John Wei PGY 2 Rash Decisions 65 year


![Presentation • Systemic symptoms include fever (38 to 40°C [100. 4 to 104°F]), malaise, Presentation • Systemic symptoms include fever (38 to 40°C [100. 4 to 104°F]), malaise,](https://slidetodoc.com/presentation_image_h/dc3df3349911d9ecb8dde9f799428f9f/image-12.jpg)



- Slides: 40
John Wei PGY‐ 2 Rash Decisions
65 year old man • With PMHx otherwise unremarkable apart from recent hospitalization for left 2 nd digit MRSA infection, decision made to attempt salvage with antibiotics as opposed to amputation. • He was started on Vancomycin immediately prior to discharge and following roughly 10 days of outpatient therapy was noted to have developed suspected “red man” syndrome; infusion rate was slowed the subsequent day without significant effect and he was subsequently changed to Daptomycin by ID.
Presentation • He now presents for a worsening rash over his entire body also associated with fevers up to 102 F at home (also documented in emergency room).
• CBC and CMP initially ordered and normal except as noted below: Initial Labs • • Na 129 AST 95 Albumin 3. 0 WBC 11. 4 • What other labs would you want to order?


• SJS/TEN • Vasculitis • Viral exanthem Differential? • Angio‐immunoblastic lymphadenopathy • Psoriasis • Erythema Nodosum • Acute febrile neutrophilic dermatosis
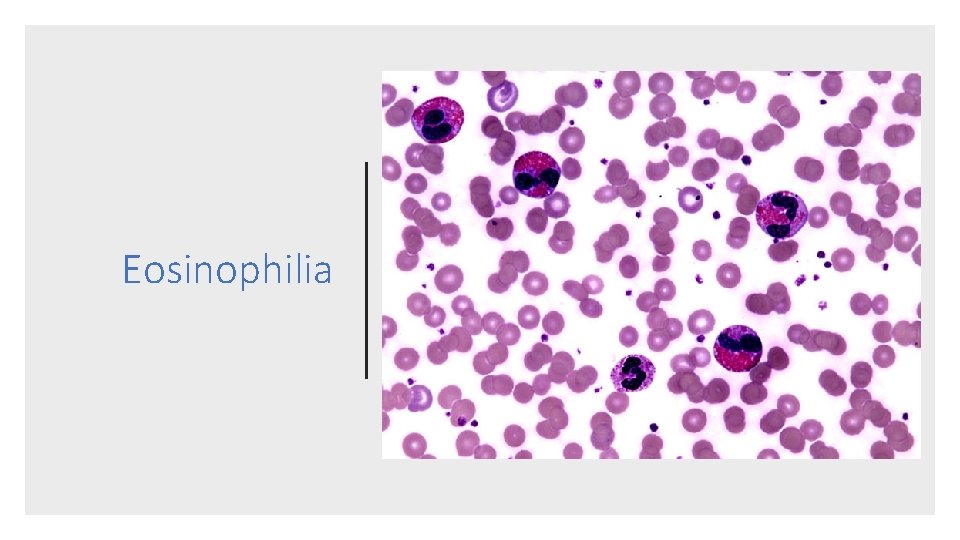
• Developed kidney injury (Cr up to 1. 88) • Developed Liver injury (AST up to 125) • Worsening hypoalbuminemia to 1. 6 Further Work Up • Persistent leukocytosis (WBC to 26. 5) • Noted eosinophilia up to 1. 4 (WBC 23. 6) • Autoimmune Labs • C 3 > 350 • C 4, ANCA, ANA, Hepatitis A, B, C, HHV 6, CMV, EBV, all negative • Mild eosinophilia noted on peripheral smear
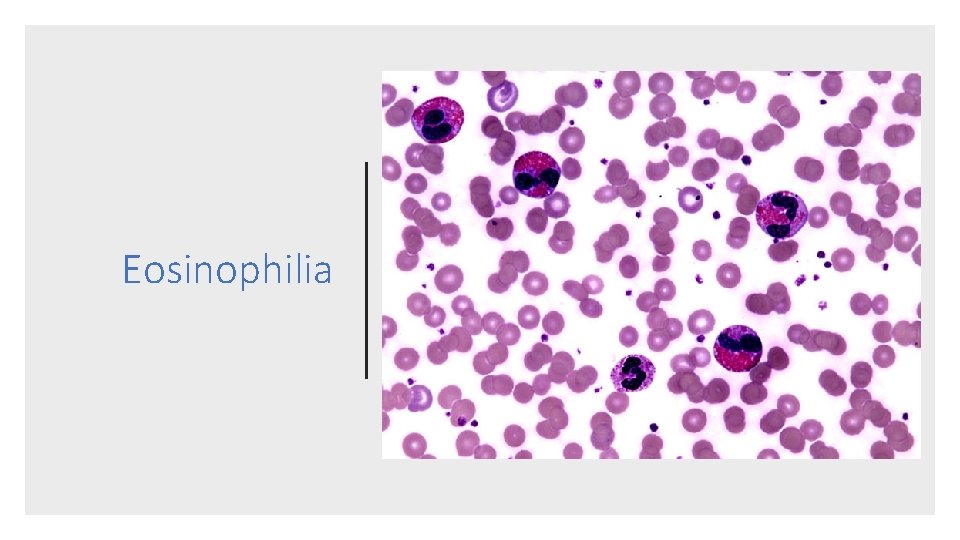
Eosinophilia
Dress Syndrome
Definition • The eruption is usually an exuberant morbilliform eruption with prominent facial edema, lymphadenopathy, fever, and, in severe cases, hypotension
![Presentation Systemic symptoms include fever 38 to 40C 100 4 to 104F malaise Presentation • Systemic symptoms include fever (38 to 40°C [100. 4 to 104°F]), malaise,](https://slidetodoc.com/presentation_image_h/dc3df3349911d9ecb8dde9f799428f9f/image-12.jpg)
Presentation • Systemic symptoms include fever (38 to 40°C [100. 4 to 104°F]), malaise, lymphadenopathy, and symptoms related to visceral involvement • Delayed onset following exposure to a triggering agent.
Skin eruption (morbilliform or diffuse, confluent, and infiltrated) Fever (38 to 40°C [100. 4 to 104°F]) Physical Exam Facial edema Enlarged lymph nodes

DRESS Rash
Pathogenesis Drug‐specific Immune Response‐ A strong, drug‐specific immune response is a key factor in the pathogenesis of drug reaction with eosinophilia and systemic symptoms (DRESS) T cell expansion and activation of CD 8, CD 4, and T Regulatory cells.
