Isolation Precaution Techniques MAURE E N S PE



- Slides: 48
Isolation Precaution Techniques MAURE E N S PE NCER, M. ED, BS N, RN, CIC , FAPIC INFE CTION P REVENTION CO NSU LTANT WW W. MA URE EN SPENC ER. CO M
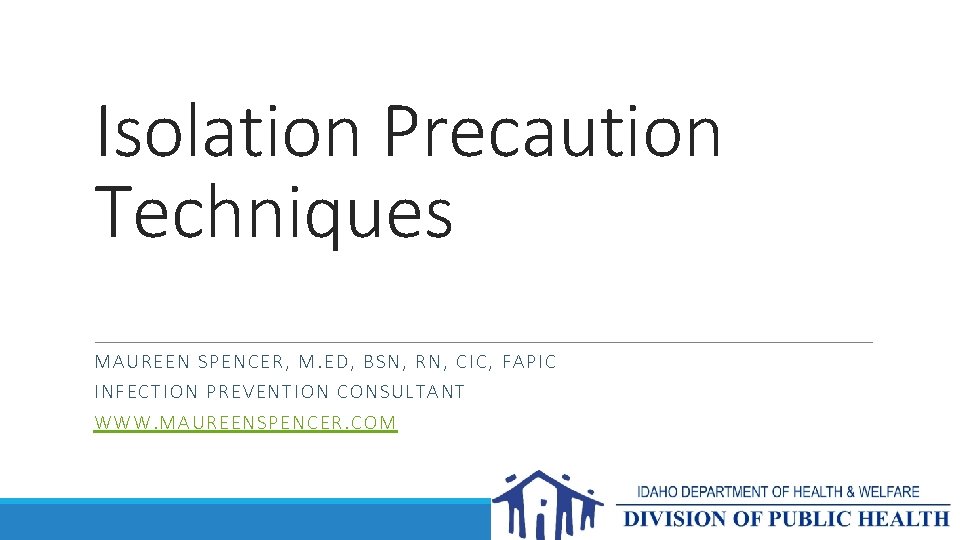
Categories of Precautions = Mode of Transmission Modes of Transmission: Direct contact with blood and bodily fluids (HIV, HBV) Indirect contact with contaminated items and patient care equipment and the environment (MRSA, VRE, C. difficile) Droplet nuclei (Influenza, Pertussis, Bacterial Meningitis, SARS) Airborne route (TB, Chickenpox, Measles) Vector (West Nile Virus, Malaria, Ebola Virus)
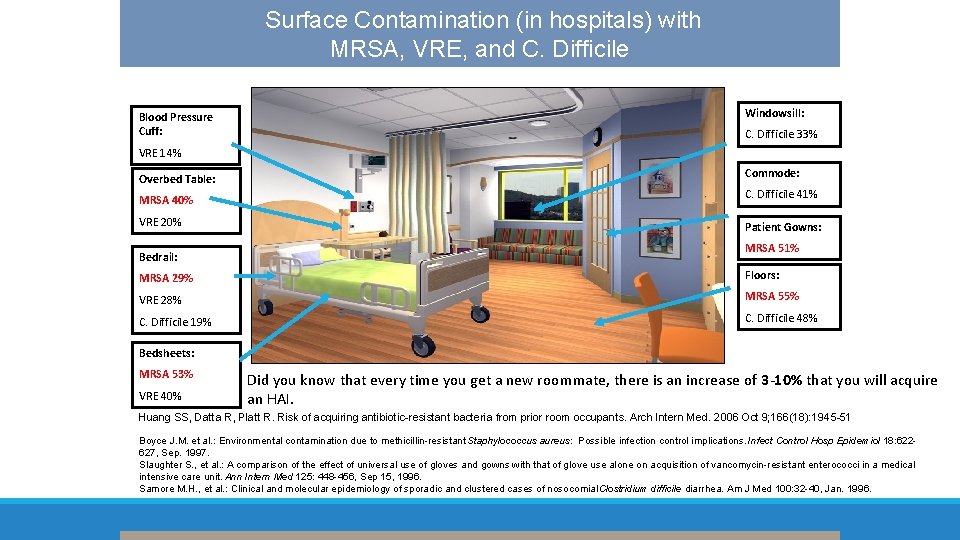
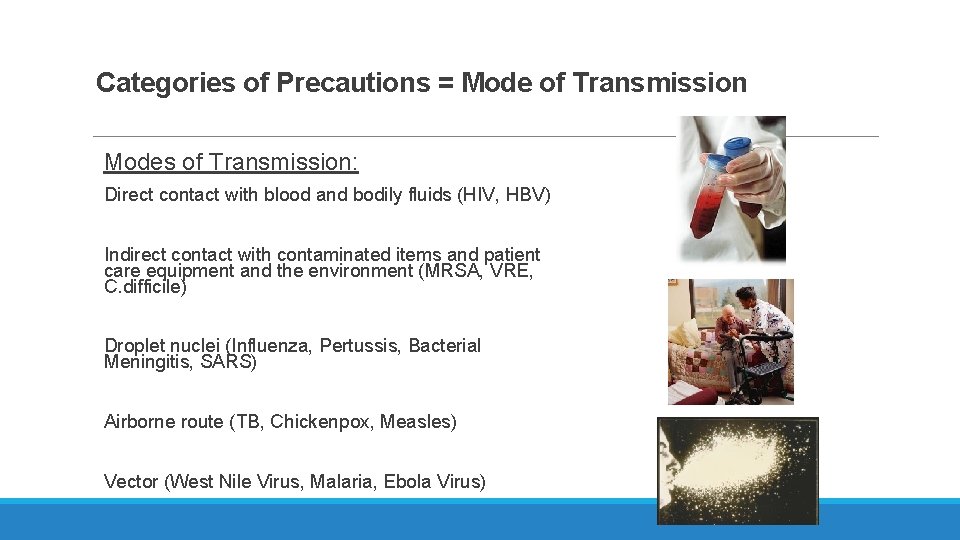
Surface Contamination (in hospitals) with MRSA, VRE, and C. Difficile Blood Pressure Cuff: Windowsill: C. Difficile 33% VRE 14% Overbed Table: Commode: MRSA 40% C. Difficile 41% VRE 20% Patient Gowns: Bedrail: MRSA 51% MRSA 29% Floors: VRE 28% MRSA 55% C. Difficile 19% C. Difficile 48% Bedsheets: MRSA 53% VRE 40% Did you know that every time you get a new roommate, there is an increase of 3 -10% that you will acquire an HAI. Huang SS, Datta R, Platt R. Risk of acquiring antibiotic-resistant bacteria from prior room occupants. Arch Intern Med. 2006 Oct 9; 166(18): 1945 -51 Boyce J. M. et al. : Environmental contamination due to methicillin-resistant Staphylococcus aureus: Possible infection control implications. Infect Control Hosp Epidemiol 18: 622627, Sep. 1997. Slaughter S. , et al. : A comparison of the effect of universal use of gloves and gowns with that of glove use alone on acquisition of vancomycin-resistant enterococci in a medical intensive care unit. Ann Intern Med 125: 448 -456, Sep 15, 1996. Samore M. H. , et al. : Clinical and molecular epidemiology of sporadic and clustered cases of nosocomial Clostridium difficile diarrhea. Am J Med 100: 32 -40, Jan. 1996.
