JUNCTIONA L ARRHYTHMI AS INTRODUCTION If the SA




- Slides: 35


JUNCTIONA L ARRHYTHMI AS
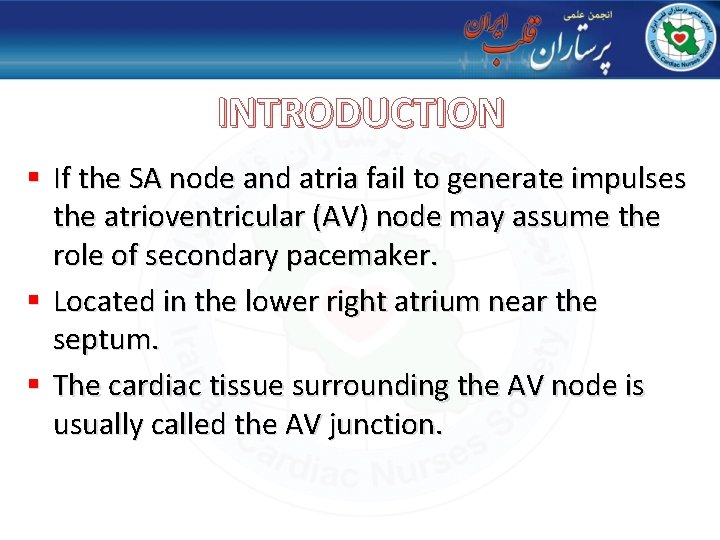
INTRODUCTION § If the SA node and atria fail to generate impulses the atrioventricular (AV) node may assume the role of secondary pacemaker. § Located in the lower right atrium near the septum. § The cardiac tissue surrounding the AV node is usually called the AV junction.
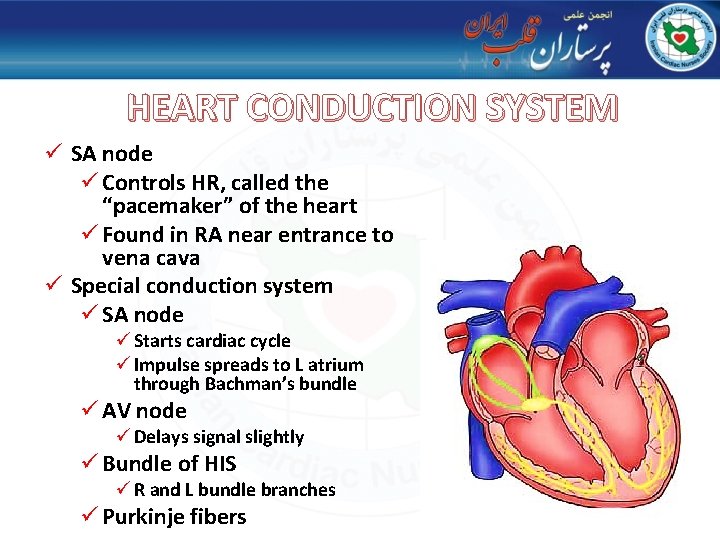
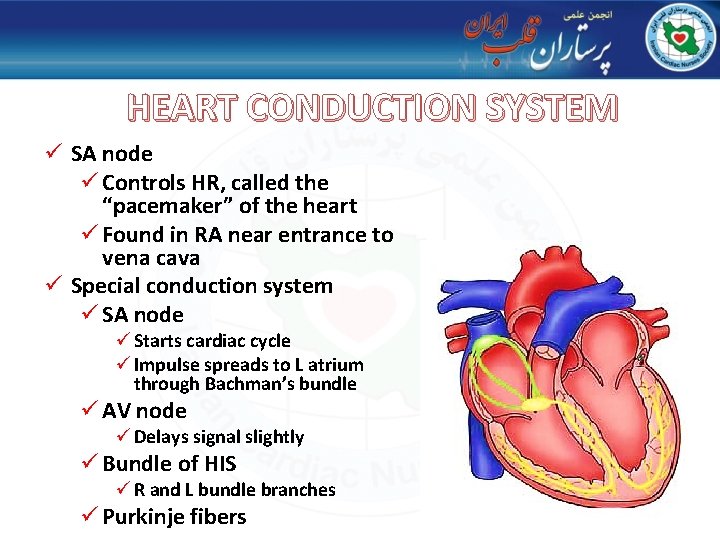
HEART CONDUCTION SYSTEM ü SA node ü Controls HR, called the “pacemaker” of the heart ü Found in RA near entrance to vena cava ü Special conduction system ü SA node ü Starts cardiac cycle ü Impulse spreads to L atrium through Bachman’s bundle ü AV node ü Delays signal slightly ü Bundle of HIS ü R and L bundle branches ü Purkinje fibers
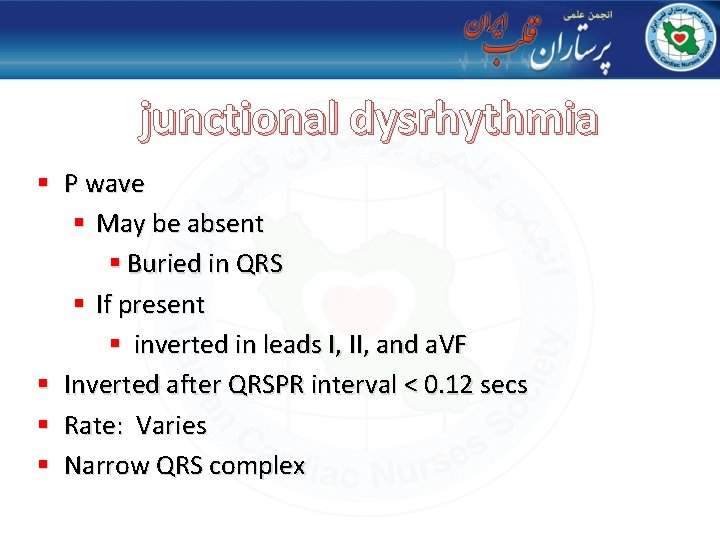
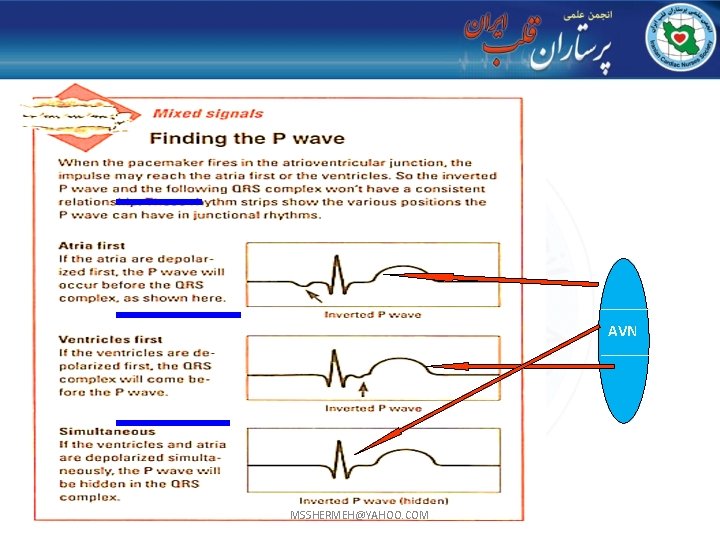
junctional dysrhythmia § P wave § May be absent § Buried in QRS § If present § inverted in leads I, II, and a. VF § Inverted after QRSPR interval < 0. 12 secs § Rate: Varies § Narrow QRS complex
junctional dysrhythmia 6
AVN MSSHERMEH@YAHOO. COM
junctional dysrhythmia § The Av Junction Is Capable Of Initiating Electrical Impulses. § Impulses That Start In The Av Node Or Av Junctional Area Are Called Junctional Or Nodal Rhythms. § The Av Junction Is Not As Efficient As The Sa Node Therefore It Has A Slower Rate. § The Inherent Heart Rate Of The Av Junctional Area Is 40 To 60 Impulses Per Minute.