Pathogenesis Continued Viral Reactivation ‐ Reactivation of several viruses of the herpes group (human herpesvirus HHV‐ 6, HHV‐ 7, EBV, and CMV) is frequent in DRESS is primarily a strong, drug ‐specific immune reaction that acts as a trigger of viral reactivation.
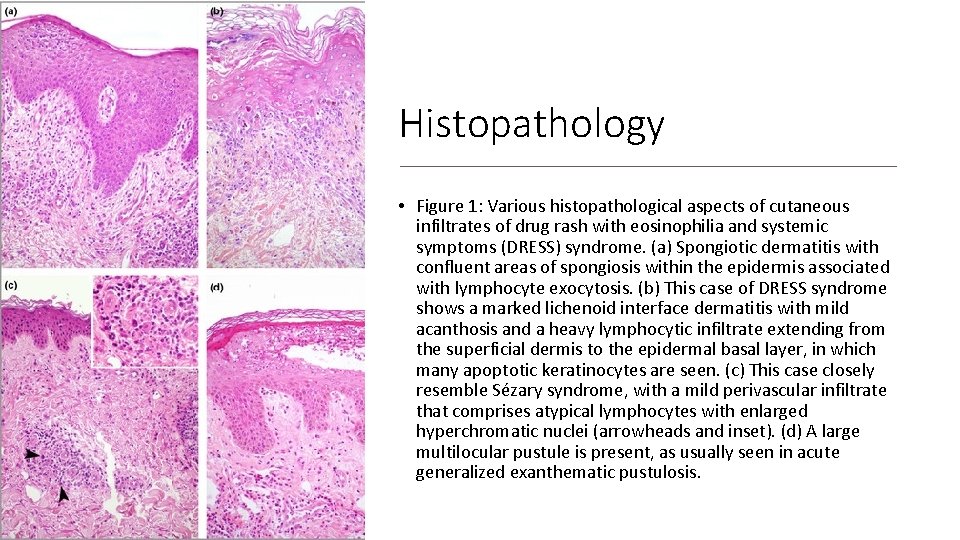
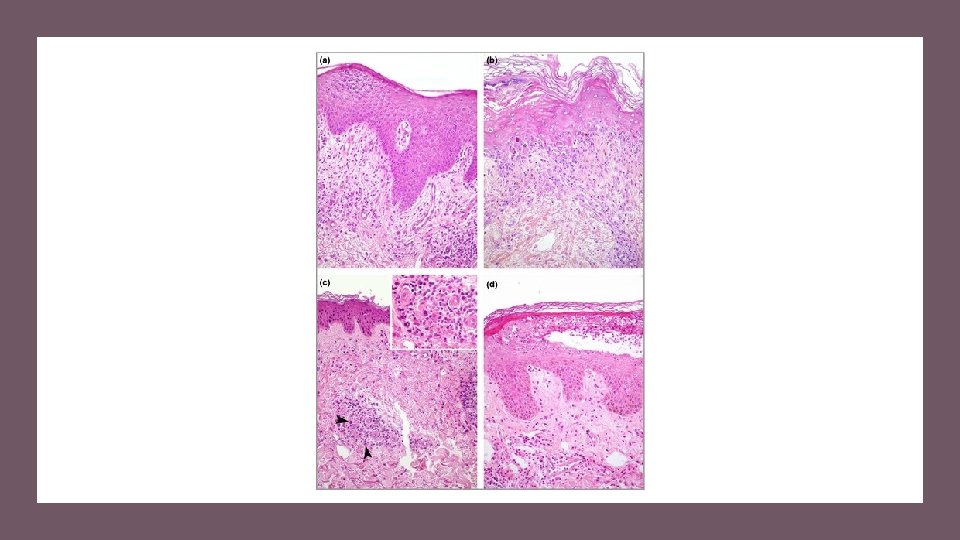
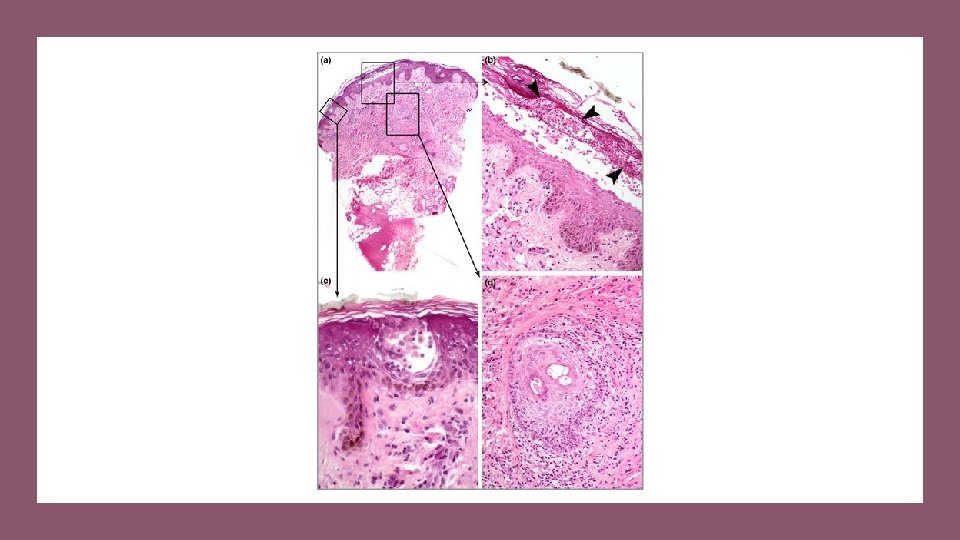
Pathologic Features • Histopathologic examination of a skin biopsy reveals a variable combination of spongiosis, acanthosis, interface vacuolization, a lymphocytic infiltrate in the superficial dermis, predominantly perivascular, variable presence of eosinophils, and dermal edema.
