Joint Injection Workshop Clinical Reviews and Primary Care









- Slides: 88
Joint Injection Workshop Clinical Reviews and Primary Care Update FAFP Jennifer Roth, MD Casey Mc. Clone, MD Mayo Clinic Florida

DISCLOSURE Relevant Financial Relationship(s) None Off Label Usage None
Injection Key Concepts • • Know the anatomy in 3 -D Identify landmarks Indications Contraindications Safety- of provider AND patient Injectables Technique Aftercare instructions
Why inject? • • Local delivery of medicine Avoid NSAIDs Patient satisfaction Immediate pain relief & improved function Diagnostic and therapeutic Enhance physician-patient relationship Treat without referral Revenue

Where to inject? • Intra-articular • Intramuscular • Intrabursal • Pericapsular • Periligamentous • Tendon/Tendon sheath
What to inject? • • MOST COMMON Local anesthetic Corticosteroid Viscosupplementation • • • ALTERNATIVE Prolotherapy Platelet rich plasma Autologous blood Botulism toxin
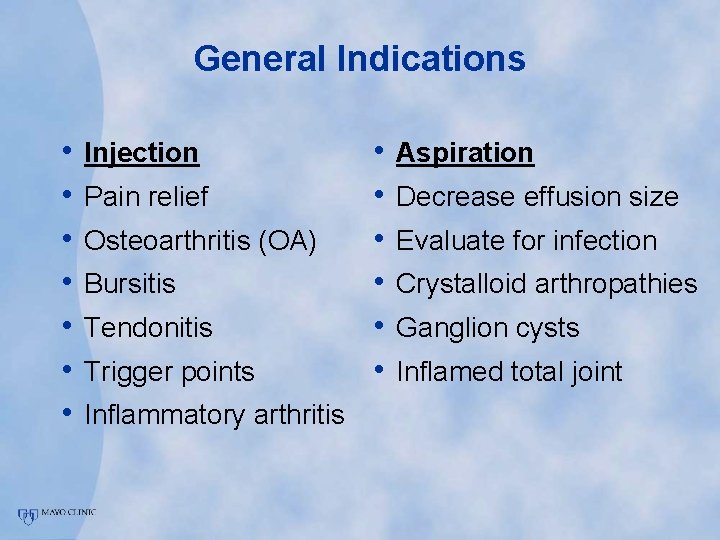
General Indications • • Injection Pain relief Osteoarthritis (OA) Bursitis Tendonitis Trigger points Inflammatory arthritis • • • Aspiration Decrease effusion size Evaluate for infection Crystalloid arthropathies Ganglion cysts Inflamed total joint
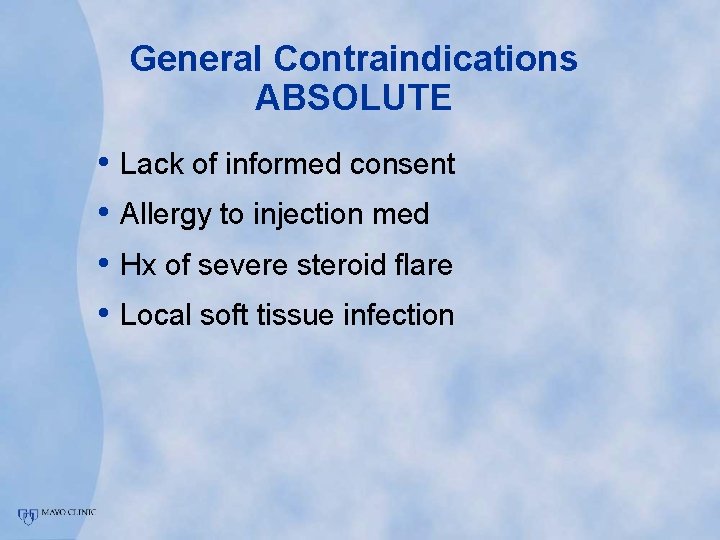
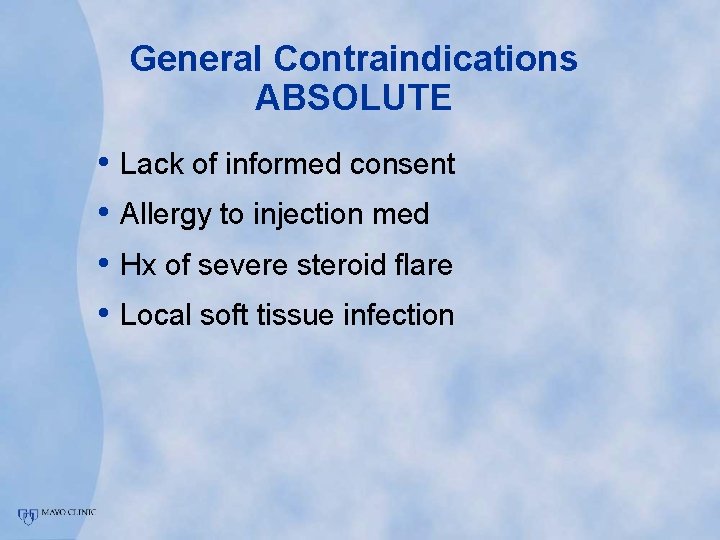
General Contraindications ABSOLUTE • Lack of informed consent • Allergy to injection med • Hx of severe steroid flare • Local soft tissue infection
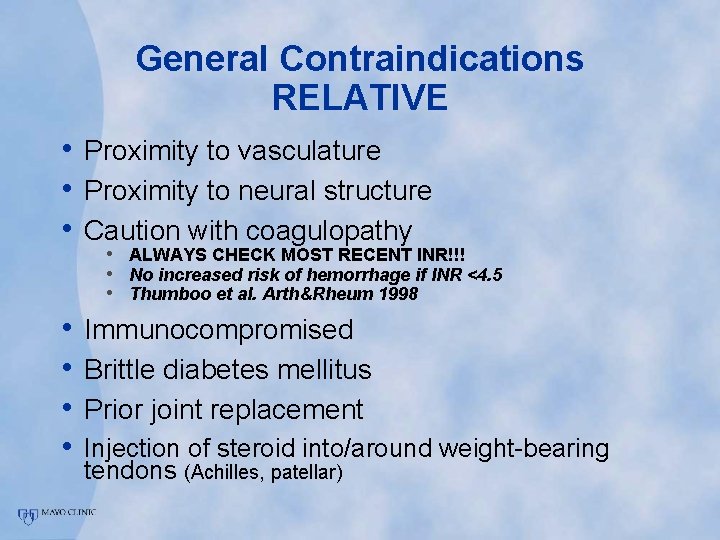
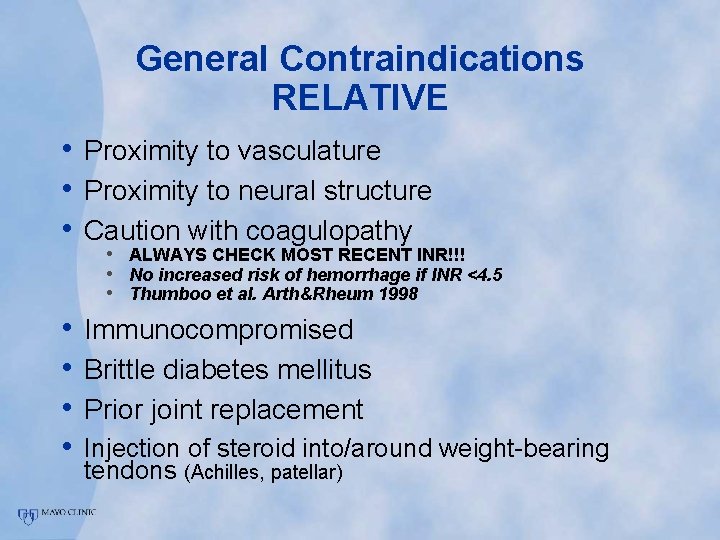
General Contraindications RELATIVE • Proximity to vasculature • Proximity to neural structure • Caution with coagulopathy • ALWAYS CHECK MOST RECENT INR!!! • No increased risk of hemorrhage if INR <4. 5 • Thumboo et al. Arth&Rheum 1998 • Immunocompromised • Brittle diabetes mellitus • Prior joint replacement • Injection of steroid into/around weight-bearing tendons (Achilles, patellar)
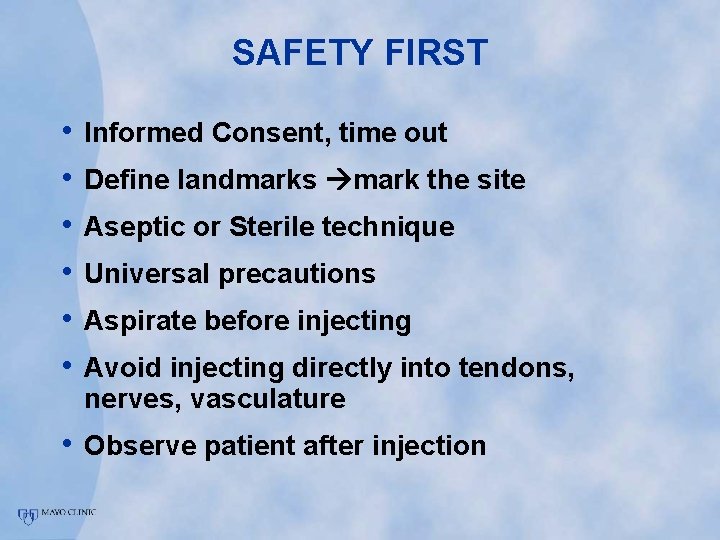
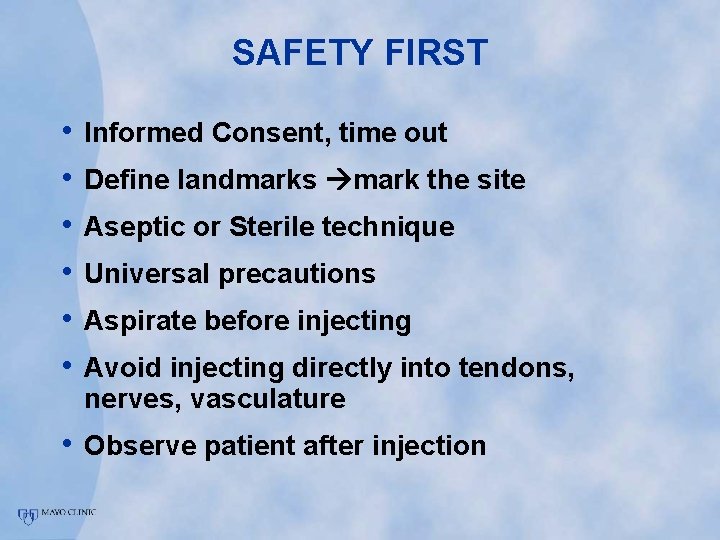
SAFETY FIRST • • • Informed Consent, time out Define landmarks mark the site Aseptic or Sterile technique Universal precautions Aspirate before injecting Avoid injecting directly into tendons, nerves, vasculature • Observe patient after injection
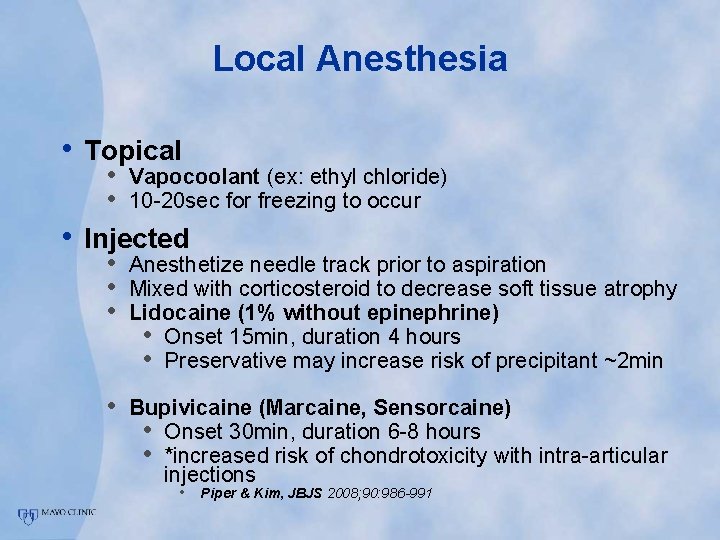
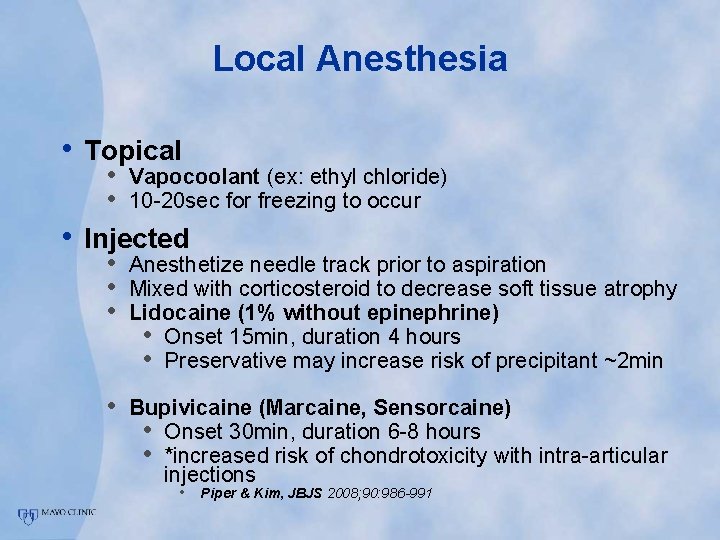
Local Anesthesia • Topical • • Vapocoolant (ex: ethyl chloride) • 10 -20 sec for freezing to occur Injected • Anesthetize needle track prior to aspiration • Mixed with corticosteroid to decrease soft tissue atrophy • Lidocaine (1% without epinephrine) • Onset 15 min, duration 4 hours • Preservative may increase risk of precipitant ~2 min • Bupivicaine (Marcaine, Sensorcaine) • Onset 30 min, duration 6 -8 hours • *increased risk of chondrotoxicity with intra-articular injections • Piper & Kim, JBJS 2008; 90: 986 -991
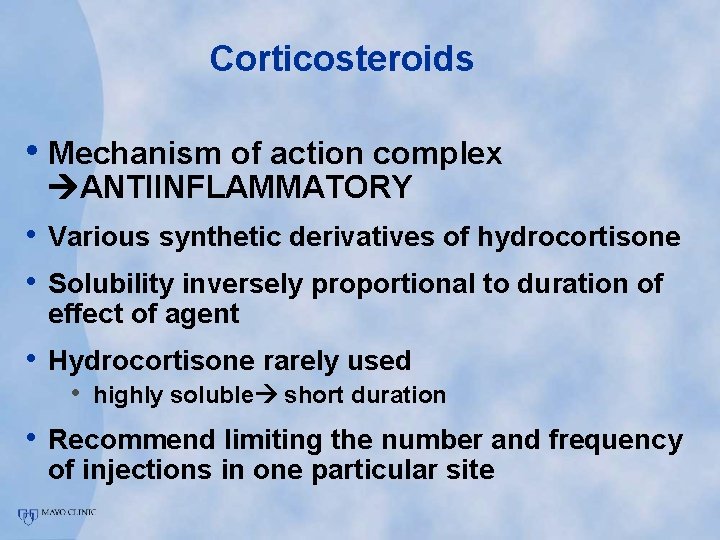
Corticosteroids • Mechanism of action complex ANTIINFLAMMATORY • Various synthetic derivatives of hydrocortisone • Solubility inversely proportional to duration of effect of agent • Hydrocortisone rarely used • highly soluble short duration • Recommend limiting the number and frequency of injections in one particular site
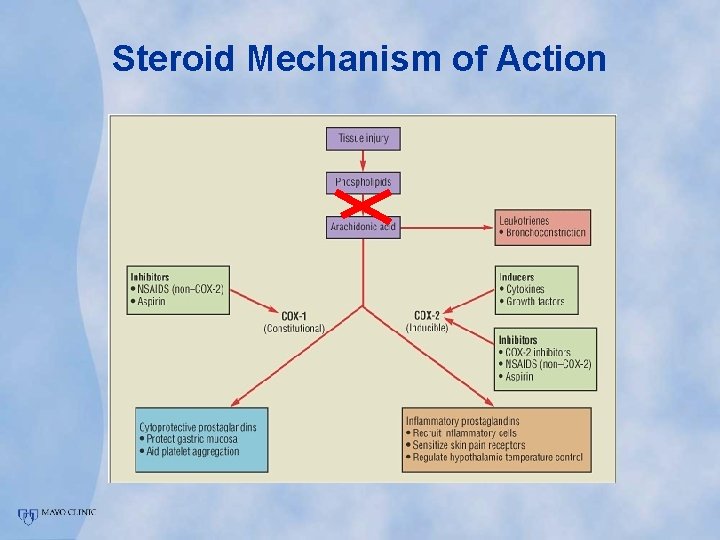
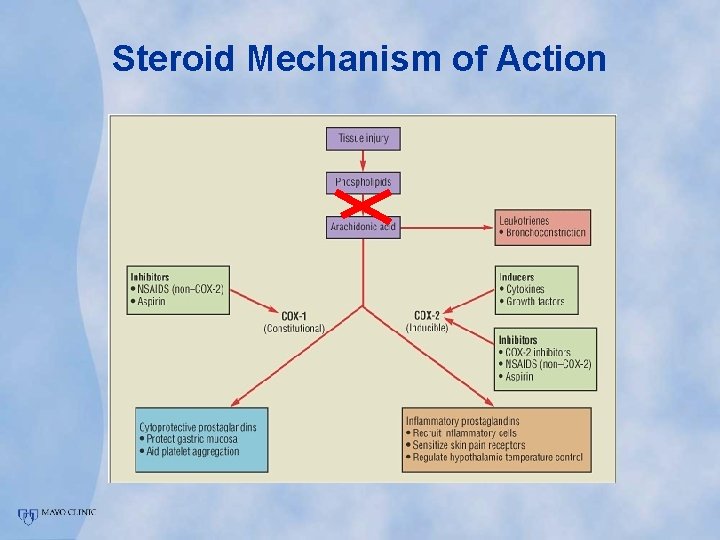
Steroid Mechanism of Action
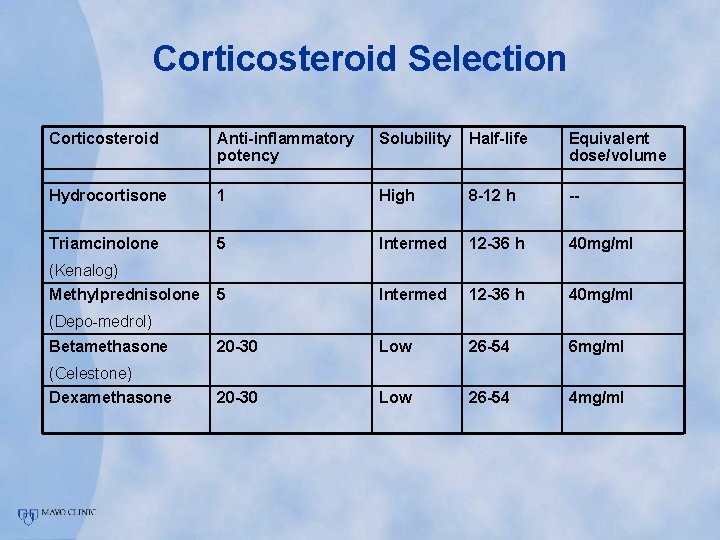
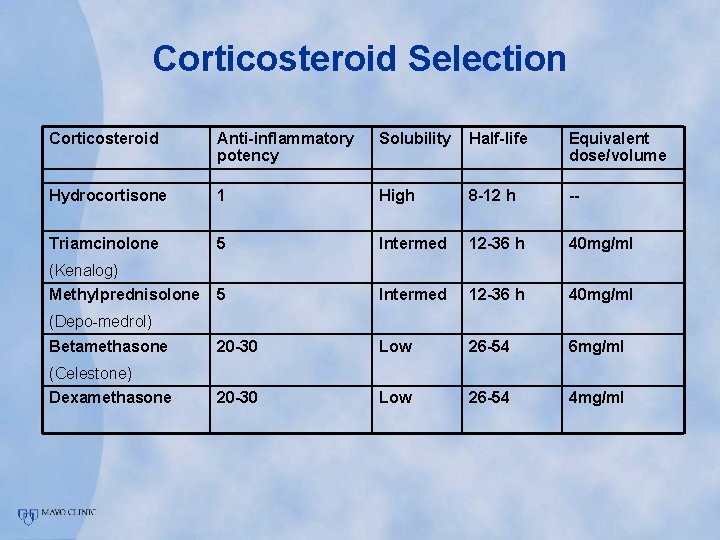
Corticosteroid Selection Corticosteroid Anti-inflammatory potency Solubility Half-life Equivalent dose/volume Hydrocortisone 1 High 8 -12 h -- Triamcinolone 5 Intermed 12 -36 h 40 mg/ml 20 -30 Low 26 -54 6 mg/ml 20 -30 Low 26 -54 4 mg/ml (Kenalog) Methylprednisolone (Depo-medrol) Betamethasone (Celestone) Dexamethasone
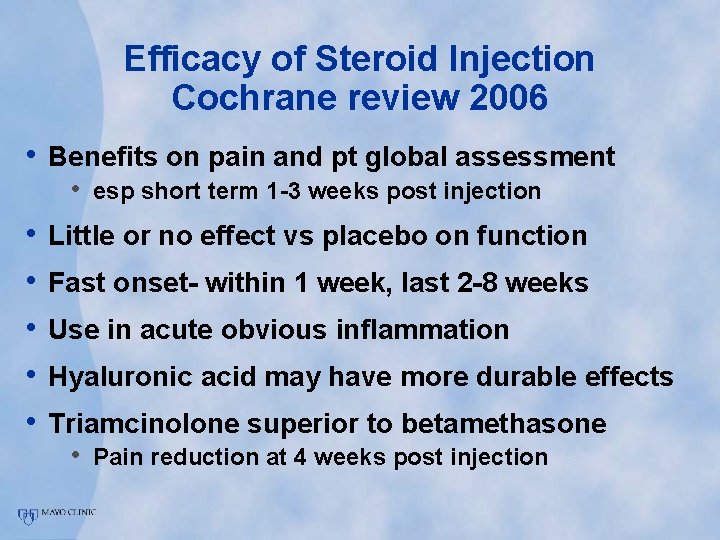