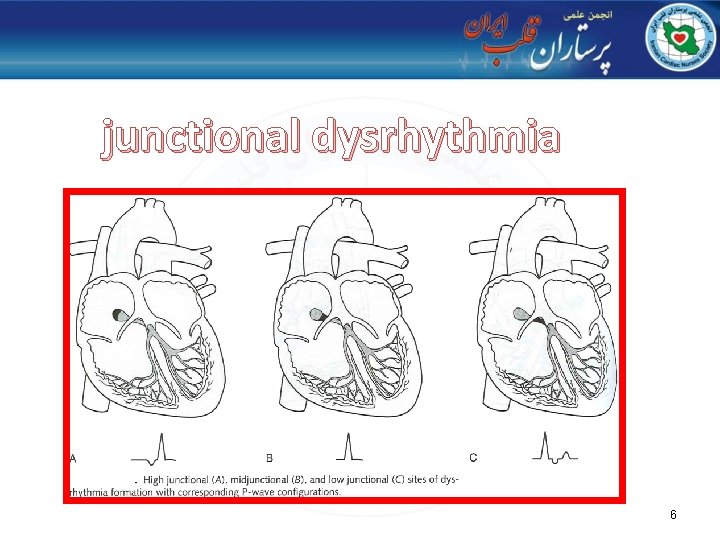
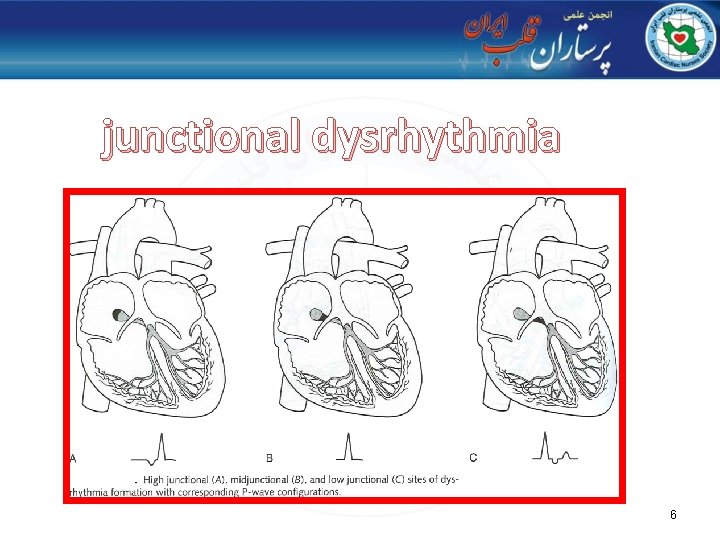
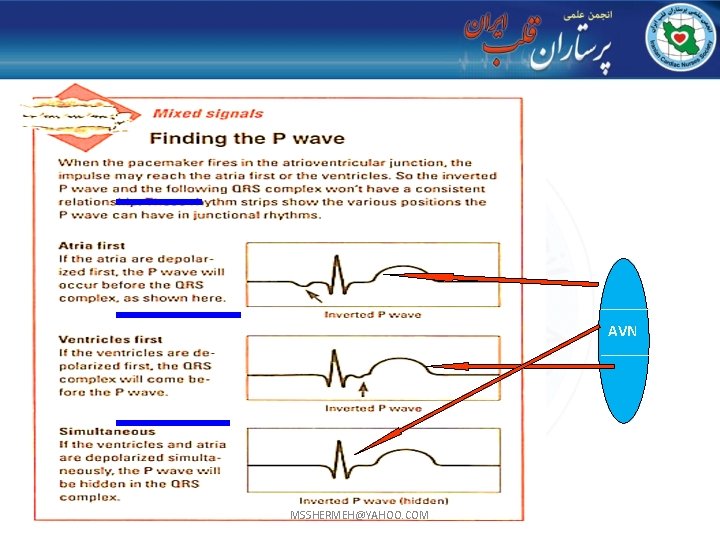
junctional dysrhythmia Inverted p wave AVN § If the impulse originates high in the av junctional area the atria depolarize quickly in a retrograde manner. § The p wave will be upside down or retrograde. § Since the impulse distance is shorter to depolarize the ventricles the PR interval is less than 0. 12 seconds.
Buried or hidden p wave AVN § If The Impulse Originates In The Mid Av Junctional Area The Distance The Impulse Must Travel Up Through The Atria And Down The Ventricles Is Almost The Same. § This Causes The Atria And Ventricles To Depolarize At Almost The Same Time. § The Force Of Atrial Depolarization Is Less Than The Force Of Ventricular Depolarization The P Wave Is Hidden By The Qrs. § The P Wave Is Hidden And A Pri Will Not Be Seen.