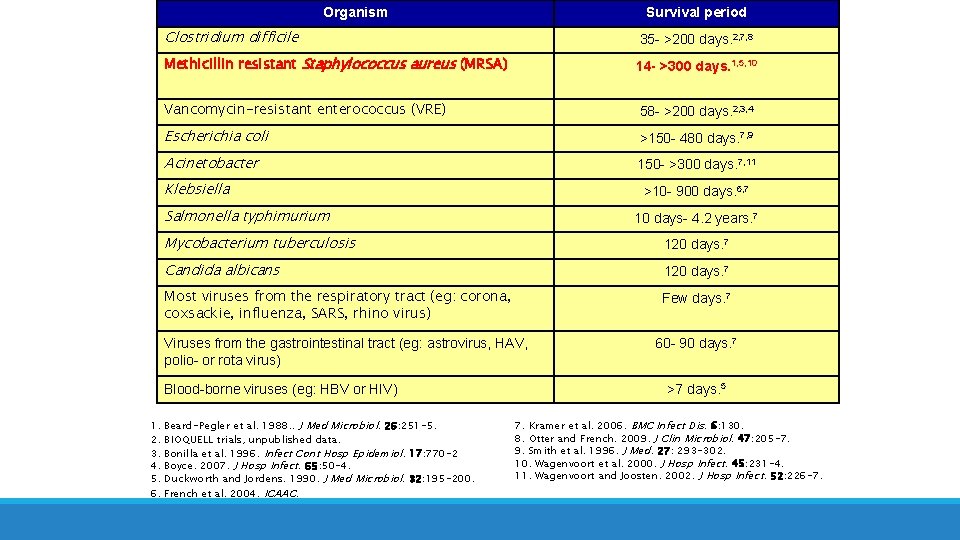
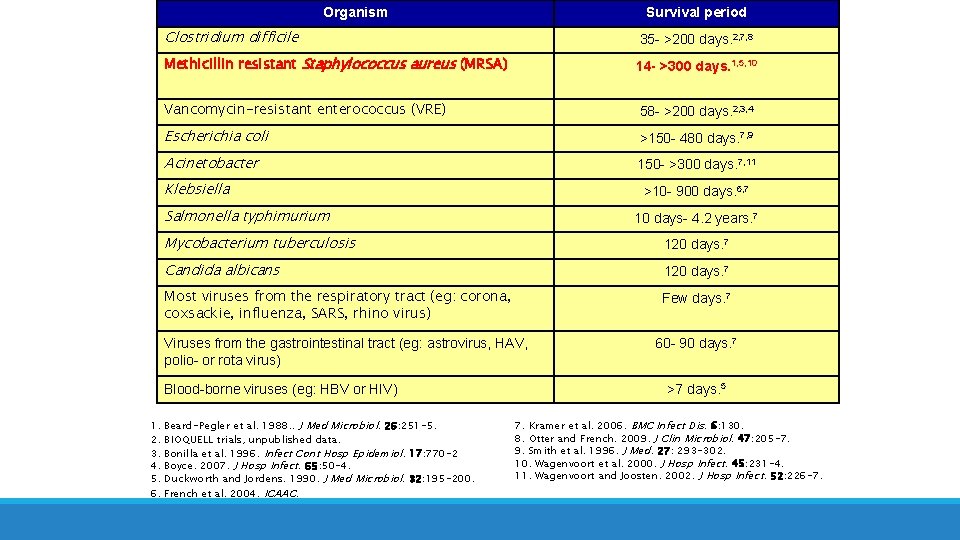
Organism Survival period Clostridium difficile 35 - >200 days. 2, 7, 8 Methicillin resistant Staphylococcus aureus (MRSA) 14 - >300 days. 1, 5, 10 Vancomycin-resistant enterococcus (VRE) 58 - >200 days. 2, 3, 4 Escherichia coli >150 - 480 days. 7, 9 Acinetobacter 150 - >300 days. 7, 11 Klebsiella >10 - 900 days. 6, 7 Salmonella typhimurium 10 days- 4. 2 years. 7 Mycobacterium tuberculosis 120 days. 7 Candida albicans 120 days. 7 Most viruses from the respiratory tract (eg: corona, coxsackie, influenza, SARS, rhino virus) Few days. 7 Viruses from the gastrointestinal tract (eg: astrovirus, HAV, polio- or rota virus) Blood-borne viruses (eg: HBV or HIV) 1. 2. 3. 4. 5. 6. Beard-Pegler et al. 1988. . J Med Microbiol. 26: 251 -5. BIOQUELL trials, unpublished data. Bonilla et al. 1996. Infect Cont Hosp Epidemiol. 17: 770 -2 Boyce. 2007. J Hosp Infect. 65: 50 -4. Duckworth and Jordens. 1990. J Med Microbiol. 32: 195 -200. French et al. 2004. ICAAC. 60 - 90 days. 7 >7 days. 5 7. Kramer et al. 2006. BMC Infect Dis. 6: 130. 8. Otter and French. 2009. J Clin Microbiol. 47: 205 -7. 9. Smith et al. 1996. J Med. 27: 293 -302. 10. Wagenvoort et al. 2000. J Hosp Infect. 45: 231 -4. 11. Wagenvoort and Joosten. 2002. J Hosp Infect. 52: 226 -7.
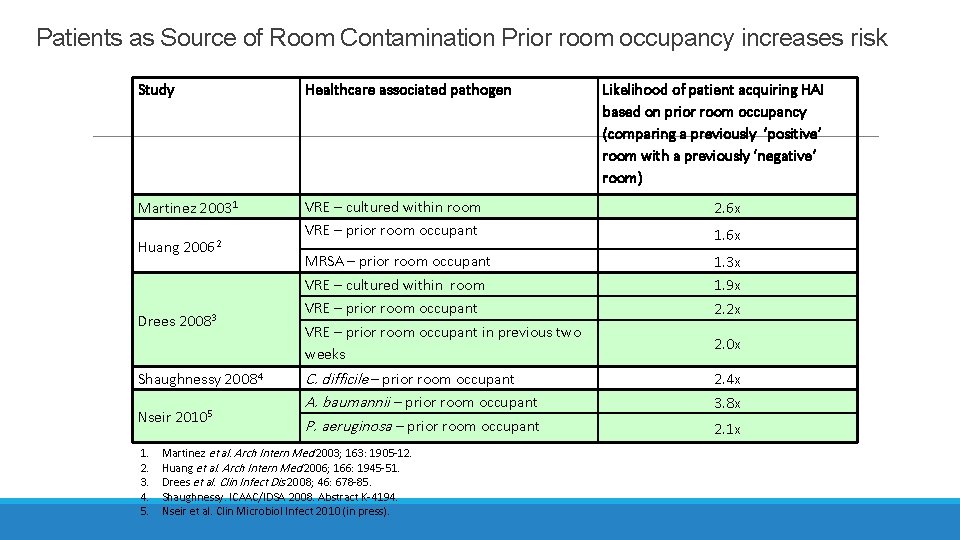
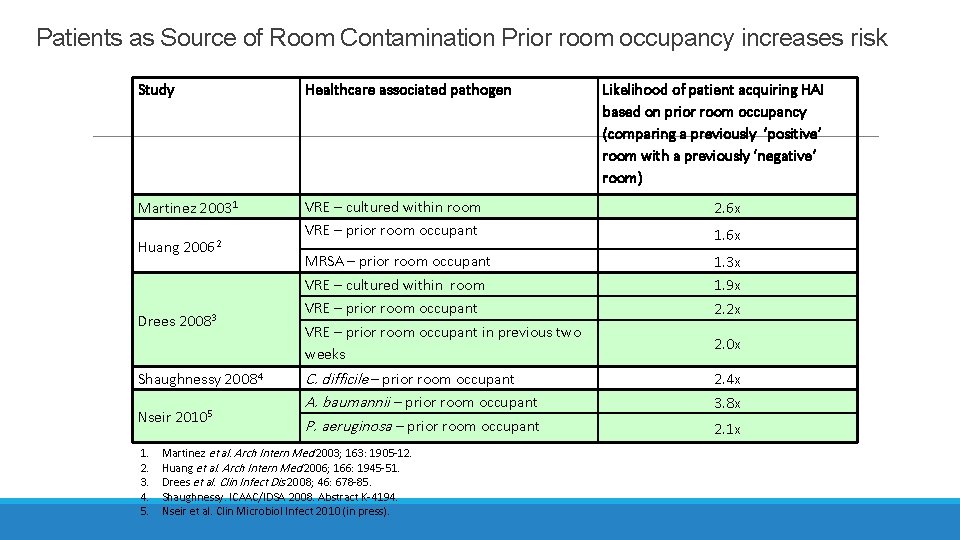
Patients as Source of Room Contamination Prior room occupancy increases risk Study Healthcare associated pathogen Martinez 20031 VRE – cultured within room VRE – prior room occupant 2. 6 x MRSA – prior room occupant VRE – cultured within room VRE – prior room occupant in previous two weeks 1. 3 x 1. 9 x 2. 2 x C. difficile – prior room occupant A. baumannii – prior room occupant P. aeruginosa – prior room occupant 2. 4 x 3. 8 x Huang 20062 Drees 20083 Shaughnessy 20084 Nseir 20105 1. 2. 3. 4. 5. Martinez et al. Arch Intern Med 2003; 163: 1905 -12. Huang et al. Arch Intern Med 2006; 166: 1945 -51. Drees et al. Clin Infect Dis 2008; 46: 678 -85. Shaughnessy. ICAAC/IDSA 2008. Abstract K-4194. Nseir et al. Clin Microbiol Infect 2010 (in press). Likelihood of patient acquiring HAI based on prior room occupancy (comparing a previously ‘positive’ room with a previously ‘negative’ room) 1. 6 x 2. 0 x 2. 1 x
Precautions are used for both colonized and infected patients Colonization: The complex process of new organisms becoming a part of the endogenous flora of an area of the body with no signs of active infection Infection: The presence of signs and symptoms of a host/pathogen response (fever, drainage, cough, purulence, inflammation, etc. )
Standard Precautions Applies to everyone Hand washing Gloves, masks and gowns when deemed necessary to protect you Cleaning patient care equipment between patient use Environmental controls Careful handling of linen Appropriate patient placement
Precaution Materials *Precaution Gowns *Gloves *Masks *Private Room *Precaution Cart or Mounted Container *Signage *Dedicated Equipment (stethoscope, sphgmanometer, commodes) *Alcohol Hand Rub *Red Bags for Infectious Waste Disposal
Additions to Standard Precautions Safer injection practices ◦ ◦ ◦ multiple outbreaks of infections attributed to unsafe injection practices use a sterile single-use needle and syringe for each injection use single-use medication vials whenever possible and avoid using multiple dose vials avoid reinsertion of used needles in multiple dose vials or solutions avoid use of single-use needles and syringes to administer intravenous medication to multiple patients Special lumbar puncture procedures ◦ Use a face mask during spinal procedures (e. g. , lumbar punctures, myelogram, and spinal anesthesia) ◦ mask prevents oral contamination during lumbar puncture procedures Respiratory hygiene/cough etiquette ◦ Respiratory hygiene and cough etiquette include covering the mouth and nose during coughing and sneezing with a tissue or offering a surgical mask to the coughing patient ◦ discarding the mask or tissue appropriately ◦ performing hand hygiene ◦ posting signs in public areas in languages appropriate to the population served ◦ educating healthcare staff, patients, and visitors
