KEY FEATURE PROBLEMS KFP A Arhami Dolatabadi Associated

KEY FEATURE PROBLEMS (KFP) A. Arhami Dolatabadi Associated Professor of Shahid Beheshti University of Medical sciences
OVERVIEW What are key feature problems Why use key features problems How do you write key features problems?
KEY FEATURES CONCEPT Introduced by Bordage and Page following a review and analysis by Norman et al (1985) of the research on the nature and assessment of CDM skills.
PROBLEM WITH PMP Although its high authenticity and face validity made it popular, it became clear that the PMP format had serious drawbacks. the reliability of the test was very low. In practical terms, this required many hours of testing in order to obtain a reliable result. the expected differences in performance between junior and experienced doctors were not found Scores on PMP tests correlated highly with scores on knowledge tests, suggesting that they added little additional measurement information
PROBLEM WITH PMP Key features problems are now used in a variety of testing situations. Medical Council of Canada uses a 4 -hour KFP, together with a 3. 5 -hour MCQ test. Royal Australian College of General Practitioners (RACGP) 3 -hour KFP paper, together with a 4 -hour written test and a 3 hour (OSCE). The American College of Physicians Self-Assessment Program for continuing medical education
WRITING KEY FEATURE PROBLEMS PROBLEM DEFINITION an undifferentiated complaint; a single typical problem; a multiple or multi‐system problem; a life‐threatening event; and preventive care and health promotion.
WRITING KEY FEATURE PROBLEMS SELECTING KEY FEATURES select a clinical problem (e. g. , shortness of breath on exertion) select an age group (e. g. , adult), select a clinical situation (e. g. , an undifferentiated complaint), address the question, Write lead in “What are the critical steps in the resolution of this problem for patients of this age group presenting in this way? ʺ
WRITING KEY FEATURE PROBLEMS DEVELOPING CASE SCENARIOS Case scenarios can vary considerably in length. in diagnostic work‐up , the scenario is often very brief. in laboratory or management issues, the scenario will typically be longer The usual elements common to any case scenario: age and gender the setting presenting condition or reason for seeking care, clinical details are required prior to the presentation of the first question.
WRITING KEY FEATURE PROBLEMS QUESTION FORMATS Two formats of questions are recommended for clinical decision‐making cases: short‐answer ʺwrite‐inʺ (WI) and examinees supply their responses ʺshort‐menuʺ (SM). examinees select their responses from prepared lists of options
