IRON DEFICIENCY ANEMIA Dr S Hasan Amir Introduction
- Slides: 36
IRON DEFICIENCY ANEMIA Dr. S. Hasan Amir.
Introduction Ø Iron deficiency is the most common type of anaemia. Ø 83 -90% of all anemia constitute IDA Ø Every day about 30 mg iron is used to make new hemoglobin. Ø Daily iron loss is around 1 mg. Ø In women menstruation and childbirth increase iron losses to about 1. 5 mg/day.
DIETARY IRON Ø There are 2 types of iron in the diet 1. Heme iron 2. Non-heme iron Ø Heme iron is present in Hb containing animal food like meat, liver & spleen. Ø Non-heme iron is obtained from cereals, vegetables & beans.
IRON ABSORPTION Ø Site- Proximal small intestine i. e. duodenum (first part - maximum absorption) and jejunum. Ø 10% of dietary iron is absorbed Ø It is determined by intraluminal factor i. e. p. H and redox potential. Ø Therapeutic ferrous iron is well absorbed on empty stomach. Ø Haem iron is not affected by ingestion of other food items. Ø Heme iron → Acid and gastric juices release it from apoprotein → Oxidised → hemin → directly absorb through mucosal cell intact.
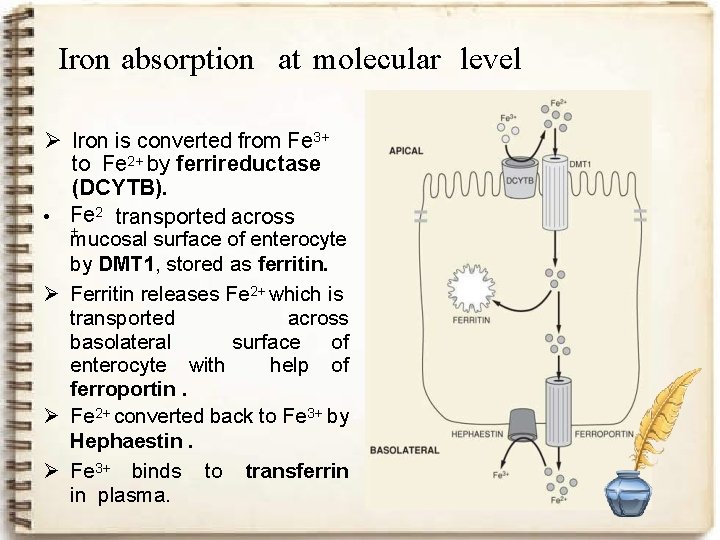
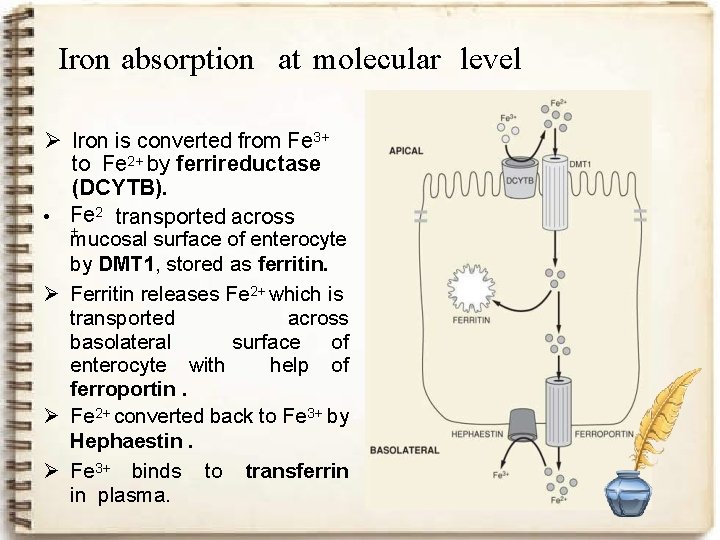
Iron absorption at molecular level Ø Iron is converted from Fe 3+ to Fe 2+ by ferrireductase (DCYTB). • Fe 2 transported across + mucosal surface of enterocyte by DMT 1, stored as ferritin. Ø Ferritin releases Fe 2+ which is transported across basolateral surface of enterocyte with help of ferroportin. Ø Fe 2+ converted back to Fe 3+ by Hephaestin. Ø Fe 3+ binds to transferrin in plasma.
Promoters of Iron Absorption Ø Foods containing ascorbic acid like citrus fruits, broccoli & other dark green vegetables Ø Foods containing muscle protein Ø Food fermentation aids iron absorption by reducing the phytate content of diet
INHIBITORS OF IRON ABSORPTION q Food with polyphenol compounds Ø Cereals like sorghum & oats Ø Vegetables such as spinach and spices Ø Beverages like tea, coffee, cocoa and wine. Ø A single cup of tea taken with meal reduces iron absorption by up to 11%. Ø Food containing phytic acid i. e. Bran Ø Cow’s milk due to its high calcium & casein contents.
