Ketamine Facilitator Barbara Bischoff BSN RN Case Study

Ketamine • Facilitator: Barbara Bischoff, BSN, RN
Case Study • A 51 year old woman presents to ED with right shoulder pain 11/25/14 • Stage 4 Breast Cancer • Carcinoma of breast/Cellulitis • History of left side Mastectomy • Port to left side of chest wall • Pt weight 70 kilograms
Case Study (continued) Initial Medications • Duragesic Patch 100 mcg/hr (Fentynal) 1 patch Q 72 hr • Hydrocodone (APAP) 5 mg/325 mg (Norco) 1 tab PO Q 6 hr PRN • Morphine Sulfate (MS Contin) 60 mg tab PO Q 12 hr • Miralax 17 gm 1 time daily PO • Ondansetron (Zophran) 8 mg tab PO Q 6 hr
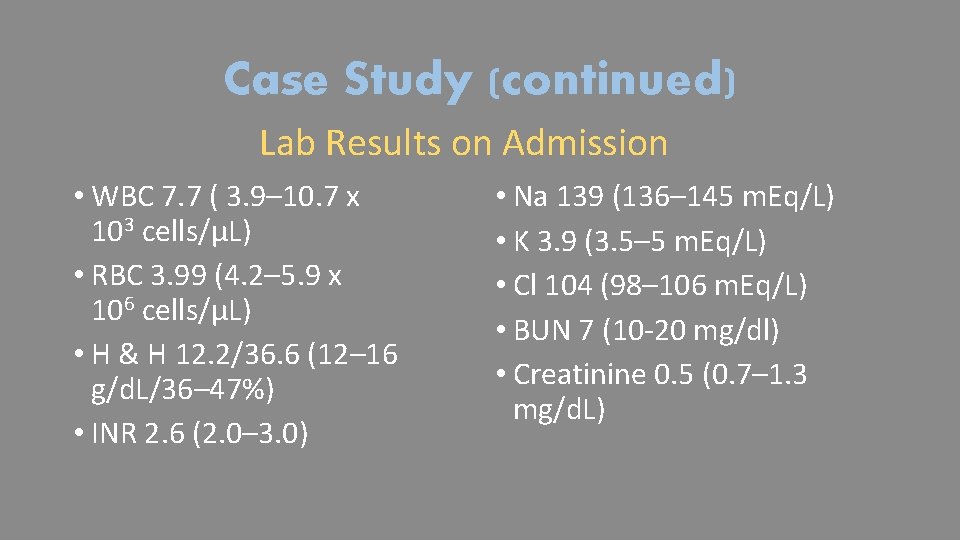
Case Study (continued) Lab Results on Admission • WBC 7. 7 ( 3. 9– 10. 7 x 103 cells/μL) • RBC 3. 99 (4. 2– 5. 9 x 106 cells/μL) • H & H 12. 2/36. 6 (12– 16 g/d. L/36– 47%) • INR 2. 6 (2. 0– 3. 0) • Na 139 (136– 145 m. Eq/L) • K 3. 9 (3. 5– 5 m. Eq/L) • Cl 104 (98– 106 m. Eq/L) • BUN 7 (10 -20 mg/dl) • Creatinine 0. 5 (0. 7– 1. 3 mg/d. L)
Case Study (continued) • Patient on Maria Hall 11/25/15 -12/2/15 • Patient placed in Palliative Care • Patient transferred from Maria Hall to ICU @1300 12/2/15 • Continuous monitoring • Pain management with ketamine drip • Ketamine bolus 10 mg with doctor at bedside • Ketamine drip initiated Ketamine 12 mg/Dilaudid 10 mg/hr