WRITING KEY FEATURE PROBLEMS SCORING KEYS A scoring key consists of the list of the correct responses to a question and a system of assigning numerical scores to these keyed responses
EXAMPLES OF KFP Clinical Problem Third Trimester Bleeding Life Span Period Pregnancy neonatal/infant (up to 1 year) pediatric (1‐ 11 years) adolescence (12‐ 18 years) adult (19‐ 64 years) geriatric (over 65 years)
EXAMPLES OF KFP Clinical Situation undifferentiated complaint single typical problem multiple or multisystem problem life‐threatening event preventive care and health promotion
EXAMPLES OF KFP Location/Setting Emergency Department Patientʹs Age ‐ 20‐ 30 years Patientʹs ‐ Gender Female
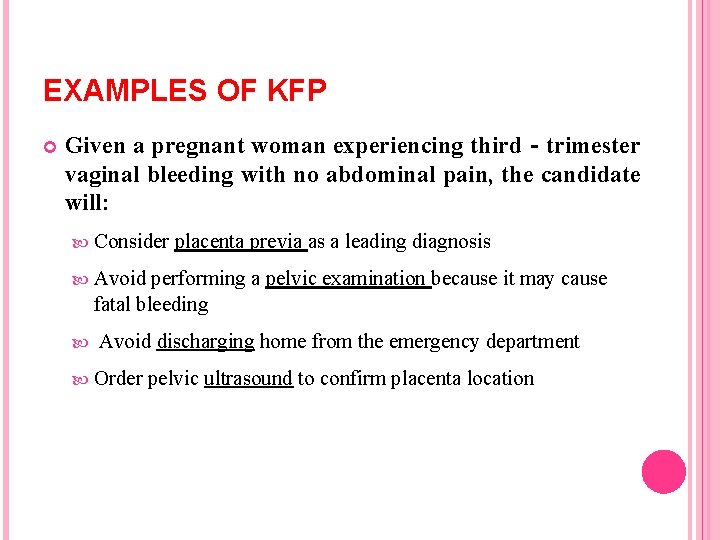
EXAMPLES OF KFP Given a pregnant woman experiencing third‐trimester vaginal bleeding with no abdominal pain, the candidate will: Consider placenta previa as a leading diagnosis Avoid performing a pelvic examination because it may cause fatal bleeding Avoid discharging home from the emergency department Order pelvic ultrasound to confirm placenta location
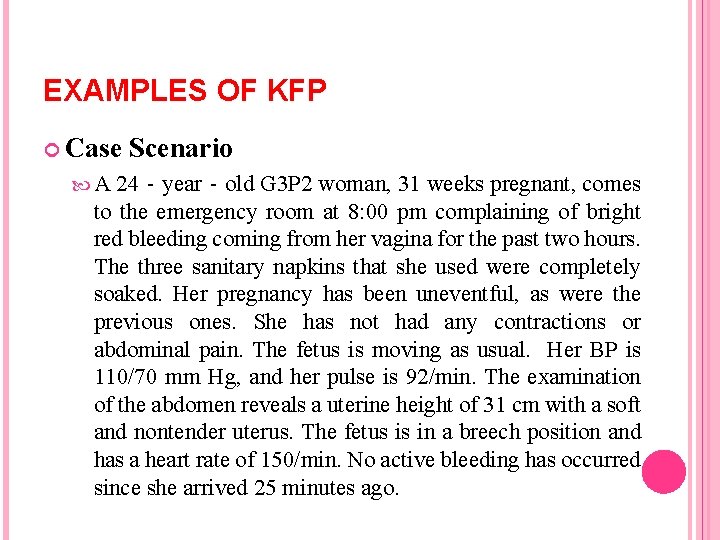