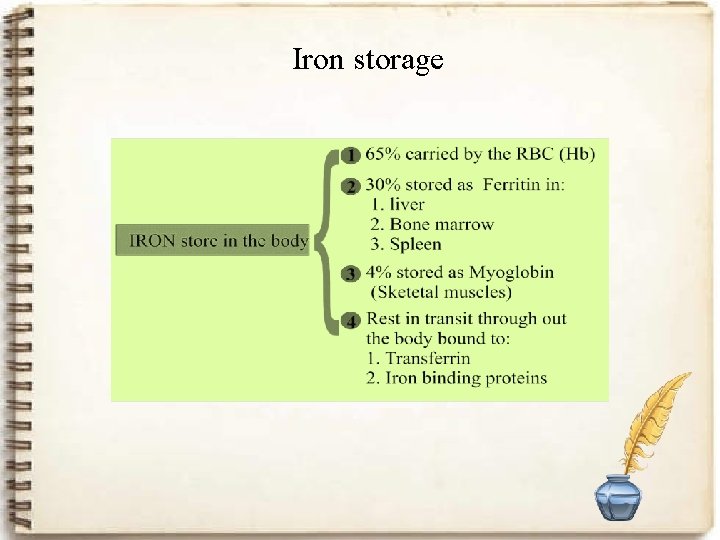
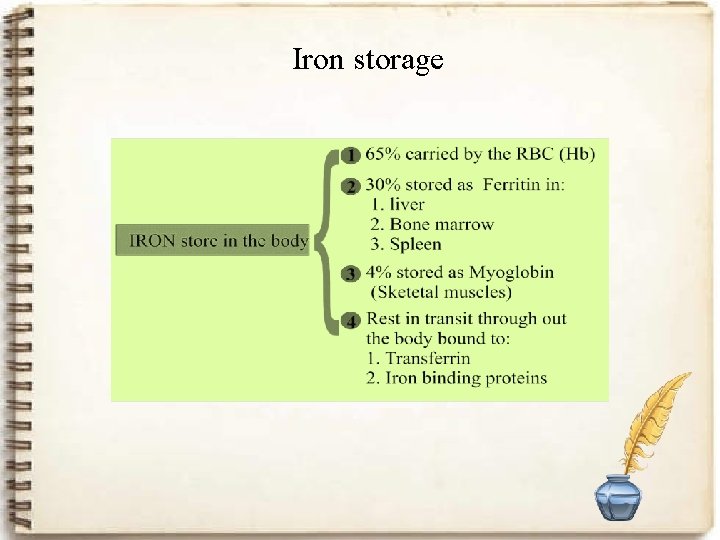
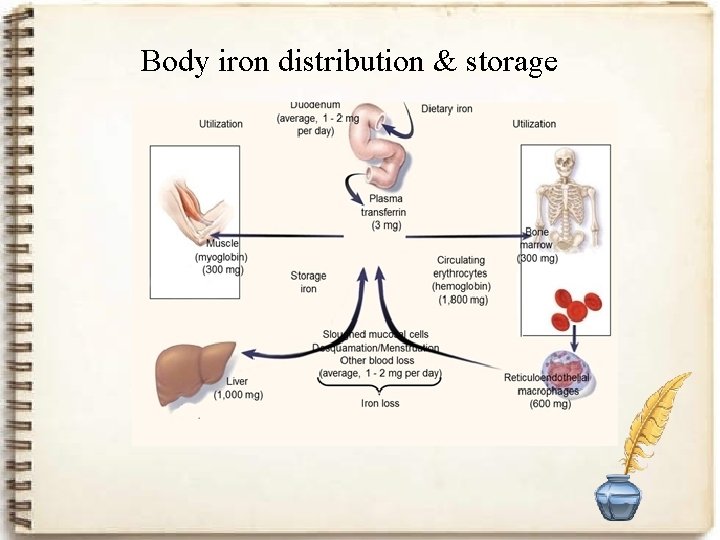
Iron storage
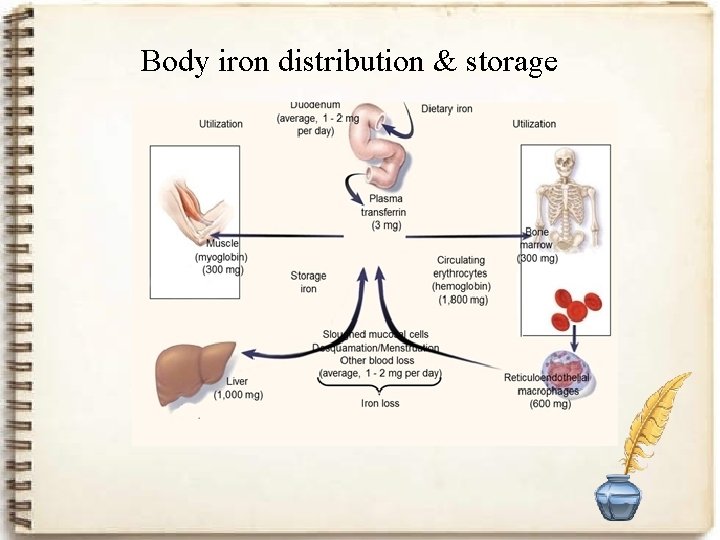
Body iron distribution & storage
Body composition Ø The total content of iron in the body - about 4. 2 g. I. 75 -80% belongs to the hemoglobin I. 20 - 25% reserve II. 5 -10% part of the myoglobin III. -1% is part of the enzyme for the tissue respiration
AT RISK GROUPS 1. Infants 2. Under 5 children 3. Children of school age 4. Women of child bearing age 5. Geriatric age group
Causes of iron deficiency Ø Ø Ø Ø Chronic blood loss Increased demand Malabsorbtion of iron Inadequate iron intake Intravascular hemolysis hemoglobinuria- hemosiderinuria Combinations
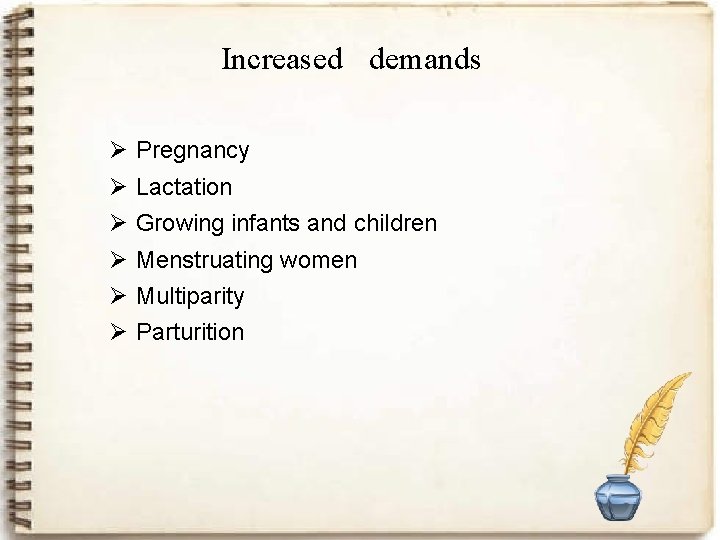
Increased demands Ø Ø Ø Pregnancy Lactation Growing infants and children Menstruating women Multiparity Parturition
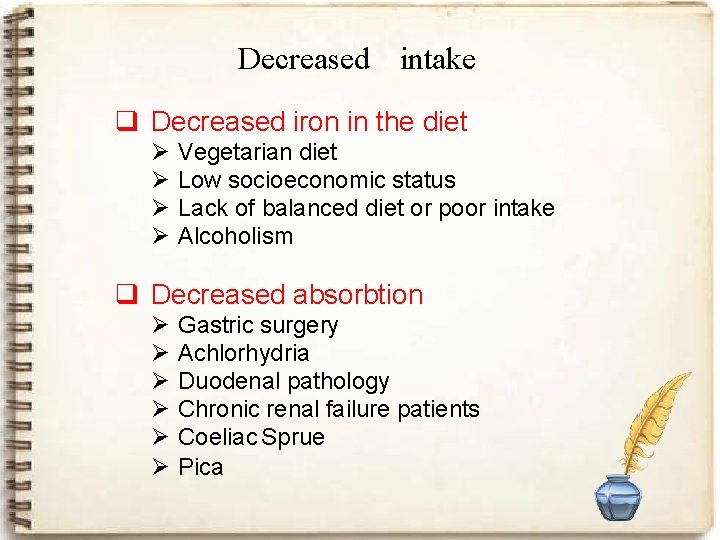
Decreased intake q Decreased iron in the diet Ø Ø Vegetarian diet Low socioeconomic status Lack of balanced diet or poor intake Alcoholism q Decreased absorbtion Ø Ø Ø Gastric surgery Achlorhydria Duodenal pathology Chronic renal failure patients Coeliac Sprue Pica
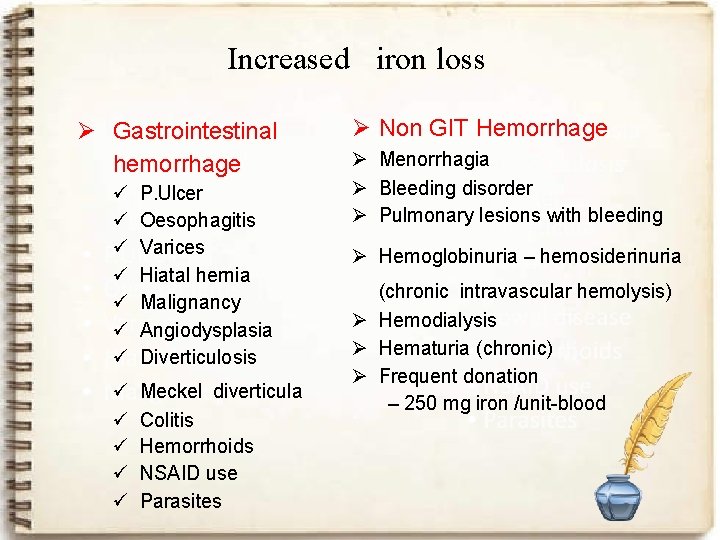