Ketamine • • • Pain Management Mechanism of Action Clinical Effects Therapeutic Administration Use as an analgesic in palliative care (FDA, 2014; Micromedex, 2015)
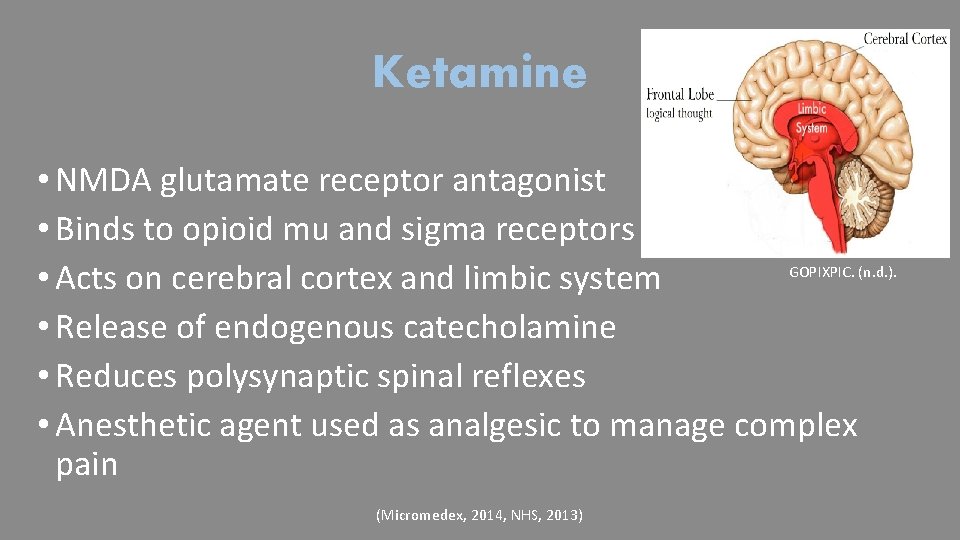
Ketamine • NMDA glutamate receptor antagonist • Binds to opioid mu and sigma receptors GOPIXPIC. (n. d. ). • Acts on cerebral cortex and limbic system • Release of endogenous catecholamine • Reduces polysynaptic spinal reflexes • Anesthetic agent used as analgesic to manage complex pain (Micromedex, 2014, NHS, 2013)
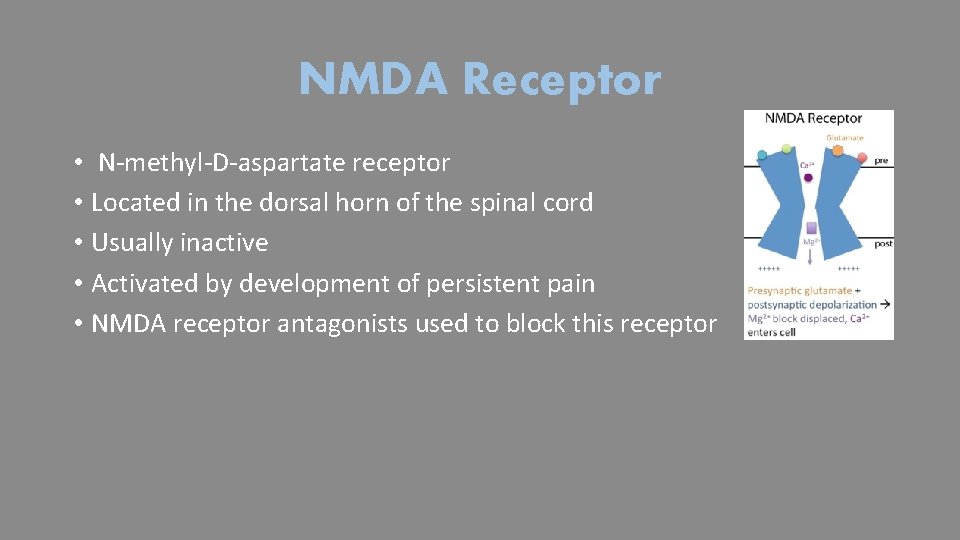
NMDA Receptor • N-methyl-D-aspartate receptor • Located in the dorsal horn of the spinal cord • Usually inactive • Activated by development of persistent pain • NMDA receptor antagonists used to block this receptor
Problem Description • Increasing number of opioid tolerant patients. • High Tolerance • Usual multimodal regimen: • Opioids • Non-opioids • NSAIDs • Gabapentanoids • Muscle Relaxers • May not manage pain. (Colfer, Wolo & Viscusi, 2013).
