Introduction to Verbal Program HWCs Verbal Program HWCs
Introduction to Verbal Program
HWC’s Verbal Program § HWC’s Philosophy § Tension-Tension Reduction Cycle (T/TRC) § Soild Object Relationship Model (SORM) § Role Plays
HWC’s Philosophy Handle With Care’s entire program is dedicated to the reduction of violence through: § Tension Reduction Staff’s use of preventative actions that result in a decrease in the need for the use of escalated interventions such as calling 911 § Creating a universal perception of physical and psychological safety in the clinics
HWC’s Philosophy All verbal interventions operate from the following assumptions: § There is no dignity in allowing a patient to hurt him/herself or someone else § Staff safety and patient safety are equally important § Patient’s sometimes need assistance in protecting themselves from the consequences of their behavior
HWC’s Philosophy § In order to act in the patient’s best interest, staff need to be in control of our own feelings and behaviors § The out of control patient is generally aware at some level that they are out of control § The out of control patient expects staff to demonstrate the capacity to help them manage their feelings safely § A person in crisis will know the difference between something done for them and something done to them only if we are clear about it first

Comprehensive Verbal Skills Workshop 6
The Tension / Tension Reduction Cycle Purpose / Goal Understanding the dynamics of escalating and de-escalating tension
The Tension / Tension Reduction Cycle § The T/TRC is a theoretical model HWC uses to illustrate the dynamics of escalating and de-escalating tension. It is based on an eastern philosophical perspective of balanced but opposing universal forces, i. e. , tension/relaxation § There are essentially three phases of escalation a person goes through 1) Early - Low level of tension or anxiety 2) Middle - The window or opportunity to de-escalate without higher intervention (911) 3) Violence - Not everyone reaches the highest level of aggression, but should we miss the opportunity to de-escalate, higher level of intervention (ie. calling 911) will be necessary to keep the patient, staff, and other patients safe
The Tension / Tension Reduction Cycle § T/TRC teaches staff how to recognize signs for each level of behavior/aggression so that (1) staff can appropriately calibrate their level of response, and (2) recognize the signs of increasing tension/conflict so that they can intervene earlier in the tension/conflict cycle § The T/TRC is a timing model, not a time dependent model i. e. some individuals accelerate rapidly, and others over an extended period of time § As a timing model, the T/TRC teaches staff how to recognize when tension levels are rising and “time” their intervention to match the level of tension presented
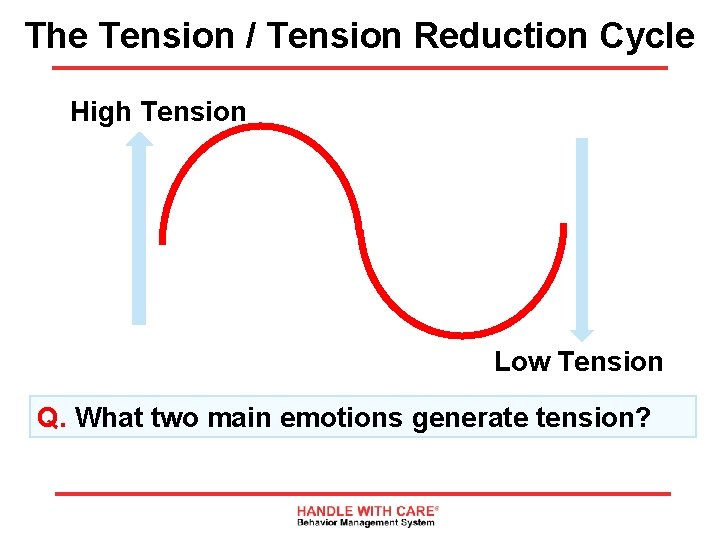
The Tension / Tension Reduction Cycle High Tension Low Tension Q. What two main emotions generate tension?
