Ka SAPI Extending Phil Healths Coverage to Workers






- Slides: 36
Ka. SAPI Extending Phil. Health’s Coverage to Workers in the Informal Economy Philippines Annie A. Asanza, MD 1

Context 2
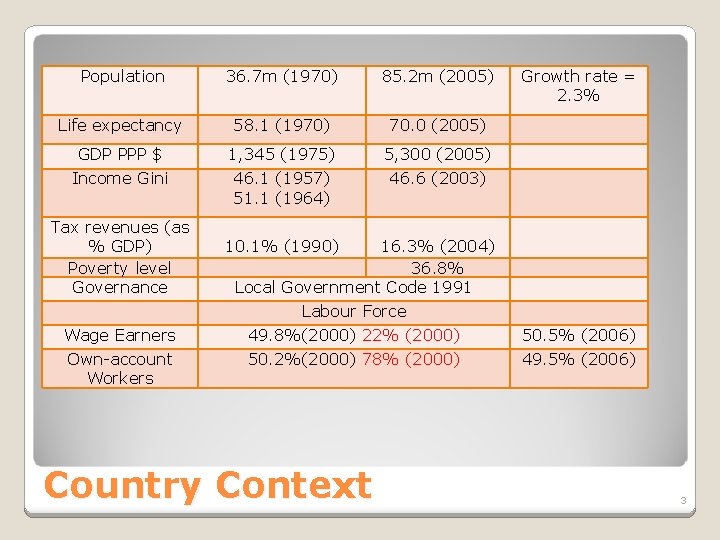
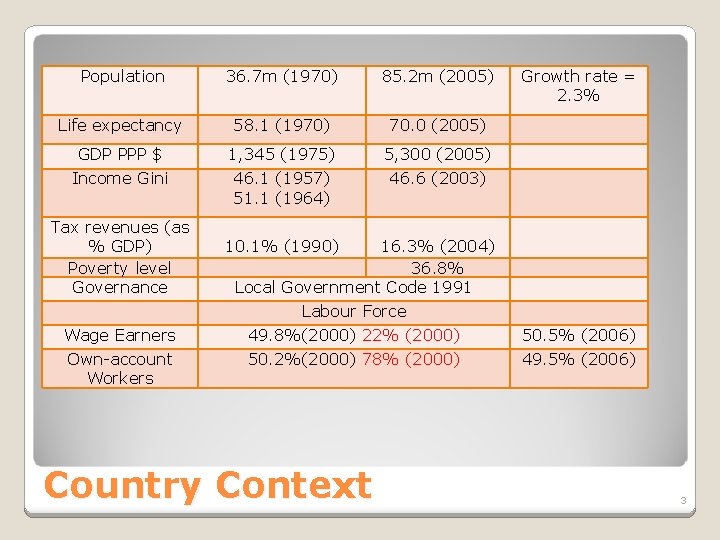
Population 36. 7 m (1970) 85. 2 m (2005) Life expectancy 58. 1 (1970) 70. 0 (2005) GDP PPP $ 1, 345 (1975) 5, 300 (2005) Income Gini 46. 1 (1957) 51. 1 (1964) 46. 6 (2003) Tax revenues (as % GDP) Poverty level Governance Wage Earners Own-account Workers Growth rate = 2. 3% 10. 1% (1990) 16. 3% (2004) 36. 8% Local Government Code 1991 Labour Force 49. 8%(2000) 22% (2000) 50. 2%(2000) 78% (2000) Country Context 50. 5% (2006) 49. 5% (2006) 3
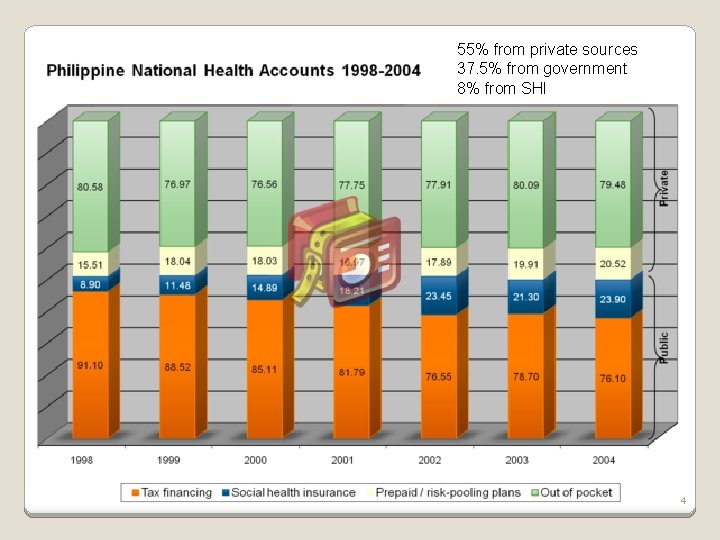
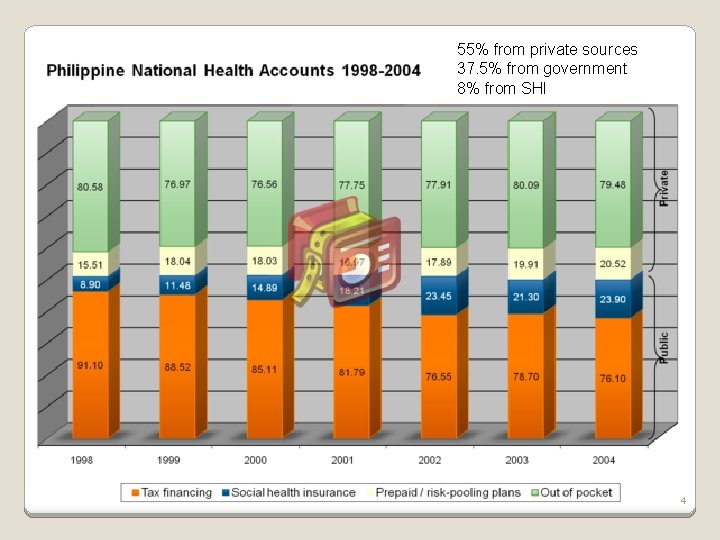
55% from private sources 37. 5% from government 8% from SHI 4
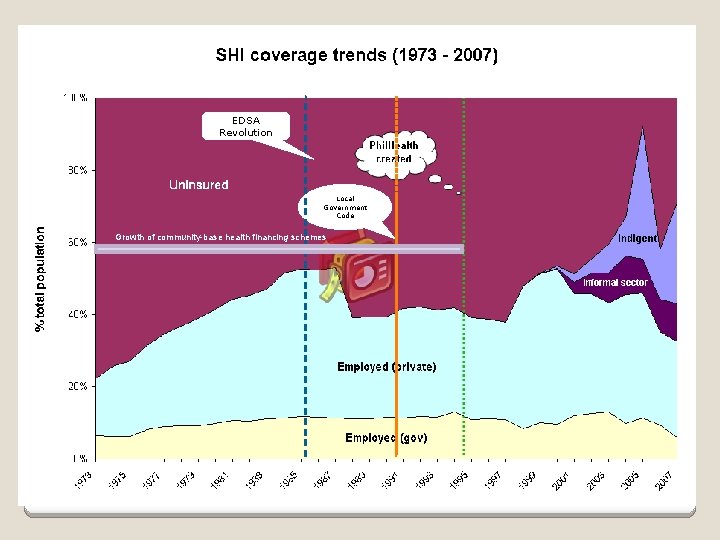
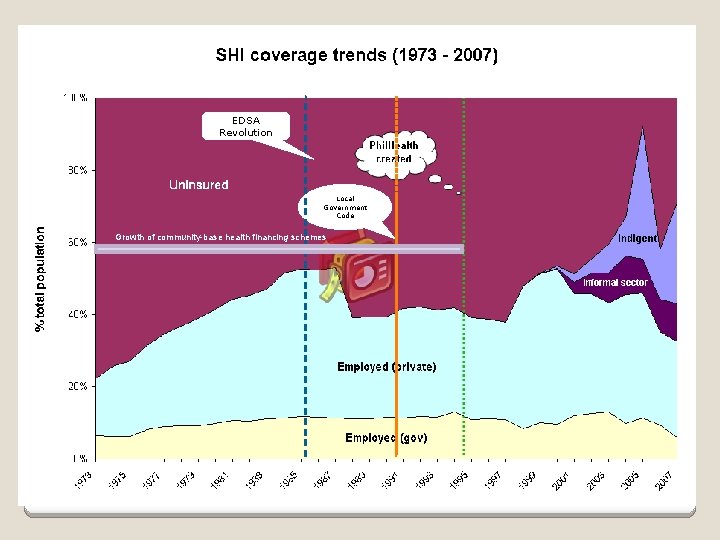
EDSA Revolution Local Government Code Growth of community-base health financing schemes 5
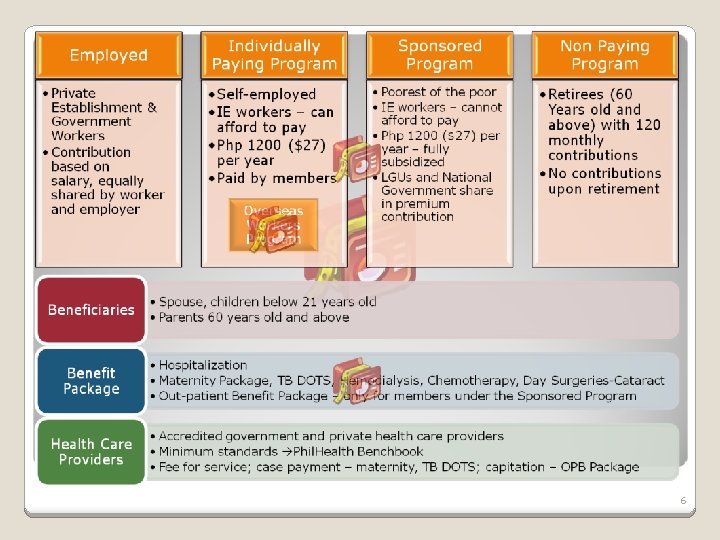
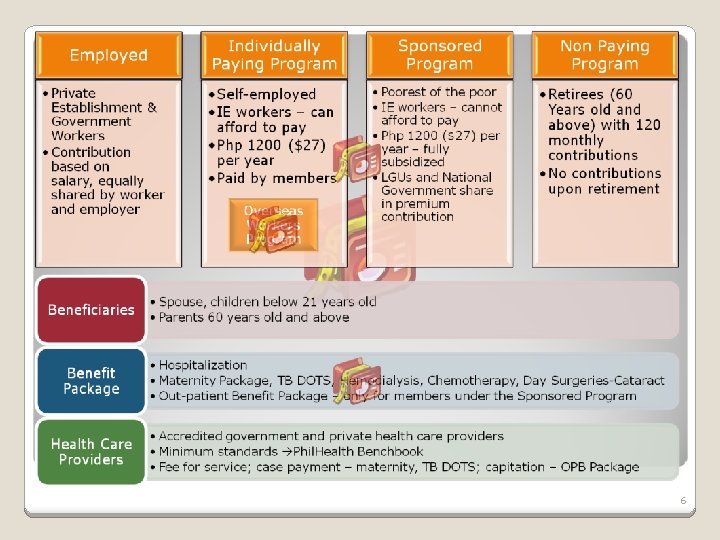
6
Ka. SAPI 7