Transmission-Based Precautions Contact Special Contact (Clostridium difficile) Droplet Airborne
Contact Precautions ØUsed for diseases transmitted by contact with the patient or the patient’s environment ØDiseases caused by organisms that have been demonstrated to cause heavy environmental contamination, such as vancomycin-resistant Enterococcus (VRE), methicillin-resistant Staphylococcus aureus (MRSA), or respiratory syncytial virus (RSV) in infants, children, and immunocompromised adults ØRequire gowns and gloves on room entry
Contact Precautions Patient Placement: A single room is preferred; however, patients with the same disease or organism may share a room Avoid placing immunocompromised patients or other patients who may have adverse outcomes from infection with a patient on Contact Precautions. Personal Protective Equipment (PPE): Wear a gown and gloves on room entry. Change the gown and gloves between patients even if both patients share a room and both are on Contact Precautions.
Contact Precautions MRSA, VRE, C. Difficile, Abscess, Draining Cellulitis, Herpes Zoster (vesicles), Impetigo, Staph aureus wound infections, Streptococcus wound infections, MDR-Acinetobacter, E. Coli, Klebsiella New: CRE, MERS-Co. V, H 7 N 9 Remember also for significant fecal incontinence - 2/3 of feces is pure organisms!
Contact Precautions Techniques Gloves for EVERYONE entering the room – including physicians, visitors, family members
Contact Precautions Techniques Inside the Room: ◦ Covered linen hamper ◦ Red lined trash container ◦ Alcohol Hand Rub ◦ Stethoscope and Blood Pressure Equipment ◦ Disposable Thermometers ◦ Red Bags for disposal of contaminated dressings and items used in patient care ◦ Sani. Cloths– lid must be kept closed to prevent evaporation
MRSA contamination in precaution rooms 70% of rooms had environmental contamination when the patient was colonized or infected 42% of nurses’ gloves cultured were contaminated after touching environmental surfaces WITHOUT touching the patient! Boyce, J et al. Infec Cont Hosp Epid 1977
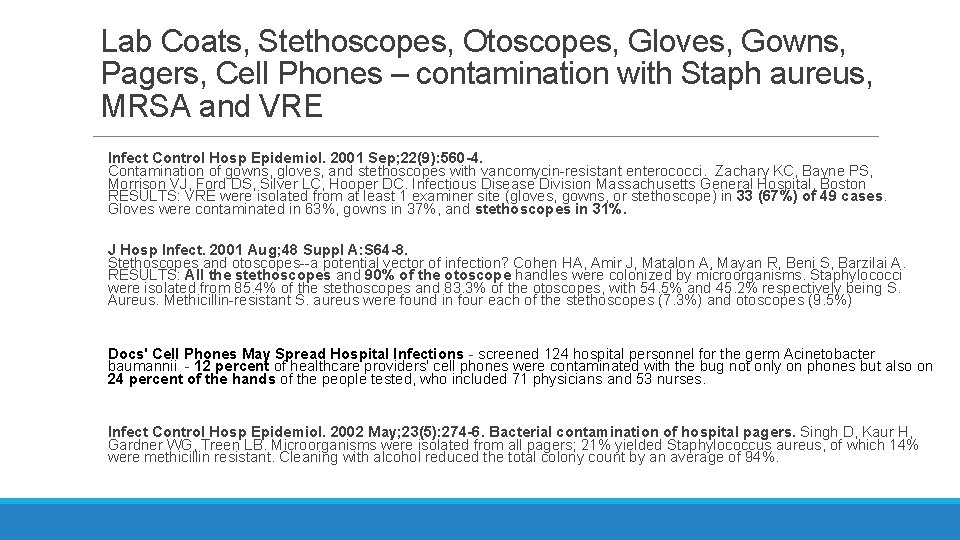
Lab Coats, Stethoscopes, Otoscopes, Gloves, Gowns, Pagers, Cell Phones – contamination with Staph aureus, MRSA and VRE Infect Control Hosp Epidemiol. 2001 Sep; 22(9): 560 -4. Contamination of gowns, gloves, and stethoscopes with vancomycin-resistant enterococci. Zachary KC, Bayne PS, Morrison VJ, Ford DS, Silver LC, Hooper DC. Infectious Disease Division Massachusetts General Hospital, Boston RESULTS: VRE were isolated from at least 1 examiner site (gloves, gowns, or stethoscope) in 33 (67%) of 49 cases. Gloves were contaminated in 63%, gowns in 37%, and stethoscopes in 31%. J Hosp Infect. 2001 Aug; 48 Suppl A: S 64 -8. Stethoscopes and otoscopes--a potential vector of infection? Cohen HA, Amir J, Matalon A, Mayan R, Beni S, Barzilai A. RESULTS: All the stethoscopes and 90% of the otoscope handles were colonized by microorganisms. Staphylococci were isolated from 85. 4% of the stethoscopes and 83. 3% of the otoscopes, with 54. 5% and 45. 2% respectively being S. Aureus. Methicillin-resistant S. aureus were found in four each of the stethoscopes (7. 3%) and otoscopes (9. 5%) Docs' Cell Phones May Spread Hospital Infections - screened 124 hospital personnel for the germ Acinetobacter baumannii - 12 percent of healthcare providers' cell phones were contaminated with the bug not only on phones but also on 24 percent of the hands of the people tested, who included 71 physicians and 53 nurses. Infect Control Hosp Epidemiol. 2002 May; 23(5): 274 -6. Bacterial contamination of hospital pagers. Singh D, Kaur H, Gardner WG, Treen LB. Microorganisms were isolated from all pagers; 21% yielded Staphylococcus aureus, of which 14% were methicillin resistant. Cleaning with alcohol reduced the total colony count by an average of 94%.
