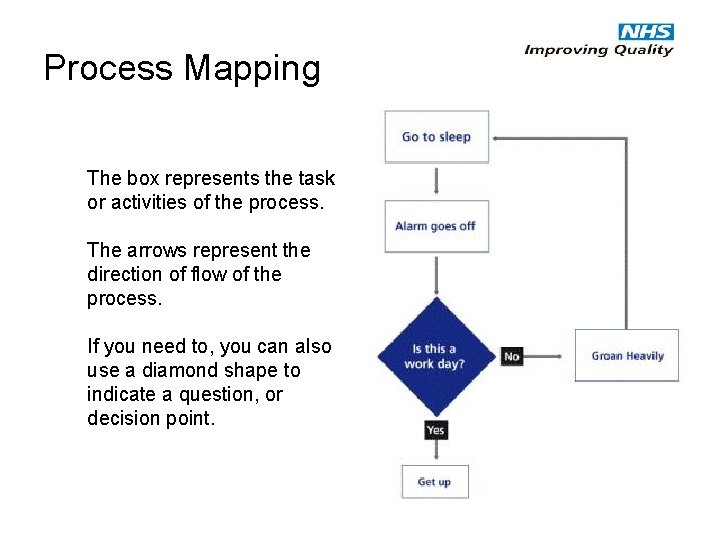
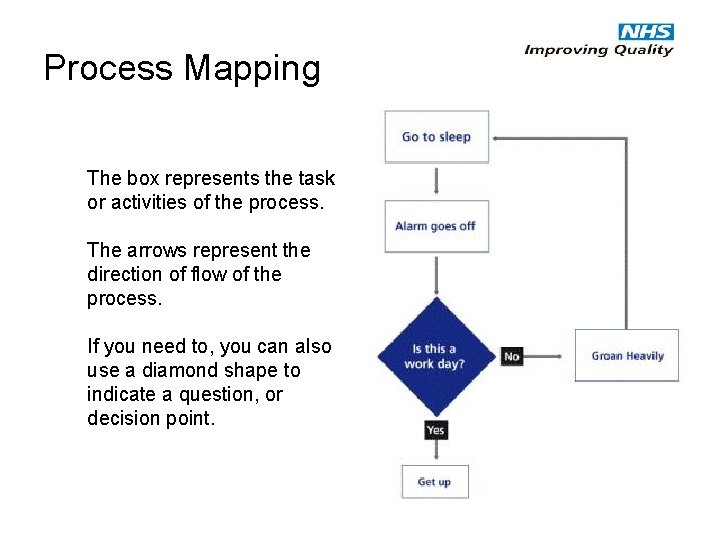
Process Mapping The box represents the task or activities of the process. The arrows represent the direction of flow of the process. If you need to, you can also use a diamond shape to indicate a question, or decision point.
Why Map a Process? “If you can’t describe what you are doing as a process, you don’t know what you’re doing. ” – William Edwards Deming
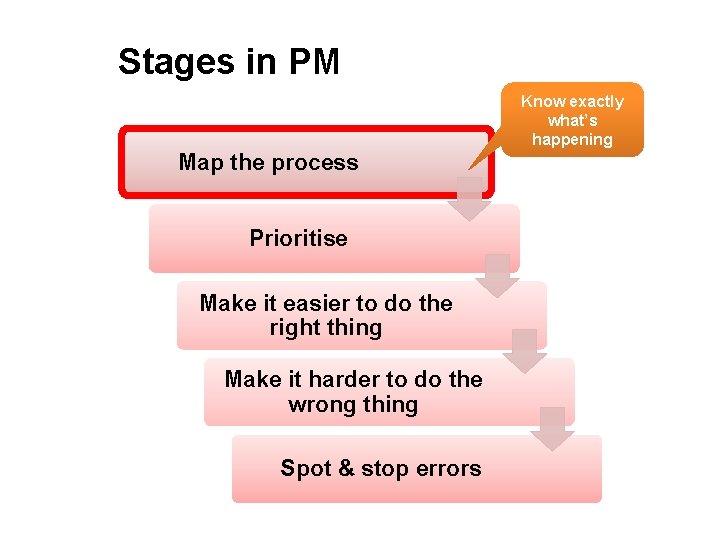
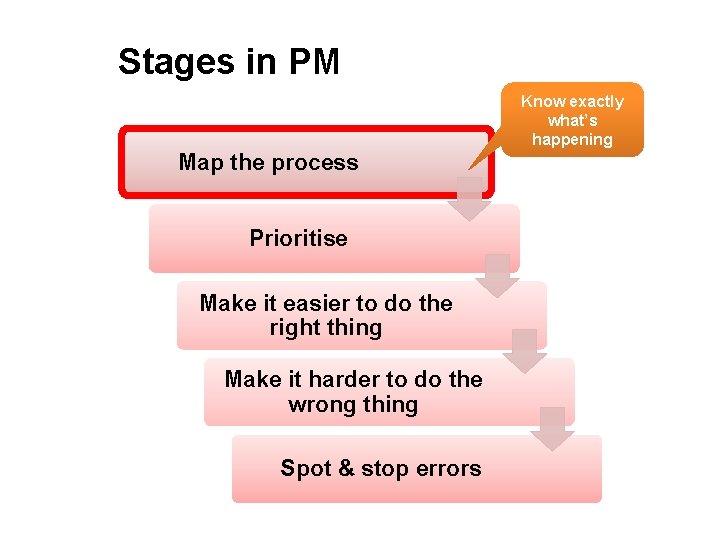
Stages in PM Know exactly what’s happening Map the process Prioritise Make it easier to do the right thing Make it harder to do the wrong thing Spot & stop errors
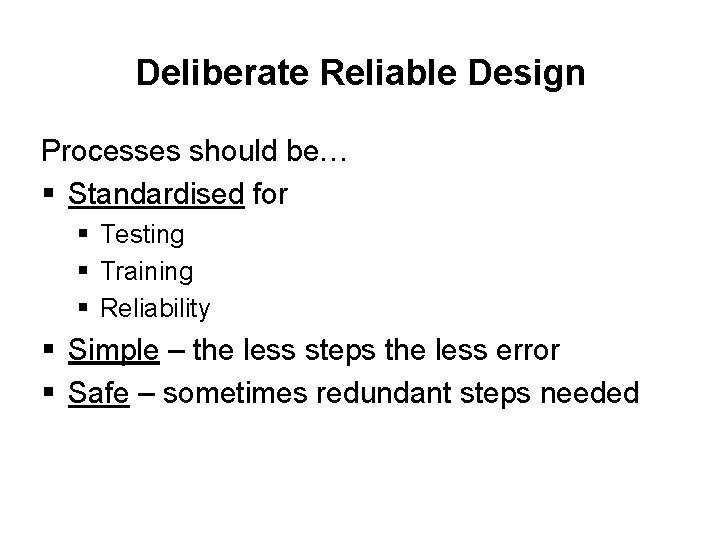
Deliberate Reliable Design Processes should be… § Standardised for § Testing § Training § Reliability § Simple – the less steps the less error § Safe – sometimes redundant steps needed
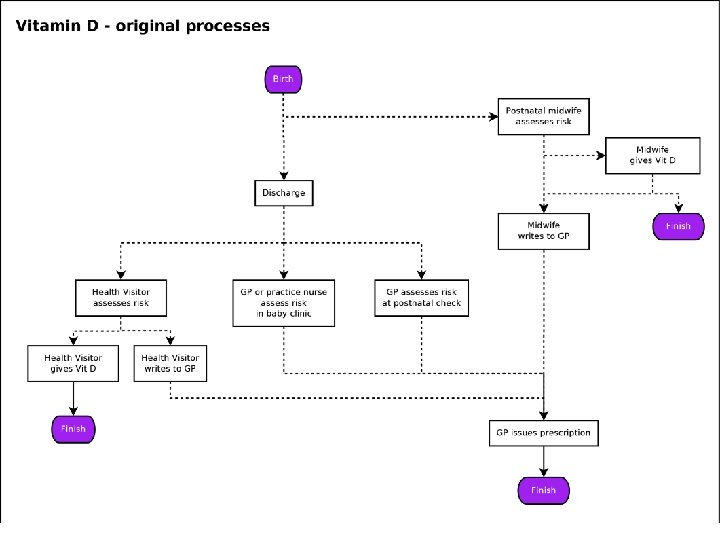
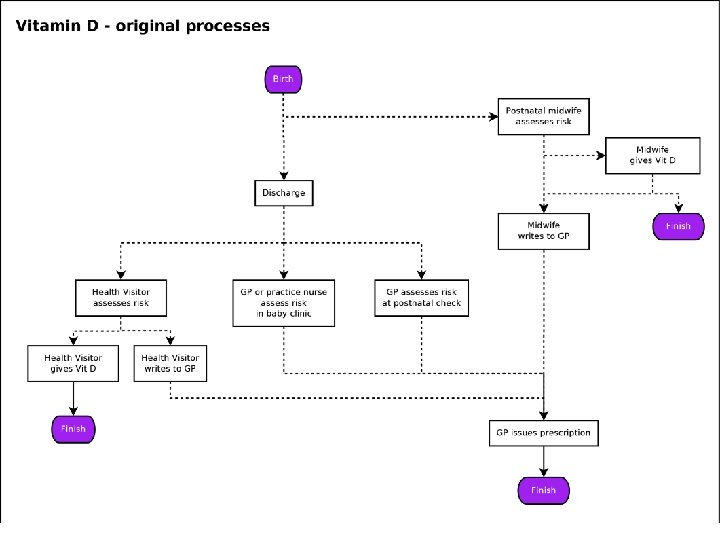
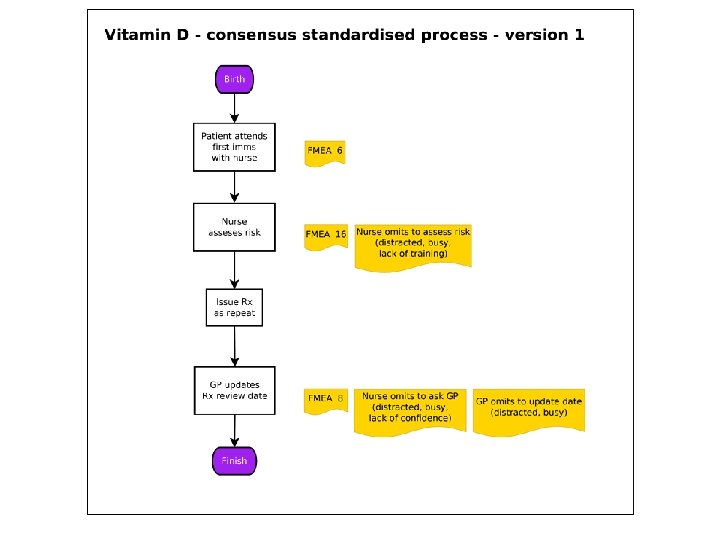
Deliberate reliable design – ? ? ? eg How do at-risk infants get Vitamin D?
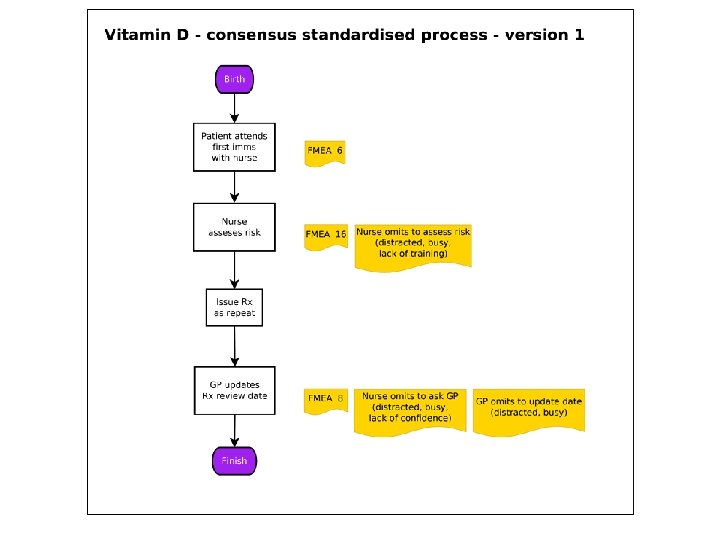
Process Mapping - 2 Stages • Stage 1 - Understand what actually happens to the Patient, where it happens and who is involved. • Stage 2 - Use the map to identify steps that could be changed.
PM Stage 1 – What actually happens? • How many times is the Patient passed from one person to another (Hand offs)? • Approximate task time • Approximate time between tasks (wait times) • Total time taken • Number of steps
PM Stage 2 – Identify problems Look for any… • Bottle necks or constraints (Queues) • Delays? (Wait for clinician/consent/results/parking) • Repetition? (e. g. Patient identity check) • Unnecessary travel or movement in the department. (Patient, staff, kit or notes) • Unnecessary steps? • Inefficient order of events?
Look at the whole process, not just the individual steps. Mind the gap !

Have a go! Look at the anticoagulant clinic process map and see if you can come up with improvements OR Try and draw a process map. Choose something you think you know well. Swap with neighbour and look for possible improvements.
Helpful resources • NHS Institute Innovation and Improvement – An Overview of Process Mapping • Scottish Health Council – Process Mapping • NHS Institute for Innovation and Improvement – Improvement Leaders Guide (Capability)

Problem Found! But what to do about it?