The Tension / Tension Reduction Cycle Answer: Anger Fear These emotions can be the result of both internally and externally produced conflicts
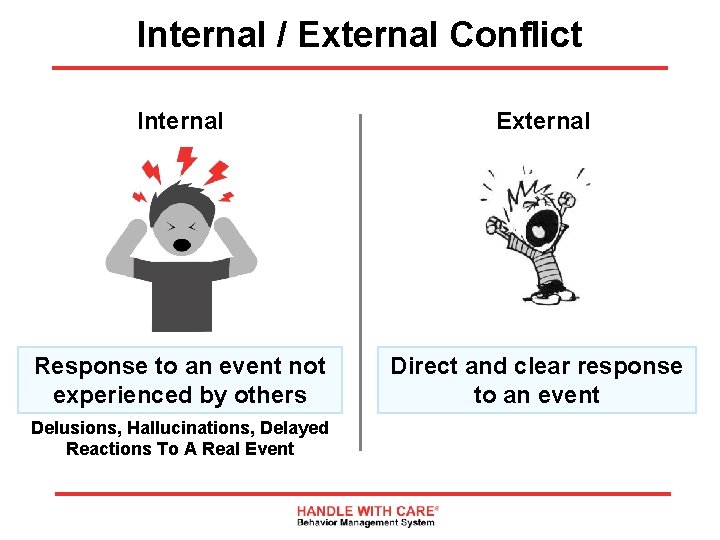
Internal / External Conflict Internal External Response to an event not experienced by others Direct and clear response to an event Delusions, Hallucinations, Delayed Reactions To A Real Event
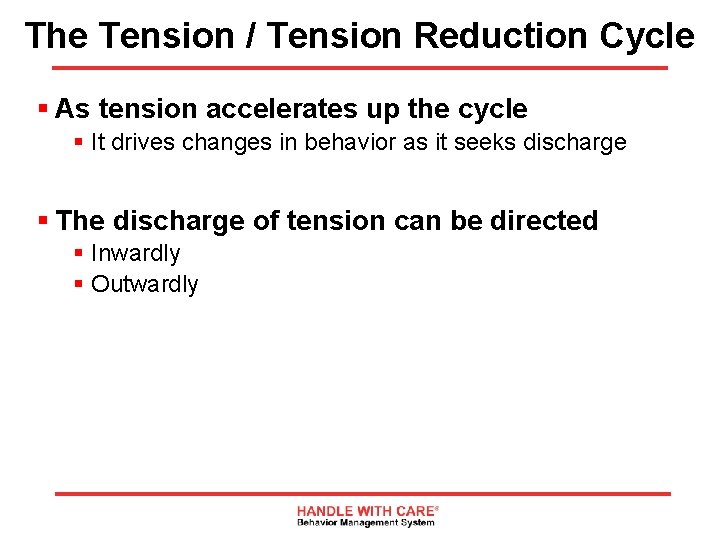
The Tension / Tension Reduction Cycle § As tension accelerates up the cycle § It drives changes in behavior as it seeks discharge § The discharge of tension can be directed § Inwardly § Outwardly
Tension Released Inwardly Features of an inwardly directed or delayed style of discharging tension § Acceleration tends to be more gradual § Social withdrawal marked by: § § Decrease in motor activity Speech production Avoidance of eye contact Quiet and withdrawn, moody § Ruminating or repeating thoughts with depressive, suicidal or violent themes § Clinically depressed
Tension Released Outwardly Features of outwardly directed or immediate style of discharging tension: § Acceleration is more rapid, impulsive and usually over a short timeframe § History of discharging tension in negative ways § Instigating others to the above Most people fall into one of the two styles of discharging tension; some can have features of both 15
The Discharge of Tension can be: 1. Immediate 2. Delayed 3. Both Q. Which is more dangerous?