RETROGRADE P WAVE AVN § Impulse Originates In The Lower Part Of The Av Junctional Area. § The Impulse Distance Is Greater To The Atria Than Ventricles. § The Atria Depolarize Slightly Later Than The Ventricles. § The P Wave Appears After The Qrs Complex. § No Measurable Pri, P Wave Is Inverted.
junctional dysrhythmia Types: § Premature Junctional Contractions § Junctional Escape Rhythm § Accelerated Junctional Rhythm § Junctional Tachycardia § Reentrant Tachycardia § AVNRT
PREMATURE JUNCTIONAL CONTRACTIONS (PJC)
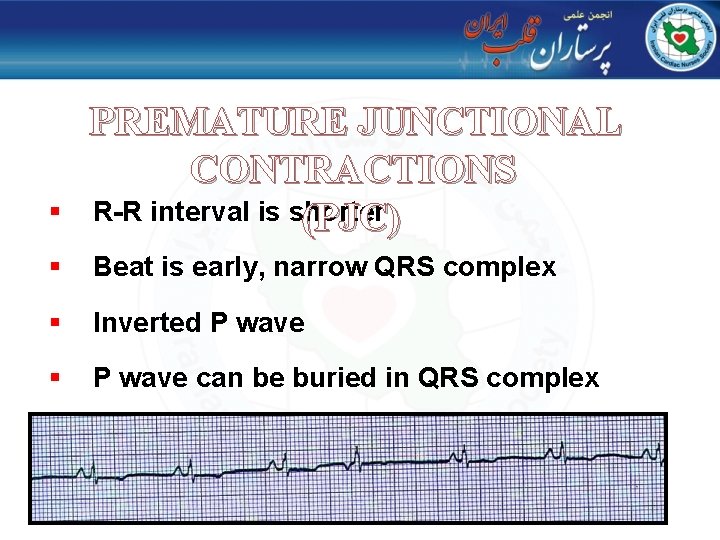
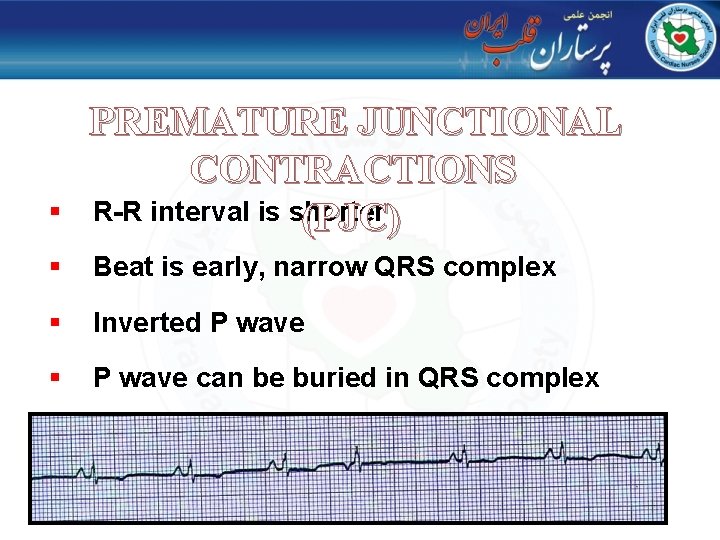
§ PREMATURE JUNCTIONAL CONTRACTIONS R-R interval is shorter (PJC) § Beat is early, narrow QRS complex § Inverted P wave § P wave can be buried in QRS complex
Cause of PJC Caused by increased irritability of The cardiac cells. May be caused by: § Digitalis, atropine, § Nicotine, caffeine, and amphetamines. § Pain, fever, fear, anxiety, exercise, sudden excitement.
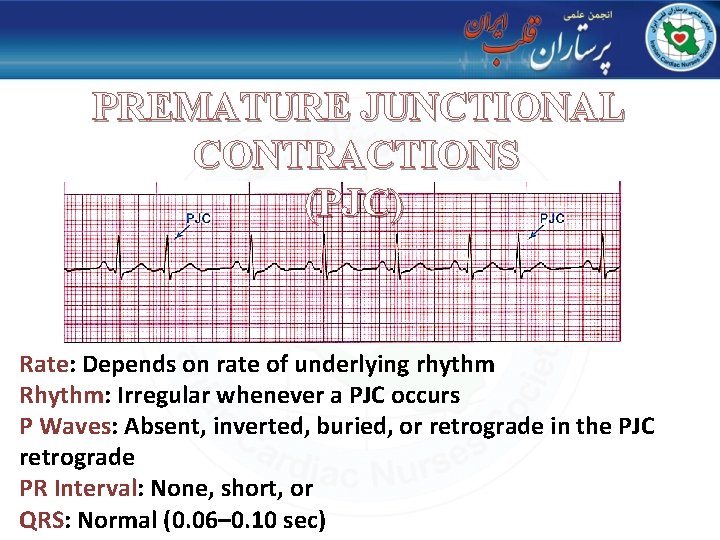
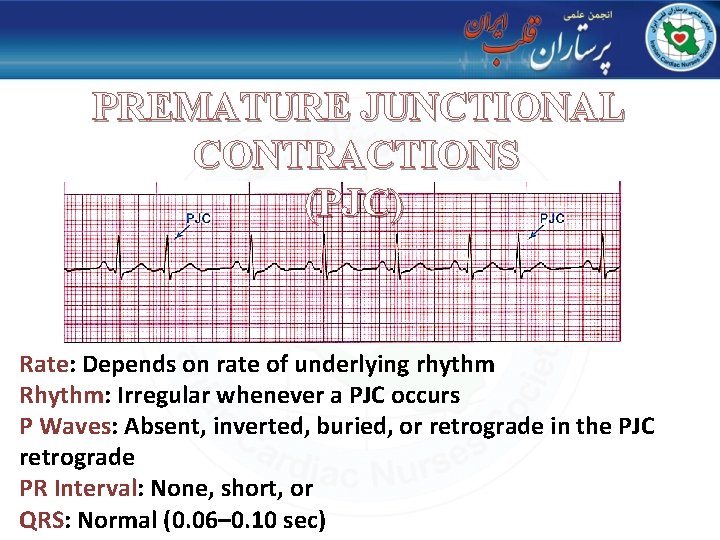
PREMATURE JUNCTIONAL CONTRACTIONS (PJC) Rate: Depends on rate of underlying rhythm Rhythm: Irregular whenever a PJC occurs P Waves: Absent, inverted, buried, or retrograde in the PJC retrograde PR Interval: None, short, or QRS: Normal (0. 06– 0. 10 sec)
§ PREMATURE JUNCTIONAL CONTRACTIONS An individual complex. (PJC) § Originates from a single site in the av junctional area. § Occurs earlier than the next expected complex of the underlying rhythm. § PJC’s are not rhythms. § Has the same characteristics as other junctional complexes.