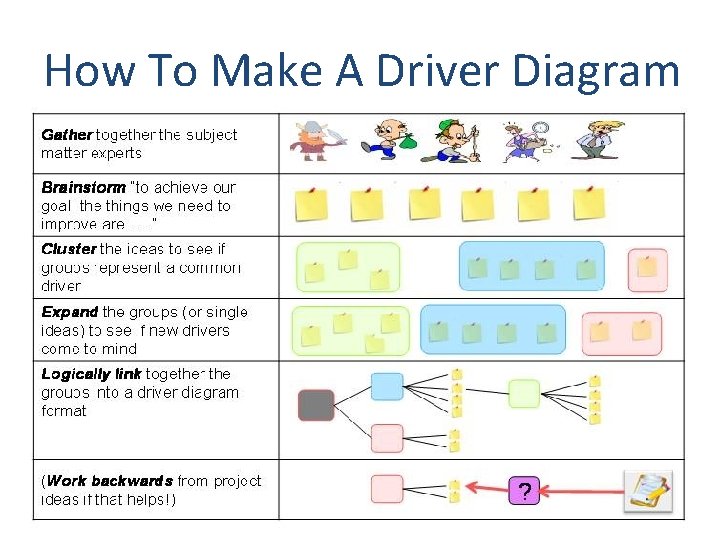
What should we tackle first? Introducing driver diagrams
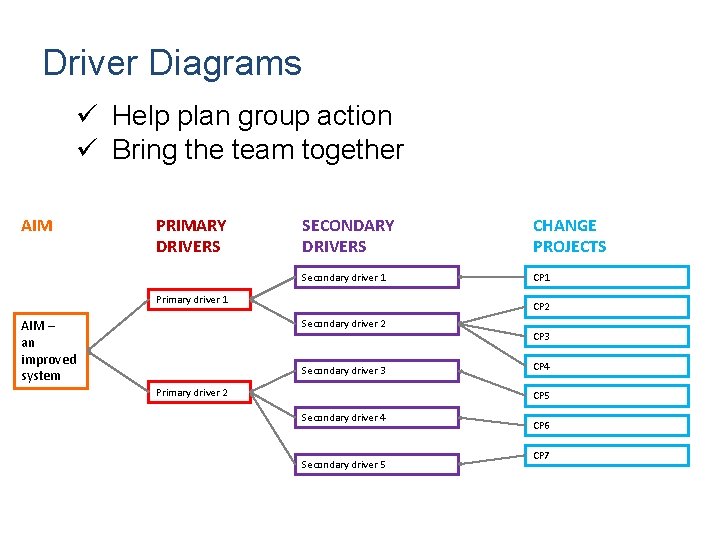
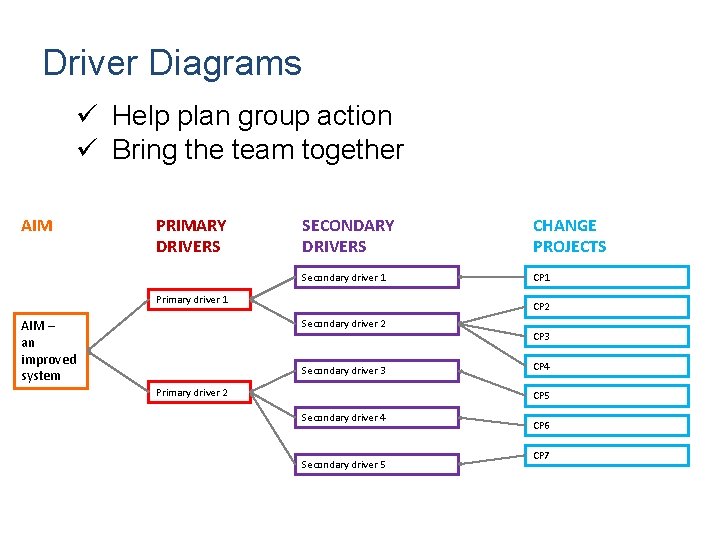
Driver Diagrams ü Help plan group action ü Bring the team together AIM PRIMARY DRIVERS SECONDARY DRIVERS CHANGE PROJECTS Secondary driver 1 CP 1 Primary driver 1 AIM – an improved system CP 2 Secondary driver 3 Primary driver 2 CP 3 CP 4 CP 5 Secondary driver 4 Secondary driver 5 CP 6 CP 7
Avoid silver bullet thinking www. em. hee. nhs. uk
Avoid blindspots www. em. hee. nhs. uk

innovate AND improve 2012, 13 & 15 – Tour de France winners 2008 & 12 – 8 Olympic Golds 2004 – 2 Olympic Golds www. em. hee. nhs. uk
Philosophy of ‘Marginal Gains’ The whole principle came from the idea that if you broke down everything you could think of that goes into riding a bike, and then improved it by 1%, you will get a significant increase when you put them all together“ David Brailsford, 2012 e. g. take your own pillow (change project; secondary driver, sleep better)
Everything you can think of? AIM Improve access Waiting room info, list clinician interests/languages, web info, Rx access (Feel Better Faster), signpost more (WIC/HV/minor inj/Secs/DNs/A&E), Chronic disease training, care planning, review periods, get it right first time, test results processing, teamworking/multiskilling, results line hours, protocols for test results, widen skill mix, BP machine in watiting room, update rpt Rx, pharmacist planning, streamline processes, streamline recalls, education & reflection, up-to-date pt contact details, know what appt is for, pt registration management, Triage, Care planning / pathways, more Tel. C, email. C, clinical buddies/teams, test results, repeat Rx, forwarding tasks + results, check + update usual GP, results actioned by right person, advance appt booking, reserve list, ask pt who they want, rota in advance, notekeeping w plan + pt info, Consult skills, comp skills, speed reading/typing, forms + equipment, multi-skilling, longer appts, No emerg appts, Test results, Care planning, High risk processes, Referral chase-up, results continuity, streamline processes, streamline recalls, clear up alerts, handling of normal results, self-checkin, fast-track queue
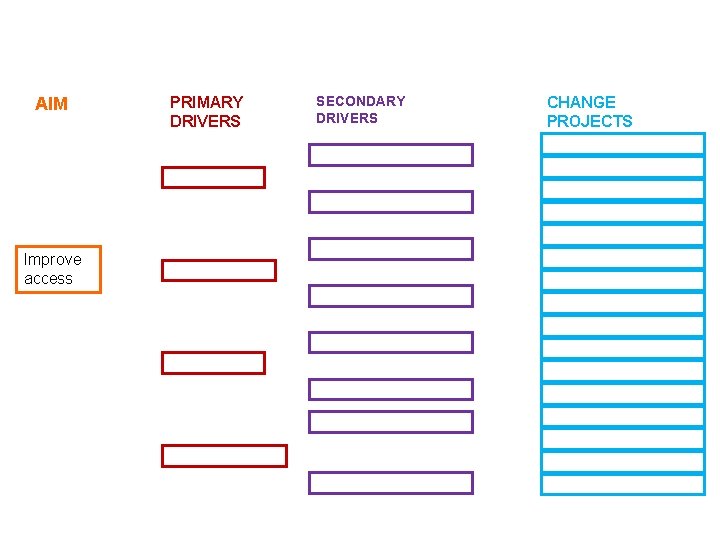
AIM Improve access PRIMARY DRIVERS SECONDARY DRIVERS CHANGE PROJECTS
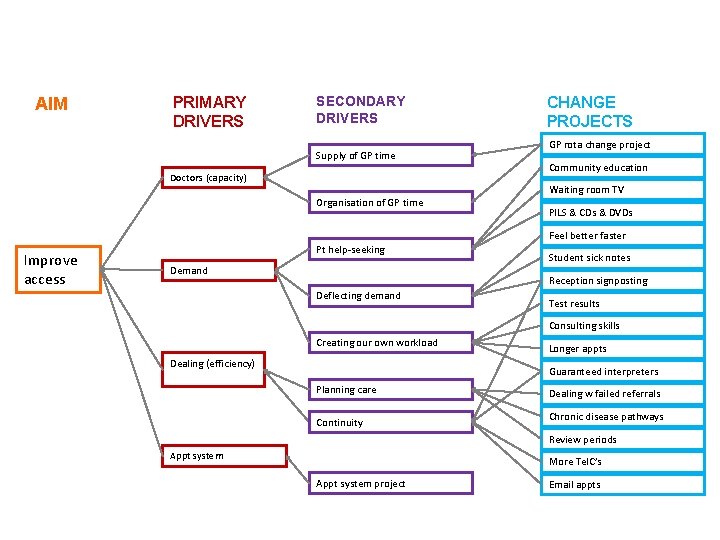
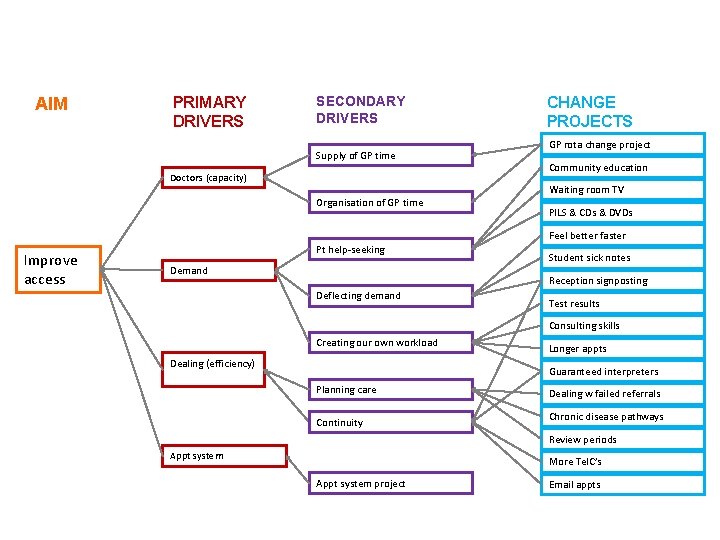
AIM PRIMARY DRIVERS SECONDARY DRIVERS Supply of GP time Doctors (capacity) Organisation of GP time CHANGE PROJECTS GP rota change project Community education Waiting room TV PILS & CDs & DVDs Feel better faster Improve access Pt help-seeking Demand Student sick notes Reception signposting Deflecting demand Test results Consulting skills Creating our own workload Dealing (efficiency) Longer appts Guaranteed interpreters Planning care Continuity Dealing w failed referrals Chronic disease pathways Review periods Appt system More Tel. C’s Appt system project Email appts