Who is more dangerous? A: Most people will answer, the inwardly/delayed Q. Why? § They tend to attract less attention if they are quiet and withdrawn whereas the immediate style attracts staff intervention earlier in the cycle because of the clearer signals i. e. pacing and other behaviors § A person who becomes more outwardly agitated creates more opportunities to “bleed off” tension, which in turn provide opportunities for therapeutic intervention. The delayed style “holds onto” tension
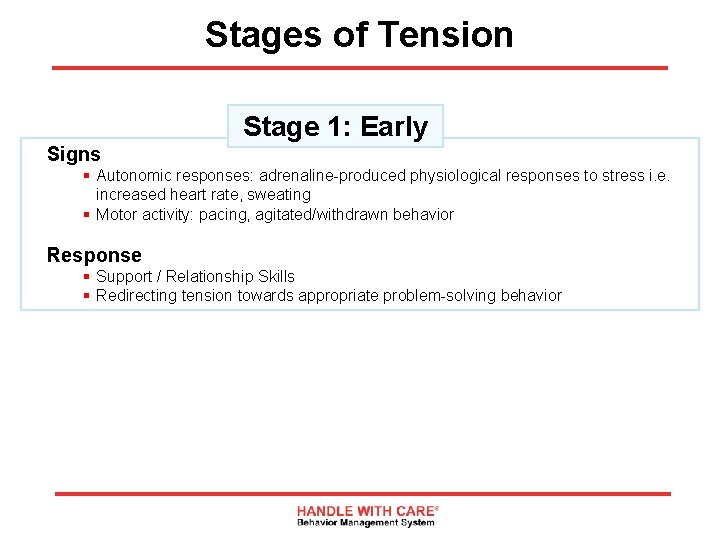
Stages of Tension Stage 1: Early Signs § Autonomic responses: adrenaline-produced physiological responses to stress i. e. increased heart rate, sweating § Motor activity: pacing, agitated/withdrawn behavior Response § Support / Relationship Skills § Redirecting tension towards appropriate problem-solving behavior
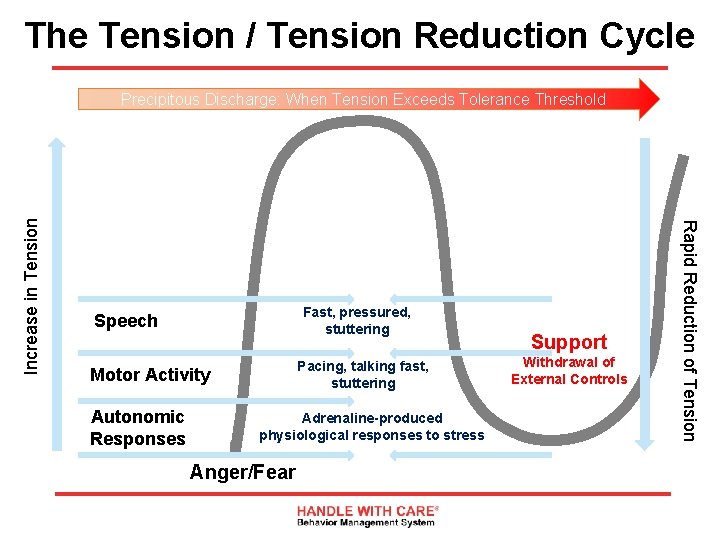
The Tension / Tension Reduction Cycle Fast, pressured, stuttering Speech Pacing, talking fast, stuttering Motor Activity Autonomic Responses Support Withdrawal of External Controls Adrenaline-produced physiological responses to stress Anger/Fear 19 Rapid Reduction of Tension Increase in Tension Precipitous Discharge: When Tension Exceeds Tolerance Threshold
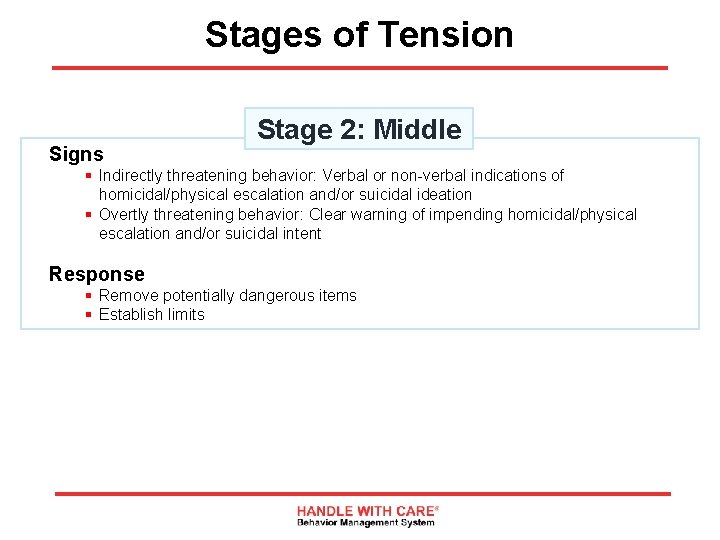
Stages of Tension Signs Stage 2: Middle § Indirectly threatening behavior: Verbal or non-verbal indications of homicidal/physical escalation and/or suicidal ideation § Overtly threatening behavior: Clear warning of impending homicidal/physical escalation and/or suicidal intent Response § Remove potentially dangerous items § Establish limits
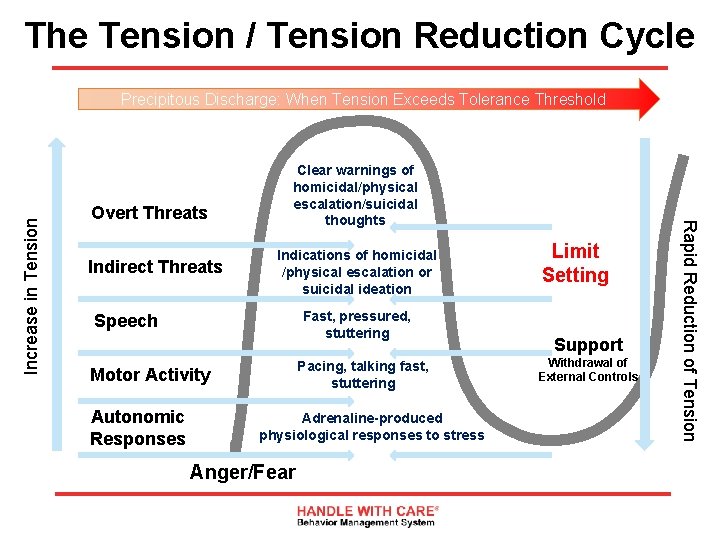
The Tension / Tension Reduction Cycle Overt Threats Indirect Threats Clear warnings of homicidal/physical escalation/suicidal thoughts Indications of homicidal /physical escalation or suicidal ideation Fast, pressured, stuttering Speech Pacing, talking fast, stuttering Motor Activity Autonomic Responses Limit Setting Support Withdrawal of External Controls Adrenaline-produced physiological responses to stress Anger/Fear 21 Rapid Reduction of Tension Increase in Tension Precipitous Discharge: When Tension Exceeds Tolerance Threshold
