Ischemic Stroke Results of NAISD National Acute Ischemic


- Slides: 23
Ischemic Stroke: Results of NAISD National Acute Ischemic Stroke Database Bhojo A. Khealani Assistant Professor Neurology-Medicine Aga Khan University, Karachi, Pakistan NHSymp_NAISDB_BK Feb 2014

Team and Institutions Bhojo A Khealani Muhammad Tariq Maria Khan Safia Awan Mohammad Wasay Abdul Malik Feb 2014 NHSymp_NAISDB_BK Alam I Siddiqi
Background • Stroke is the leading cause of disability and the second leading cause of mortality in the world. » WHO. Global status report on noncommunicable diseases 2010. Geneva: World Health Organization. 2011. » Mathers CD, Fat DM, Boerma JT. The global burden of disease: 2004 update. World Health Organization; 2008. • Burden of stroke is expected to decrease in high income countries whereas it is expected to double in low and middle income countries » Feigin VL, Lawes CMM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. The Lancet Neurology. 2009; 8(4): 355 -69. Feb 2014 NHSymp_NAISDB_BK
Background • Exact Stroke burden in Pakistan is not Known • Risk factors are prevalent • Poor Preventive strategies » Khan FS et al. The burden of non-communicable disease in transition communities in an Asian megacity: baseline findings from a cohort study in Karachi, Pakistan. Plo. S one. 2013; 8(2): e 56008. » Hashmi M, Khan M, Wasay M. Growing burden of stroke in Pakistan: a review of progress and limitations. International Journal of Stroke. 