Investigations Urine examination Serum K Serum creatinine Blood
Investigations: • Urine examination. • Serum K. • Serum creatinine. • Blood Sugar. • Hb.

Investigations: • Serum uric acid. • Lipid profile. • ECG. • Fundus. • More extensive investigations are needed in secondary hypertension.
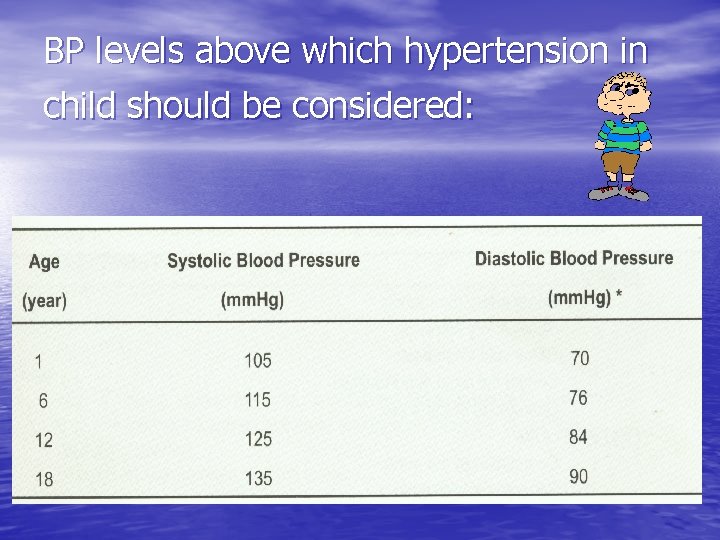
BP levels above which hypertension in child should be considered:
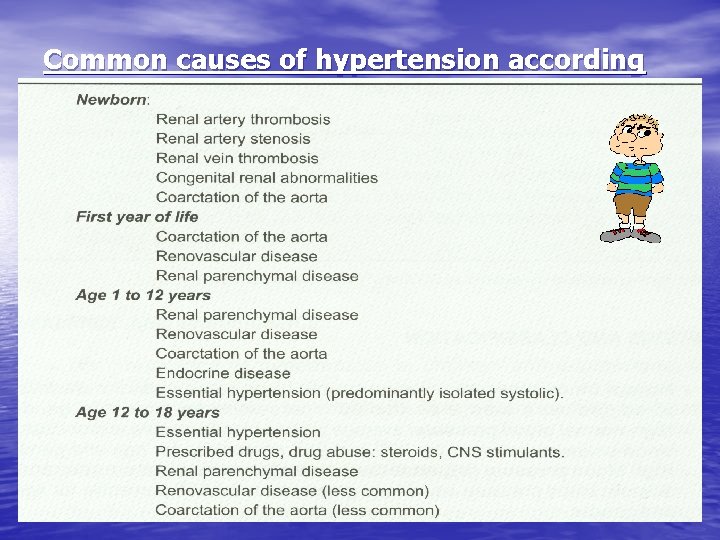
Common causes of hypertension according to age
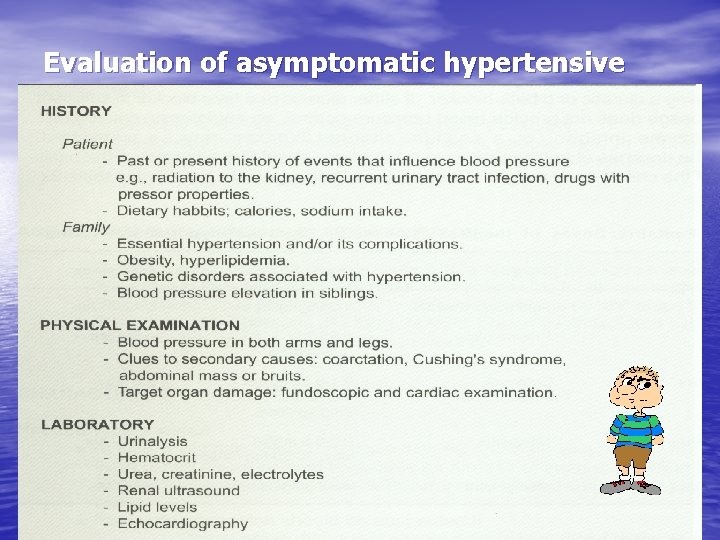
Evaluation of asymptomatic hypertensive child:
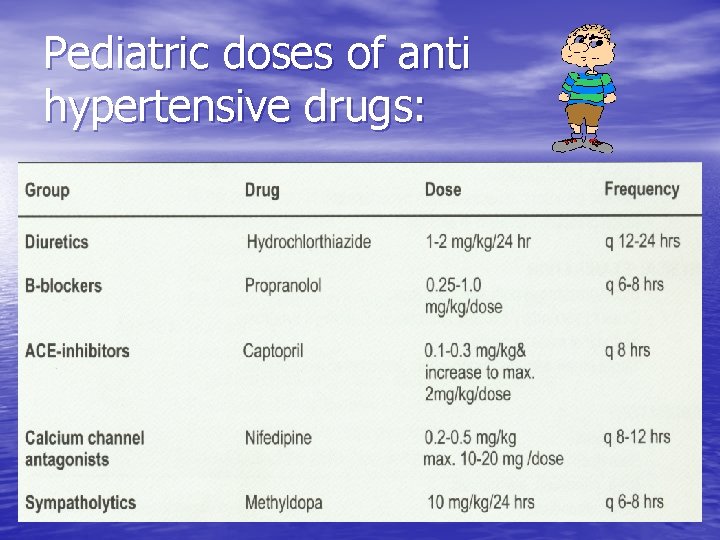
Pediatric doses of anti hypertensive drugs:
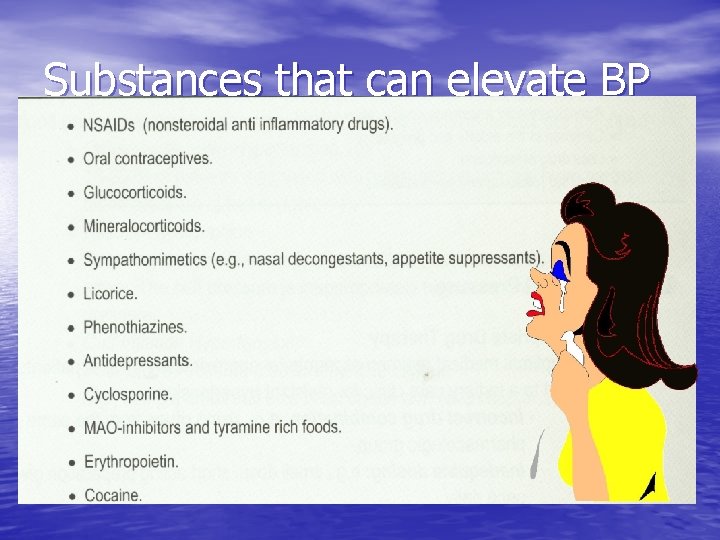
Substances that can elevate BP
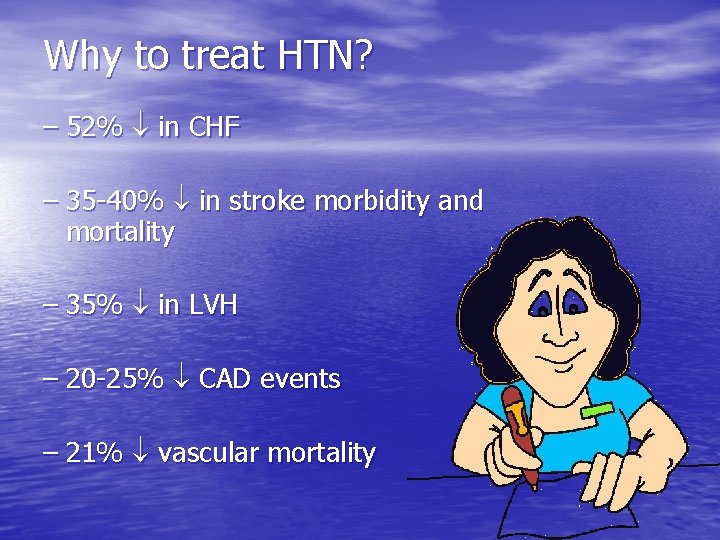
