IOL DISLOCATION AFTER VITREORETINAL PLUS PHACO SURGERY DEPENDING
- Slides: 1
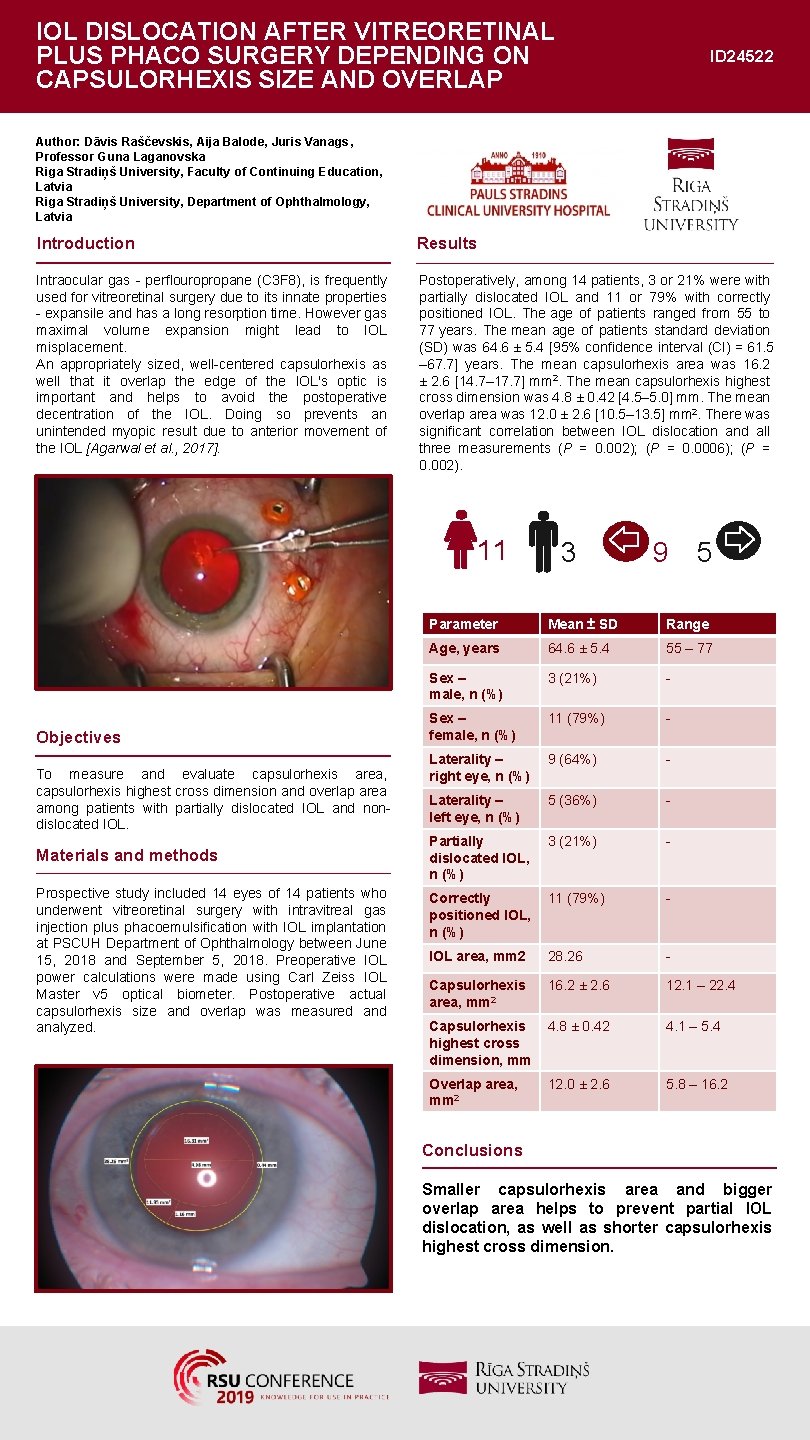
IOL DISLOCATION AFTER VITREORETINAL PLUS PHACO SURGERY DEPENDING ON CAPSULORHEXIS SIZE AND OVERLAP ID 24522 Author: Dāvis Raščevskis, Aija Balode, Juris Vanags , Professor Guna Laganovska Riga Stradiņš University, Faculty of Continuing Education, Latvia Riga Stradiņš University, Department of Ophthalmology, Latvia Introduction Results Intraocular gas - perflouropropane (C 3 F 8), is frequently used for vitreoretinal surgery due to its innate properties - expansile and has a long resorption time. However gas maximal volume expansion might lead to IOL misplacement. An appropriately sized, well-centered capsulorhexis as well that it overlap the edge of the IOL's optic is important and helps to avoid the postoperative decentration of the IOL. Doing so prevents an unintended myopic result due to anterior movement of the IOL [Agarwal et al. , 2017]. Postoperatively, among 14 patients, 3 or 21% were with partially dislocated IOL and 11 or 79% with correctly positioned IOL. The age of patients ranged from 55 to 77 years. The mean age of patients standard deviation (SD) was 64. 6 ± 5. 4 [95% confidence interval (CI) = 61. 5 – 67. 7] years. The mean capsulorhexis area was 16. 2 ± 2. 6 [14. 7– 17. 7] mm 2. The mean capsulorhexis highest cross dimension was 4. 8 ± 0. 42 [4. 5– 5. 0] mm. The mean overlap area was 12. 0 ± 2. 6 [10. 5– 13. 5] mm 2. There was significant correlation between IOL dislocation and all three measurements (P = 0. 002); (P = 0. 0006); (P = 0. 002). 11 Objectives To measure and evaluate capsulorhexis area, capsulorhexis highest cross dimension and overlap area among patients with partially dislocated IOL and nondislocated IOL. Materials and methods Prospective study included 14 eyes of 14 patients who underwent vitreoretinal surgery with intravitreal gas injection plus phacoemulsification with IOL implantation at PSCUH Department of Ophthalmology between June 15, 2018 and September 5, 2018. Preoperative IOL power calculations were made using Carl Zeiss IOL Master v 5 optical biometer. Postoperative actual capsulorhexis size and overlap was measured analyzed. 3 9 5 Parameter Mean ± SD Range Age, years 64. 6 ± 5. 4 55 – 77 Sex – male, n (%) 3 (21%) - Sex – female, n (%) 11 (79%) - Laterality – right eye, n (%) 9 (64%) - Laterality – left eye, n (%) 5 (36%) - Partially dislocated IOL, n (%) 3 (21%) - Correctly positioned IOL, n (%) 11 (79%) - IOL area, mm 2 28. 26 - Capsulorhexis area, mm 2 16. 2 ± 2. 6 12. 1 – 22. 4 Capsulorhexis highest cross dimension, mm 4. 8 ± 0. 42 4. 1 – 5. 4 Overlap area, mm 2 12. 0 ± 2. 6 5. 8 – 16. 2 Conclusions Smaller capsulorhexis area and bigger overlap area helps to prevent partial IOL dislocation, as well as shorter capsulorhexis highest cross dimension.