Isolation Identification of Staphylococci Staphylococci Characteristics Staphylococci are




- Slides: 34
ﺑﺴﻢ ﺍﻟﻠﻪ ﺍﻟﺮﺣﻤﻦ ﺍﻟﺮﺣﻴﻢ Isolation & Identification of Staphylococci
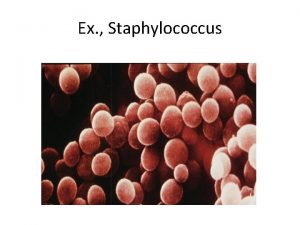
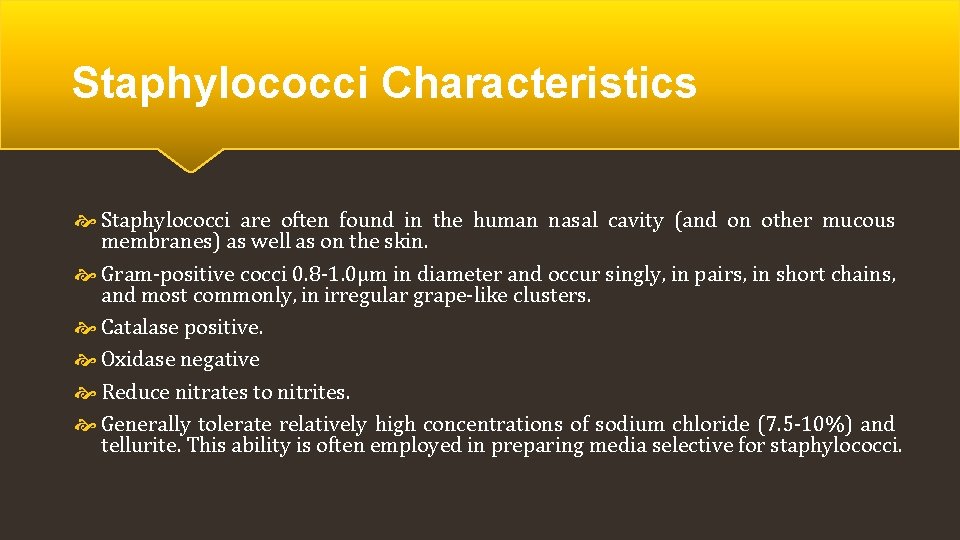
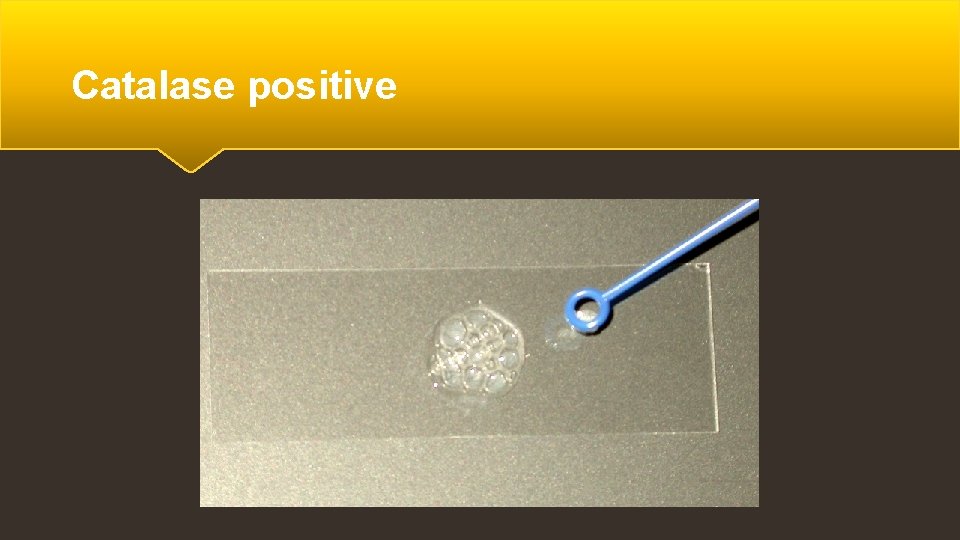
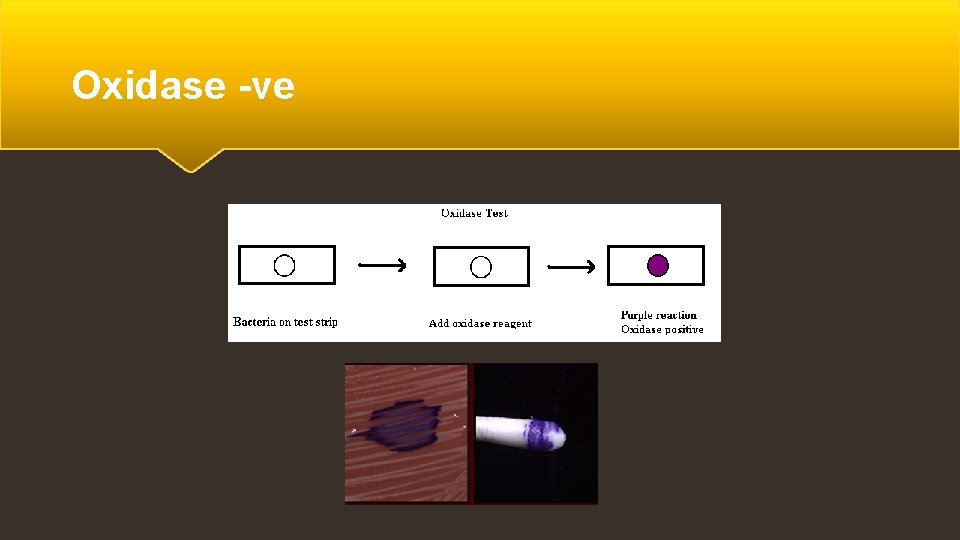
Staphylococci Characteristics Staphylococci are often found in the human nasal cavity (and on other mucous membranes) as well as on the skin. Gram-positive cocci 0. 8 -1. 0µm in diameter and occur singly, in pairs, in short chains, and most commonly, in irregular grape-like clusters. Catalase positive. Oxidase negative Reduce nitrates to nitrites. Generally tolerate relatively high concentrations of sodium chloride (7. 5 -10%) and tellurite. This ability is often employed in preparing media selective for staphylococci.
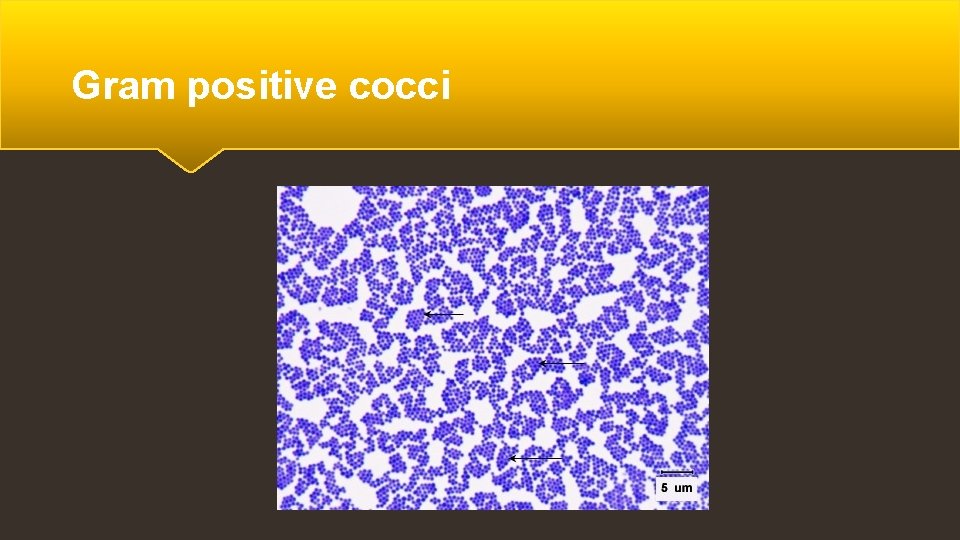
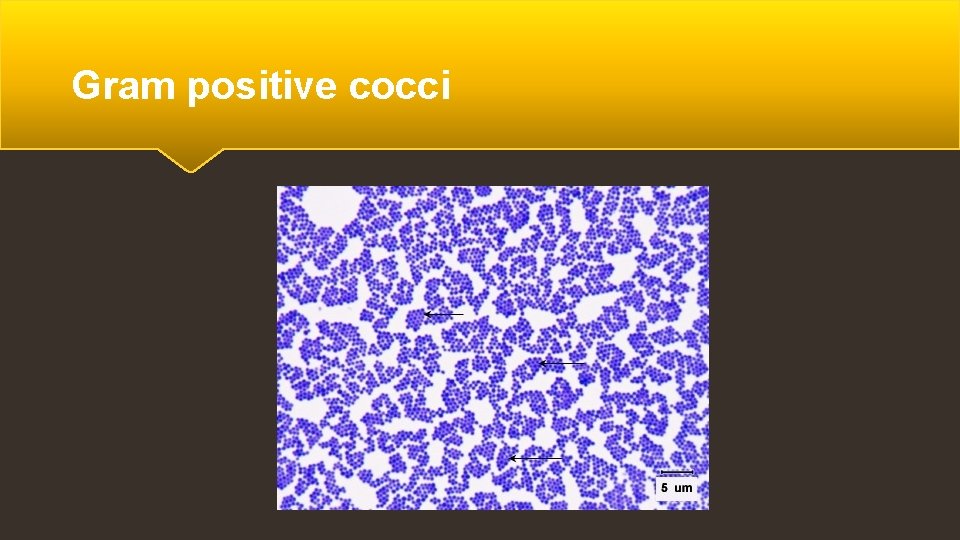
Gram positive cocci
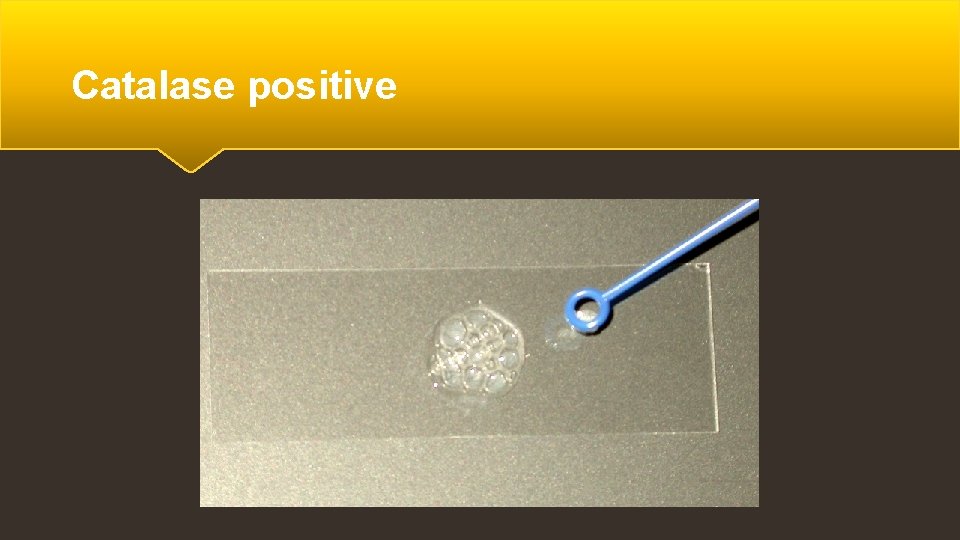
Catalase positive
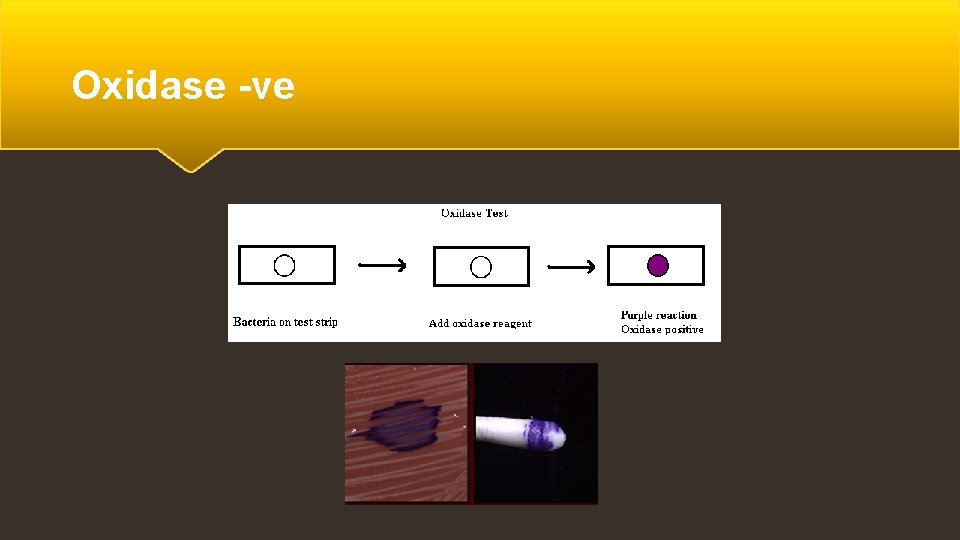
Oxidase -ve
Staphylococci Species There are five species of staphylococci commonly associated with clinical infections: 1) Staphylococcus aureus. 2) Staphylococcus epidermidis. 3) Staphylococcus haemolyticus. 4) Staphylococcus saprophyticus.
