Iodine Supplementation an overview Kate Jolly Professor of


![Methods 1: Decision tree The model is identical at every node ending with [+] Methods 1: Decision tree The model is identical at every node ending with [+]](https://slidetodoc.com/presentation_image/1ce75f440bf22996d5091e991e0528b6/image-12.jpg)

- Slides: 17
Iodine Supplementation: an overview Kate Jolly Professor of Public Health & Primary Care University of Birmingham

Methods of iodine supplementation • Salt fortification with iodine – Universal: fortification of all salt for human and animal consumption (USI) – Fortification of all salt for human consumption – Fortification of salt used in certain foodstuffs e. g. bread
Methods of iodine supplementation • Fortification of animal fodder (Finland) • Accidental by product of iodophores used in dairy industry • Iodised oil • Iodised water, sugar, tea… • Oral supplements for pregnant or lactating mothers - (where <90% of households are using iodised salt and median UI is <100µg/l in school children)
Current UK guidance for pregnancy supplements • Recommended supplements: – 400 µg folic acid from before pregnant until 12 weeks pregnant – 10 µg vitamin D daily throughout pregnancy • Do not take vitamin A • Healthy Start vitamins available from 10 weeks gestation – contain folic acid; vitamins C and D • Iodine guidance – SACN recommend no increase in iodine intake during pregnancy: 140 µg/day – WHO recommend 250 µg intake daily
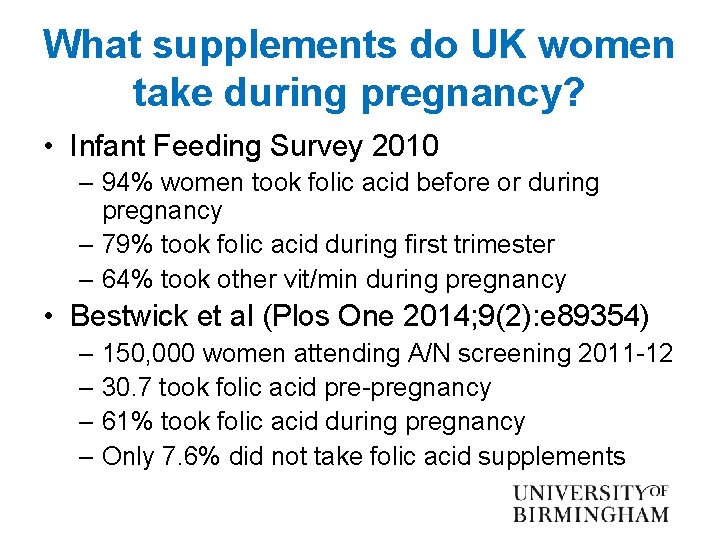
What supplements do UK women take during pregnancy? • Infant Feeding Survey 2010 – 94% women took folic acid before or during pregnancy – 79% took folic acid during first trimester – 64% took other vit/min during pregnancy • Bestwick et al (Plos One 2014; 9(2): e 89354) – 150, 000 women attending A/N screening 2011 -12 – 30. 7 took folic acid pre-pregnancy – 61% took folic acid during pregnancy – Only 7. 6% did not take folic acid supplements
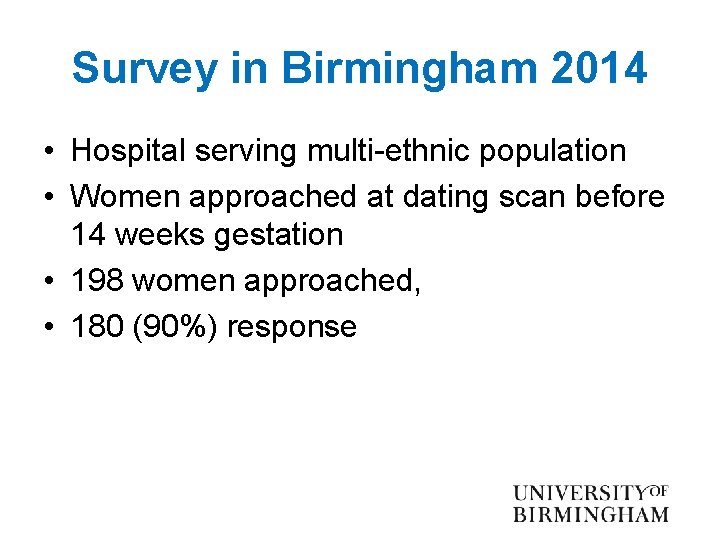
Survey in Birmingham 2014 • Hospital serving multi-ethnic population • Women approached at dating scan before 14 weeks gestation • 198 women approached, • 180 (90%) response

