Iron deficiency anemia Dr YASSER ALAHMADI Definition of
- Slides: 23
Iron deficiency anemia Dr. YASSER AL-AHMADI
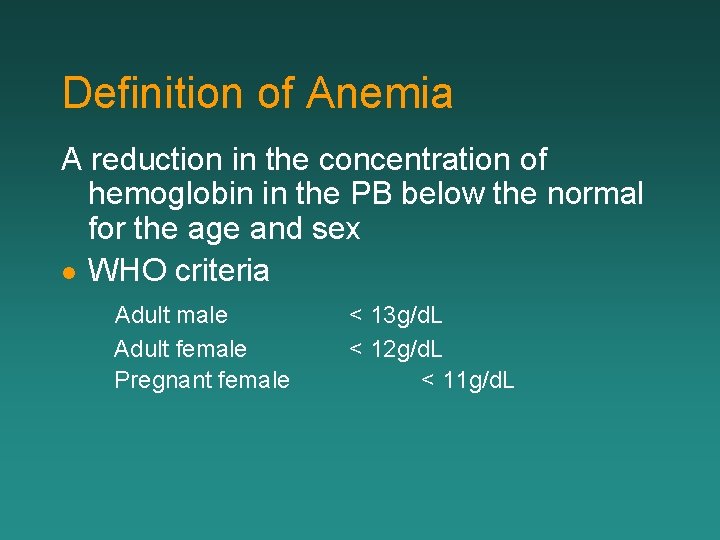
Definition of Anemia A reduction in the concentration of hemoglobin in the PB below the normal for the age and sex l WHO criteria Adult male Adult female Pregnant female < 13 g/d. L < 12 g/d. L < 11 g/d. L
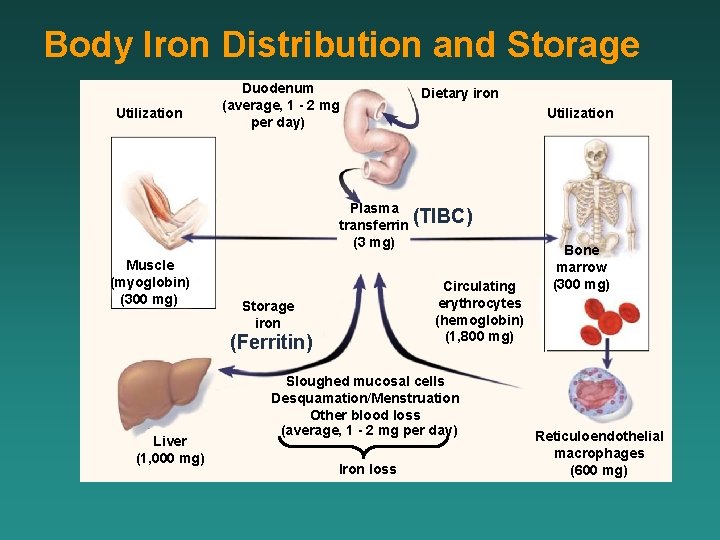
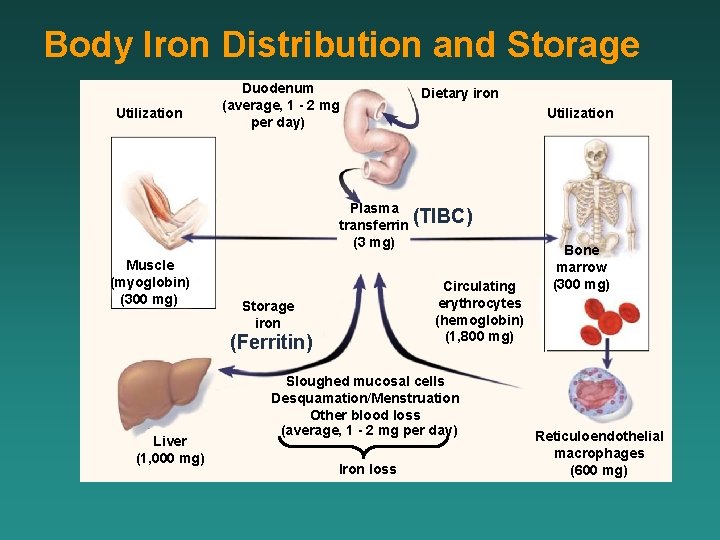
Body Iron Distribution and Storage Utilization Duodenum (average, 1 - 2 mg per day) Dietary iron Utilization Plasma (TIBC) transferrin (3 mg) Muscle (myoglobin) (300 mg) Circulating erythrocytes (hemoglobin) (1, 800 mg) Storage iron (Ferritin) Liver (1, 000 mg) Sloughed mucosal cells Desquamation/Menstruation Other blood loss (average, 1 - 2 mg per day) Iron loss Bone marrow (300 mg) Reticuloendothelial macrophages (600 mg)
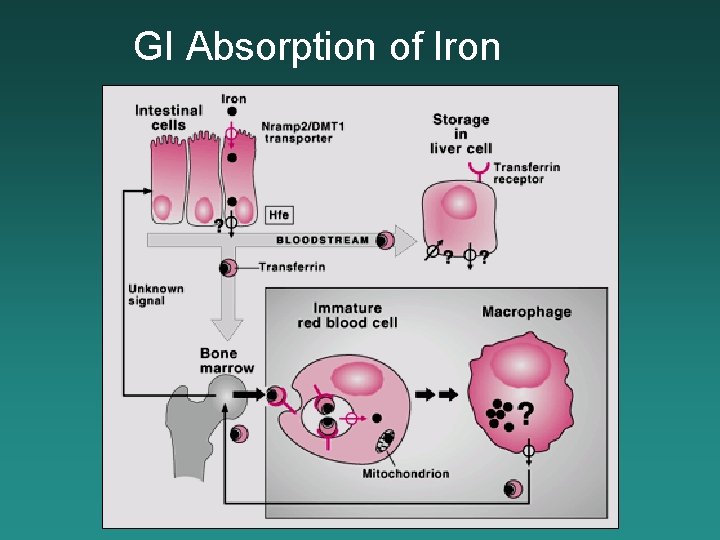
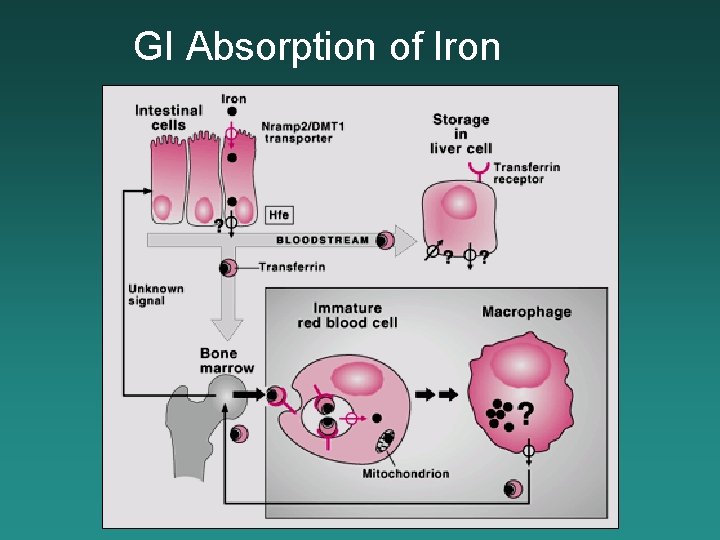
GI Absorption of Iron
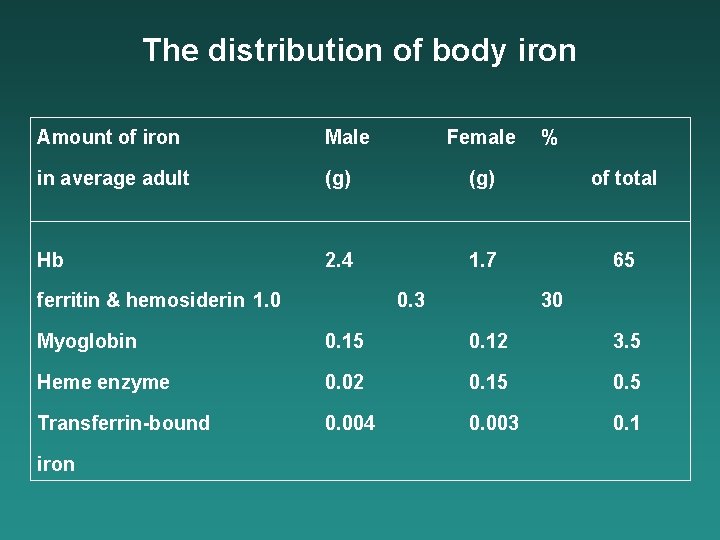
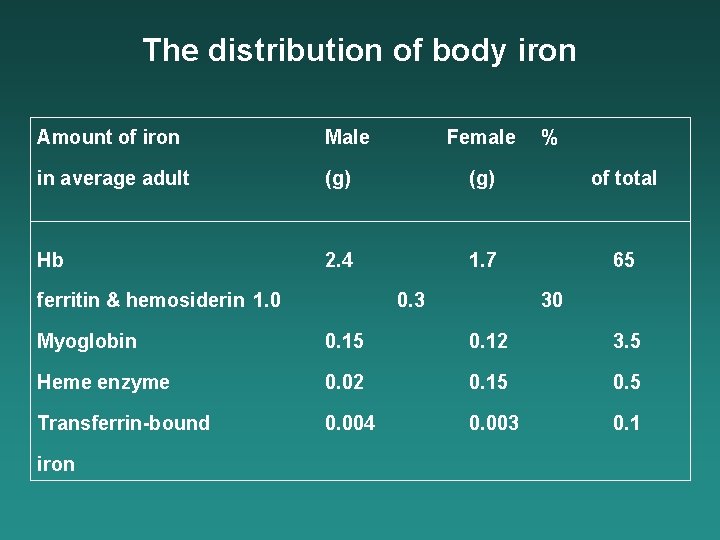