Goals of Acute Pain Management in Opioid Tolerant Patients • Identify at-risk population • Prevent withdrawal symptoms/complications • Effective analgesic treatment in acute pain • Treatment of psychological disorders • Rehabilitation to maintenance therapy (Bourne, 2010)
Opioid-tolerant patients in practice • Three main groups of opioid-tolerant patients : • Patients with cancer pain • Patients with chronic non-cancer pain • Patients with current addiction to opioid drugs • Patients on a maintenance drug program (ANZCA, 2010)
Opioids Alone • Compromise patient safety • Cause side effects • Nausea • Vomiting • Dependence • Respiratory Depression (Colfer, Wolo & Viscusi, 2013)
Chronic Wounds/Chronic Pain • A wound that fails to heal within 3 months. • Social, psychological, physical and economic cost • Consequences: • Severe impairment of quality of life • Restriction of daily activity • Emotional distress • Lengthy treatment • High treatment expense (Frykberg, 2011; Werdin et al. , 2009; Ruttermann et al. , 2013)
Position Statement Pain Management • American Society for Pain Management Nursing • Nurses must advocate for optimal • Pain management • Symptom relief • A meta-analysis • 52 studies • Spanning 40 years • Found 64% of advanced cancer patients have pain (Reynolds, Drew & Dunwoody, 2013, Colfer, Wolo & Viscusi, 2013)
Policy Statement • Oral or IV Ketamine will be initiated upon order from a physician via CPOE. • First 24 hours or TBD by MD • Administered by nurses in critical care • Follow standing order set (NHS, 2013; Zittel, 2011)
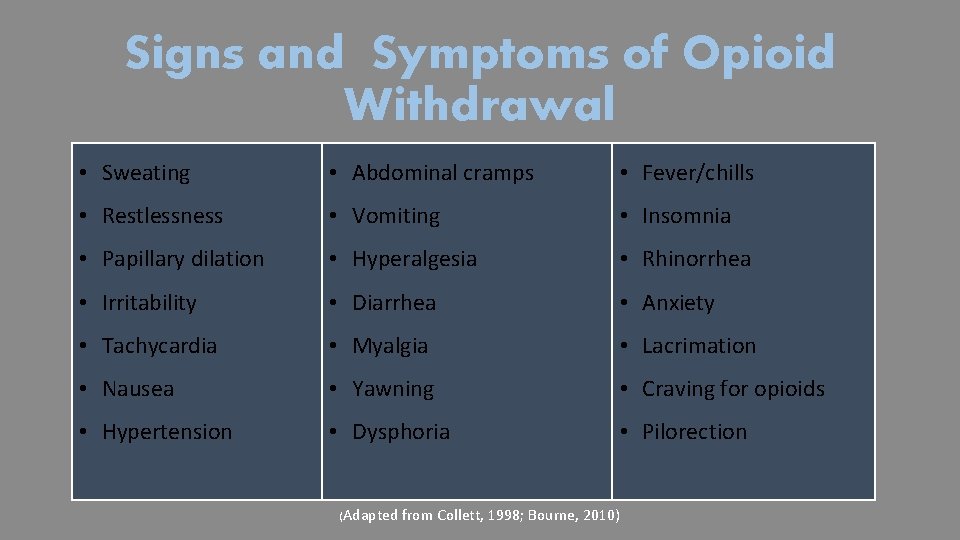
Signs and Symptoms of Opioid Withdrawal • Sweating • Abdominal cramps • Fever/chills • Restlessness • Vomiting • Insomnia • Papillary dilation • Hyperalgesia • Rhinorrhea • Irritability • Diarrhea • Anxiety • Tachycardia • Myalgia • Lacrimation • Nausea • Yawning • Craving for opioids • Hypertension • Dysphoria • Pilorection (Adapted from Collett, 1998; Bourne, 2010)
Process • Patient specific order • Infusions prepared by pharmacy • Infuse through dedicated line via most proximal port • Use portless IV tubing • No bolus without anesthesia provider (Zittel, 2011; DRE, 2015)
Low-dose Ketamine Defined • Bolus < 2 mg/kg intramuscular administration • Bolus < 1 mg/kg intravenous administration • Continuous IV is < or = 20 microg/kg per min (Schmidt, Sandler & Katz, 1999)