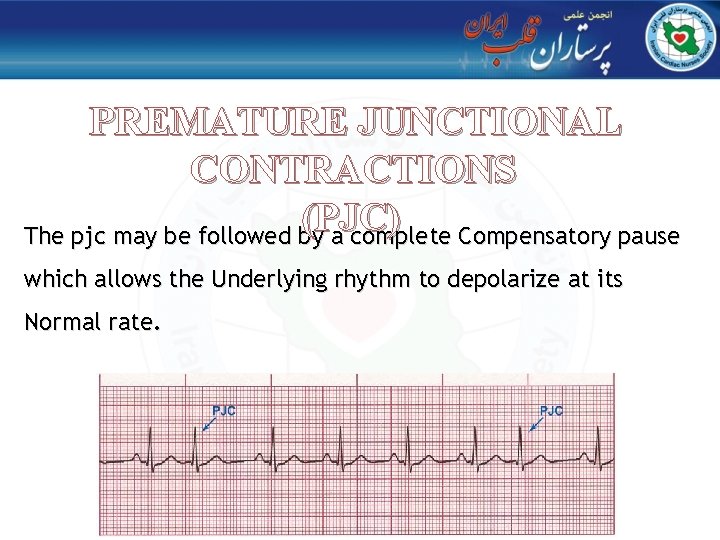
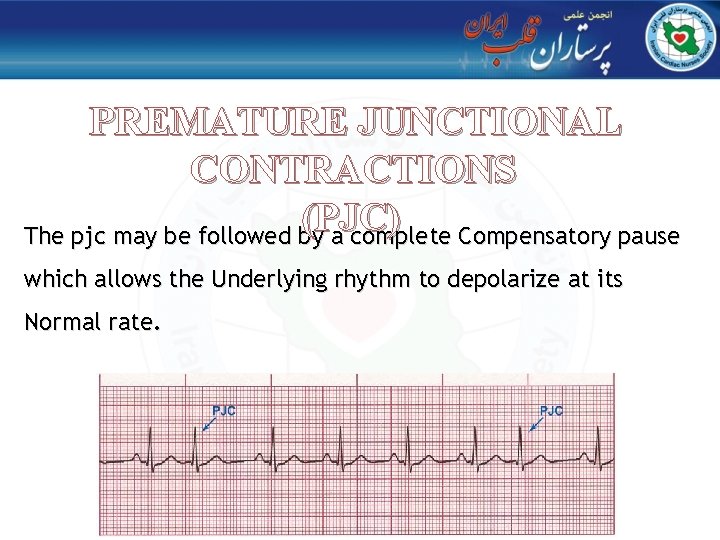
PREMATURE JUNCTIONAL CONTRACTIONS (PJC) The pjc may be followed by a complete Compensatory pause which allows the Underlying rhythm to depolarize at its Normal rate.
JUNCTIONAL ESCAPE RHYTHM
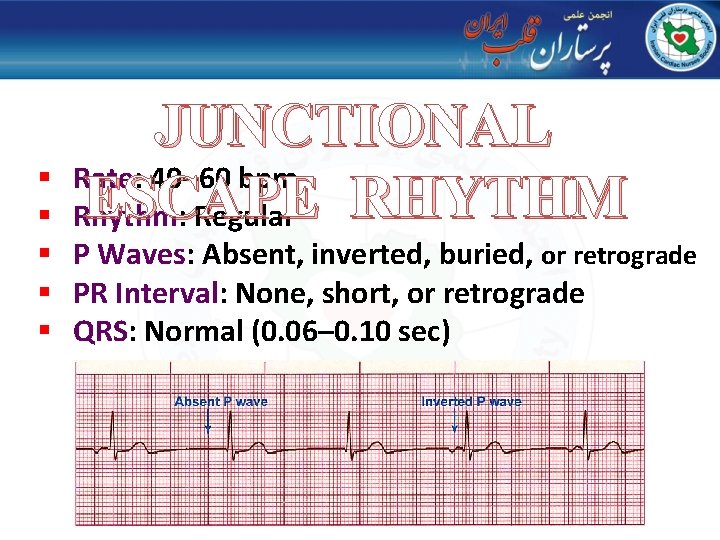
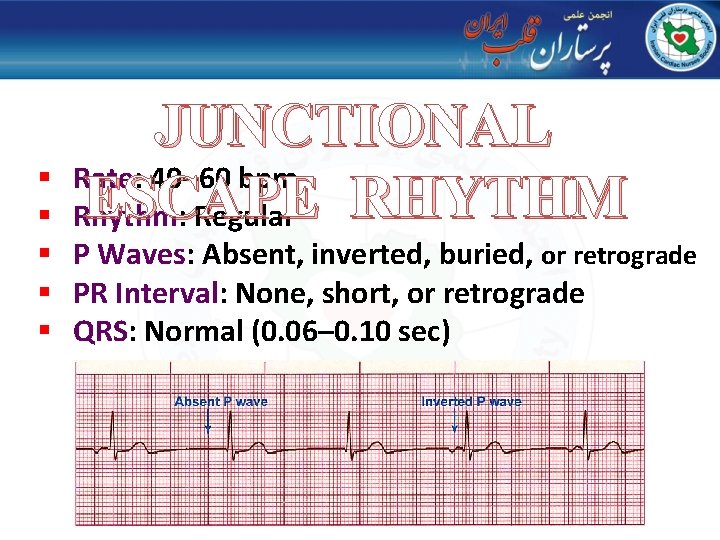
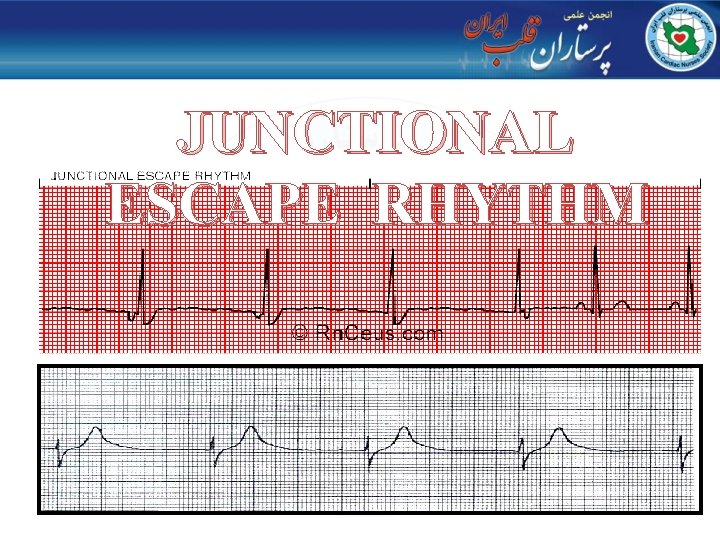
JUNCTIONAL Rate: 40– 60 bpm ESCAPE RHYTHM Rhythm: Regular § § § P Waves: Absent, inverted, buried, or retrograde § PR Interval: None, short, or retrograde § QRS: Normal (0. 06– 0. 10 sec)
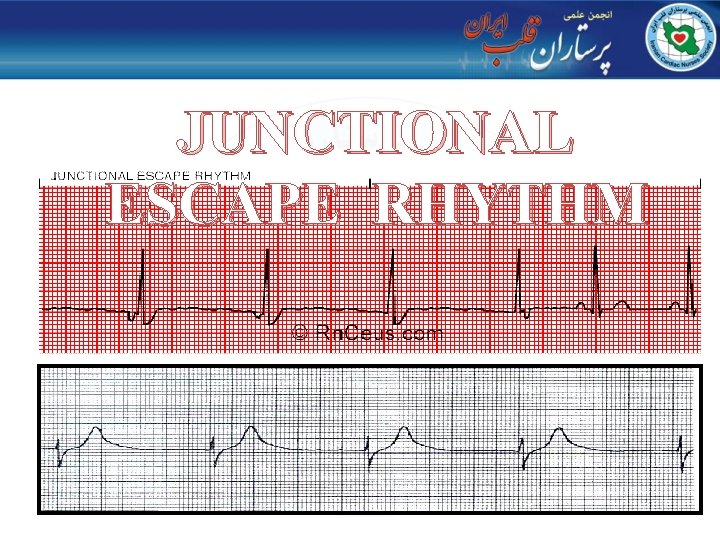
JUNCTIONAL ESCAPE RHYTHM
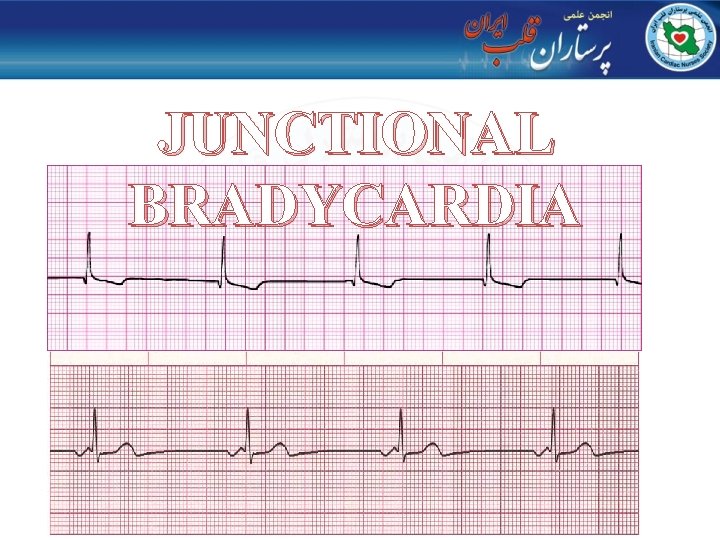