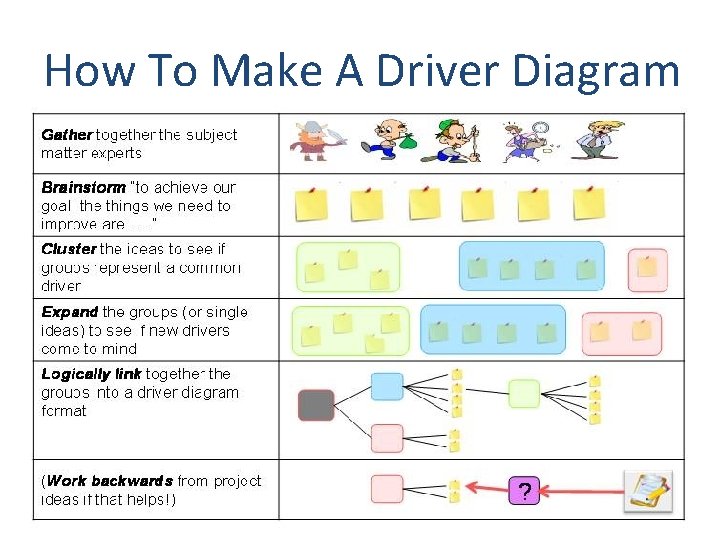
How To Make A Driver Diagram
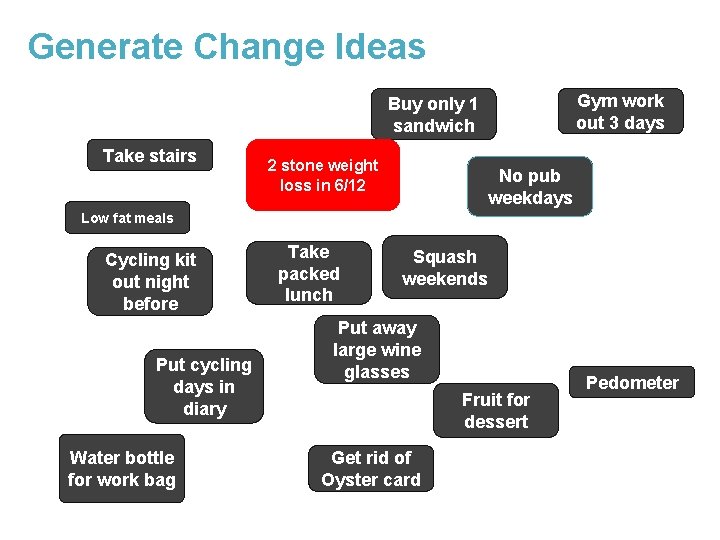
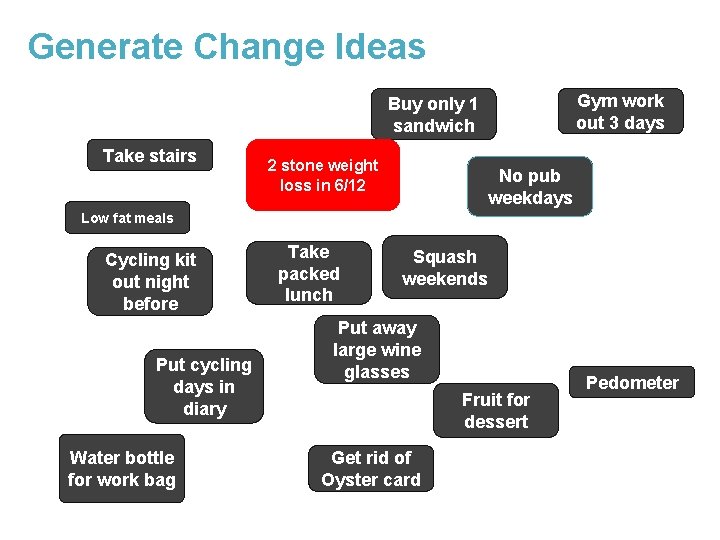
Generate Change Ideas Gym work out 3 days Buy only 1 sandwich Take stairs 2 stone weight loss in 6/12 No pub weekdays Low fat meals Cycling kit out night before Put cycling days in diary Water bottle for work bag Take packed lunch Squash weekends Put away large wine glasses Fruit for dessert Get rid of Oyster card Pedometer
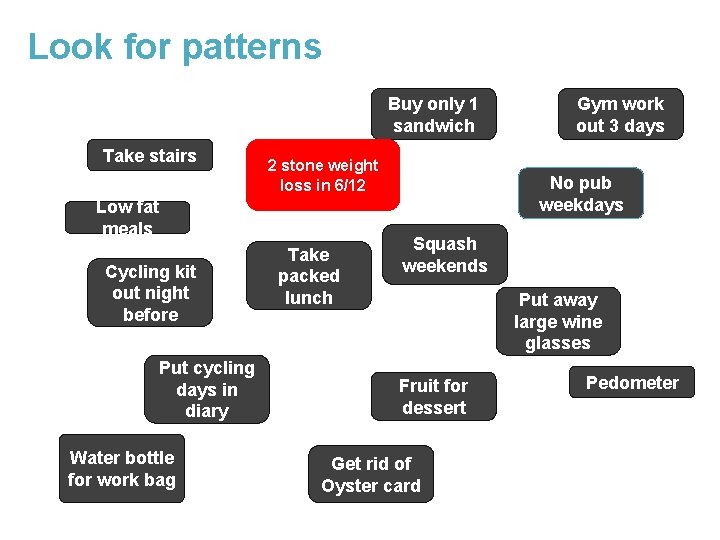
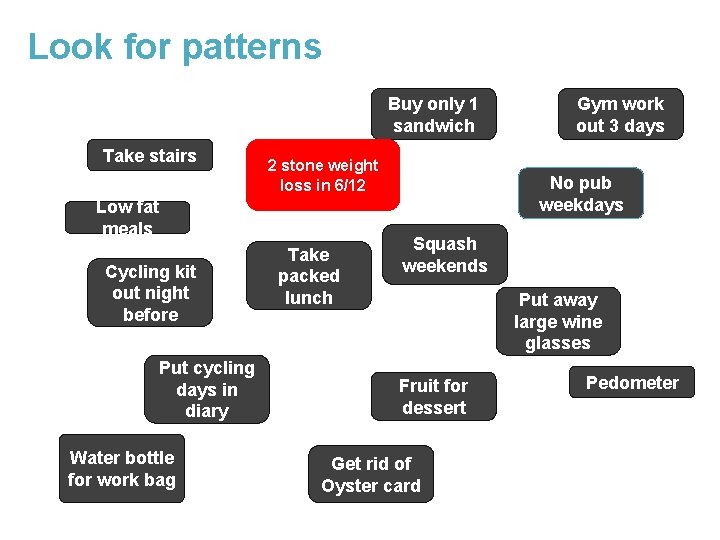
Look for patterns Buy only 1 sandwich Take stairs 2 stone weight loss in 6/12 Low fat meals Cycling kit out night before Put cycling days in diary Water bottle for work bag Take packed lunch Gym work out 3 days No pub weekdays Squash weekends Put away large wine glasses Fruit for dessert Get rid of Oyster card Pedometer

Marshall the mass of ideas Take packed lunch Low fat meals Substitute lower calorie foods Eat less Buy only 1 Water bottle sandwich for work bag Fruit for dessert Put cycling days in diary Cycling kit out night Do sport before Gym work out 3 days Squash weekends Drink less alcohol No pub weekdays Put away large wine glasses 2 stone weight loss in 6/12 Be more active during the day Pedometer Take stairs Get rid of Oyster card
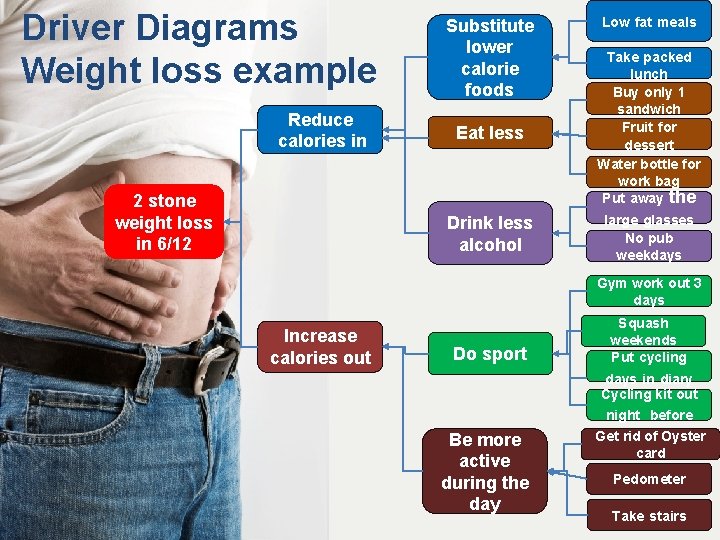
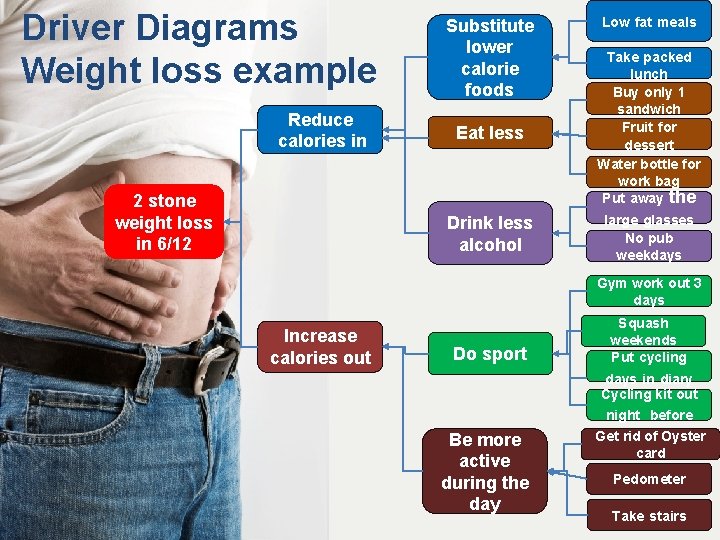
Driver Diagrams Weight loss example Reduce calories in 2 stone weight loss in 6/12 Substitute lower calorie foods Low fat meals Eat less Take packed lunch Buy only 1 sandwich Fruit for dessert Water bottle for work bag Put away the Drink less alcohol large glasses No pub weekdays Gym work out 3 days Increase calories out Do sport Squash weekends Put cycling days in diary Cycling kit out night before Be more active during the day Get rid of Oyster card Pedometer Take stairs
What Do You Want to Change? In your practice you could… 1. Identify an aim 2. Come up with lots of ideas – think small i. Through team meeting ii. Or suggestion box 3. Group them 4. Remove duplications/Expand other ideas 5. Identify idea(s) to implement

Any Questions? www. em. hee. nhs. uk
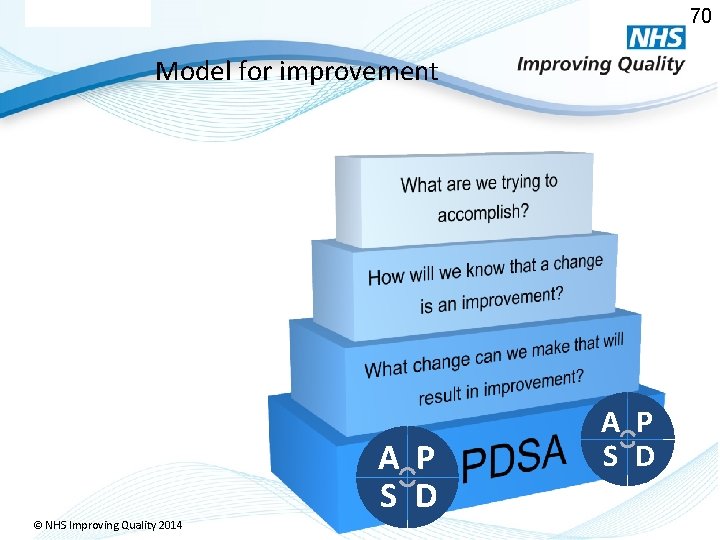
NHS Model For Improvement
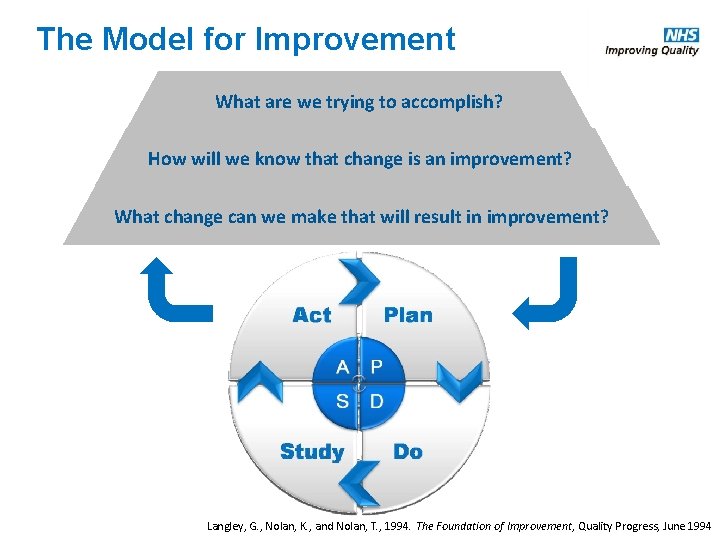
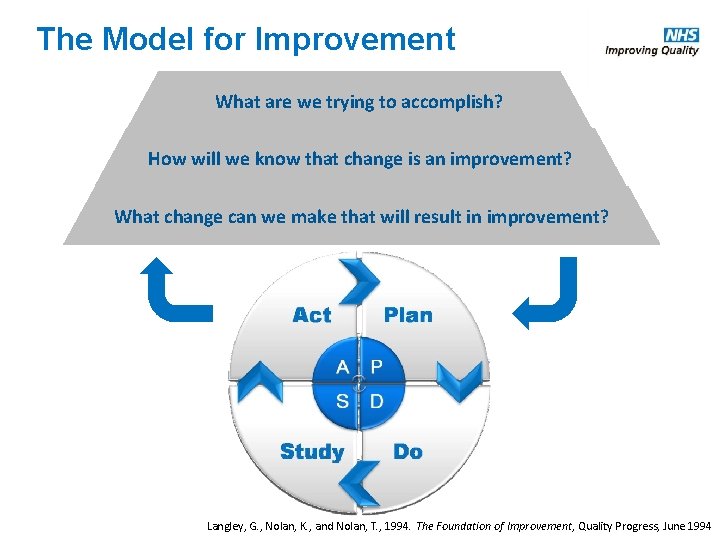
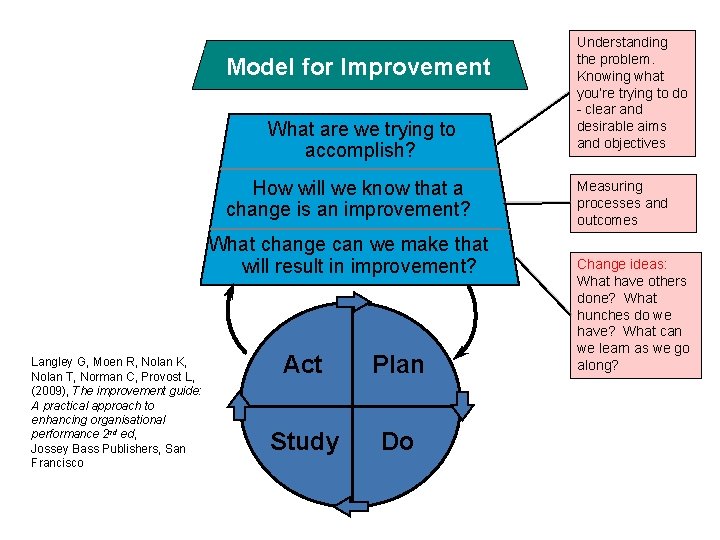
The Model for Improvement What are we trying to accomplish? How will we know that change is an improvement? What change can we make that will result in improvement? Langley, G. , Nolan, K. , and Nolan, T. , 1994. The Foundation of Improvement, Quality Progress, June 1994
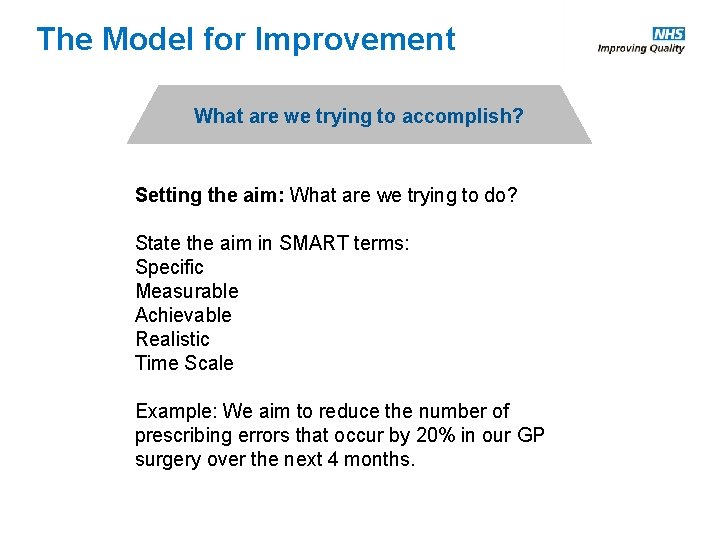
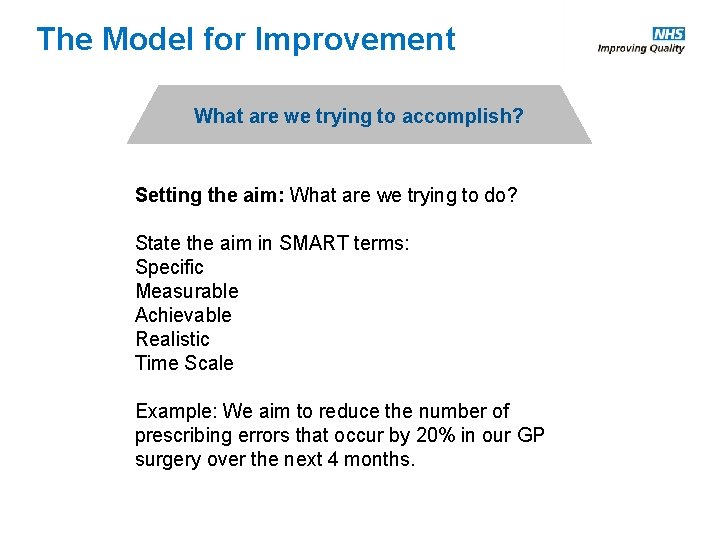
The Model for Improvement What are we trying to accomplish? Setting the aim: What are we trying to do? State the aim in SMART terms: Specific Measurable Achievable Realistic Time Scale Example: We aim to reduce the number of prescribing errors that occur by 20% in our GP surgery over the next 4 months.