The distribution of body iron Amount of iron Male in average adult (g) of total Hb 2. 4 1. 7 65 ferritin & hemosiderin 1. 0 Female 0. 3 % 30 Myoglobin 0. 15 0. 12 3. 5 Heme enzyme 0. 02 0. 15 0. 5 Transferrin-bound 0. 004 0. 003 0. 1 iron
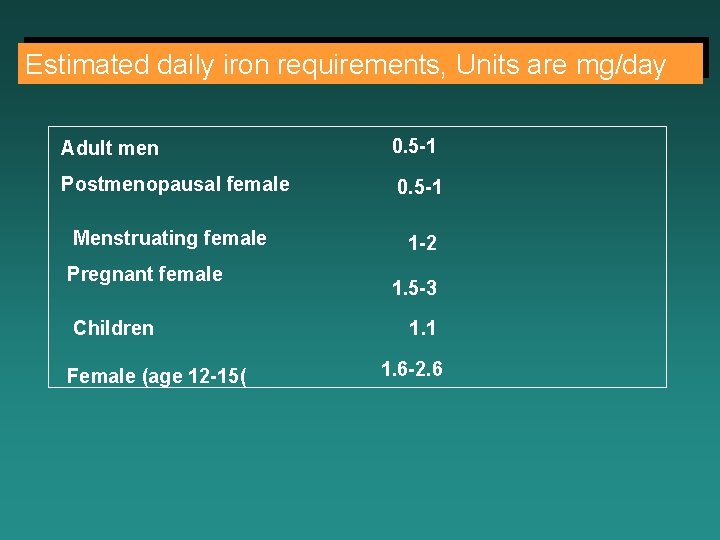
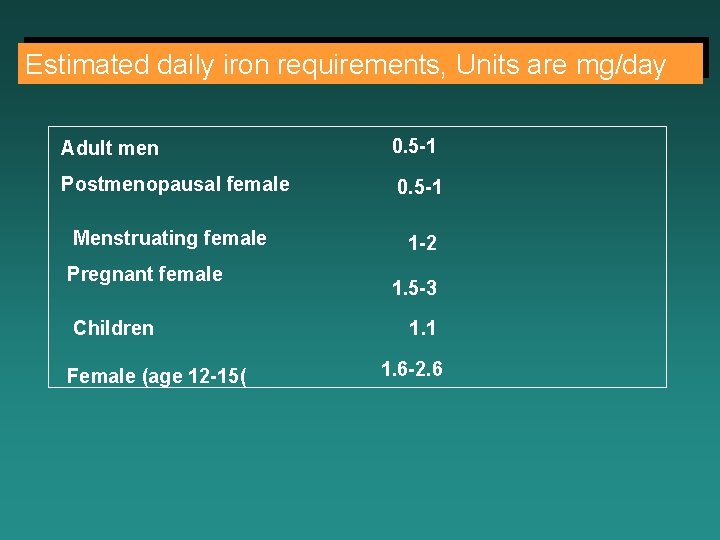
Estimated daily iron requirements, Units are mg/day Adult men 0. 5 -1 Postmenopausal female 0. 5 -1 Menstruating female 1 -2 Pregnant female Children Female (age 12 -15( 1. 5 -3 1. 1 1. 6 -2. 6
What is iron-deficiency anemia? It is the lack of iron in the blood, which is necessary to make hemoglobin.