Why to treat HTN? – 52% in CHF – 35 -40% in stroke morbidity and mortality – 35% in LVH – 20 -25% CAD events – 21% vascular mortality
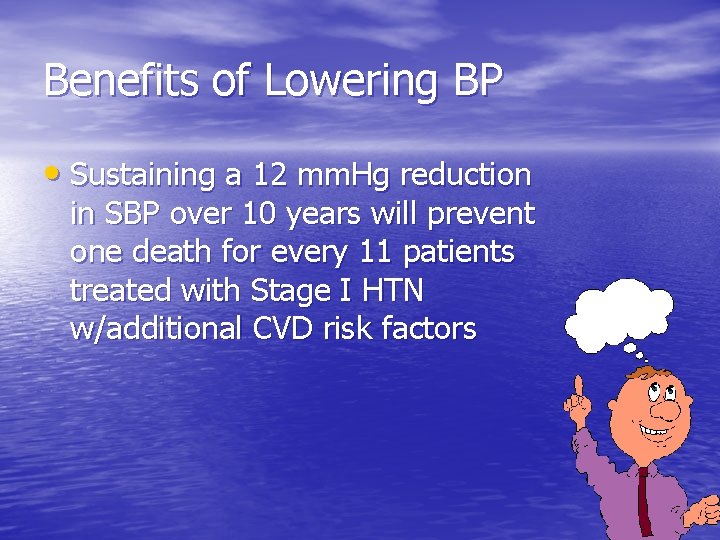
Benefits of Lowering BP • Sustaining a 12 mm. Hg reduction in SBP over 10 years will prevent one death for every 11 patients treated with Stage I HTN w/additional CVD risk factors
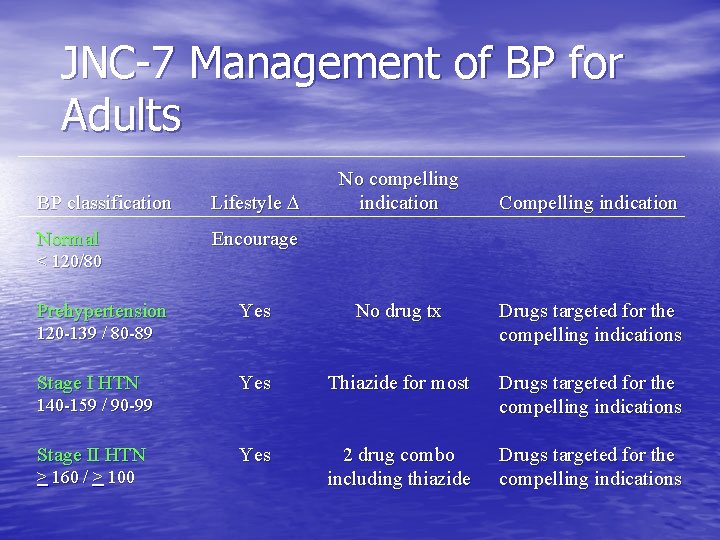
JNC-7 Management of BP for Adults BP classification Lifestyle Normal Encourage No compelling indication Compelling indication < 120/80 Prehypertension Yes No drug tx Drugs targeted for the compelling indications Yes Thiazide for most Drugs targeted for the compelling indications Yes 2 drug combo including thiazide Drugs targeted for the compelling indications 120 -139 / 80 -89 Stage I HTN 140 -159 / 90 -99 Stage II HTN > 160 / > 100