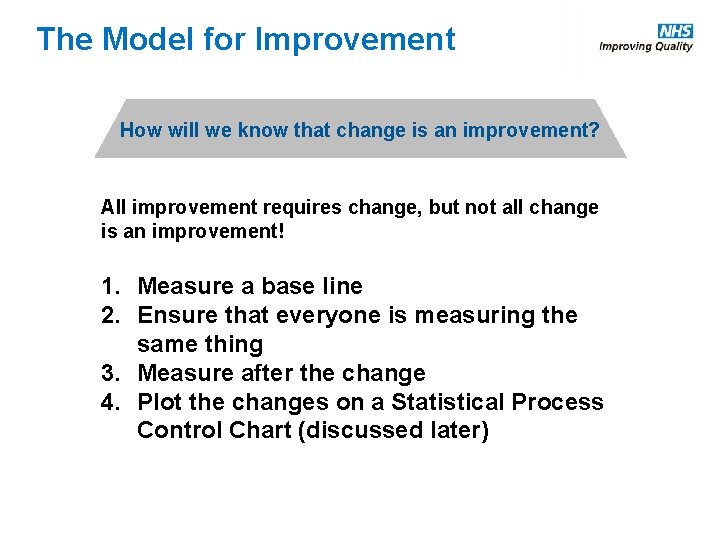
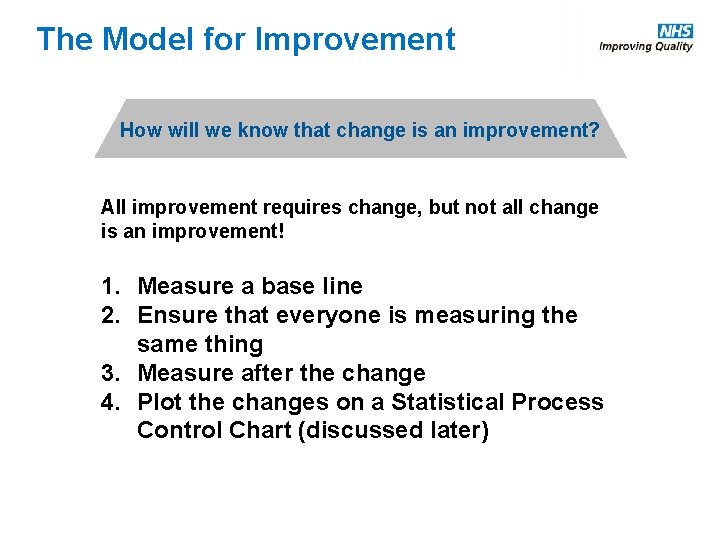
The Model for Improvement How will we know that change is an improvement? All improvement requires change, but not all change is an improvement! 1. Measure a base line 2. Ensure that everyone is measuring the same thing 3. Measure after the change 4. Plot the changes on a Statistical Process Control Chart (discussed later)

The Model for Improvement What change can we make that will result in improvement? Whole team involvement Brainstorming Ideas on post its Process Mapping Driver Diagrams Search for Precedents
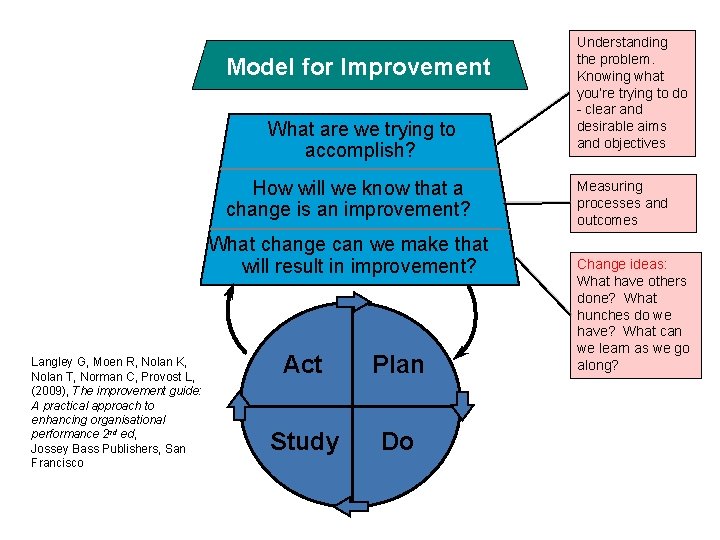
Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? Langley G, Moen R, Nolan K, Nolan T, Norman C, Provost L, (2009), The improvement guide: A practical approach to enhancing organisational performance 2 nd ed, Jossey Bass Publishers, San Francisco Act Plan Study Do Understanding the problem. Knowing what you’re trying to do - clear and desirable aims and objectives Measuring processes and outcomes Change ideas: What have others done? What hunches do we have? What can we learn as we go along?
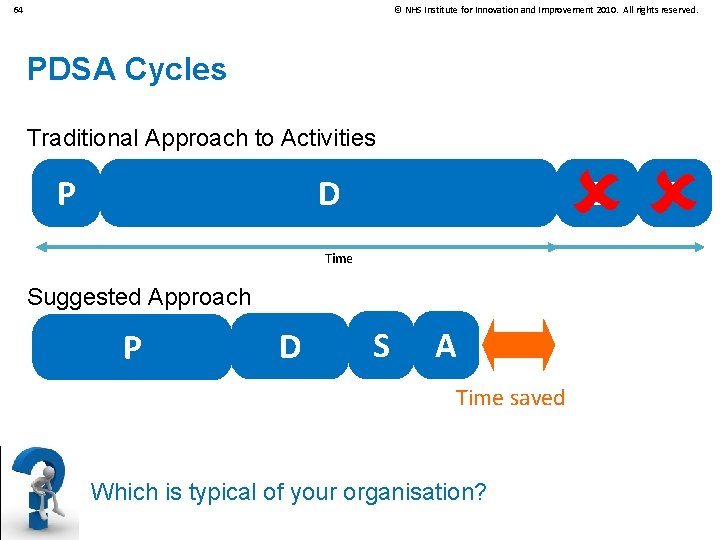
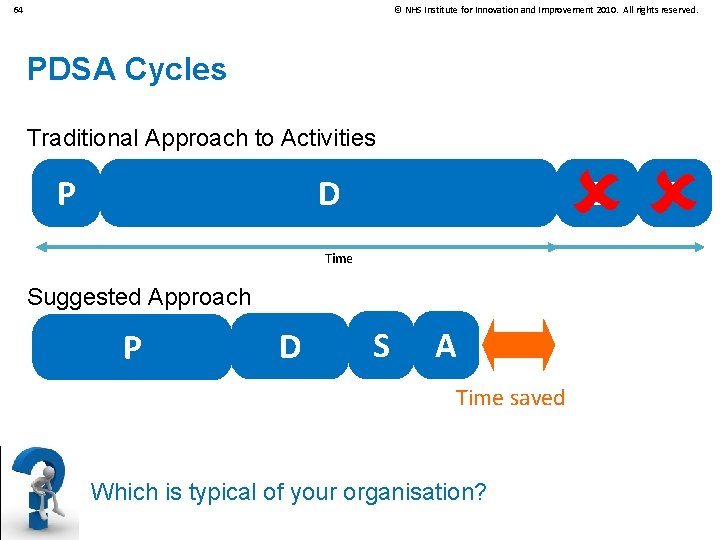
64 © NHS Institute for Innovation and Improvement 2010. All rights reserved. PDSA Cycles Traditional Approach to Activities D P S Time Suggested Approach P D S A Time saved Which is typical of your organisation? A
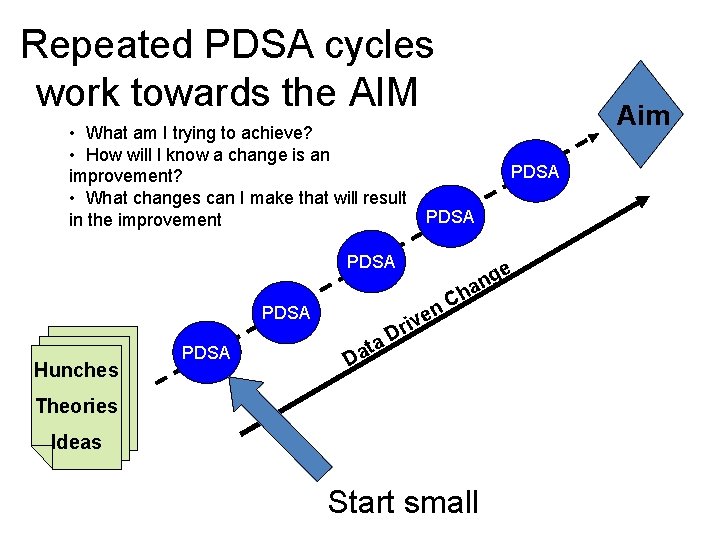
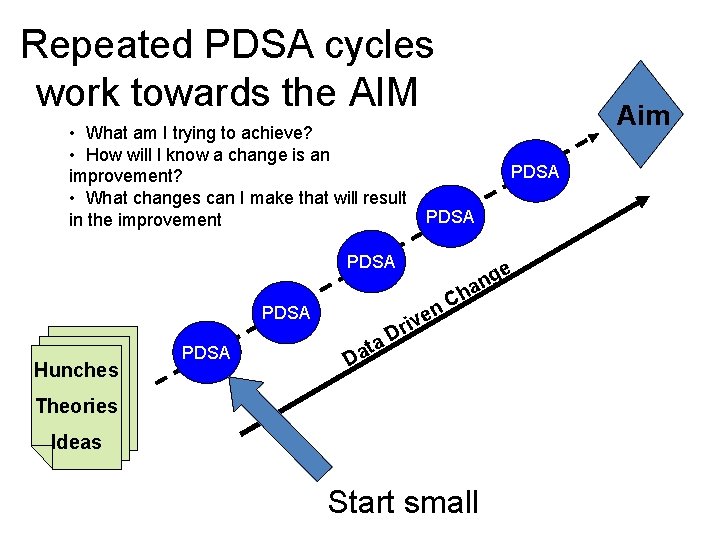
Repeated PDSA cycles work towards the AIM • What am I trying to achieve? • How will I know a change is an improvement? • What changes can I make that will result PDSA in the improvement PDSA Hunches PDSA ge n a h C n e riv D a t Da Aim Theories Ideas Start small
Benefits of this approach • • • easier to start produces better solutions more quickly engages people better reduces waste easier to continue

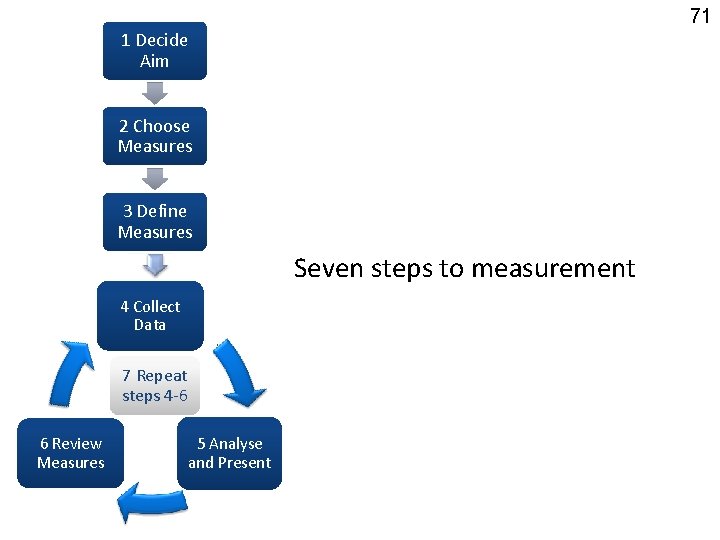
Measurement for Improvement
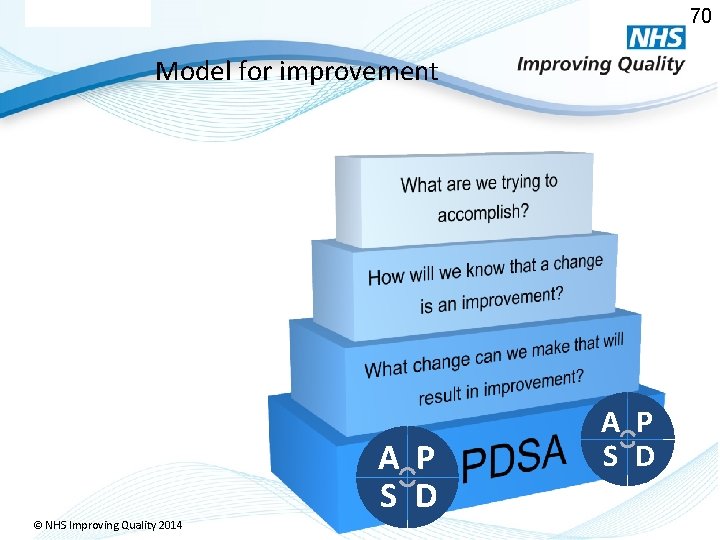
70 Model for improvement A P S D © NHS Improving Quality 2014 A P S D
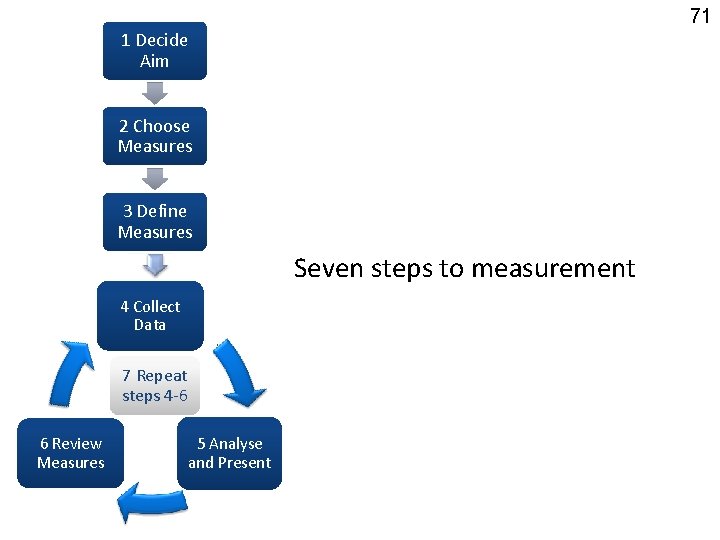
71 1 Decide Aim 2 Choose Measures 3 Define Measures Seven steps to measurement 4 Collect Data 7 Repeat steps 4 -6 6 Review Measures © NHS Improving Quality 2014 5 Analyse and Present
Step 1 – Decide Aim Make it SMART
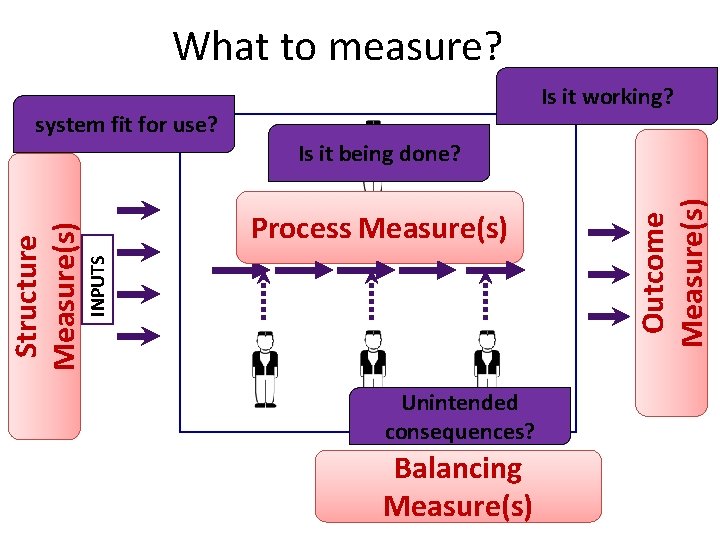
Steps 2 & 3 Choose & Define Measures. Structure, Process, Outcome & Balancing measures.