Discontinuation of Precautions for MRSA One negative PCR for MRSA If using a culture - three negative surveillance cultures from nares obtained on separate days Patient must be off mupirocin and antibiotic therapy for MRSA One negative culture from original site of infection (urine, wound, g-tube, sputum, etc. )
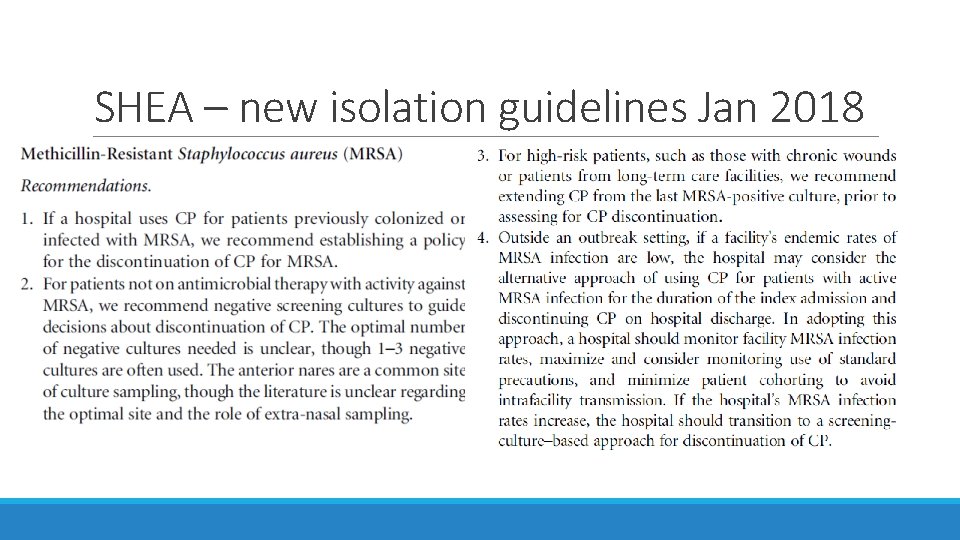
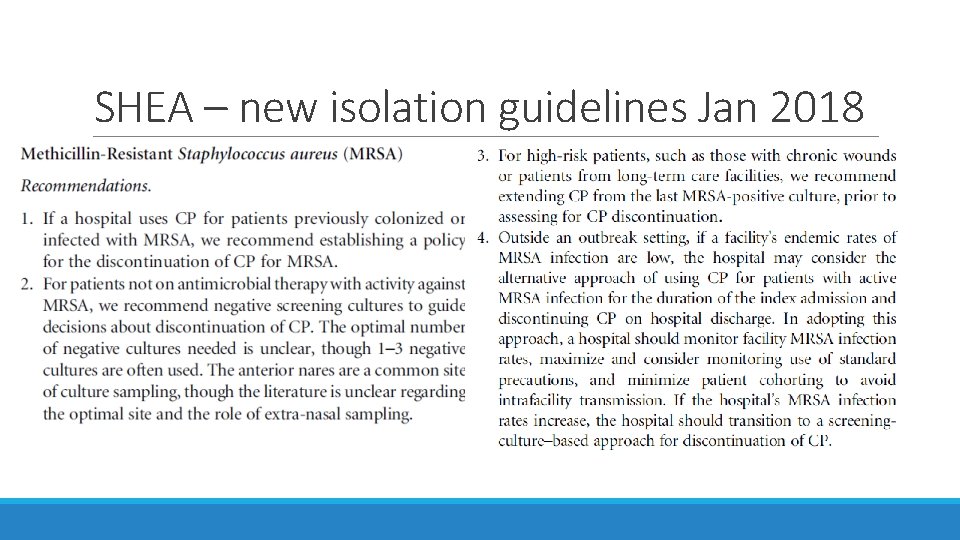
SHEA – new isolation guidelines Jan 2018
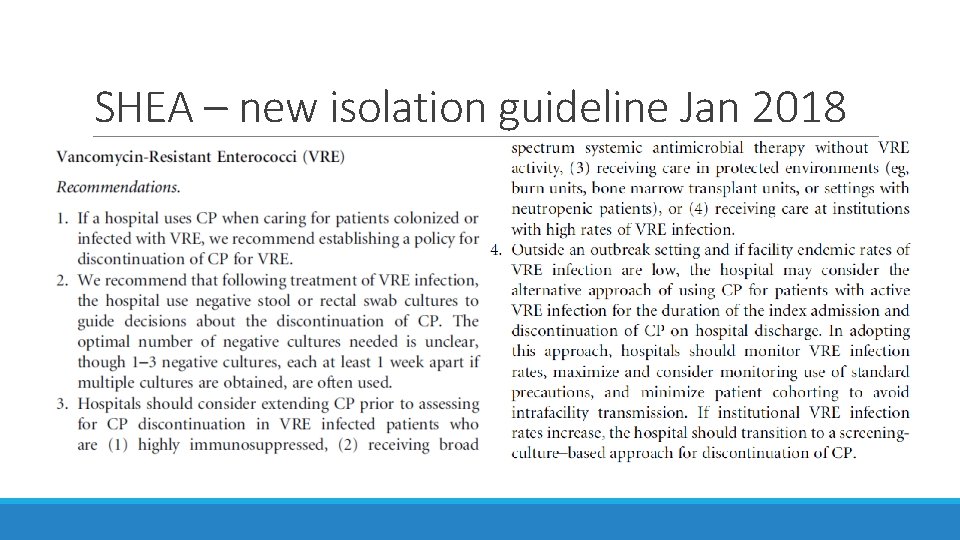
Discontinuation of Precautions for VRE Three negative surveillance cultures from rectal/stool specimen obtained on separate days Patient must be off antibiotic therapy for VRE One negative cultures from original site of infection (urine, wound, g-tube, sputum, etc. )
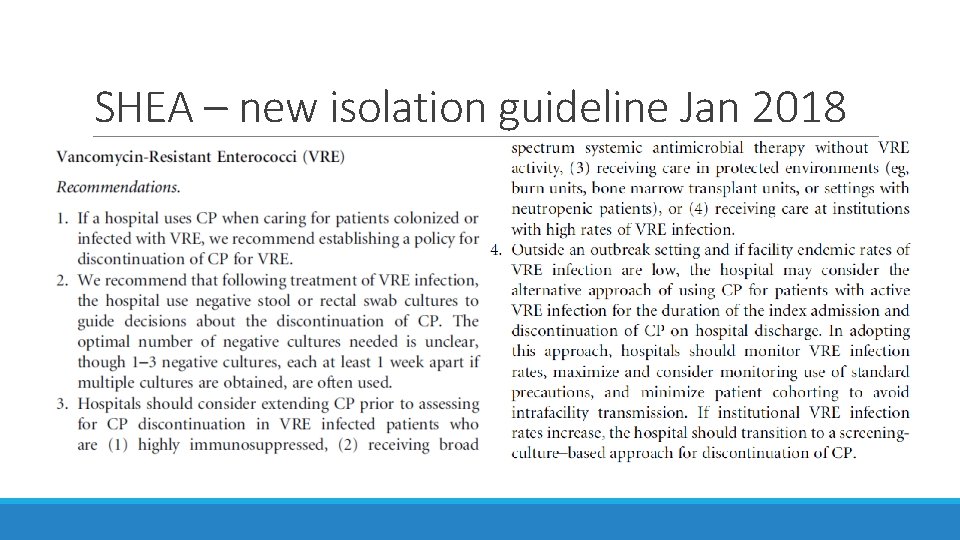
SHEA – new isolation guideline Jan 2018
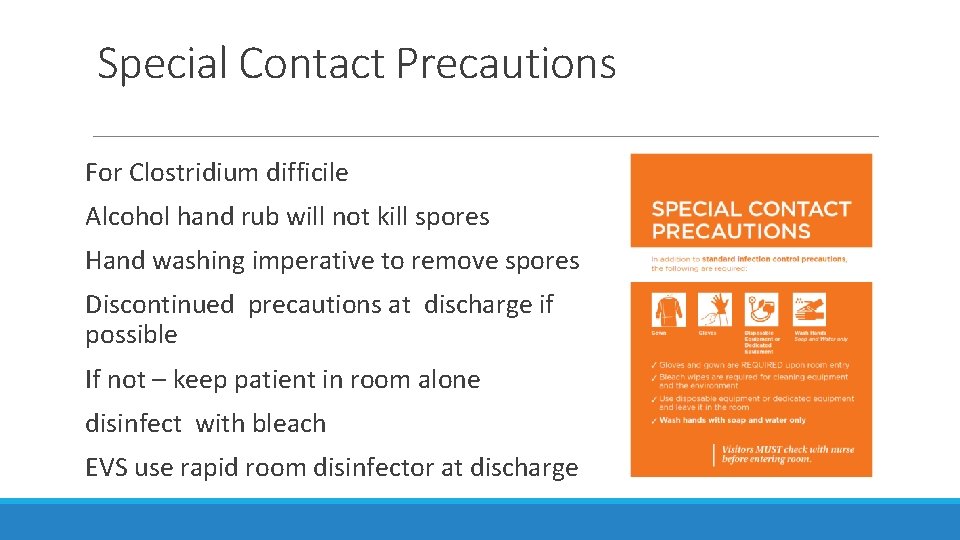
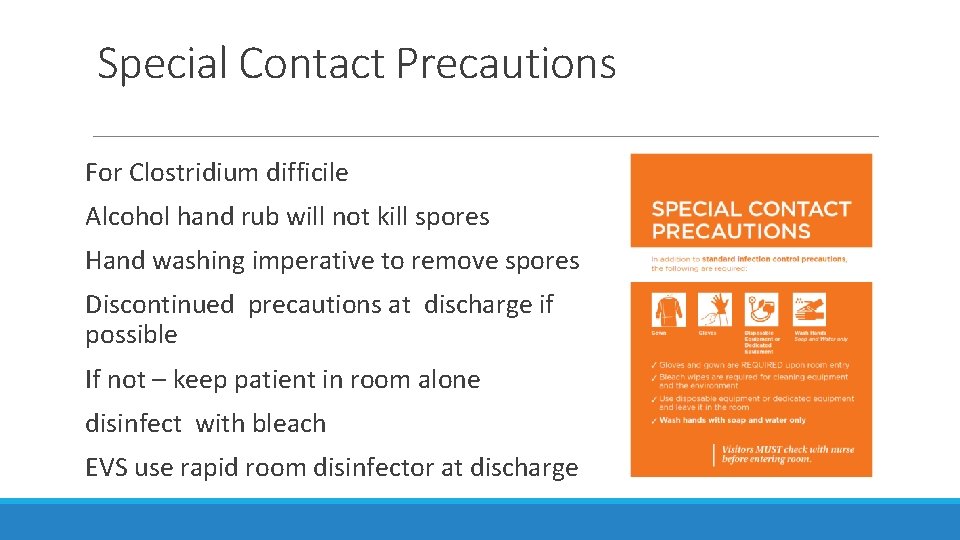
Special Contact Precautions For Clostridium difficile Alcohol hand rub will not kill spores Hand washing imperative to remove spores Discontinued precautions at discharge if possible If not – keep patient in room alone disinfect with bleach EVS use rapid room disinfector at discharge