JUNCTIONAL BRADYCARDI A
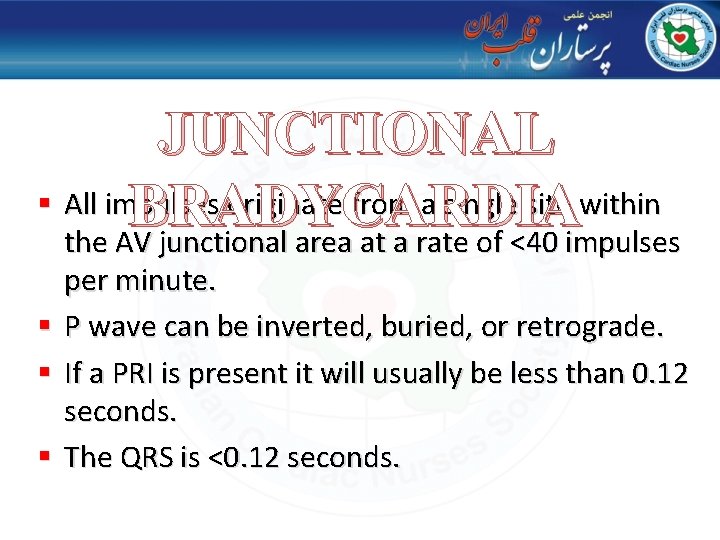
JUNCTIONAL § All impulses originate from a single site within BRADYCARDIA the AV junctional area at a rate of <40 impulses § § § per minute. P wave can be inverted, buried, or retrograde. If a PRI is present it will usually be less than 0. 12 seconds. The QRS is <0. 12 seconds.
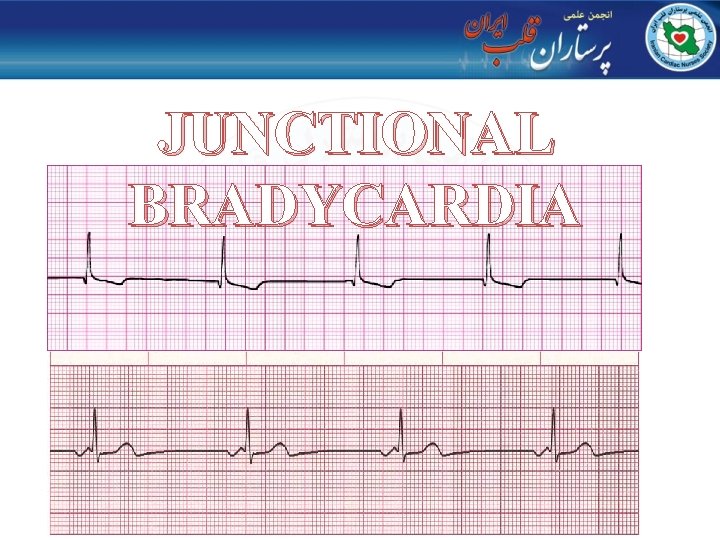
JUNCTIONAL BRADYCARDIA
§ JUNCTIONAL BRADYCARDIA The rate can vary, but must be less than 40 per minute. § This dysrhythmia may become symptomatic is the rate falls significantly. § Only a junctional rhythm with a rate below 40 can be called a junctional bradycardia.