EXAMPLES OF KFP Case A Scenario 24‐year‐old G 3 P 2 woman, 31 weeks pregnant, comes to the emergency room at 8: 00 pm complaining of bright red bleeding coming from her vagina for the past two hours. The three sanitary napkins that she used were completely soaked. Her pregnancy has been uneventful, as were the previous ones. She has not had any contractions or abdominal pain. The fetus is moving as usual. Her BP is 110/70 mm Hg, and her pulse is 92/min. The examination of the abdomen reveals a uterine height of 31 cm with a soft and nontender uterus. The fetus is in a breech position and has a heart rate of 150/min. No active bleeding has occurred since she arrived 25 minutes ago.
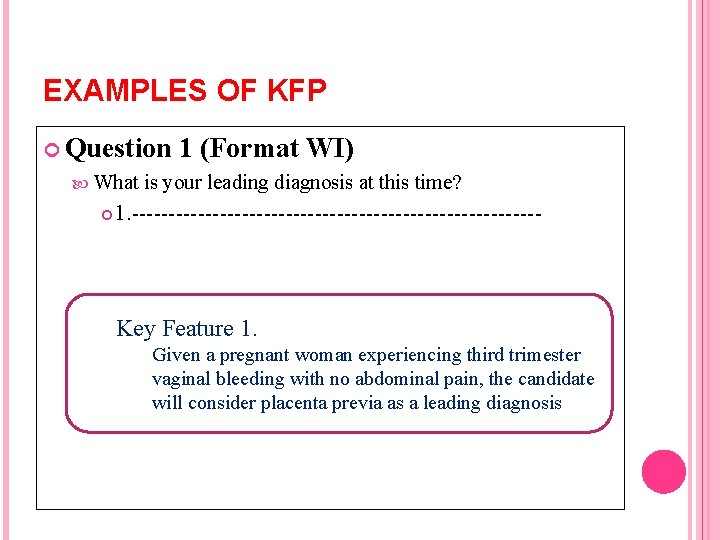
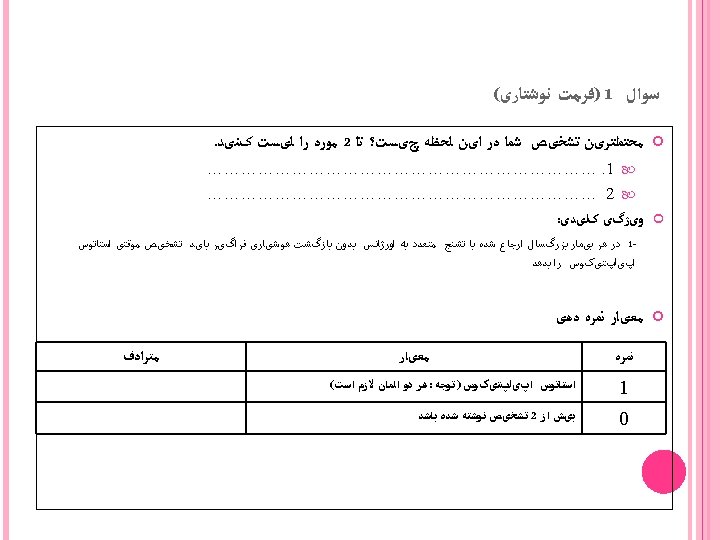
EXAMPLES OF KFP Question 1 (Format WI) What is your leading diagnosis at this time? 1. ---------------------------- Key Feature 1. Given a pregnant woman experiencing third trimester vaginal bleeding with no abdominal pain, the candidate will consider placenta previa as a leading diagnosis
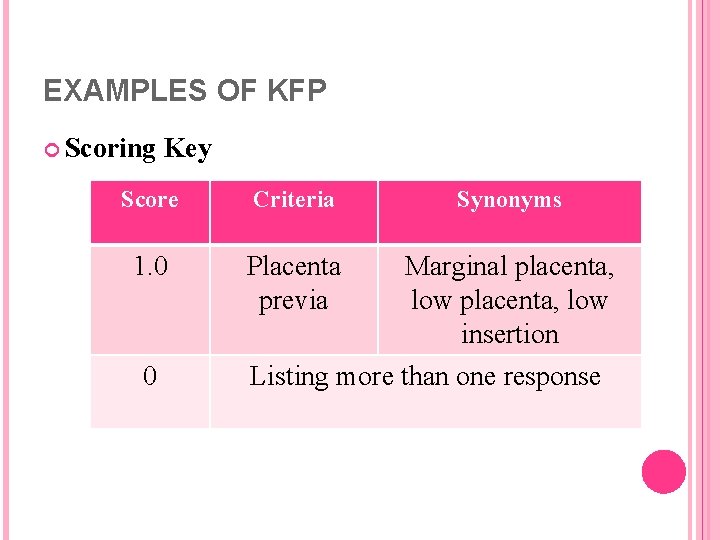
EXAMPLES OF KFP Scoring Key Score Criteria Synonyms 1. 0 Placenta previa Marginal placenta, low insertion 0 Listing more than one response
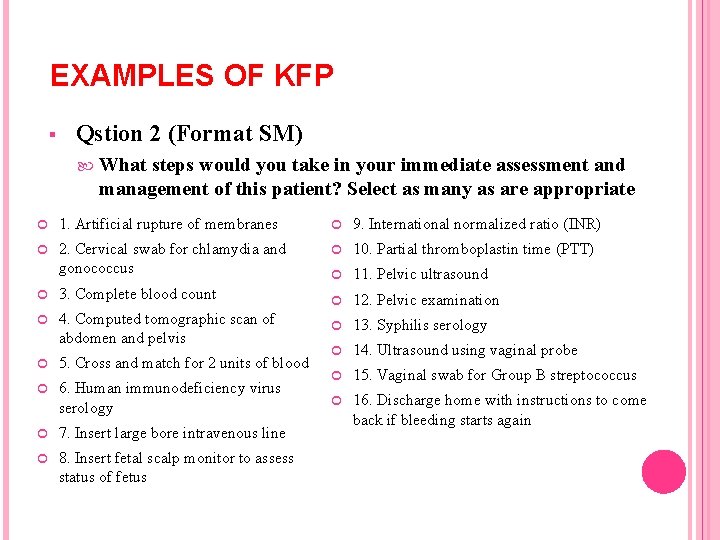
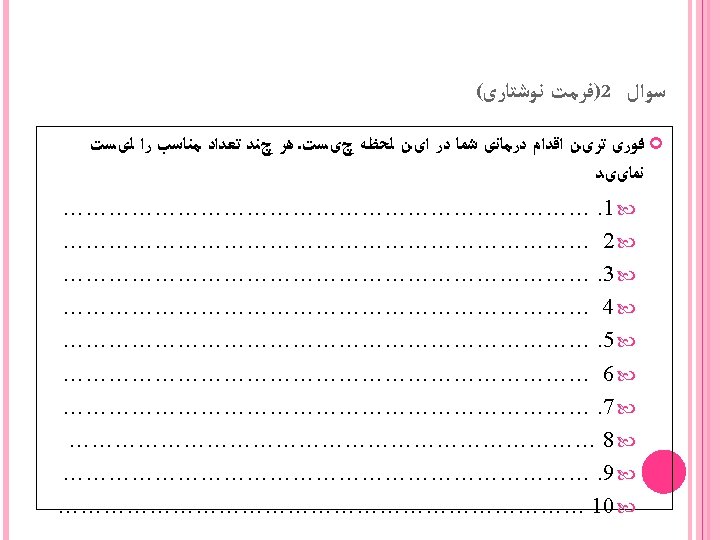