2012. » Mehndiratta MM. Current Status of Trends in Ischemic and Hemorrhagic Strokes. Neuroepidemiology. 2012; 39(1): 43 -4. » Chronic diseases. NHS of Pakistan; 1990 -94. Health profile of peoples of Pakistan. 1998: 49 -69 Feb 2014 NHSymp_NAISDB_BK
Background • Community based research » Kamal AK et al. The burden of stroke and TIAs in Pakistan: a community based prevalence study. BMC Neurology 2009, 9: 58 doi: 10. 1186/1471 -2377 -9 -58 • Hospital based research – Paucity – Single center based » Bhojo A Khealani, Wasay M. Burden of stroke in Pakistan. Int J Stroke. 2008 Nov; 3(4): 293 -6. Feb 2014 NHSymp_NAISDB_BK

Objectives • To establish a multicenter ischemic stroke registry – to provide insight • • Feb 2014 Epidemiology Stroke subtypes Risk factors of ischemic strokes Acute outcome NHSymp_NAISDB_BK
Materials and Methods • Four academic centers (three urban and one rural) participated in this project. – Well established acute neurology services • Trained Neurologists • Imaging facilities • Recruitment – January 1, 2007 to December 31, 2007 • Evaluation – Clinical by trained Neurologist – Brain imaging Feb 2014 NHSymp_NAISDB_BK
Materials and Methods • Inclusion criteria – Age >14 years – Clinical Acute neurological deficit suggestive of acute ischemic stroke – Imaging: Supported by imaging • Exclusion Criteria – Refuse to give consent – ICH on brain imaging – Other cause that could explain the focal neurologic deficit Feb 2014 NHSymp_NAISDB_BK