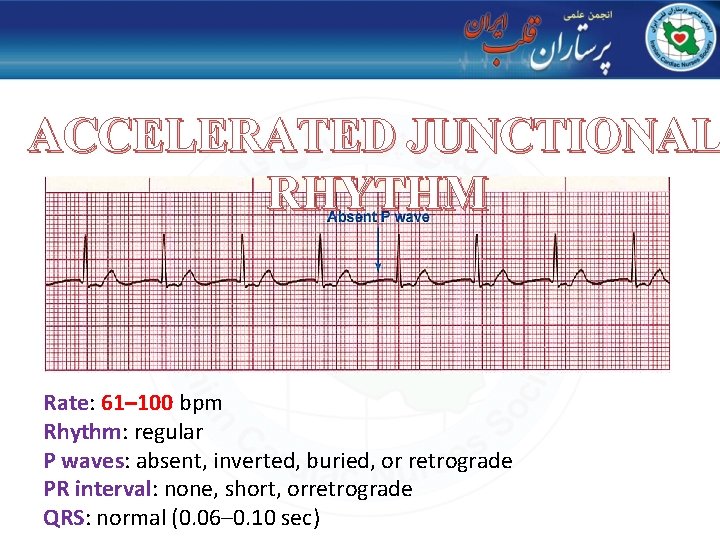
ACCELERATED JUNCTIONAL RHYTHM
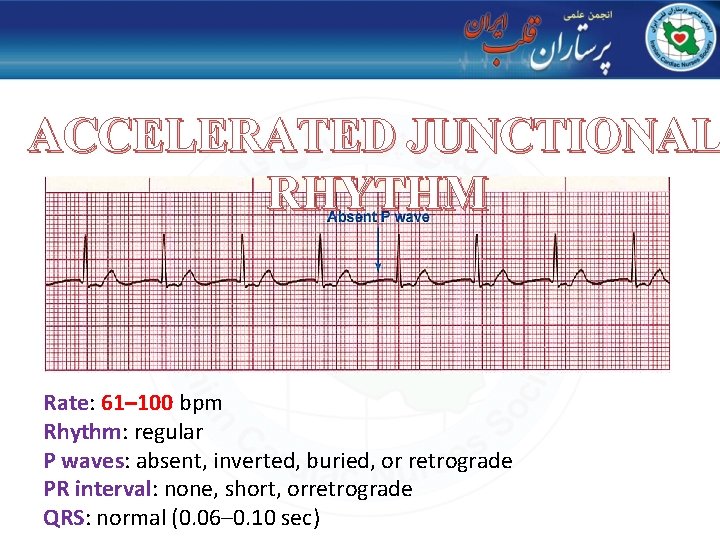
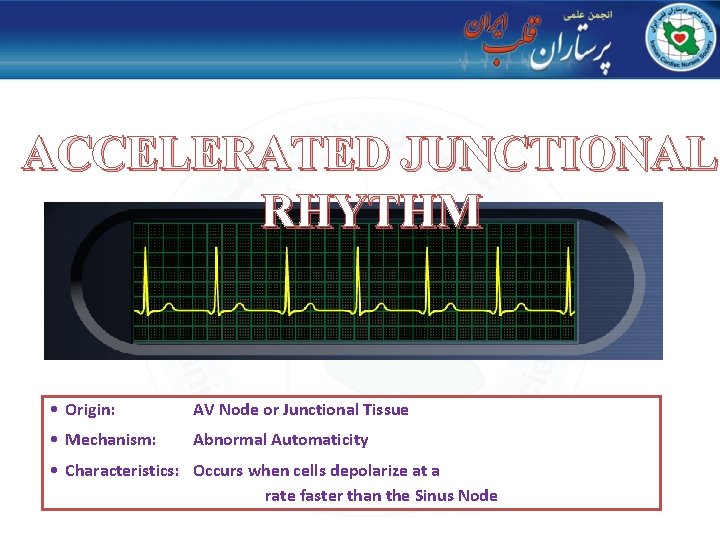
ACCELERATED JUNCTIONAL RHYTHM Rate: 61– 100 bpm Rhythm: regular P waves: absent, inverted, buried, or retrograde PR interval: none, short, orretrograde QRS: normal (0. 06– 0. 10 sec)
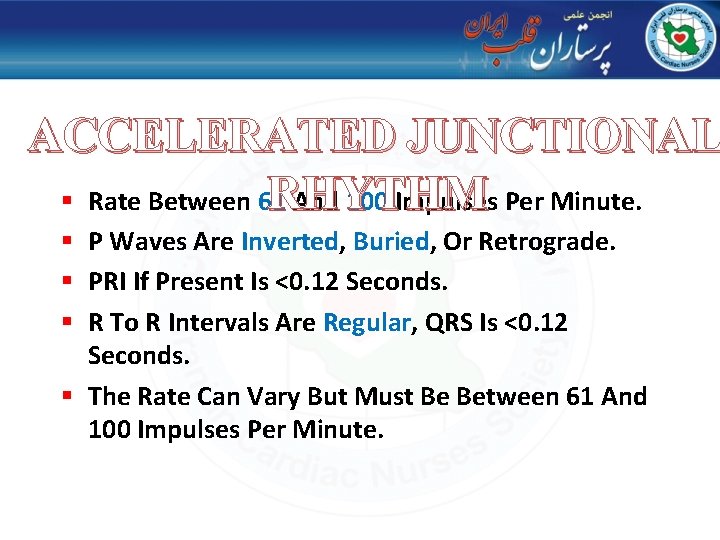
ACCELERATED JUNCTIONAL RHYTHM § Rate Between 61 And 100 Impulses Per Minute. § P Waves Are Inverted, Buried, Or Retrograde. § PRI If Present Is <0. 12 Seconds. § R To R Intervals Are Regular, QRS Is <0. 12 Seconds. § The Rate Can Vary But Must Be Between 61 And 100 Impulses Per Minute.