Year 2003 low coverage of informal economy workers through the Individually Paying Program Phil. Health embarked on a tie-up with small credit cooperatives for enrollment of their members Tested with 11 cooperatives in 2 regions Cooperatives were evaluated based on financial indicators used for cooperatives by the Department of Finance allowing them to perform functions i. e. marketing, collection based on their classification Cooperatives gets an incentive for every new member and amount remitted to Phil. Health Organized Group Interface (POGI) 8
Cooperatives used loans to pay for Phil. Health premiums high default rate High administrative cost for partner organization groups Not attractive enough high out of pocket spending due to expensive medicines & unregulated practice of health care providers Low awareness on health insurance increase advocacy on its advatages and benefits Strengthen Phil. Health’s administrative capacity ILO-GTZ-WHO Evaluation of POGI March 2005 9
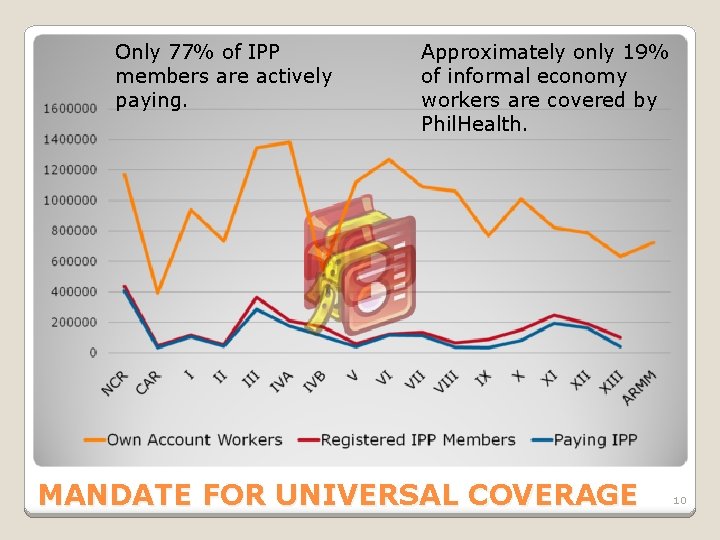
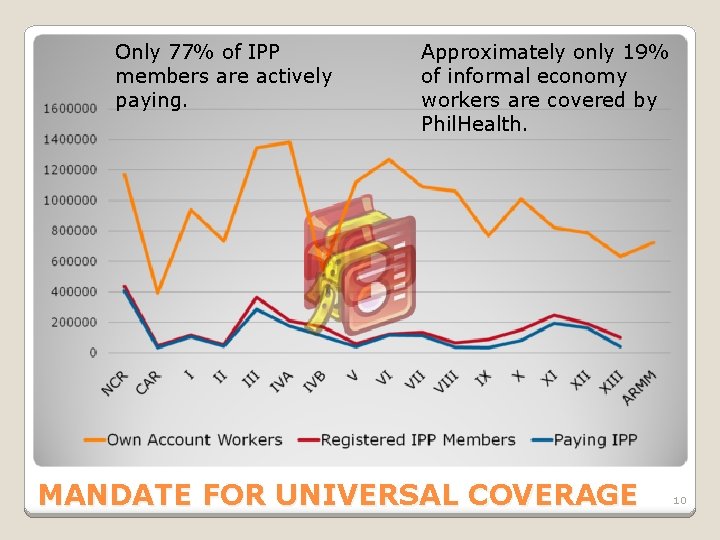
Only 77% of IPP members are actively paying. Approximately only 19% of informal economy workers are covered by Phil. Health. MANDATE FOR UNIVERSAL COVERAGE 10
Problems on demand-side De facto voluntary decision for household. As a result, low coverage levels – approx 14% of the target group enrolled. Premium $20 per annum for family; generally acceptable but people want to pay weekly/monthly