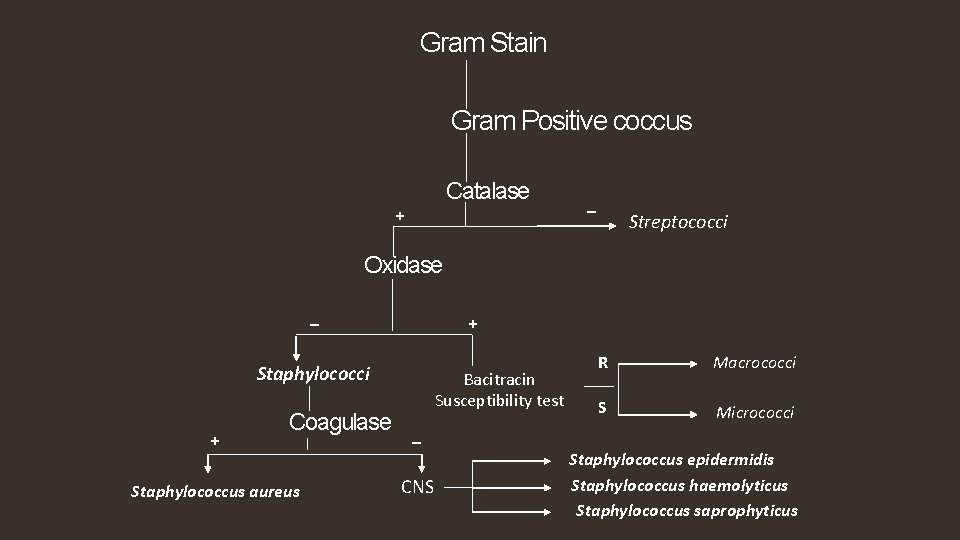
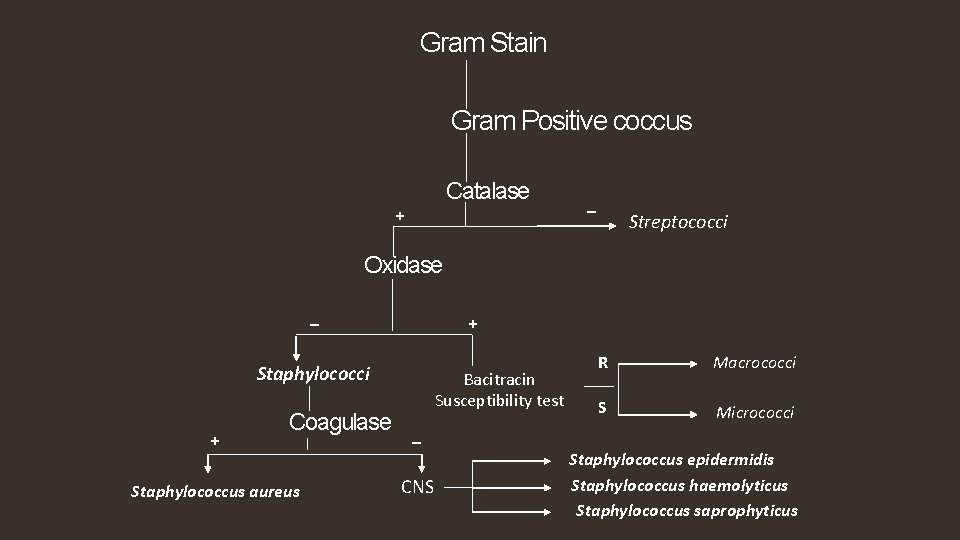
Gram Stain Gram Positive coccus Catalase + _ Streptococci Oxidase _ + Staphylococci + Coagulase Staphylococcus aureus Bacitracin Susceptibility test R Macrococci S Micrococci _ CNS Staphylococcus epidermidis Staphylococcus haemolyticus Staphylococcus saprophyticus
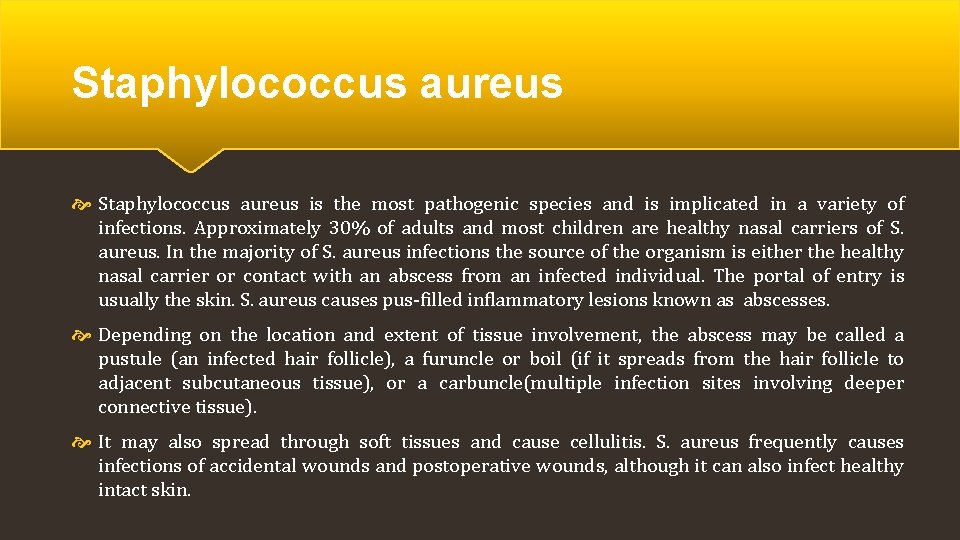
Staphylococcus aureus is the most pathogenic species and is implicated in a variety of infections. Approximately 30% of adults and most children are healthy nasal carriers of S. aureus. In the majority of S. aureus infections the source of the organism is either the healthy nasal carrier or contact with an abscess from an infected individual. The portal of entry is usually the skin. S. aureus causes pus-filled inflammatory lesions known as abscesses. Depending on the location and extent of tissue involvement, the abscess may be called a pustule (an infected hair follicle), a furuncle or boil (if it spreads from the hair follicle to adjacent subcutaneous tissue), or a carbuncle(multiple infection sites involving deeper connective tissue). It may also spread through soft tissues and cause cellulitis. S. aureus frequently causes infections of accidental wounds and postoperative wounds, although it can also infect healthy intact skin.
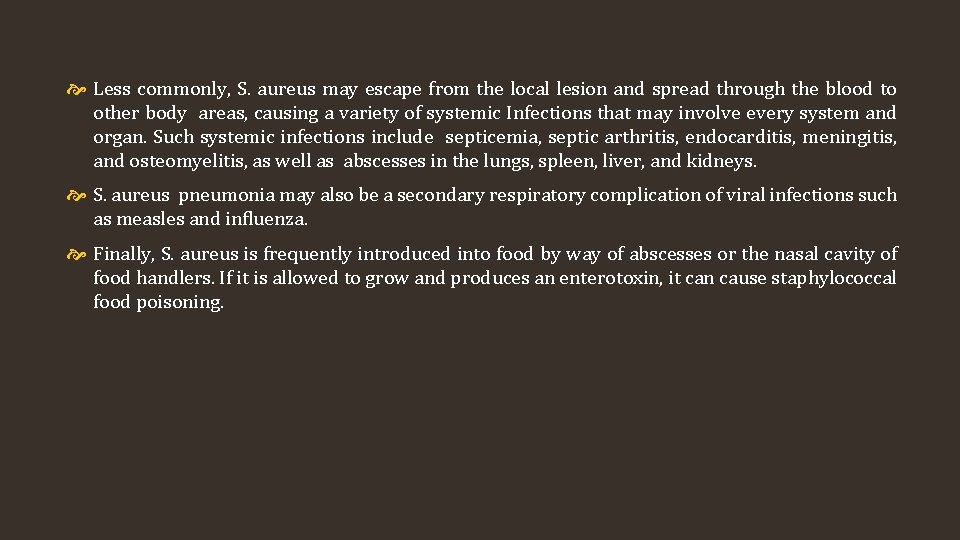
Less commonly, S. aureus may escape from the local lesion and spread through the blood to other body areas, causing a variety of systemic Infections that may involve every system and organ. Such systemic infections include septicemia, septic arthritis, endocarditis, meningitis, and osteomyelitis, as well as abscesses in the lungs, spleen, liver, and kidneys. S. aureus pneumonia may also be a secondary respiratory complication of viral infections such as measles and influenza. Finally, S. aureus is frequently introduced into food by way of abscesses or the nasal cavity of food handlers. If it is allowed to grow and produces an enterotoxin, it can cause staphylococcal food poisoning.
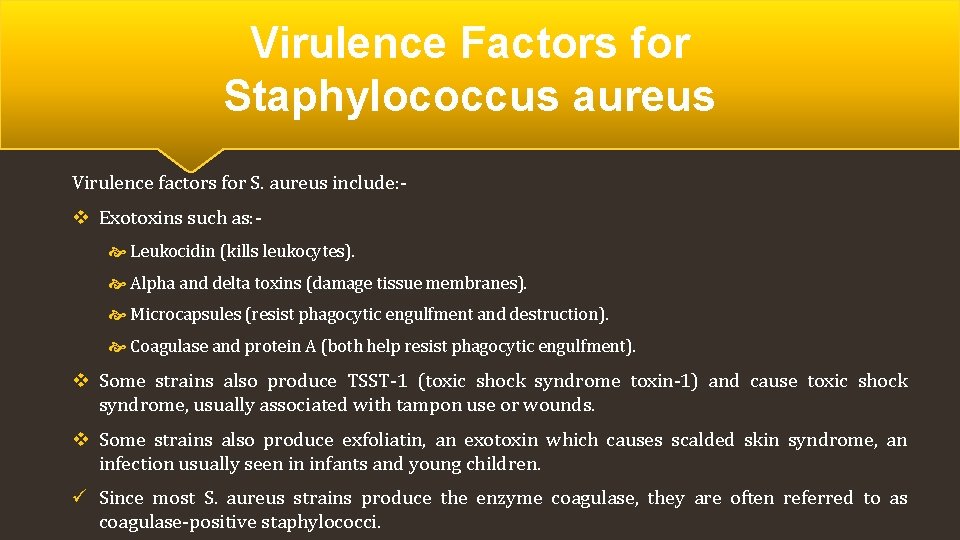
Virulence Factors for Staphylococcus aureus Virulence factors for S. aureus include: - v Exotoxins such as: Leukocidin (kills leukocytes). Alpha and delta toxins (damage tissue membranes). Microcapsules (resist phagocytic engulfment and destruction). Coagulase and protein A (both help resist phagocytic engulfment). v Some strains also produce TSST-1 (toxic shock syndrome toxin-1) and cause toxic shock syndrome, usually associated with tampon use or wounds. v Some strains also produce exfoliatin, an exotoxin which causes scalded skin syndrome, an infection usually seen in infants and young children. ü Since most S. aureus strains produce the enzyme coagulase, they are often referred to as coagulase-positive staphylococci.