EXAMPLES OF KFP § Qstion 2 (Format SM) What steps would you take in your immediate assessment and management of this patient? Select as many as are appropriate 1. Artificial rupture of membranes 9. International normalized ratio (INR) 2. Cervical swab for chlamydia and gonococcus 10. Partial thromboplastin time (PTT) 11. Pelvic ultrasound 12. Pelvic examination 13. Syphilis serology 14. Ultrasound using vaginal probe 15. Vaginal swab for Group B streptococcus 16. Discharge home with instructions to come back if bleeding starts again 3. Complete blood count 4. Computed tomographic scan of abdomen and pelvis 5. Cross and match for 2 units of blood 6. Human immunodeficiency virus serology 7. Insert large bore intravenous line 8. Insert fetal scalp monitor to assess status of fetus
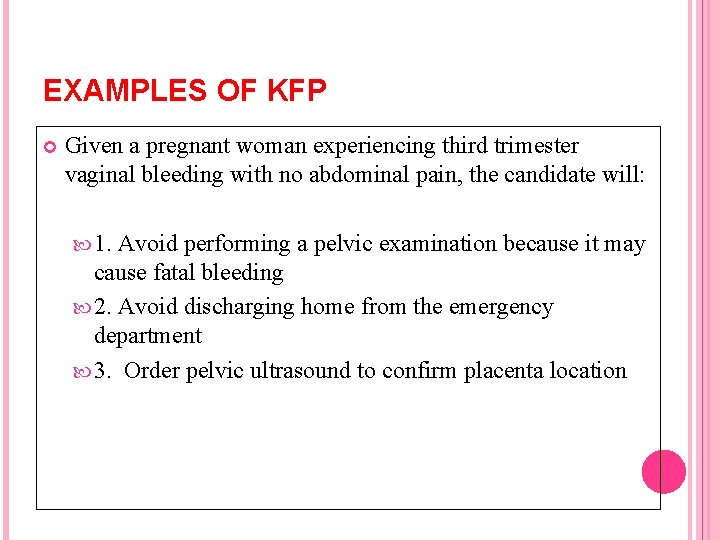
EXAMPLES OF KFP Given a pregnant woman experiencing third trimester vaginal bleeding with no abdominal pain, the candidate will: 1. Avoid performing a pelvic examination because it may cause fatal bleeding 2. Avoid discharging home from the emergency department 3. Order pelvic ultrasound to confirm placenta location
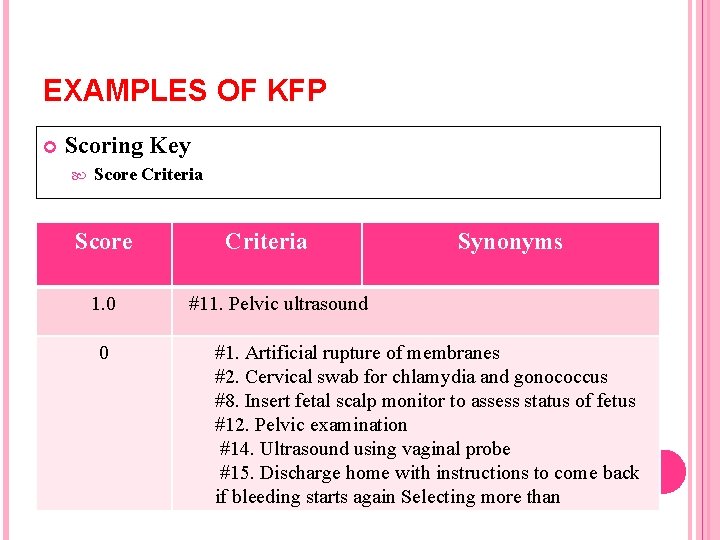
EXAMPLES OF KFP Scoring Key Score Criteria Score 1. 0 0 Criteria Synonyms #11. Pelvic ultrasound #1. Artificial rupture of membranes #2. Cervical swab for chlamydia and gonococcus #8. Insert fetal scalp monitor to assess status of fetus #12. Pelvic examination #14. Ultrasound using vaginal probe #15. Discharge home with instructions to come back if bleeding starts again Selecting more than



