IVRA BIERS BLOCK Presented by DR ATIF KHALID

IVRA (BIER’S BLOCK) Presented by: DR ATIF KHALID Moderator: Dr Nazia Tauheed
OVERVIEW Introduction Procedure & Mechanism of Action Indications & Advantages Limitations/Contraindications Complications Conclusion

INTRODUCTION
First introduced by Dr. August K. G. Bier in 1908 Repopularized by Holmes in 1963 DEFINITION: Consists of injecting local anaesthetic solutions into the venous system of an upper or lower extremity that has been exsanguinated by compression or gravity & that has been isolated by means of a tourniquet from the central circulation.
PROCEDURE & MECHANISM
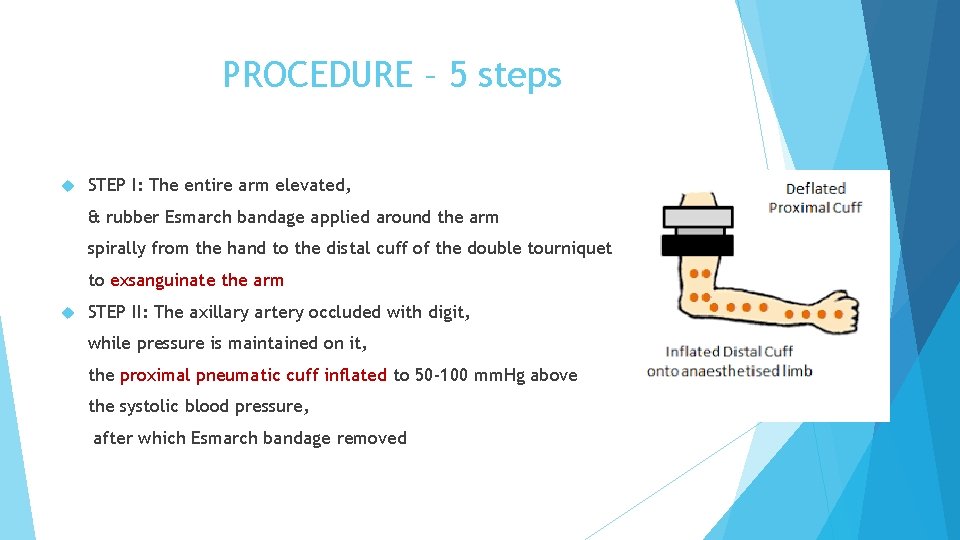
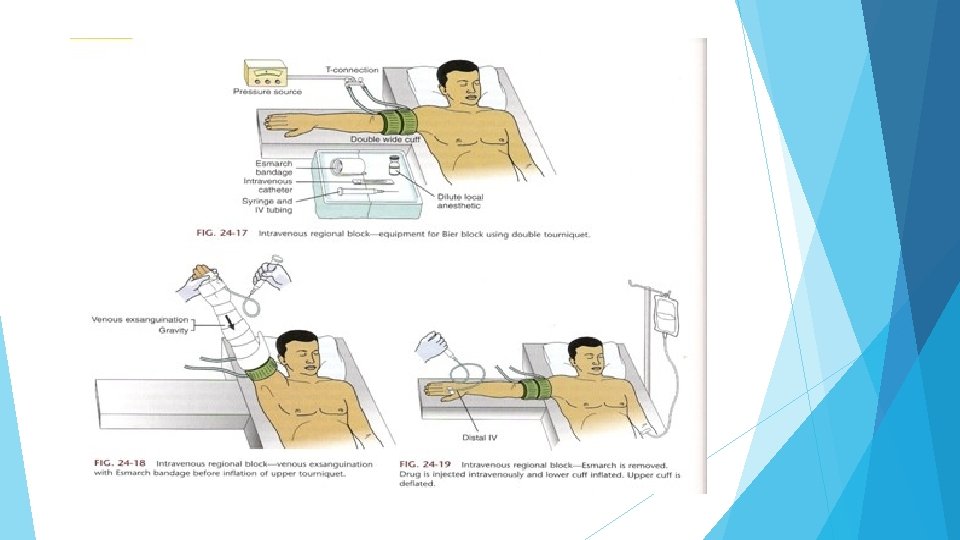
PROCEDURE – 5 steps STEP I: The entire arm elevated, & rubber Esmarch bandage applied around the arm spirally from the hand to the distal cuff of the double tourniquet to exsanguinate the arm STEP II: The axillary artery occluded with digit, while pressure is maintained on it, the proximal pneumatic cuff inflated to 50 -100 mm. Hg above the systolic blood pressure, after which Esmarch bandage removed
STEP III: 30 -50 ml of 0. 5% lidocaine injected via the indwelling cannula, volume depending on size of arm being anesthetized. STEP IV: The arm is now brought down to the level of the procedure table, the IV cannula in the surgical extremity is withdrawn, and pressure quickly applied over the site of cannulation.
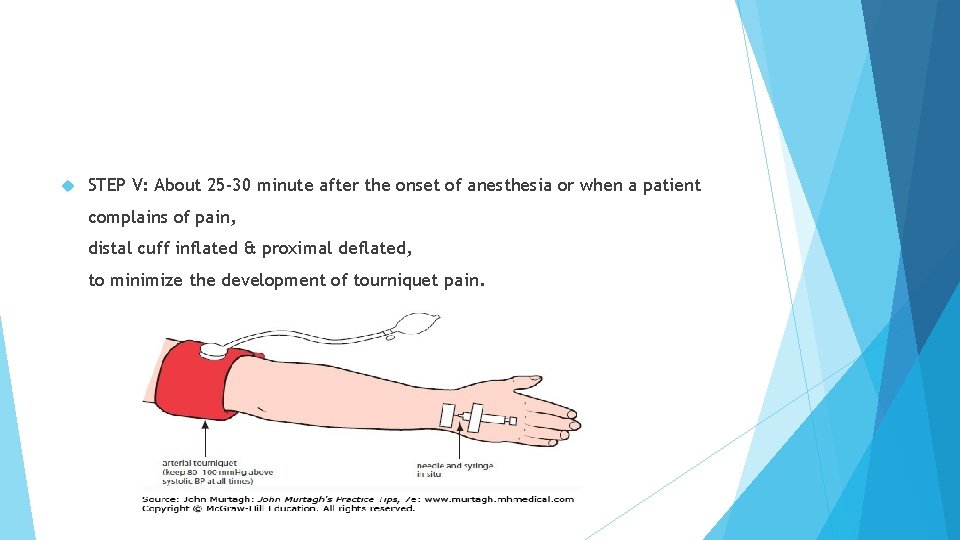
STEP V: About 25 -30 minute after the onset of anesthesia or when a patient complains of pain, distal cuff inflated & proximal deflated, to minimize the development of tourniquet pain.
EQUIPMENTS Operative and reliable double cuff tourniquet 22 gauge intravenous cannula Flexible extension tubing Running IV in non operative arm Resuscitation equipment Esmarch bandage (about 150 cm in length, 10 cm in width) 20 ml syringes with local anesthetic Pressure source
SEQUENCE OF EVENTS RESULTING IN ANESTHESIA AND ANALGESIA INJECTION OF LOCAL ANESTHETICInitial analgesia produced by LA action on major nerve trunks, small nerves, & nerve endings ASPYHXIAAsphyxia at 20 -30 minutes complementing local anesthetic action. Local anesthetic molecules transverse venous walls into surrounding tissue HYPOTHERMIA AND ACIDOSISresult in enhanced local anesthetic activity.
MINIMUM TIME FOR TOURNIQUET INFLATION The tourniquet should be up for at least 25 minutesmay result in toxicity releasing it before this Releasing the tourniquet in cyclic deflations (2 minutes intervals) will decrease peak levels of local anesthetic
DRUGS AND DOSAGE 1) PRILOCAINE- § The drug of choice as it is least toxic § Largest therapeutic index § Dose 3 mg/kg § One complication is methemoglobinemia. Prilocaine is metabolized to o-toluidine derivatives which convert hemoglobin to methemoglobin. Treat with 1 -2 mg/kg of 1% methylene blue given over 5 minutes § Onset 2 -15 minutes § Duration 1 -4 hours
2) BUPIVACAINE • Not suitable • It is too toxic, particularly to the myocardium • Slower onset
3) LIGNOCAINE • Acceptable alternative only if prilocaine is not available • Dose is 3 mg/kg • Onset 1. 5 -5 minutes • Duration 1 -4 hours • Never use Epinephrine containing solution
DOSAGE The arm dosage can be 30 -40 ml of 0. 5% prilocaine or 0. 5% lidocaine In leg, larger volumes 50 -60 ml Start the procedure after 3 -6 minutes
MECHANISM OF ACTION Peripheral nerve endings of the extremities nourished by small blood vessels Injection of LA solution into venous system → diffusion of LA into the nerve endings → development of anesthesia Holds true as long as concentration of LA in the venous system remains relatively high.
MECHANISM OF ACTION Not clearly understood Local anesthetics, ischemia, asphyxia, hypothermia, and acidosis may play a role.