Materials and Methods • Willing to participate – Written consent • Questionnaire – Demographics – stroke severity » NIHSS » m. RS – vascular risk factors – stroke workup » Brain and vascular imaging » Echocardiogram, electrocardiogram, holter » Other workup – stroke subtype » TOAST Feb 2014 NHSymp_NAISDB_BK
Materials and Methods • SPSS 19. 0 • continuous variables – means along with standard deviations • categorical data – frequencies and percentages are reported • For gender comparison – chi square test of independence was used for categorical variables – student’s t-test for continuous variables • Predictors of poor outcome – Binary logistic regression – P value of 0. 05 was taken as significant. Feb 2014 NHSymp_NAISDB_BK
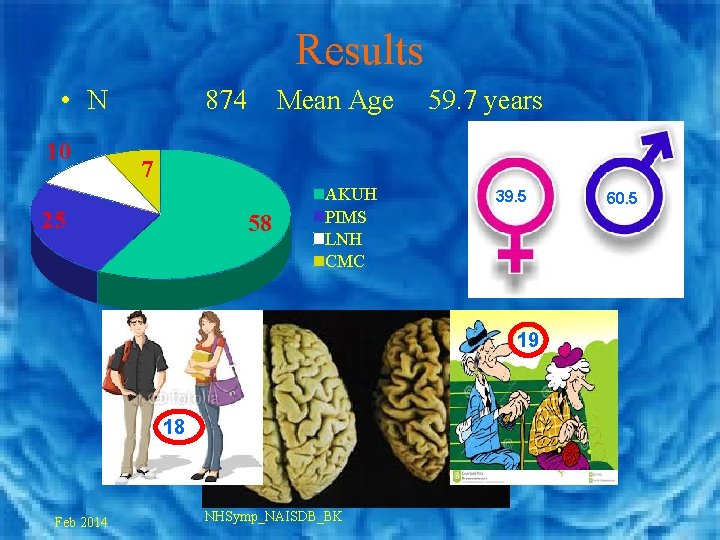
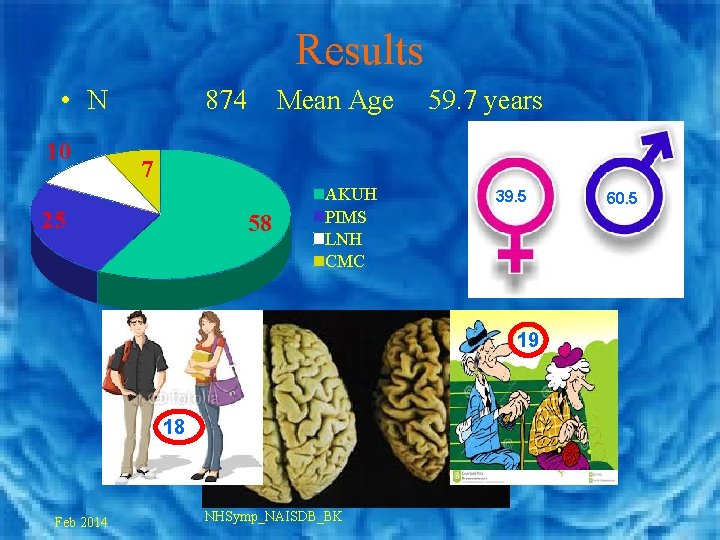
Results • N 10 874 Mean Age 59. 7 years 7 25 58 AKUH PIMS LNH CMC 39. 5 19 18 Feb 2014 NHSymp_NAISDB_BK 60. 5
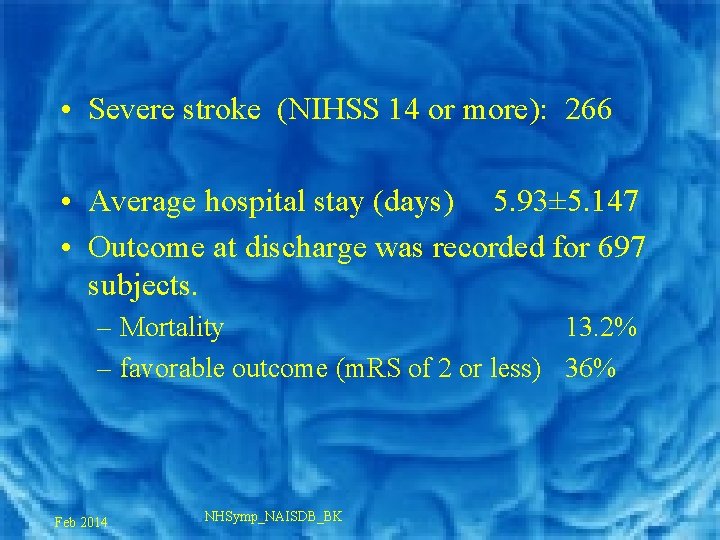
• Severe stroke (NIHSS 14 or more): 266 • Average hospital stay (days) 5. 93± 5. 147 • Outcome at discharge was recorded for 697 subjects. – Mortality 13. 2% – favorable outcome (m. RS of 2 or less) 36% Feb 2014 NHSymp_NAISDB_BK
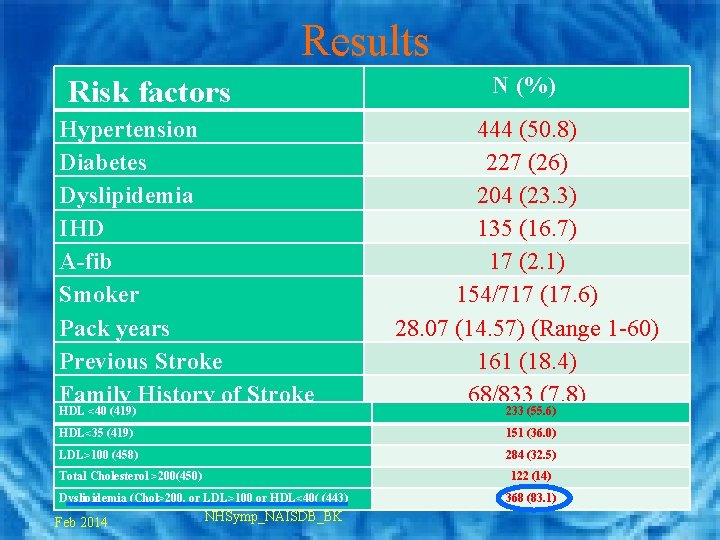
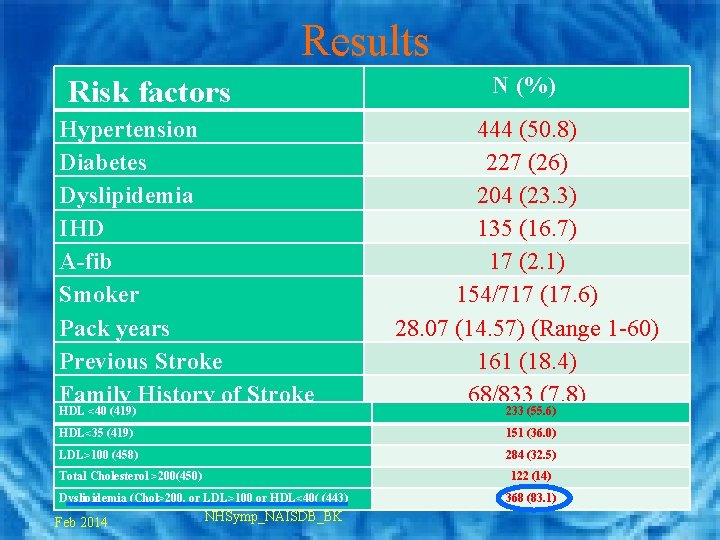