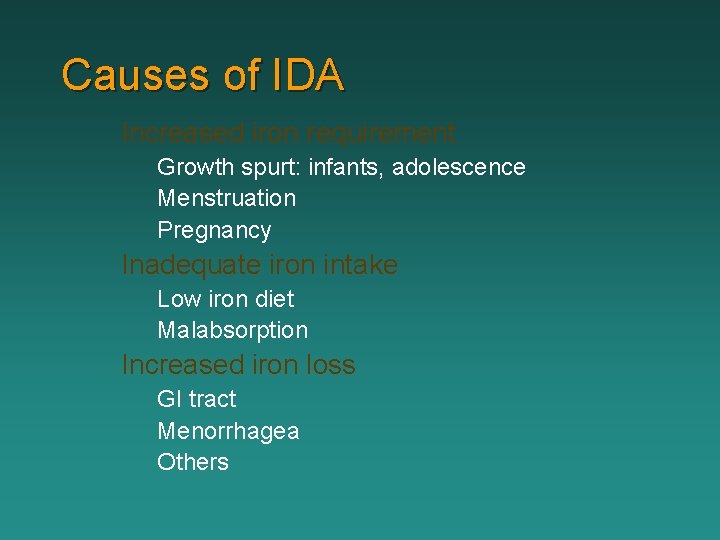
Causes of IDA Increased iron requirement Growth spurt: infants, adolescence Menstruation Pregnancy Inadequate iron intake Low iron diet Malabsorption Increased iron loss GI tract Menorrhagea Others
Diagnosis of Anemia l l l History Physical Examination Laboratory Investigation
Patient History Symptoms and its duration Fatigue, muscle weakness, headache, vertigo, syncope, dyspnea, palpitations, indigestion, etc Dietary habits/Pica Blood loss: Melena, Hematochezia, Hemorrhoid, Menstruation(Menorrhagea) Medications Previous record Family history
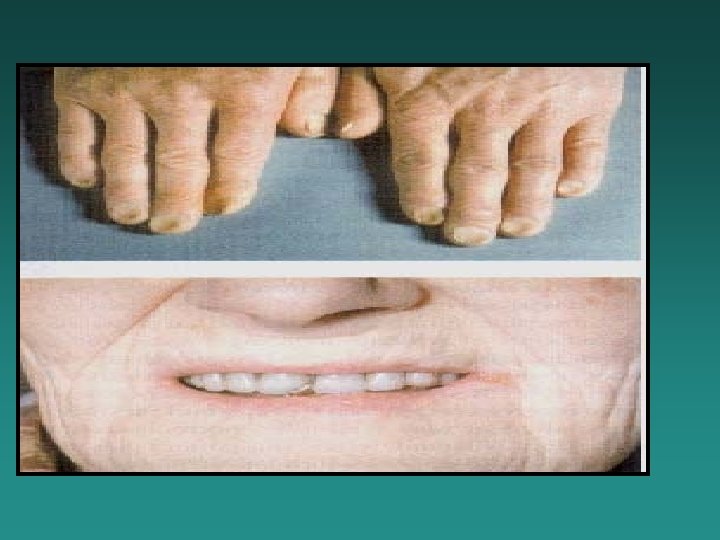
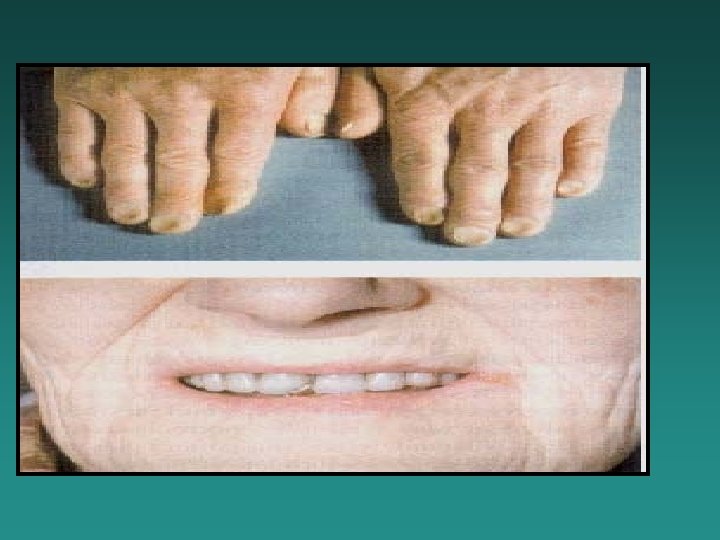
Physical Examination l Skin pallor Pale conjunctiva/Jaundice Smooth tongue/Stomatitis Splenomegaly/Hepatomegaly l Koilonychia (Nail spooning) l Esophageal Web l l l
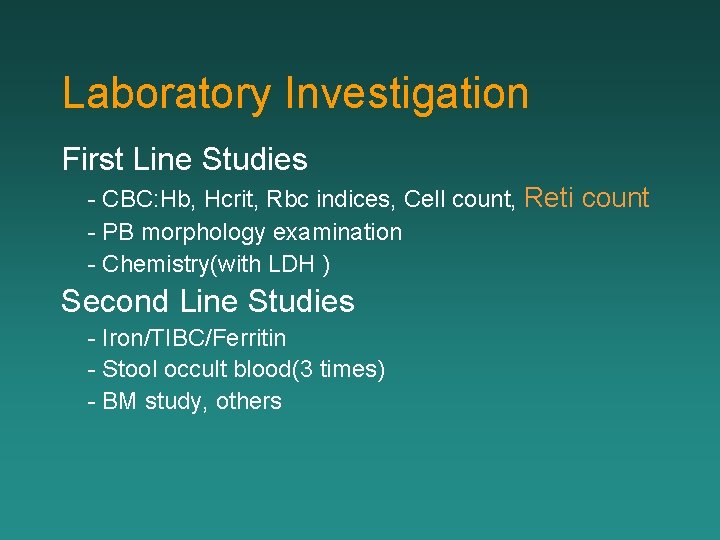
Laboratory Investigation First Line Studies - CBC: Hb, Hcrit, Rbc indices, Cell count, Reti count - PB morphology examination - Chemistry(with LDH ) Second Line Studies - Iron/TIBC/Ferritin - Stool occult blood(3 times) - BM study, others