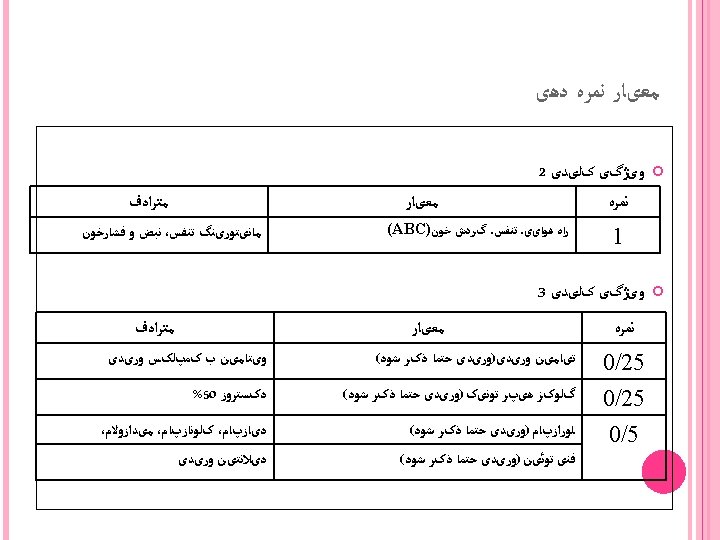
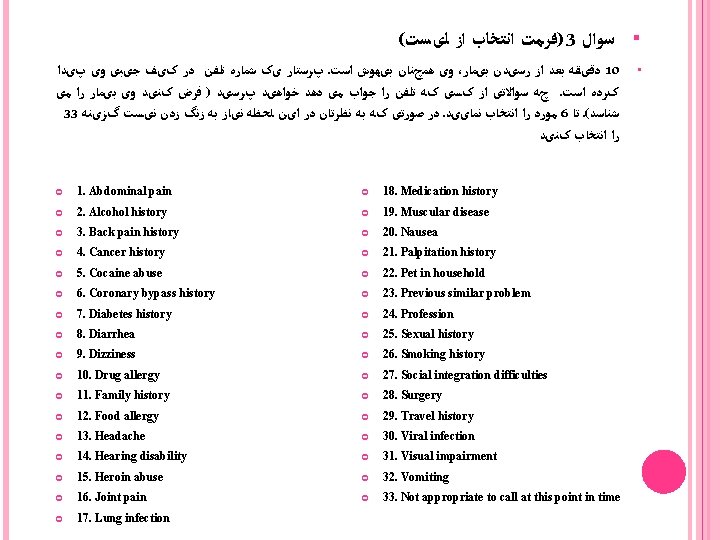
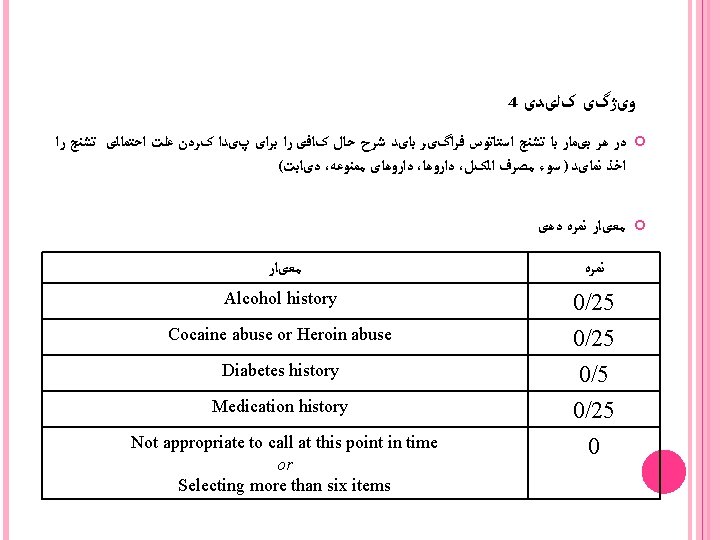
( )ﻓﺮﻣﺖ ﺍﻧﺘﺨﺎﺏ ﺍﺯ ﻟیﺴﺖ 3 ﺳﻮﺍﻝ پﺮﺳﺘﺎﺭ یک ﺷﻤﺎﺭﻩ ﺗﻠﻔﻦ ﺩﺭ کیﻒ ﺟیﺒی ﻭی پیﺪﺍ. ﻭی ﻫﻤچﻨﺎﻥ ﺑیﻬﻮﺵ ﺍﺳﺖ ، ﺩﻗیﻘﻪ ﺑﻌﺪ ﺍﺯ ﺭﺳیﺪﻥ ﺑیﻤﺎﺭ 10 چﻪ ﺳﻮﺍﻻﺗی ﺍﺯ کﺴی کﻪ ﺗﻠﻔﻦ ﺭﺍ ﺟﻮﺍﺏ ﻣی ﺩﻫﺪ ﺧﻮﺍﻫیﺪ پﺮﺳیﺪ ) ﻓﺮﺽ کﻨیﺪ ﻭی ﺑیﻤﺎﺭ ﺭﺍ ﻣی. کﺮﺩﻩ ﺍﺳﺖ 33 ﺩﺭ ﺻﻮﺭﺗی کﻪ ﺑﻪ ﻧﻈﺮﺗﺎﻥ ﺩﺭ ﺍیﻦ ﻟﺤﻈﻪ ﻧیﺎﺯ ﺑﻪ ﺯﻧگ ﺯﺩﻥ ﻧیﺴﺖ گﺰیﻨﻪ. ﻣﻮﺭﺩ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎییﺪ 6 ﺗﺎ. ( ﺷﻨﺎﺳﺪ ﺭﺍ ﺍﻧﺘﺨﺎﺏ کﻨیﺪ 1. Abdominal pain 18. Medication history 2. Alcohol history 19. Muscular disease 3. Back pain history 20. Nausea 4. Cancer history 21. Palpitation history 5. Cocaine abuse 22. Pet in household 6. Coronary bypass history 23. Previous similar problem 7. Diabetes history 24. Profession 8. Diarrhea 25. Sexual history 9. Dizziness 26. Smoking history 10. Drug allergy 27. Social integration difficulties 11. Family history 28. Surgery 12. Food allergy 29. Travel history 13. Headache 30. Viral infection 14. Hearing disability 31. Visual impairment 15. Heroin abuse 32. Vomiting 16. Joint pain 33. Not appropriate to call at this point in time 17. Lung infection § •
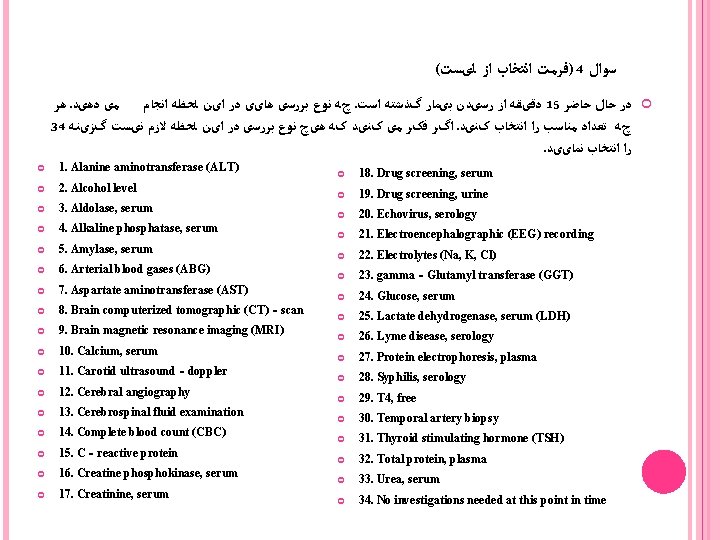
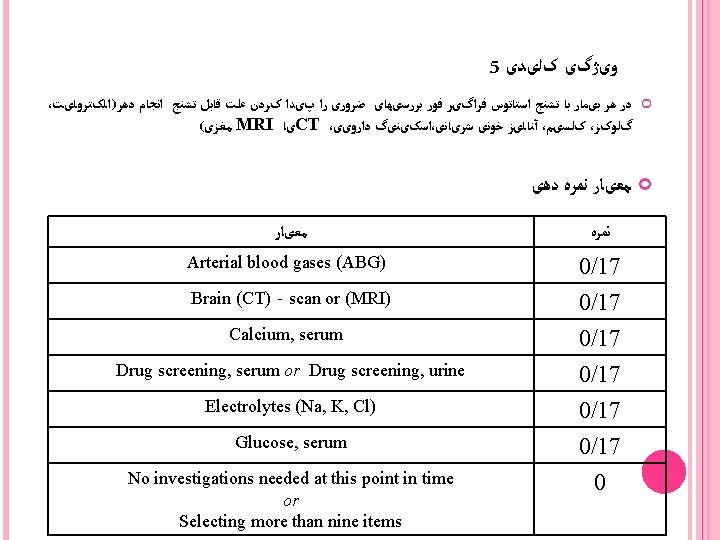