Administration • Initial ketamine concurrent with opioid. • Monitor for sedation or confusion • If drowsy notify MD • Ketamine side effects (patient not drowsy): • Hallucinations or dysphoria • Administer as ordered by MD: • Haloperidol • Midazolam (NHS, 2013)
Administration Process Dosing By Pharmacy • Prepare new syringe every 24 hours. • Dilute ketamine with sodium chloride 0. 9%. • Check: Syringe is not cloudy • Protect it from light. • Check: Stability and compatibility. • Rotate SC infusion site daily. (NHS. , 2013)
Monitor • Vital signs • Alertness • Orientation • Evidence of: • Nystagmus • Bad dreams • Unpleasant hallucinations. (Zittel, 2011)
Report • Heart rate > 100 beats per minute • Systolic B/P < 90 mm. Hg • Respiratory < 10 breaths per minute • Oxygen saturation of < 93% • Emergence reaction symptoms: • Bad dream • Hallucinations • Nystagmus (Zittel, 2011)
Onset and Duration • Rapid Onset: • IV within 30 seconds • Half-life: • 10 -15 min (Alpha phase) • > 2. 5 h (Beta phase) • IM within 3 -4 minutes. • Duration: • IV 2 mg/kg lasts 5 -10 minutes • IM 9 to 13 mg/kg lasts 12 -25 minutes (SEMAC, Micromedex, 2015)
Common Side Effects • Dizziness • Tachycardia • Altered mental status • Anxiety • Palpitations • Slurred speech • Hallucinations • Nystagmus • Mydriasis • Muscular hypertonus • Trismus • Psychomotor reactions • Psychomimetic reactions • Emergence delirium • Hypertension • Chest Pain
Converting from IV to Oral Ketamine • Oral ketamine is more potent than IV ketamine • Dose reduction with change • Prescribed in divided doses - four times daily • Titrated in 5 -10 mg increments per order • IV infusion may be stopped with the first dose • Or gradually reduced with increase of oral infusion. (NHS. , 2013)
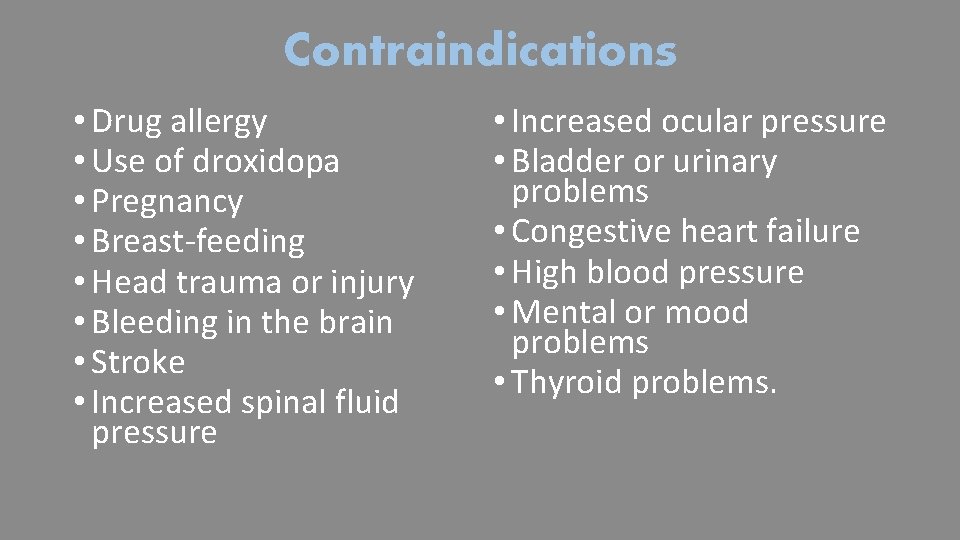
Contraindications • Drug allergy • Use of droxidopa • Pregnancy • Breast-feeding • Head trauma or injury • Bleeding in the brain • Stroke • Increased spinal fluid pressure • Increased ocular pressure • Bladder or urinary problems • Congestive heart failure • High blood pressure • Mental or mood problems • Thyroid problems.
Pain Management Resource Sites • American Society of Regional Anesthesia and Pain Management • • http: //www. asra. com/ • American Society for Pain Management • • http: //www. aspmn. org/ • American Society of Anesthesiologists • • http: //www. asahq. org/ • Food and Drug Administration • • http: //www. fda. gov/Drugs/ • Anesthesia Patient Safety Foundation • • Colfer, Wolo & Viscusi, 2013). http: //www. apsf. org/ (
Thank you for your Time Questions? Comments?