BLOOD AND BONE MARROW SMEAR BLOOD: microcytosis, hipochromia, anulocytes, anisocytosis poikilocytosis BONE MARROW high cellularity mild to moderate erythroid hyperplasia (25 -35%; N 16 – 18%) polychromatic and pyknotic cytoplasm of erythroblasts is vacuolated and irregular in outline (micronormoblastic erythropoiesis) absence of stainable iron
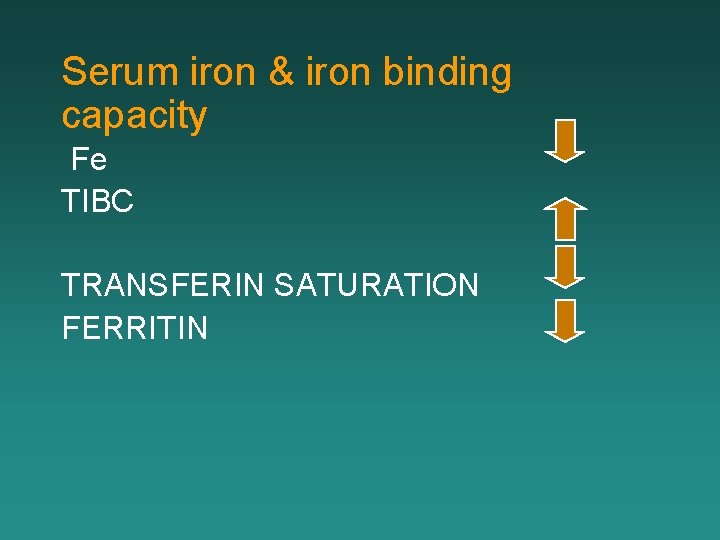
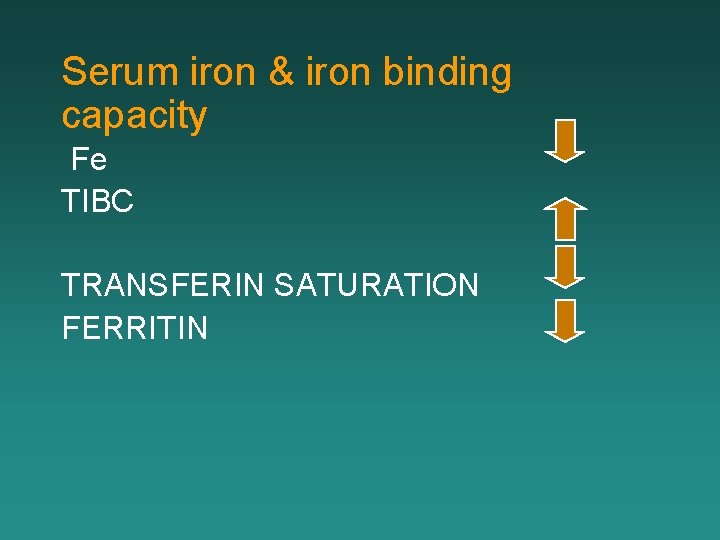
Serum iron & iron binding capacity Fe TIBC TRANSFERIN SATURATION FERRITIN
Treatment of IDA Correct underlying cause, if present Iron supplementation l l Oral iron: The best preperation is ferrous sulphate which contains 67 mg of iron in each 200 mg (anhydrous) tablet and is best given on an empty stomach in doses spaced by at least 6 hours. if side effects occur (e. g. nausea, abd pain , costipation or diahrea) these can be reduced by giving iron with food or by using a preparation of lower iron content e. g. ferrous gluconate which contains less iron 37 mg per 300 mg tablet. The hb should rise at the rate of about 2 g/dl every 3 weeks.