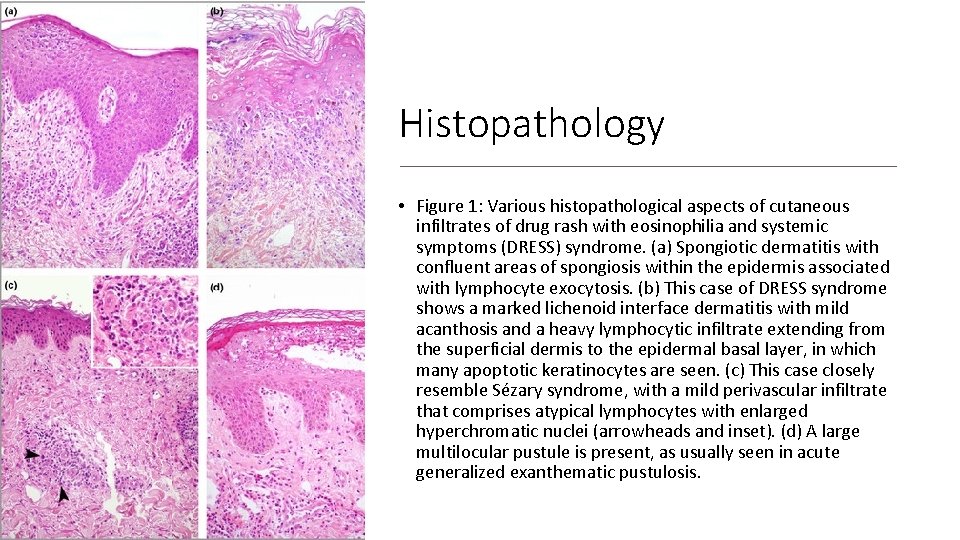
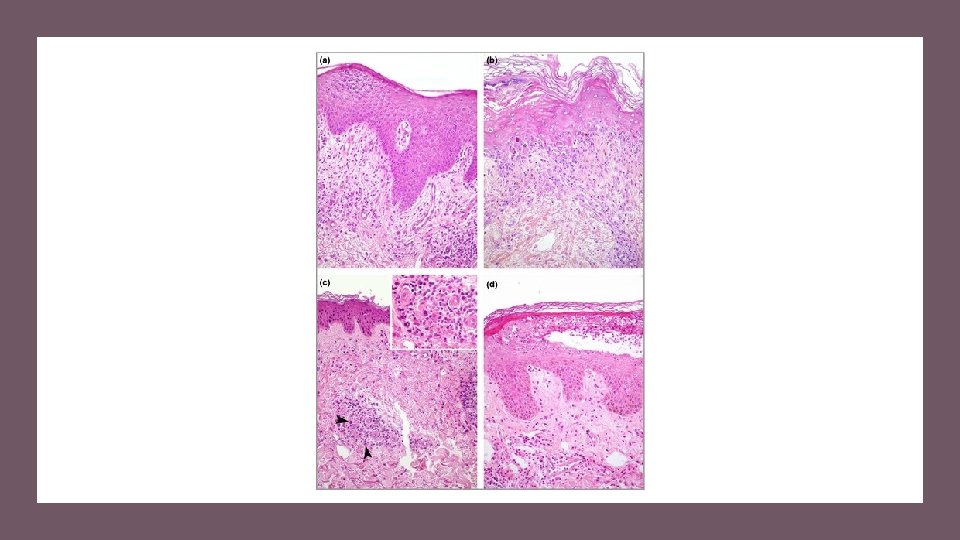
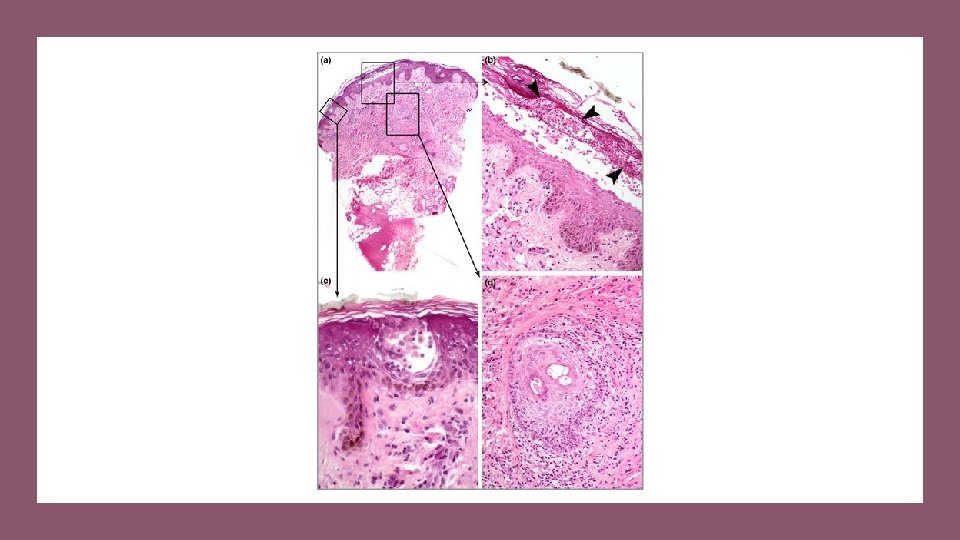
Histopathology • Figure 1: Various histopathological aspects of cutaneous infiltrates of drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. (a) Spongiotic dermatitis with confluent areas of spongiosis within the epidermis associated with lymphocyte exocytosis. (b) This case of DRESS syndrome shows a marked lichenoid interface dermatitis with mild acanthosis and a heavy lymphocytic infiltrate extending from the superficial dermis to the epidermal basal layer, in which many apoptotic keratinocytes are seen. (c) This case closely resemble Sézary syndrome, with a mild perivascular infiltrate that comprises atypical lymphocytes with enlarged hyperchromatic nuclei (arrowheads and inset). (d) A large multilocular pustule is present, as usually seen in acute generalized exanthematic pustulosis.