Results Risk factors Hypertension Diabetes Dyslipidemia IHD A-fib Smoker Pack years Previous Stroke Family History of Stroke HDL <40 (419) N (%) 444 (50. 8) 227 (26) 204 (23. 3) 135 (16. 7) 17 (2. 1) 154/717 (17. 6) 28. 07 (14. 57) (Range 1 -60) 161 (18. 4) 68/833 (7. 8) 233 (55. 6) HDL<35 (419) 151 (36. 0) LDL>100 (458) 284 (32. 5) Total Cholesterol >200(450) 122 (14) Dyslipidemia (Chol>200, or LDL>100 or HDL<40( (443) Feb 2014 NHSymp_NAISDB_BK 368 (83. 1)
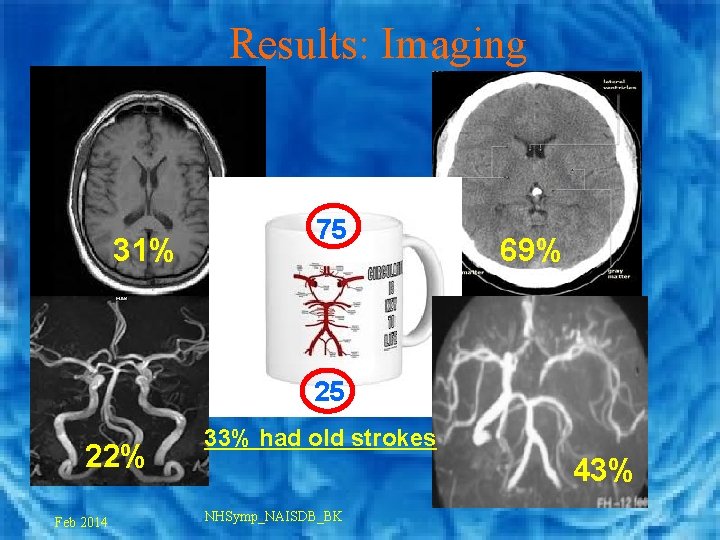
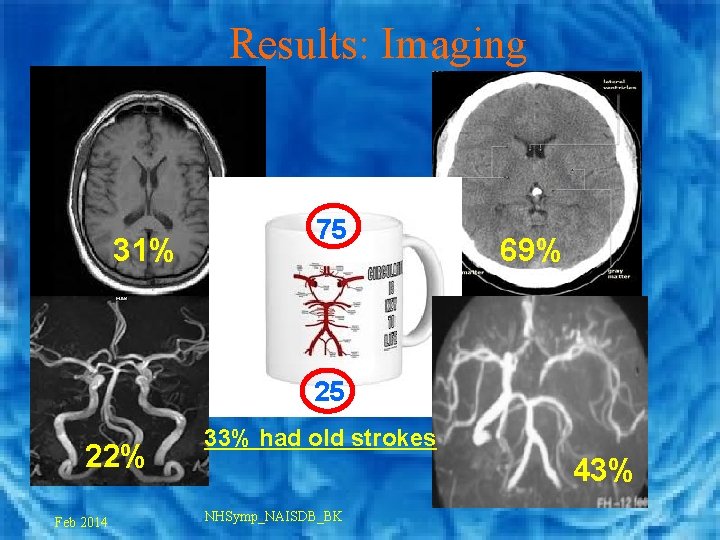
Results: Imaging 31% 75 69% 25 22% Feb 2014 33% had old strokes 43% NHSymp_NAISDB_BK
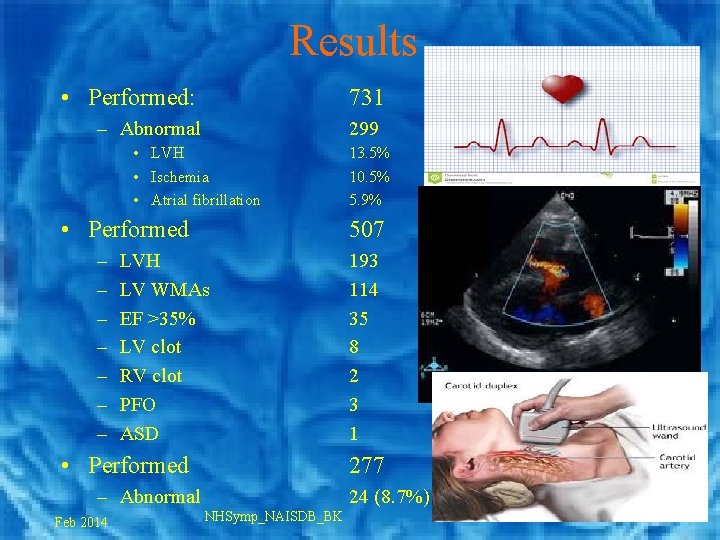
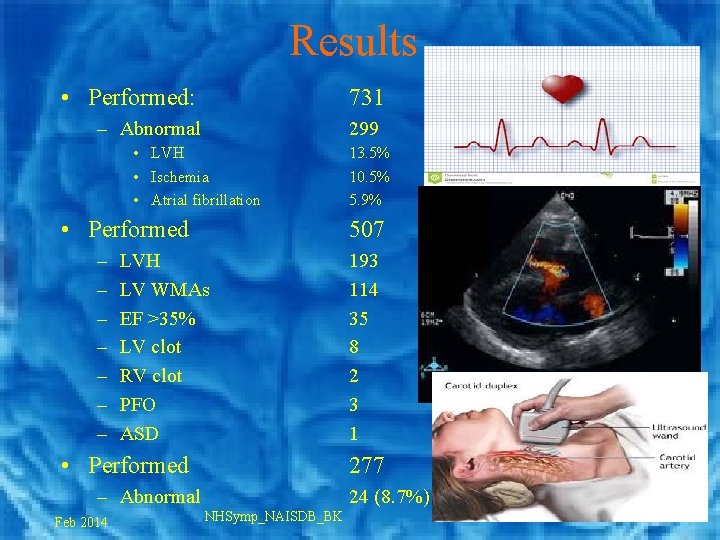
Results • Performed: 731 – Abnormal 299 • LVH • Ischemia • Atrial fibrillation • Performed – – – – 507 LVH LV WMAs EF >35% LV clot RV clot PFO ASD • Performed 193 114 35 8 2 3 1 277 – Abnormal Feb 2014 13. 5% 10. 5% 5. 9% 24 (8. 7%) NHSymp_NAISDB_BK
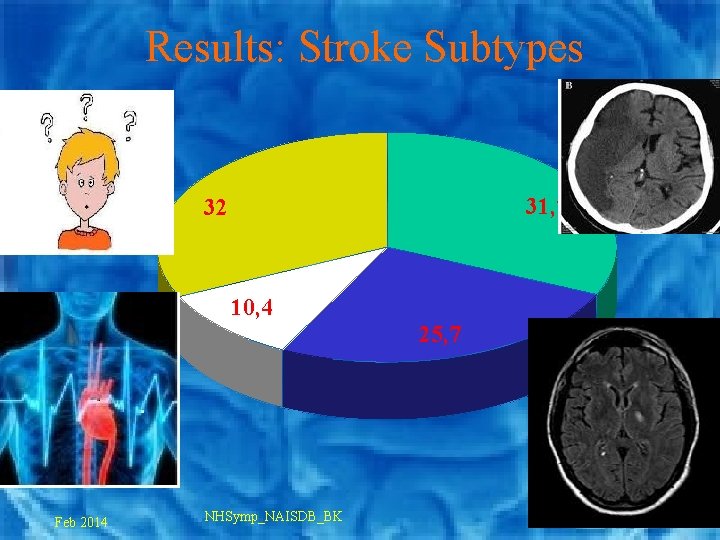
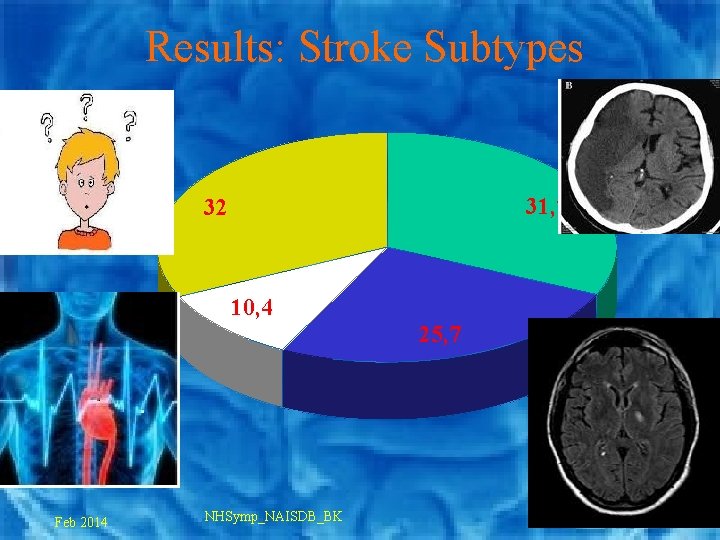
Results: Stroke Subtypes 31, 7 32 10, 4 25, 7 Feb 2014 NHSymp_NAISDB_BK
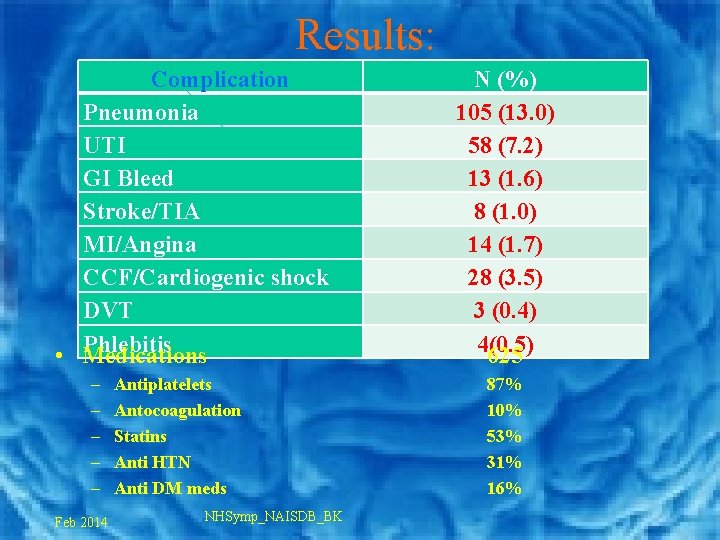
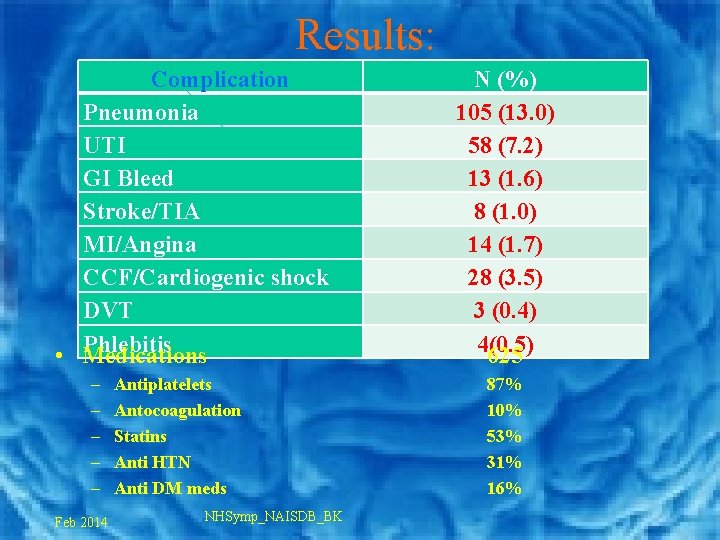
Results: Complication Pneumonia UTI GI Bleed Stroke/TIA MI/Angina CCF/Cardiogenic shock DVT Phlebitis • Medications – – – Feb 2014 Antiplatelets Antocoagulation Statins Anti HTN Anti DM meds NHSymp_NAISDB_BK N (%) 105 (13. 0) 58 (7. 2) 13 (1. 6) 8 (1. 0) 14 (1. 7) 28 (3. 5) 3 (0. 4) 4(0. 5) 625 87% 10% 53% 31% 16%
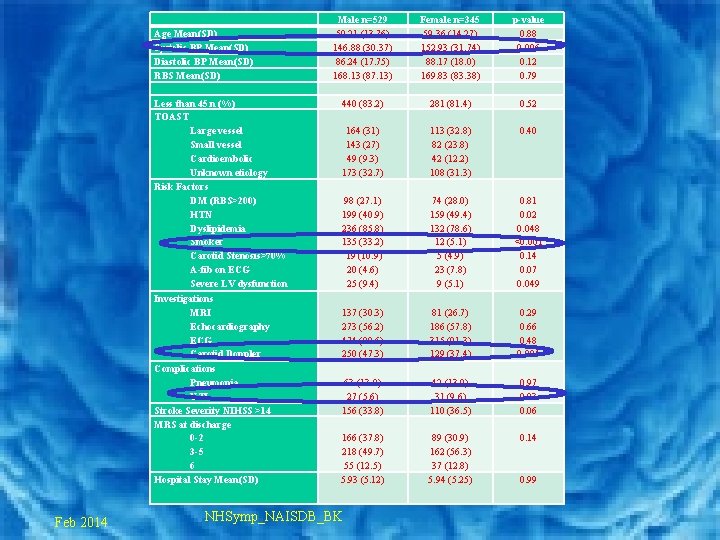
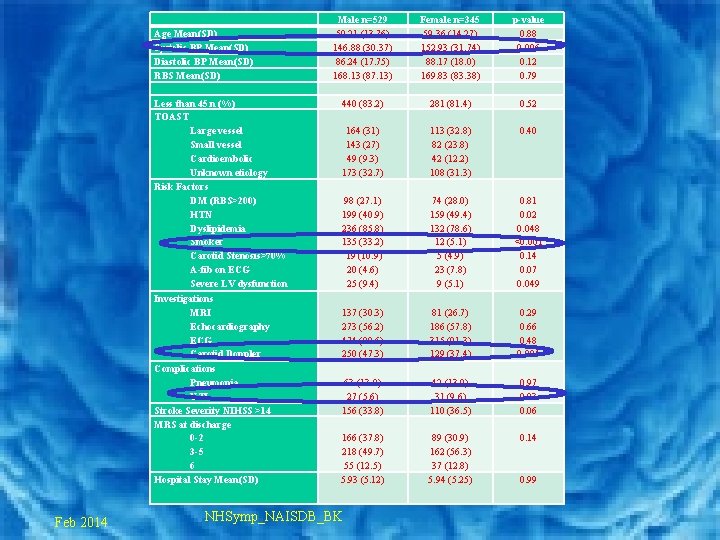