given uncertain income. Many remote communities, with little health infra. Irregular contributions / coverage: only two-third of members registered in Phil. Health’s voluntary ‘individual paying programme’ pay regularly Adverse selection creates financial instability: Estimated that programme targeting informal sector made 121% loss in 2005
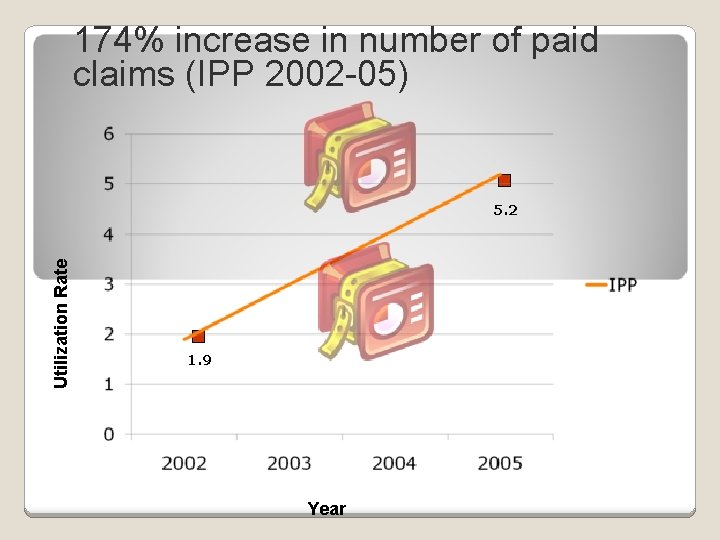
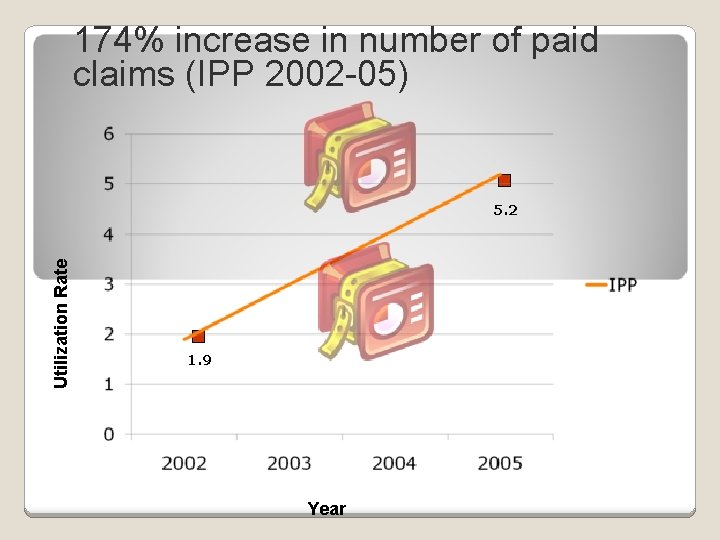
174% increase in number of paid claims (IPP 2002 -05) Utilization Rate 5. 2 1. 9 Year
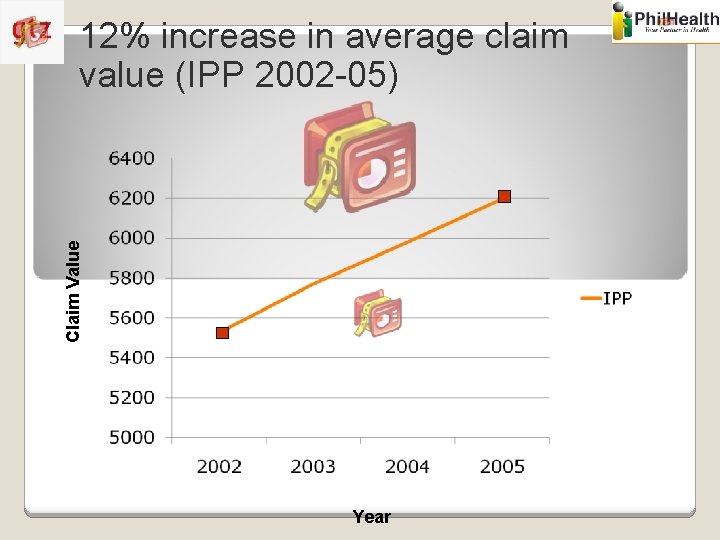
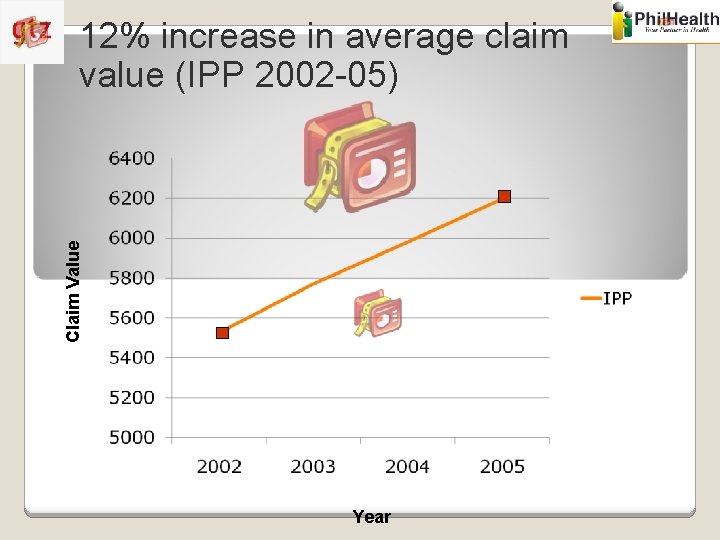
Claim Value 12% increase in average claim value (IPP 2002 -05) Year
Problems on supply-side Large public sector bureaucracy has limitations in: Marketing and selling health insurance Developing flexible payment systems which meet demands of target group Phil. Health ideally wants annual premium payments (to stabilise irregular payments), but target population want the opposite Chasing individual households administratively expensive and highly inefficient
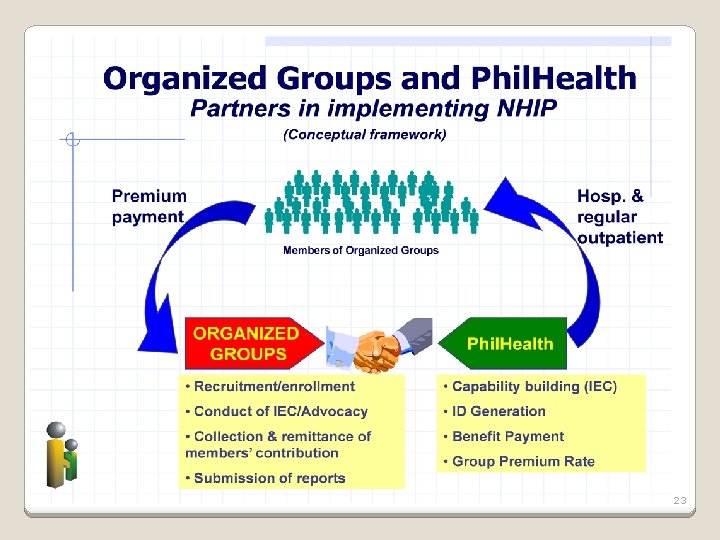