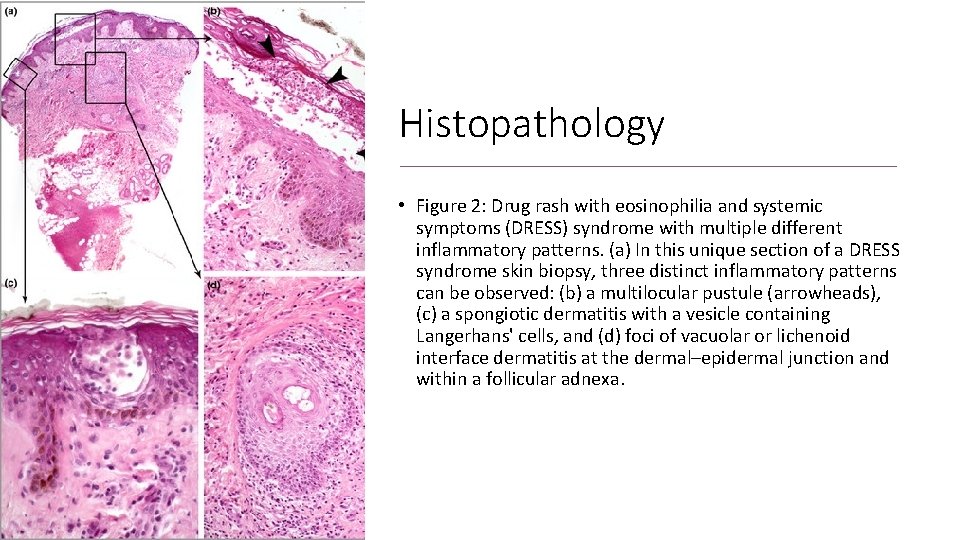
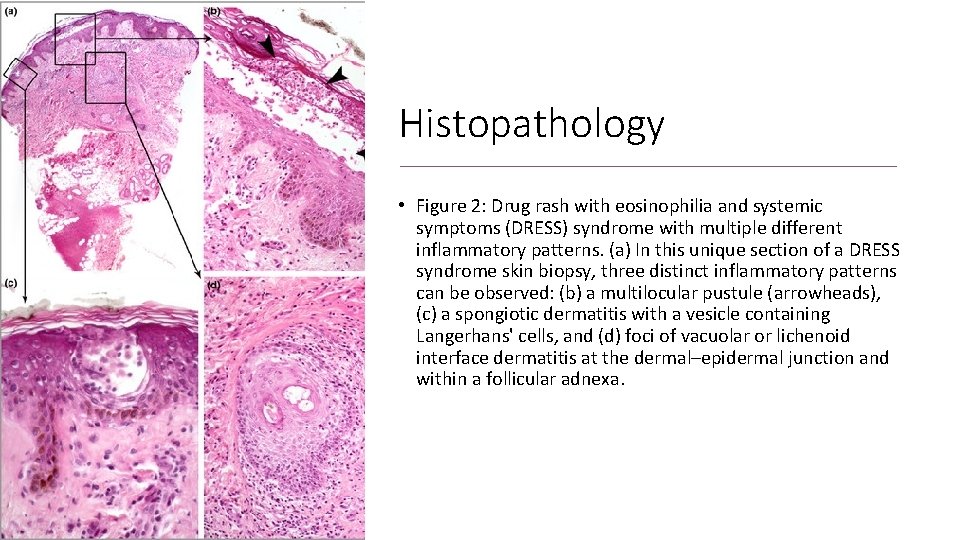
Histopathology • Figure 2: Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome with multiple different inflammatory patterns. (a) In this unique section of a DRESS syndrome skin biopsy, three distinct inflammatory patterns can be observed: (b) a multilocular pustule (arrowheads), (c) a spongiotic dermatitis with a vesicle containing Langerhans' cells, and (d) foci of vacuolar or lichenoid interface dermatitis at the dermal–epidermal junction and within a follicular adnexa.
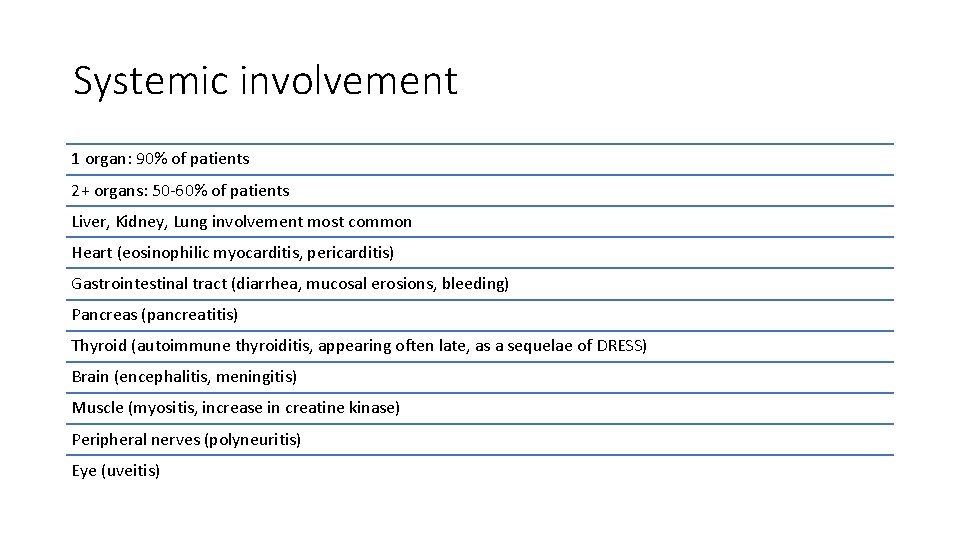
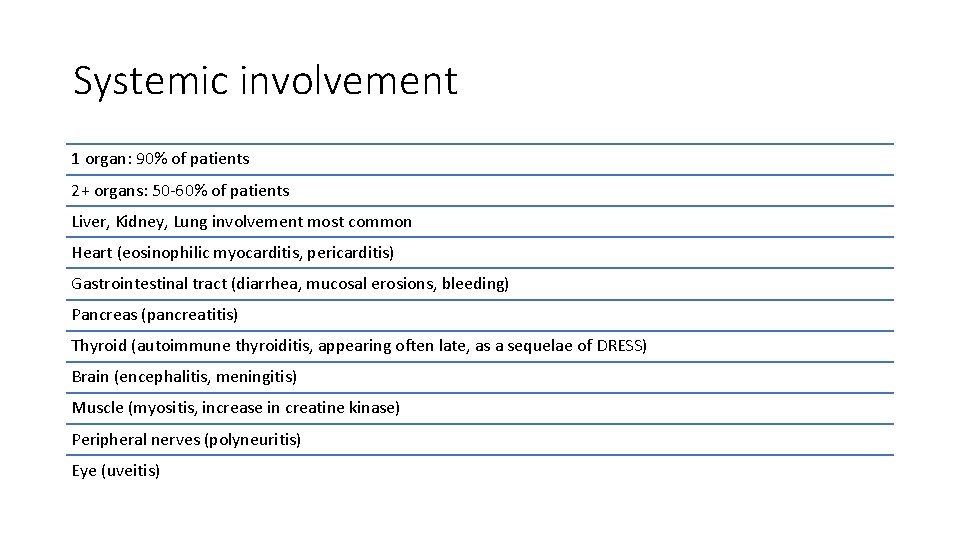
Systemic involvement 1 organ: 90% of patients 2+ organs: 50‐ 60% of patients Liver, Kidney, Lung involvement most common Heart (eosinophilic myocarditis, pericarditis) Gastrointestinal tract (diarrhea, mucosal erosions, bleeding) Pancreas (pancreatitis) Thyroid (autoimmune thyroiditis, appearing often late, as a sequelae of DRESS) Brain (encephalitis, meningitis) Muscle (myositis, increase in creatine kinase) Peripheral nerves (polyneuritis) Eye (uveitis)
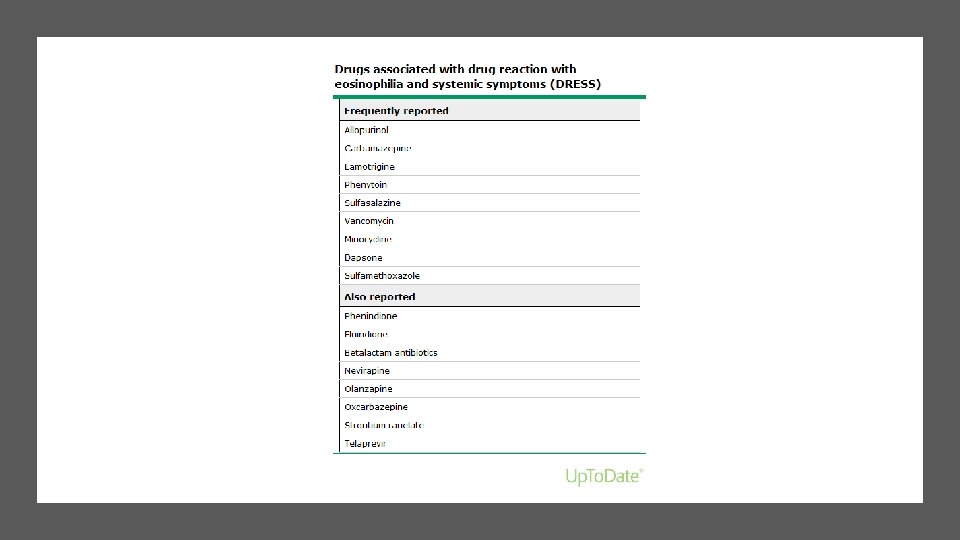
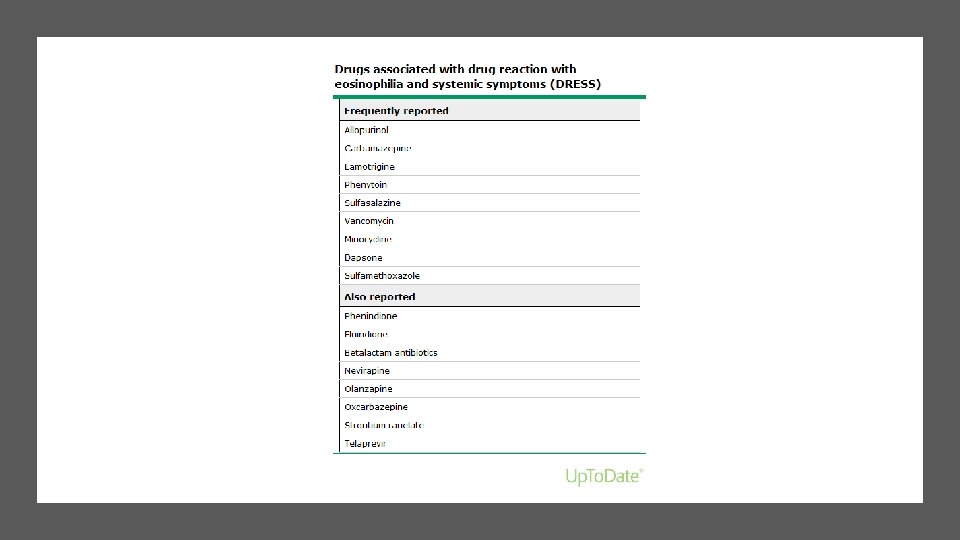
Etiologies?
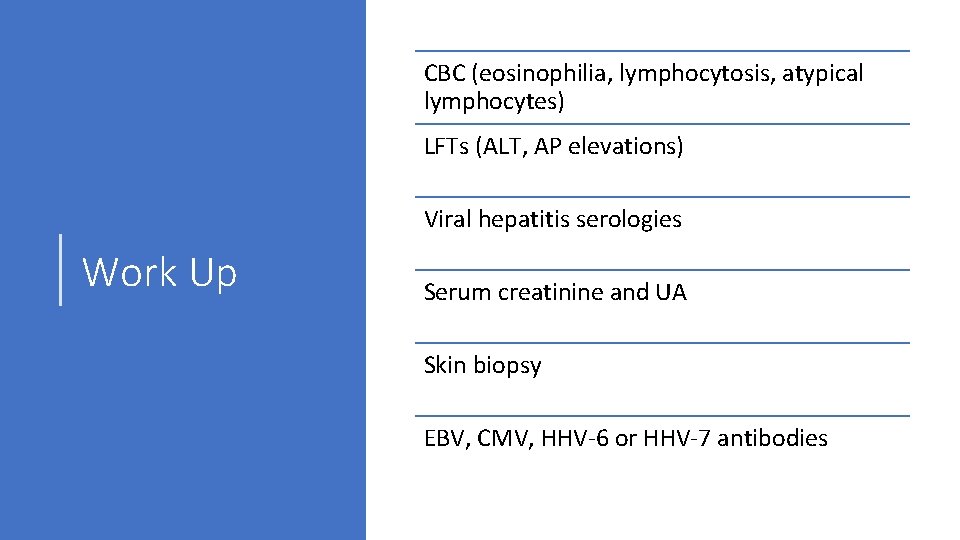
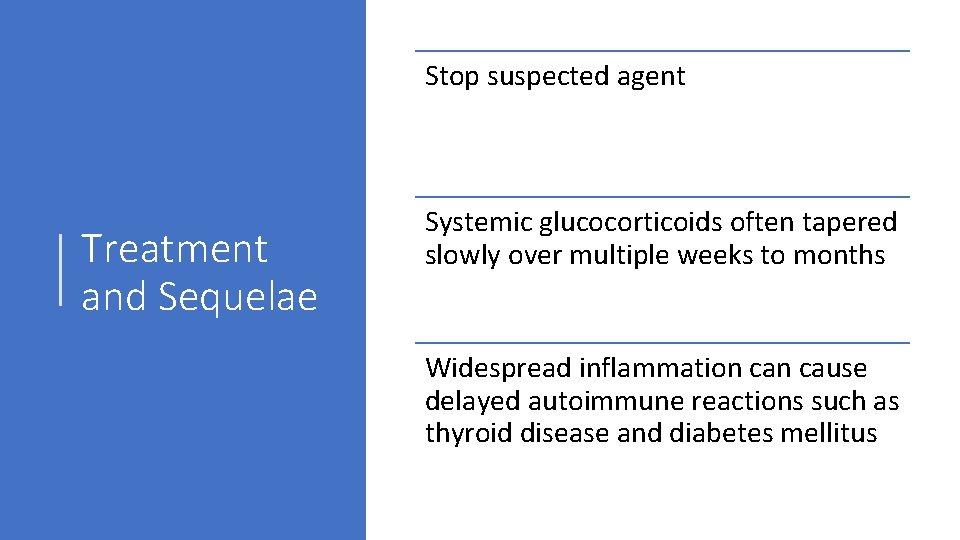
CBC (eosinophilia, lymphocytosis, atypical lymphocytes) LFTs (ALT, AP elevations) Viral hepatitis serologies Work Up Serum creatinine and UA Skin biopsy EBV, CMV, HHV‐ 6 or HHV‐ 7 antibodies
Stop suspected agent Treatment and Sequelae Systemic glucocorticoids often tapered slowly over multiple weeks to months Widespread inflammation cause delayed autoimmune reactions such as thyroid disease and diabetes mellitus
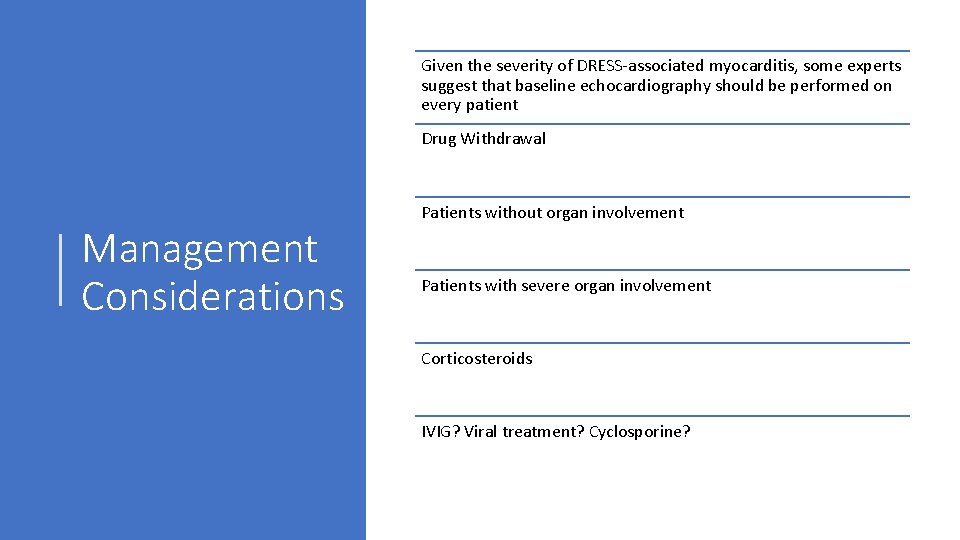
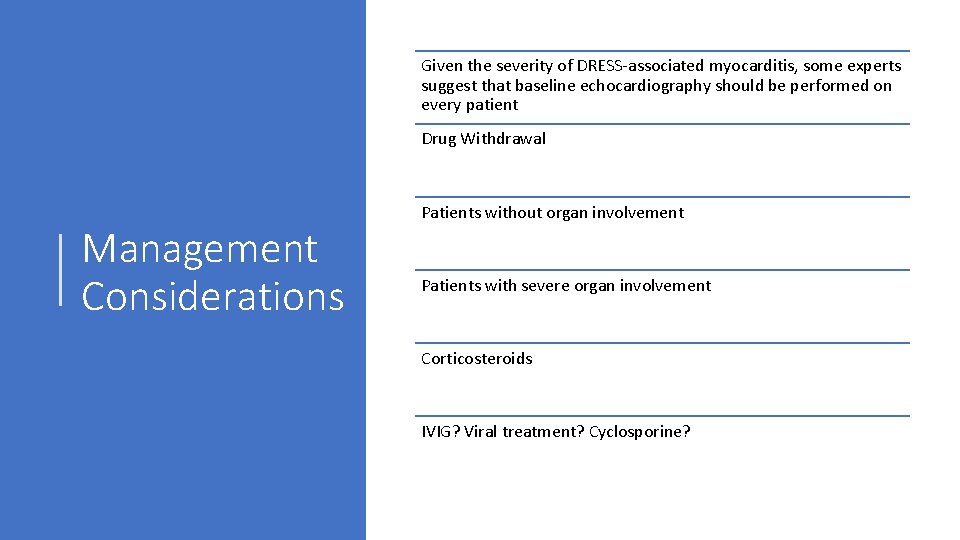
Given the severity of DRESS‐associated myocarditis, some experts suggest that baseline echocardiography should be performed on every patient Drug Withdrawal Management Considerations Patients without organ involvement Patients with severe organ involvement Corticosteroids IVIG? Viral treatment? Cyclosporine?
Gradual improvement following drug withdrawal over an average of 6‐ 9 weeks Course Overall, a more severe presentation and organ involvement suggests a possible prolonged course for at least 3 months and up to a year. Case reports exist for flares or relapses of DRESS with introduction of new medications, including beta‐lactam antibiotics
Prognosis and Recovery 1 Complete recovery in weeks to months after drug withdrawal. 2 Noted autoimmune diseases in some patients months or years after the resolution of the drug reaction. 3 Benefit from monitoring following acute phase of disease.