Stages of Tension Signs Stage 3: Violence / Physical Aggression § Obvious: This is the point when tension is about to exceed tolerance threshold Response § Call 911 and alert other staff; make sure other patients are safe
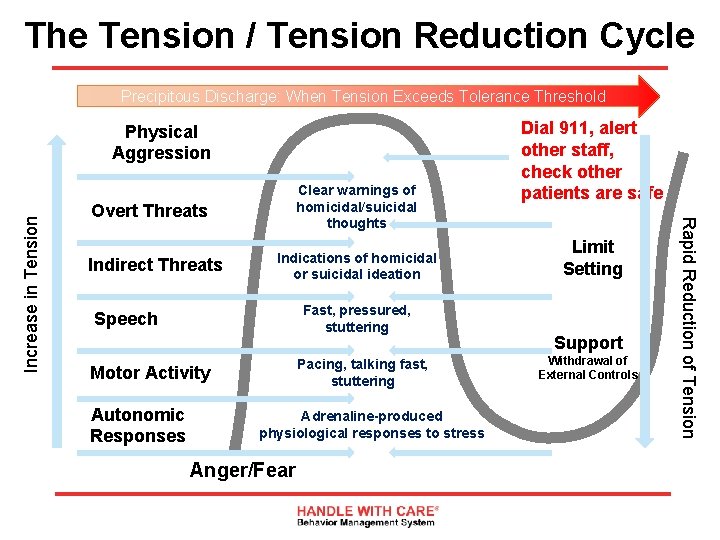
The Tension / Tension Reduction Cycle Precipitous Discharge: When Tension Exceeds Tolerance Threshold Clear warnings of homicidal/suicidal thoughts Overt Threats Indirect Threats Indications of homicidal or suicidal ideation Fast, pressured, stuttering Speech Pacing, talking fast, stuttering Motor Activity Autonomic Responses Dial 911, alert other staff, check other patients are safe Limit Setting Support Withdrawal of External Controls Adrenaline-produced physiological responses to stress Anger/Fear 23 Rapid Reduction of Tension Increase in Tension Physical Aggression
Solid Object Relationship Model Bringing Crisis Into Balance
SORM Assumptions Assumption No. 1 § An angry or fearful person in crisis is “aware” of his emotional instability and instinctively seeks equilibrium by holding on to or “attaching” himself to a more stable object or person § Example: If I suddenly pushed you from behind, you’d instinctively try to hold on to something – anything –rather than fall down § Predictably, a patient in crisis “tests” the emotional solidity of the people (objects) around them by activating anger and fear responses § HWC’s Verbal Program motivates staff to identify their emotional liabilities in a crisis and learn how to manage them
SORM Assumptions Assumption No. 2 § A person who is out of control is aware at some level that they are out of control and expects staff to demonstrate the capacity to help them manage their feelings safely
Identifying a Solid Object Setting the stage: § You have a patient who is emotionally out-of-control and being dealt with by several staff. Out of all the staff members dealing with the situation the individual focuses his attention on one particular staff member and immediately starts to calm down. You notice that this occurs in almost every crisis this staff member is involved in Q. What qualities does this staff member demonstrate?