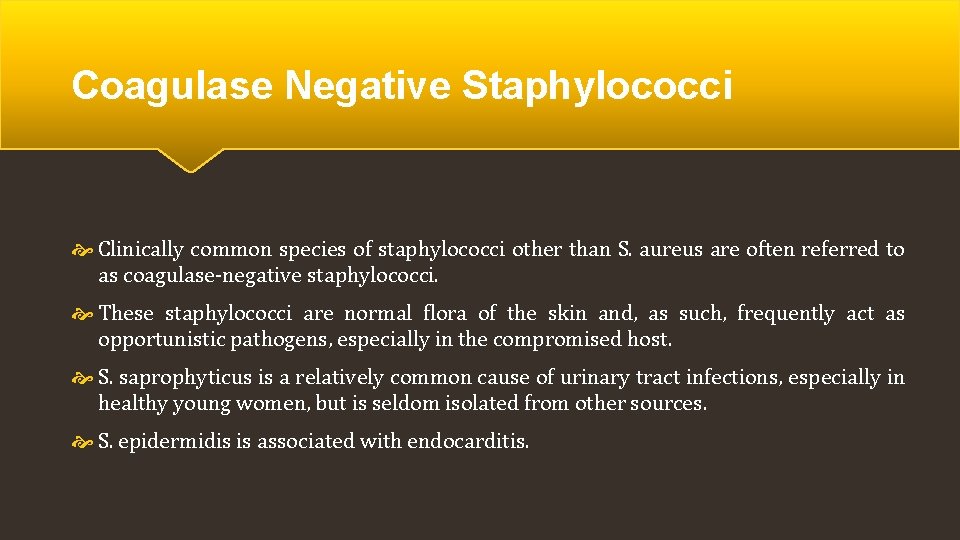
Coagulase Negative Staphylococci Clinically common species of staphylococci other than S. aureus are often referred to as coagulase-negative staphylococci. These staphylococci are normal flora of the skin and, as such, frequently act as opportunistic pathogens, especially in the compromised host. S. saprophyticus is a relatively common cause of urinary tract infections, especially in healthy young women, but is seldom isolated from other sources. S. epidermidis is associated with endocarditis.
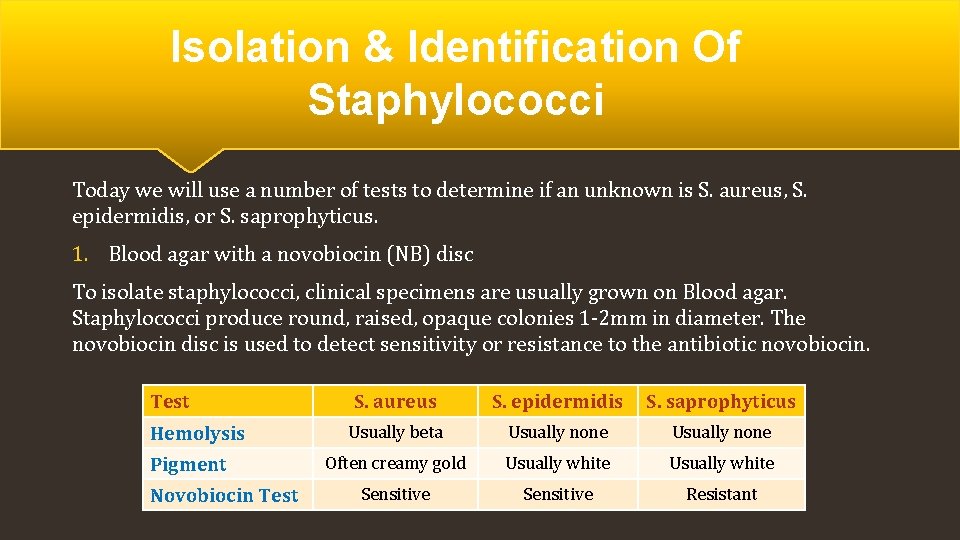
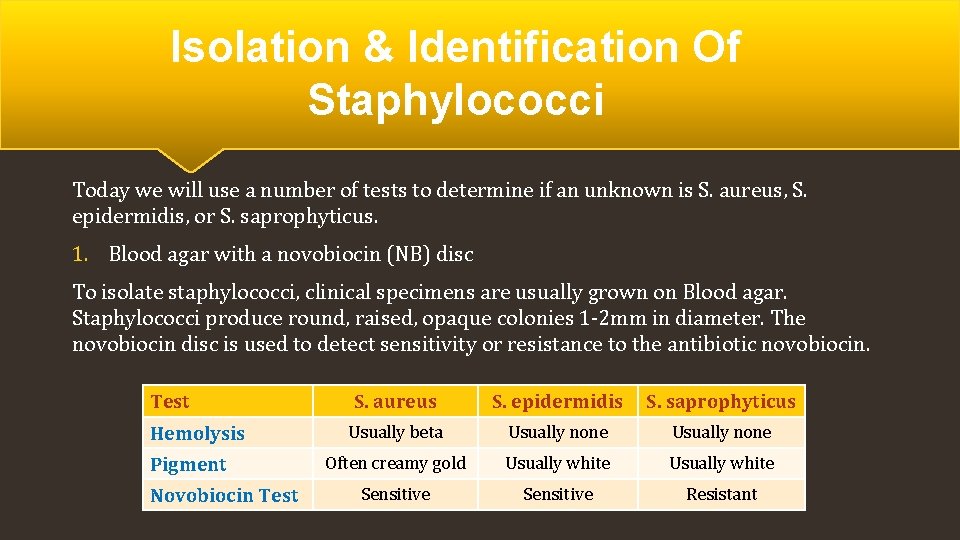
Isolation & Identification Of Staphylococci Today we will use a number of tests to determine if an unknown is S. aureus, S. epidermidis, or S. saprophyticus. 1. Blood agar with a novobiocin (NB) disc To isolate staphylococci, clinical specimens are usually grown on Blood agar. Staphylococci produce round, raised, opaque colonies 1 -2 mm in diameter. The novobiocin disc is used to detect sensitivity or resistance to the antibiotic novobiocin. Test Hemolysis Pigment Novobiocin Test S. aureus S. epidermidis S. saprophyticus Usually beta Usually none Often creamy gold Usually white Sensitive Resistant

Non-hemolytic Staphylococcus species: Staphylococcus epidermidis
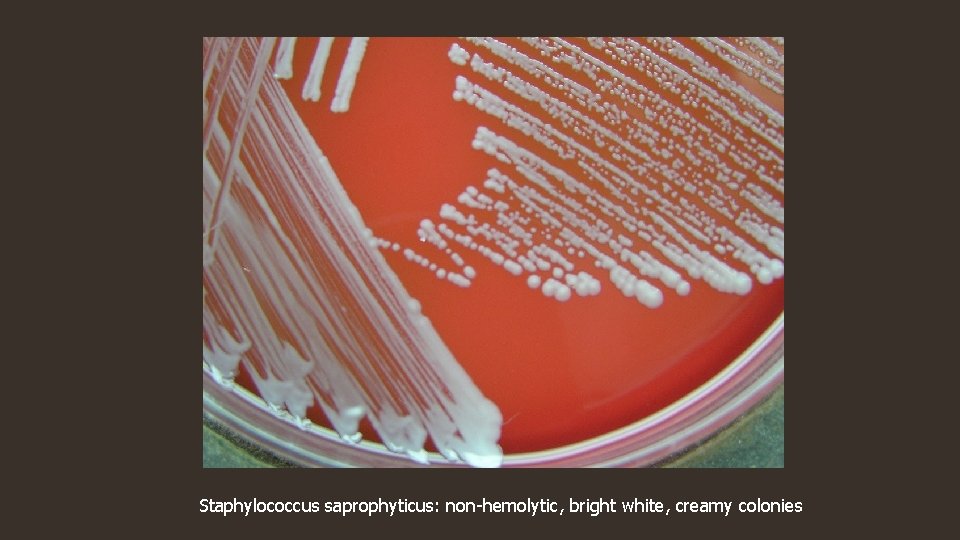
