Isoimmunization Ch 16 2009 2010 Academic Year MSIII

- Slides: 10
Isoimmunization Ch 16 2009 -2010 Academic Year MSIII Ob/Gyn Clerkship Self-Directed Study
Case Study 24 yo G 2 P 0010 at 12 weeks ega presents for routine antenatal visit. Blood type is A negative. She had a spontaneous abortion with her first pregnancy 2 years ago. She cannot remember if she ever received Rhogam. On her initial OB labs, her antibody titer returns at 1: 128. Discuss this case, including management of Rh- women with respect to antibody titer and fetal risks.
APGO Educational Topic 19: • A. Describe the pathophysiology of isoimmunization, including: – Red blood cell antigens. – Clinical circumstances under which D isoimmunization is likely to occur. • B. Discuss the use of immunoglobulin prophylaxis during pregnancy for the prevention of isoimmunization. • C. Discuss the methods used to identify maternal isoimmunization and the severity of fetal involvement.
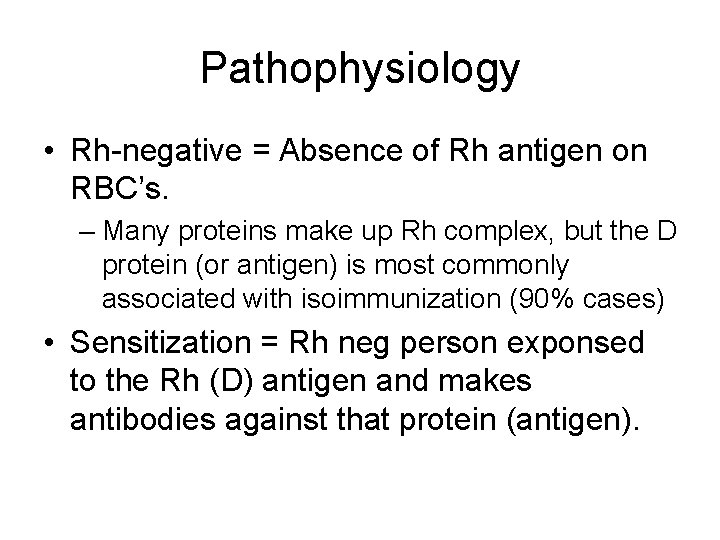
Pathophysiology • Rh-negative = Absence of Rh antigen on RBC’s. – Many proteins make up Rh complex, but the D protein (or antigen) is most commonly associated with isoimmunization (90% cases) • Sensitization = Rh neg person exponsed to the Rh (D) antigen and makes antibodies against that protein (antigen).
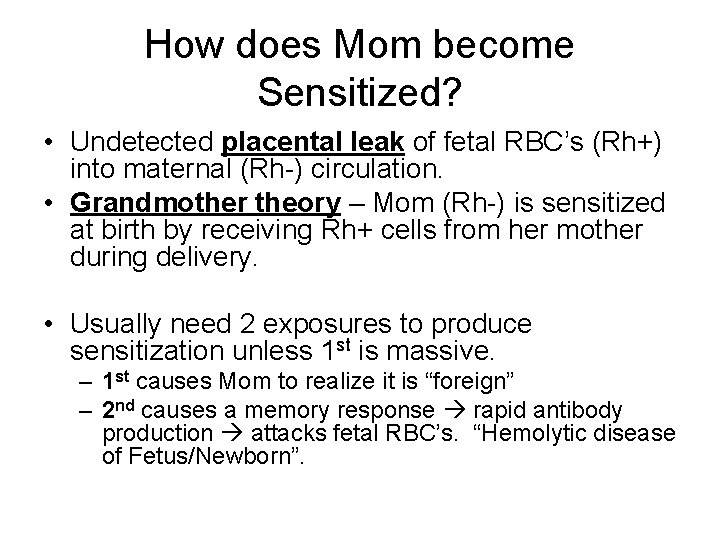
How does Mom become Sensitized? • Undetected placental leak of fetal RBC’s (Rh+) into maternal (Rh-) circulation. • Grandmother theory – Mom (Rh-) is sensitized at birth by receiving Rh+ cells from her mother during delivery. • Usually need 2 exposures to produce sensitization unless 1 st is massive. – 1 st causes Mom to realize it is “foreign” – 2 nd causes a memory response rapid antibody production attacks fetal RBC’s. “Hemolytic disease of Fetus/Newborn”.