Increased iron loss Ø Gastrointestinal hemorrhage ü ü ü ü P. Ulcer Oesophagitis Varices Hiatal hernia Malignancy Angiodysplasia Diverticulosis ü ü ü Meckel diverticula Colitis Hemorrhoids NSAID use Parasites Ø Non GIT Hemorrhage Ø Menorrhagia Ø Bleeding disorder Ø Pulmonary lesions with bleeding Ø Hemoglobinuria – hemosiderinuria (chronic intravascular hemolysis) Ø Hemodialysis Ø Hematuria (chronic) Ø Frequent donation – 250 mg iron /unit-blood
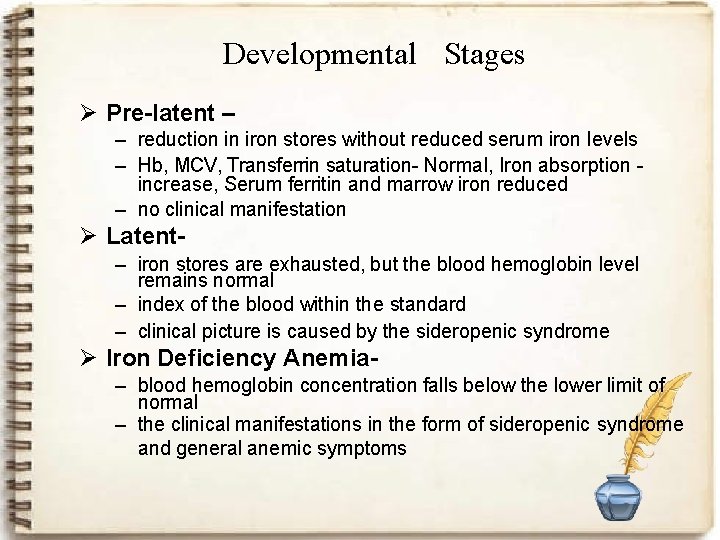
Developmental Stages Ø Pre-latent – – reduction in iron stores without reduced serum iron levels – Hb, MCV, Transferrin saturation- Normal, Iron absorption increase, Serum ferritin and marrow iron reduced – no clinical manifestation Ø Latent– iron stores are exhausted, but the blood hemoglobin level remains normal – index of the blood within the standard – clinical picture is caused by the sideropenic syndrome Ø Iron Deficiency Anemia– blood hemoglobin concentration falls below the lower limit of normal – the clinical manifestations in the form of sideropenic syndrome and general anemic symptoms
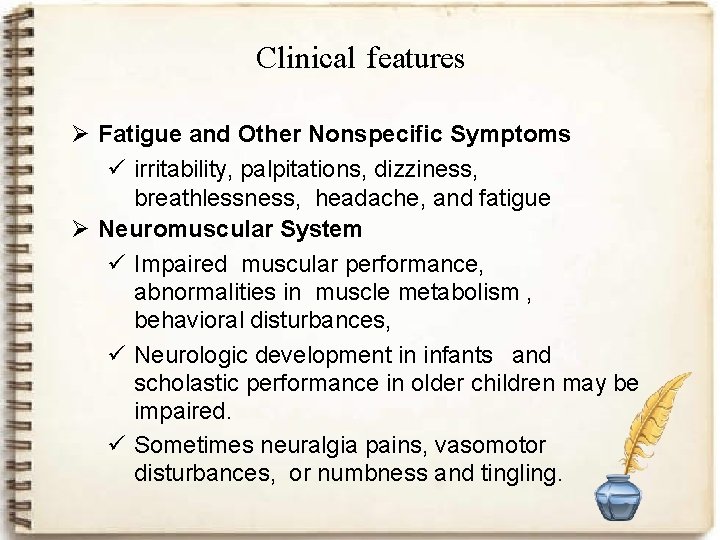
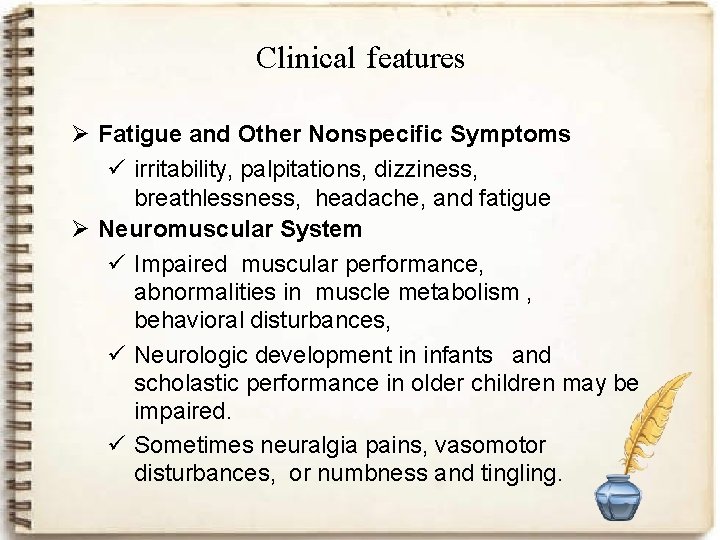
Clinical features Ø Fatigue and Other Nonspecific Symptoms ü irritability, palpitations, dizziness, breathlessness, headache, and fatigue Ø Neuromuscular System ü Impaired muscular performance, abnormalities in muscle metabolism , behavioral disturbances, ü Neurologic development in infants and scholastic performance in older children may be impaired. ü Sometimes neuralgia pains, vasomotor disturbances, or numbness and tingling.