Hospital stay 9 days Outcome for our patient? Initially switched from Vancomycin to Daptomycin but due to some concern for continued allergy, this was held in favor of linezolid Dermatology also following who favored diagnosis of DRESS (saw inpatient) and patient will be following with academic dermatology clinic
Vancomycin Induced Skin Eruptions • • • Red Man Syndrome DRESS Vancomycin hypersensitivity Linear Ig. A‐mediated bullous dermatosis SJS/TEN Interstitial Nephritis

DRESS Rash
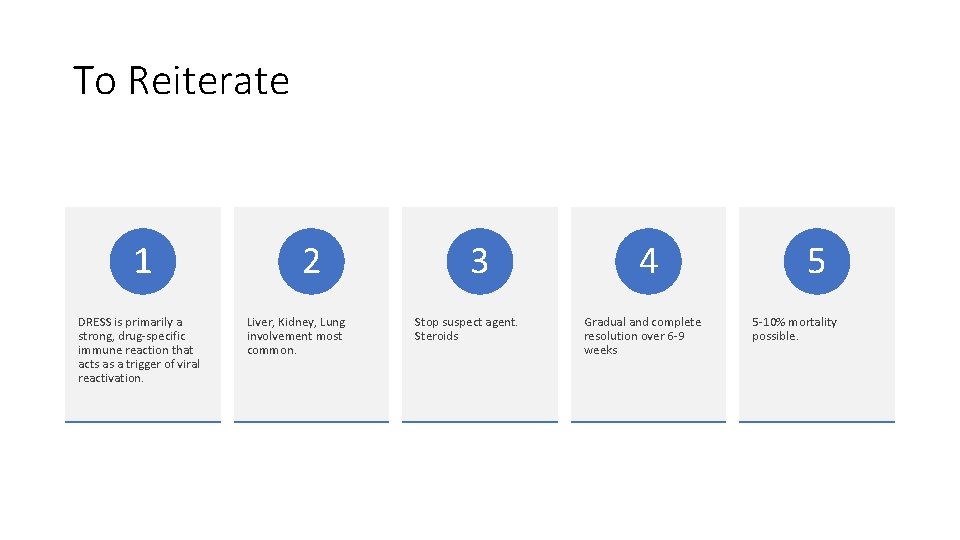
To Reiterate 1 DRESS is primarily a strong, drug‐specific immune reaction that acts as a trigger of viral reactivation. 2 Liver, Kidney, Lung involvement most common. 3 Stop suspect agent. Steroids 4 Gradual and complete resolution over 6‐ 9 weeks 5 5‐ 10% mortality possible.
Identification and consideration of DRESS syndrome as diagnosis Takeaway points Consideration of alternative, equally threatening diagnoses such as SJS/TEN Appropriate treatment and initial management on presumption prior to biopsy‐proven diagnosis