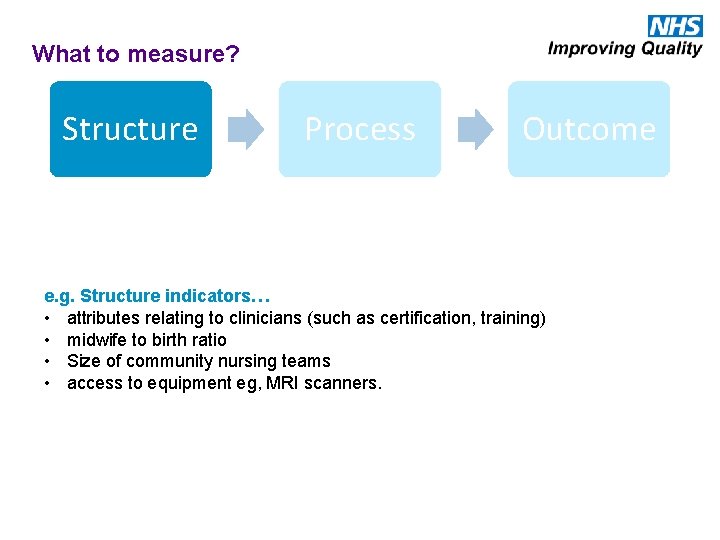
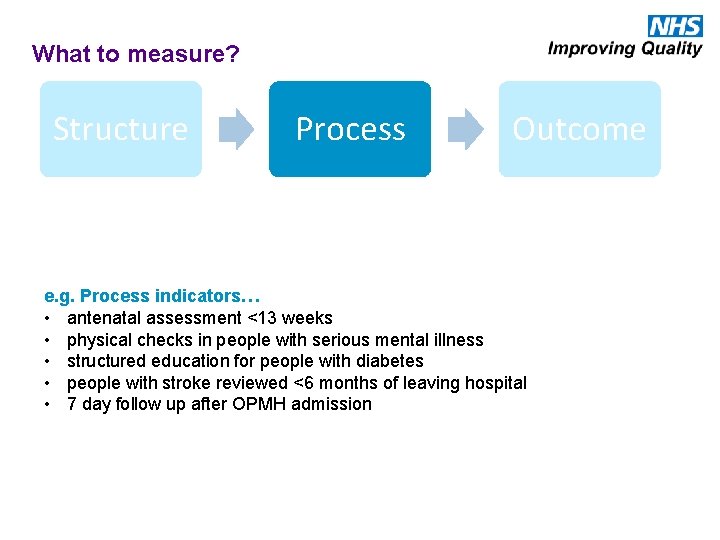
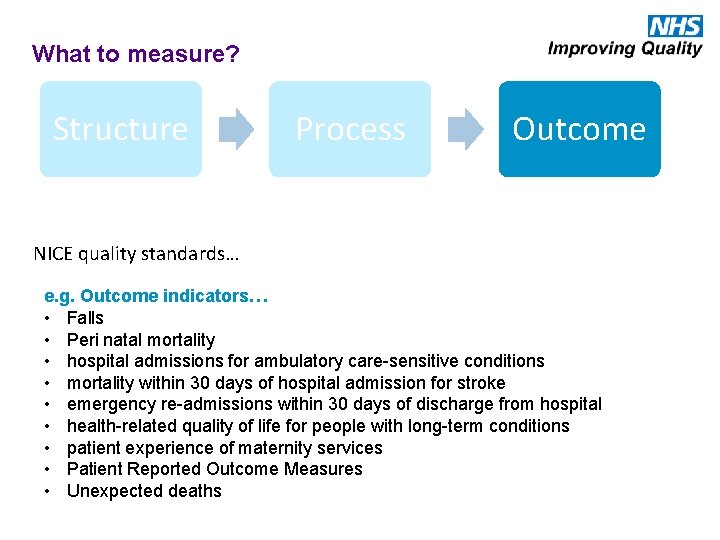
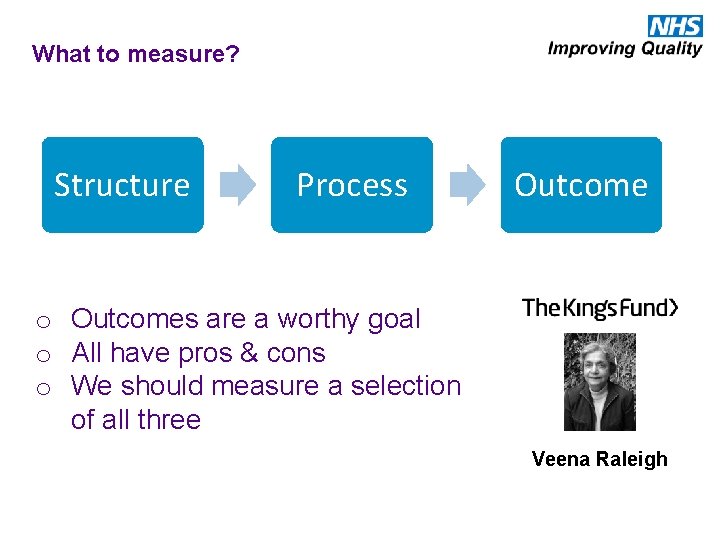
What to measure? Structure Process Outcome The environment in which care occurs What care is delivered, and how The impact on patients and the population ‘Outcomes remain the ultimate validators of the effectiveness and quality of medical care’ but they ‘must be used with discrimination’ Avedis Donabedian
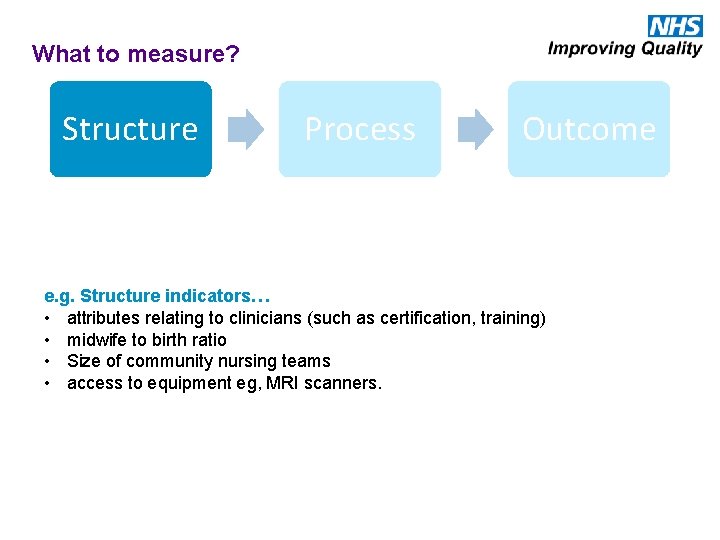
What to measure? Structure Process Outcome e. g. Structure indicators… • attributes relating to clinicians (such as certification, training) • midwife to birth ratio • Size of community nursing teams • access to equipment eg, MRI scanners.
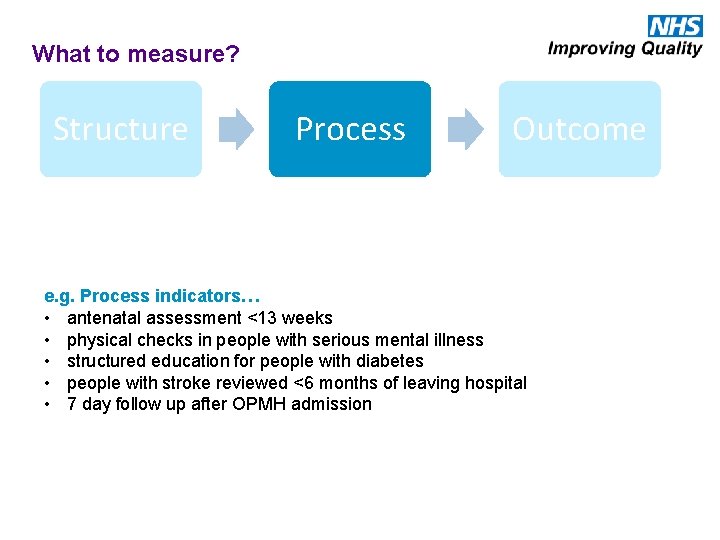
What to measure? Structure Process Outcome e. g. Process indicators… • antenatal assessment <13 weeks • physical checks in people with serious mental illness • structured education for people with diabetes • people with stroke reviewed <6 months of leaving hospital • 7 day follow up after OPMH admission
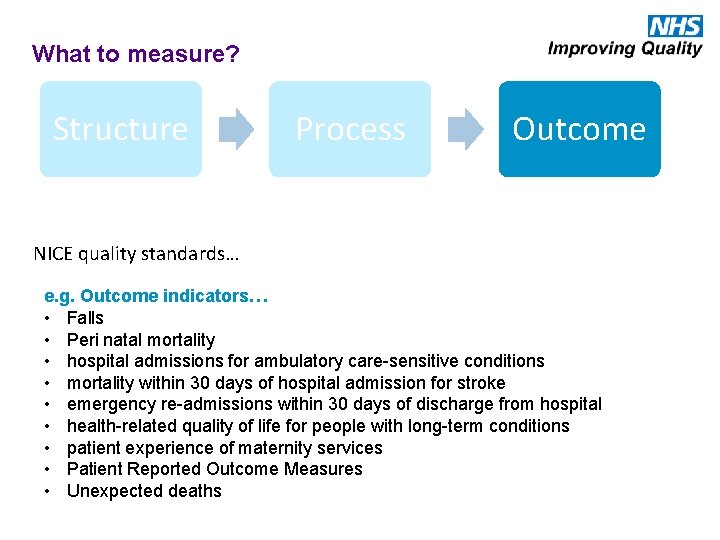
What to measure? Structure Process Outcome NICE quality standards… e. g. Outcome indicators… • Falls • Peri natal mortality • hospital admissions for ambulatory care-sensitive conditions • mortality within 30 days of hospital admission for stroke • emergency re-admissions within 30 days of discharge from hospital • health-related quality of life for people with long-term conditions • patient experience of maternity services • Patient Reported Outcome Measures • Unexpected deaths
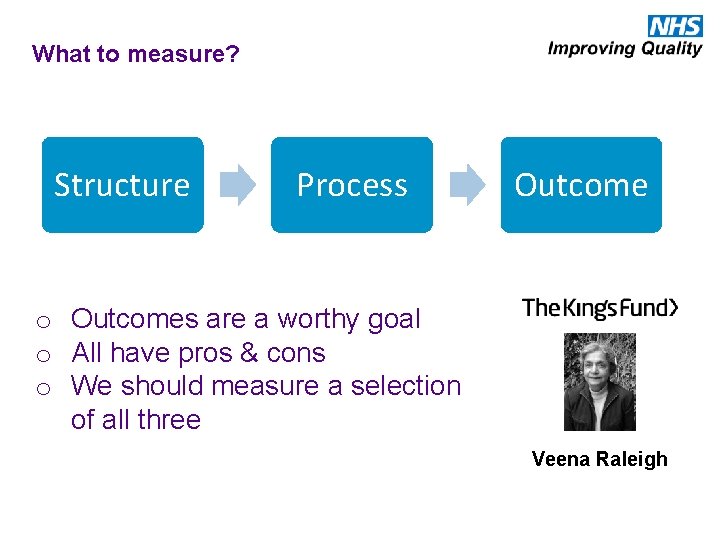
What to measure? Structure Process Outcome o Outcomes are a worthy goal o All have pros & cons o We should measure a selection of all three Veena Raleigh
Balancing measures
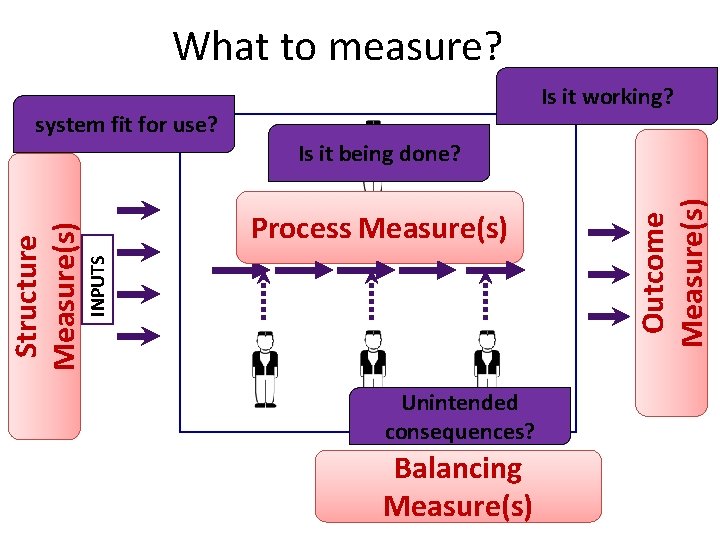
What to measure? Is it being done? HUMAN FACTORS Process Measure(s) INPUTS Structure Measure(s) FACTORS INTERNAL PROCESSES & PROCECEDURES HUMAN FACTORS Unintended consequences? Balancing Measure(s) OUTPUTS Outcome Measure(s) EXTERNAL system fit for use? Is it working?