Efficacy of Steroid Injection Cochrane review 2006 • Benefits on pain and pt global assessment • esp short term 1 -3 weeks post injection • • • Little or no effect vs placebo on function Fast onset- within 1 week, last 2 -8 weeks Use in acute obvious inflammation Hyaluronic acid may have more durable effects Triamcinolone superior to betamethasone • Pain reduction at 4 weeks post injection
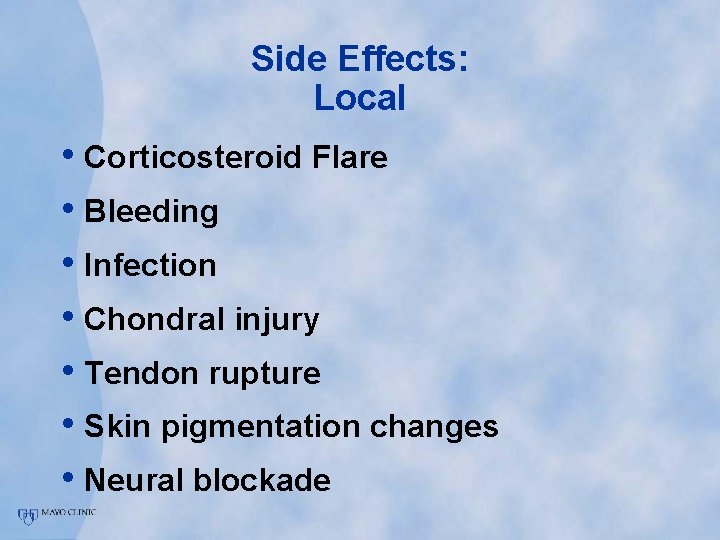
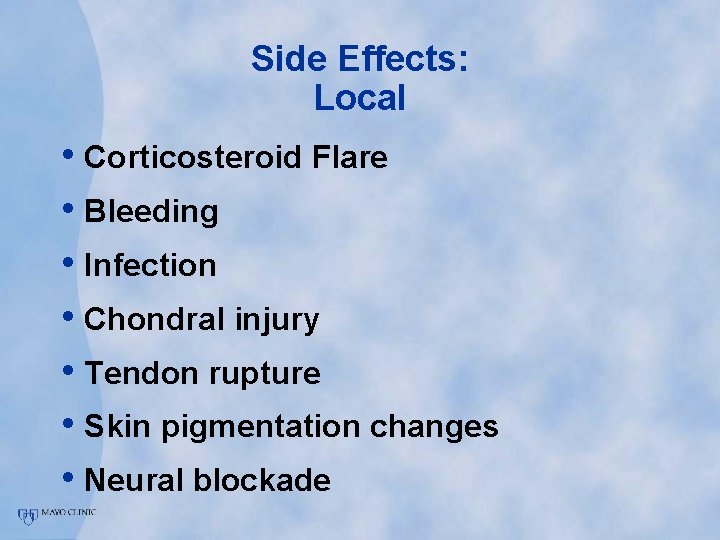
Side Effects: Local • Corticosteroid Flare • Bleeding • Infection • Chondral injury • Tendon rupture • Skin pigmentation changes • Neural blockade
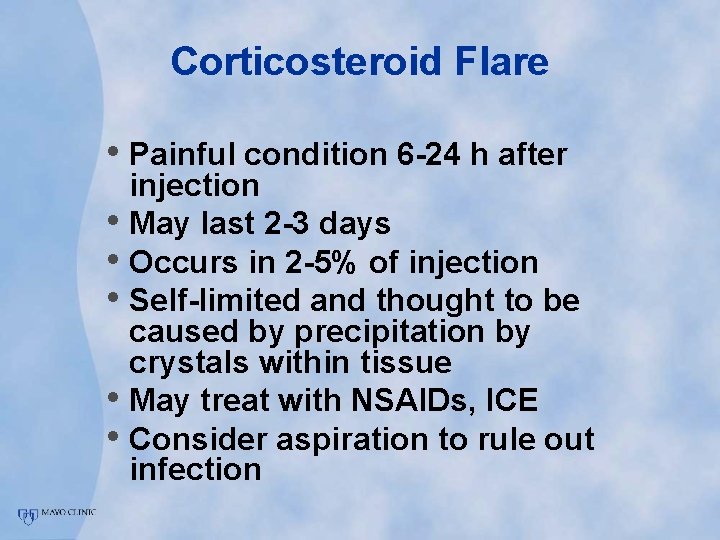
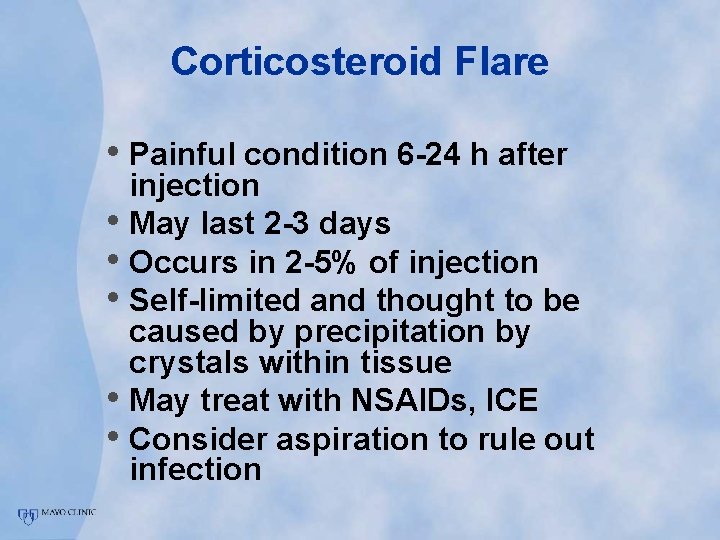
Corticosteroid Flare • Painful condition 6 -24 h after injection • May last 2 -3 days • Occurs in 2 -5% of injection • Self-limited and thought to be caused by precipitation by crystals within tissue • May treat with NSAIDs, ICE • Consider aspiration to rule out infection
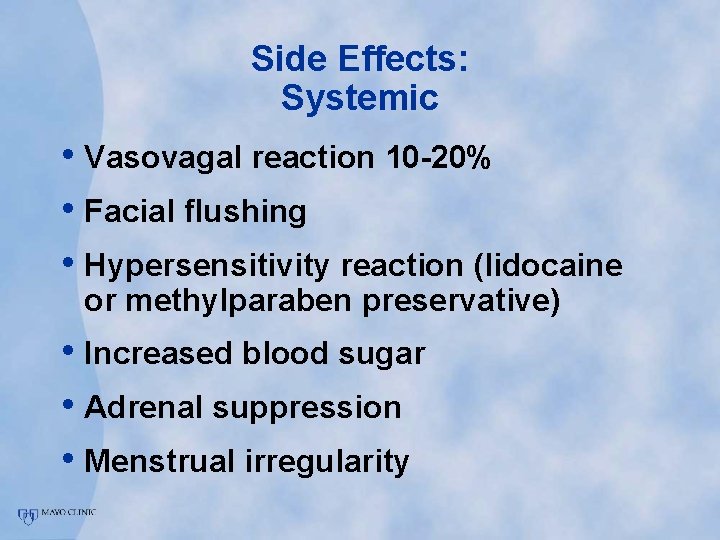
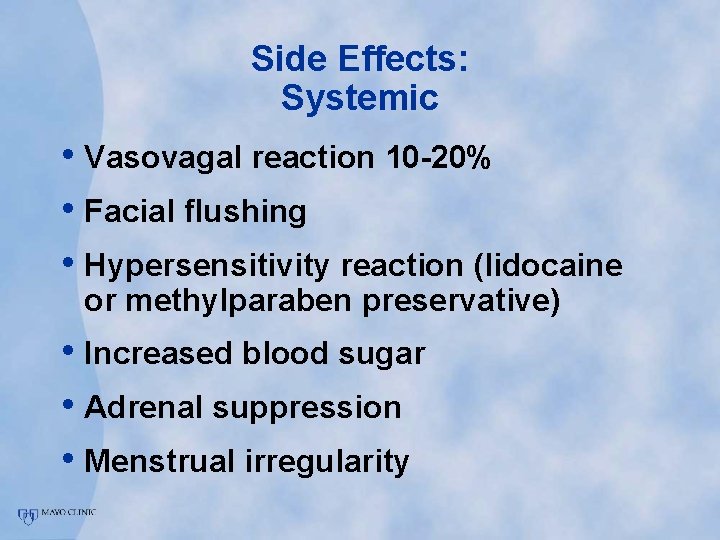
Side Effects: Systemic • Vasovagal reaction 10 -20% • Facial flushing • Hypersensitivity reaction (lidocaine or methylparaben preservative) • Increased blood sugar • Adrenal suppression • Menstrual irregularity
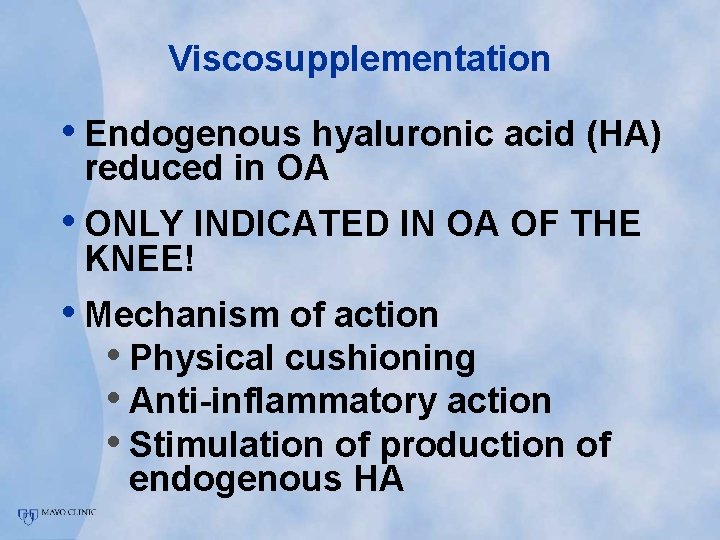
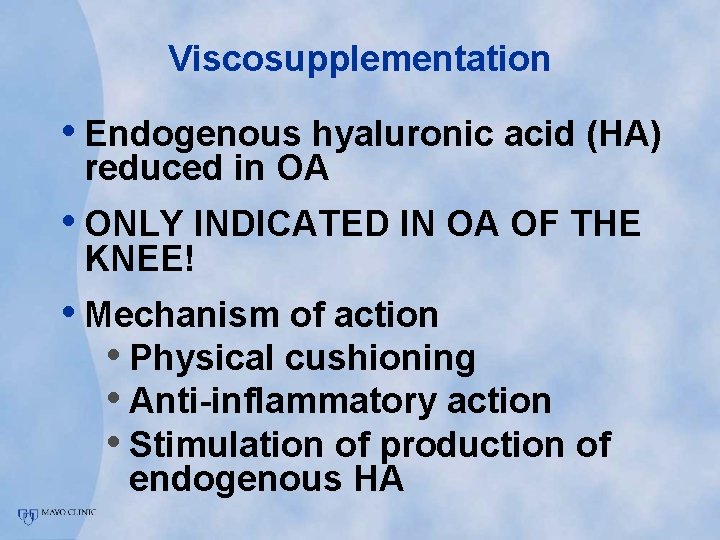
Viscosupplementation • Endogenous hyaluronic acid (HA) reduced in OA • ONLY INDICATED IN OA OF THE KNEE! • Mechanism of action • Physical cushioning • Anti-inflammatory action • Stimulation of production of endogenous HA
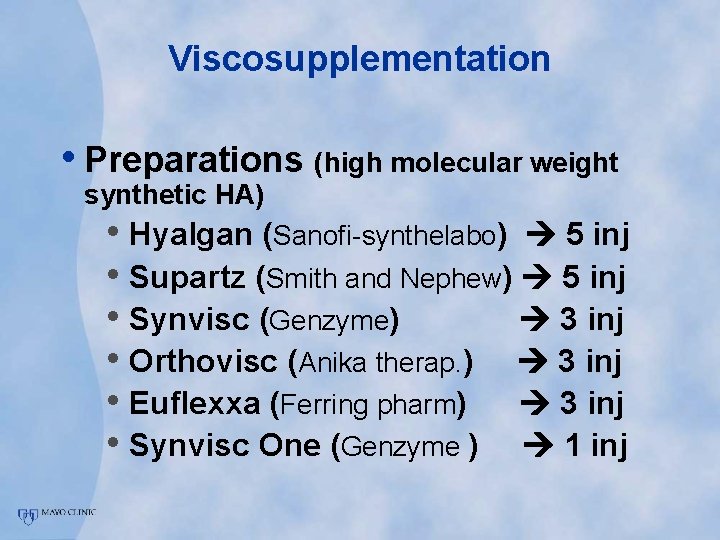
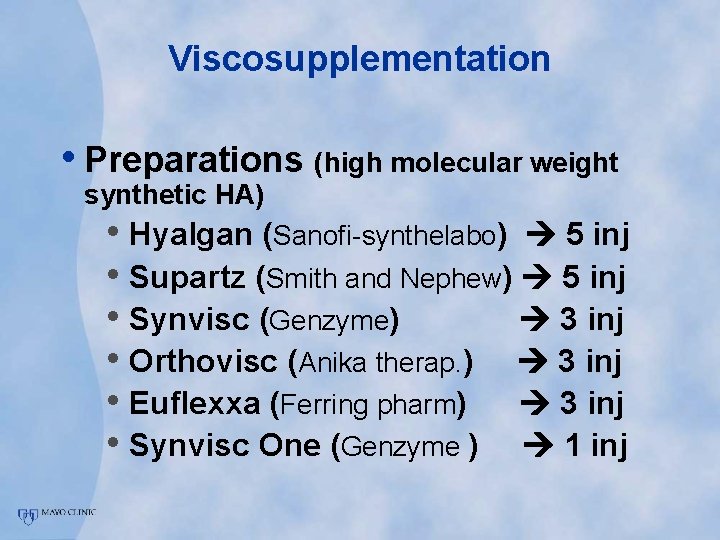
Viscosupplementation • Preparations (high molecular weight synthetic HA) • Hyalgan (Sanofi-synthelabo) 5 inj • Supartz (Smith and Nephew) 5 inj • Synvisc (Genzyme) 3 inj • Orthovisc (Anika therap. ) 3 inj • Euflexxa (Ferring pharm) 3 inj • Synvisc One (Genzyme ) 1 inj
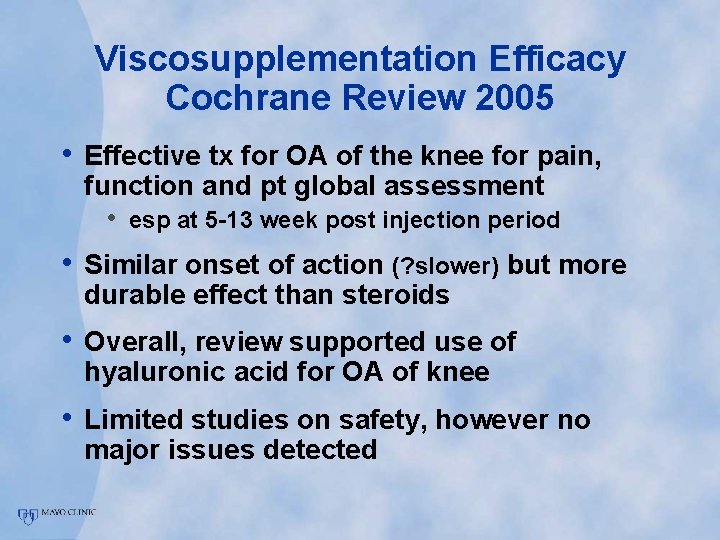
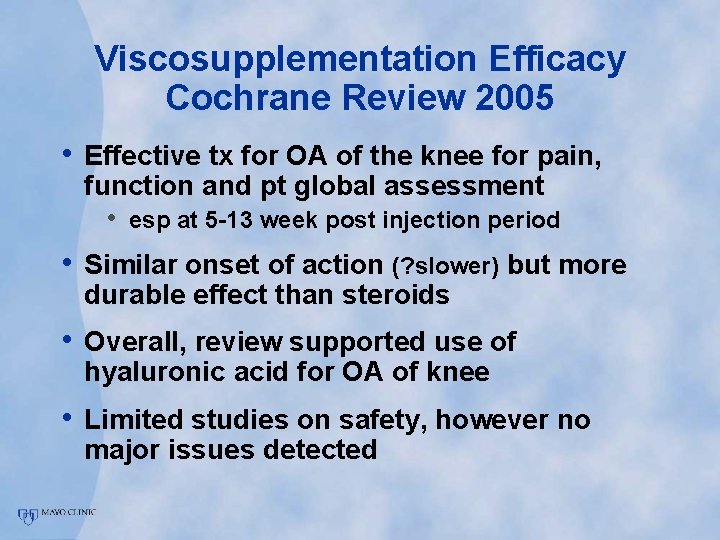
Viscosupplementation Efficacy Cochrane Review 2005 • Effective tx for OA of the knee for pain, function and pt global assessment • esp at 5 -13 week post injection period • Similar onset of action (? slower) but more durable effect than steroids • Overall, review supported use of hyaluronic acid for OA of knee • Limited studies on safety, however no major issues detected
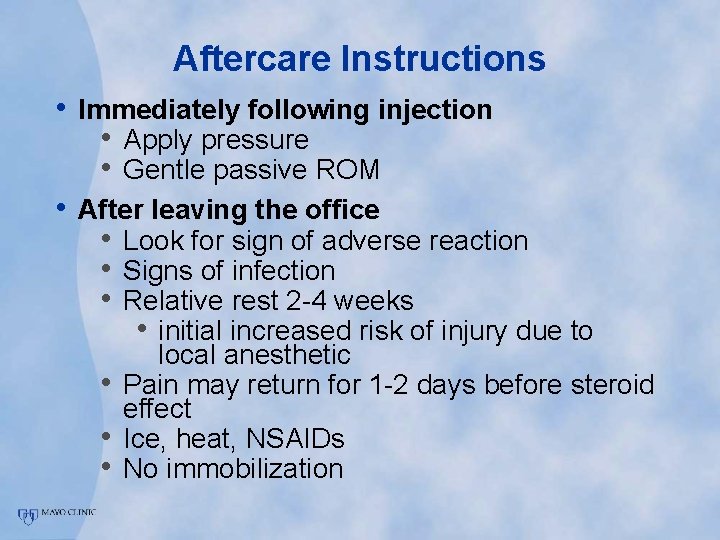
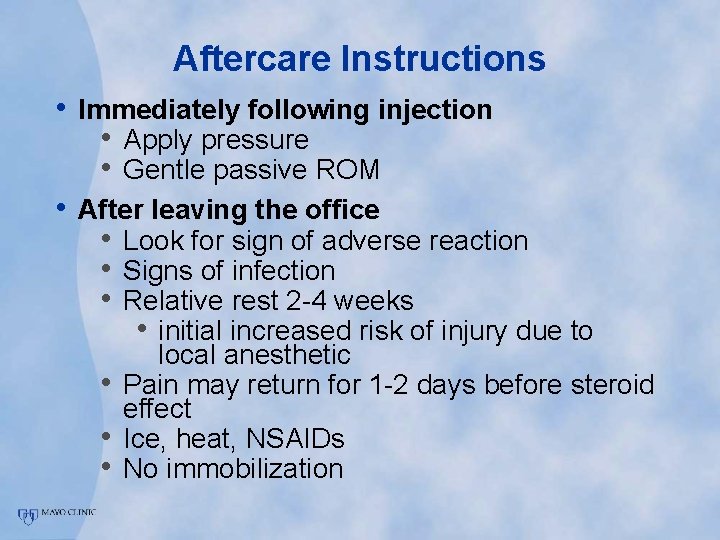
Aftercare Instructions • Immediately following injection • Apply pressure • Gentle passive ROM • After leaving the office • Look for sign of adverse reaction • Signs of infection • Relative rest 2 -4 weeks • initial increased risk of injury due to • • • local anesthetic Pain may return for 1 -2 days before steroid effect Ice, heat, NSAIDs No immobilization
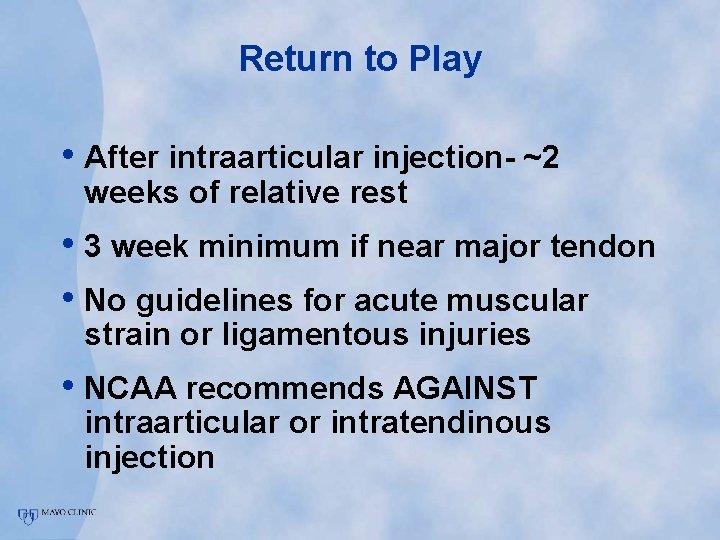
Return to Play • After intraarticular injection- ~2 weeks of relative rest • 3 week minimum if near major tendon • No guidelines for acute muscular strain or ligamentous injuries • NCAA recommends AGAINST intraarticular or intratendinous injection
Injection Technique The SHOULDER
The Shoulder • Subacromial (posterior approach) • Glenohumeral • Acromioclavicular
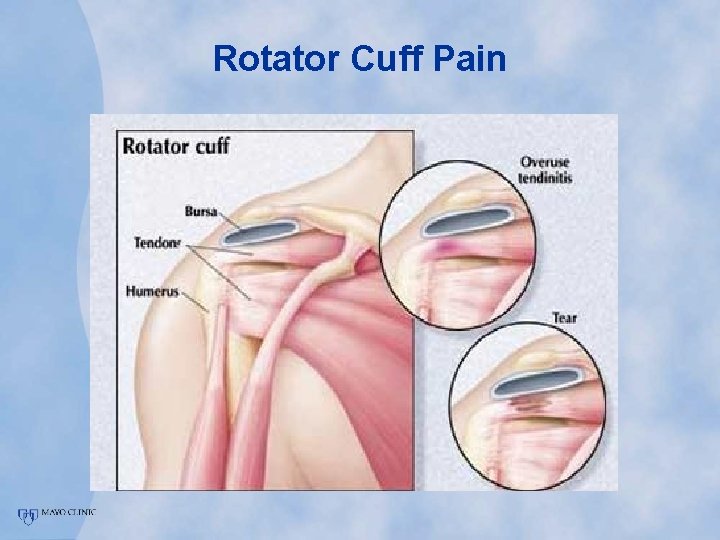
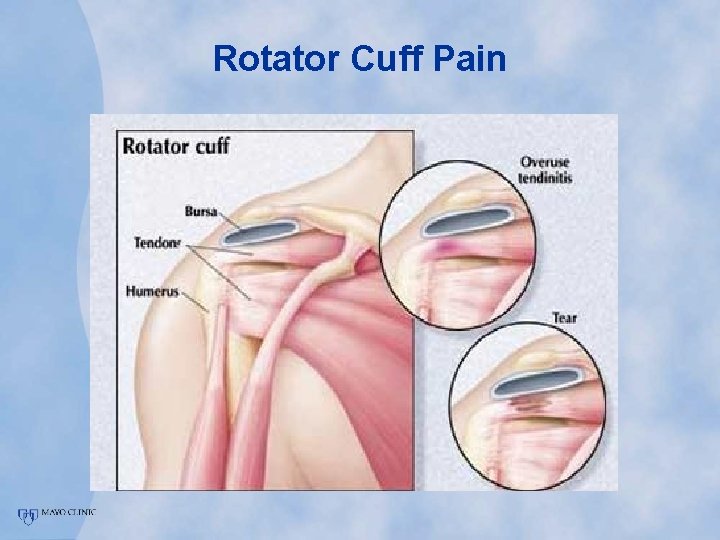
Rotator Cuff Pain
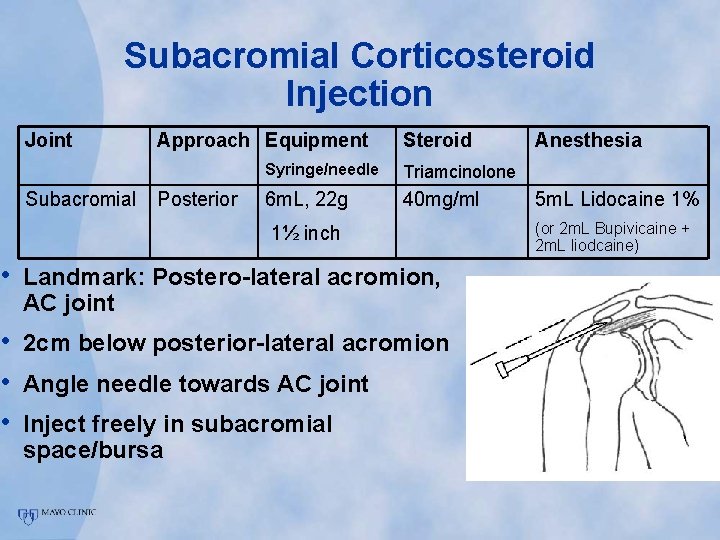
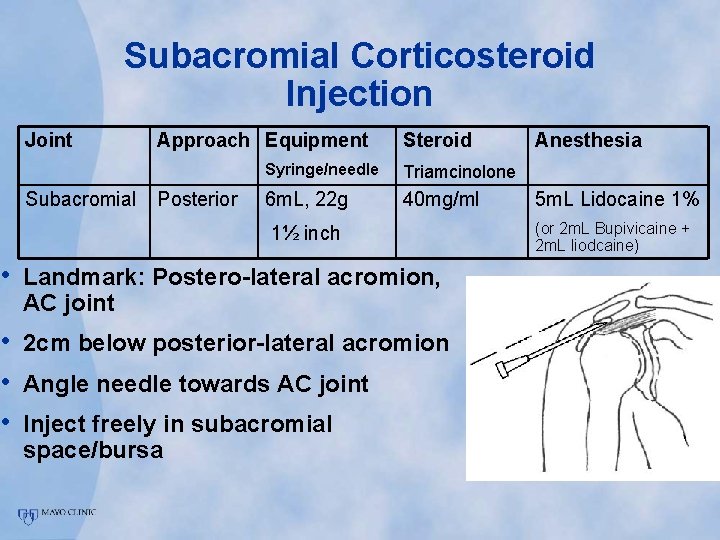
Subacromial Corticosteroid Injection Joint Subacromial Approach Equipment Posterior Steroid Syringe/needle Triamcinolone 6 m. L, 22 g 40 mg/ml 1½ inch • Landmark: Postero-lateral acromion, AC joint • 2 cm below posterior-lateral acromion • Angle needle towards AC joint • Inject freely in subacromial space/bursa Anesthesia 5 m. L Lidocaine 1% (or 2 m. L Bupivicaine + 2 m. L liodcaine)

Subacromial Injection Video
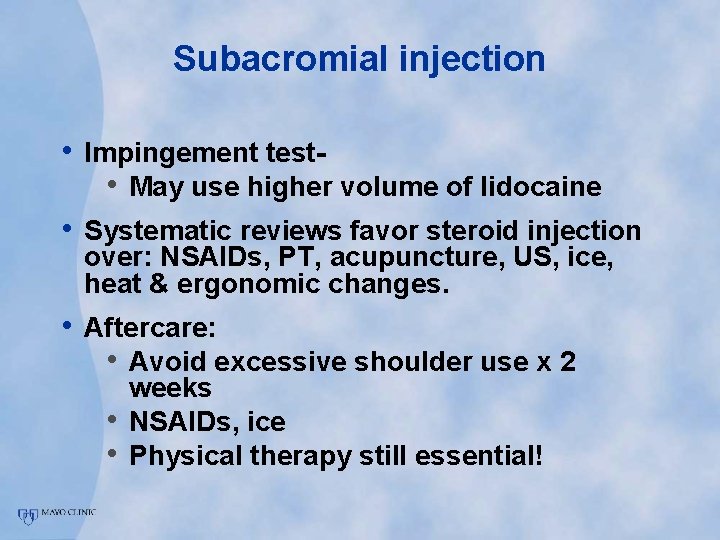
Subacromial injection • Impingement test • May use higher volume of lidocaine • Systematic reviews favor steroid injection over: NSAIDs, PT, acupuncture, US, ice, heat & ergonomic changes. • Aftercare: • Avoid excessive shoulder use x 2 • • weeks NSAIDs, ice Physical therapy still essential!