Response to unstable coverage / contributions Rather than targeting individual households directly, target groups, and mirror employeremployee relationship (admin efficiency gains, limit adverse selection). Piggy-back on collection systems of microfinance / cooperative organisations who collect very regularly from clients (greater flexibility for client). This partnership allows Phil. Health to respond to household’s demand to pay small amounts regularly, whilst the organisation remits annual/semi-annual/quarterly payments to Phil. Health. Up to each partner how to organise internally.
Response to adverse selection Promote mandatory enrolment within microfinance organisation (efficient risksharing). Strong demand for health insurance by MFI/Coop management for their members. Set minimum group size. Currently set at 70% (counter adverse selection). How to enforce? Offer discounted premium. Similar approach to private health insurance approaching companies. Should also help to limit coverage instability – partner loses income (through discounted premium) if enrolment drops below 70%.
Kalusugang Sigurado at Abot. Kaya sa Phil. Health Insurance 17
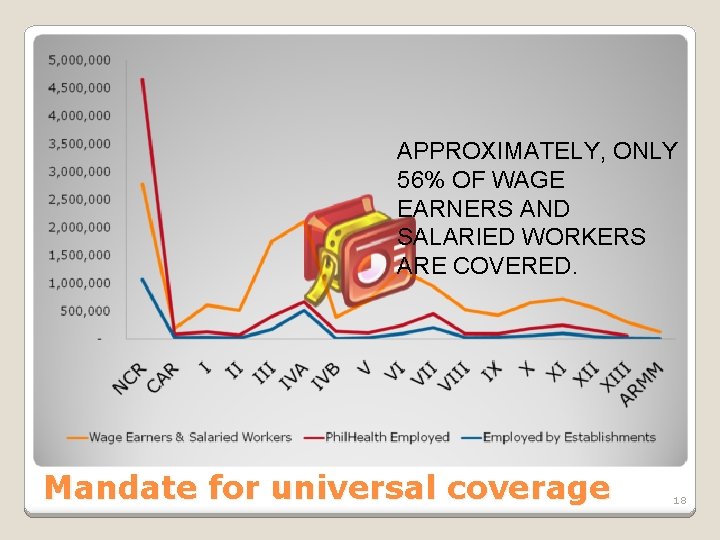
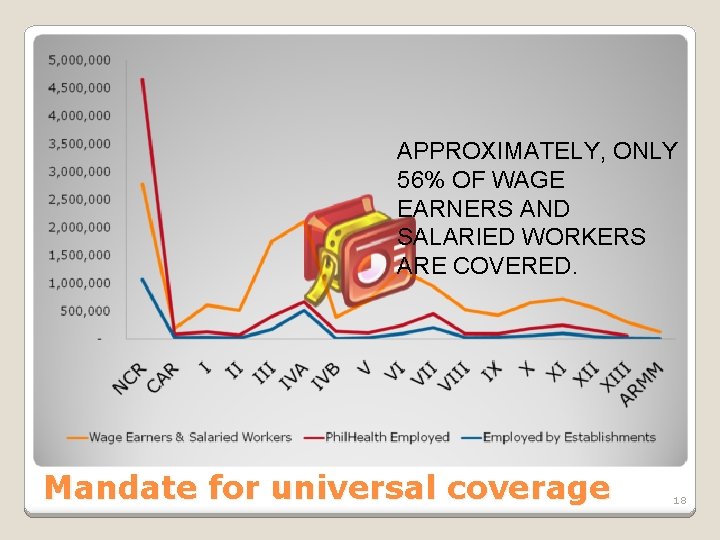
APPROXIMATELY, ONLY 56% OF WAGE EARNERS AND SALARIED WORKERS ARE COVERED. Mandate for universal coverage 18
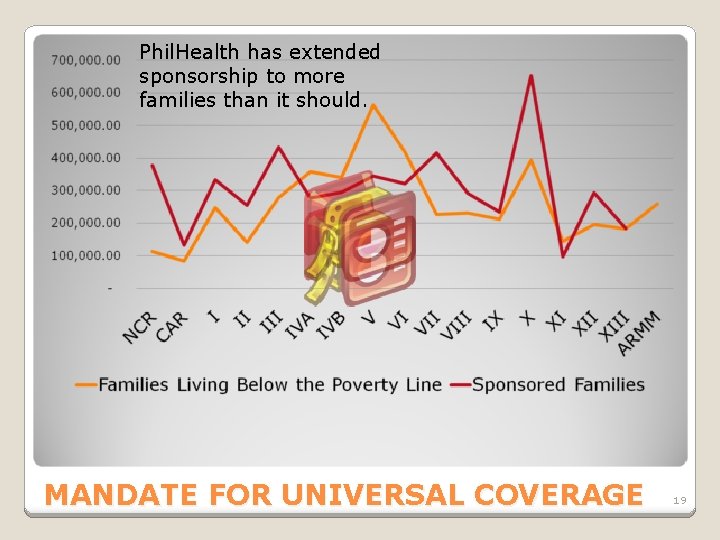
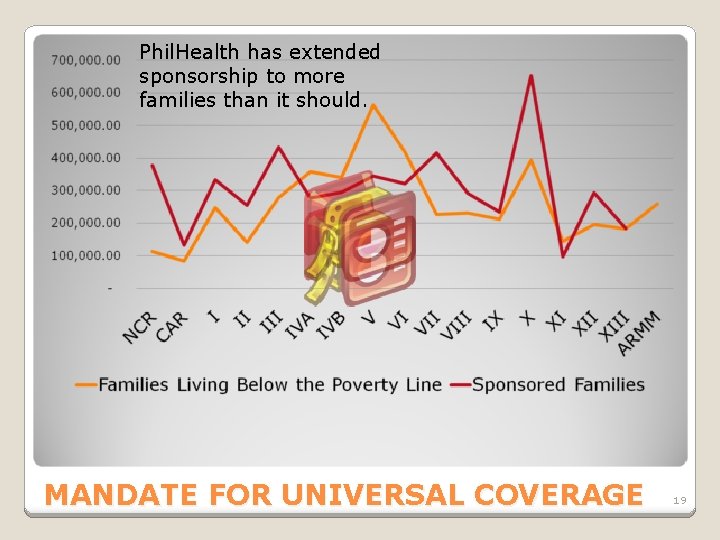