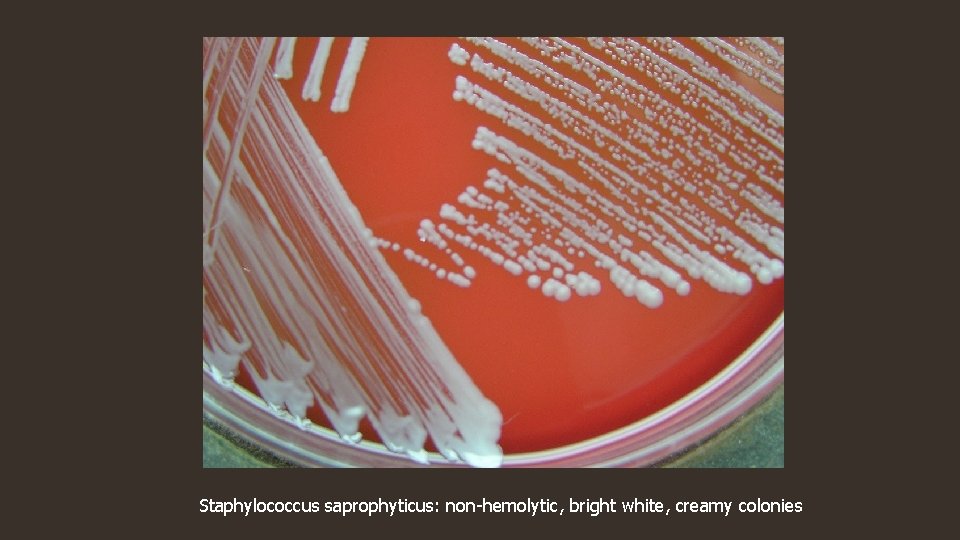
Staphylococcus saprophyticus: non-hemolytic, bright white, creamy colonies

Strains of Staphylococcus aureus produce a golden yellow pigment
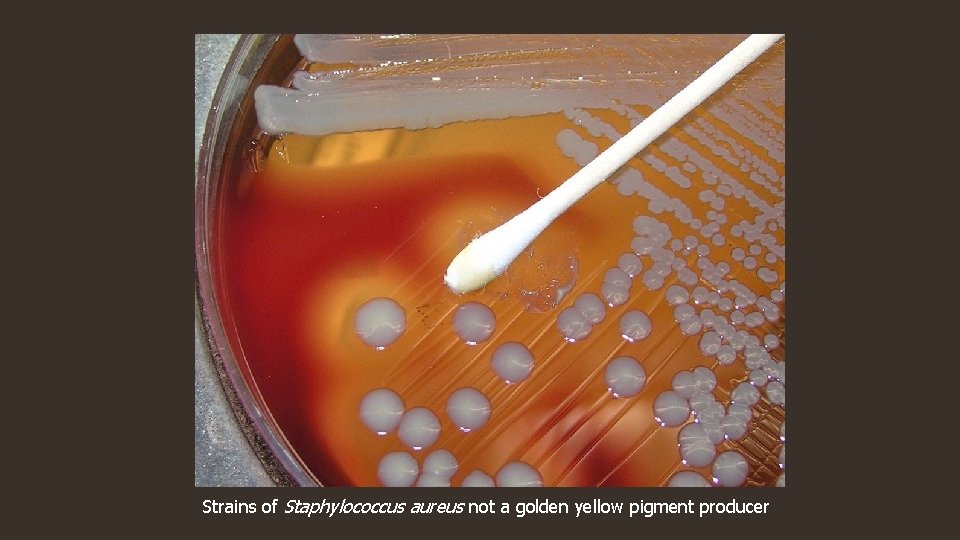
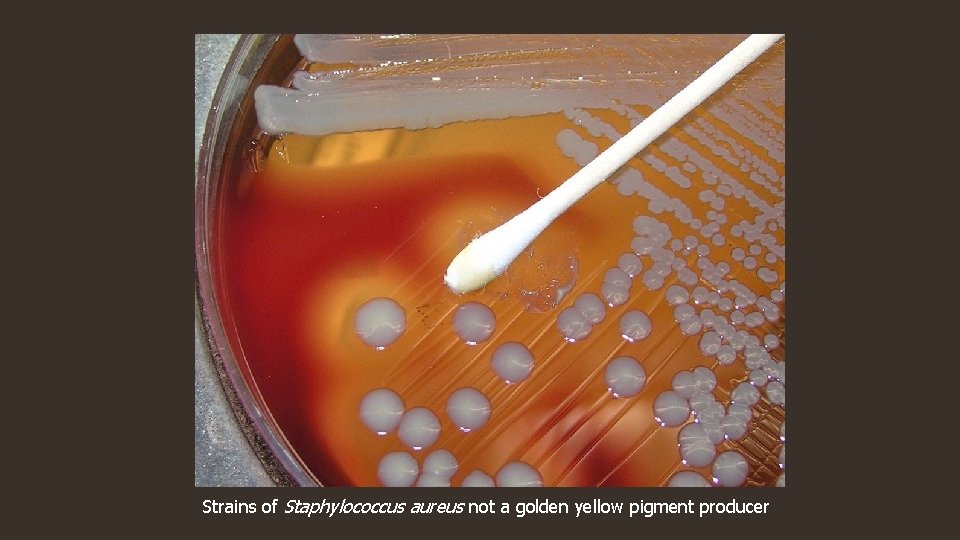
Strains of Staphylococcus aureus not a golden yellow pigment producer

Staphylococcus haemolyticus on Blood Agar
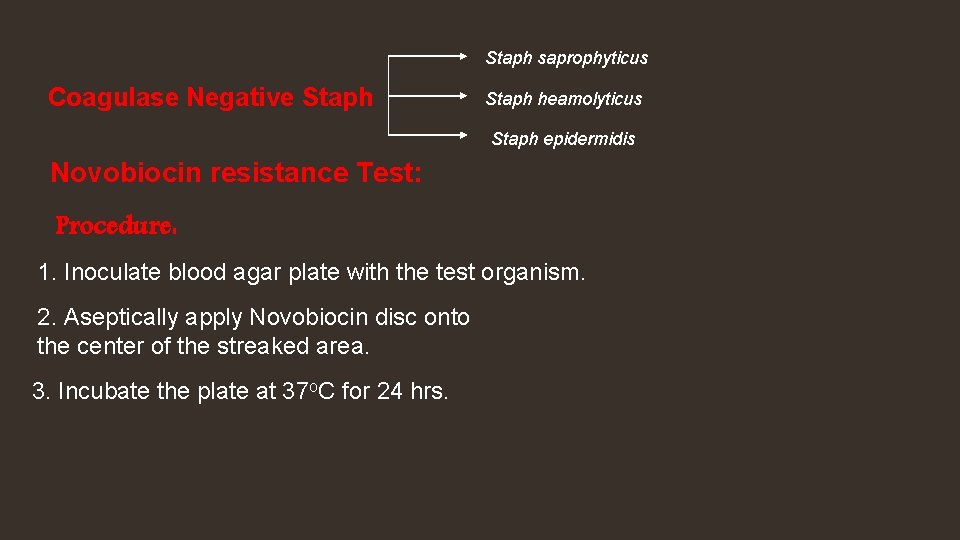
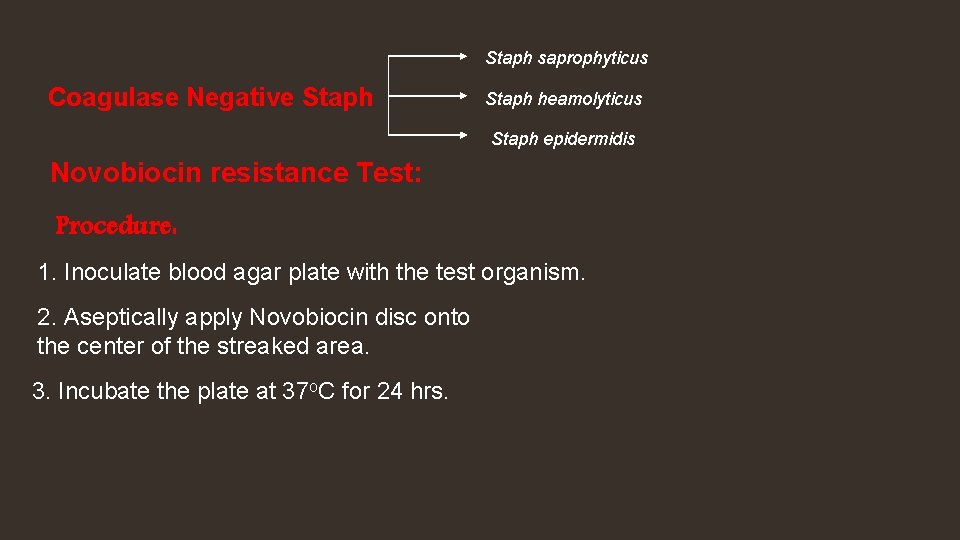
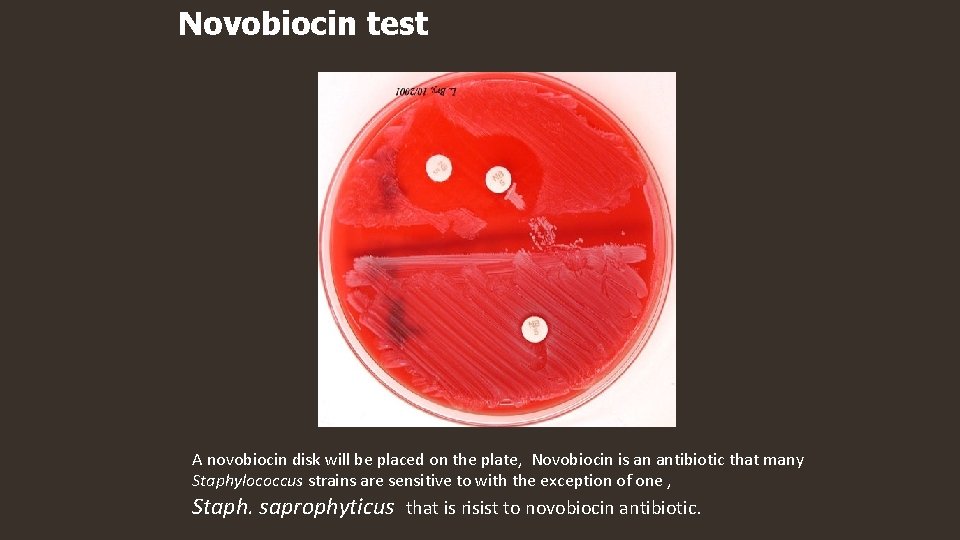
Staph saprophyticus Coagulase Negative Staph heamolyticus Staph epidermidis Novobiocin resistance Test: Procedure: 1. Inoculate blood agar plate with the test organism. 2. Aseptically apply Novobiocin disc onto the center of the streaked area. 3. Incubate the plate at 37 o. C for 24 hrs.
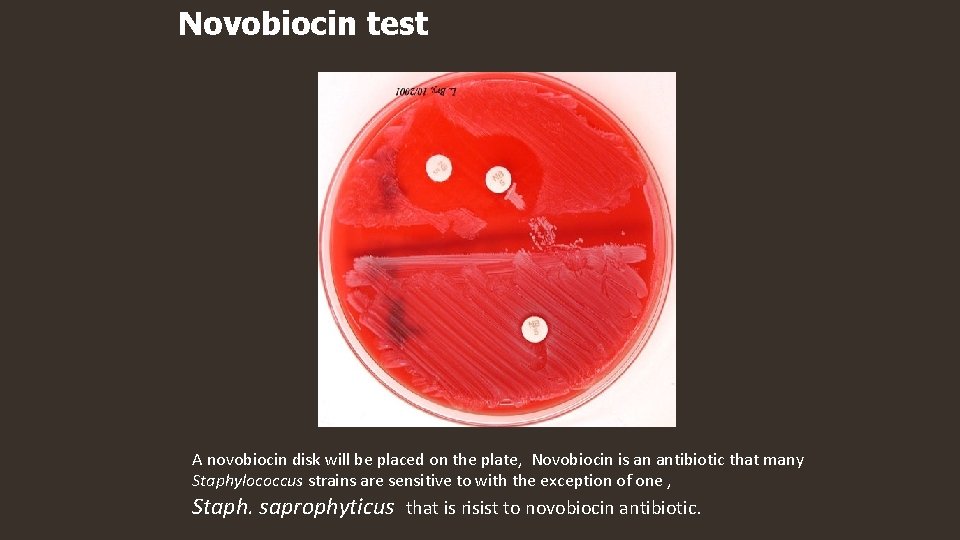
Novobiocin test A novobiocin disk will be placed on the plate, Novobiocin is an antibiotic that many Staphylococcus strains are sensitive to with the exception of one , Staph. saprophyticus that is risist to novobiocin antibiotic.
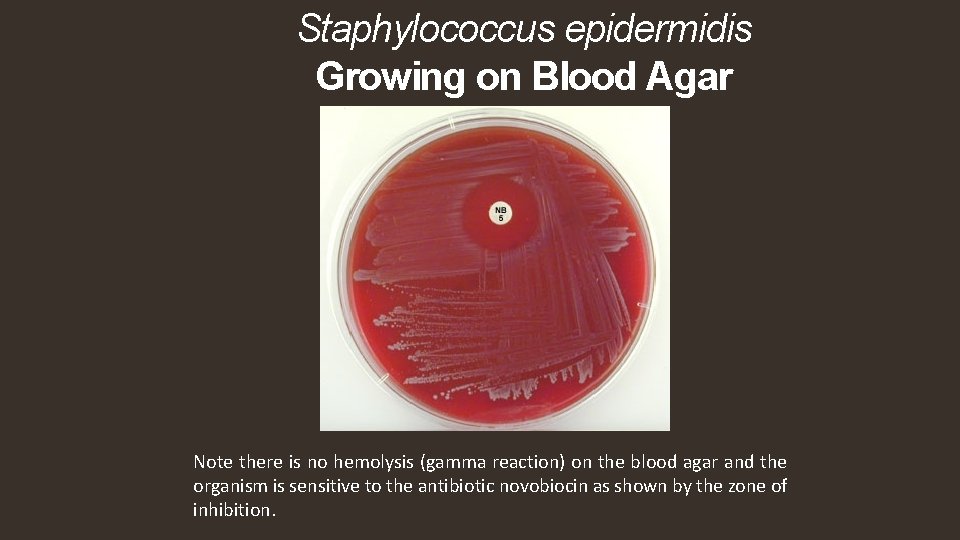
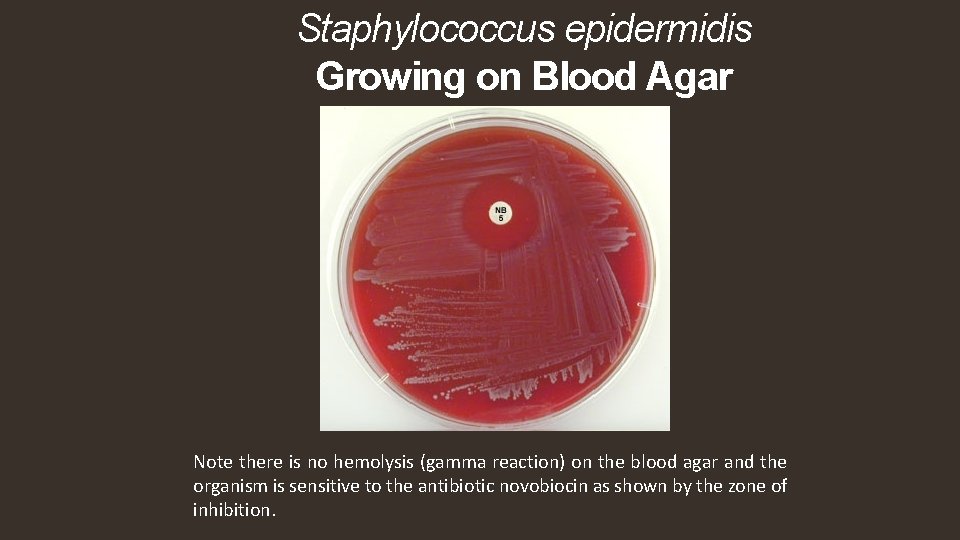
Staphylococcus epidermidis Growing on Blood Agar Note there is no hemolysis (gamma reaction) on the blood agar and the organism is sensitive to the antibiotic novobiocin as shown by the zone of inhibition.