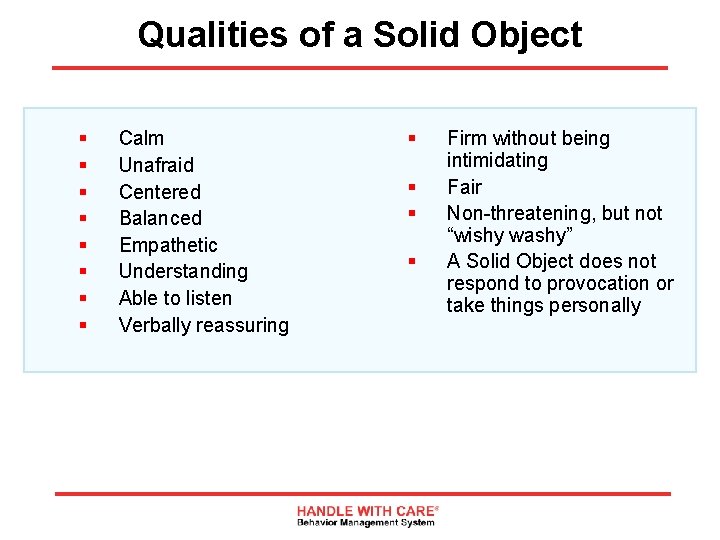
Qualities of a Solid Object § § § § Calm Unafraid Centered Balanced Empathetic Understanding Able to listen Verbally reassuring § § Firm without being intimidating Fair Non-threatening, but not “wishy washy” A Solid Object does not respond to provocation or take things personally
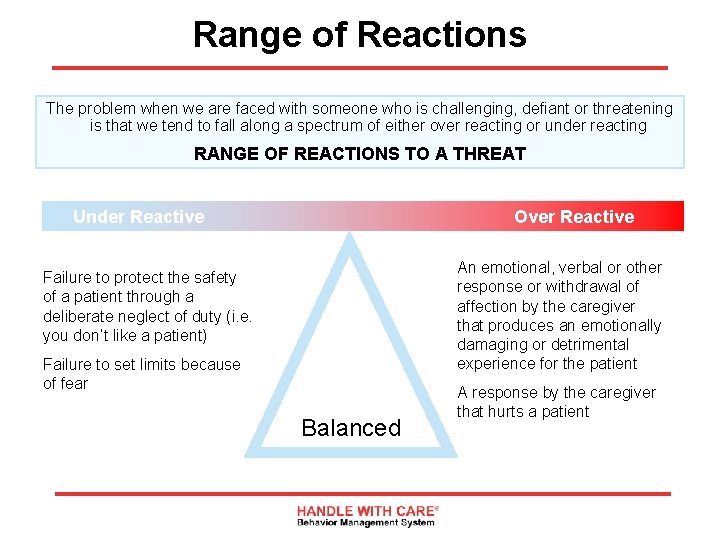
Range of Reactions The problem when we are faced with someone who is challenging, defiant or threatening is that we tend to fall along a spectrum of either over reacting or under reacting RANGE OF REACTIONS TO A THREAT Under Reactive Over Reactive An emotional, verbal or other response or withdrawal of affection by the caregiver that produces an emotionally damaging or detrimental experience for the patient Failure to protect the safety of a patient through a deliberate neglect of duty (i. e. you don’t like a patient) Failure to set limits because of fear Balanced A response by the caregiver that hurts a patient
Transference and Countertransference The production of positive or negative feelings about individuals is a phenomenon in psychoanalysis characterized by unconscious redirection of feelings for one person to another § React to others as if they were someone else § The transfer of associations or past experiences to this person Countertransference The same as the above except the feelings are transferred from the staff to the patient. A staff person’s attunement to his/her own counter-transference is nearly as critical as understanding the transference. Not only does this help the staff regulate their emotions in therapeutic relationship, but it also gives the staff valuable insight into what the patient is attempting to elicit in them
Nonverbal and Verbal Intervention Techniques Putting the pieces together 31
Keys to De-escalation The key to de-escalation is your relationship with the patient § Form a relationship by behaving as a solid object § Calm, confident, centered, non-reactive, focused, empathetic, allow the connection/attachment to take place. Some patients will require time and a prolonged testing process to connect. How long depends, in part, on you § Avoid responding emotionally to provocation – it’s not personal – it’s just a test § Appeal to the healthy components of the patient’s personality in order to form an alliance § What you say is not as important as how you say (or act) it § Look for a hurt or disappointment under a top (and much more visible) layer of anger § Continuously assess the effectiveness of your approach based on the actual effect it has on the patient’s tension level § If being quiet or ignoring the patient accelerates their tension level, become more proactive § Conversely, if being too involved or talkative is increasing tension, assume a less active or intrusive posture. It is just as possible to try too hard as it is to try too little § The higher the patient falls on the T/TRC, external controls become more critical
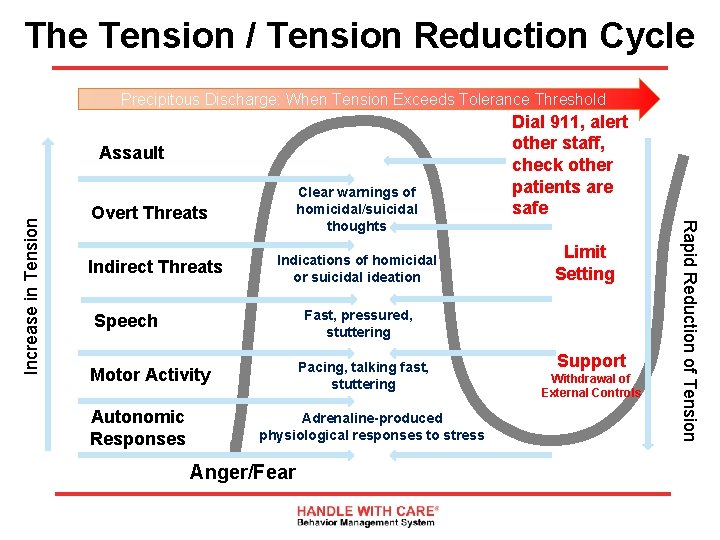
The Tension / Tension Reduction Cycle Precipitous Discharge: When Tension Exceeds Tolerance Threshold Clear warnings of homicidal/suicidal thoughts Overt Threats Indirect Threats Indications of homicidal or suicidal ideation Fast, pressured, stuttering Speech Pacing, talking fast, stuttering Motor Activity Autonomic Responses Limit Setting Adrenaline-produced physiological responses to stress Anger/Fear Support Withdrawal of External Controls Rapid Reduction of Tension Increase in Tension Assault Dial 911, alert other staff, check other patients are safe
Levels of Intervention Three Levels of Intervention 1. 2. 3. Support Limit Setting External level of intervention (calling 911)
Level 1: Support Help the patient articulate feelings and channel his/her tensions towards appropriate behavior § Listen: Allow ventilation without becoming judgmental § Accept: Consider the validity of the feeling if not the behavior It is impossible to tell another person how to feel § Focus: Focus on one issue at a time § Encourage: Assertion (as opposed to aggression) § Offer: Alternative choices the patient can make; contrasted by the inappropriate choices with their attending consequences § Contract: Persuade the individual to agree on the course of action to be taken § Redirect