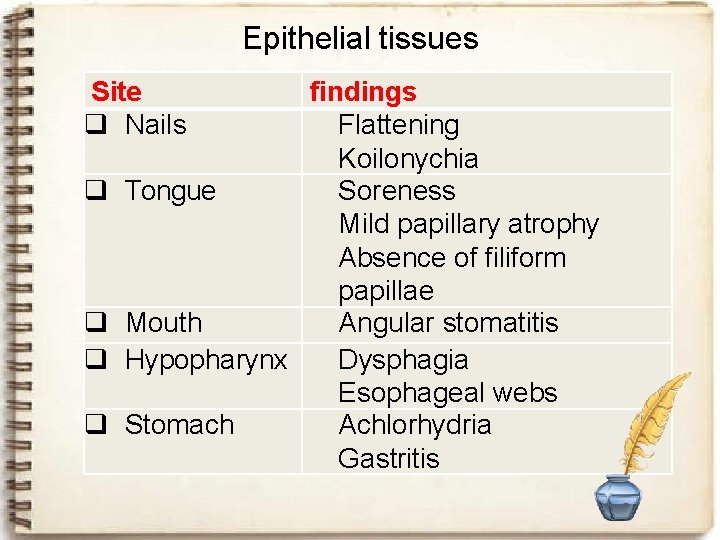
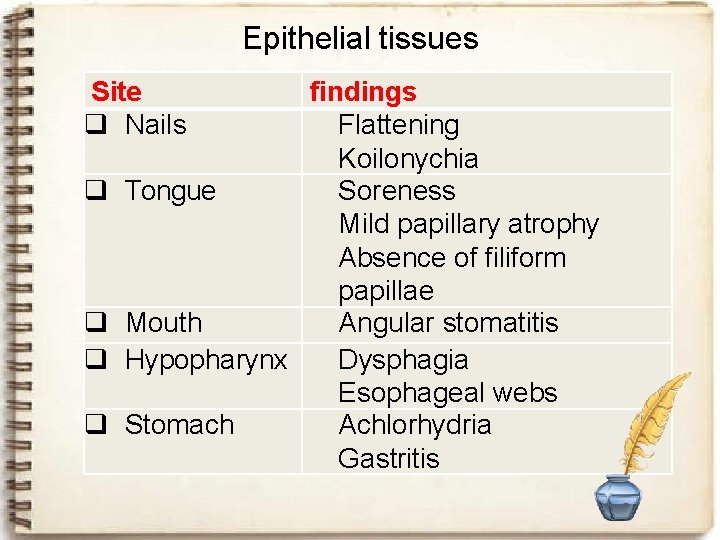
Epithelial tissues Site q Nails findings Flattening Koilonychia q Tongue Soreness Mild papillary atrophy Absence of filiform papillae q Mouth Angular stomatitis q Hypopharynx Dysphagia Esophageal webs q Stomach Achlorhydria Gastritis
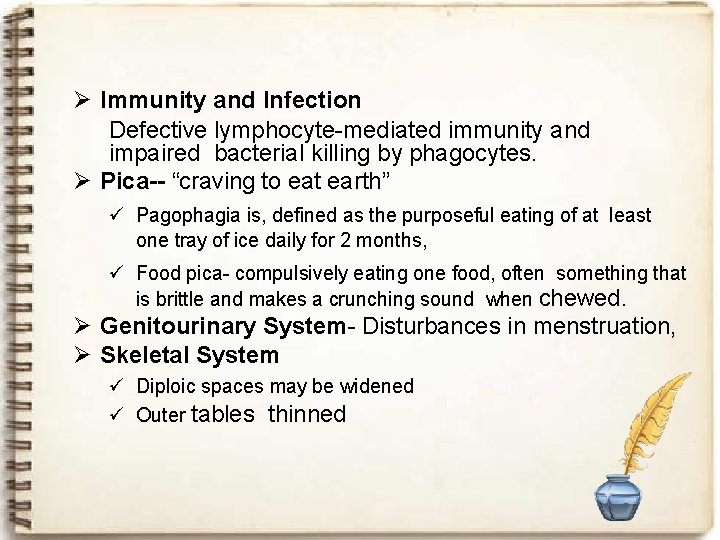
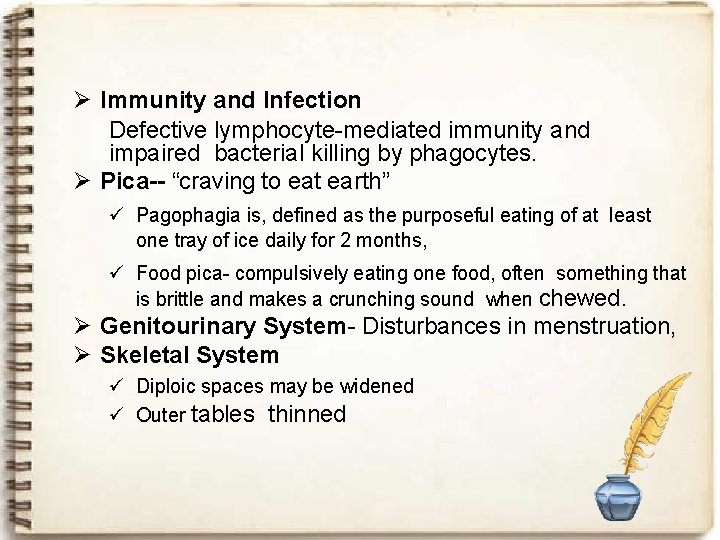
Ø Immunity and Infection Defective lymphocyte-mediated immunity and impaired bacterial killing by phagocytes. Ø Pica-- “craving to eat earth” ü Pagophagia is, defined as the purposeful eating of at least one tray of ice daily for 2 months, ü Food pica- compulsively eating one food, often something that is brittle and makes a crunching sound when chewed. Ø Genitourinary System- Disturbances in menstruation, Ø Skeletal System ü Diploic spaces may be widened ü Outer tables thinned
Laboratory diagnosis 1. Complete blood count 2. Bone marrow study 3. Serum parameter
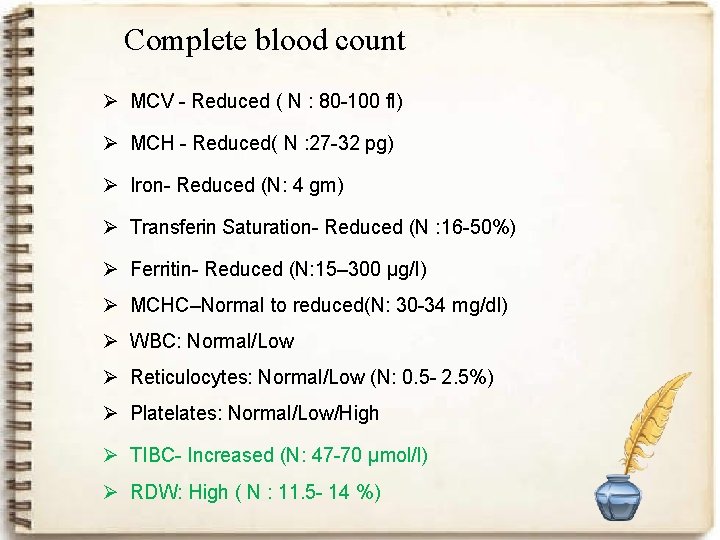
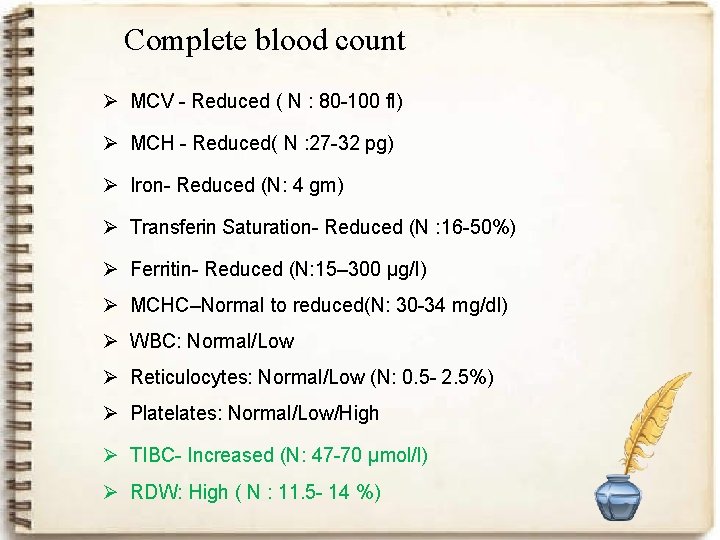