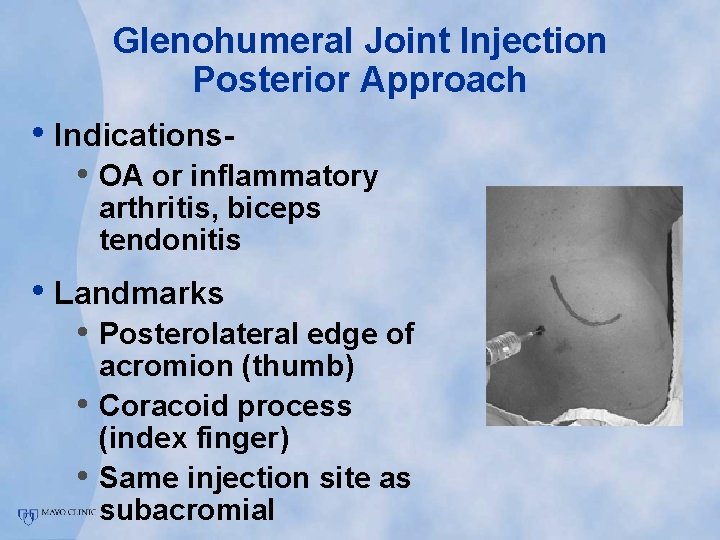
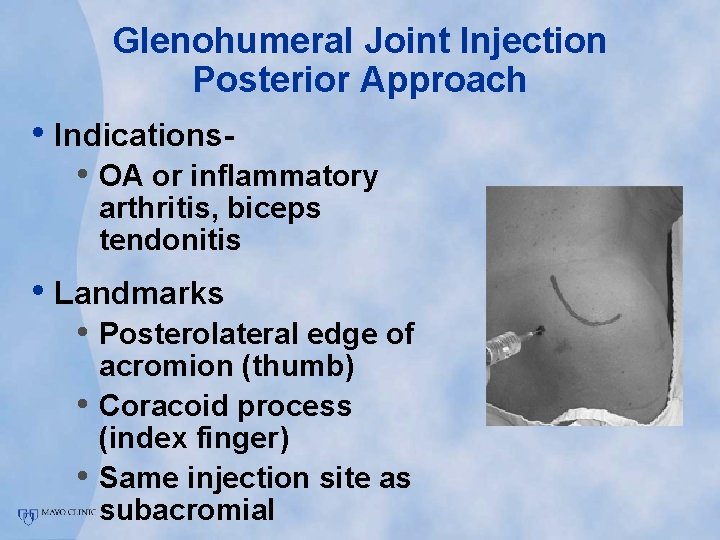
Glenohumeral Joint Injection Posterior Approach • Indications- • OA or inflammatory arthritis, biceps tendonitis • Landmarks • Posterolateral edge of • • acromion (thumb) Coracoid process (index finger) Same injection site as subacromial
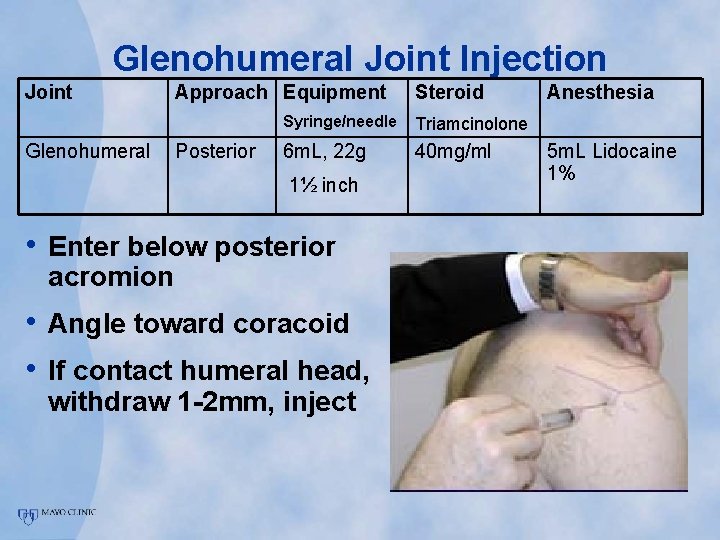
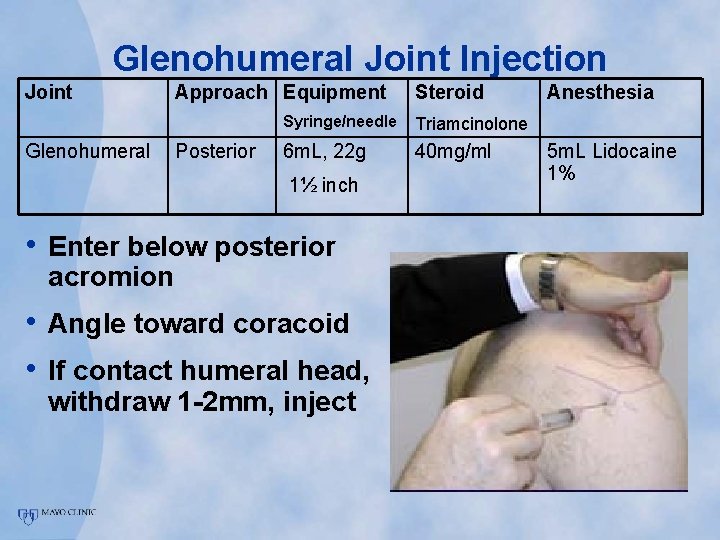
Glenohumeral Joint Injection Joint Glenohumeral Approach Equipment Posterior Steroid Syringe/needle Triamcinolone 6 m. L, 22 g 40 mg/ml 1½ inch • Enter below posterior acromion • Angle toward coracoid • If contact humeral head, withdraw 1 -2 mm, inject Anesthesia 5 m. L Lidocaine 1%
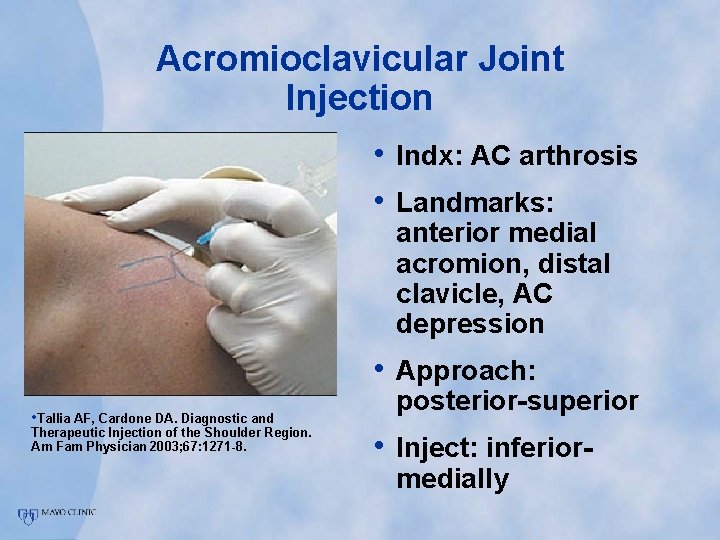
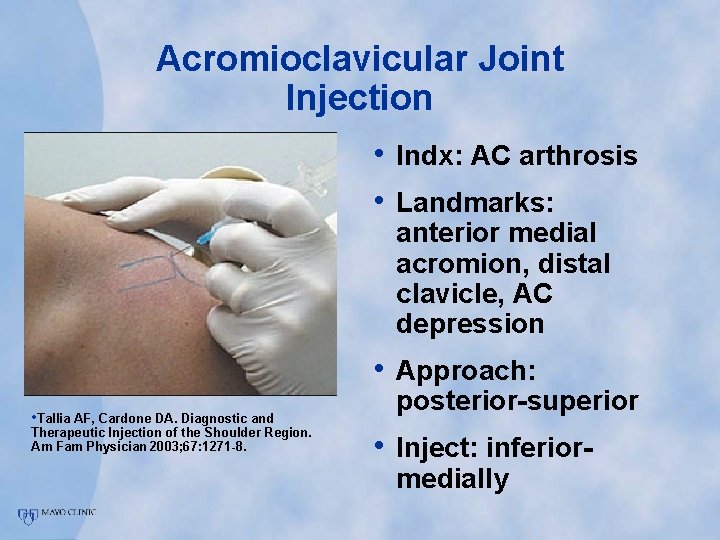
Acromioclavicular Joint Injection • Indx: AC arthrosis • Landmarks: anterior medial acromion, distal clavicle, AC depression • Approach: • Tallia AF, Cardone DA. Diagnostic and Therapeutic Injection of the Shoulder Region. Am Fam Physician 2003; 67: 1271 -8. posterior-superior • Inject: inferiormedially
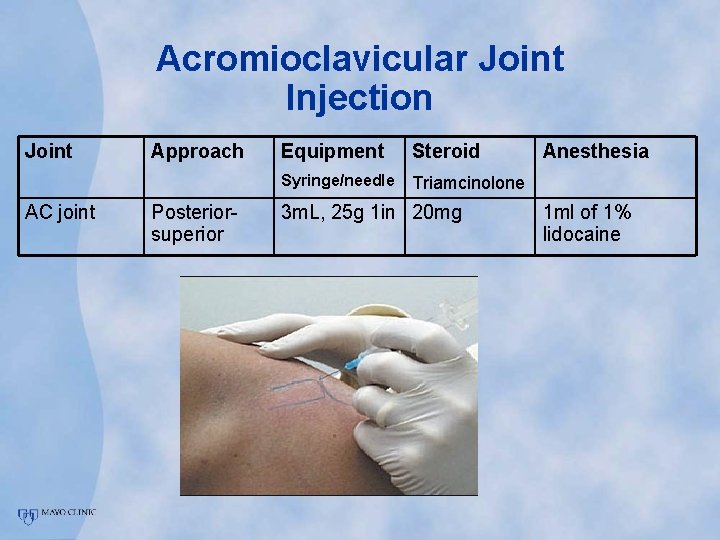
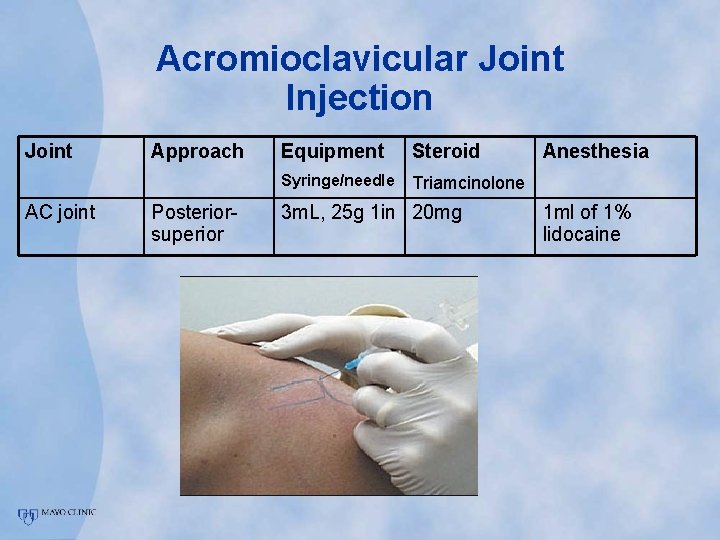
Acromioclavicular Joint Injection Joint AC joint Approach Posteriorsuperior Equipment Steroid Syringe/needle Triamcinolone 3 m. L, 25 g 1 in 20 mg Anesthesia 1 ml of 1% lidocaine
Injection Technique The ELBOW
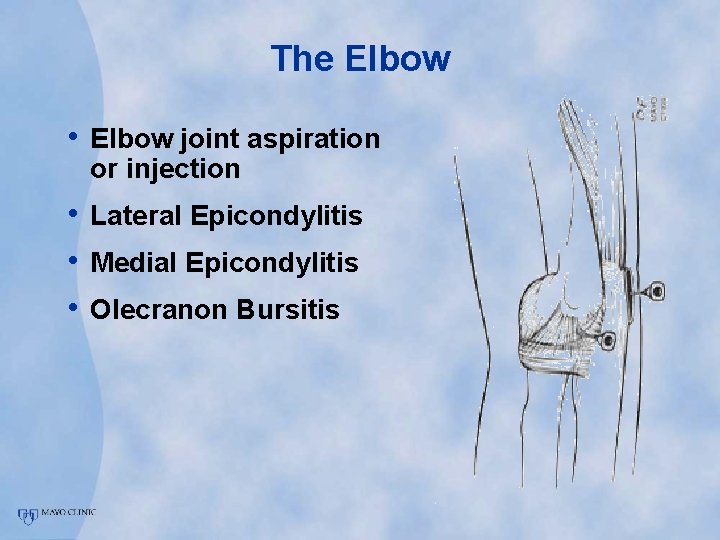
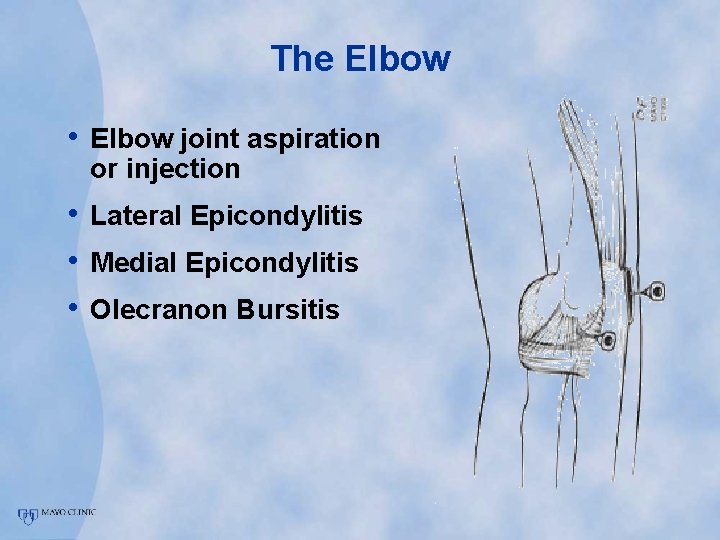
The Elbow • Elbow joint aspiration or injection • Lateral Epicondylitis • Medial Epicondylitis • Olecranon Bursitis
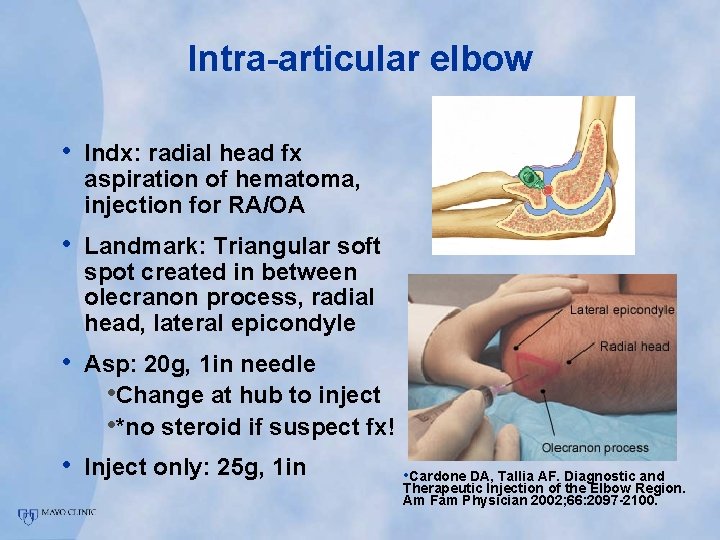
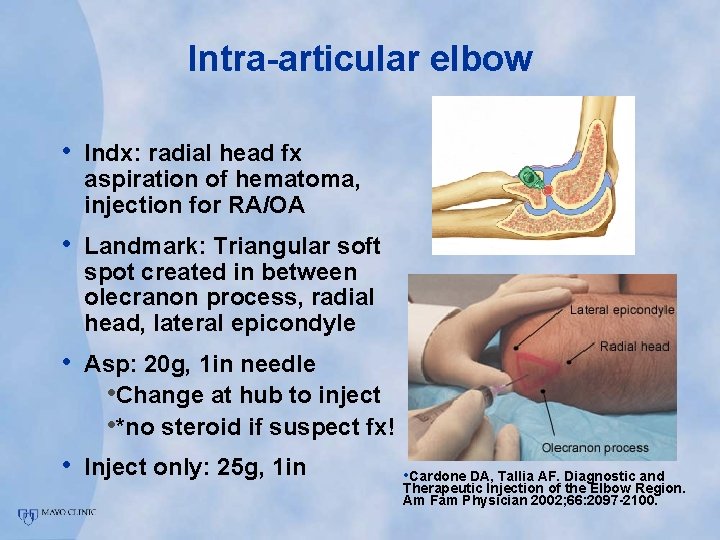
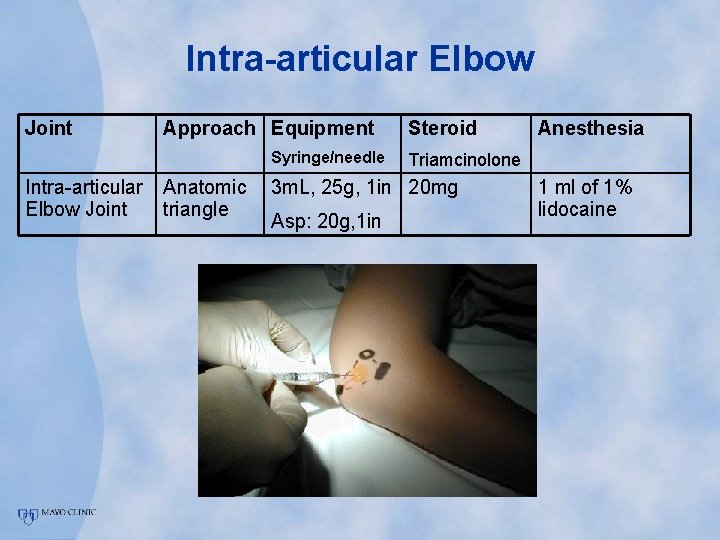
Intra-articular elbow • Indx: radial head fx aspiration of hematoma, injection for RA/OA • Landmark: Triangular soft spot created in between olecranon process, radial head, lateral epicondyle • Asp: 20 g, 1 in needle • Change at hub to inject • *no steroid if suspect fx! • Inject only: 25 g, 1 in • Cardone DA, Tallia AF. Diagnostic and Therapeutic Injection of the Elbow Region. Am Fam Physician 2002; 66: 2097 -2100.