Special Contact Precautions Meticulous environmental cleaning and use of products with a C. difficile inactivation label claim (such as bleach) Strict hand hygiene Good laundry practices are recommended to decrease transmission of C. difficile Commodes should have a commode liner
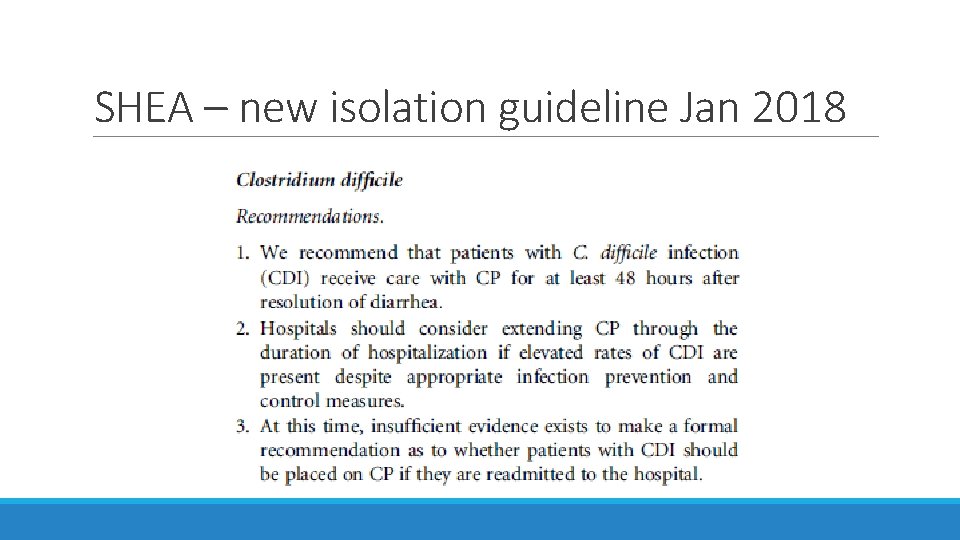
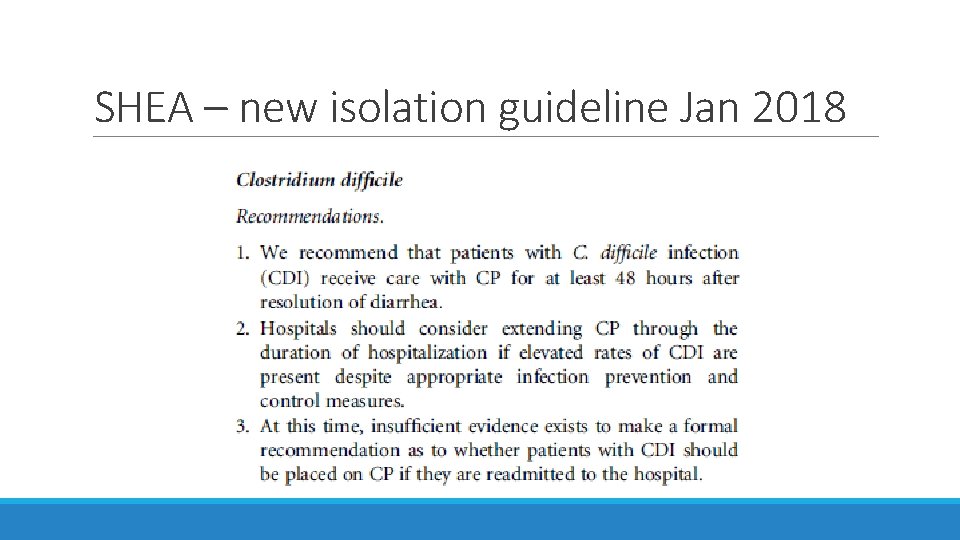
SHEA – new isolation guideline Jan 2018
Discontinuation of Precautions for Clostridium Difficile No policy requiring surveillance cultures for C. difficile Maintain precautions until discharge (if possible) ◦ Up to 70 percent of patients may have skin contamination with C. difficile 6 days after the resolution of diarrhea and 40 percent may have skin contamination up to 9 days after the resolution of diarrhea
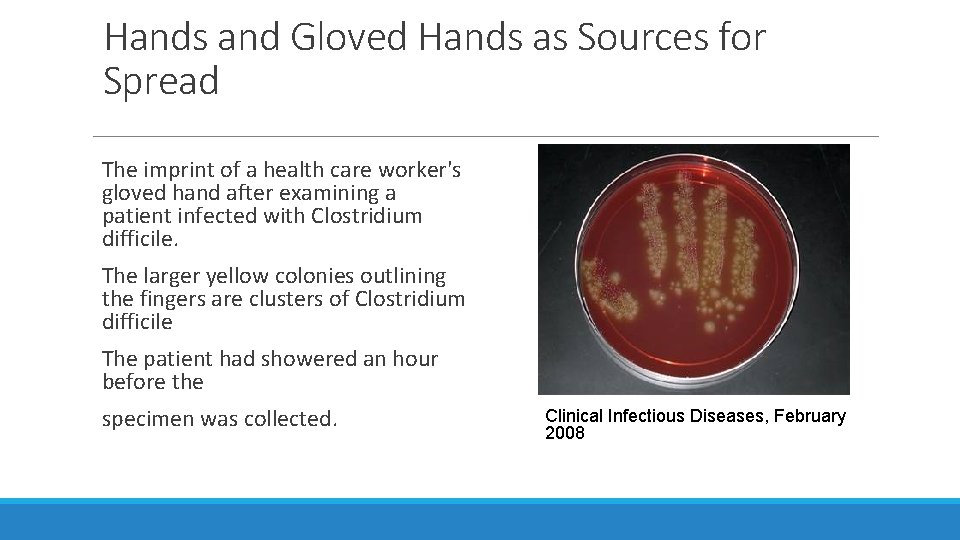
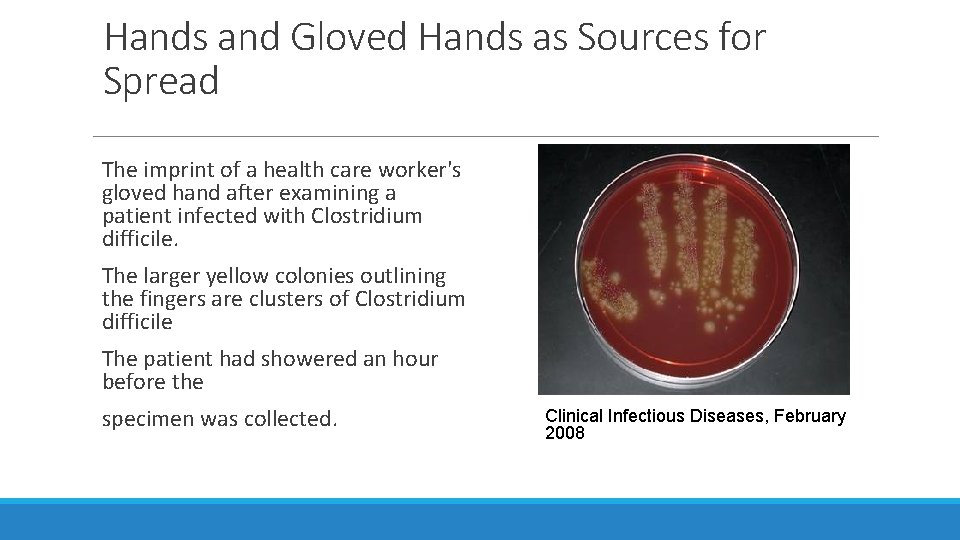
Hands and Gloved Hands as Sources for Spread The imprint of a health care worker's gloved hand after examining a patient infected with Clostridium difficile. The larger yellow colonies outlining the fingers are clusters of Clostridium difficile The patient had showered an hour before the specimen was collected. Clinical Infectious Diseases, February 2008