Complete blood count Ø MCV - Reduced ( N : 80 -100 fl) Ø MCH - Reduced( N : 27 -32 pg) Ø Iron- Reduced (N: 4 gm) Ø Transferin Saturation- Reduced (N : 16 -50%) Ø Ferritin- Reduced (N: 15– 300 µg/l) Ø MCHC–Normal to reduced(N: 30 -34 mg/dl) Ø WBC: Normal/Low Ø Reticulocytes: Normal/Low (N: 0. 5 - 2. 5%) Ø Plates: Normal/Low/High Ø TIBC- Increased (N: 47 -70 µmol/l) Ø RDW: High ( N : 11. 5 - 14 %)
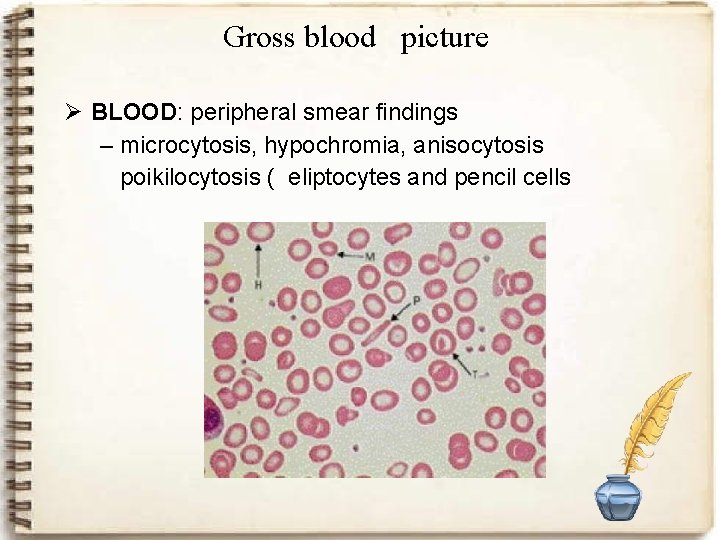
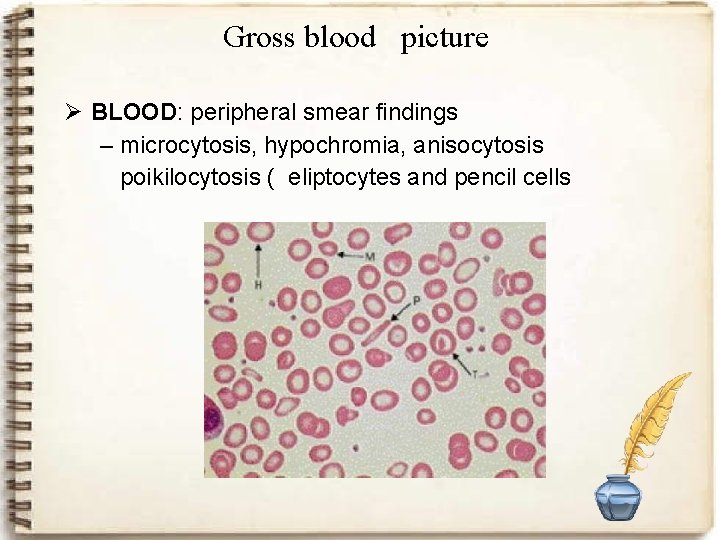
Gross blood picture Ø BLOOD: peripheral smear findings – microcytosis, hypochromia, anisocytosis poikilocytosis ( eliptocytes and pencil cells
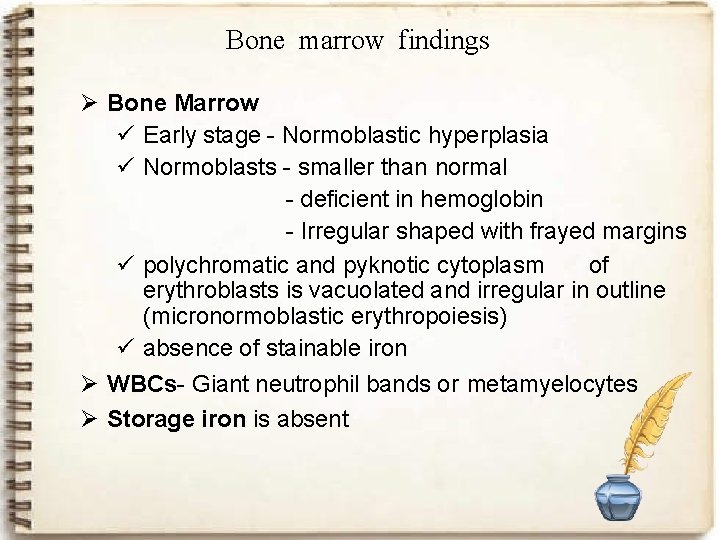
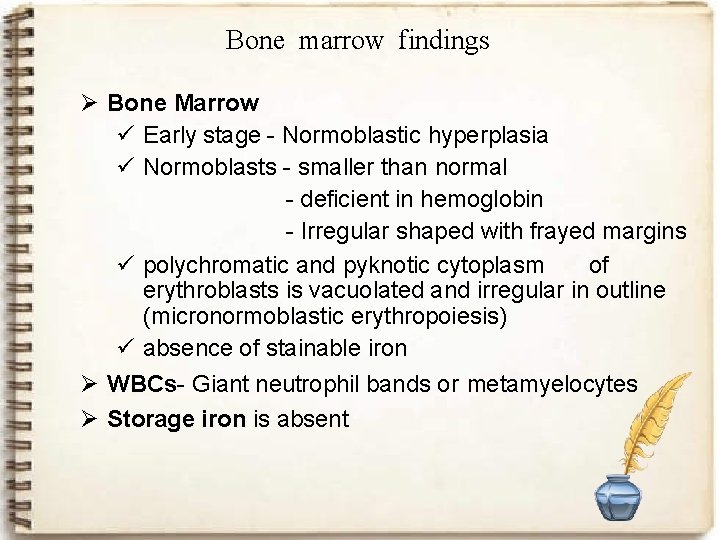
Bone marrow findings Ø Bone Marrow ü Early stage - Normoblastic hyperplasia ü Normoblasts - smaller than normal - deficient in hemoglobin - Irregular shaped with frayed margins ü polychromatic and pyknotic cytoplasm of erythroblasts is vacuolated and irregular in outline (micronormoblastic erythropoiesis) ü absence of stainable iron Ø WBCs- Giant neutrophil bands or metamyelocytes Ø Storage iron is absent
