IRON METABOLISM AND DISORDERS Lecturer Dr E I
IRON METABOLISM AND DISORDERS Lecturer: Dr. E. I. Ugwuja Ph. D; AIBMS (UK) 13/01/2022 1
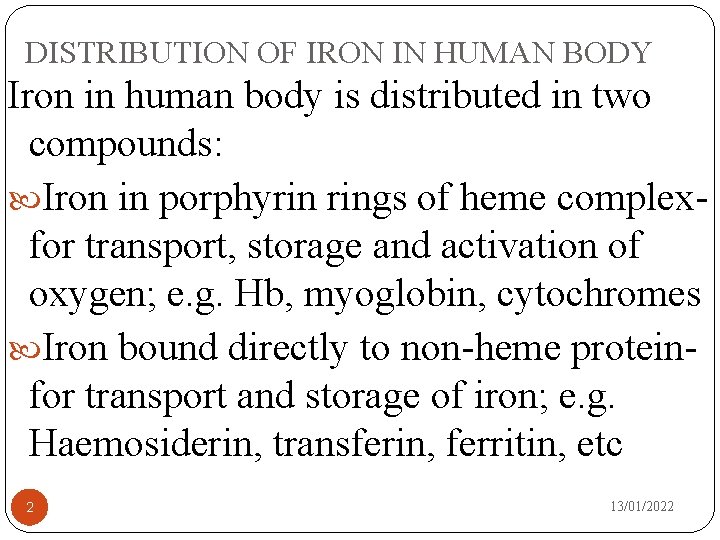
DISTRIBUTION OF IRON IN HUMAN BODY Iron in human body is distributed in two compounds: Iron in porphyrin rings of heme complexfor transport, storage and activation of oxygen; e. g. Hb, myoglobin, cytochromes Iron bound directly to non-heme proteinfor transport and storage of iron; e. g. Haemosiderin, transferin, ferritin, etc 2 13/01/2022
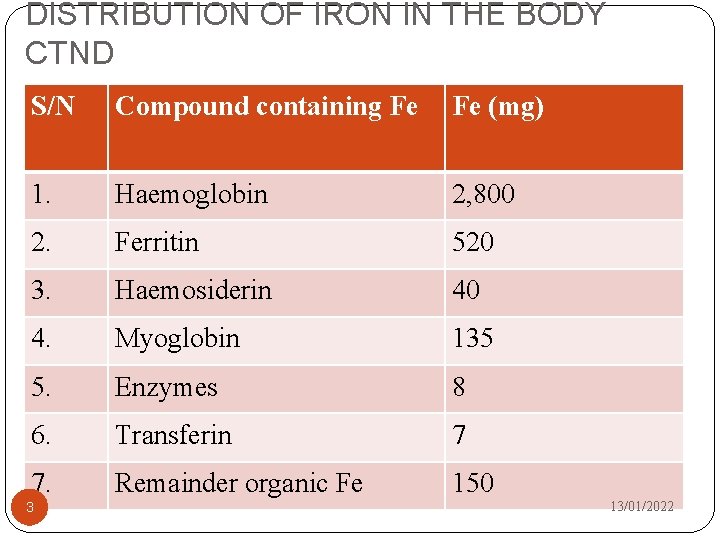
DISTRIBUTION OF IRON IN THE BODY CTND S/N Compound containing Fe Fe (mg) 1. Haemoglobin 2, 800 2. Ferritin 520 3. Haemosiderin 40 4. Myoglobin 135 5. Enzymes 8 6. Transferin 7 7. Remainder organic Fe 150 3 13/01/2022
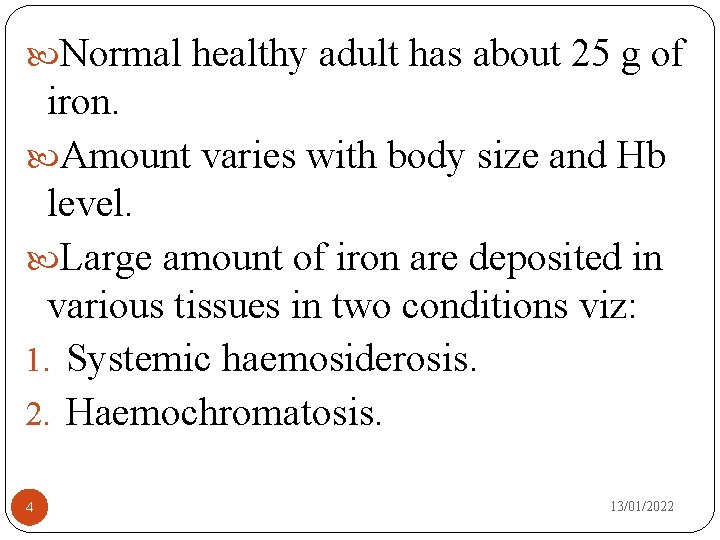
Normal healthy adult has about 25 g of iron. Amount varies with body size and Hb level. Large amount of iron are deposited in various tissues in two conditions viz: 1. Systemic haemosiderosis. 2. Haemochromatosis. 4 13/01/2022
IRON METABOLISM Unlike other elements, Fe homeostasis is regulated strictly by absorption and not by excretion. The capacity/capability of human to excrete Fe is very limited and inflexible. Therefore absorption has to be rigidly controlled to avoid toxic accumulation of Fe in tissues. Average daily Fe requirements for a healthy adult is 0. 9 mg. This take care of losses through various sources. 5 13/01/2022
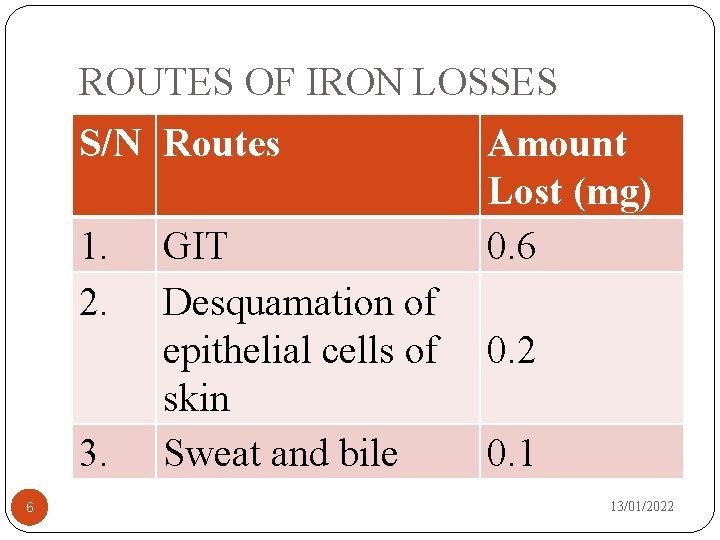
ROUTES OF IRON LOSSES S/N Routes 1. 2. 3. 6 GIT Desquamation of epithelial cells of skin Sweat and bile Amount Lost (mg) 0. 6 0. 2 0. 1 13/01/2022
For the healthy female, average requirement is about 1. 3 mg. Females need extra iron to take care of losses through menstruation, pregnancy and lactation Average diet provides 10 -15 mg Fe of which only 10% is absorbed. This may be enough for male. Female under certain circumstances may need Fe supplementation due to increased demand. 7 13/01/2022
SOURCES OF IRON Organ meat (liver, kidney) Egg yolk Fish Oysters Dry legumes Sea foods etc 8 13/01/2022