Phil. Health has extended sponsorship to more families than it should. MANDATE FOR UNIVERSAL COVERAGE 19
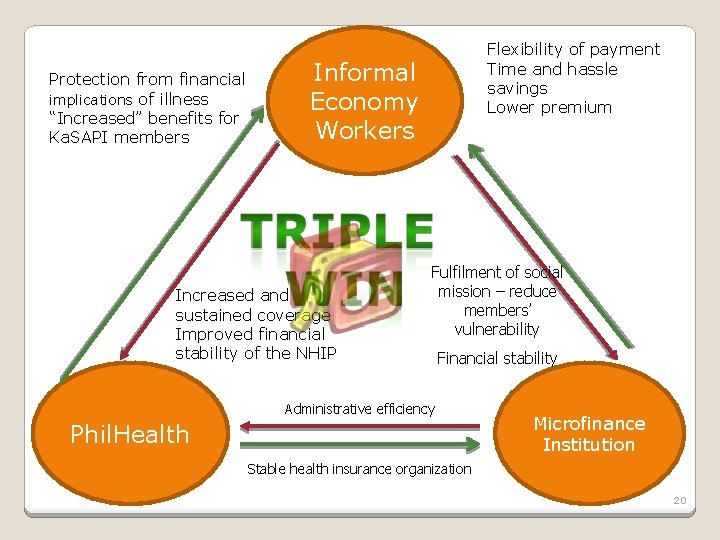
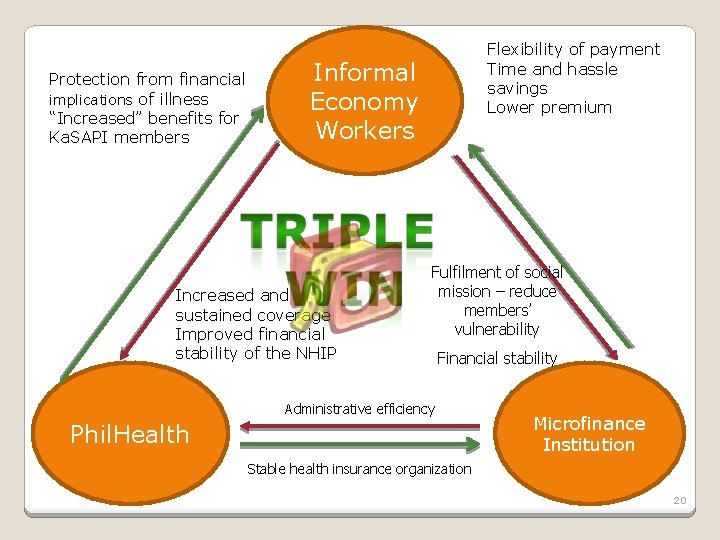
Protection from financial implications of illness “Increased” benefits for Ka. SAPI members Flexibility of payment Time and hassle savings Lower premium Informal Economy Workers Increased and sustained coverage Improved financial stability of the NHIP Fulfilment of social mission – reduce members’ vulnerability Financial stability Administrative efficiency Phil. Health Microfinance Institution Stable health insurance organization 20
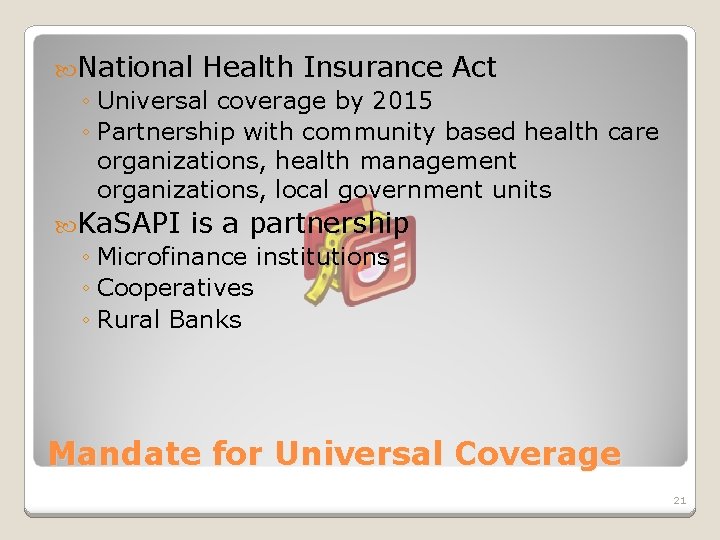
National Health Insurance Act ◦ Universal coverage by 2015 ◦ Partnership with community based health care organizations, health management organizations, local government units Ka. SAPI is a partnership ◦ Microfinance institutions ◦ Cooperatives ◦ Rural Banks Mandate for Universal Coverage 21
Phil. Health Board Resolution 719 approved September 2004 Ka. SAPI launched on September 2005 in 7 pilot regions At present, 15 partners …. And counting Ka. SAPI 22
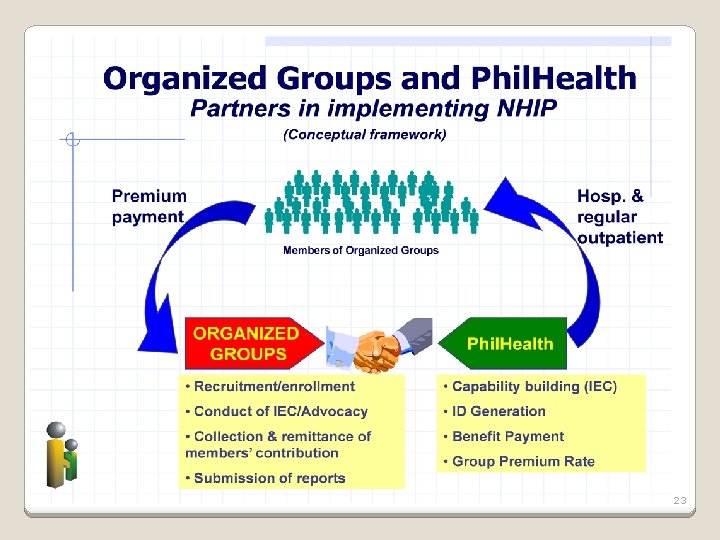
23
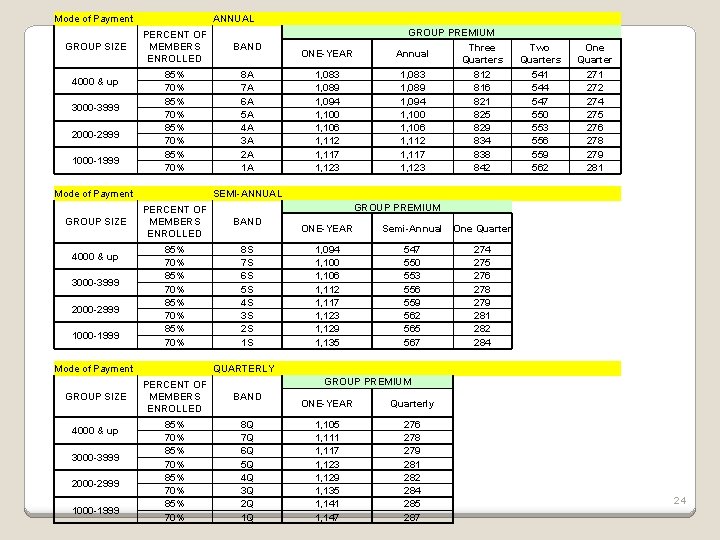
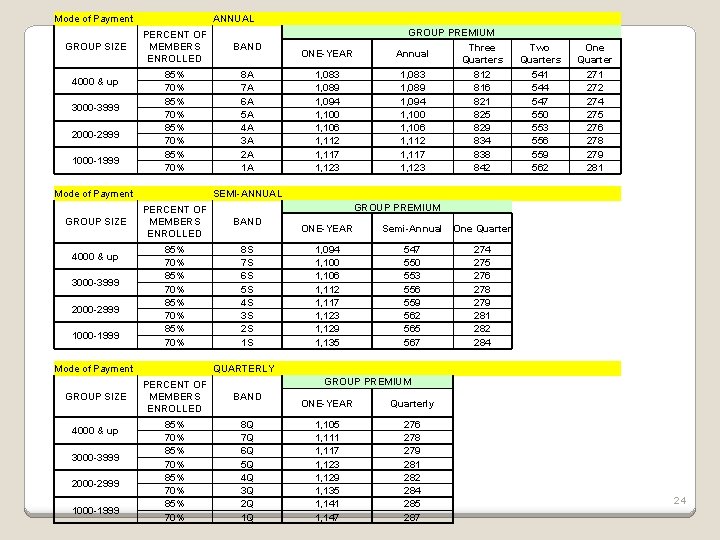