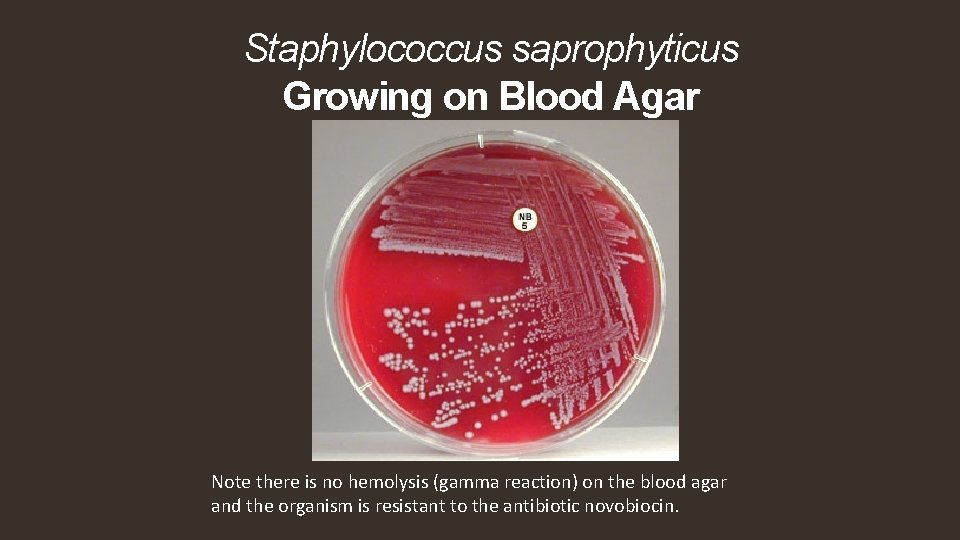
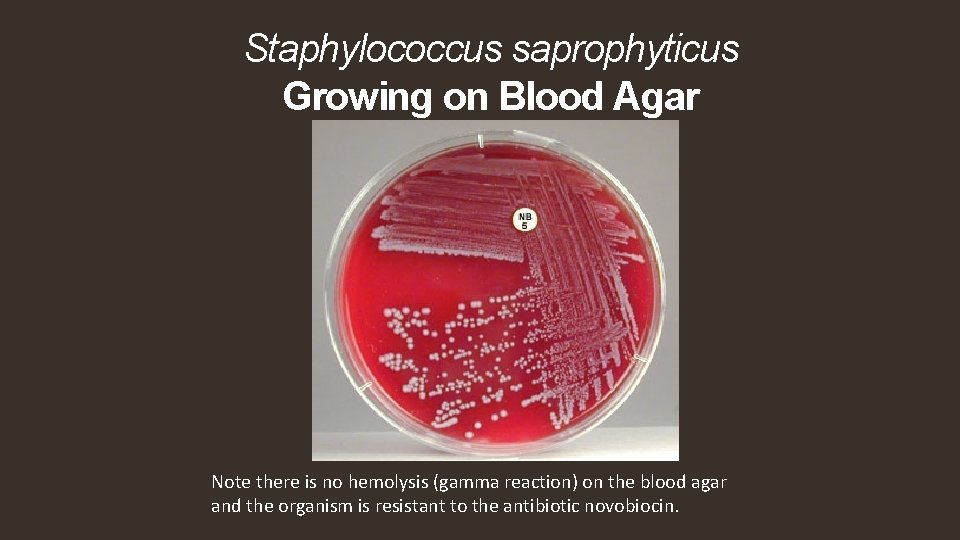
Staphylococcus saprophyticus Growing on Blood Agar Note there is no hemolysis (gamma reaction) on the blood agar and the organism is resistant to the antibiotic novobiocin.
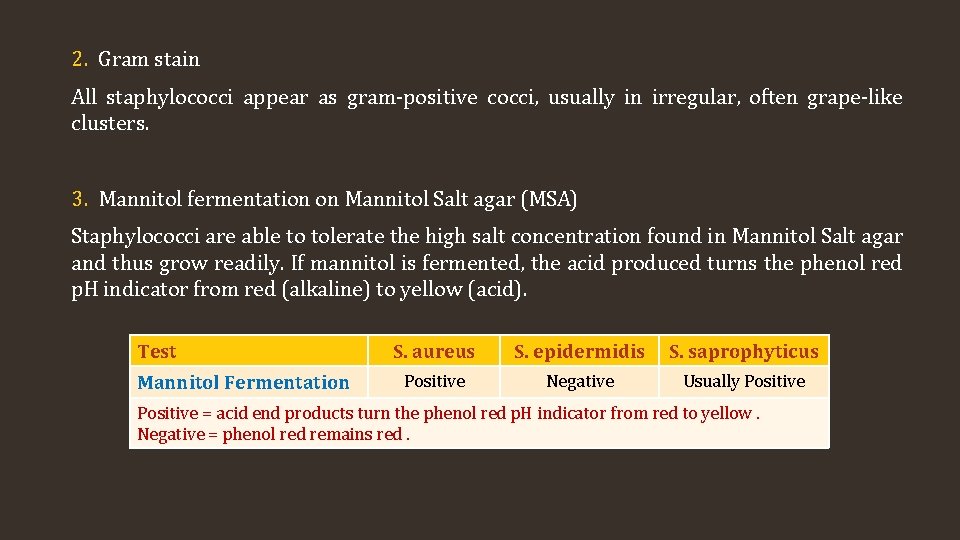
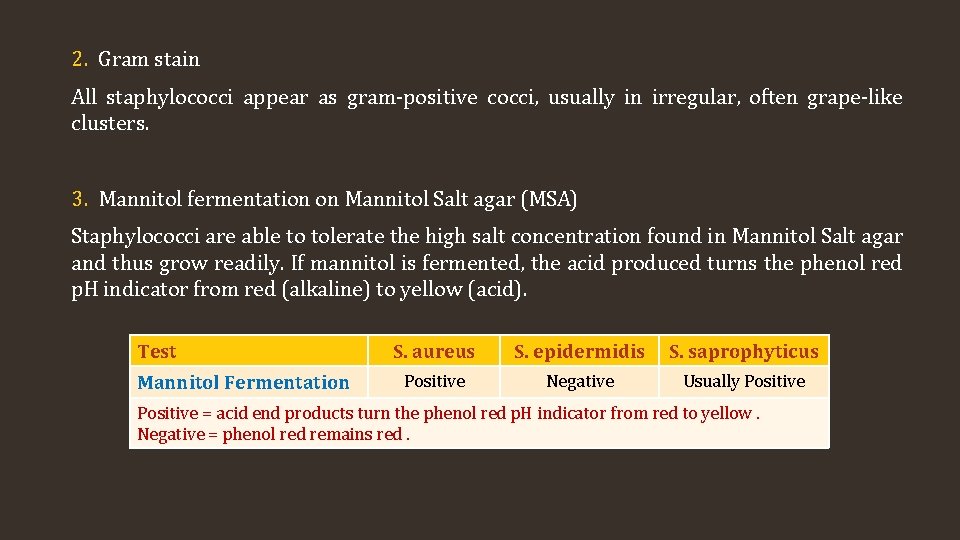
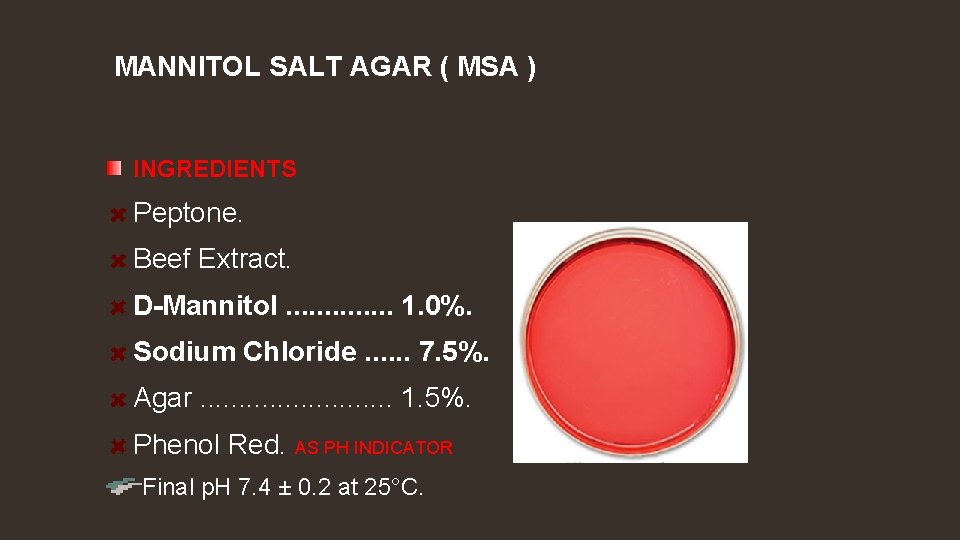
2. Gram stain All staphylococci appear as gram-positive cocci, usually in irregular, often grape-like clusters. 3. Mannitol fermentation on Mannitol Salt agar (MSA) Staphylococci are able to tolerate the high salt concentration found in Mannitol Salt agar and thus grow readily. If mannitol is fermented, the acid produced turns the phenol red p. H indicator from red (alkaline) to yellow (acid). Test Mannitol Fermentation S. aureus S. epidermidis S. saprophyticus Positive Negative Usually Positive = acid end products turn the phenol red p. H indicator from red to yellow. Negative = phenol red remains red.
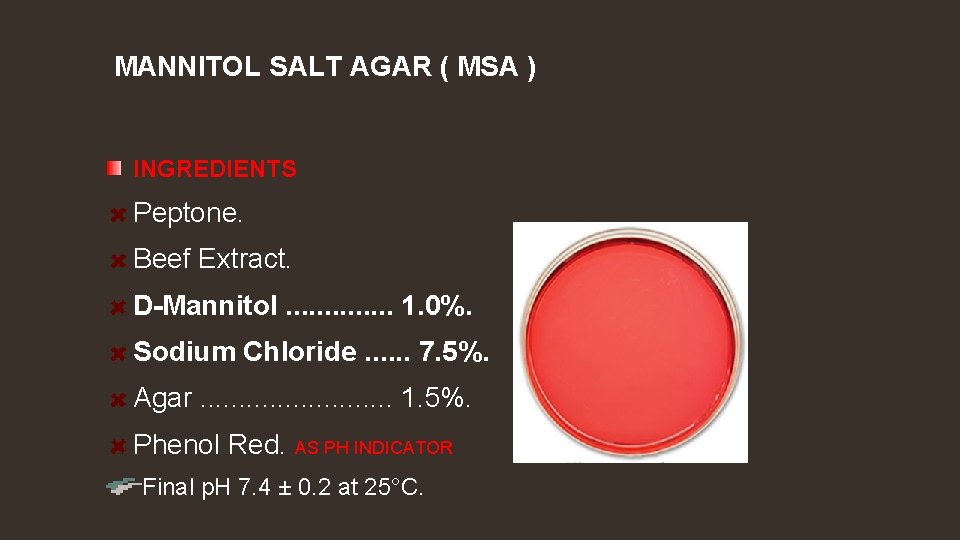
MANNITOL SALT AGAR ( MSA ) INGREDIENTS Peptone. Beef Extract. D-Mannitol. . . 1. 0%. Sodium Chloride. . . 7. 5%. Agar. . . 1. 5%. Phenol Red. AS PH INDICATOR Final p. H 7. 4 ± 0. 2 at 25°C.
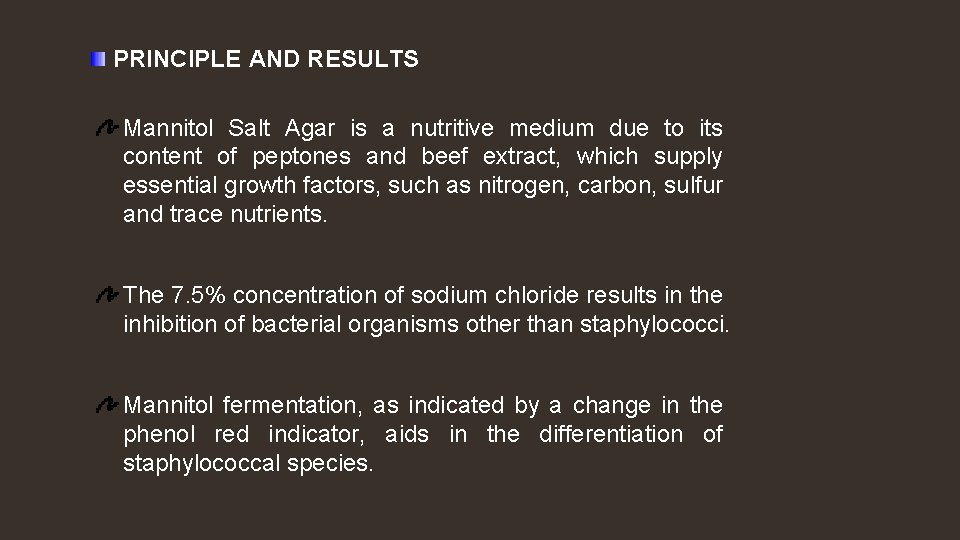
PRINCIPLE AND RESULTS Mannitol Salt Agar is a nutritive medium due to its content of peptones and beef extract, which supply essential growth factors, such as nitrogen, carbon, sulfur and trace nutrients. The 7. 5% concentration of sodium chloride results in the inhibition of bacterial organisms other than staphylococci. Mannitol fermentation, as indicated by a change in the phenol red indicator, aids in the differentiation of staphylococcal species.