ABSORPTION OF IRON Major sites of iron absorption are the duodenum and upper jejunum. Small amount of Fe is also absorbed in the stomach Fe is absorbed in reduced form (Fe 2+). Fe absorption is effected by chaelation of Fe to amino acids. Apart from exogenous Fe, about 25 -30 mg of Fe is released endogenously through breakdown of RBC. Most of absorbed Fe is bound to transferin while unbound Fe are retained in the intestinal mucosa cells, where it attaches to apoprotein to form ferritin. 13/01/2022 9
FACTORS AFFECTING FE ABSORPTION Acid gastric juice facilitates Fe absorbtion Alcohol increases Fe absorption Ascorbic acid, citrate, fructose all favour Fe absorption Fe in eggs and green vegetables is less readily absorbed that Fe in bread and meat. Fe absorption is inhibited by presence of large amount of PO 43 - , phytate, fat, Ca++ in the diet. N/B: Free iron is extremely toxic and little 10 13/01/2022
DISORDERS OF IRON METABOLISM Disorders of iron metabolism can be considered under two major categories viz: Deficiency of iron (Haematologist). 2. Accummulation of iron (Chemical Pathologist)(a). Haemachromatosis and 1. 11 13/01/2022
PATHWAYS OF IRON ACCUMULATION Increased absorption. Excessive breakdown of erythrocytes. Impaired utilisation of absorbed iron. 12 13/01/2022
INCREASE ABSORPTION OF IRON Increased Fe absorption is associated with: Large amount of iron in diet; e. g. The Bantus of S/A. Ingestion of iron medication over a long period. Habitual intake of red wine Genetic factors. 13 13/01/2022
EXCESSIVE BREAKDOWN OF RBC This is associated with: Multiple transfusion of blood. Transfused blood has shorter lifespan than endogenous blood. Haemolytic disease; e. g G 6 PD, spherocytosis etc. 14 13/01/2022
IMPAIRED UTILISATION OF IRON Absorption of Fe will continue despite adequate body stores. Therefore in thalasaemia, absorbed Fe is not efficiently utilised and Fe is deposited in the body. 15 13/01/2022
HAEMOCHROMATOSIS Most important disorder of Fe metabolism Characterized by: i. Glycosuria with hyperglycaemia (DM) ii. Pigment cirrhosis iii. Siderosis of other organs iv. Pancreatic siderosis and fibrosis v. Skin pigmentation vi. Greatly increased body store of Fe (Upto 80 g) vii. High plasma Fe (≥ 200 -250µg/dl)-RR (100 -150) viii. Excessive saturation of transferin (60 -70%)-RR 16 (20 -50) 13/01/2022