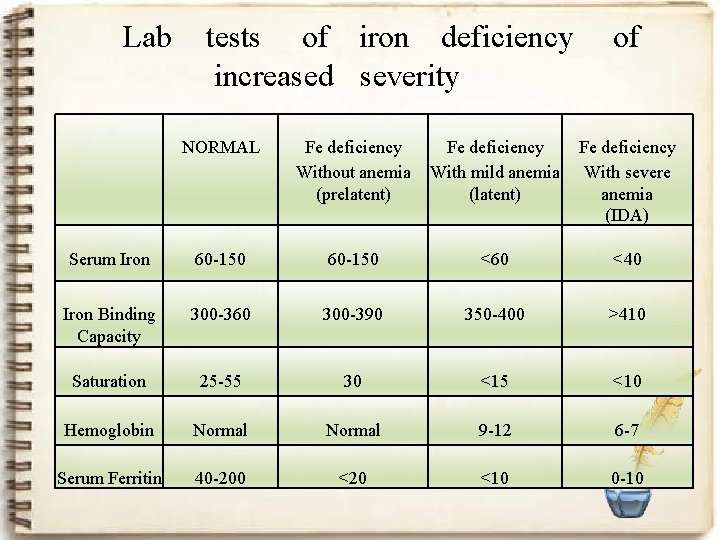
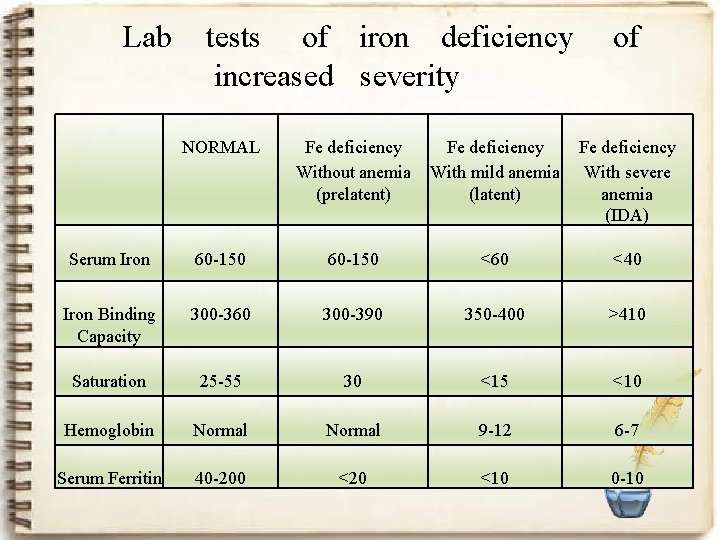
Lab tests of iron deficiency increased severity of NORMAL Fe deficiency Without anemia (prelatent) Fe deficiency With mild anemia (latent) Fe deficiency With severe anemia (IDA) Serum Iron 60 -150 <60 <40 Iron Binding Capacity 300 -360 300 -390 350 -400 >410 Saturation 25 -55 30 <15 <10 Hemoglobin Normal 9 -12 6 -7 Serum Ferritin 40 -200 <20 <10 0 -10
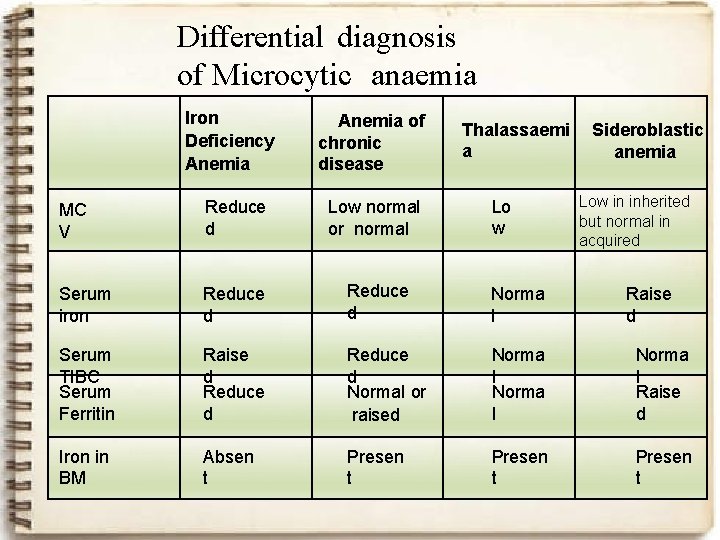
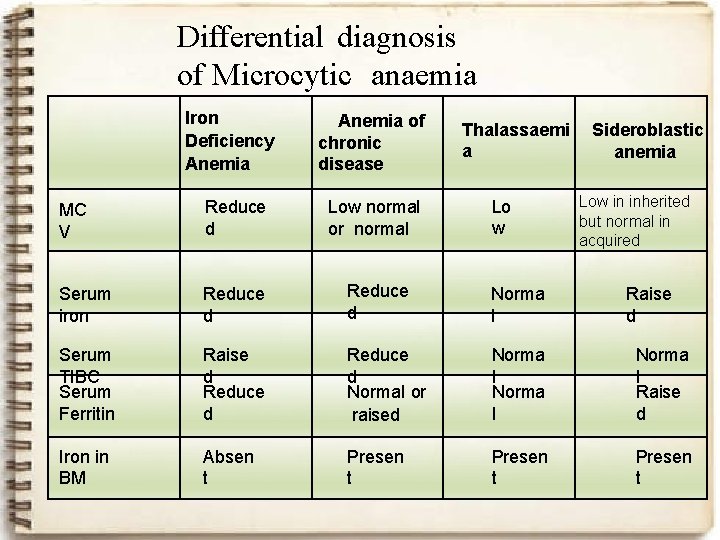
Differential diagnosis of Microcytic anaemia Iron Deficiency Anemia of chronic disease Thalassaemi a Lo w Sideroblastic anemia Low in inherited but normal in acquired MC V Reduce d Low normal or normal Serum iron Reduce d Norma l Serum TIBC Serum Ferritin Raise d Reduce d Normal or raised Norma l Raise d Iron in BM Absen t Presen t Raise d
TREATMENT Ø Iron deficiency anemia is treated with oral or parenteral iron preparation. Ø Oral iron corrects the anemia just as rapidly and completely as parenteral iron