Age Mean(SD) Systolic BP Mean(SD) Diastolic BP Mean(SD) RBS Mean(SD) Less than 45 n (%) TOAST Large vessel Small vessel Cardioembolic Unknown etiology Risk Factors DM (RBS>200) HTN Dyslipidemia Smoker Carotid Stenosis>70% A-fib on ECG Severe LV dysfunction Investigations MRI Echocardiography ECG Carotid Doppler Complications Pneumonia UTI Stroke Severity NIHSS >14 MRS at discharge 0 -2 3 -5 6 Hospital Stay Mean(SD) Feb 2014 Male n=529 59. 21 (13. 76) 146. 88 (30. 37) 86. 24 (17. 75) 168. 13 (87. 13) Female n=345 59. 36 (14. 27) 152. 93 (31. 74) 88. 17 (18. 0) 169. 83 (83. 38) p-value 0. 88 0. 006 0. 12 0. 79 440 (83. 2) 281 (81. 4) 0. 52 164 (31) 143 (27) 49 (9. 3) 173 (32. 7) 113 (32. 8) 82 (23. 8) 42 (12. 2) 108 (31. 3) 0. 40 98 (27. 1) 199 (40. 9) 236 (85. 8) 135 (33. 2) 19 (10. 9) 20 (4. 6) 25 (9. 4) 74 (28. 0) 159 (49. 4) 132 (78. 6) 12 (5. 1) 5 (4. 9) 23 (7. 8) 9 (5. 1) 0. 81 0. 02 0. 048 <0. 001 0. 14 0. 07 0. 049 137 (30. 3) 273 (56. 2) 474 (89. 6) 250 (47. 3) 81 (26. 7) 186 (57. 8) 315 (91. 3) 129 (37. 4) 0. 29 0. 66 0. 48 0. 004 63 (13. 0) 27 (5. 6) 156 (33. 8) 42 (13. 0) 31 (9. 6) 110 (36. 5) 0. 97 0. 03 0. 06 166 (37. 8) 218 (49. 7) 55 (12. 5) 5. 93 (5. 12) 89 (30. 9) 162 (56. 3) 37 (12. 8) 5. 94 (5. 25) 0. 14 NHSymp_NAISDB_BK 0. 99
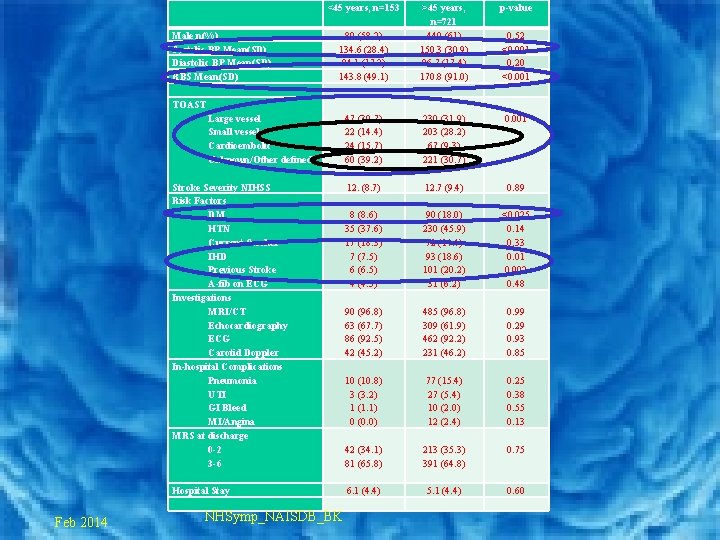
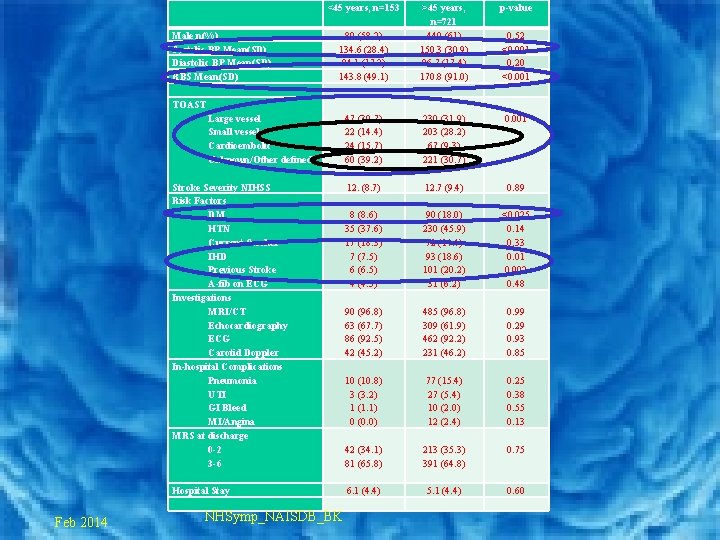
<45 years, n=153 Male n(%) Systolic BP Mean(SD) Diastolic BP Mean(SD) RBS Mean(SD) p-value 89 (58. 2) 134. 6 (28. 4) 84. 1 (17. 2) 143. 8 (49. 1) >45 years, n=721 440 (61) 150. 3 (30. 9) 86. 7 (17. 4) 170. 8 (91. 0) 47 (30. 