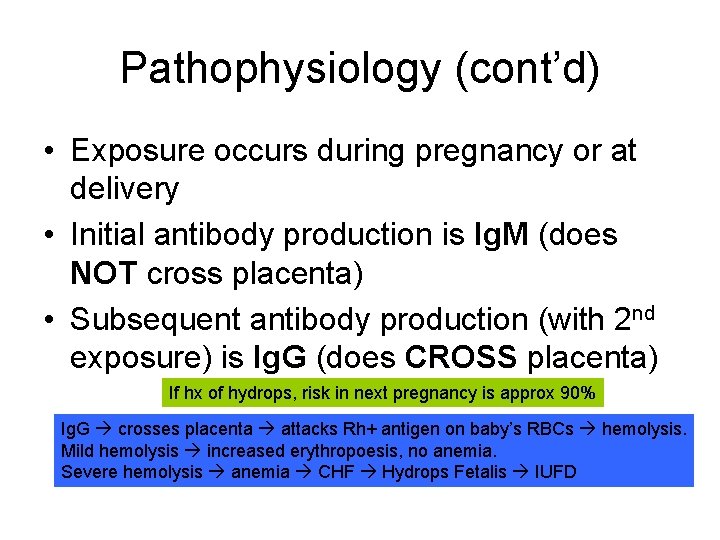
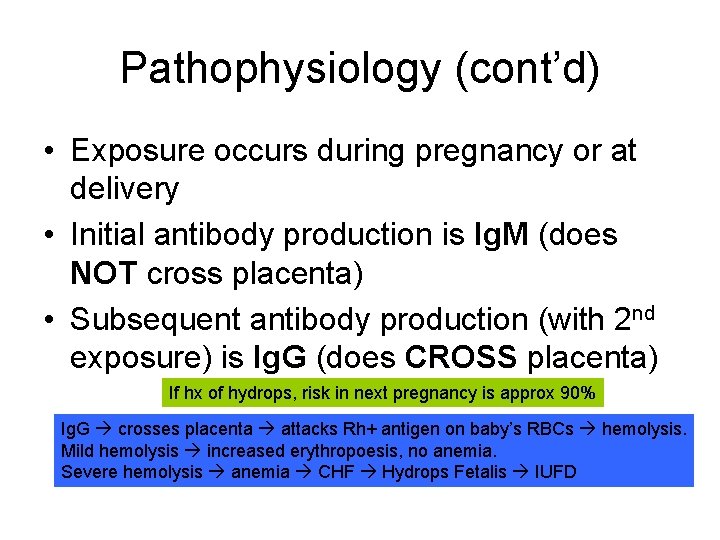
Pathophysiology (cont’d) • Exposure occurs during pregnancy or at delivery • Initial antibody production is Ig. M (does NOT cross placenta) • Subsequent antibody production (with 2 nd exposure) is Ig. G (does CROSS placenta) If hx of hydrops, risk in next pregnancy is approx 90% Ig. G crosses placenta attacks Rh+ antigen on baby’s RBCs hemolysis. Mild hemolysis increased erythropoesis, no anemia. Severe hemolysis anemia CHF Hydrops Fetalis IUFD
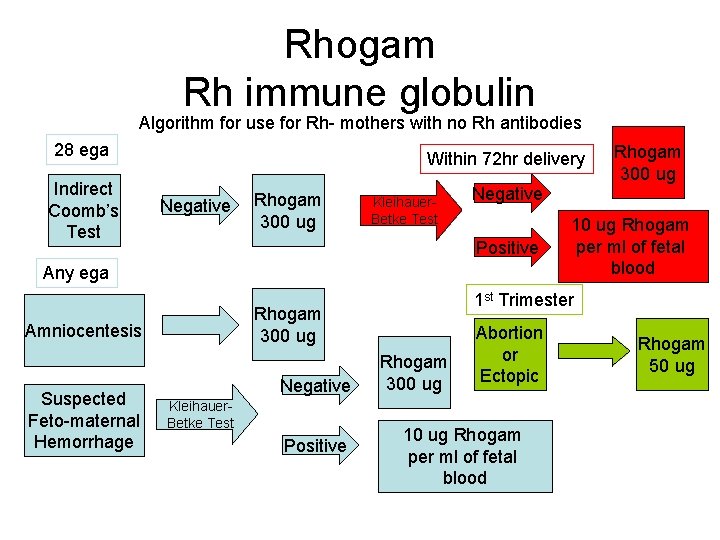
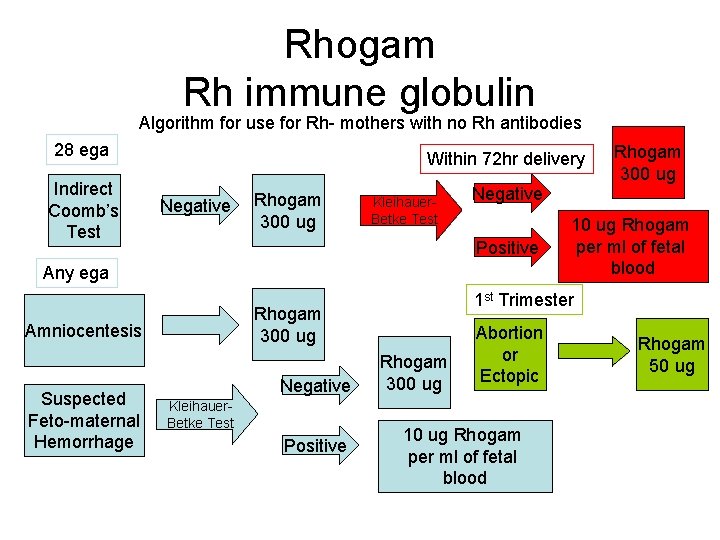
Rhogam Rh immune globulin Algorithm for use for Rh- mothers with no Rh antibodies 28 ega Indirect Coomb’s Test Within 72 hr delivery Negative