Parentral iron - Iron –sorbitol-citrate (jectofer) is given as repeated i. m injections whereas ferric hydroxide -sucrose (venofer) is administered by slow i. v inj or infusion. There may be hypersensitivity or anaphylactoid reactions and parentaral iron is therefore only given when it is considered necessary to replenish body iron rapidly (late pregnancy or p. t on hemodialysis and erythropoietin therapy or when oral iron is ineffective (e. g. severe malabsorption ). the hematological response is the same as in oral therapy. l
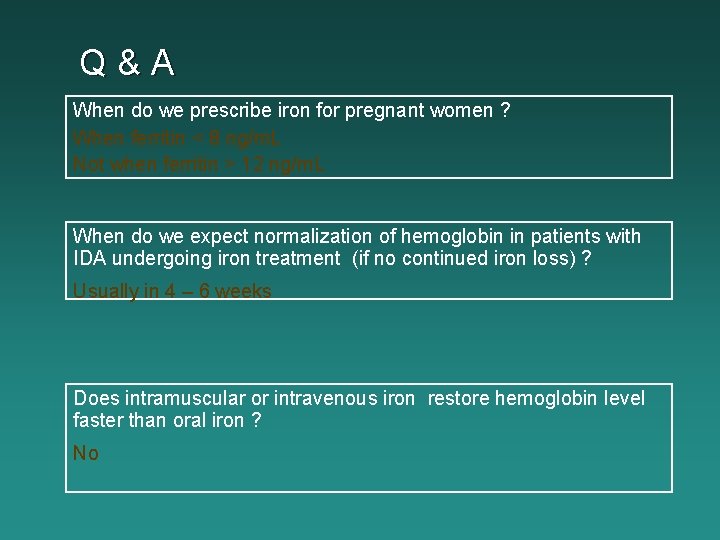
Q&A When do we prescribe iron for pregnant women ? When ferritin < 8 ng/m. L Not when ferritin > 12 ng/m. L When do we expect normalization of hemoglobin in patients with IDA undergoing iron treatment (if no continued iron loss) ? Usually in 4 – 6 weeks Does intramuscular or intravenous iron restore hemoglobin level faster than oral iron ? No