Steps 4& 5 Collecting , analysing and presenting data.
I use run charts & statistical process control (SPC) I know about run charts & statistical process control (SPC) I don’t know about run charts & statistical process control (SPC)
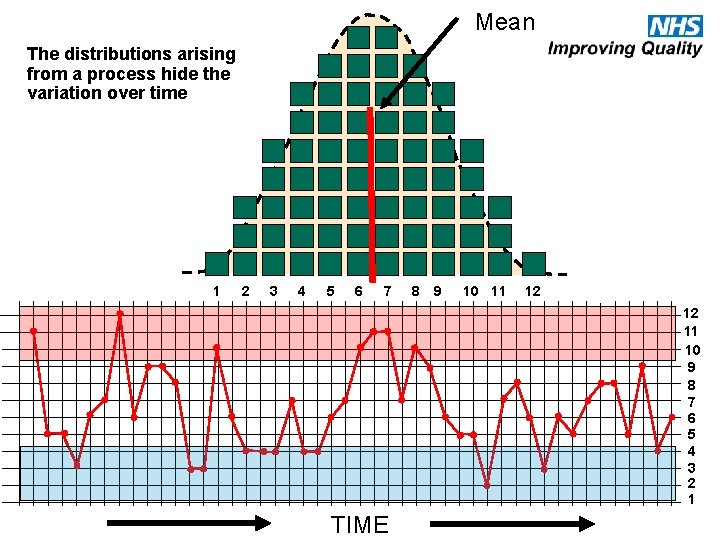
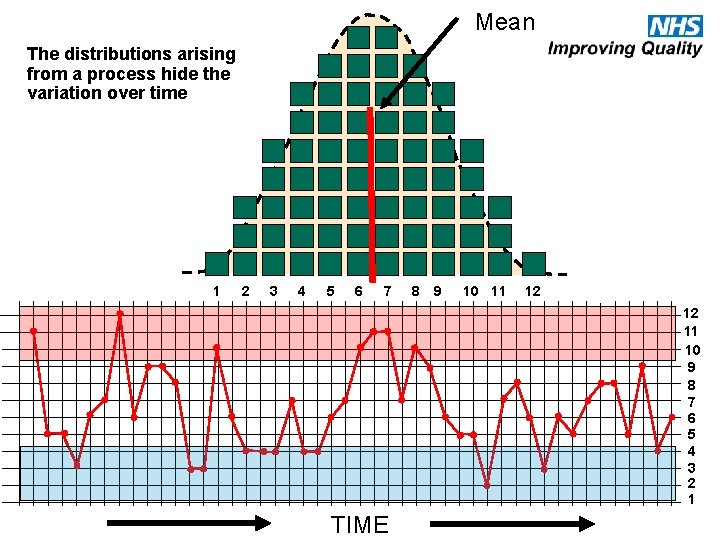
Mean The distributions arising from a process hide the variation over time 1 2 3 4 5 6 7 8 9 10 11 12 12 11 10 9 8 7 6 5 4 3 2 1 TIME
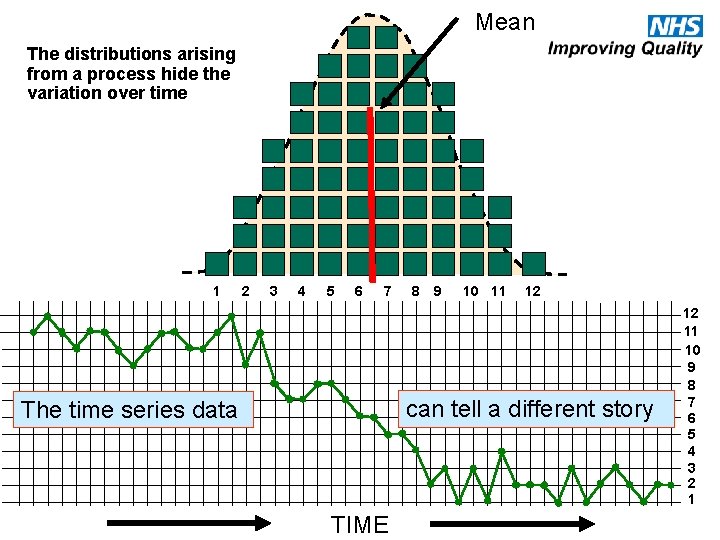
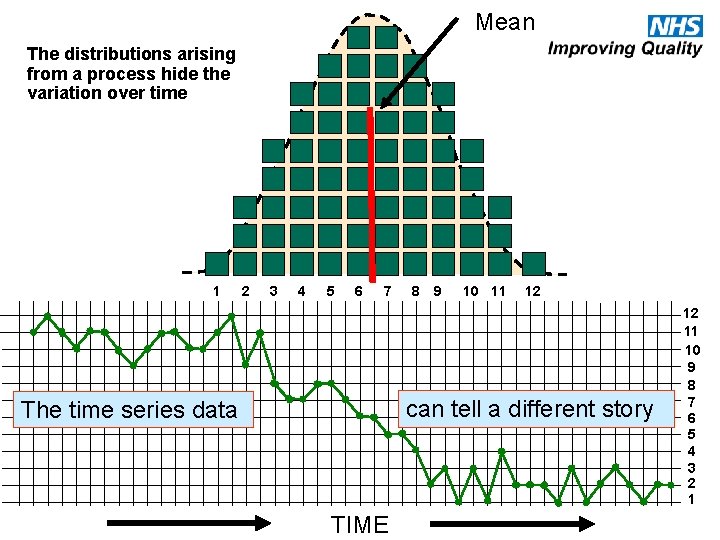
Mean The distributions arising from a process hide the variation over time 1 2 3 4 5 6 7 8 9 10 11 12 can tell a different story The time series data TIME 12 11 10 9 8 7 6 5 4 3 2 1
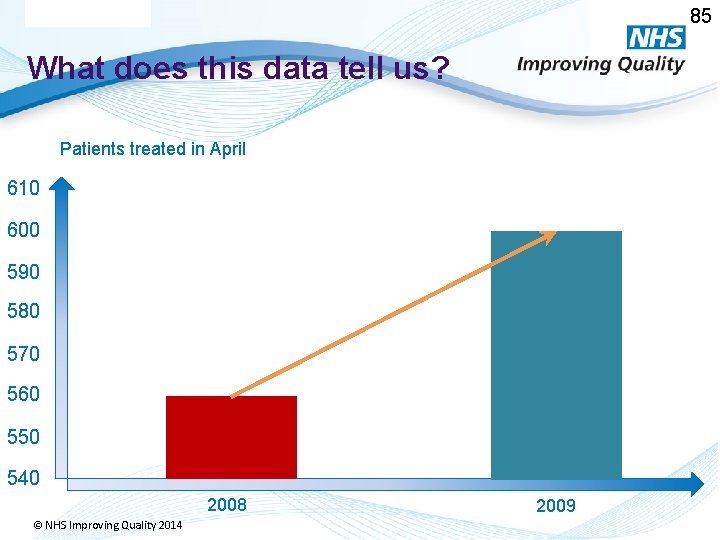
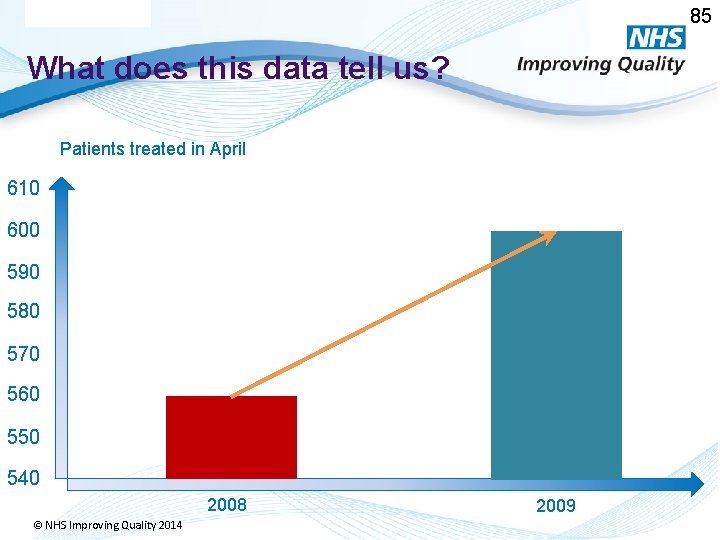
85 What does this data tell us? Patients treated in April 610 600 590 580 570 560 550 540 2008 © NHS Improving Quality 2014 2009
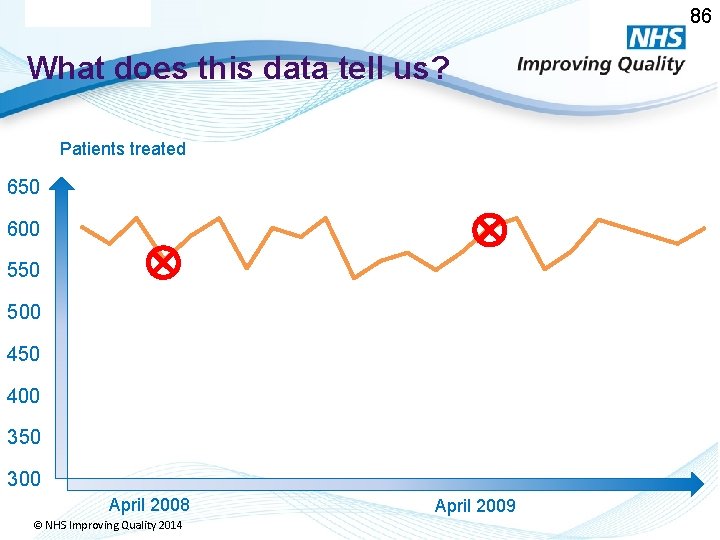
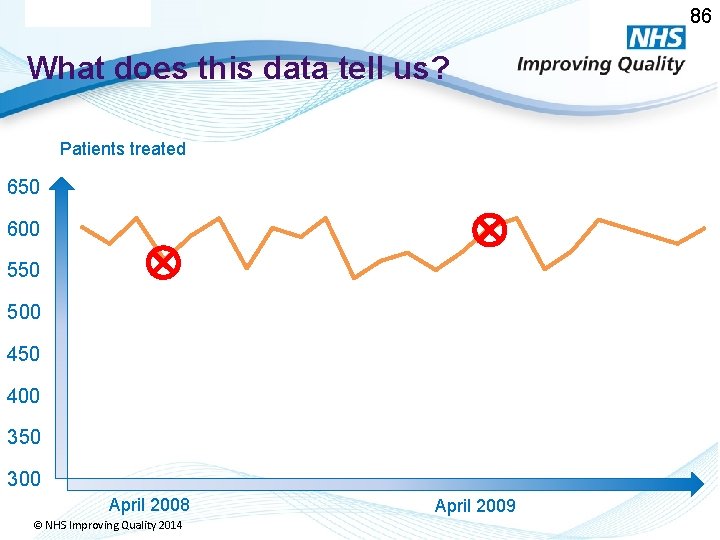
86 What does this data tell us? Patients treated 650 600 550 500 450 400 350 300 April 2008 © NHS Improving Quality 2014 April 2009