7) 22 (14. 4) 24 (15. 7) 60 (39. 2) 230 (31. 9) 203 (28. 2) 67 (9. 3) 221 (30. 7) 0. 001 12. (8. 7) 12. 7 (9. 4) 0. 89 8 (8. 6) 35 (37. 6) 17 (18. 3) 7 (7. 5) 6 (6. 5) 4 (4. 3) 90 (18. 0) 230 (45. 9) 72 (14. 4) 93 (18. 6) 101 (20. 2) 31 (6. 2) <0. 025 0. 14 0. 33 0. 01 0. 002 0. 48 90 (96. 8) 63 (67. 7) 86 (92. 5) 42 (45. 2) 485 (96. 8) 309 (61. 9) 462 (92. 2) 231 (46. 2) 0. 99 0. 29 0. 93 0. 85 10 (10. 8) 3 (3. 2) 1 (1. 1) 0 (0. 0) 77 (15. 4) 27 (5. 4) 10 (2. 0) 12 (2. 4) 0. 25 0. 38 0. 55 0. 13 42 (34. 1) 81 (65. 8) 213 (35. 3) 391 (64. 8) 0. 75 6. 1 (4. 4) 5. 1 (4. 4) 0. 60 0. 52 <0. 001 0. 20 <0. 001 TOAST Large vessel Small vessel Cardioembolic Unknown/Other defined Stroke Severity NIHSS Risk Factors DM HTN Current Smoker IHD Previous Stroke A-fib on ECG Investigations MRI/CT Echocardiography ECG Carotid Doppler In-hospital Complications Pneumonia UTI GI Bleed MI/Angina MRS at discharge 0 -2 3 -6 Hospital Stay Feb 2014 NHSymp_NAISDB_BK
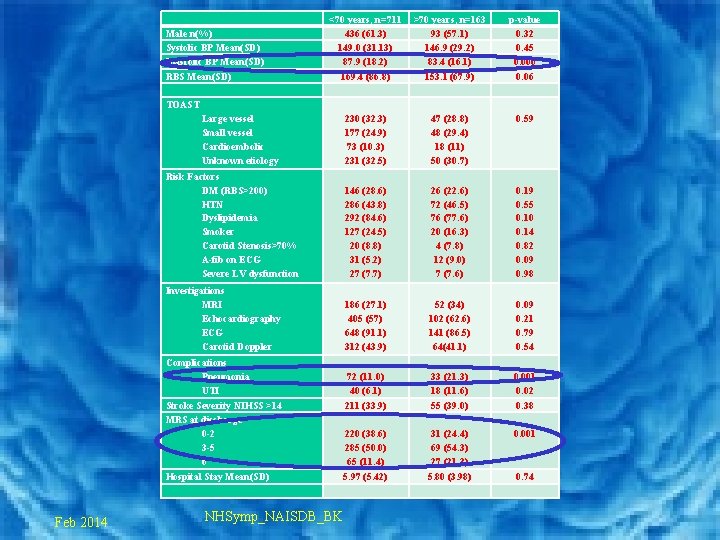
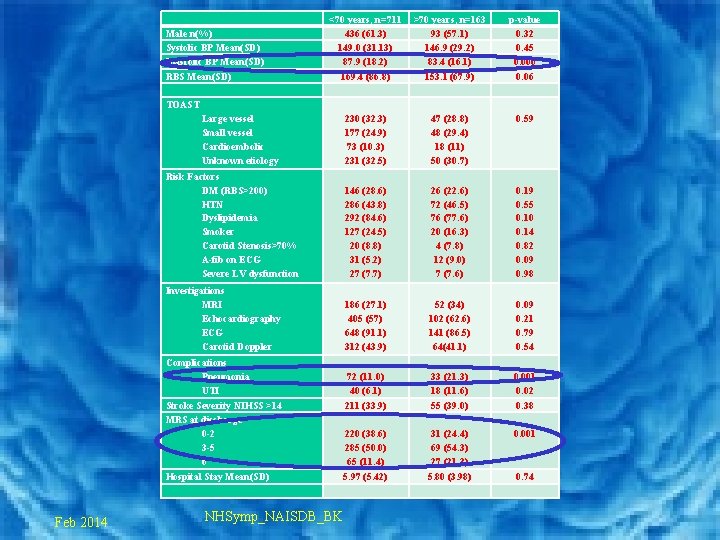
<70 years, n=711 436 (61. 3) 149. 0 (31. 13) 87. 9 (18. 2) 169. 4 (86. 8) >70 years, n=163 93 (57. 1) 146. 9 (29. 2) 83. 4 (16. 1) 153. 1 (67. 9) p-value 0. 32 0. 45 0. 006 0. 06 230 (32. 3) 177 (24. 9) 73 (10. 3) 231 (32. 5) 47 (28. 8) 48 (29. 4) 18 (11) 50 (30. 7) 0. 59 Risk Factors DM (RBS>200) HTN Dyslipidemia Smoker Carotid Stenosis>70% A-fib on ECG Severe LV dysfunction 146 (28. 6) 286 (43. 8) 292 (84. 6) 127 (24. 5) 20 (8. 8) 31 (5. 