New Technology for Environmental Disinfection Movable UV-C robots for terminal cleaning (Steriliz) Copper surfaces (EOScu) Permanent fixture white light disinfection (Indigo Clean) Disinfecting Ceiling Light Units (Vitashield) Movable air treatment system with HEPA filer and UV (Aerobiotix) Spencer M, et al: A model for choosing an automated ultraviolet-C disinfection system and building a case for the C-suite: Two case reports. AJIC 2016
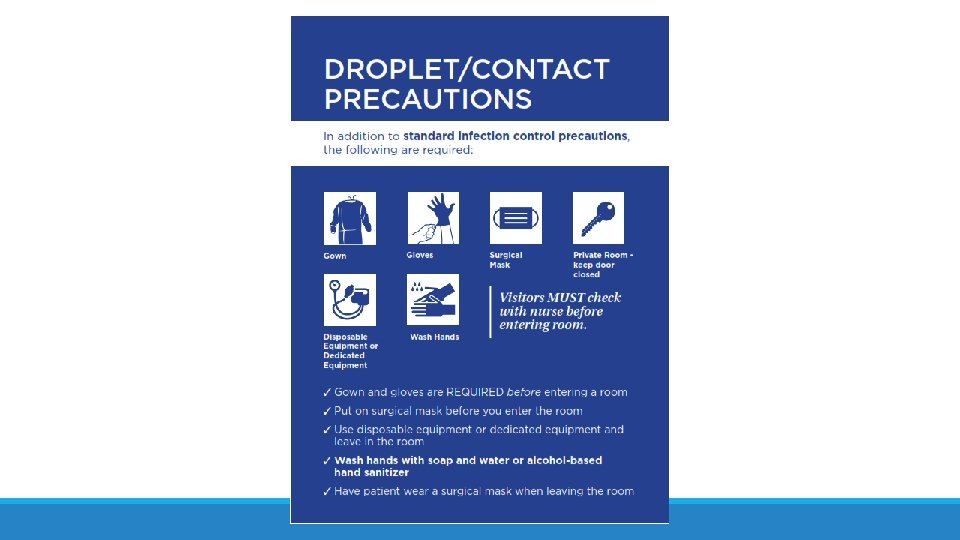
Droplet Precautions Prevent transmission of diseases caused by large respiratory droplets that are generated by coughing, sneezing, or talking H 3 N 2 flu season 2017 -2018 is transmitted by even talking – ineffective vaccine this year as well
Droplet Precautions Influenza Meningitis - Hemophilus Meningococcemia Mumps Pertussis Rubella Sudden Acute Respiratory Syndrome (SARS)
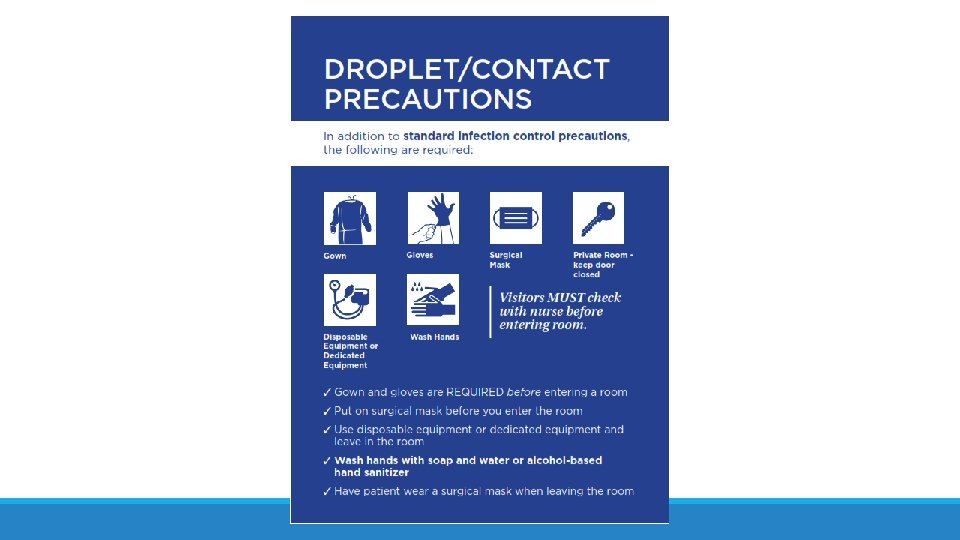
Droplet Precautions Private Room (does not have to be a negative pressure room) Masks for all entering the room
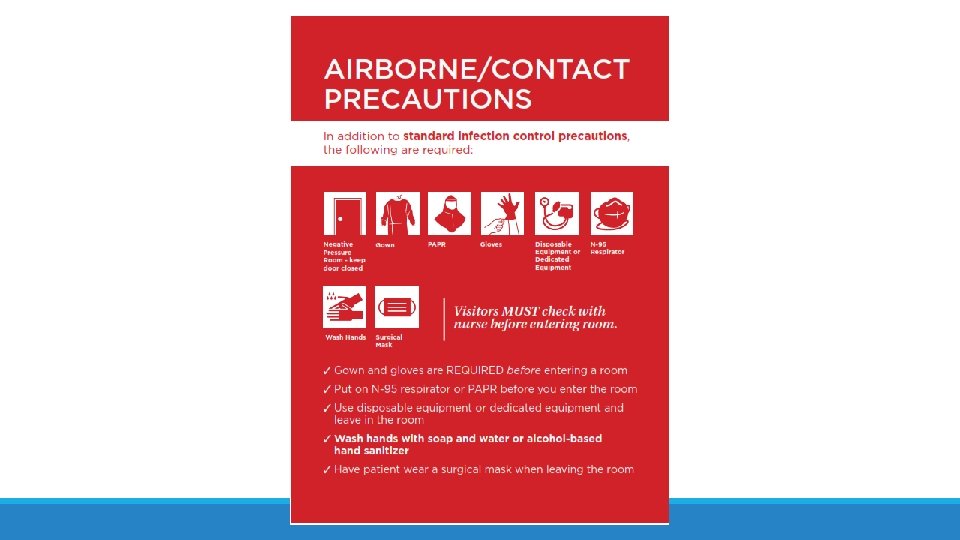
Airborne Precautions Pulmonary Tuberculosis Sputum AFB Positive Chickenpox Disseminated Herpes Zoster Measles Avian Flu NEW: MERS-Co. V, H 7 N 9
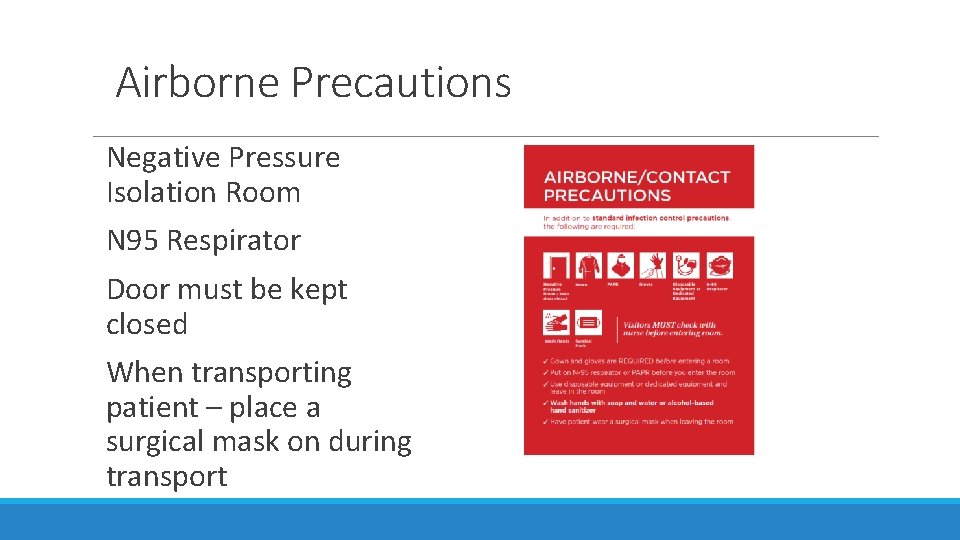