Mannitol Salt agar
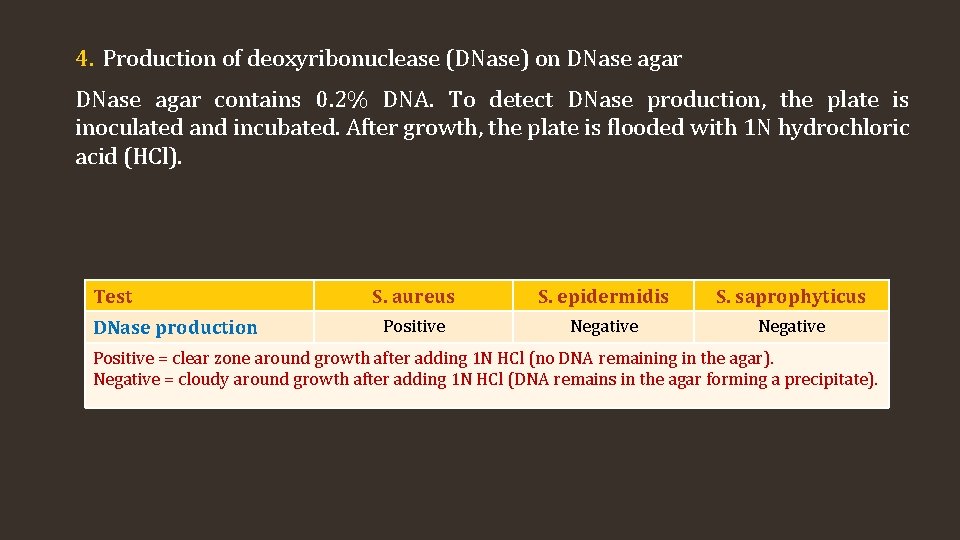
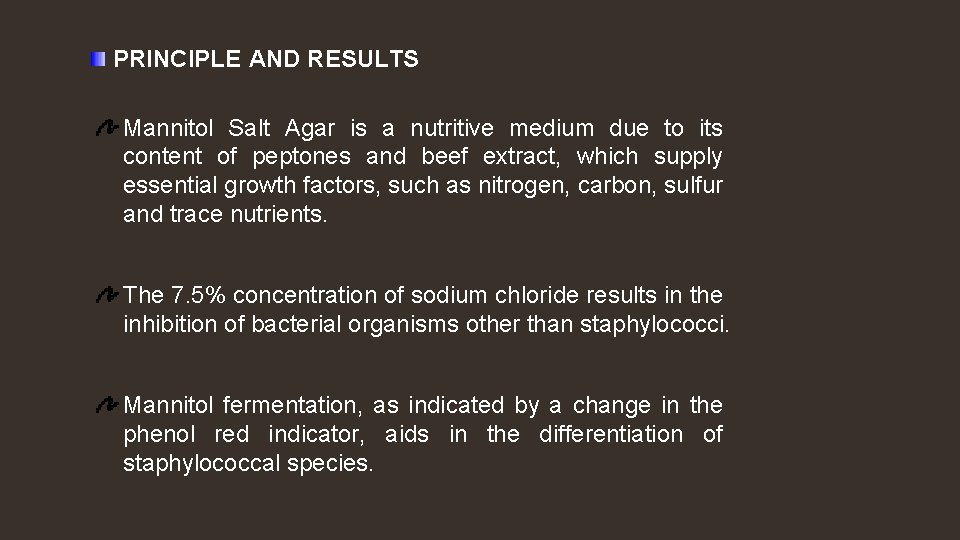
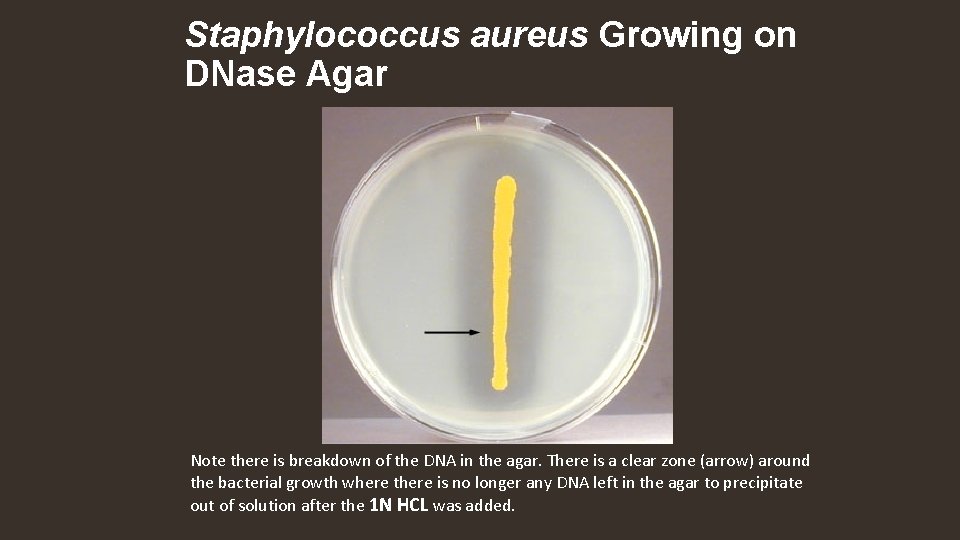
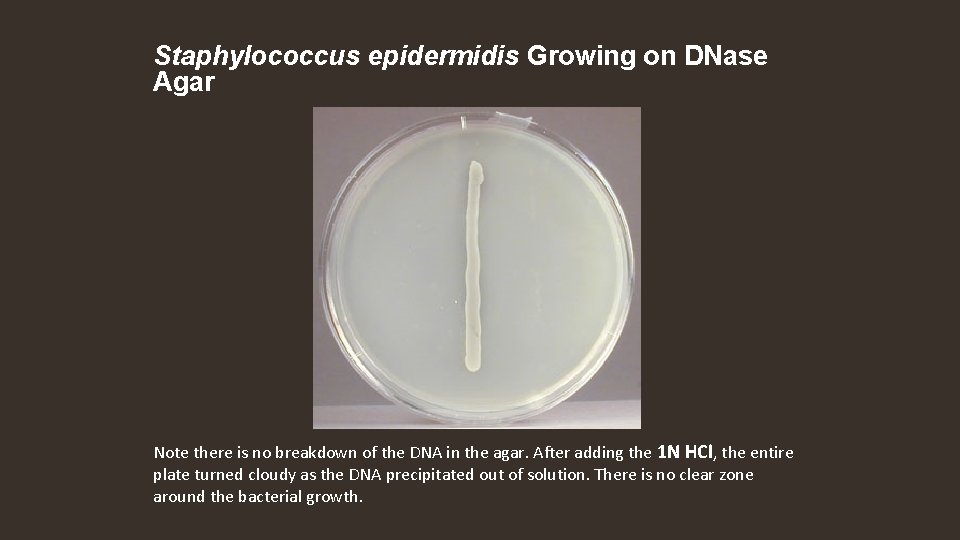
4. Production of deoxyribonuclease (DNase) on DNase agar contains 0. 2% DNA. To detect DNase production, the plate is inoculated and incubated. After growth, the plate is flooded with 1 N hydrochloric acid (HCl). Test DNase production S. aureus S. epidermidis S. saprophyticus Positive Negative Positive = clear zone around growth after adding 1 N HCl (no DNA remaining in the agar). Negative = cloudy around growth after adding 1 N HCl (DNA remains in the agar forming a precipitate).
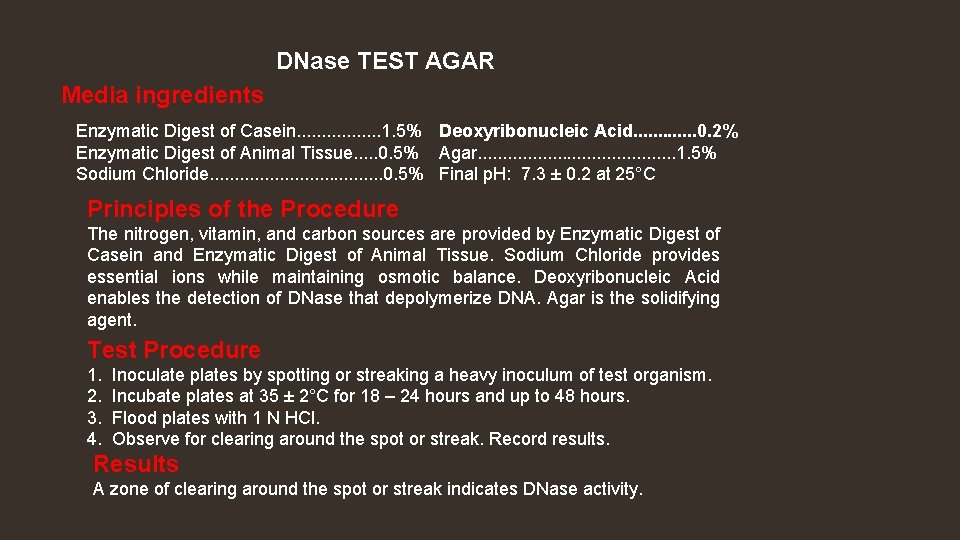
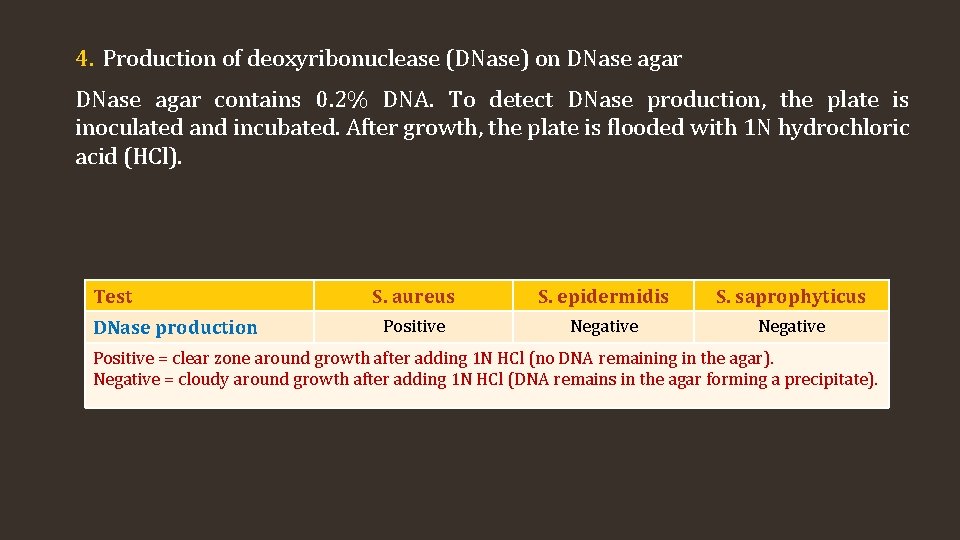
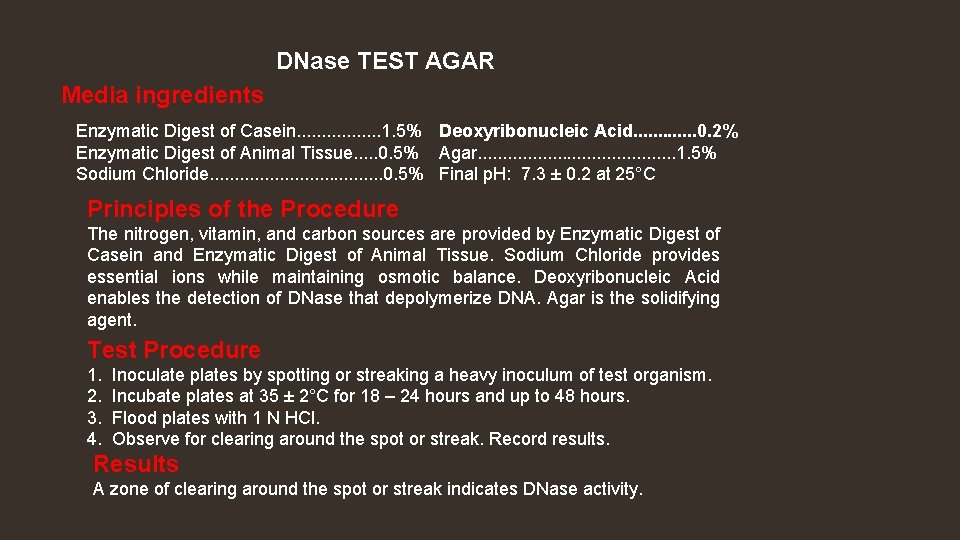
DNase TEST AGAR Media ingredients Enzymatic Digest of Casein. . . . 1. 5% Deoxyribonucleic Acid. . . 0. 2% Enzymatic Digest of Animal Tissue. . . 0. 5% Agar. . . . . 1. 5% Sodium Chloride. . . . . 0. 5% Final p. H: 7. 3 ± 0. 2 at 25°C Principles of the Procedure The nitrogen, vitamin, and carbon sources are provided by Enzymatic Digest of Casein and Enzymatic Digest of Animal Tissue. Sodium Chloride provides essential ions while maintaining osmotic balance. Deoxyribonucleic Acid enables the detection of DNase that depolymerize DNA. Agar is the solidifying agent. Test Procedure 1. 2. 3. 4. Inoculate plates by spotting or streaking a heavy inoculum of test organism. Incubate plates at 35 ± 2°C for 18 – 24 hours and up to 48 hours. Flood plates with 1 N HCl. Observe for clearing around the spot or streak. Record results. Results A zone of clearing around the spot or streak indicates DNase activity.