in most cases if iron absorption from the GIT is normal. Ø Different iron salt provide different amount of elemental iron. Ø In iron deficient individual, about 50 -80 mg of iron can be incorporated in hemoglobin daily and about 25% of oral ferrous salt can be absorbed. .
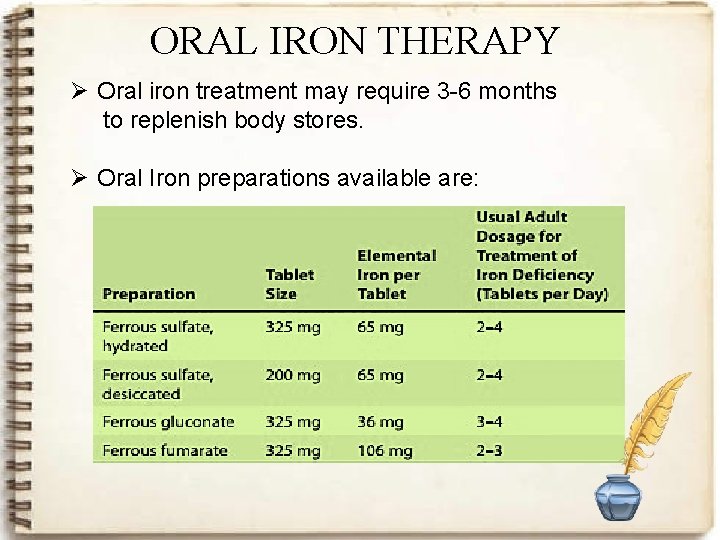
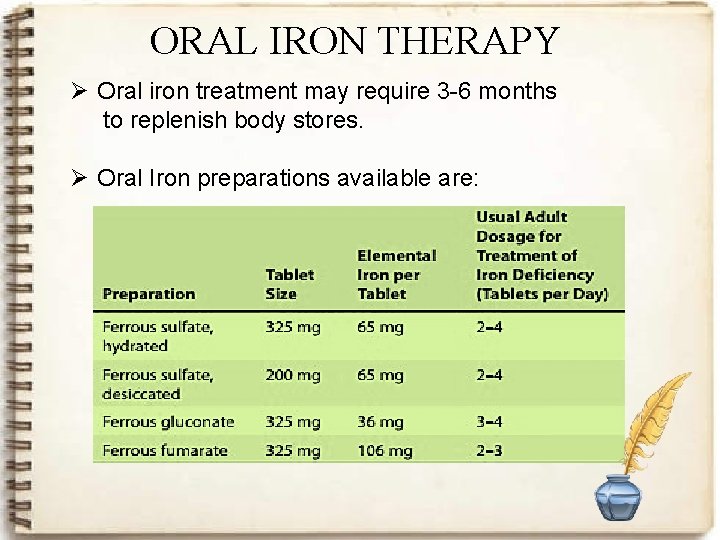
ORAL IRON THERAPY Ø Oral iron treatment may require 3 -6 months to replenish body stores. Ø Oral Iron preparations available are:
q FERROUS ASCORBATE: Ø It is a synthetic molecule of ascorbic acid and iron. Ø Ascorbic acid enhances absorption of iron. Ø It reduces ferric iron to ferrous iron, which remains soluble even at neutral p. H. Ø A significant improvement was seen in Hb levels, signs and symptoms of IDA like fatigue, pallor, breathlessness with FDC of ferrous ascorbate and folic acid. Ø This FDC of ferrous ascorbate and folic acid also showed excellent gastrointestinal tolerability. Ø There are no published studies on efficacy of FDC of ferrous ascorbate and folic acid in the treatment of IDA.