2) 27 (7. 7) 26 (22. 6) 72 (46. 5) 76 (77. 6) 20 (16. 3) 4 (7. 8) 12 (9. 0) 7 (7. 6) 0. 19 0. 55 0. 10 0. 14 0. 82 0. 09 0. 98 Investigations MRI Echocardiography ECG Carotid Doppler 186 (27. 1) 405 (57) 648 (91. 1) 312 (43. 9) 52 (34) 102 (62. 6) 141 (86. 5) 64(41. 1) 0. 09 0. 21 0. 79 0. 54 Complications Pneumonia UTI 72 (11. 0) 40 (6. 1) 33 (21. 3) 18 (11. 6) 0. 001 0. 02 Stroke Severity NIHSS >14 MRS at discharge 0 -2 3 -5 6 211 (33. 9) 55 (39. 0) 0. 38 220 (38. 6) 285 (50. 0) 65 (11. 4) 31 (24. 4) 69 (54. 3) 27 (21. 3) 0. 001 Hospital Stay Mean(SD) 5. 97 (5. 42) 5. 80 (3. 98) 0. 74 Male n(%) Systolic BP Mean(SD) Diastolic BP Mean(SD) RBS Mean(SD) TOAST Large vessel Small vessel Cardioembolic Unknown etiology Feb 2014 NHSymp_NAISDB_BK
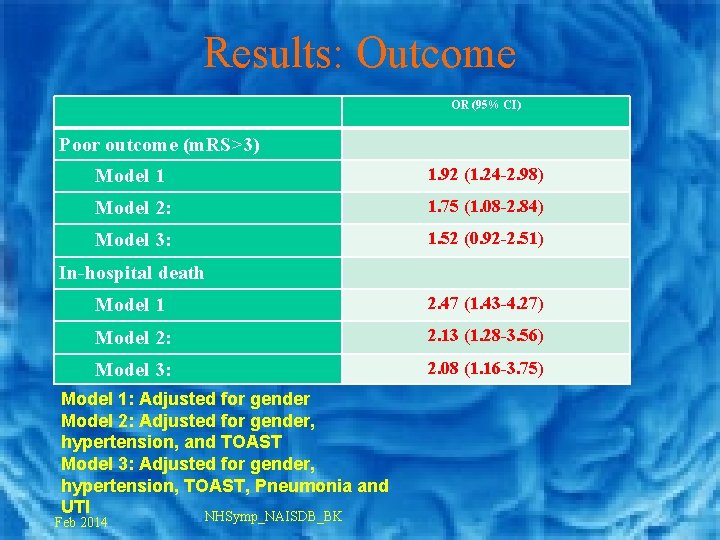
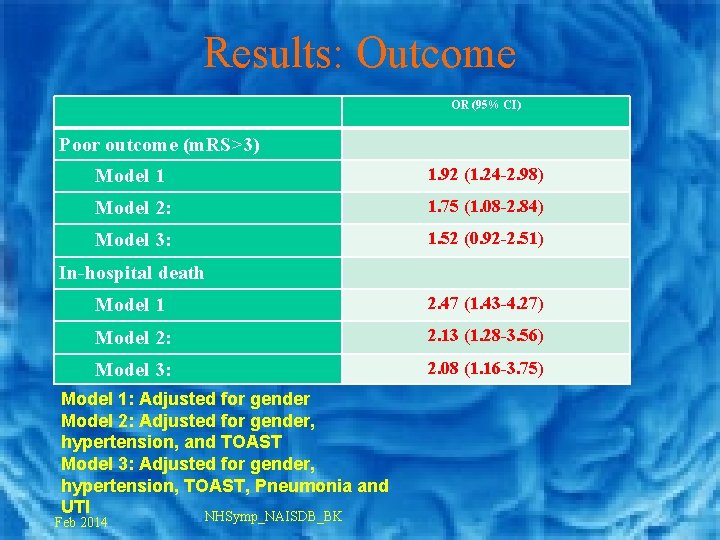
Results: Outcome OR (95% CI) Poor outcome (m. RS>3) Model 1 1. 92 (1. 24 -2. 98) Model 2: 1. 75 (1. 08 -2. 84) Model 3: 1. 52 (0. 92 -2. 51) In-hospital death Model 1 2. 47 (1. 43 -4. 27) Model 2: 2. 13 (1. 28 -3. 56) Model 3: 2. 08 (1. 16 -3. 75) Model 1: Adjusted for gender Model 2: Adjusted for gender, hypertension, and TOAST Model 3: Adjusted for gender, hypertension, TOAST, Pneumonia and UTI NHSymp_NAISDB_BK Feb 2014
Conclusion • Hypertension and dyslipidemia were the commonest risk factors • Large vessel atherosclerosis was the commonest stroke etiology. • Elderly patients were significantly – more likely to have in-hospital complications – to die during hospital stay – to have a higher modified Rankin score at discharge. Feb 2014 NHSymp_NAISDB_BK