Treatment Outline • Goals of Therapy • Lifestyle modification • Pharmacologic treatment • Follow-up and monitoring
Goals of Therapy • Reduce CVD and renal morbidity and mortality • Treat to BP < 140/90 mm. Hg or BP <130/80 mm. Hg in patients with DM or less in patients with chronic KD

Goals of Therapy • Achieve BP goal especially in persons > 50 years of age • Maintain QOL • Minimize side effects
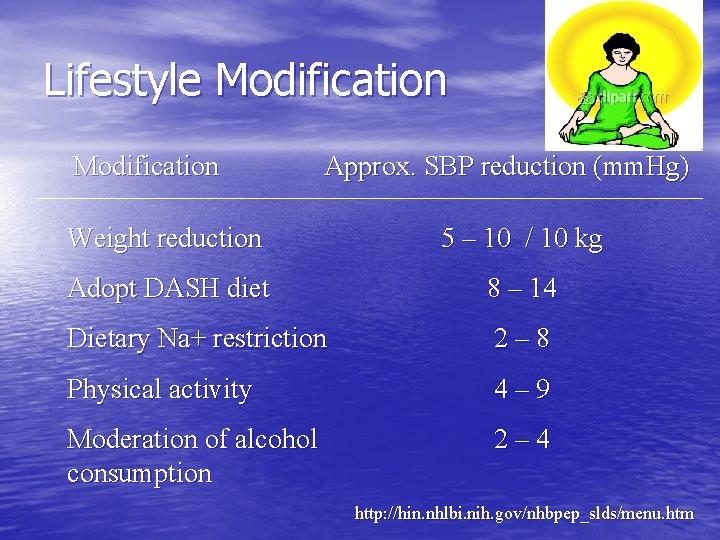
Lifestyle Modification Approx. SBP reduction (mm. Hg) Weight reduction 5 – 10 / 10 kg Adopt DASH diet 8 – 14 Dietary Na+ restriction 2– 8 Physical activity 4– 9 Moderation of alcohol consumption 2– 4 http: //hin. nhlbi. nih. gov/nhbpep_slds/menu. htm