Rhogam 300 ug Kleihauer. Betke Test Negative Positive Any ega Suspected Feto-maternal Hemorrhage Negative Kleihauer. Betke Test Positive 10 ug Rhogam per ml of fetal blood 1 st Trimester Rhogam 300 ug Amniocentesis Rhogam 300 ug Abortion or Ectopic 10 ug Rhogam per ml of fetal blood Rhogam 50 ug
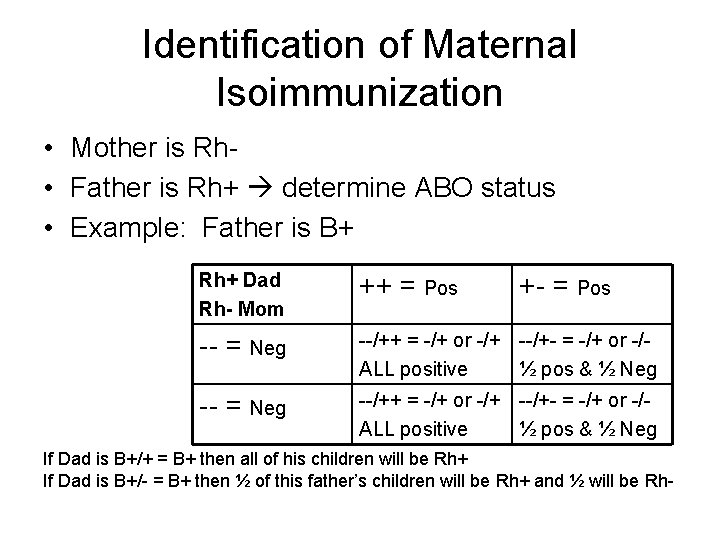
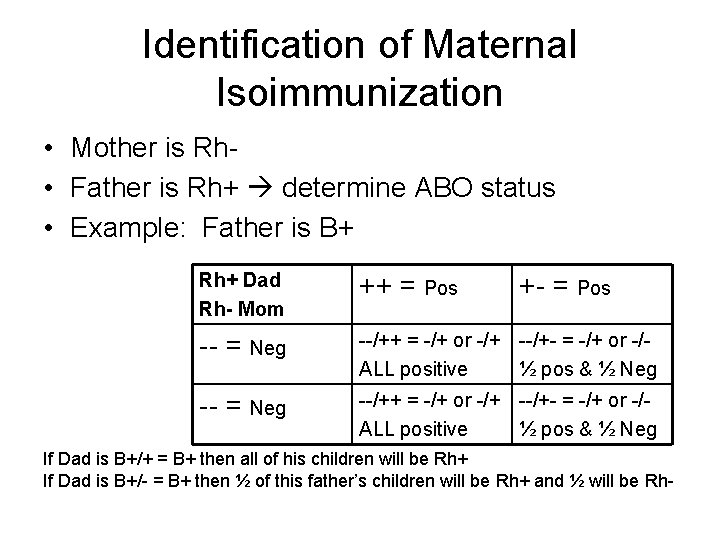
Identification of Maternal Isoimmunization • Mother is Rh • Father is Rh+ determine ABO status • Example: Father is B+ Rh+ Dad Rh- Mom ++ = Pos -- = Neg --/++ = -/+ or -/+ --/+- = -/+ or -/ALL positive ½ pos & ½ Neg +- = Pos If Dad is B+/+ = B+ then all of his children will be Rh+ If Dad is B+/- = B+ then ½ of this father’s children will be Rh+ and ½ will be Rh-