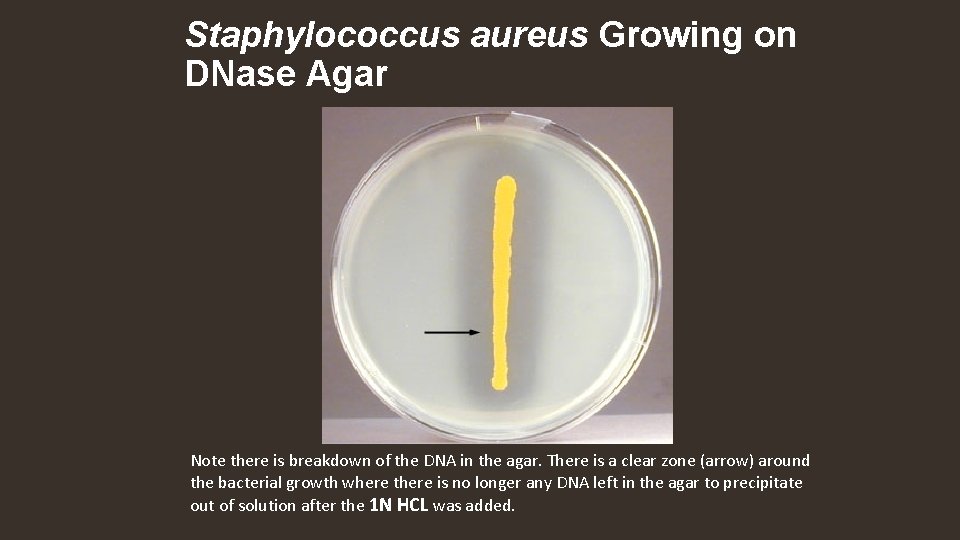
Staphylococcus aureus Growing on DNase Agar Note there is breakdown of the DNA in the agar. There is a clear zone (arrow) around the bacterial growth where there is no longer any DNA left in the agar to precipitate out of solution after the 1 N HCL was added.
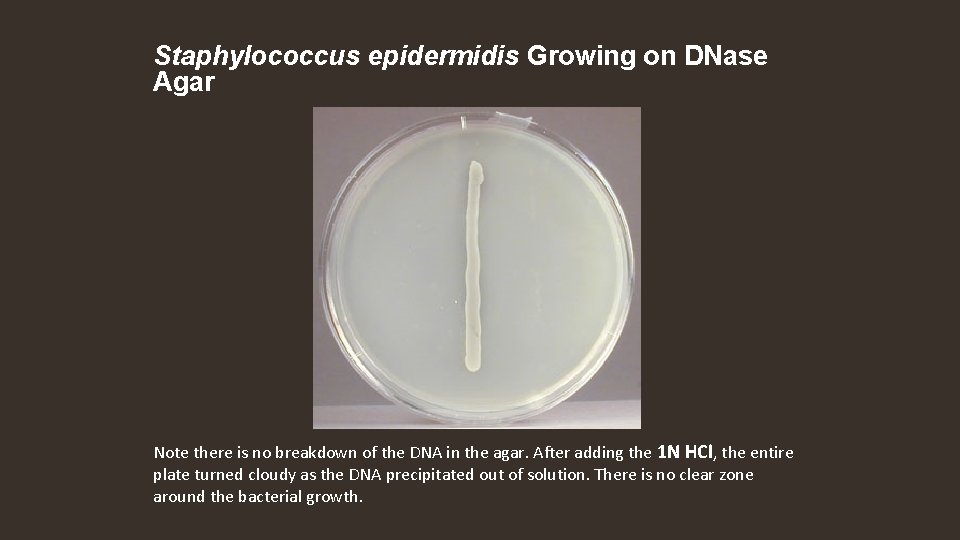
Staphylococcus epidermidis Growing on DNase Agar Note there is no breakdown of the DNA in the agar. After adding the 1 N HCl, the entire plate turned cloudy as the DNA precipitated out of solution. There is no clear zone around the bacterial growth.
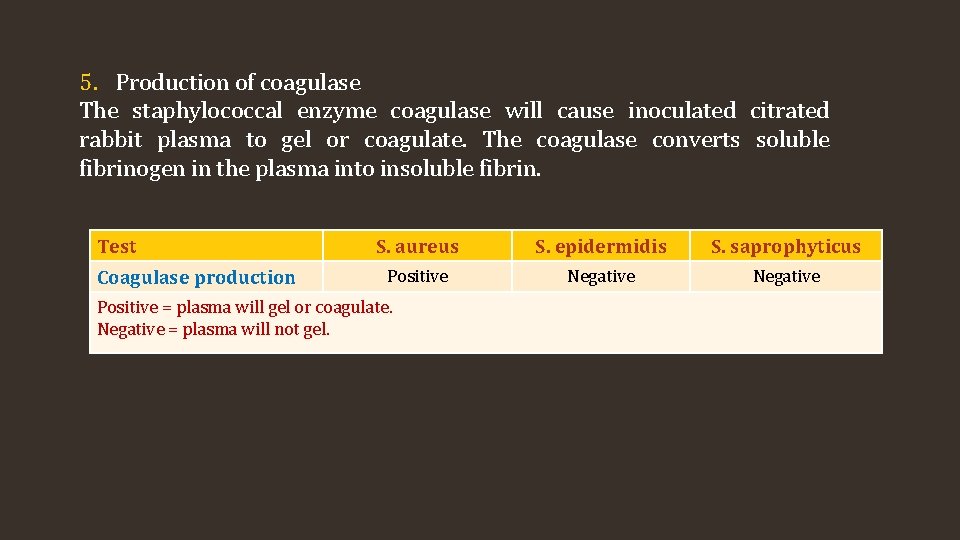
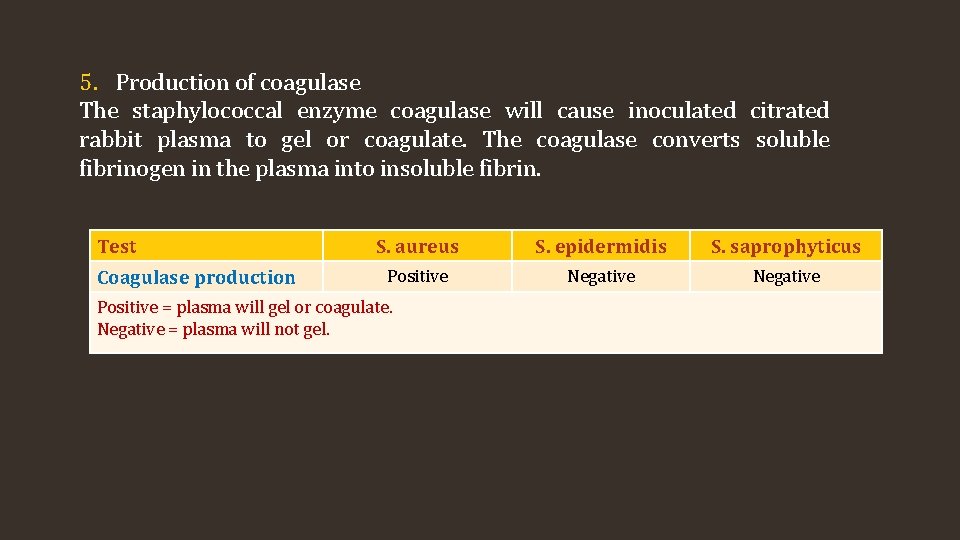
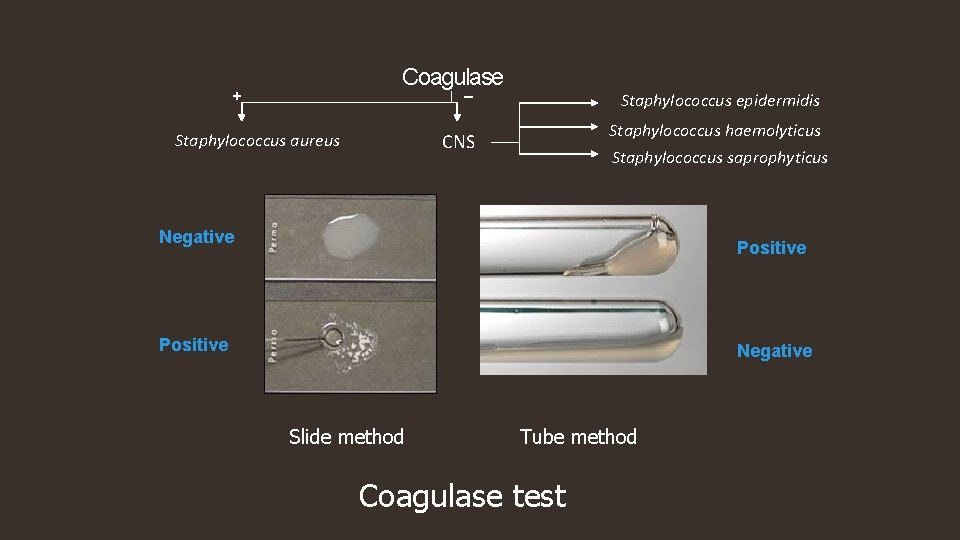
5. Production of coagulase The staphylococcal enzyme coagulase will cause inoculated citrated rabbit plasma to gel or coagulate. The coagulase converts soluble fibrinogen in the plasma into insoluble fibrin. Test Coagulase production S. aureus S. epidermidis S. saprophyticus Positive Negative Positive = plasma will gel or coagulate. Negative = plasma will not gel.