The sample • Age – 12 (6. 7%) <20 years – 157 (87. 2%) 20 -40 years – 11 (6. 1%) >40 years • Post school education 80 (44. 4%) • First pregnancy 69 (38. 3%) • Ethnic group – 72 (40. 0%) white – 60 (33. 3%) South Asian • English not first language 56 (31. 1%) • Born in UK 118 (65. 6%)
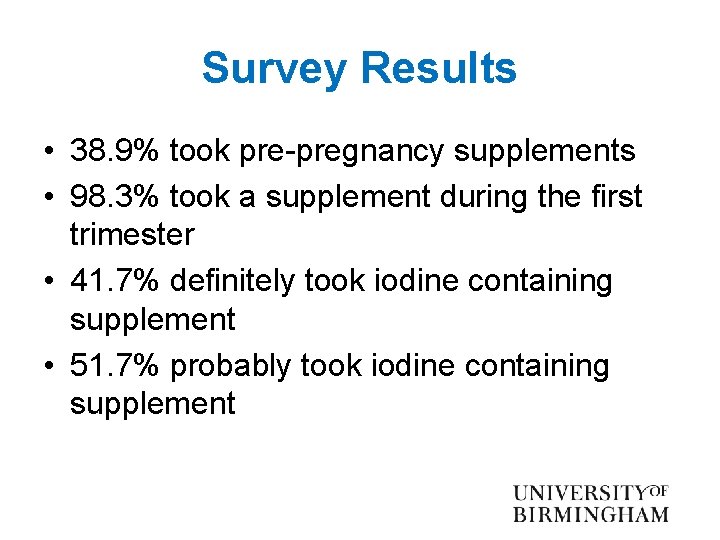
Survey Results • 38. 9% took pre-pregnancy supplements • 98. 3% took a supplement during the first trimester • 41. 7% definitely took iodine containing supplement • 51. 7% probably took iodine containing supplement
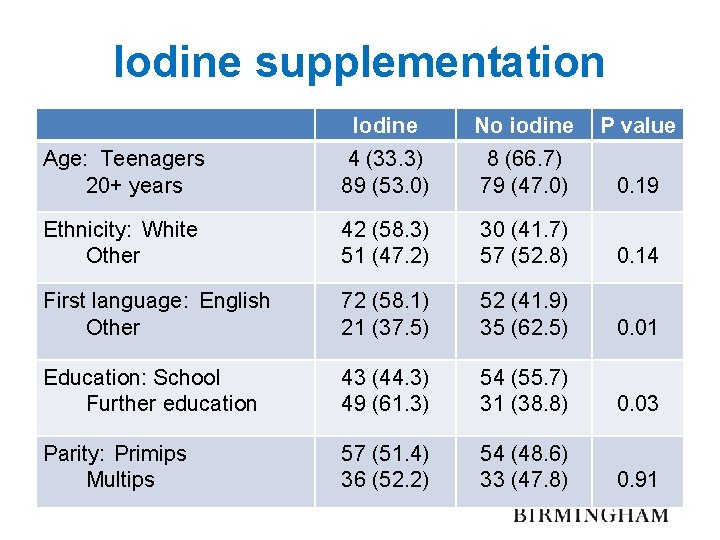
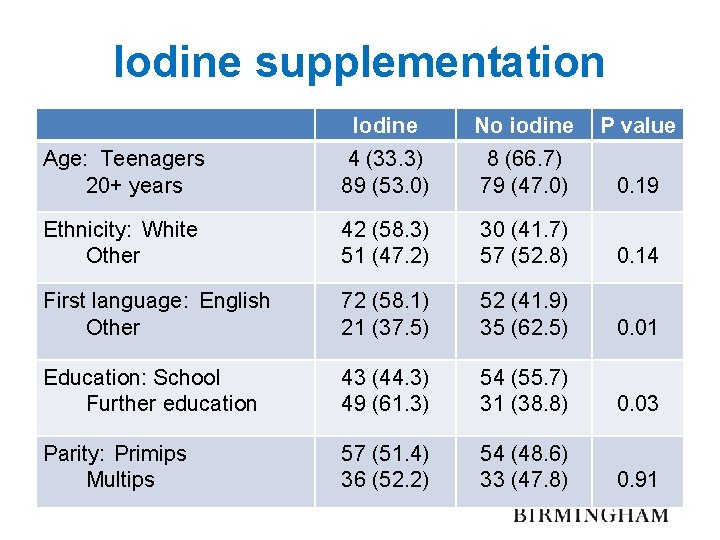
Iodine supplementation Iodine No iodine P value Age: Teenagers 20+ years 4 (33. 3) 89 (53. 0) 8 (66. 7) 79 (47. 0) 0. 19 Ethnicity: White Other 42 (58. 3) 51 (47. 2) 30 (41. 7) 57 (52. 8) 0. 14 First language: English Other 72 (58. 1) 21 (37. 5) 52 (41. 9) 35 (62. 5) 0. 01 Education: School Further education 43 (44. 3) 49 (61. 3) 54 (55. 7) 31 (38. 8) 0. 03 Parity: Primips Multips 57 (51. 4) 36 (52. 2) 54 (48. 6) 33 (47. 8) 0. 91
Costs & benefits of iodine supplementation for pregnant women in mildly iodine deficient population Monahan M, Boelaert K, Jolly K, Chan S, Barton P, Roberts T Lancet Diabetes and Endocrinology 2015; 3(9): 712 -722
Aims and Approach • To compare the costs and benefits of a strategy of iodine supplementation for pregnant women in a mild to moderately iodine deficient population against no iodine supplementation • A model based analysis • Assumptions aimed to limit the benefits of iodine supplementation and over-estimate potential harms
![Methods 1 Decision tree The model is identical at every node ending with Methods 1: Decision tree The model is identical at every node ending with [+]](https://slidetodoc.com/presentation_image/1ce75f440bf22996d5091e991e0528b6/image-12.jpg)
Methods 1: Decision tree The model is identical at every node ending with [+]
Assumptions relating to iodine • IQ gain taken from Bath et al – 2. 2 points in mild/mod deficiency – 3. 0 points in children of severely deficient mothers • Prevalence of deficiency 68% (Vanderpump) • 11% of those with deficiency were severely deficient (Bath) • Women took iodine supplements from early pregnancy until cessation of exclusive breastfeeding