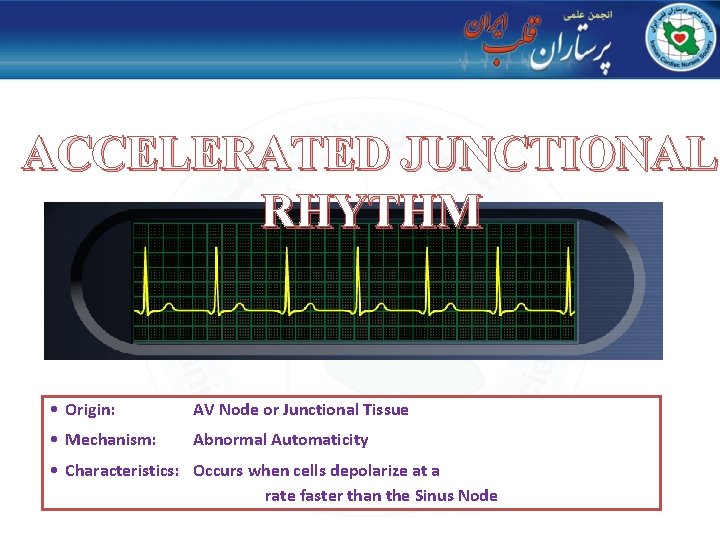
ACCELERATED JUNCTIONAL RHYTHM • Origin: AV Node or Junctional Tissue • Mechanism: Abnormal Automaticity • Characteristics: Occurs when cells depolarize at a rate faster than the Sinus Node

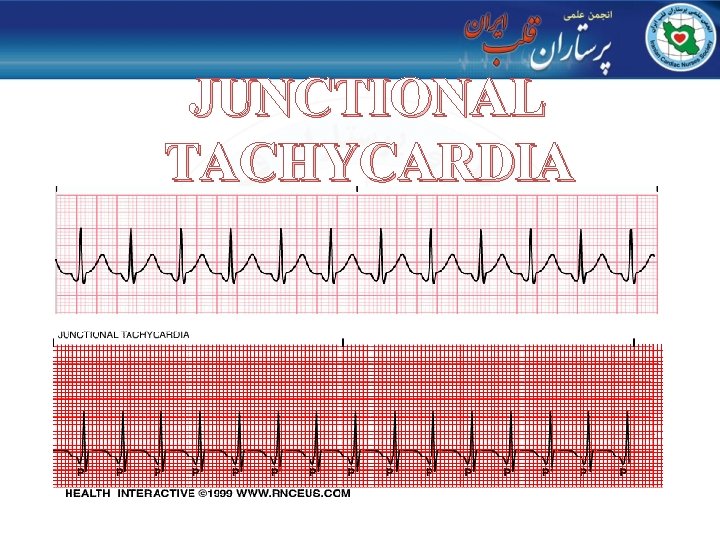
JUNCTIONAL TACHYCARDIA
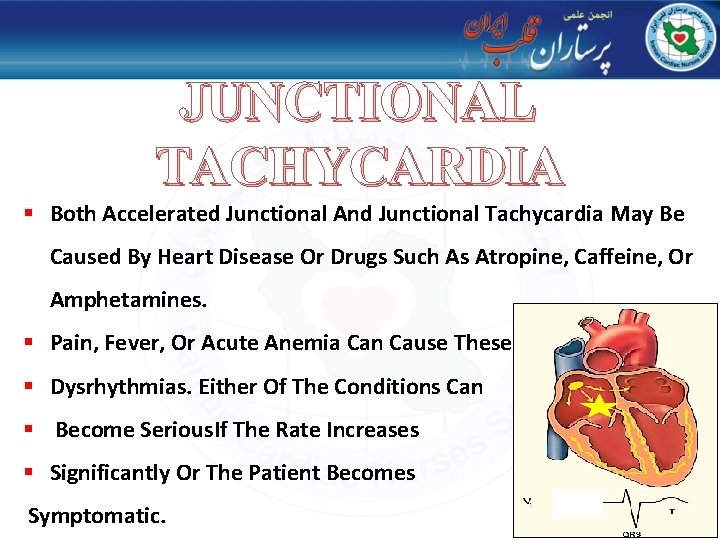
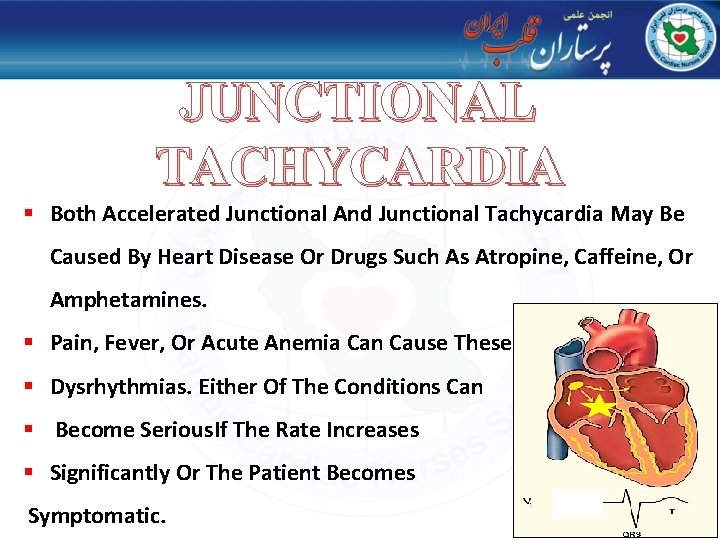
JUNCTIONAL TACHYCARDIA § Both Accelerated Junctional And Junctional Tachycardia May Be Caused By Heart Disease Or Drugs Such As Atropine, Caffeine, Or Amphetamines. § Pain, Fever, Or Acute Anemia Can Cause These § Dysrhythmias. Either Of The Conditions Can § Become Serious. If The Rate Increases § Significantly Or The Patient Becomes Symptomatic.