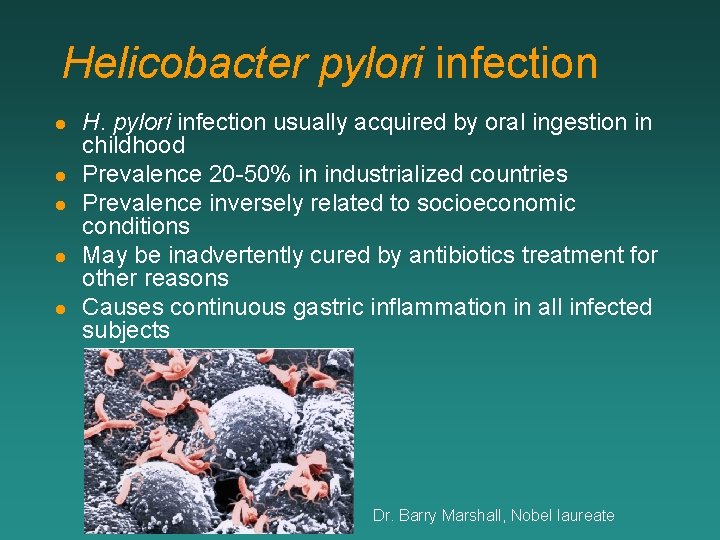
Helicobacter pylori infection l l l H. pylori infection usually acquired by oral ingestion in childhood Prevalence 20 -50% in industrialized countries Prevalence inversely related to socioeconomic conditions May be inadvertently cured by antibiotics treatment for other reasons Causes continuous gastric inflammation in all infected subjects Dr. Barry Marshall, Nobel laureate
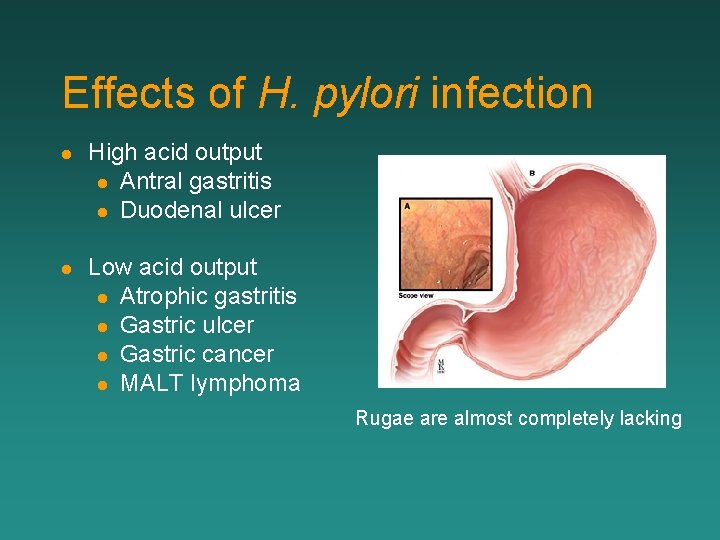
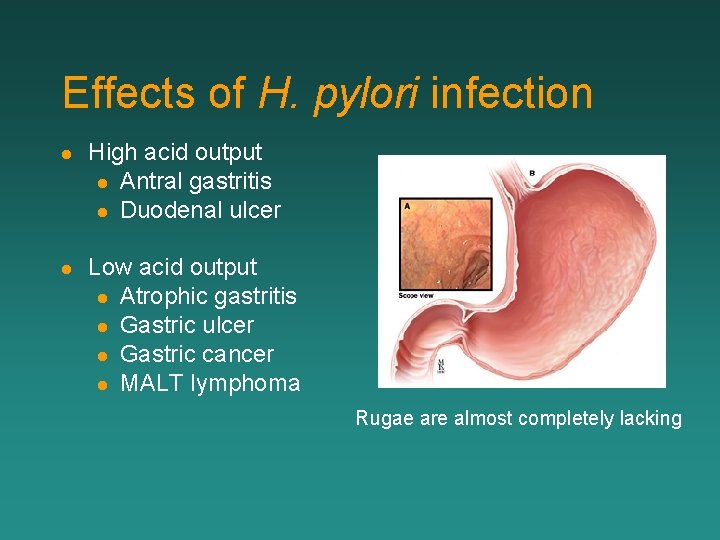
Effects of H. pylori infection l High acid output l Antral gastritis l Duodenal ulcer l Low acid output l Atrophic gastritis l Gastric ulcer l Gastric cancer l MALT lymphoma Rugae are almost completely lacking
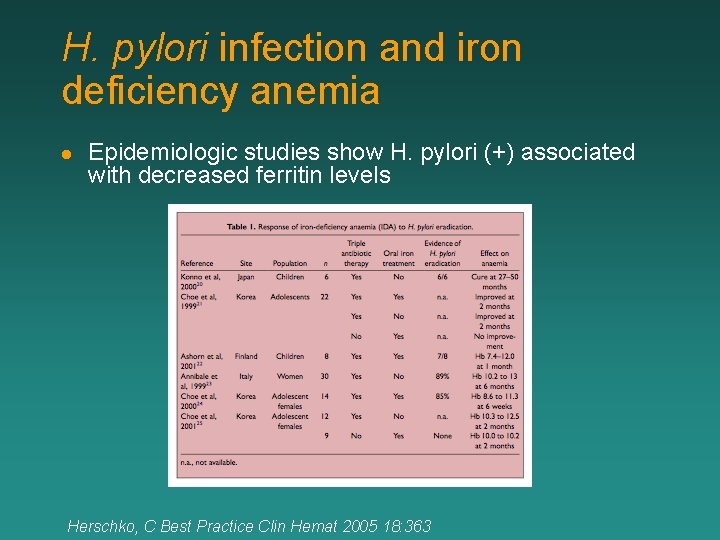
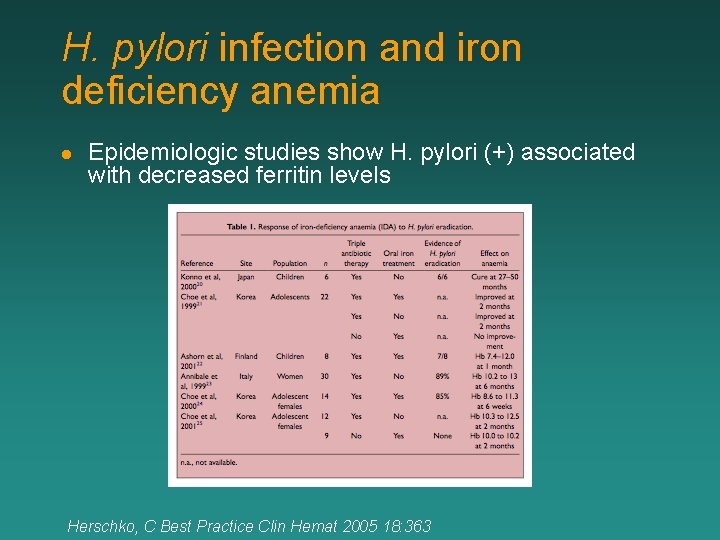