COMMON ADVERSE EFFECTS OF ORAL IRON THERAPY Ø Ø Ø Nausea Epigastric discomfort Abdominal cramps Constipation and diarrhea. Black stool These effects are usually dose-related
CAUTION Ø Avoid taking any other multivitamin or mineral product within 2 hours before or after taking your iron supplement. Ø Avoid antibiotic such as ciprofloxacin, demeclocycline, doxycycline, levofloxacin, lomefloxacin , minocycline , norfloxacin , or tetracycline. Ø Avoid antacids within 2 hours before or after meals when taking your iron medication.
PARENTERAL IRON THERAPY q Indications: Ø Failure to oral therapy Ø Non compliance or intolerance to oral theray Ø Malabsorption or IBD Ø Small bowel resection Ø Cotraindication to blood transfusion Ø Contraindication to oral therapy Ø In combination with recombinant erythropoietin Ø First time seen during last 8 to 10 weeks of pregnancy with severe anemia
PARENTERAL IRON THERAPY PREPARATIONS v Iron Dextran AND iron sorbitolØ contain 50 mg of elemental iron per milliliter of solution. Ø It can be given deep IM injection or IV infusion. Adverse effect: ü light-headedness, fever, arthralgias, ü back pain, urticaria, bronchospasm and ü hypersensitivity reaction
v Iron sucrose complex : Ø These are indicated for patient with hypersensitivity reactions to oral iron salts. Ø Contains 20 mg of elemental iron per ml of solution Ø Route of administration: IV route Ø Caution: For patient who are treated chronically with iron, it is important to monitor the iron level to avoid serious toxicity associated with iron overload. Ø Adverse effect same as iron dextran.
v Ferric carboxymaltose: Ø Ø Ø Contains 50 mg of elemental iron per ml of solution Dose: 15 mg per kg body weight Route of administration: only IV Caution : serious hypersensitivity reaction Adverse reaction: nausea, vomiting , flushing, dizziness , pruritus , rash , hypersensitivity reaction.
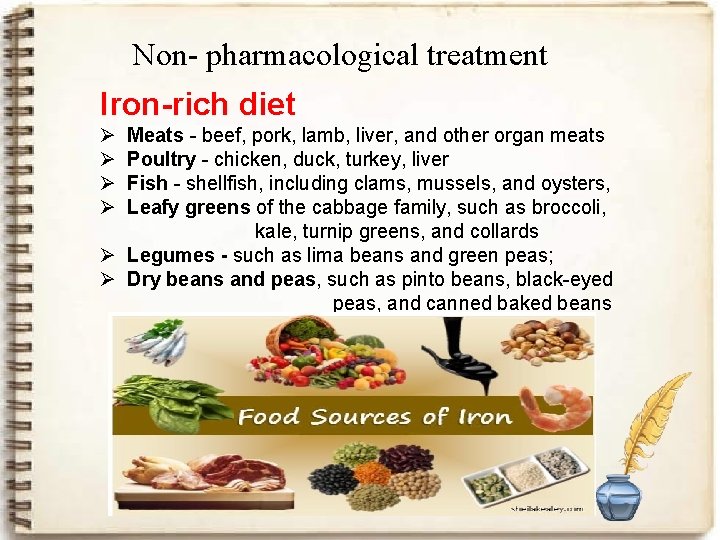
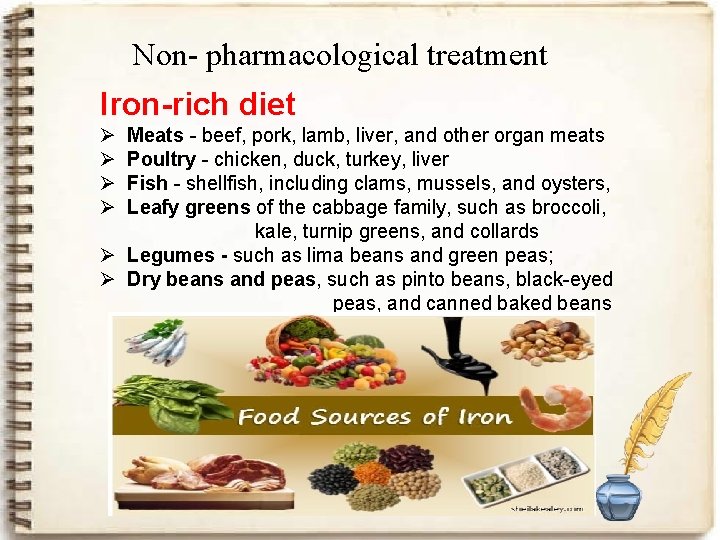
Non- pharmacological treatment Iron-rich diet Ø Ø Meats - beef, pork, lamb, liver, and other organ meats Poultry - chicken, duck, turkey, liver Fish - shellfish, including clams, mussels, and oysters, Leafy greens of the cabbage family, such as broccoli, kale, turnip greens, and collards Ø Legumes - such as lima beans and green peas; Ø Dry beans and peas, such as pinto beans, black-eyed peas, and canned baked beans
Thank You