References • ANZCA (Australian and New Zealand College of Anesthetists, Faculty of Pain Medicine). (2010). Acute Pain Management: Scientific Evidence (3 rd ed. ). Melbourne, Victoria, Australia. ANZCA. • Bourne, N. (2010). Acute pain management in the opioid-tolerant patient. Nursing Standard. 25, 12, 35 -39. • Chin, M. L. (2014). Multimodal analgesia: Role of non opioid analgesics. American Society of Regional Anesthesia and Pain. Retrieved from https: //www. asra. com/painresource/article/35/multimodal-analgesia-role-of-non-opioid-analgesics • Colfer, K. , Wolo, E. & Viscusi, E. R. (2013). Acute pain management: Current trends, technologies, and new agents. Journal of Legal Nurse Consulting, 24(1), 11 -19. • Collett, B. J. (1998). Opioid tolerance: the clinical perspective. British Journal of Anaesthesia, 81(1), 58 -68. • Dickenson, A. H. (1997). NMDA receptor antagonists: Interactions with opioids. Acta Anaethesiologica Scandinavica, 41(1), 112 -115.
References (Cont) • Drugs. com. (2015). Droxidopa. Retrieved from http: //www. drugs. com/mtm/droxidopa. html • FDA (U. S Food and Drug Administration). (2014). "Off-Label" and investigational use Of marketed drugs, biologics, and medical devices - information sheet guidance for institutional review boards and clinical investigators. Retrieved from http: //www. fda. gov/regulatoryinformation/guidances/ucm 126486. htm • Frykberg, R. G. (2011). The science of advanced wound care: What should you be using in your office? Podiatry Today Supplement: Emerging evidence on advanced wound care for diabetic foot ulcerations. HMP Communications, LLC (HMP), 1 -3, 815. • GOPIXPIC. (n. d. ). Cerebral cortex. Limbic system. Image retrieved from http: //www. gopixpic. com/limbic-system-not/ • Loftus, R. W. , Yeager, M. P. , Clark, J. A. , Brown, J. R. , Abdu, W. A. , Sengupta, D. K. & Beach, M. L. (2010). Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. Anesthesiology, 113(3), 639 -646. doi: 10. 1097/ALN. 0 b 013 e 3181 e 90914.
References (Cont) • Medtronic. (2014). Common Types of chronic pain. Retrieved from http: //www. medtronicneuro. com. au/chronic_pain_commontypes. html • Micromedex. (2014). Ketamine Hydrochloride. Drug. Point Summery. Retrieved from http: //www. micromedexsolutions. com/micromedex 2/librarian/PFDefault. Action. I d/evidence • NHS. (2013). Ketamine in palliative care. Lothian. • Reynolds, J. , Drew, D. & Dunwoody, C. 2013. American Society for Pain Management Nursing Position Statement: Pain Management at the End of Life. • Ruttermann M. , Maier-Hasselmann, A. , Nink-Grebe, B. & Burckhardt, M. (2013). Clinical practice guideline: Local treatment of chronic wounds in patients with peripheral vascular disease, chronic venous insufficiency, and diabetes. Dtsch Arztebl Int; 110(3): 25– 31. DOI: 10. 3238/arztebl. 2013. 0025
References (Cont) • Schmid, R. L. , Sandler, A. N. & Katz, J. (1999). Use and efficacy of low-dose ketamine in the management of acute postoperative pain: a review of current techniques and outcomes. Pain, 82(2), 111 -125. Retrieved from http: //www. ncbi. nlm. nih. gov/pubmed/10467917 • SEMAC (State Emergency Medical Advisory Committee). (n. d. ). Ketamine. Drug Formulary. Retrieved from https: //www. health. ny. gov/professionals/ems/pdf/ketamine_formulary • Sigma-Aldrich. (2015). S-(+)-Ketamine hydrochloride. Picture retrieved from http: //www. sigmaaldrich. com/catalog/product/sigma/k 1884? lang=en® ion=US • Werdin, F. , Tennenhaus, M. , Schaller, H. E. & Rennekampff, H. O. (2009). Evidence-based Management Strategies for Treatment of Chronic Wounds. Open Access Journal of Plastic Surgery, 9(19), 169 -179.
- Slides: 32