H. pylori infection and iron deficiency anemia l Epidemiologic studies show H. pylori (+) associated with decreased ferritin levels Herschko, C Best Practice Clin Hemat 2005 18: 363
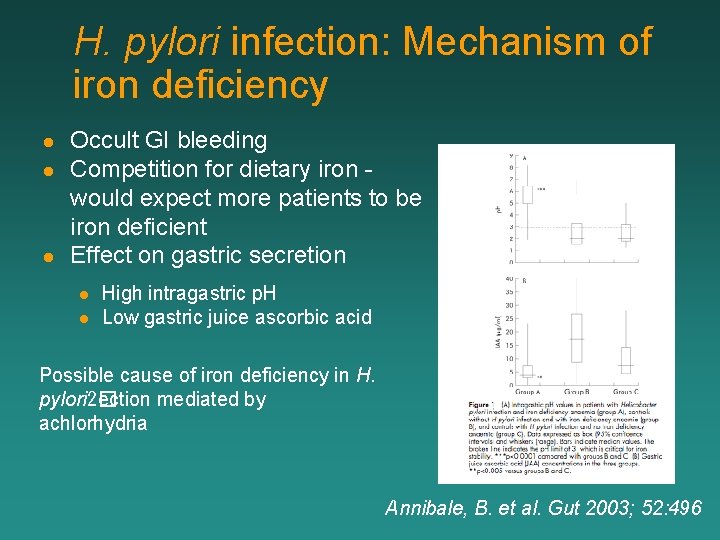
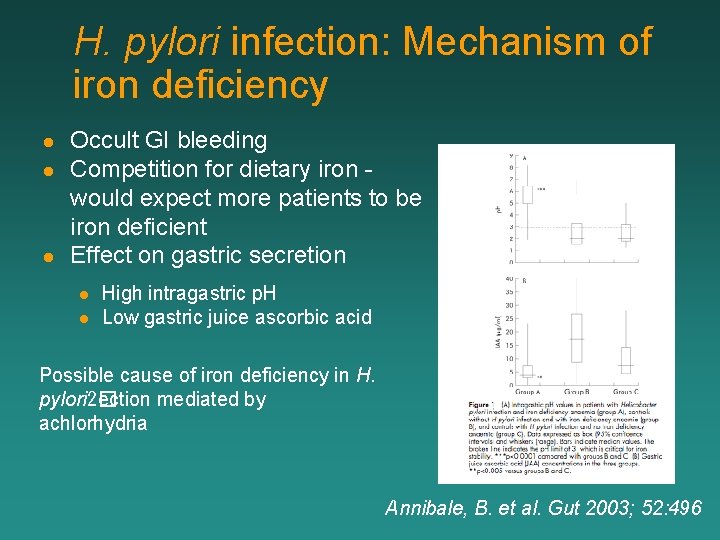
H. pylori infection: Mechanism of iron deficiency l l l Occult GI bleeding Competition for dietary iron would expect more patients to be iron deficient Effect on gastric secretion l l High intragastric p. H Low gastric juice ascorbic acid Possible cause of iron deficiency in H. pylori 2� ection mediated by achlorhydria Annibale, B. et al. Gut 2003; 52: 496
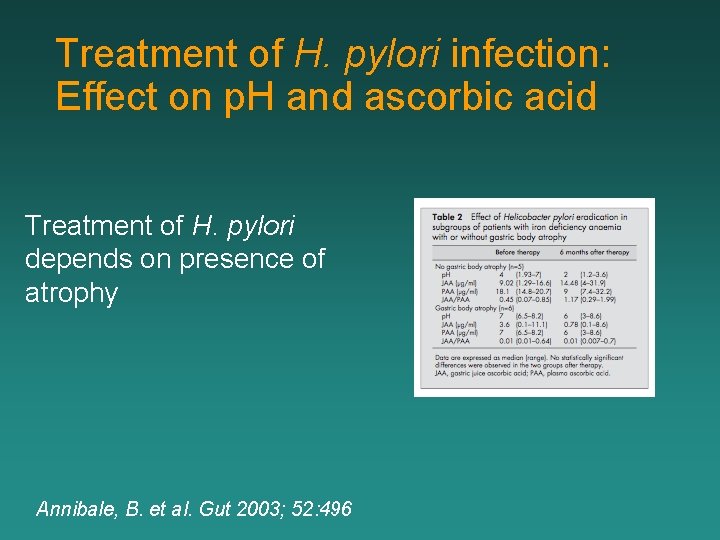
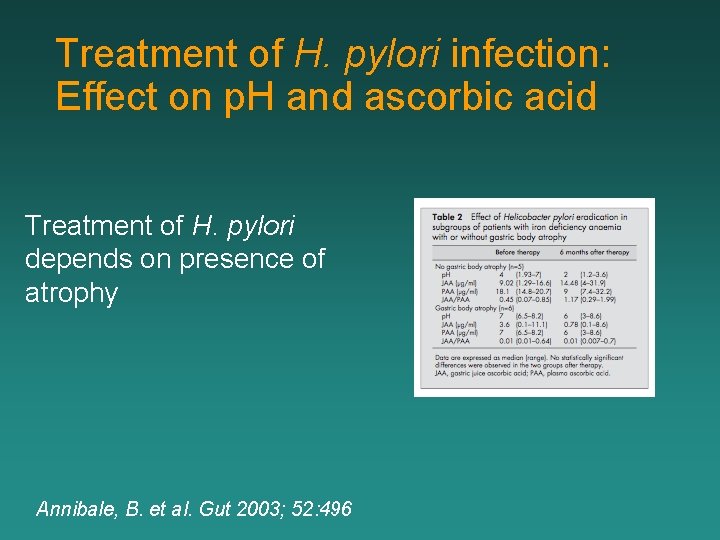
Treatment of H. pylori infection: Effect on p. H and ascorbic acid Treatment of H. pylori depends on presence of atrophy Annibale, B. et al. Gut 2003; 52: 496