Assumptions relating to pregnancy losses and complications • Estimates from literature of pregnancy loss, stillbirth, preterm birth and pre-eclampsia • Increased risk of thyroid dysfunction from iodine supplementation 0. 25% (EC 2002) • IQ loss from hypothyroidism and hyperthyroxinaemia: 7 points (Haddow) • Estimates of increased pregnancy loss, stillbirth, preterm birth and pre-eclampsia from thyroid dysfunction
Findings • NHS perspective: a saving of £ 199 per/women supplemented & 1. 22 IQ points gained • Societal perspective: a saving of £ 4476/women & 1. 22 IQ points gained • Iodine supplementation dominated the sensitivity analyses: – IQ gain for severe deficiency same as mild/mod – 1 IQ point gain for mild/mod deficiency – Halved prevalence of iodine deficiency – Doubled cost of iodine tablets….
Limitations • IQ gains could lead to shift in population norms, so relative differences remain • Uncertainty over the precise estimation of the impact of IQ on earnings. NHS perspective did not use this earnings based IQ value but still shows cost saving • Iodine status at individual level would strengthen argument and avoid unnecessary supplementation • Lack of evidence of potential harms
Conclusions • Currently only about half of women take iodine supplements in pregnancy • Lower in more socio-economically disadvantaged • Policy for all pregnant women to take iodine supplements cost effectiveassuming IQ gains seen in Bath et al (2011) and prevalence of deficiency from Vanderpump et al (2011)
 Kate jolly
Kate jolly Kate jolly
Kate jolly Erratic
Erratic Kate del castillo kate trillo del castillo
Kate del castillo kate trillo del castillo Mutual supplementation
Mutual supplementation Promotion from associate professor to professor
Promotion from associate professor to professor Jolly phonics n
Jolly phonics n Boykov and jolly 2001
Boykov and jolly 2001 Jolly phonics
Jolly phonics Heinz bodies
Heinz bodies Jolly character in waltzing matilda
Jolly character in waltzing matilda Oecd space forum
Oecd space forum Simon jolly
Simon jolly Jolly phonics b
Jolly phonics b How did blackbeard die
How did blackbeard die Jolly med
Jolly med Elks care elks share
Elks care elks share Cuerpos de howell-jolly causas
Cuerpos de howell-jolly causas