N/B: All the eight characteristics may not necessarily be present before diagnosis is made. Pancreatic siderosis & fibrosis and skin pigmentation must be present (Features iv and v). The most constant of all the features are ii, iii and vi. DM may be absent in one third of individuals. 17 13/01/2022
RECOGNITION OF PATIENTS WITH HAEMATOCHROMATOSIS Patients may be found to be diabetic and further investigations will reveal underlying Fe storage disease. Hepatomegaly with portal hypertension may call the attention to the existence of the disease. A variety of endocrine dysfunction may become apparent; e. g. Sterility, impotence & renal dysfunction. Manifestation of cardiac failure which does not respond to convectional therapy for the disease. Skin pgmentation may be helpful but rather subtle. When present, it is evident on the face, genitals and skinfolds and arms. 18 13/01/2022
Note: Combination of skin pigmentation and liver cirrhosis points strongly to bronze diabetes, particularly when DM is also present. It is also important to document the increased plasma Fe as well as excessive saturation of transferin. 19 13/01/2022
HAEMOSIDEROSIS Two forms are known: Primary syndrome Secondary 20 13/01/2022
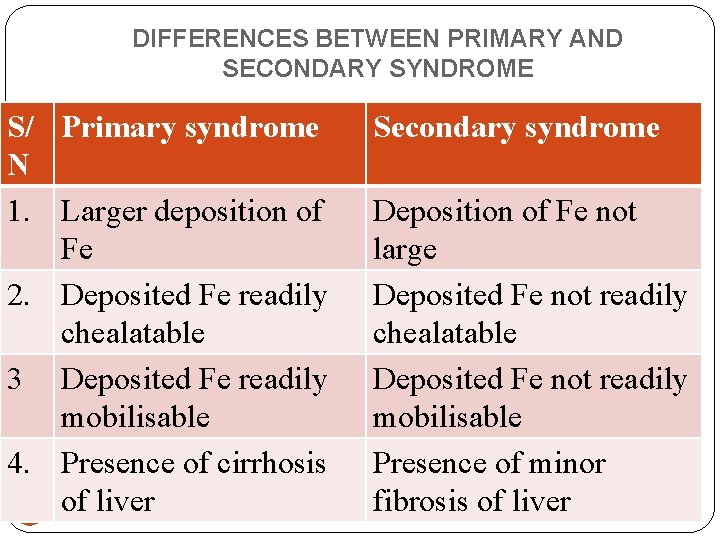
DIFFERENCES BETWEEN PRIMARY AND SECONDARY SYNDROME S/ Primary syndrome N 1. Larger deposition of Fe 2. Deposited Fe readily chealatable 3 Deposited Fe readily mobilisable 4. Presence of cirrhosis of liver 21 Secondary syndrome Deposition of Fe not large Deposited Fe not readily chealatable Deposited Fe not readily mobilisable Presence of minor fibrosis of liver 13/01/2022
MANAGEMENT/TREATMENT Two options are available: 1. Use of chealating agent. 2. Venesection (compulsory blood donation) 22 13/01/2022
Prior to venesection; 50 % of death from haemochromatosis are due to infection 17 % due to heart failure 10 % from 1 O liver cell carcinoma (PLCC) 7 % due to GI bleeding 5 % due to liver failure 23 13/01/2022
Venesection has been found to prolong the survival period of patients. It has been shown to reverse the histologic picture of the liver. Reduce hepatomegaly. Improve LFTs. Improve carbohydrate intolerance. N/B: For individuals who does not relinquish bad habits of alcohol abuse, even venesection will not improve their conditions. 24 13/01/2022
ANY QUESTIONS? 25 13/01/2022
- Slides: 25