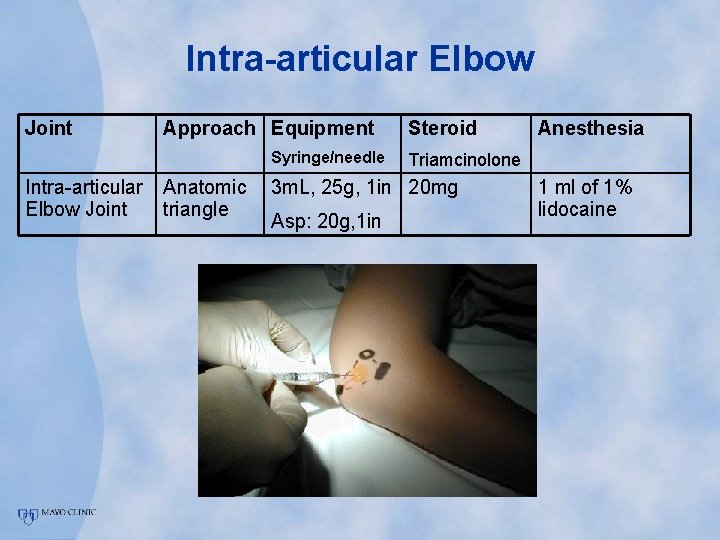
Intra-articular Elbow Joint Approach Equipment Syringe/needle Intra-articular Elbow Joint Anatomic triangle Steroid Triamcinolone 3 m. L, 25 g, 1 in 20 mg Asp: 20 g, 1 in Anesthesia 1 ml of 1% lidocaine
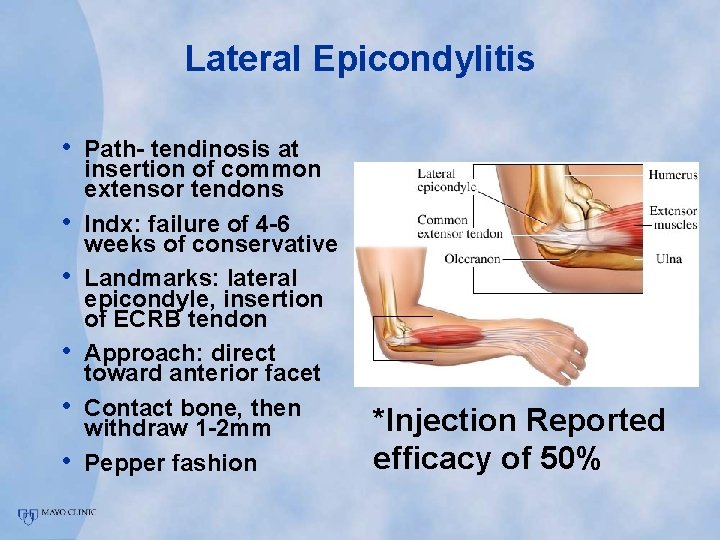
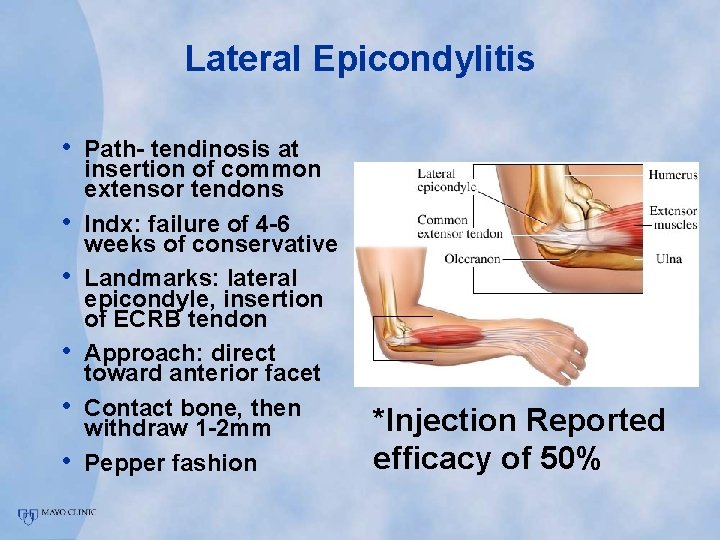
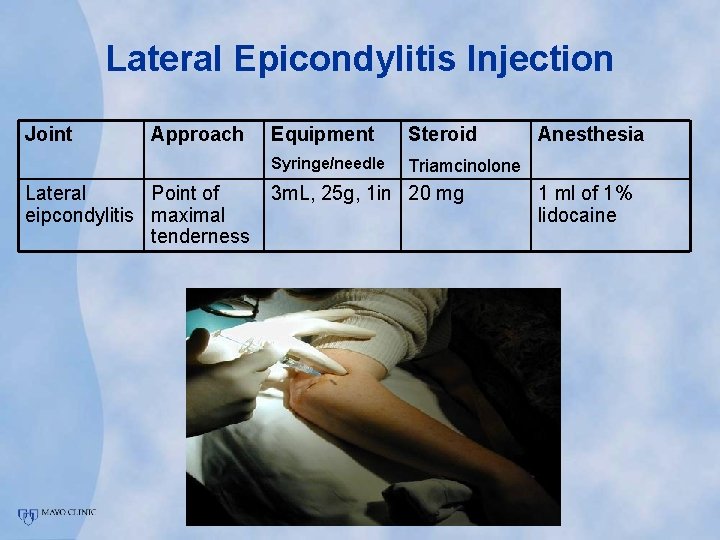
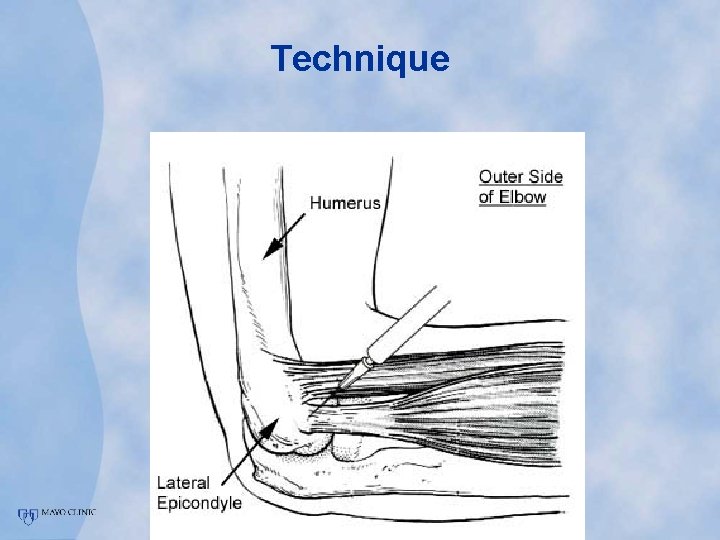
Lateral Epicondylitis • Path- tendinosis at • • • insertion of common extensor tendons Indx: failure of 4 -6 weeks of conservative Landmarks: lateral epicondyle, insertion of ECRB tendon Approach: direct toward anterior facet Contact bone, then withdraw 1 -2 mm Pepper fashion *Injection Reported efficacy of 50%
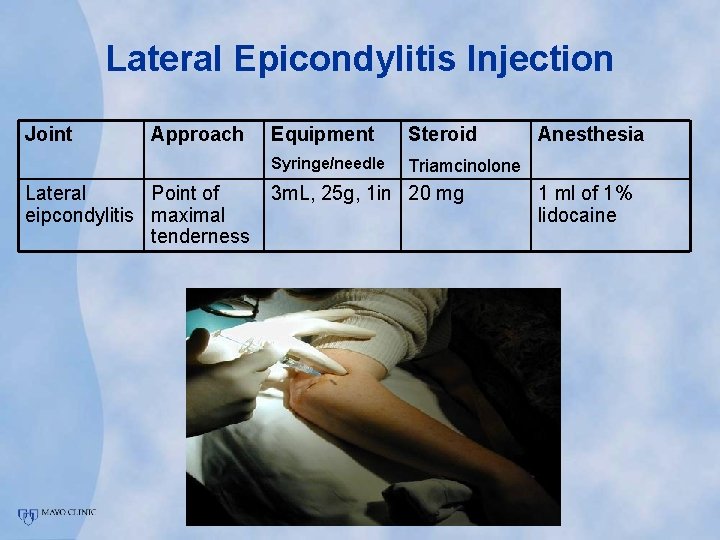
Lateral Epicondylitis Injection Joint Approach Lateral Point of eipcondylitis maximal tenderness Equipment Steroid Syringe/needle Triamcinolone 3 m. L, 25 g, 1 in 20 mg Anesthesia 1 ml of 1% lidocaine
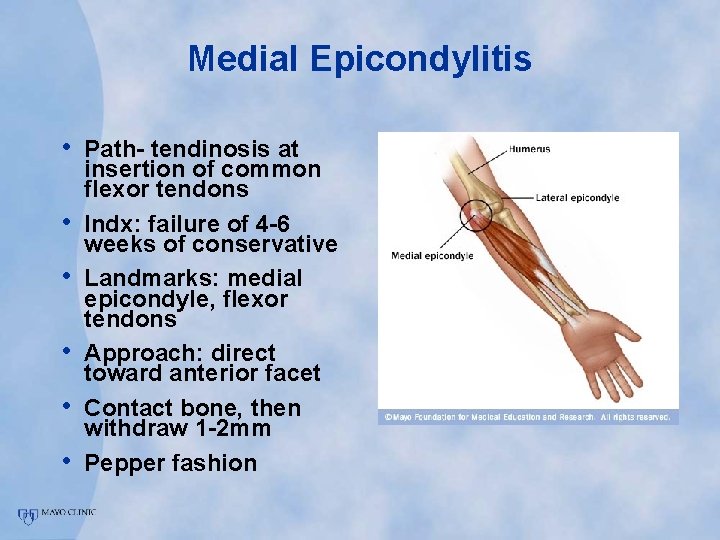
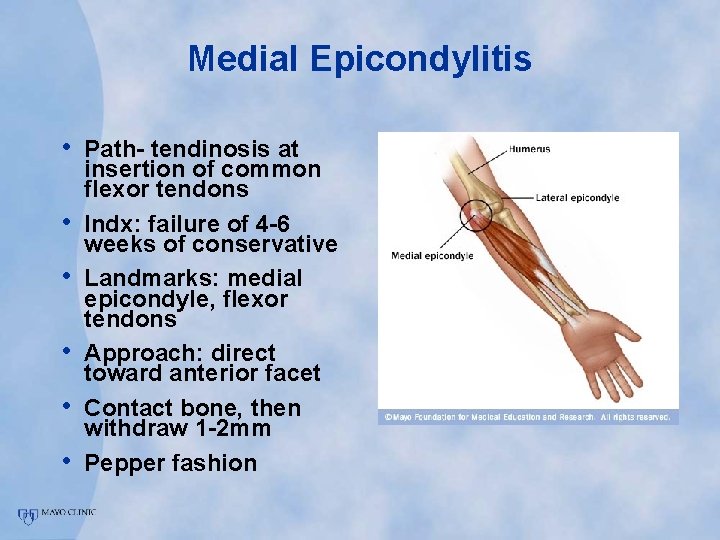
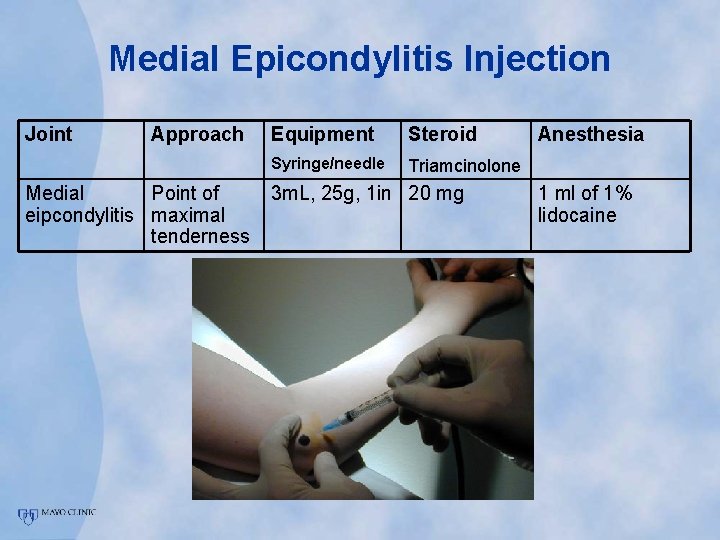
Medial Epicondylitis • Path- tendinosis at • • • insertion of common flexor tendons Indx: failure of 4 -6 weeks of conservative Landmarks: medial epicondyle, flexor tendons Approach: direct toward anterior facet Contact bone, then withdraw 1 -2 mm Pepper fashion
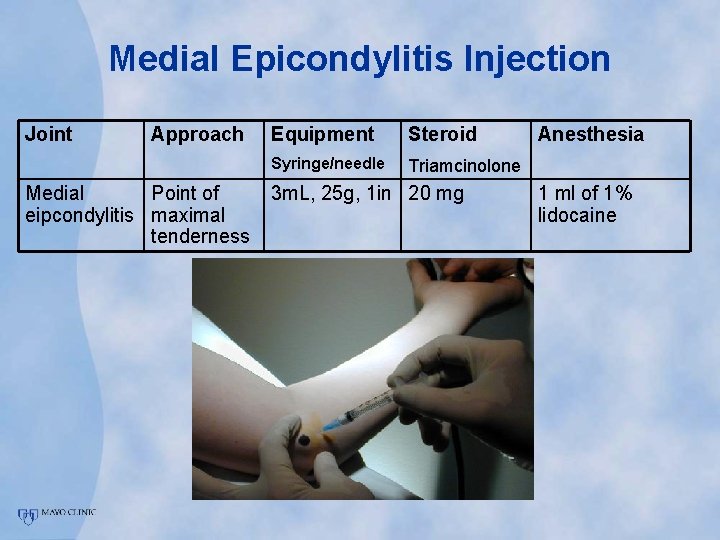
Medial Epicondylitis Injection Joint Approach Medial Point of eipcondylitis maximal tenderness Equipment Steroid Syringe/needle Triamcinolone 3 m. L, 25 g, 1 in 20 mg Anesthesia 1 ml of 1% lidocaine
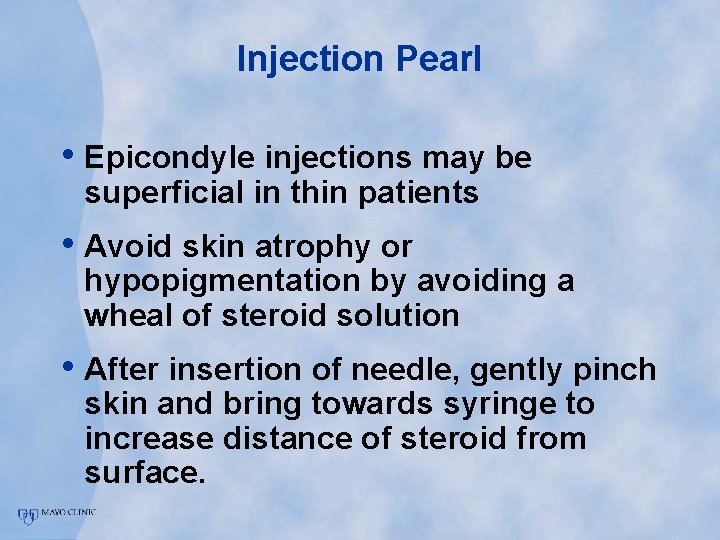
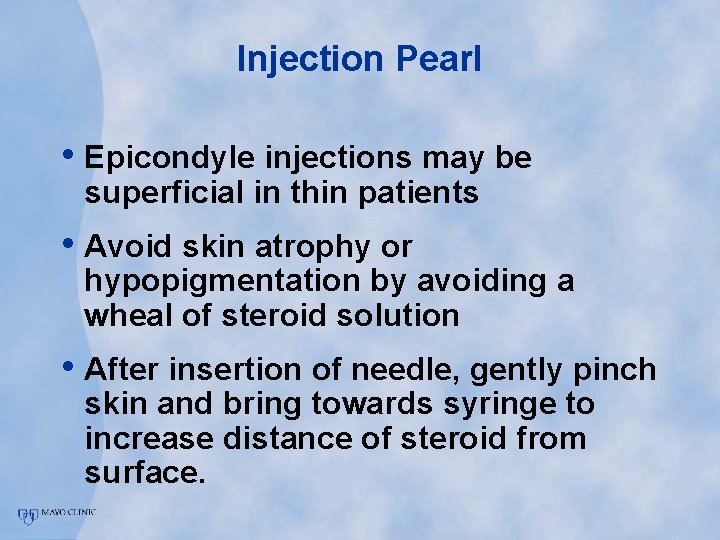
Injection Pearl • Epicondyle injections may be superficial in thin patients • Avoid skin atrophy or hypopigmentation by avoiding a wheal of steroid solution • After insertion of needle, gently pinch skin and bring towards syringe to increase distance of steroid from surface.