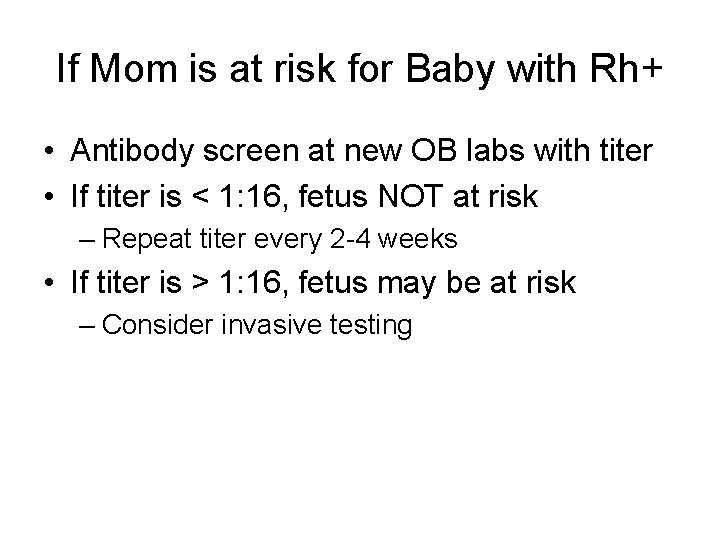
If Mom is at risk for Baby with Rh+ • Antibody screen at new OB labs with titer • If titer is < 1: 16, fetus NOT at risk – Repeat titer every 2 -4 weeks • If titer is > 1: 16, fetus may be at risk – Consider invasive testing

Testing for Fetal Disease • Amniotic Fluid Spectrophotometry – 27 weeks ega; correlates biliary pigment and fetal hct – Delta. OD 450 measurements compared on Liley chart • Ultrasound – Fetal growth; placental size and thickness; liver size; ascites; pleural effusion; pericardial effusion; skin edema – Middle Cerebral Artery (MCA) peak velocity doppler flow correlates with anemia. • Percutaneous Umbilical Blood Sampling (PUBS) – Test fetal blood for hgb, hct, blood gases, p. H, bilirubin