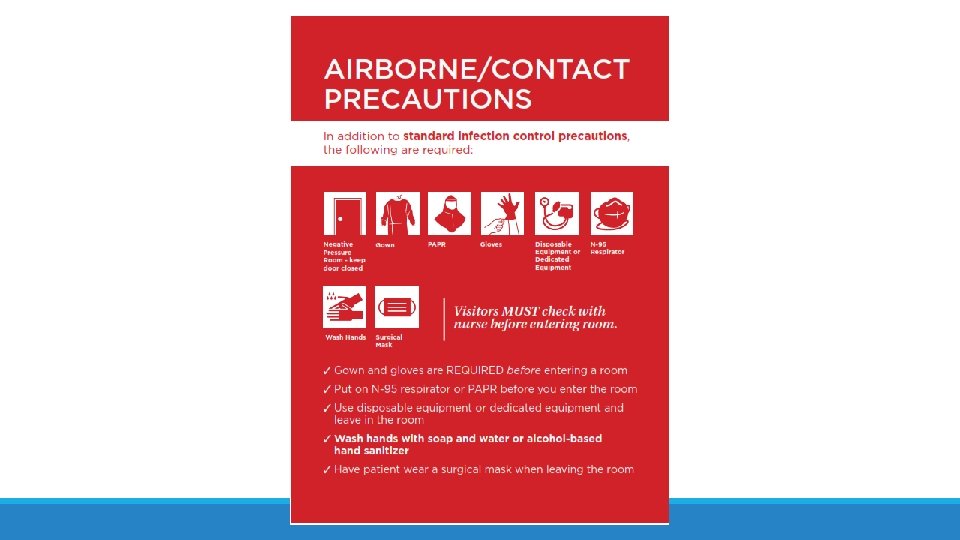
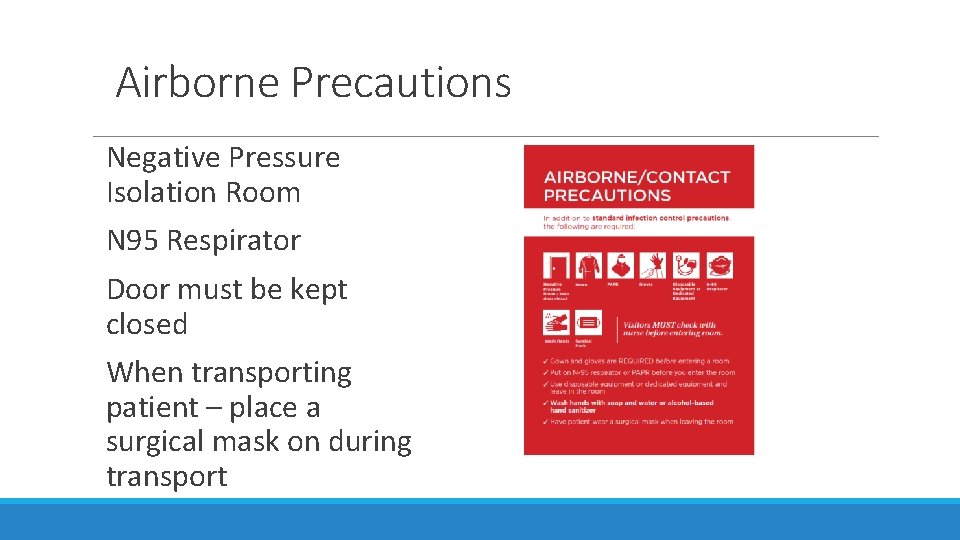
Airborne Precautions Negative Pressure Isolation Room N 95 Respirator Door must be kept closed When transporting patient – place a surgical mask on during transport
Environmental Disinfection Quaternary disinfectant used in all Contact Precaution rooms to clean bed, bedside equipment and environmental surfaces (ex 456, Virex, HBQuat) Sani Cloths are used for low level disinfection – they are bactericidal, virucidal, tuberculocidal Bleach Sani Cloths for C difficile and bathrooms Hyrdrogen peroxide sani cloths
Patient Transport Limit patient transport outside the room to medically necessary purposes Inform the receiving department of the Isolation Precautions status of the patient Cover or contain potentially infectious body fluids before transport The transporter should discard contaminated PPE before transport Don clean PPE to handle the patient at the destination
Ambulatory Settings and Long-term Care Settings Place patients on Contact Precautions in examination rooms as soon as possible In long-term care settings, patient placement should be handled on a case-by-case basis Each facility should make decisions on the basis of infection risks to other patients in the facility