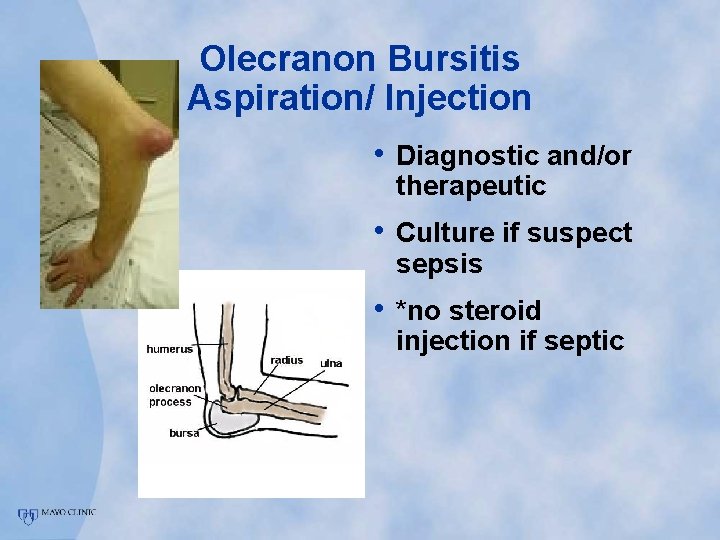
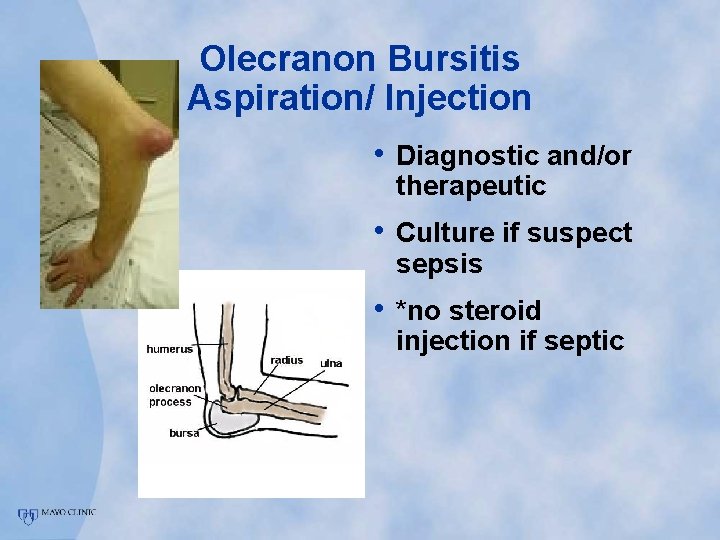
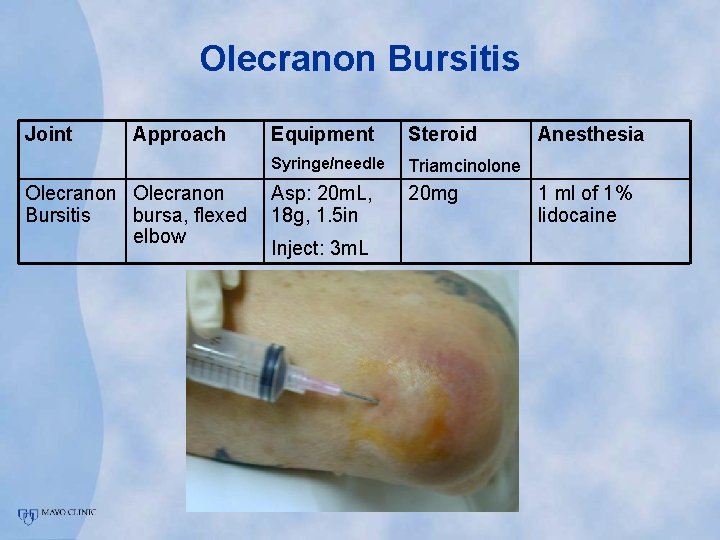
Olecranon Bursitis Aspiration/ Injection • Diagnostic and/or therapeutic • Culture if suspect sepsis • *no steroid injection if septic
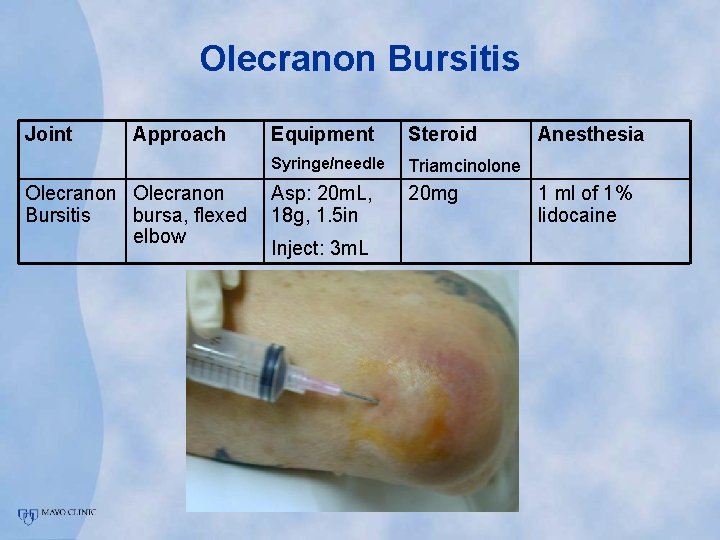
Olecranon Bursitis Joint Approach Olecranon Bursitis bursa, flexed elbow Equipment Steroid Syringe/needle Triamcinolone Asp: 20 m. L, 18 g, 1. 5 in 20 mg Inject: 3 m. L Anesthesia 1 ml of 1% lidocaine
Injection Technique The WRIST and HAND
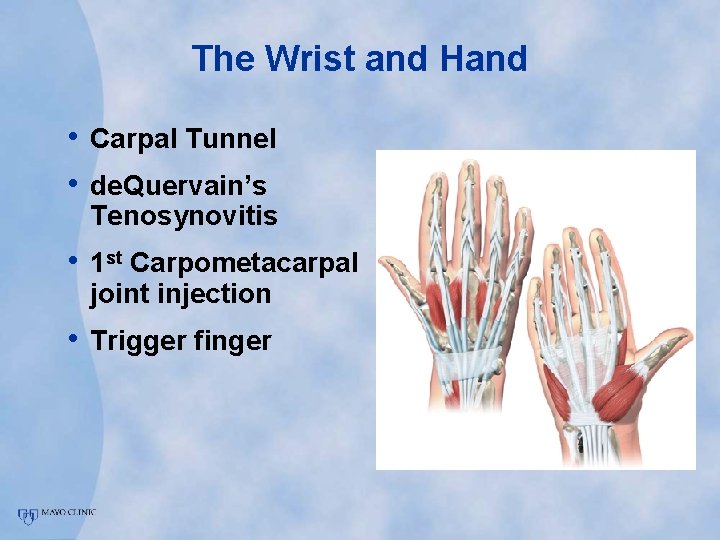
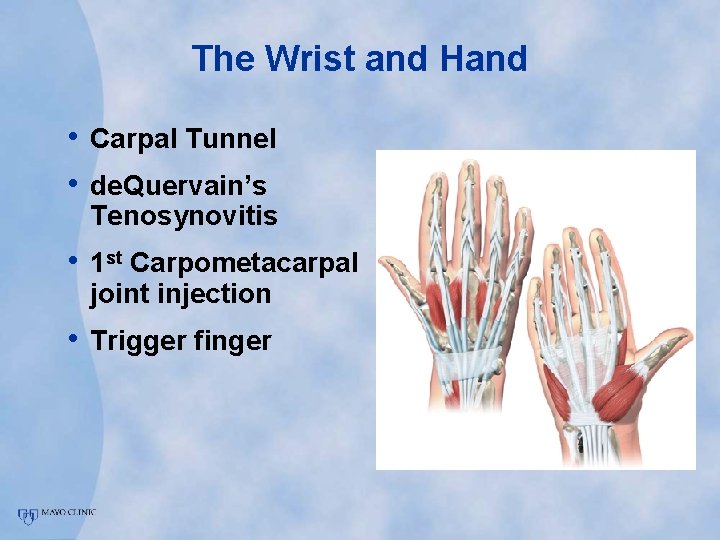
The Wrist and Hand • Carpal Tunnel • de. Quervain’s Tenosynovitis • 1 st Carpometacarpal joint injection • Trigger finger
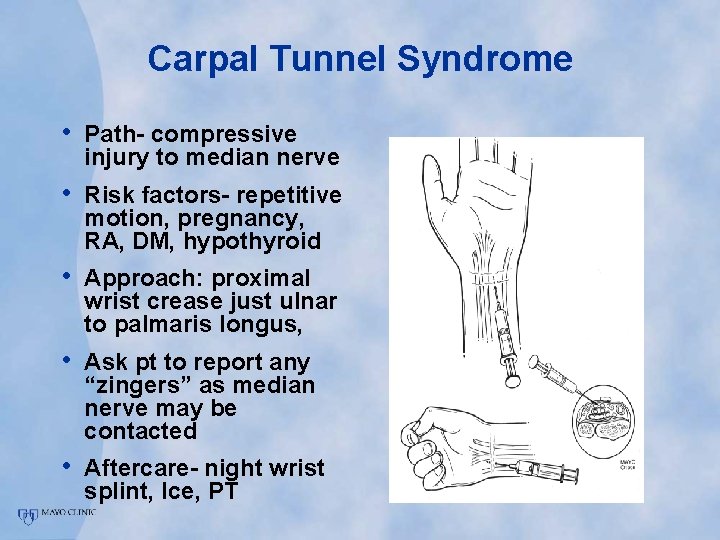
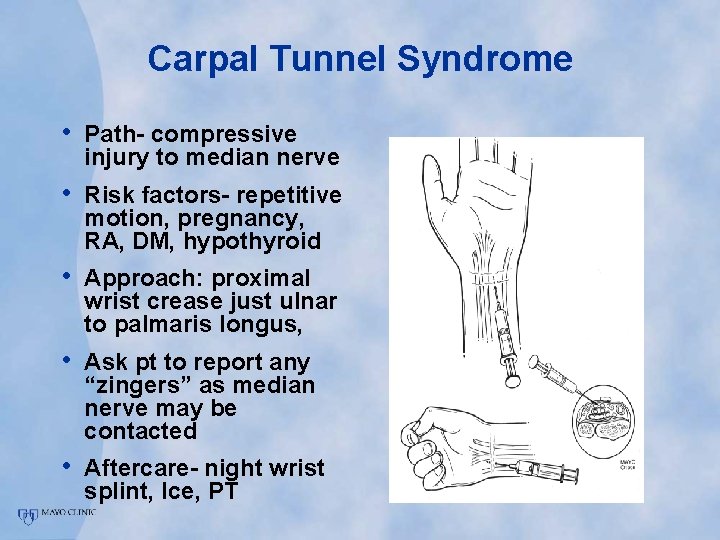
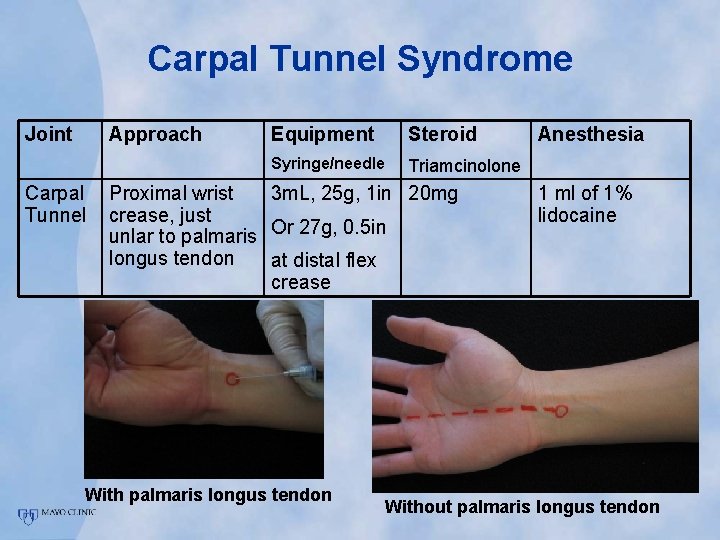
Carpal Tunnel Syndrome • Path- compressive injury to median nerve • Risk factors- repetitive motion, pregnancy, RA, DM, hypothyroid • Approach: proximal wrist crease just ulnar to palmaris longus, • Ask pt to report any “zingers” as median nerve may be contacted • Aftercare- night wrist splint, Ice, PT
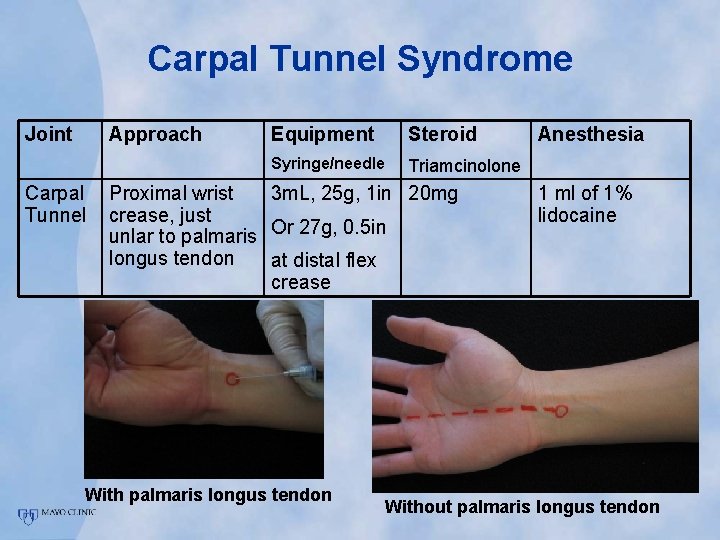
Carpal Tunnel Syndrome Joint Approach Carpal Tunnel Equipment Steroid Syringe/needle Triamcinolone Proximal wrist 3 m. L, 25 g, 1 in 20 mg crease, just unlar to palmaris Or 27 g, 0. 5 in longus tendon at distal flex crease With palmaris longus tendon Anesthesia 1 ml of 1% lidocaine Without palmaris longus tendon
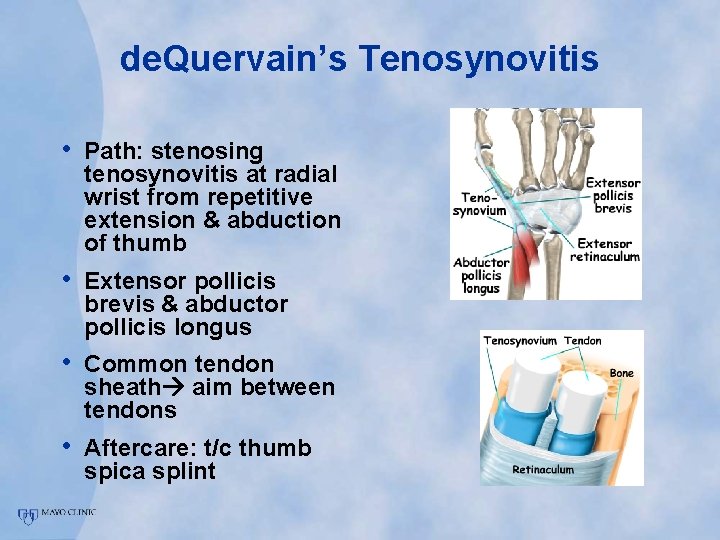
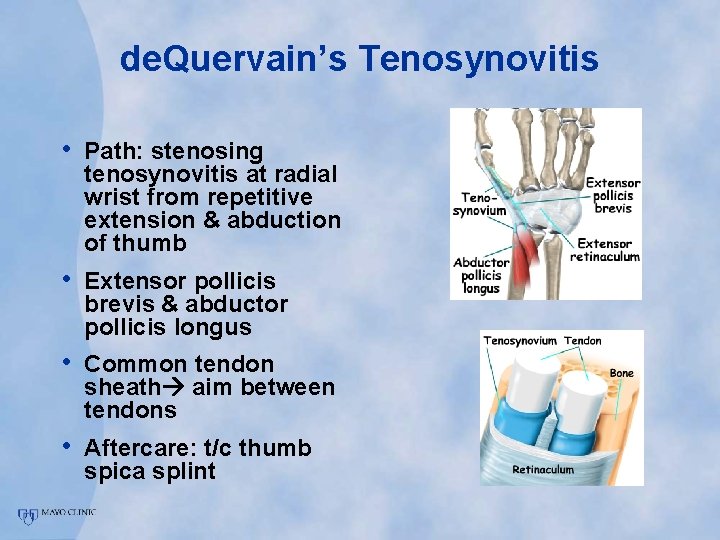
de. Quervain’s Tenosynovitis • Path: stenosing tenosynovitis at radial wrist from repetitive extension & abduction of thumb • Extensor pollicis brevis & abductor pollicis longus • Common tendon sheath aim between tendons • Aftercare: t/c thumb spica splint
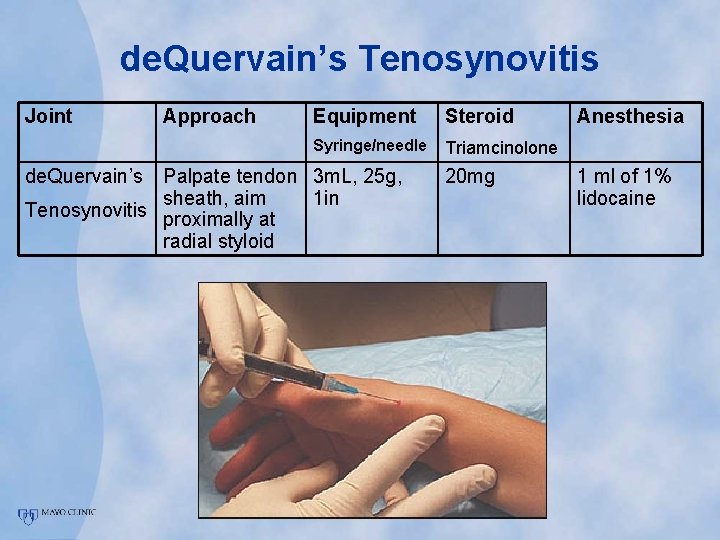
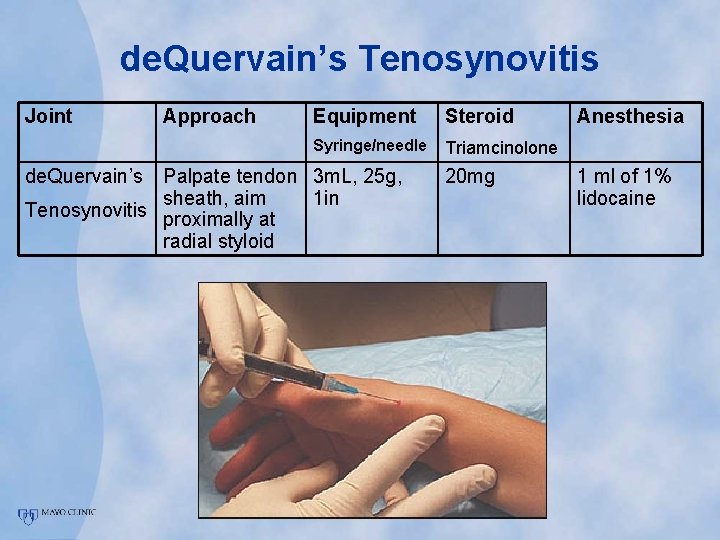
de. Quervain’s Tenosynovitis Joint de. Quervain’s Approach Equipment Steroid Syringe/needle Triamcinolone Palpate tendon 3 m. L, 25 g, sheath, aim 1 in Tenosynovitis proximally at radial styloid 20 mg Anesthesia 1 ml of 1% lidocaine
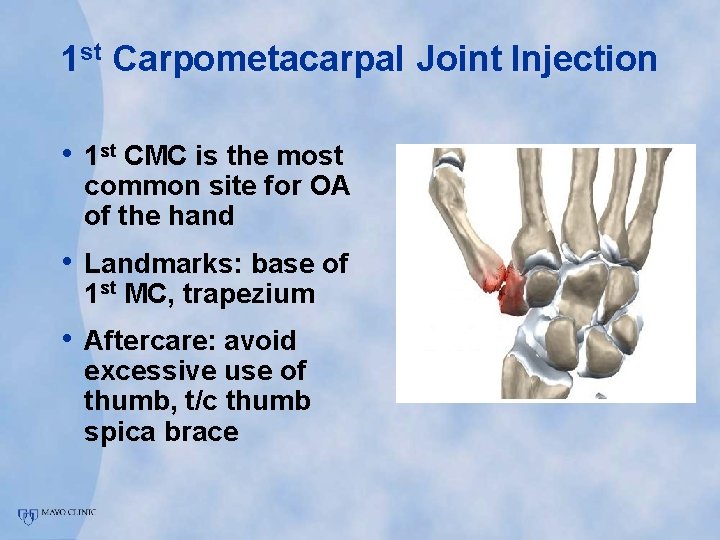
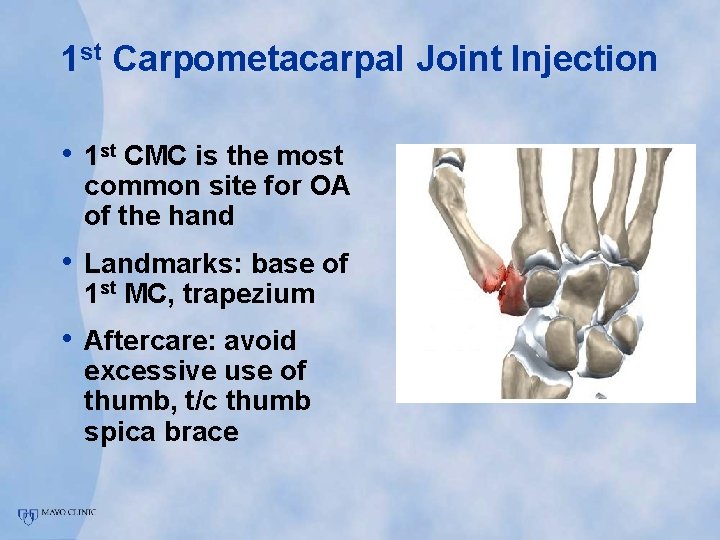
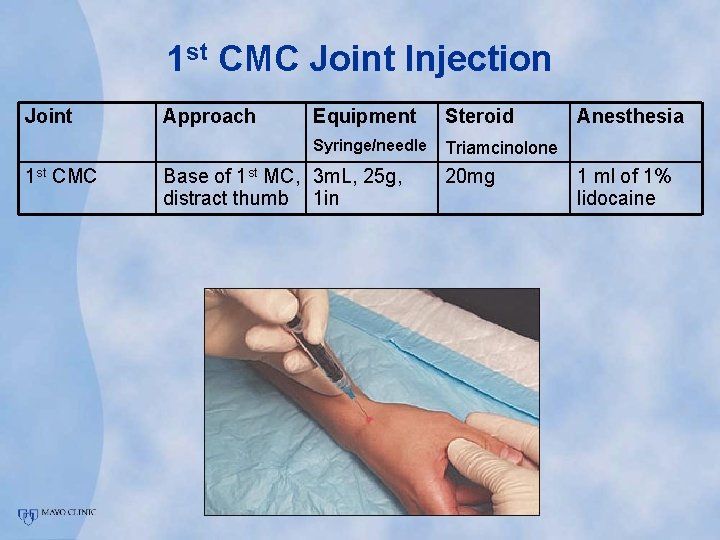
1 st Carpometacarpal Joint Injection • 1 st CMC is the most common site for OA of the hand • Landmarks: base of 1 st MC, trapezium • Aftercare: avoid excessive use of thumb, t/c thumb spica brace