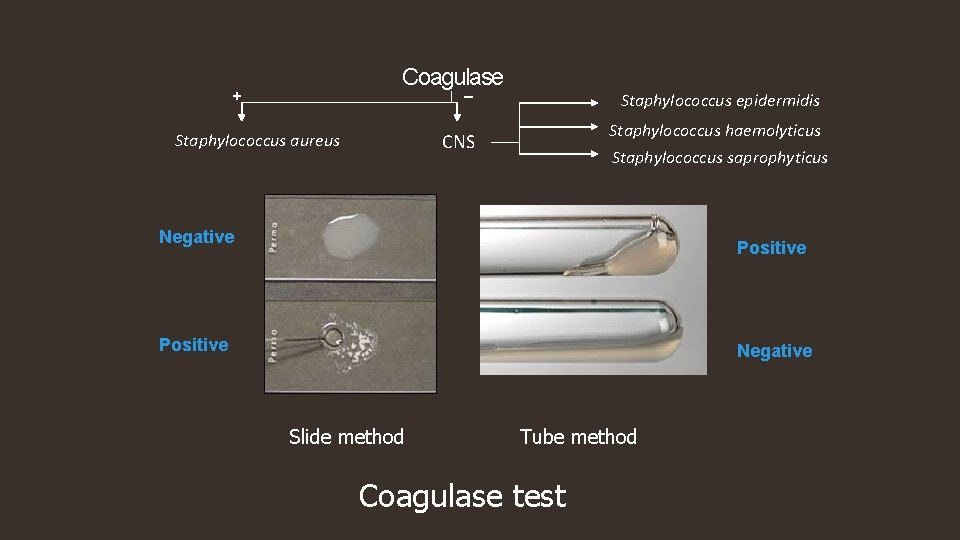
Coagulase _ + Staphylococcus epidermidis Staphylococcus haemolyticus CNS Staphylococcus aureus Staphylococcus saprophyticus Negative Positive Negative Slide method Tube method Coagulase test
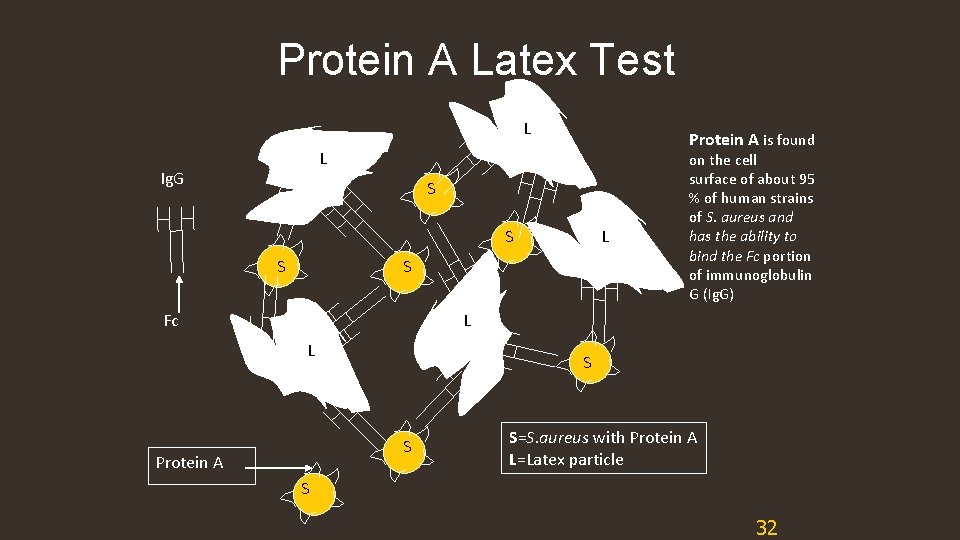
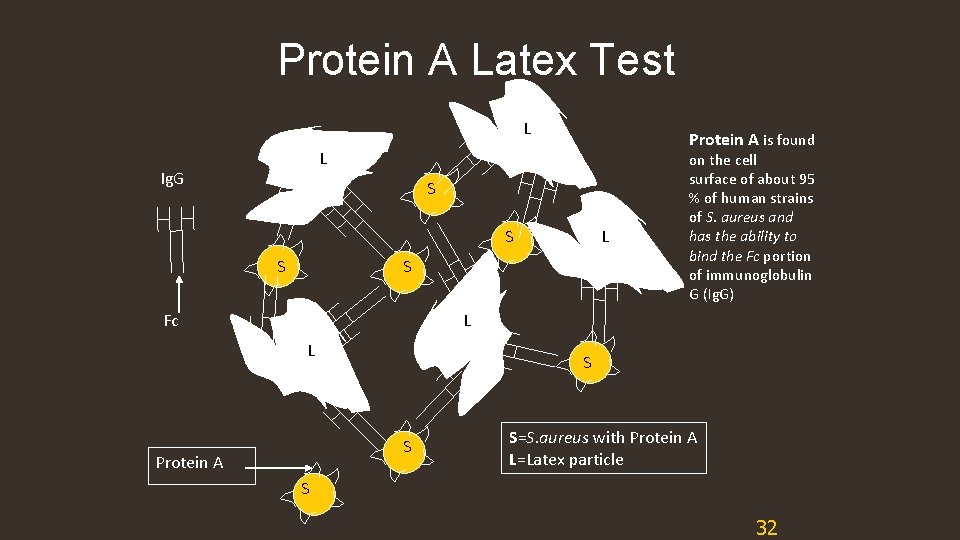
Protein A Latex Test L Protein A is found L Ig. G S S S L S Fc on the cell surface of about 95 % of human strains of S. aureus and has the ability to bind the Fc portion of immunoglobulin G (Ig. G) L L S S Protein A S=S. aureus with Protein A L=Latex particle S 32
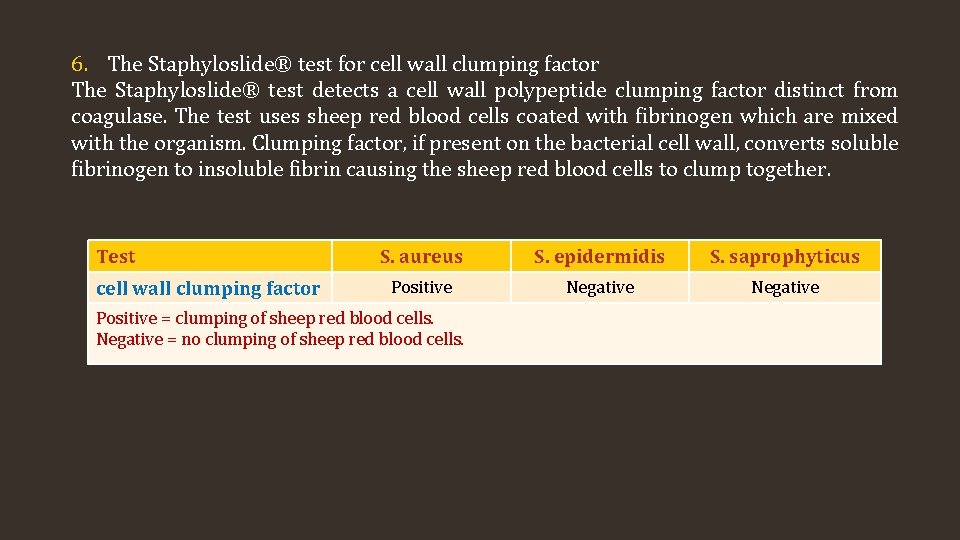
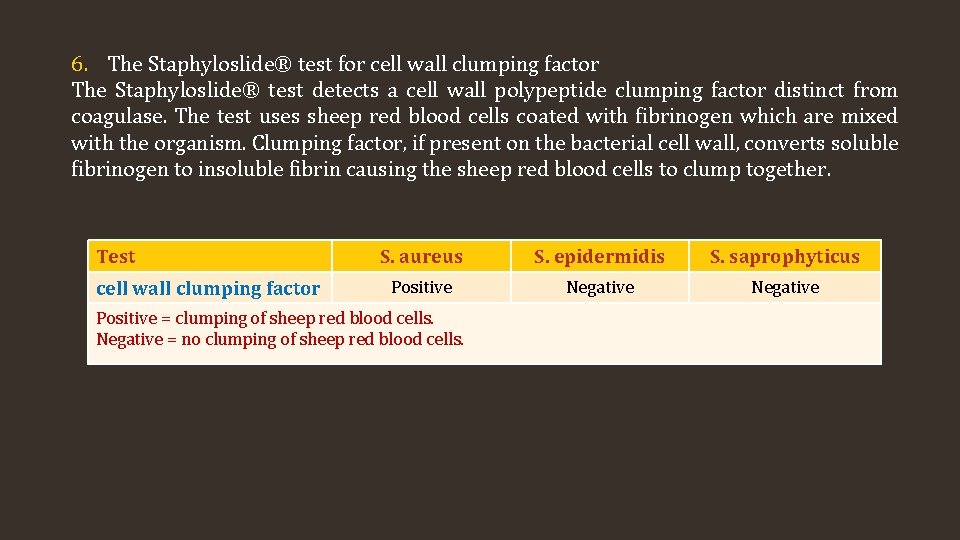
6. The Staphyloslide® test for cell wall clumping factor The Staphyloslide® test detects a cell wall polypeptide clumping factor distinct from coagulase. The test uses sheep red blood cells coated with fibrinogen which are mixed with the organism. Clumping factor, if present on the bacterial cell wall, converts soluble fibrinogen to insoluble fibrin causing the sheep red blood cells to clump together. Test cell wall clumping factor S. aureus S. epidermidis S. saprophyticus Positive Negative Positive = clumping of sheep red blood cells. Negative = no clumping of sheep red blood cells.
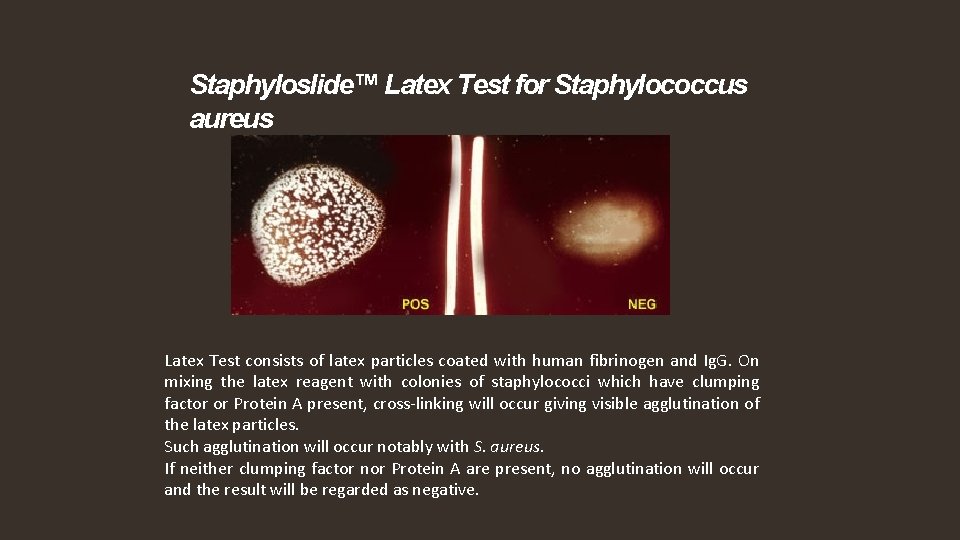
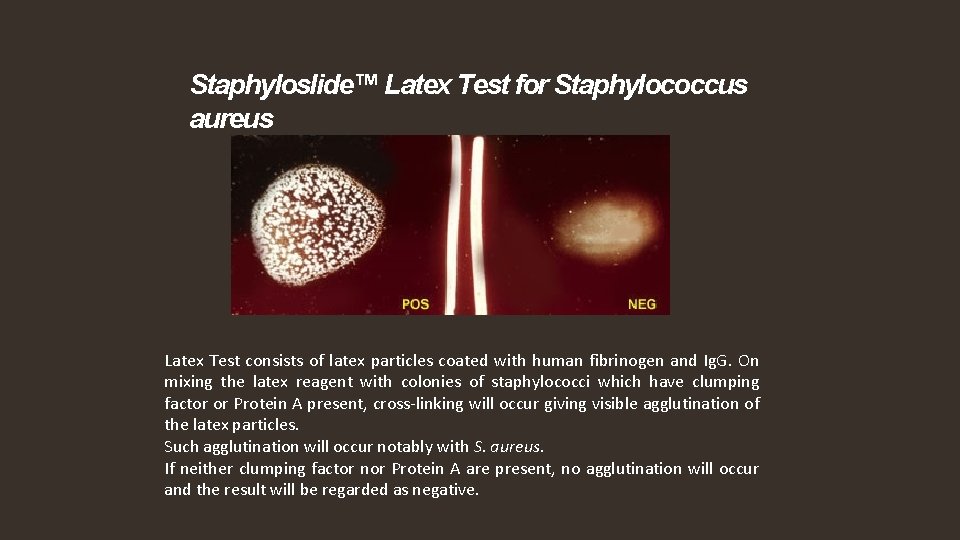
Staphyloslide™ Latex Test for Staphylococcus aureus Latex Test consists of latex particles coated with human fibrinogen and Ig. G. On mixing the latex reagent with colonies of staphylococci which have clumping factor or Protein A present, cross-linking will occur giving visible agglutination of the latex particles. Such agglutination will occur notably with S. aureus. If neither clumping factor nor Protein A are present, no agglutination will occur and the result will be regarded as negative.
 Insidan region jh
Insidan region jh Catalase test
Catalase test Staphylococci
Staphylococci Positive identification example
Positive identification example Fingerprint characteristics
Fingerprint characteristics Session 0 windows
Session 0 windows Example of postzygotic barriers
Example of postzygotic barriers Speciation can only be observed over millions of years
Speciation can only be observed over millions of years Vacuum vibration isolation
Vacuum vibration isolation Maladaptation of intimacy vs isolation
Maladaptation of intimacy vs isolation Can different species reproduce
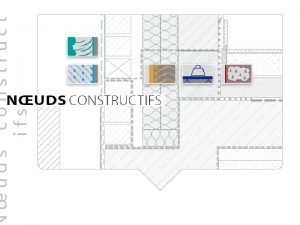
Can different species reproduce Par vapeur toiture
Par vapeur toiture Behavioral isolation
Behavioral isolation The great gatsby analysis chapter 3
The great gatsby analysis chapter 3 Fireglass browser isolation
Fireglass browser isolation Hanitat isolation
Hanitat isolation Gene pool
Gene pool Mechanical isolation in plants
Mechanical isolation in plants Isolated instrumentation amplifier
Isolated instrumentation amplifier Software fault isolation
Software fault isolation Seven forms of bias
Seven forms of bias The origin of species chapter 24
The origin of species chapter 24 Dover beach 해석
Dover beach 해석 Mechanical isolation biology
Mechanical isolation biology Connecting the concepts: macroevolution
Connecting the concepts: macroevolution Japan returns to isolation
Japan returns to isolation Chapter 19 section 3 japan returns to isolation answer key
Chapter 19 section 3 japan returns to isolation answer key Chapter 19 section 3 japan returns to isolation answer key
Chapter 19 section 3 japan returns to isolation answer key Streaking techniques in microbiology
Streaking techniques in microbiology Shallow trench isolation
Shallow trench isolation Example of industry vs inferiority
Example of industry vs inferiority Intimacy vs isolation
Intimacy vs isolation Gametic isolation example
Gametic isolation example Geographic isolation
Geographic isolation Oral sensory stage
Oral sensory stage