Lifestyle Modification • Works best in motivated individuals • Initiate at prehypertension classification • Obesity risk for HTN and DM • If > 20% over ideal body weight (IBW) – considered obese – Decrease intake by 500 cal/day – Increase exercise and activity
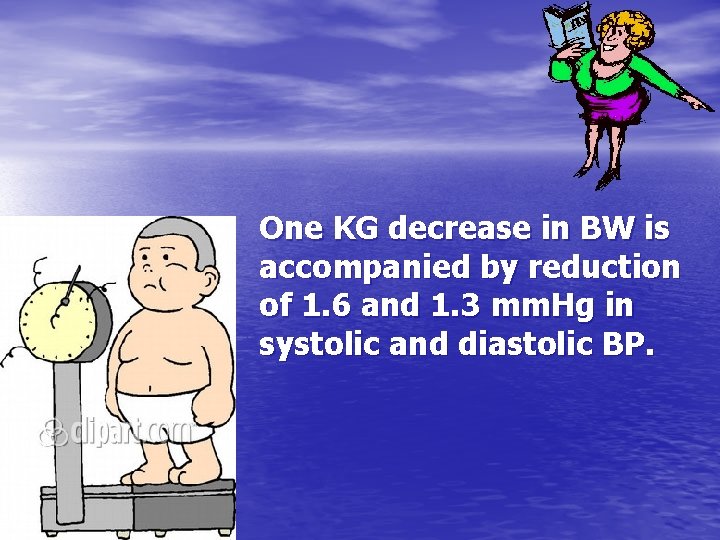
One KG decrease in BW is accompanied by reduction of 1. 6 and 1. 3 mm. Hg in systolic and diastolic BP.
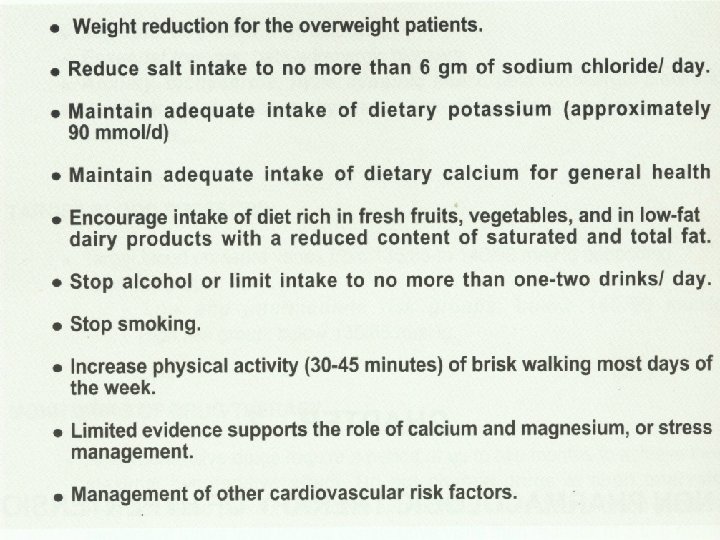
Salt sensitivity is more common in: • Elderly. • Blacks. • Type 1 diabetes. • Secondary hypertension.
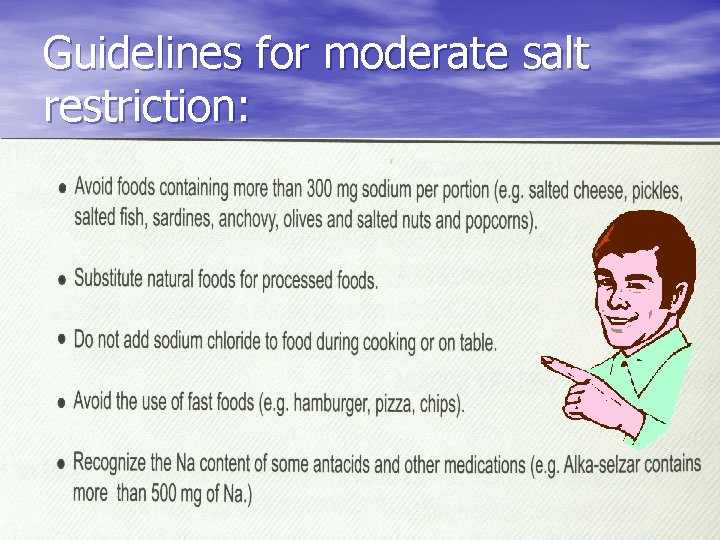
Guidelines for moderate salt restriction:
Dietary potassium: • Diet rich in fruits and vegetables is superior to pills. • Potassium supplements should be avoided in: renal insufficiency, with diuretics, ACE inhibitors or ARBs.

Food rich in potassium:
- Slides: 22