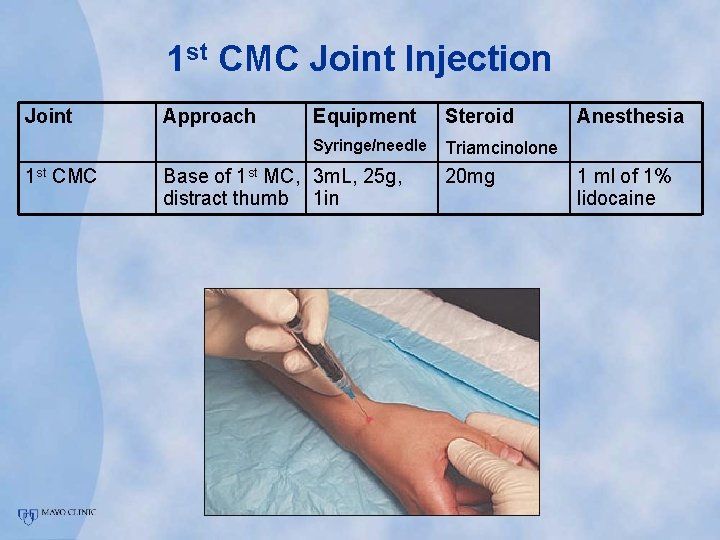
1 st CMC Joint Injection Joint 1 st CMC Approach Equipment Steroid Syringe/needle Triamcinolone Base of 1 st MC, 3 m. L, 25 g, distract thumb 1 in 20 mg Anesthesia 1 ml of 1% lidocaine

1 st CMC Joint Injection Video

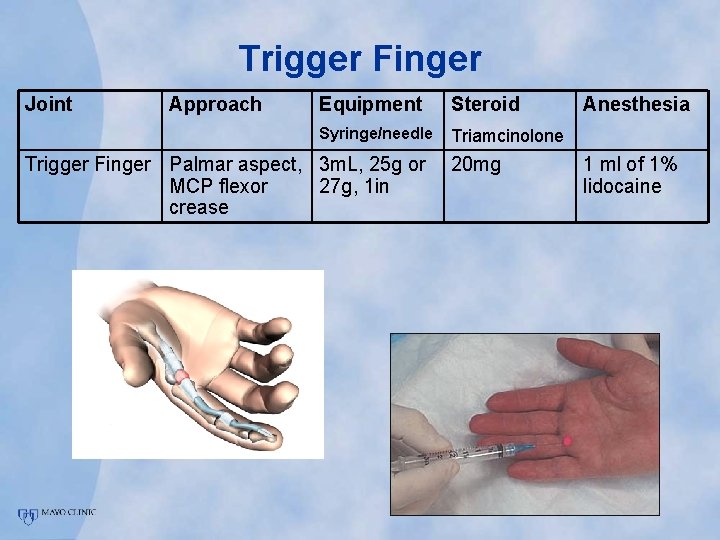
Trigger Finger • Tenosynovitis of flexor tendons • Triggering occurs at A 1 pulley • Effective treatment can avoid surgery • Risk factors- RA, DM • Aftercare- avoid excessive hand grip for 2 weeks
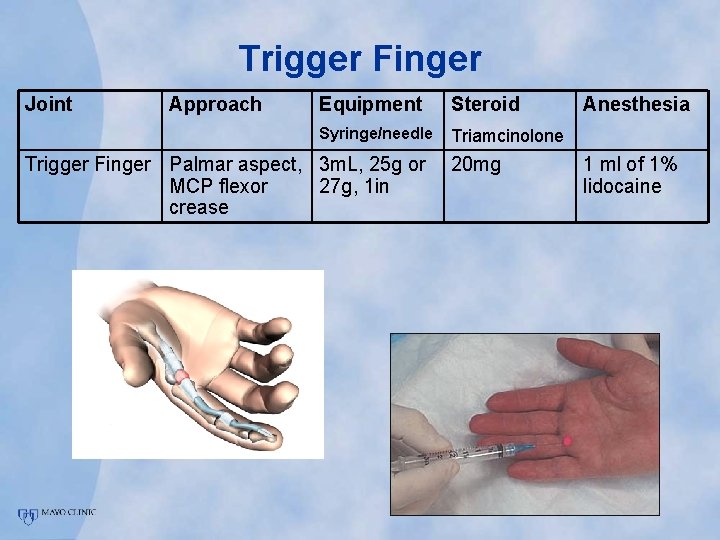
Trigger Finger Joint Approach Equipment Steroid Syringe/needle Triamcinolone Trigger Finger Palmar aspect, 3 m. L, 25 g or MCP flexor 27 g, 1 in crease 20 mg Anesthesia 1 ml of 1% lidocaine
Injection Technique The Lower Extremities
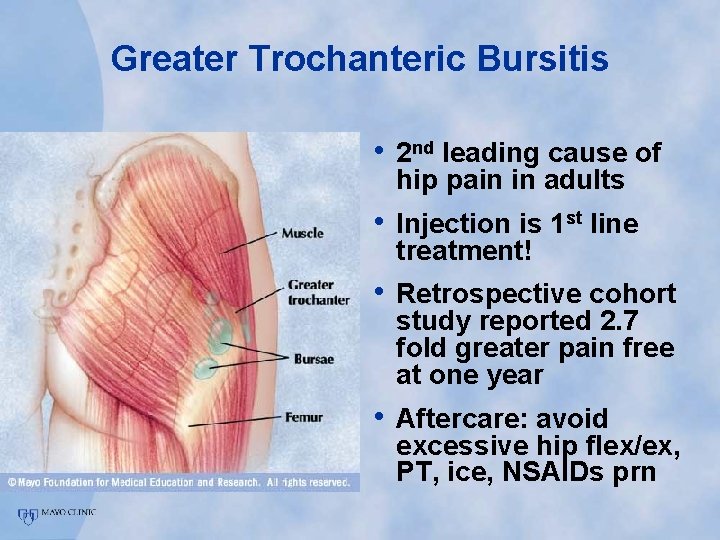
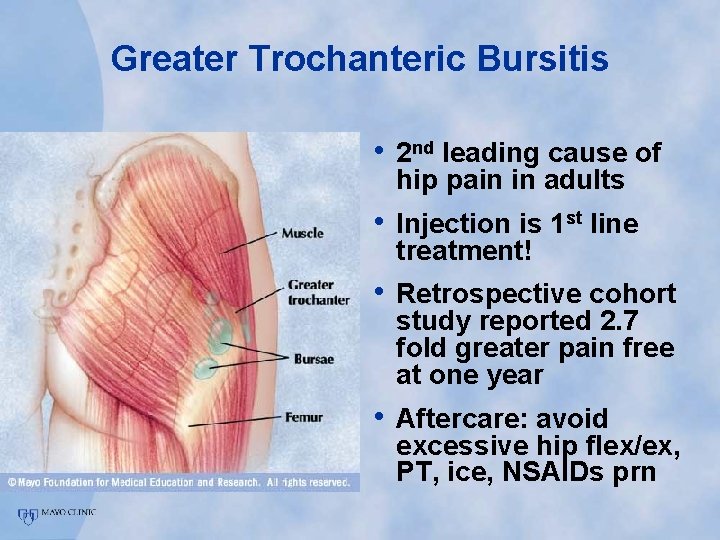
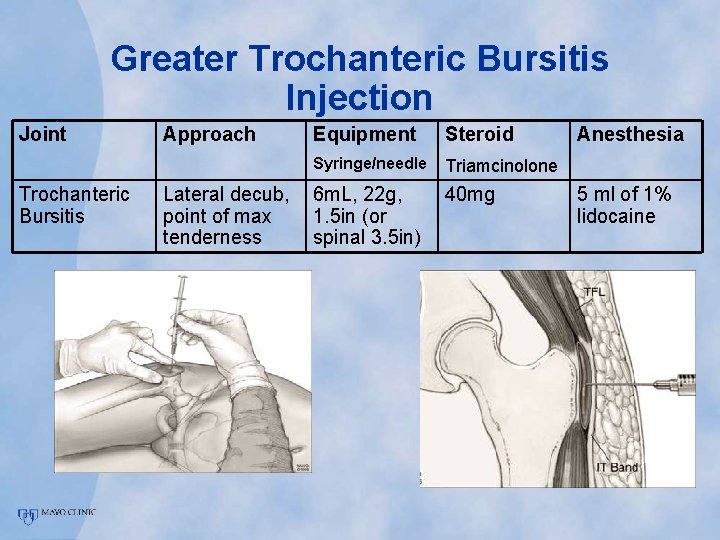
Greater Trochanteric Bursitis • 2 nd leading cause of hip pain in adults • Injection is 1 st line treatment! • Retrospective cohort study reported 2. 7 fold greater pain free at one year • Aftercare: avoid excessive hip flex/ex, PT, ice, NSAIDs prn
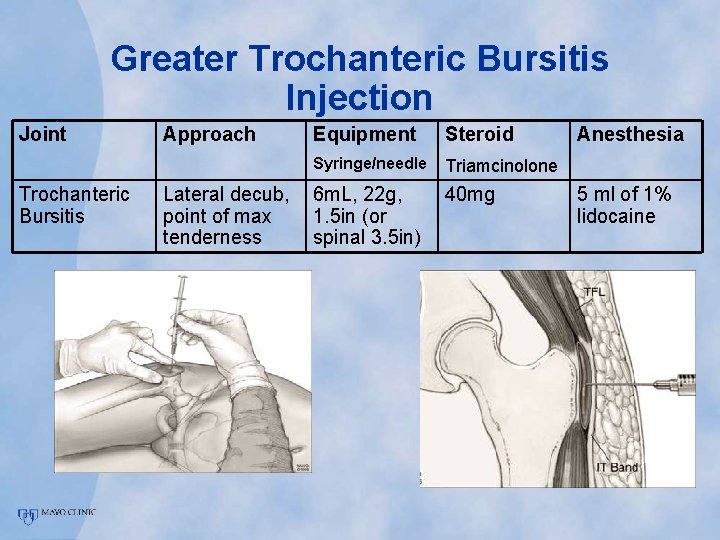
Greater Trochanteric Bursitis Injection Joint Trochanteric Bursitis Approach Lateral decub, point of max tenderness Equipment Steroid Syringe/needle Triamcinolone 6 m. L, 22 g, 1. 5 in (or spinal 3. 5 in) 40 mg Anesthesia 5 ml of 1% lidocaine
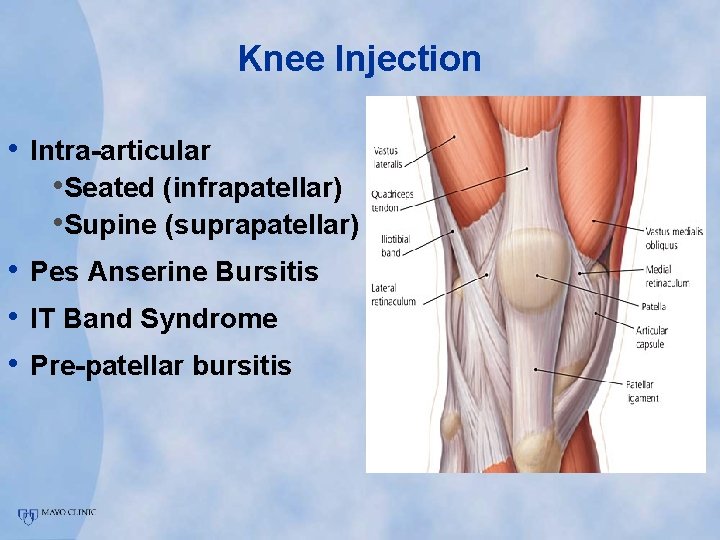
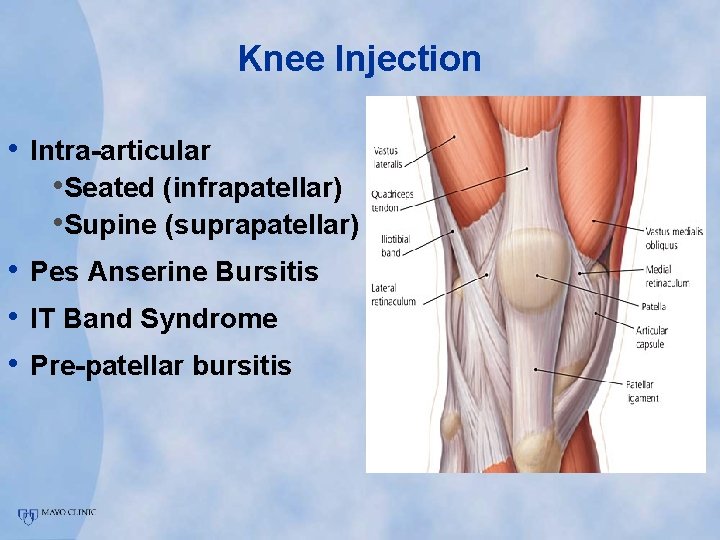
Knee Injection • Intra-articular • Seated (infrapatellar) • Supine (suprapatellar) • Pes Anserine Bursitis • IT Band Syndrome • Pre-patellar bursitis
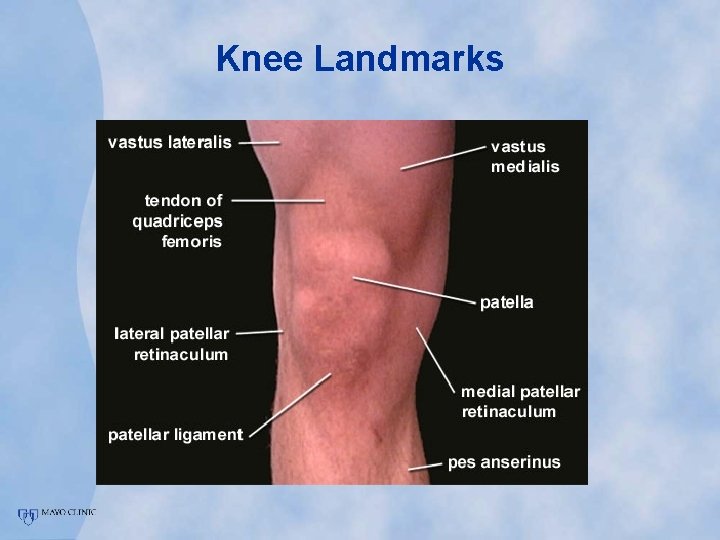
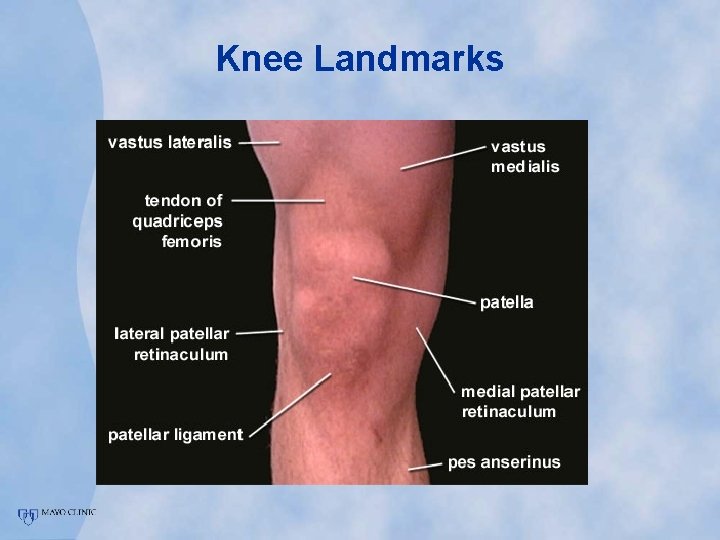
Knee Landmarks
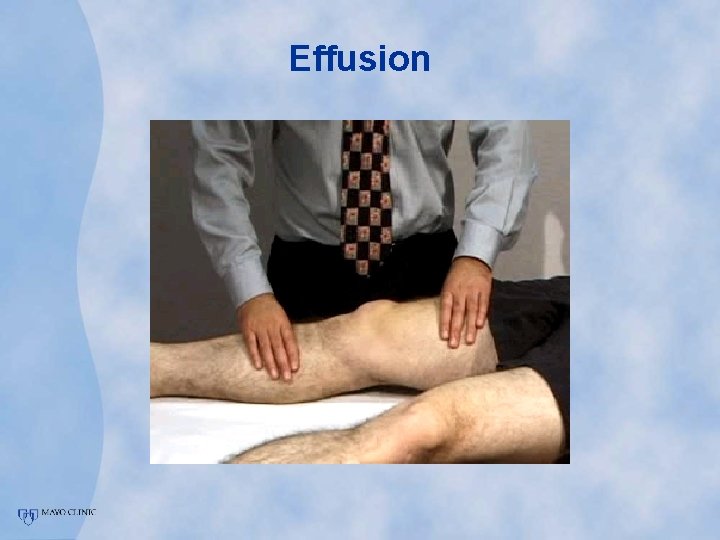
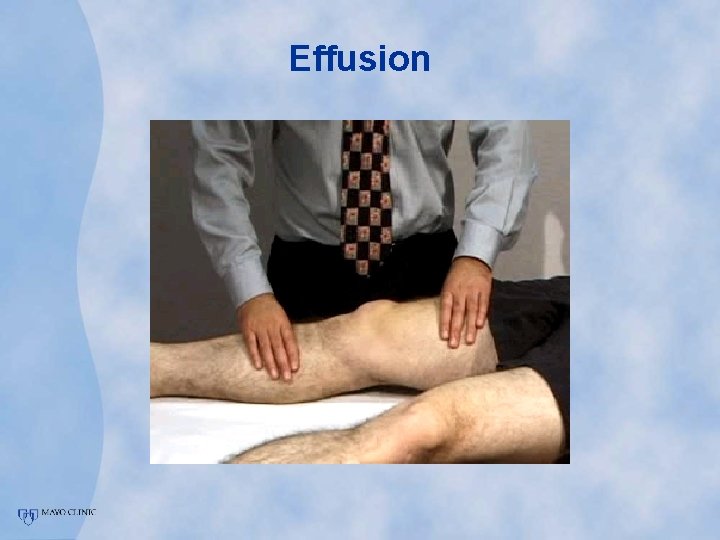
Effusion
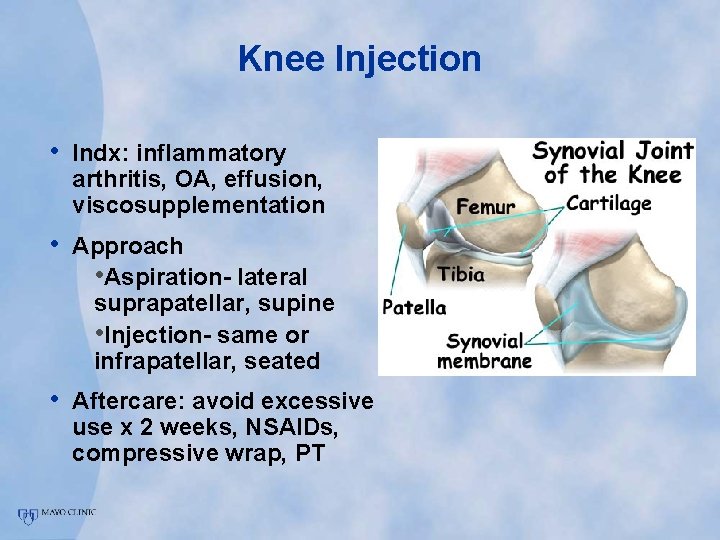
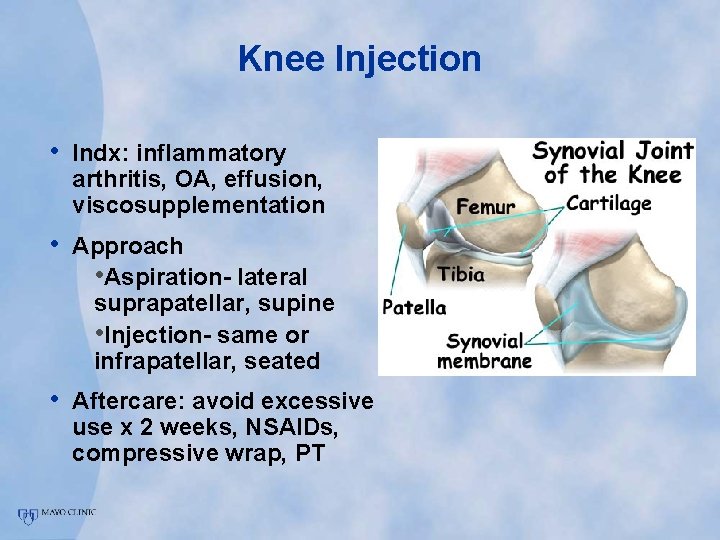
Knee Injection • Indx: inflammatory arthritis, OA, effusion, viscosupplementation • Approach • Aspiration- lateral suprapatellar, supine • Injection- same or infrapatellar, seated • Aftercare: avoid excessive use x 2 weeks, NSAIDs, compressive wrap, PT
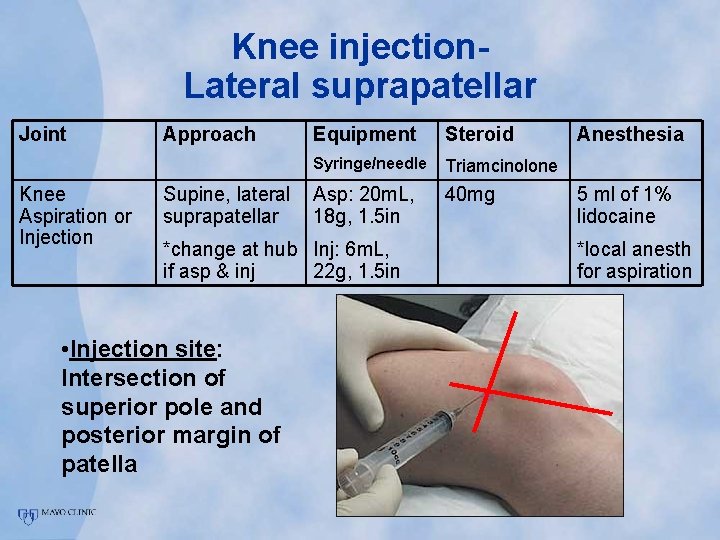
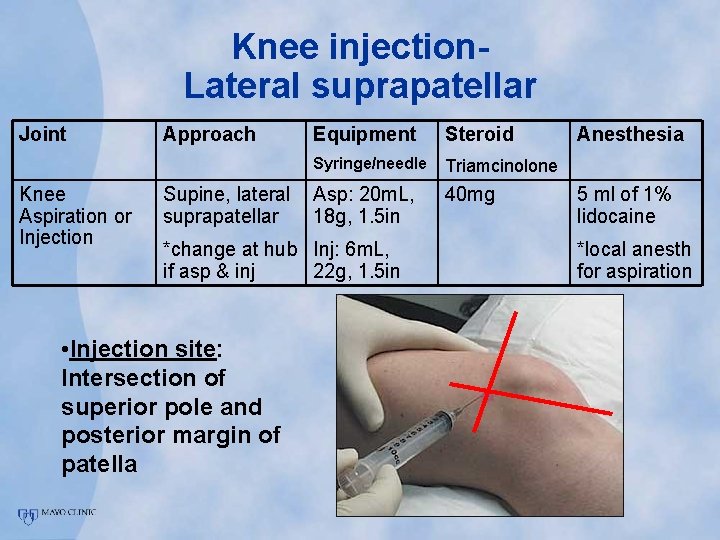