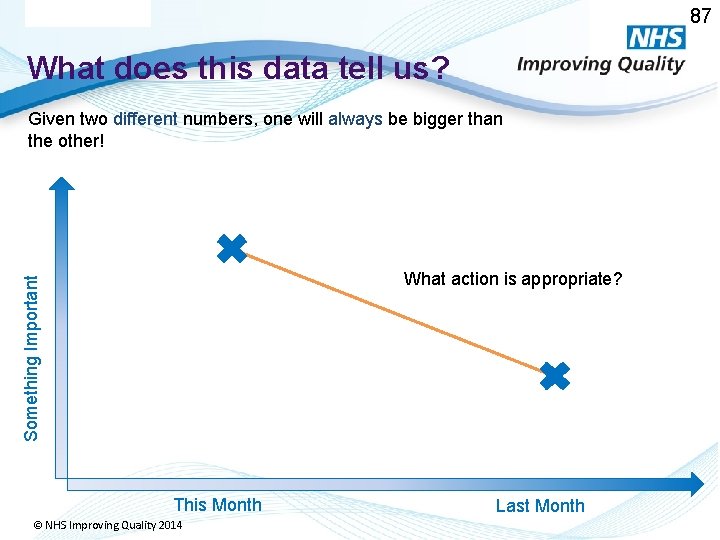
87 What does this data tell us? Given two different numbers, one will always be bigger than the other! Something Important What action is appropriate? This Month © NHS Improving Quality 2014 Last Month
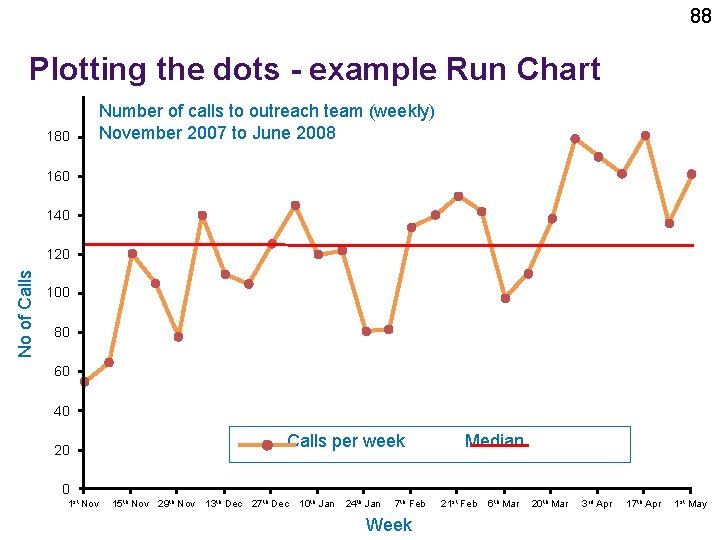
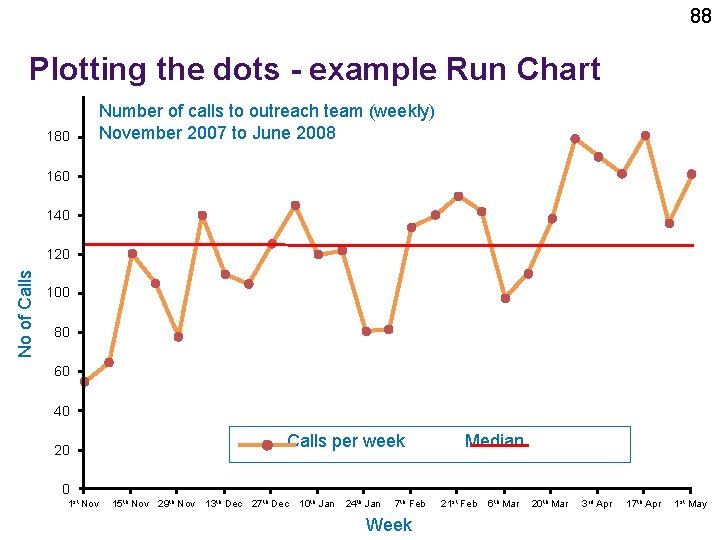
88 Plotting the dots - example Run Chart 180 Number of calls to outreach team (weekly) November 2007 to June 2008 160 140 No of Calls 120 100 80 60 40 Calls per week Median 20 0 1 st Nov 15 th Nov 29 th Nov © NHS Improving Quality 2014 13 th Dec 27 th Dec 10 th Jan 24 th Jan 7 th Feb Week 21 st Feb 6 th Mar 20 th Mar 3 rd Apr 17 th Apr 1 st May
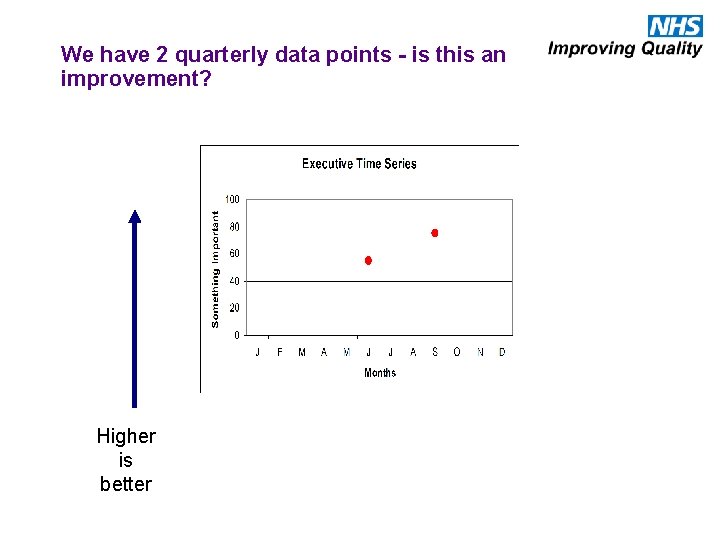
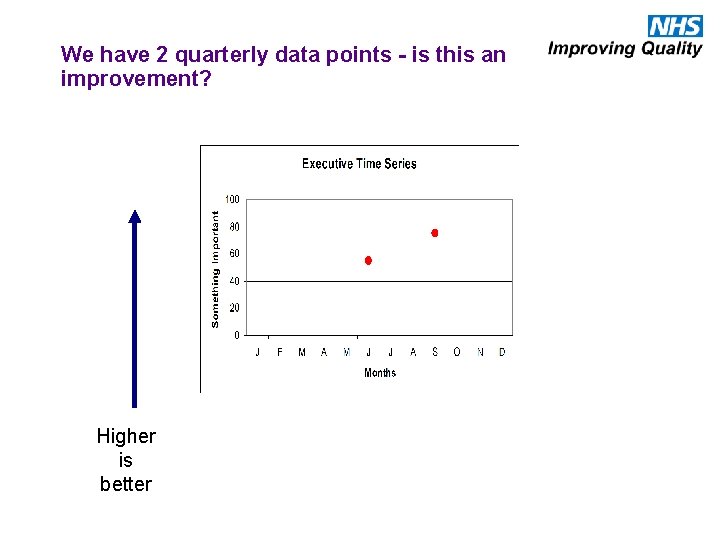
We have 2 quarterly data points - is this an improvement? Higher is better
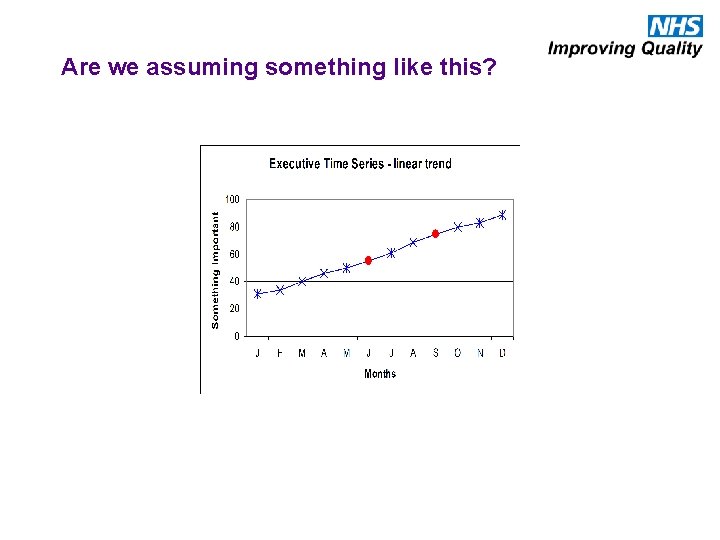
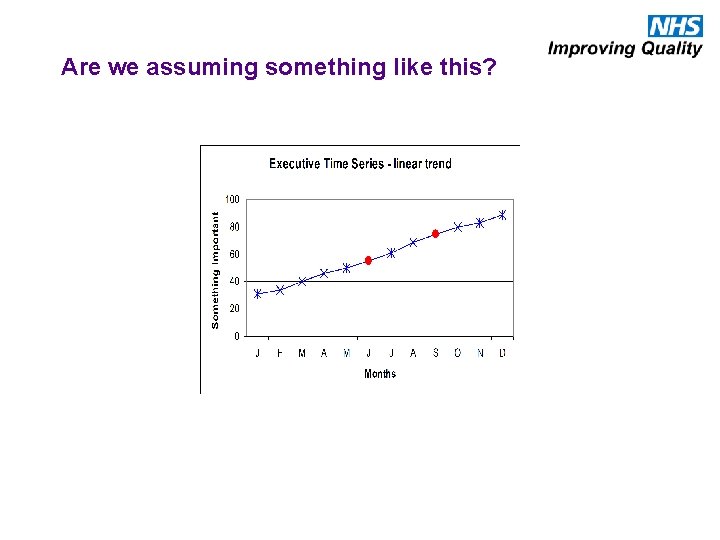
Are we assuming something like this?
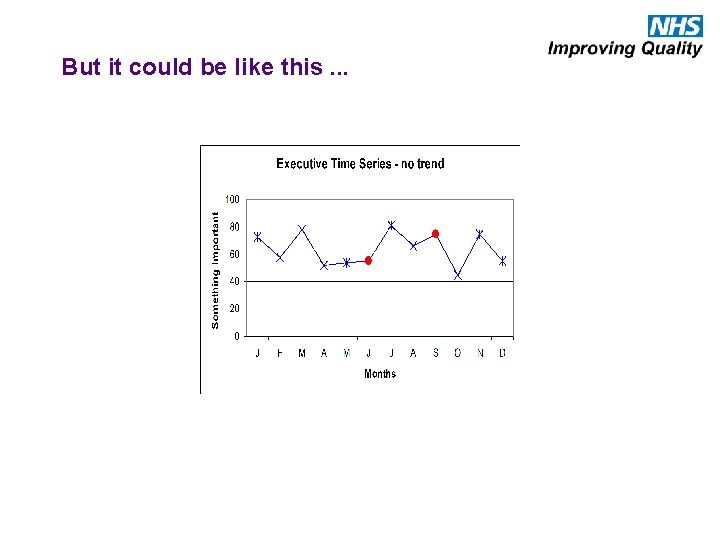
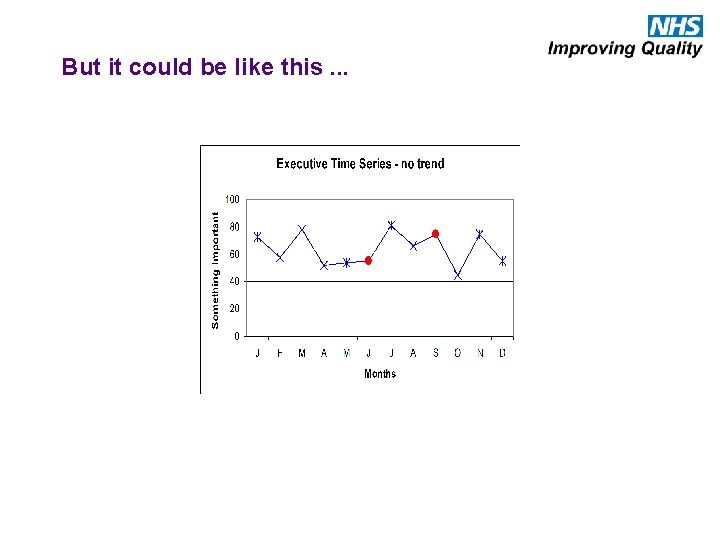
But it could be like this. . .
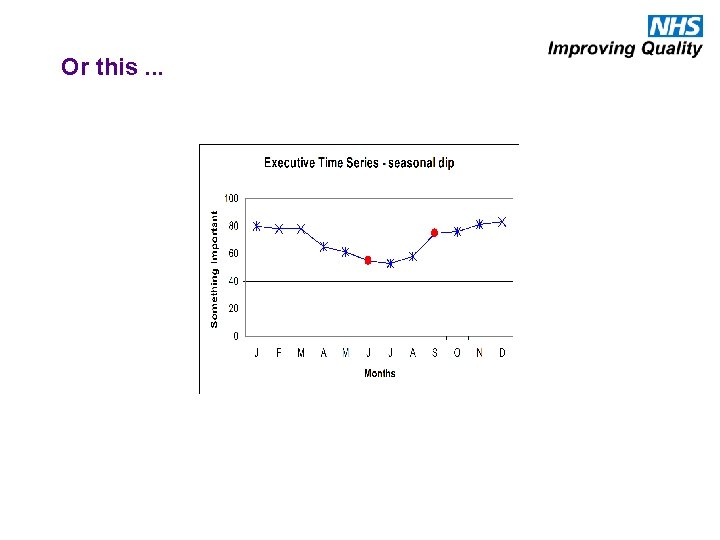
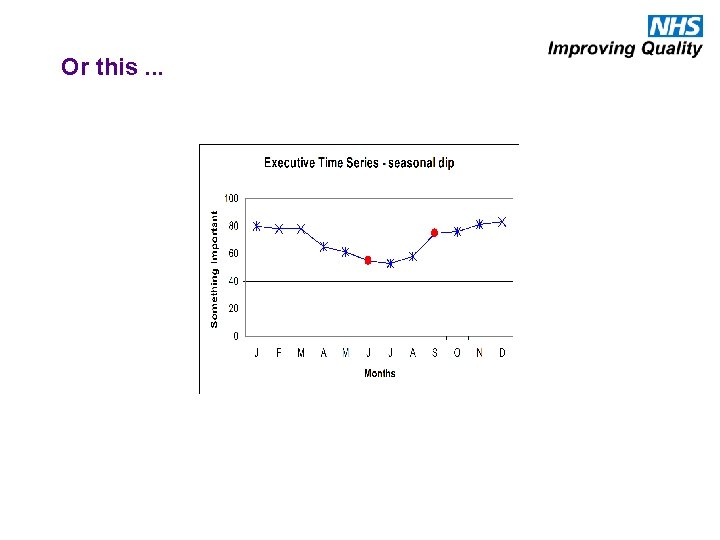
Or this. . .