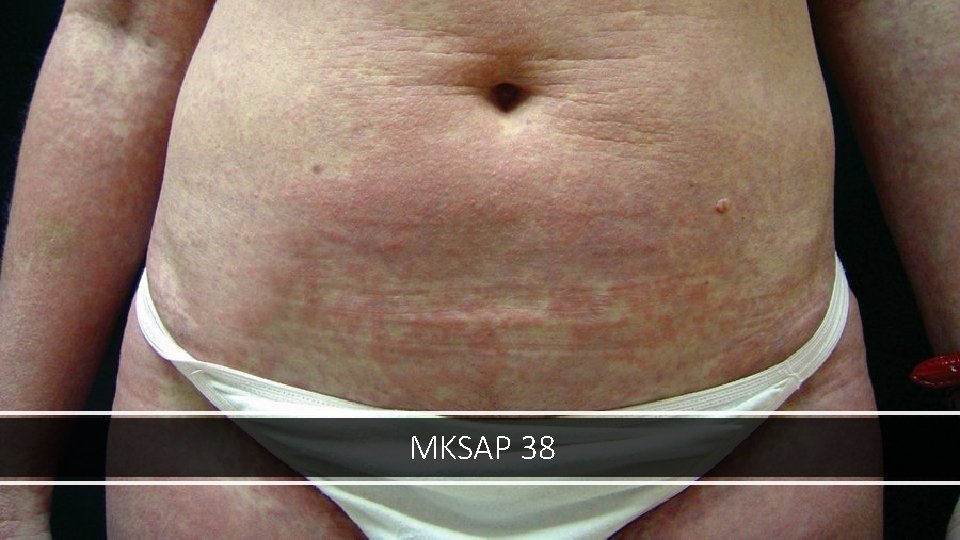
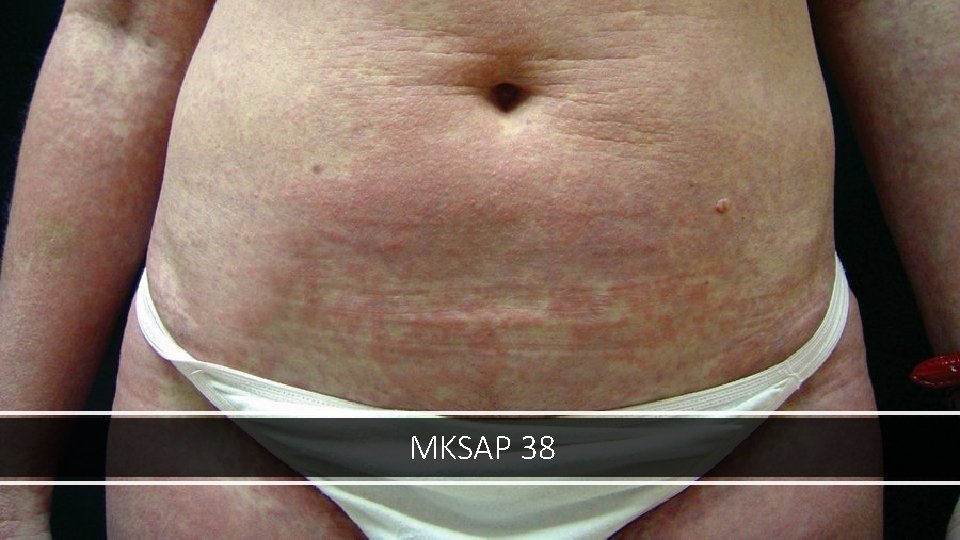
MKSAP 38
References • Ortonne, N & Valeyrie‐Allanore, L & Bastuji‐Garin, S & Wechsler, Janine & de Feraudy, S & Duong, Tu Anh & Delfau‐Larue, Marie & Chosidow, O & Wolkenstein, P & Roujeau, J. ‐C. (2015). Histopathology of drug rash with eosinophilia and systemic symptoms (DRESS): a morphologic and phenotypic study. British Journal of Dermatology. 173. . 10. 1111/bjd. 13683. • Tetart F, Picard D, Janela B, Joly P, Musette P. Prolonged Evolution of Drug Reaction With Eosinophilia and Systemic Symptoms. Clinical, Virologic, and Biological Features. JAMA Dermatol. 2014; 150(2): 206– 207. doi: 10. 1001/jamadermatol. 2013. 6698 • MKSAP Dermatology • Upto. Date
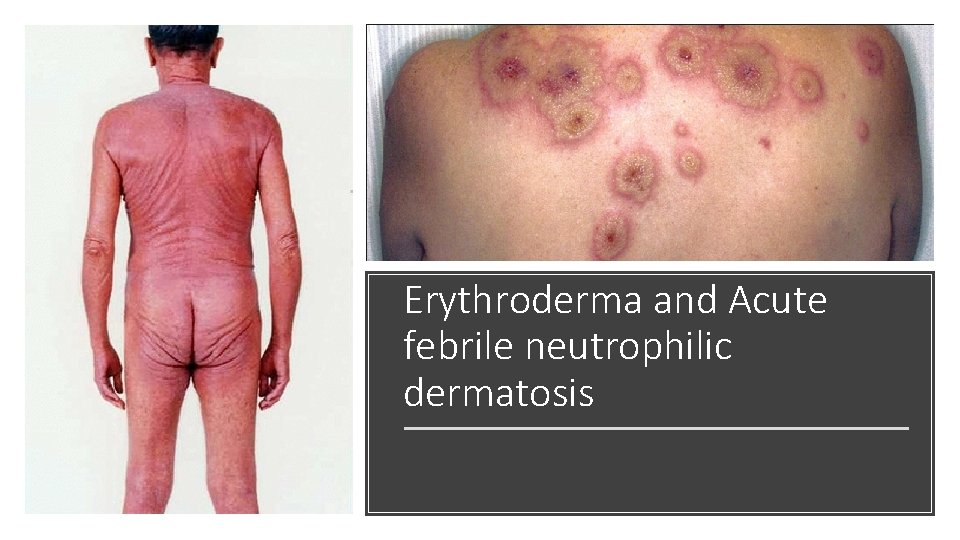
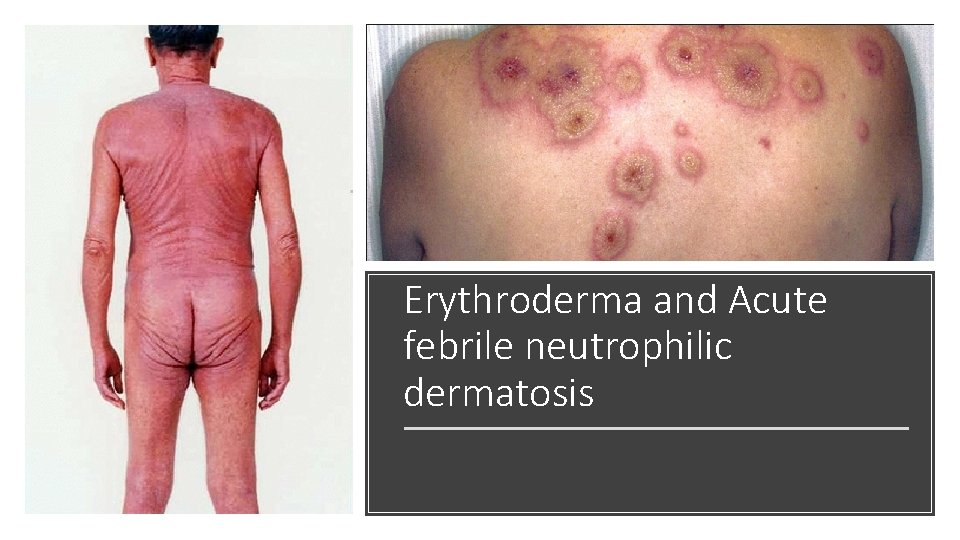
Erythroderma and Acute febrile neutrophilic dermatosis
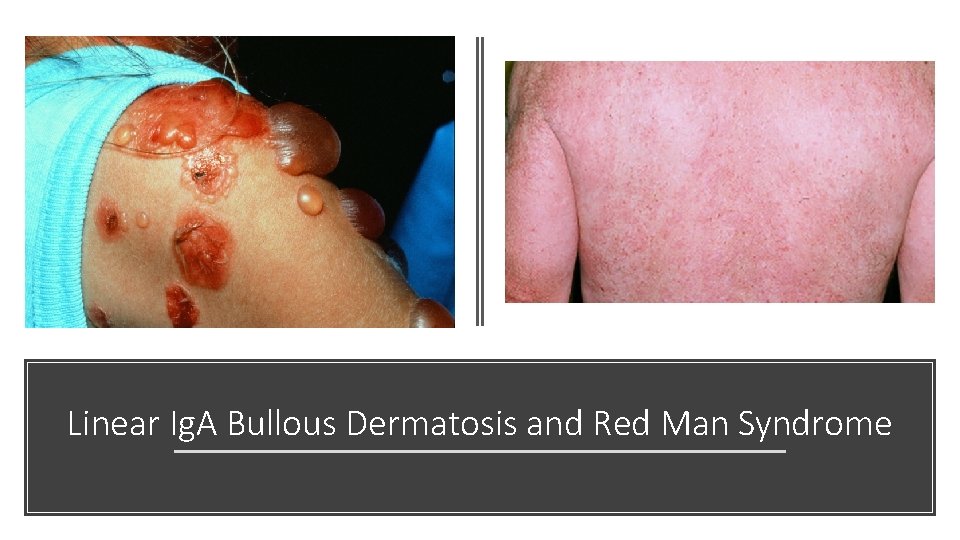
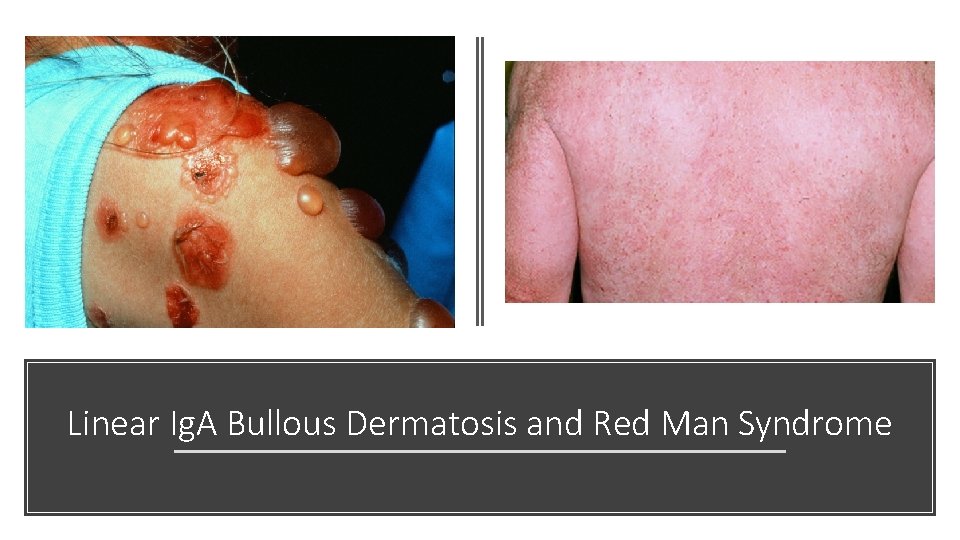
Linear Ig. A Bullous Dermatosis and Red Man Syndrome

SJS