Knee injection. Lateral suprapatellar Joint Knee Aspiration or Injection Approach Supine, lateral suprapatellar Equipment Steroid Syringe/needle Triamcinolone Asp: 20 m. L, 18 g, 1. 5 in 40 mg *change at hub Inj: 6 m. L, if asp & inj 22 g, 1. 5 in • Injection site: Intersection of superior pole and posterior margin of patella Anesthesia 5 ml of 1% lidocaine *local anesth for aspiration
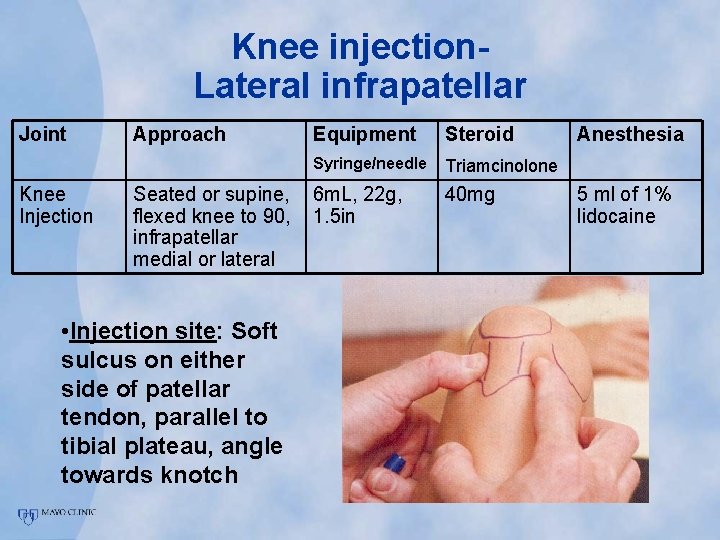
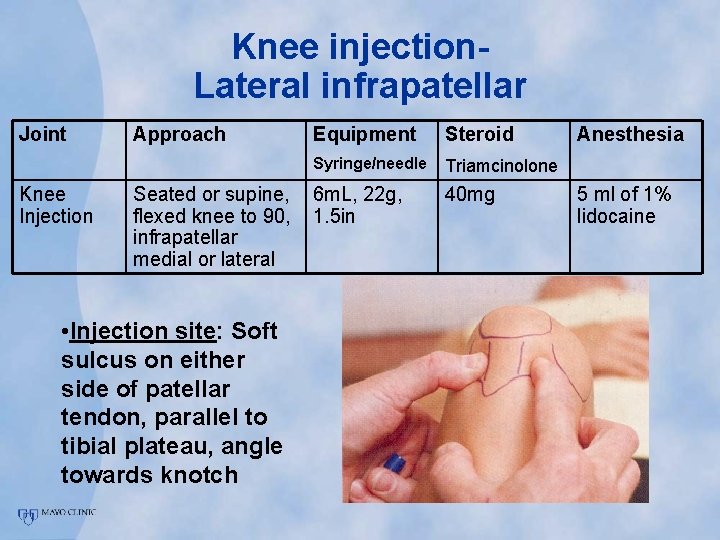
Knee injection. Lateral infrapatellar Joint Knee Injection Approach Seated or supine, flexed knee to 90, infrapatellar medial or lateral • Injection site: Soft sulcus on either side of patellar tendon, parallel to tibial plateau, angle towards knotch Equipment Steroid Syringe/needle Triamcinolone 6 m. L, 22 g, 1. 5 in 40 mg Anesthesia 5 ml of 1% lidocaine

Knee Injection Video
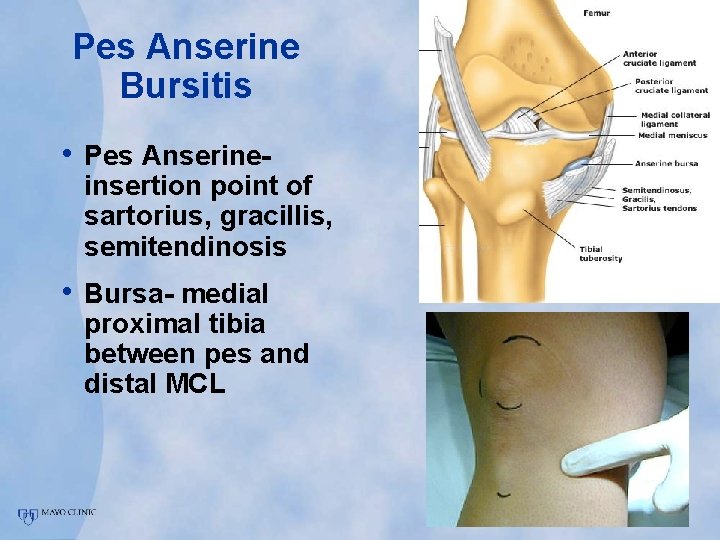
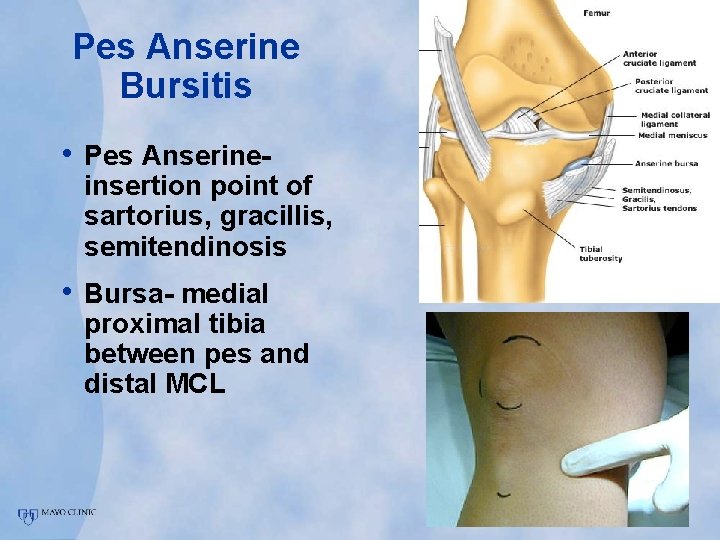
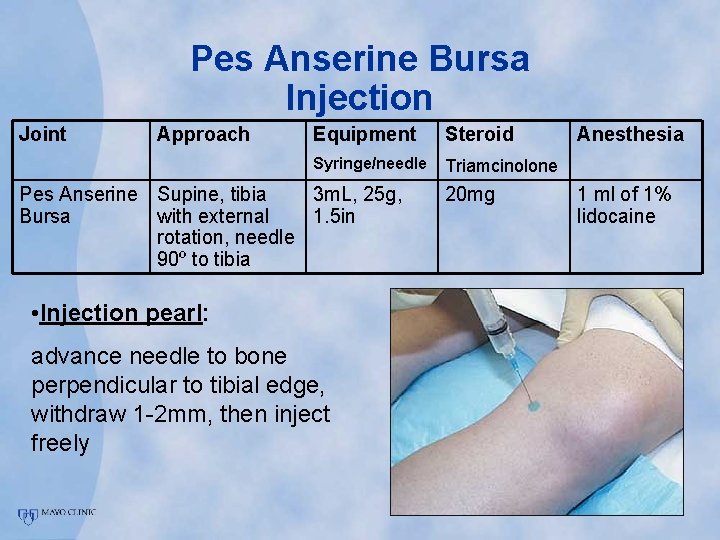
Pes Anserine Bursitis • Pes Anserine- insertion point of sartorius, gracillis, semitendinosis • Bursa- medial proximal tibia between pes and distal MCL
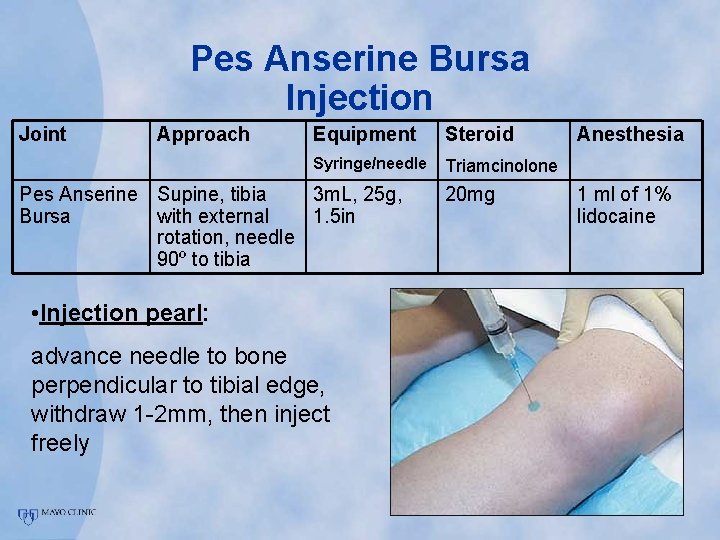
Pes Anserine Bursa Injection Joint Approach Equipment Steroid Syringe/needle Triamcinolone Pes Anserine Supine, tibia 3 m. L, 25 g, Bursa with external 1. 5 in rotation, needle 90º to tibia • Injection pearl: advance needle to bone perpendicular to tibial edge, withdraw 1 -2 mm, then inject freely 20 mg Anesthesia 1 ml of 1% lidocaine
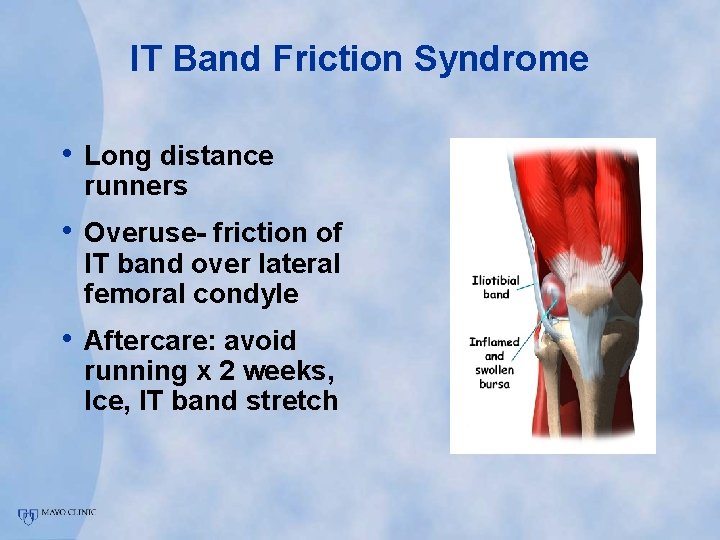
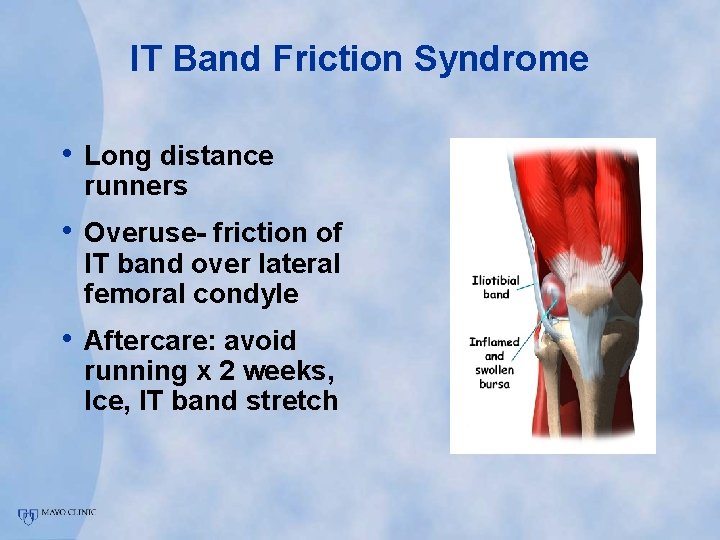
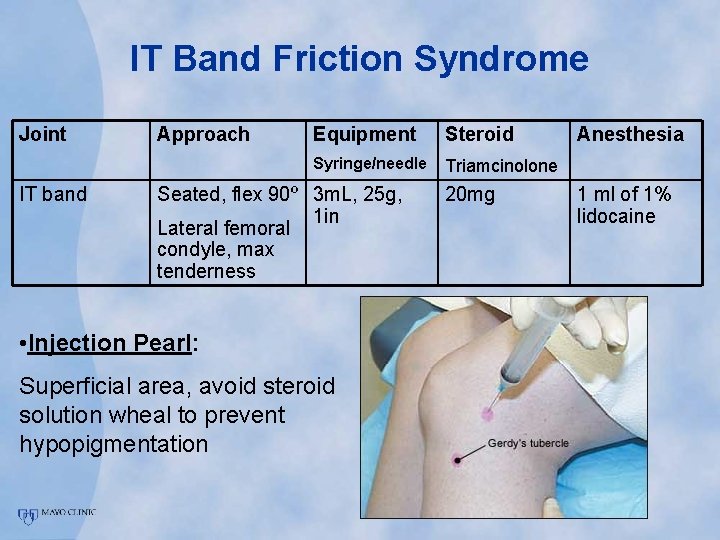
IT Band Friction Syndrome • Long distance runners • Overuse- friction of IT band over lateral femoral condyle • Aftercare: avoid running x 2 weeks, Ice, IT band stretch
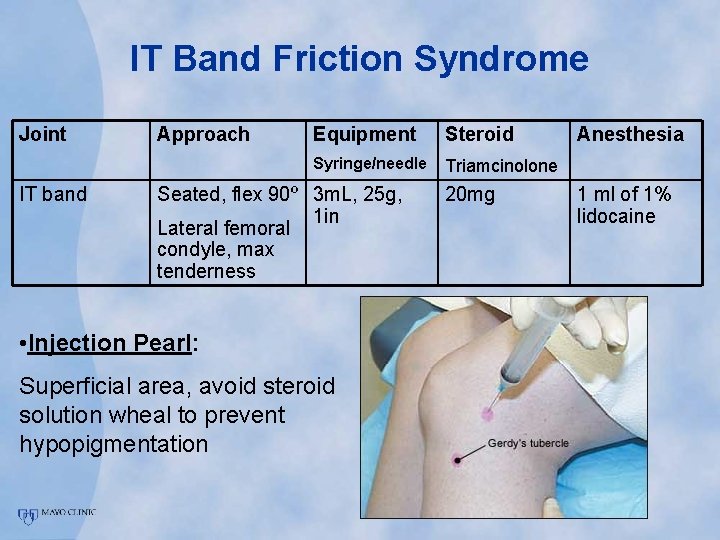
IT Band Friction Syndrome Joint IT band Approach Equipment Steroid Syringe/needle Triamcinolone Seated, flex 90º 3 m. L, 25 g, 1 in Lateral femoral condyle, max tenderness • Injection Pearl: Superficial area, avoid steroid solution wheal to prevent hypopigmentation 20 mg Anesthesia 1 ml of 1% lidocaine
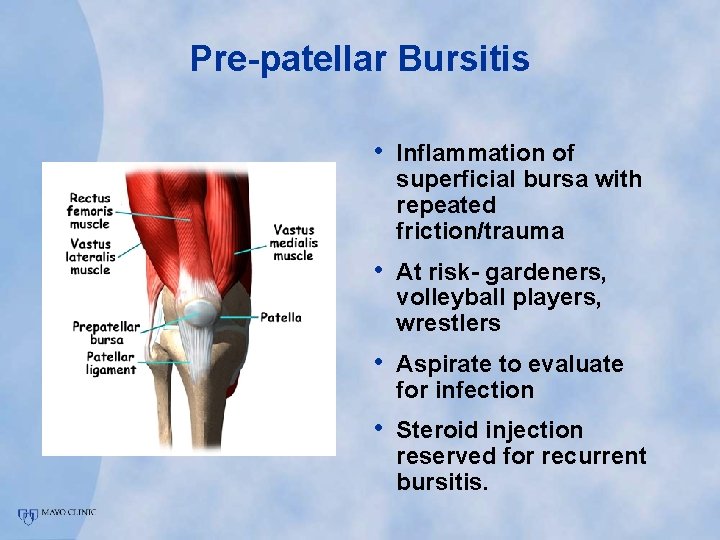
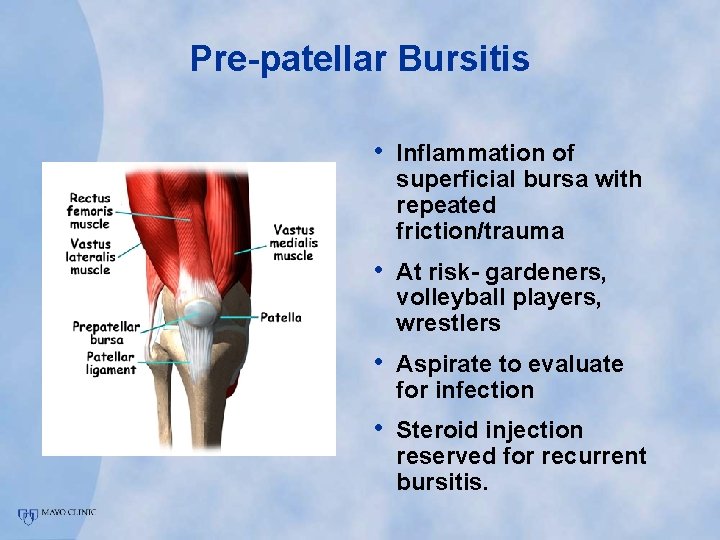
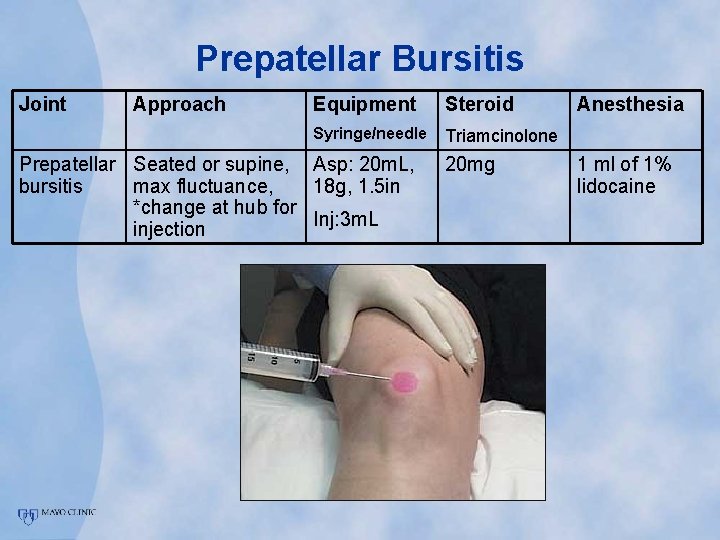
Pre-patellar Bursitis • Inflammation of superficial bursa with repeated friction/trauma • At risk- gardeners, volleyball players, wrestlers • Aspirate to evaluate for infection • Steroid injection reserved for recurrent bursitis.