Thanks Feb 2014 NHSymp_NAISDB_BK
 Stroke protocol
Stroke protocol Naisd
Naisd Mechanism of ischemic stroke
Mechanism of ischemic stroke Ischemic vs hemorrhagic stroke
Ischemic vs hemorrhagic stroke Tenecteplase stroke
Tenecteplase stroke Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Acute stroke ready certification
Acute stroke ready certification Mean arterial pressure
Mean arterial pressure Superadded changes in coronary atherosclerosis
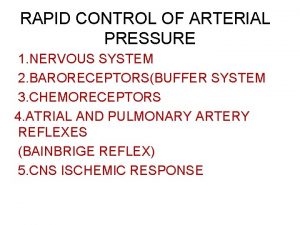
Superadded changes in coronary atherosclerosis Cns ischemic response
Cns ischemic response Ischemic bile duct injury
Ischemic bile duct injury Giant cell arteritis
Giant cell arteritis Cns ischemic response
Cns ischemic response Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Cns ischemic response
Cns ischemic response Ischemic heart disease classification
Ischemic heart disease classification National stroke audit rehabilitation services
National stroke audit rehabilitation services Stroke sentinel national audit programme
Stroke sentinel national audit programme Itus exam
Itus exam National unification and the national state
National unification and the national state Badminton serving drills
Badminton serving drills Cryotogenic
Cryotogenic Stroke coordinator boot camp
Stroke coordinator boot camp Carpet culture microbiology
Carpet culture microbiology