Mode of Payment GROUP SIZE 4000 & up 3000 -3999 2000 -2999 1000 -1999 ANNUAL BAND 85% 70% 8 A 7 A 6 A 5 A 4 A 3 A 2 A 1 A Mode of Payment GROUP SIZE 4000 & up 3000 -3999 2000 -2999 1000 -1999 ONE-YEAR Annual Three Quarters Two Quarters One Quarter 1, 083 1, 089 1, 094 1, 100 1, 106 1, 112 1, 117 1, 123 812 816 821 825 829 834 838 842 541 544 547 550 553 556 559 562 271 272 274 275 276 278 279 281 SEMI-ANNUAL GROUP PREMIUM PERCENT OF MEMBERS ENROLLED BAND 85% 70% 8 S 7 S 6 S 5 S 4 S 3 S 2 S 1 S Mode of Payment GROUP SIZE GROUP PREMIUM PERCENT OF MEMBERS ENROLLED ONE-YEAR Semi-Annual One Quarter 1, 094 1, 100 1, 106 1, 112 1, 117 1, 123 1, 129 1, 135 547 550 553 556 559 562 565 567 274 275 276 278 279 281 282 284 QUARTERLY GROUP PREMIUM PERCENT OF MEMBERS ENROLLED BAND 85% 70% 8 Q 7 Q 6 Q 5 Q 4 Q 3 Q 2 Q 1 Q ONE-YEAR Quarterly 1, 105 1, 111 1, 117 1, 123 1, 129 1, 135 1, 141 1, 147 276 278 279 281 282 284 285 287 24
25

26
Conference on Extending Social Health Insurance to Informal Economy Workers – Manila, October 2006 Involvement of other partners in the program DOF, DOLE, NEDA, DBP, RBAP, MFC, NATCCO, Pinoy. ME, labour groups http: //www. gtzhealth-philippines. org 27

Phil. Health ◦ Immersion to different types of organized groups ◦ Training of trainers on “Social Health Insurance Advocates and Champions (SHIAC) for Organized Groups” Organized Groups ◦ SHIAC ◦ Understanding Phil. Health Process Review ◦ In preparation of a national roll out by 2008 Capacity Development 28