( )ﻓﺮﻣﺖ ﺍﻧﺘﺨﺎﺏ ﺍﺯ ﻟیﺴﺖ 4 ﺳﻮﺍﻝ ﻫﺮ. چﻪ ﻧﻮﻉ ﺑﺮﺭﺳی ﻫﺎیی ﺩﺭ ﺍیﻦ ﻟﺤﻈﻪ ﺍﻧﺠﺎﻡ ﻣی ﺩﻫیﺪ. ﺩﻗیﻘﻪ ﺍﺯ ﺭﺳیﺪﻥ ﺑیﻤﺎﺭ گﺬﺷﺘﻪ ﺍﺳﺖ 15 ﺩﺭ ﺣﺎﻝ ﺣﺎﺿﺮ 34 ﺍگﺮ ﻓکﺮ ﻣی کﻨیﺪ کﻪ ﻫیچ ﻧﻮﻉ ﺑﺮﺭﺳی ﺩﺭ ﺍیﻦ ﻟﺤﻈﻪ ﻻﺯﻡ ﻧیﺴﺖ گﺰیﻨﻪ. چﻪ ﺗﻌﺪﺍﺩ ﻣﻨﺎﺳﺐ ﺭﺍ ﺍﻧﺘﺨﺎﺏ کﻨیﺪ . ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎییﺪ 1. Alanine aminotransferase (ALT) 2. Alcohol level 3. Aldolase, serum 4. Alkaline phosphatase, serum 5. Amylase, serum 6. Arterial blood gases (ABG) 7. Aspartate aminotransferase (AST) 8. Brain computerized tomographic (CT)‐scan 9. Brain magnetic resonance imaging (MRI) 10. Calcium, serum 11. Carotid ultrasound‐doppler 12. Cerebral angiography 13. Cerebrospinal fluid examination 14. Complete blood count (CBC) 15. C‐reactive protein 16. Creatine phosphokinase, serum 17. Creatinine, serum 18. Drug screening, serum 19. Drug screening, urine 20. Echovirus, serology 21. Electroencephalographic (EEG) recording 22. Electrolytes (Na, K, Cl) 23. gamma‐Glutamyl transferase (GGT) 24. Glucose, serum 25. Lactate dehydrogenase, serum (LDH) 26. Lyme disease, serology 27. Protein electrophoresis, plasma 28. Syphilis, serology 29. T 4, free 30. Temporal artery biopsy 31. Thyroid stimulating hormone (TSH) 32. Total protein, plasma 33. Urea, serum 34. No investigations needed at this point in time
Thank You ! Any Question ?
- Slides: 34