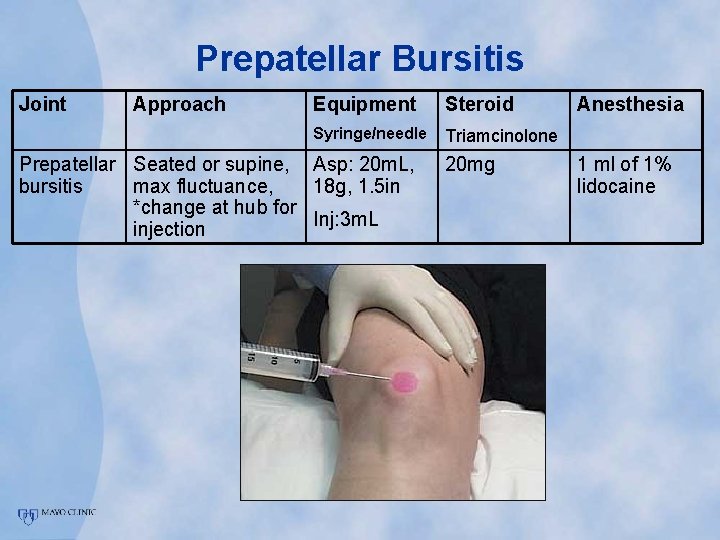
Prepatellar Bursitis Joint Approach Equipment Steroid Syringe/needle Triamcinolone Prepatellar Seated or supine, Asp: 20 m. L, bursitis max fluctuance, 18 g, 1. 5 in *change at hub for Inj: 3 m. L injection 20 mg Anesthesia 1 ml of 1% lidocaine
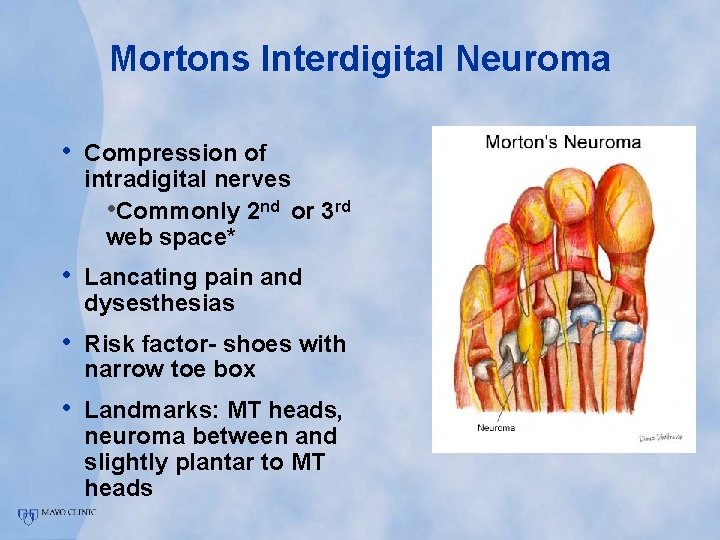
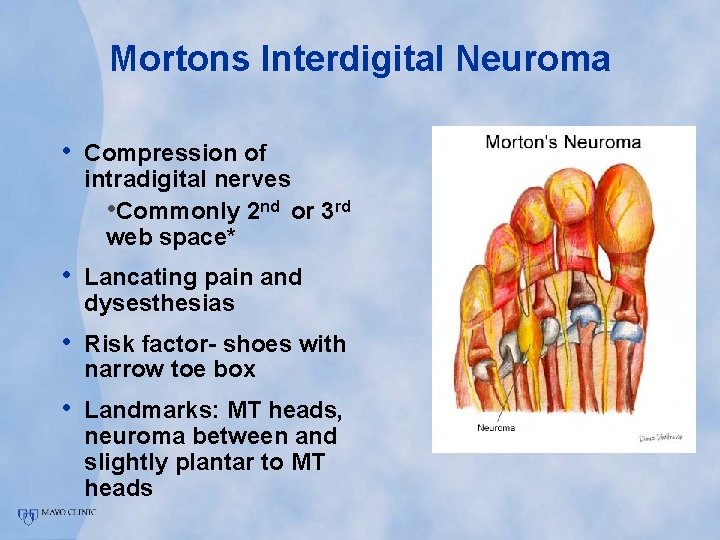
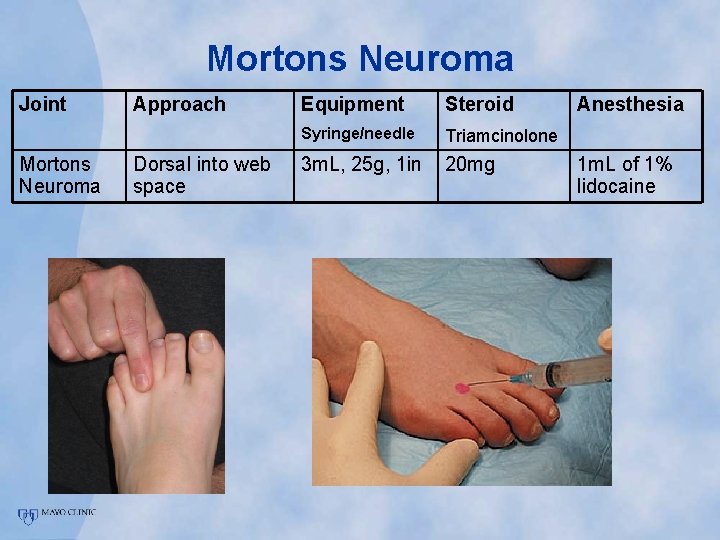
Mortons Interdigital Neuroma • Compression of intradigital nerves • Commonly 2 nd or 3 rd web space* • Lancating pain and dysesthesias • Risk factor- shoes with narrow toe box • Landmarks: MT heads, neuroma between and slightly plantar to MT heads
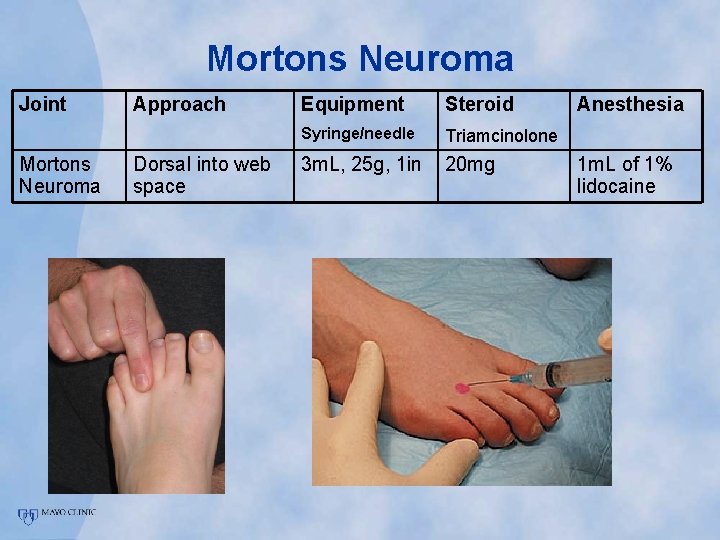
Mortons Neuroma Joint Mortons Neuroma Approach Dorsal into web space Equipment Steroid Syringe/needle Triamcinolone 3 m. L, 25 g, 1 in 20 mg Anesthesia 1 m. L of 1% lidocaine
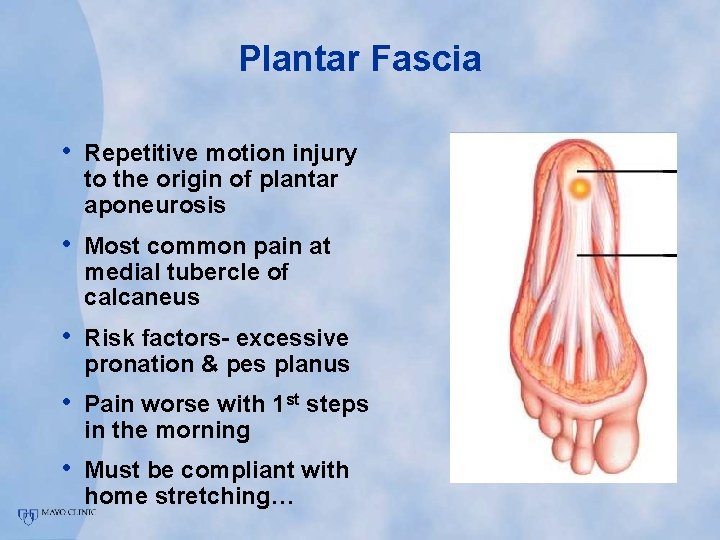
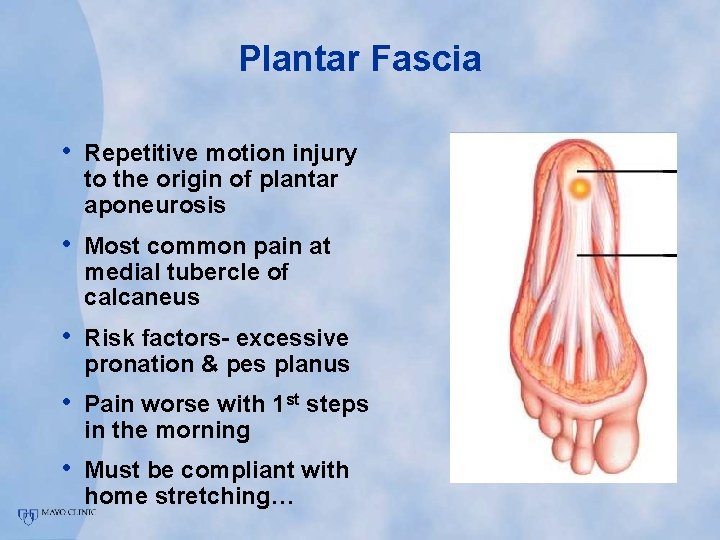
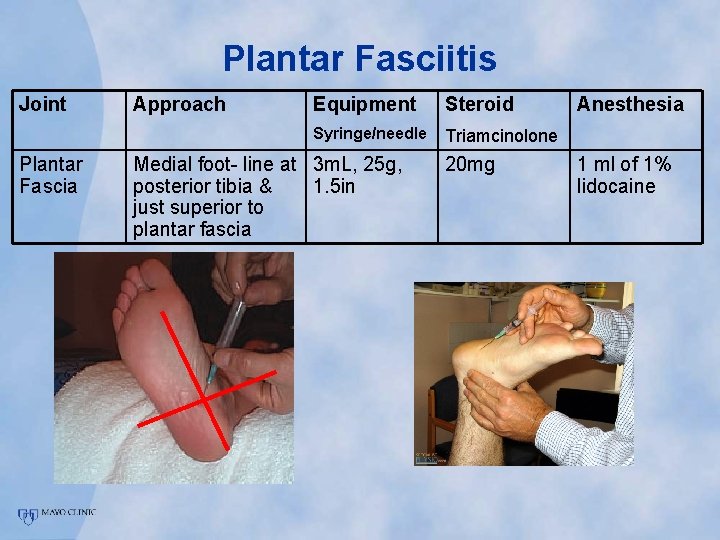
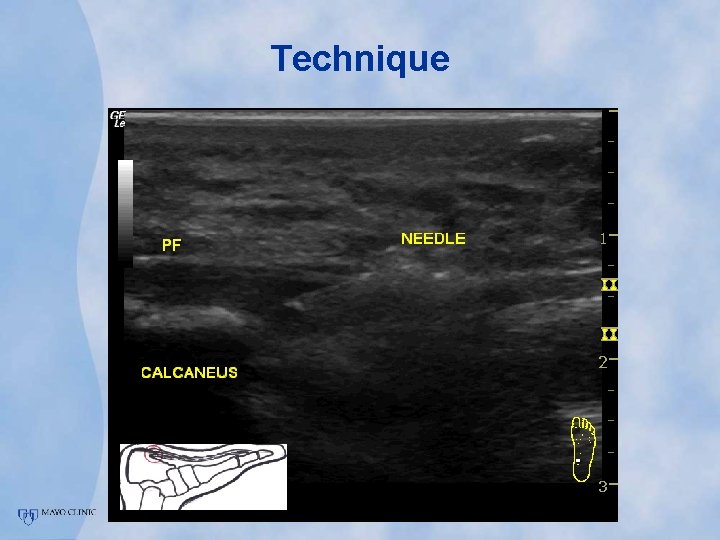
Plantar Fascia • Repetitive motion injury to the origin of plantar aponeurosis • Most common pain at medial tubercle of calcaneus • Risk factors- excessive pronation & pes planus • Pain worse with 1 st steps in the morning • Must be compliant with home stretching…
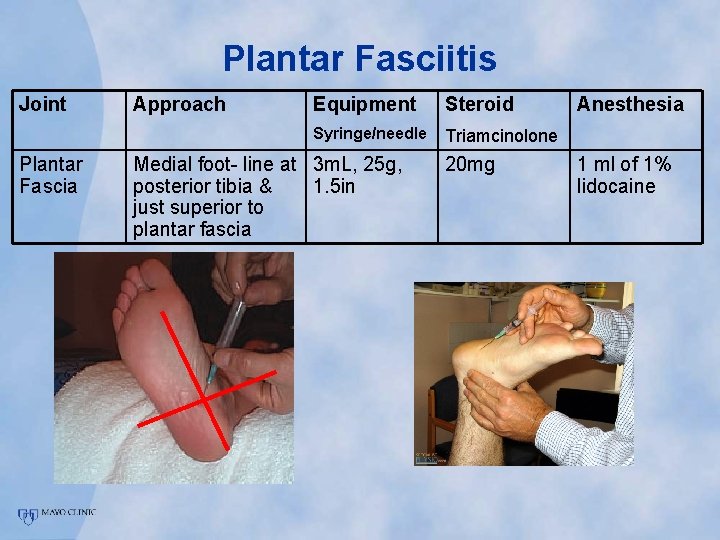
Plantar Fasciitis Joint Plantar Fascia Approach Equipment Steroid Syringe/needle Triamcinolone Medial foot- line at 3 m. L, 25 g, posterior tibia & 1. 5 in just superior to plantar fascia 20 mg Anesthesia 1 ml of 1% lidocaine

Update • Regenerative Injection Therapies • Treatment for chronic tendonopathies • Ligamentous laxity • Fasciopathy
Theory • Symptoms of chronic musculoskeletal pain are rarely due to inflammation. • Inadequate Healing • Anti-inflammatory Rx?
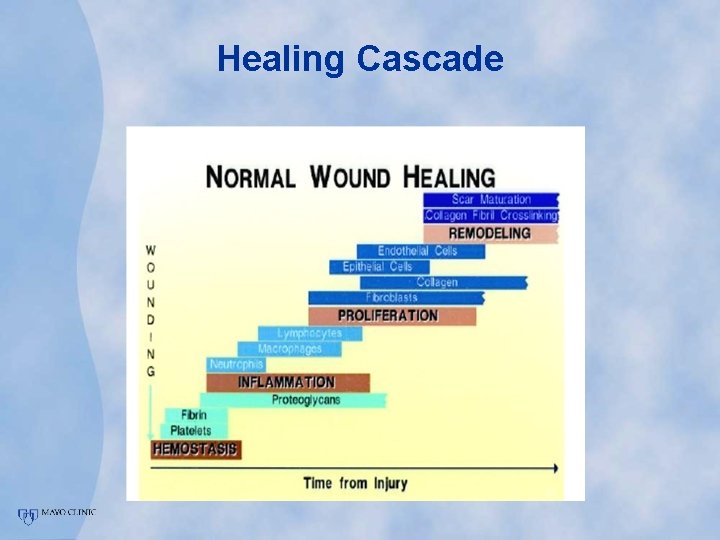
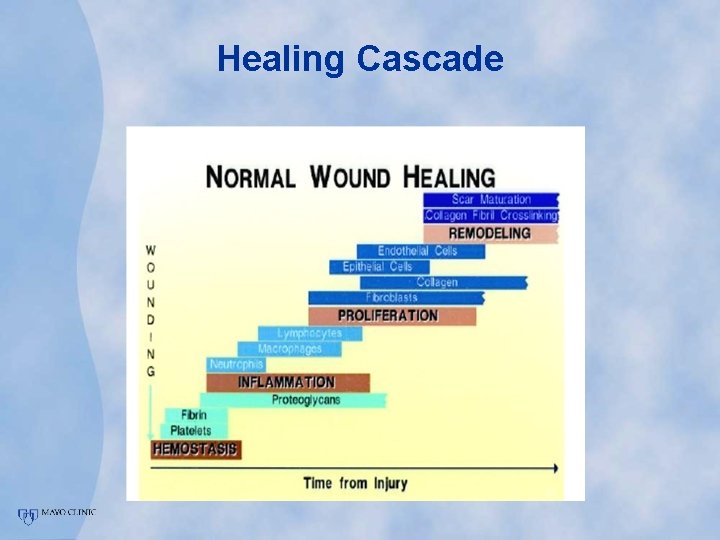
Healing Cascade
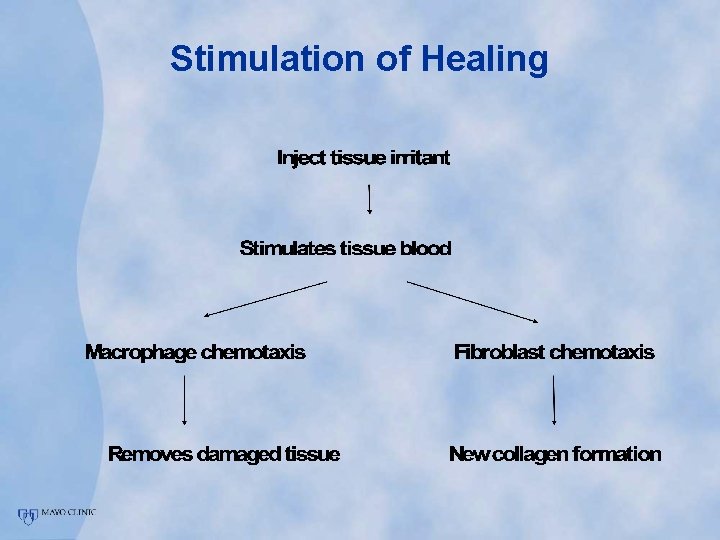
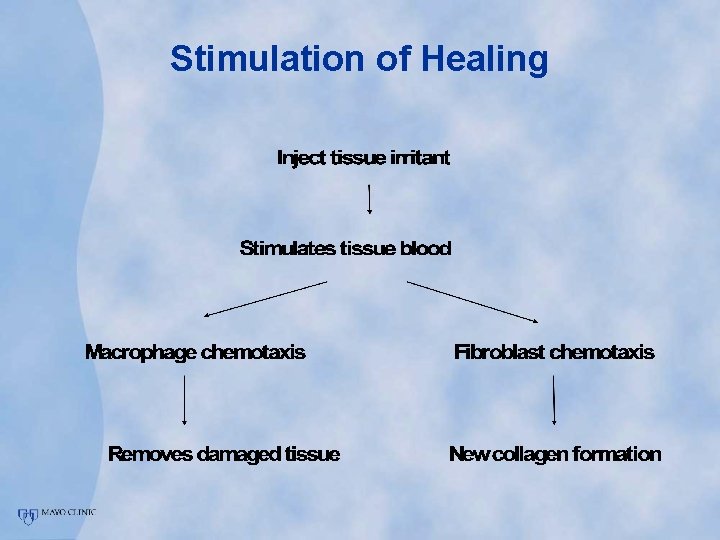
Stimulation of Healing

Regenerative Injection Therapy • Prolotherapy • Autologous Blood • Platelet Rich Plasma Injections • Sclerosing Injections
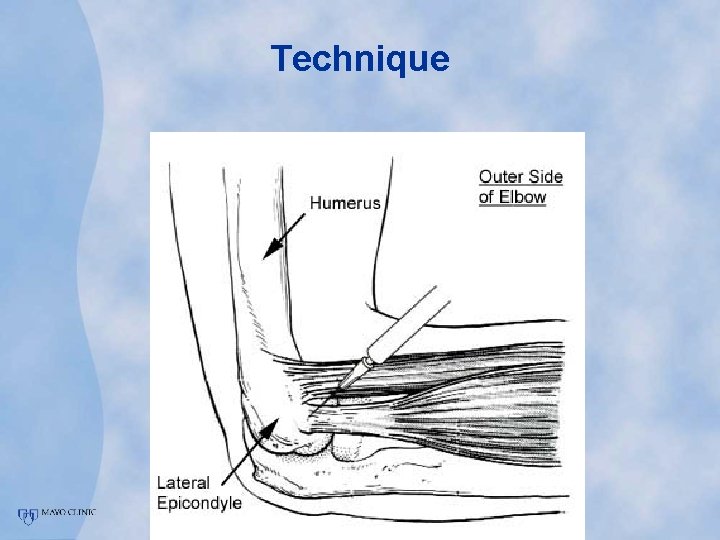
Technique

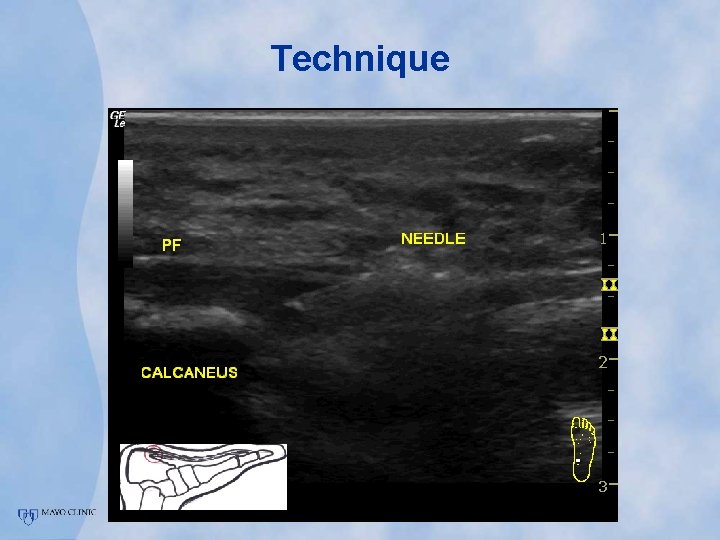
Technique
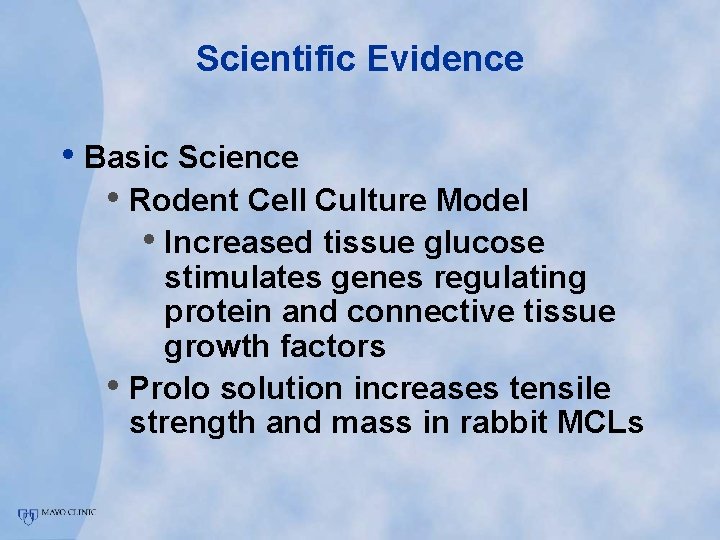
Scientific Evidence • Basic Science • Rodent Cell Culture Model • Increased tissue glucose stimulates genes regulating protein and connective tissue growth factors • Prolo solution increases tensile strength and mass in rabbit MCLs
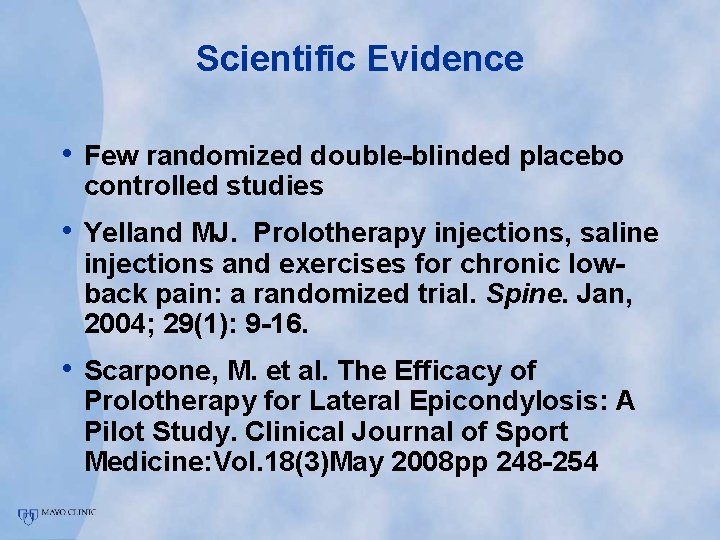
Scientific Evidence • Few randomized double-blinded placebo controlled studies • Yelland MJ. Prolotherapy injections, saline injections and exercises for chronic lowback pain: a randomized trial. Spine. Jan, 2004; 29(1): 9 -16. • Scarpone, M. et al. The Efficacy of Prolotherapy for Lateral Epicondylosis: A Pilot Study. Clinical Journal of Sport Medicine: Vol. 18(3)May 2008 pp 248 -254
Injection Key Concepts • • Know the anatomy in 3 -D Identify landmarks Indications Contraindications Safety- of provider AND patient Injectables Technique Aftercare instructions
References • Mc. Nabb J. A Practical Guide to Joint & Soft Tissue Injection & • • Aspiration. Lippincott Willimas & Wilkins. Philadelphia, © 2005. Saunders S, Longworth S. Injection Techniques in Orthopaedics and Sports Medicine. Elsevier, 2006. Waldman SD. Atlas of Pain Management Techniques. Elsevier, 2007. Cardone DA, Tallia AF. Joint and soft tissue injection. Am Fam Physician 2002; 66: 283 -288. Tallia AF, Cardone DA. Diagnostic and Therapeutic Injection of the Shoulder Region. Am Fam Physician 2003; 67: 1271 -1278. Tallia AF, Cardone DA. Diagnostic and therapeutic injection of the wrist and hand region. Am Fam Physician 2003; 67: 745 -50. Cardone DA, Tallia AF. Diagnostic and Therapeutic Injection of the Hip and Knee Am Fam Physician 2003; 67: 2147 -2152. Cardone DA, Tallia AF. Diagnostic and Therapeutic Injection of the Elbow Region. Am Fam Physician 2002; 66: 2097 -2100. Tallia AF, Cardone DA. Diagnostic and Therapeutic Injection of the Ankle and Foot. Am Fam Physician 2003; 68: 1356 -1362.
References • Thumboo J, O’Duffy JD. A prospective study of the safety of joint and soft tissue aspirations and injections in patients taking warfarin sodium. Arthritis Rheum. 1998 Apr; 41(4): 736 -9. • Bellamy N, Campbell J. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cocharane Systems Review 2006 Apr 19; (2): CD 005328 • Bellamy N, Campbell J. Viscosupplementation for the treatment of osteoarthritis of the knee. 2006 Apr 19; (2): CD 005321 • Stephens M, Beutler A, O’Connor F. Musculoskeletal Injections: A review of the Evidence. American Family Physcian. 2008 October 15.