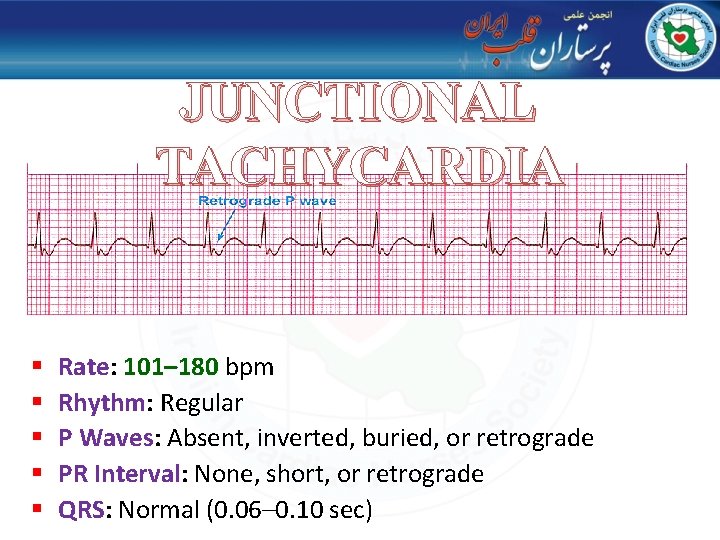
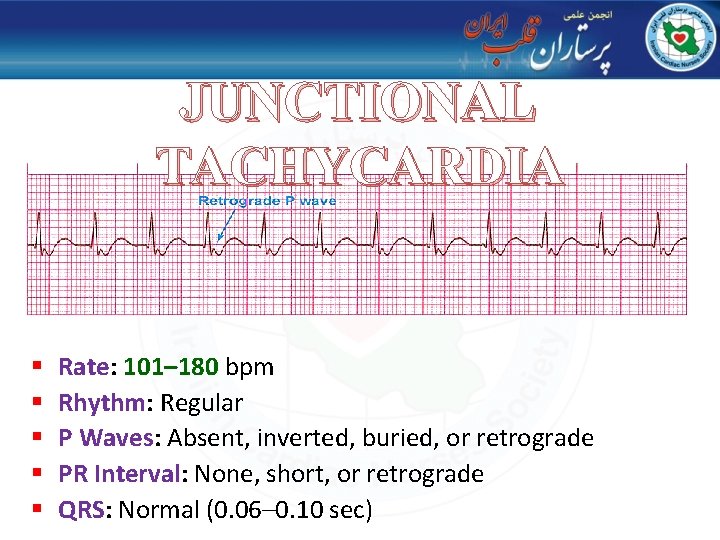
JUNCTIONAL TACHYCARDIA § § § Rate: 101– 180 bpm Rhythm: Regular P Waves: Absent, inverted, buried, or retrograde PR Interval: None, short, or retrograde QRS: Normal (0. 06– 0. 10 sec)
JUNCTIONAL TACHYCARDIA
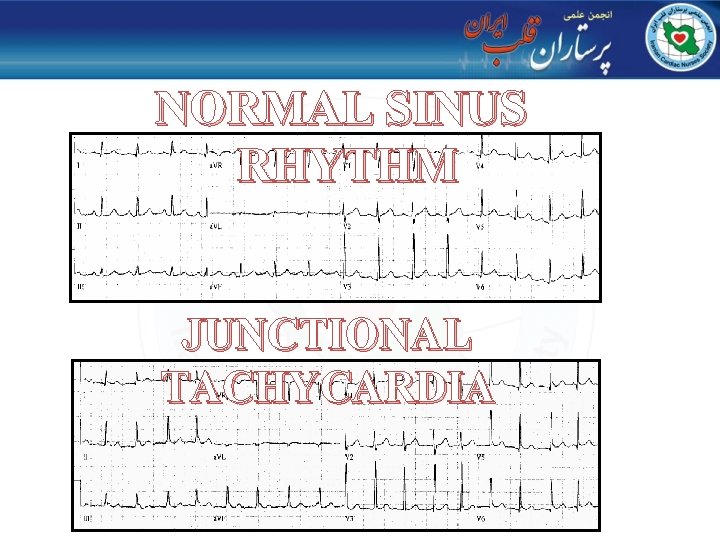
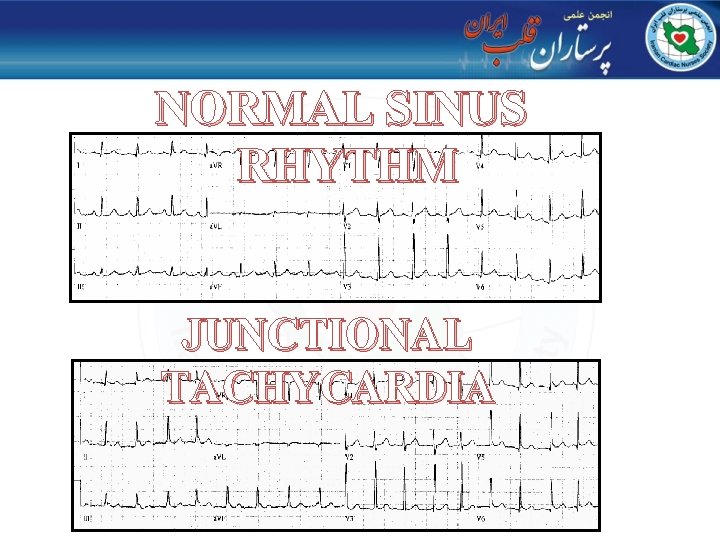
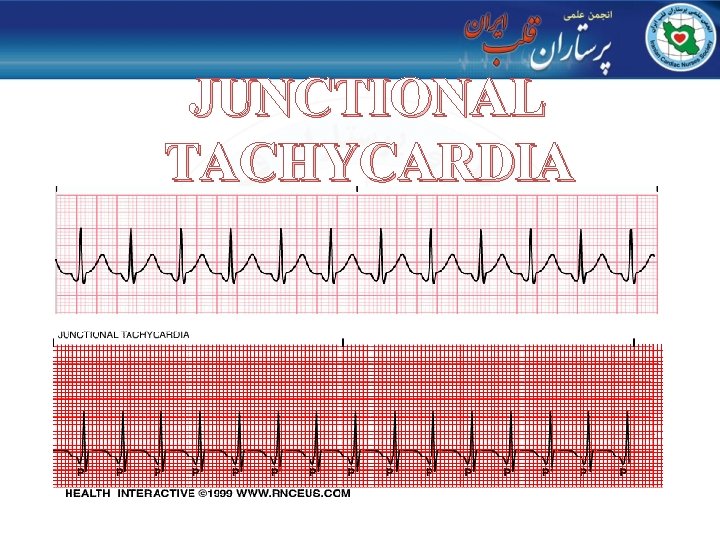
NORMAL SINUS RHYTHM JUNCTIONAL TACHYCARDIA
QUESTION?