Phil. Health needed data to support claim the illness is bad for business among MFIs Findings ◦ Illness is perceived to be a cause of loan default and drop outs from OGs ◦ Illness, by client or family member, is among causes of loan default by members ◦ Illness will affect clients more than MFIs Study: Illness as a Cause of Loan Default 29
Out of a potential 600, 000 members from the 14 OG(s), we have enrolled 4, 500 as of September 2007 ◦ Partners were also in a pilot mode, limiting enrollment to certain areas ◦ Program is voluntary in almost all partners Only NGO-MFIs have reached at least the minimum 700 enrollees ◦ Frequent contacts with members increase awareness, facilitates easier collection and monitoring What have we achieved so far? 30
Feedback mechanism on the type and quality of care given by accredited health providers ◦ Members found a venue to voice out their concerns through the OGs Membership to Phil. Health by people from “geographically isolated areas” are facilitated What have we achieved so far? 31

High drop out rate especially among those opting to pay on a quarterly basis ◦ Premiums are tied to loans particularly with MFIs ◦ Partners are now considering financing through savings, dividends or outright payment Administratively Phil. Health taxing for OGs and ◦ Social marketing activities ◦ Administrative work – seamless integration of IT system not yet fully there What are our current challenges? 32
Lack of public documents that would qualify dependents as beneficiaries Exclusion of groups that do not qualify the evaluation criteria ◦ Workers’ associations ◦ smaller groups like cooperatives that do not reach minimum number of members = 1000 Creating a consortium to reach 1000 members is very difficult What are our current challenges? 33

34
Premium financing • Small, frequent payments; sources of financing premiums other than loans Access to adequate quality health care • • Accredited health facilities and professionals Planned implementation of a quality standards Feedback mechanisms Improvement of Phil. Health’s current benefit package Universality • Extension to informal economy workers • Equitable scheme Performance (design and implementation of sound management information system) Inclusion in national strategies, legal framework Social marketing • Developing marketing messages for members, leaders of community organizations…Phil. Health officials Checklist 35

http: //www. gtzhealth-philippines. org 36