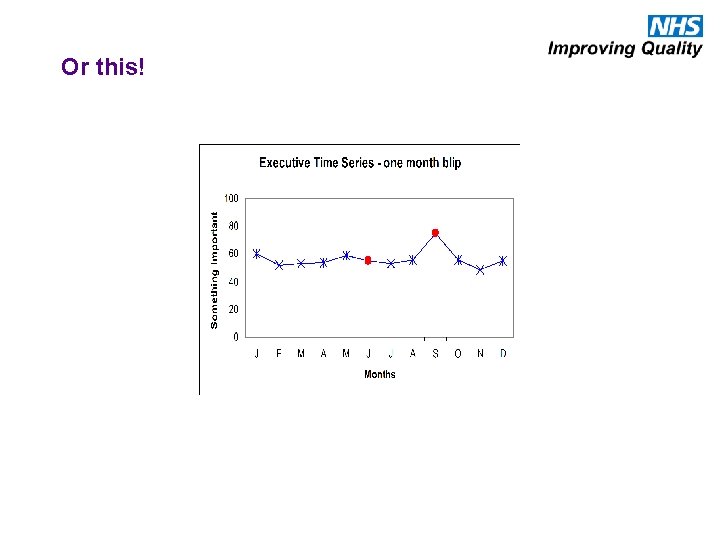
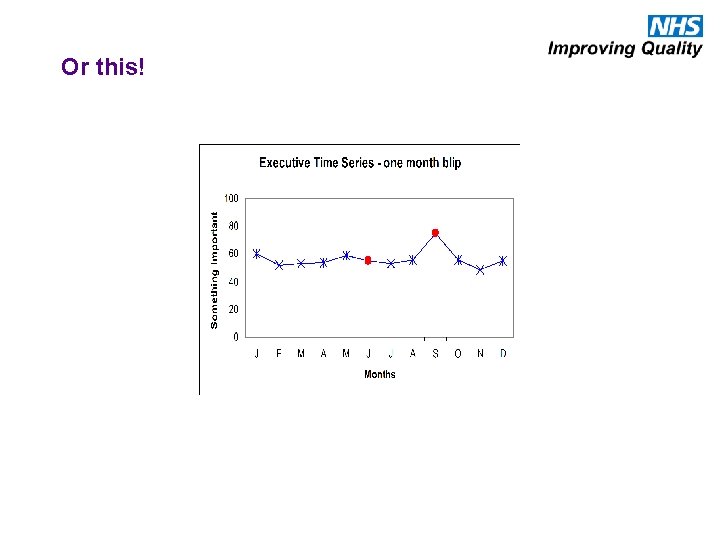
Or this!
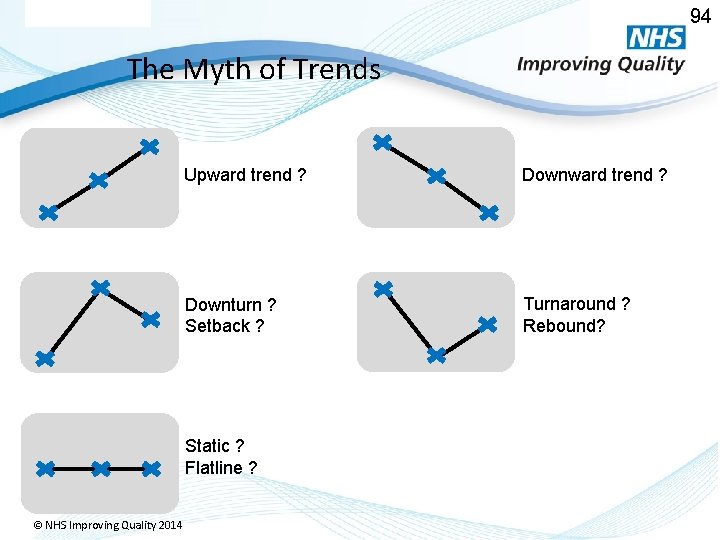
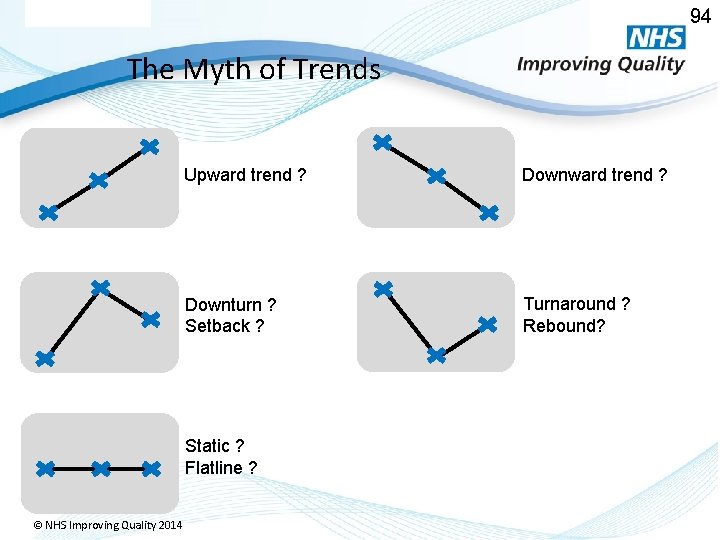
94 The Myth of Trends Upward trend ? Downturn ? Setback ? Turnaround ? Rebound? Static ? Flatline ? © NHS Improving Quality 2014
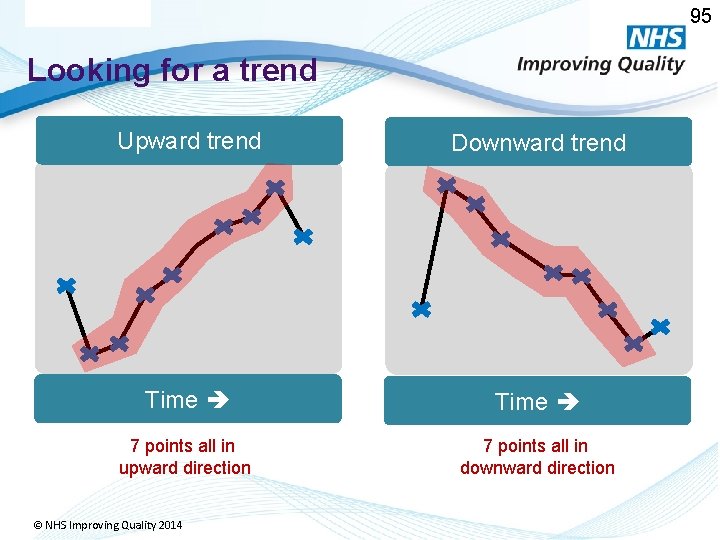
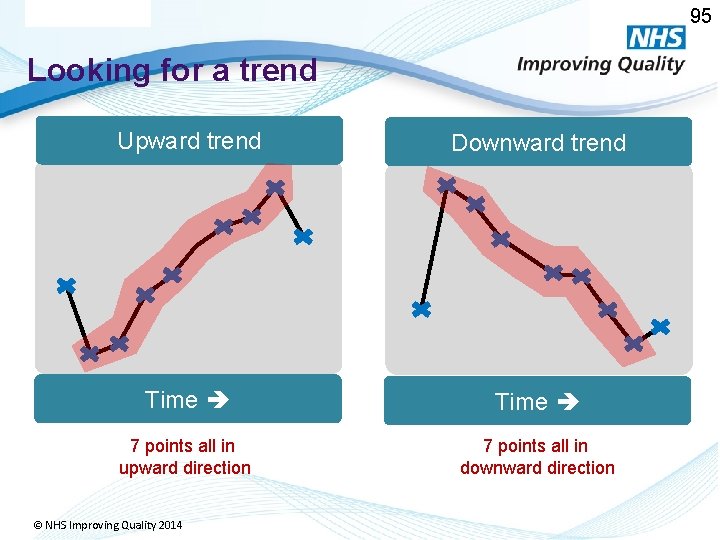
95 Looking for a trend Upward trend Downward trend Time 7 points all in upward direction 7 points all in downward direction © NHS Improving Quality 2014
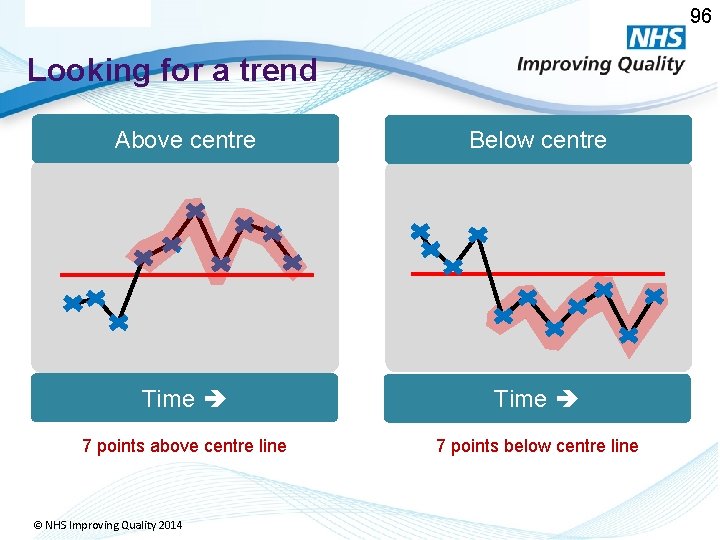
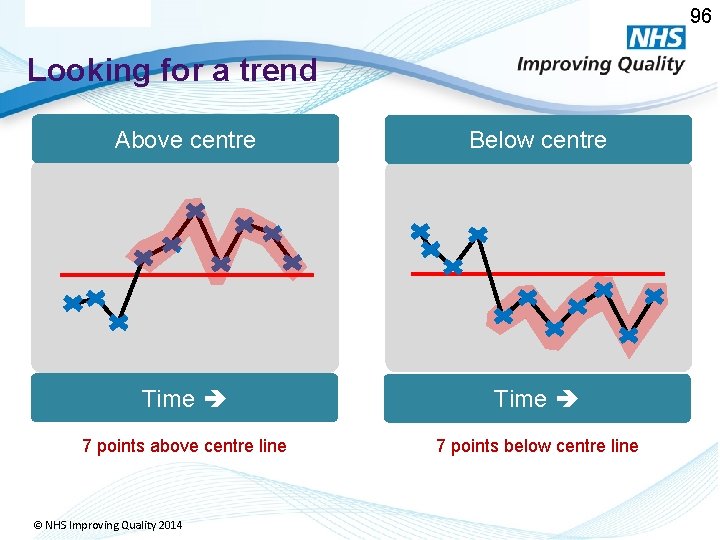
96 Looking for a trend Above centre Below centre Time 7 points above centre line 7 points below centre line © NHS Improving Quality 2014
QI Resources 108

Resources Available • BMJ Quality programme http: //quality. bmj. com/bigwins https: //www. youtube. com/user/Quality. BMJ • QI Resource website http: //www. vle. eastmidlandsdeanery. nhs. uk/cour se/view. php? id=934 • Each other • HEEM staff
QI Educational Leads • Dr Sue Cullis. APD scullis@nhs. net • Dr Susan Hadley. PD susan. hadley@nhs. net • Dr Christine Johnson. christine. johnson@nottingham. ac. uk • Dr Graham Todd todds@doctors. org. uk • Dr David Young davidj. young@nhs. net • Dr Helen Tallantyre helen. tallantyre@nhs. net
Some of the topics discussed… Lean technique, Six Sigma, PESTLE analysis, diffusion of innovation, audit, PDSA, SEA, RCA, process maps, fishbone or driver diagrams, logic models, variation, SPC, funnel plots, Swiss cheese model, Pareto principle Miller's pyramid.
Time to plan What small thing niggles you? What tools could you start using? Why? When? What are you going to change? Where? How will you measure it? Over what time scale? Who will you need to liaise with? What resources might you need? 112
What had over 100 posters, 75 abstracts, 2 keynote speakers, 4 workshops, 9 presentations, 6 award winning improvement projects and 350 delegates? HEEM Quality Improvement Forum 2015 �https: //www. youtube. com/watch? v=v. Dhfz. Q 0 Jk. FY �Happening again in 2016! �Come to present you QI project…. �…. and see others and get inspired!
Health Education East Midlands Quality Improvement Forum 2016 HEEMQIF 16 SAVE THE DATE! Health Education East Midlands are pleased to announce that the next Quality Improvement Forum will take place on 29 th June 2016 @ the Kube, Leicester Racecourse in Oadby, Leicester. Key HEEMQIF 16 activities for your diary: • Forum programme cascaded - w/c 14 th December 2015 • Call for Quality Improvement Projects Abstracts – w/c 4 th January 2016 • Call for bookings & workshop bookings open – w/c 4 th January 2016 • Abstract submissions close – w/c 28 th March 2016 • Bookings close – 31 st May 2016 • HEEMQIF 16 – 29 th June 2016 Join in the conversation on Twitter using @East. Mids. LETB #HEEMQIF 16 #loveourlearners
A Final Thought from Don Berwick “The most important single change in the NHS in response to this report would be for it to become…. a system devoted to continual learning and improvement of patient care, top to bottom and end to end. ” Don Berwick. A promise to learn - a commitment to act. August 2013.