Environmental Measures §Clean daily with a focus on high touch areas, patient bathrooms, and areas close to the patient §EVS workers should don gown and gloves before room entry to clean the patient’s room §Processes for room disinfection should be audited, especially in outbreak scenarios, to ensure compliance
Hand Hygiene

DIRECT TRANSMISSION FROM HANDS MOST COMMON WAY DISEASE IS TRANSMITTED
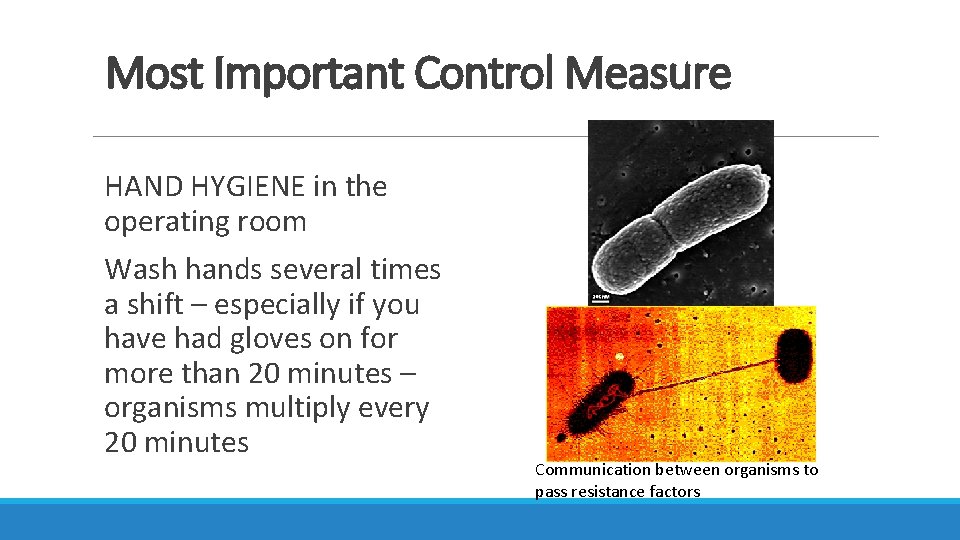
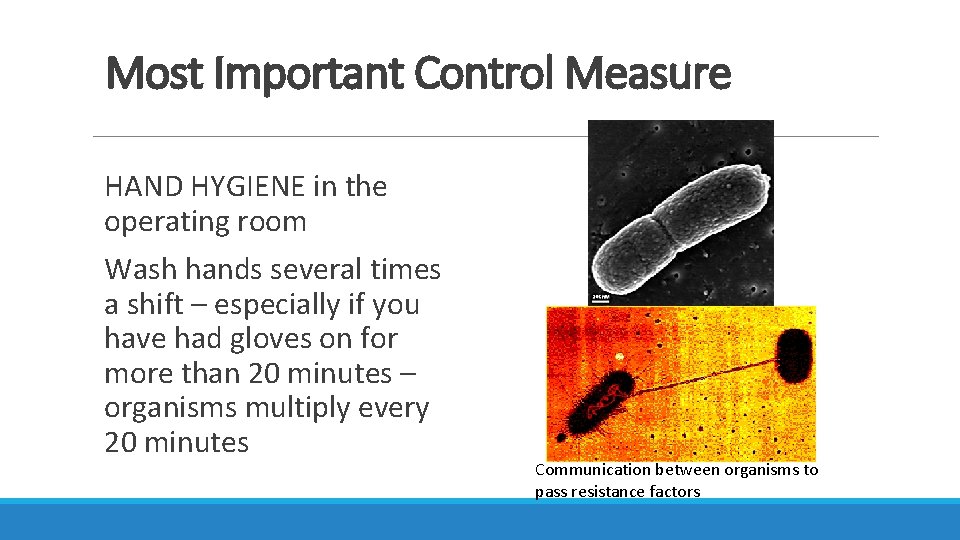
Most Important Control Measure HAND HYGIENE in the operating room Wash hands several times a shift – especially if you have had gloves on for more than 20 minutes – organisms multiply every 20 minutes Communication between organisms to pass resistance factors
Most Important Control Measure HAND HYGIENE Wash hands several times a shift – especially if you have had gloves on for more than 20 minutes – organisms multiply every 20 minutes
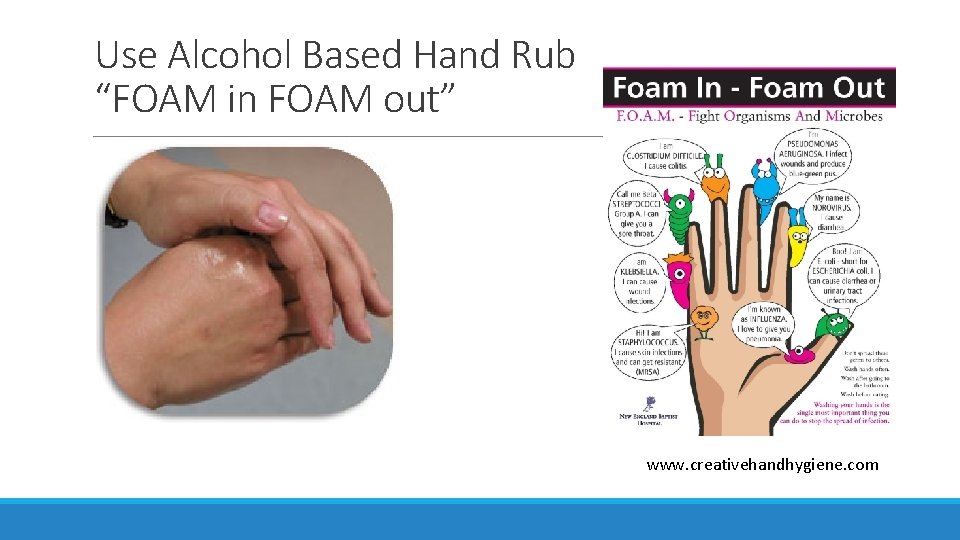
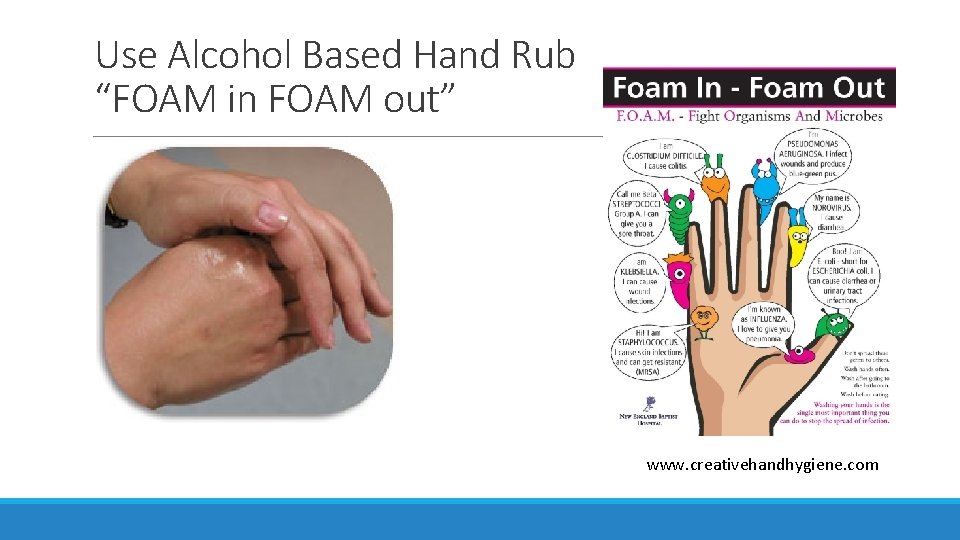
Use Alcohol Based Hand Rub “FOAM in FOAM out” www. creativehandhygiene. com

Hand Cultures – before and after
THE END M. R. S. A. “ MAKE RESISTANCE STAY AWAY”