INDICATIONS & ADVANTAGES
INDICATIONS Closed fractures Foreign body removal Burn debridement Carpal tunnel release Removal of ground-indebris Ganglionectomy Tendon contracture release Abscess Incision and drainage Laceration repair
ADVANTAGES Easy to administer Low incidence of block failure Simple and reliable Patient is awake during anesthesia Safe technique when used appropriately Rapid onset & recovery Muscle relaxation

LIMITATIONS & CONTRAINDICATIONS
LIMITATIONS Ideal for procedures lasting for 40 -60 minutes Maximum time limit 90 min, useful for only short procedures Tourniquet pain generally starts after 20 -30 minutes Lack of post-operative analgesia. Sudden cardiovascular collapse or seizures if LA released into the circulation too early. Rapid recovery may lead to post-operative pain Difficulty in providing a bloodless field
CONTRAINDICATIONS The only absolute contraindication is patient refusal RELATIVE CONTRAINDICATIONS: o Reynaud’s disease o Homozygous sickle cell disease o Crush injuries / Multiple trauma (crush injuries of relevant limb) o Shock o Younger children o Hypersensitivity to Prilocaine or Lidocaine o Must have reliable/operative tourniquet. If not guaranteed then this technique should not be used due to risk of LA toxicity.

COMPLICATIONS
COMPLICATIONS LA toxicity due to malfunctioning tourniquets or deflating tourniquet prior to 25 minute limit Haematoma Engorgement of extremity Echymoses & subcutaneous hemorrhages Tourniquet discomfort Rapid return of sensation after tourniquet release & subsequent surgical pain
CONCLUSION IVRA is a simple and valuable technique is easy to learn and perform, very safe provided excessive doses of local anesthetic are avoided, if the tourniquet pressure is carefully monitored & if resuscitation equipment always immediately available.

THANKS
RELEVANT QUESTIONS Explain in brief, the mechanism of anaesthesia in IVRA. Mention the limitations & Complications of IVRA. Write in brief about the drugs suitable for IVRA.
- Slides: 29