Level 2: Limit Setting Limit setting is a more difficult skill to acquire because it deals with laying down concrete parameters. The tension levels are higher, the stakes (risks) are higher, and your own tension levels are (potentially) higher when defiance and challenging behaviors are manifested Always offer support simultaneously with limits Shame-oriented punitive interventions, retaliation and public humiliation do not constitute limit setting
Level 2: Limit Setting Effective limit setting has three main elements Limits must be CLEAR § Intellectually clear, i. e. presented in an understandable manner § Affectively (or emotionally) clear, i. e. , without fear, anger or hostility – Affect Neutral
Level 2: Limit Setting Limits must be CONSISTENT § Limits must be consistent from staff to staff and from day to day § Limits should not be set according to the mood of the staff § In team situations with more than 1 staff person – only 1 person should talk
Level 2: Limit Setting Limits must be ENFORCEABLE § Positive and negative consequences; privileges to change or modify behavior must be consistently, fairly and conscientiously applied § The goal is absolute programmatic predictability § Remember, confront the behavior, not the person; avoid touch at this level
Level 3: External Intervention § Physical intervention by staff is never appropriate in a Clean. Slate Center clinic § Support and Limit setting do not stop while you are waiting for 911 § Once staff has called 911, they should alert other staff by pushing little green button, and other staff should attempt to assist in continued efforts to de-escalate, and assist in making sure other patients are safe
Role Plays Support role plays 1. You approach a patient who is showing signs of agitation (pacing). He is avoiding eye contact, and in the past has required eternal intervention when he is upset What do you do? 2. You are approached by a patient who tells you that he is going to punch out the Center Manager when he sees him. He states matter-of-factly What do you do? 3. A patient is refusing to participate in conversation with you and looks very depressed. He asks you to leave him alone What do you do?
Role Plays Limit setting role plays 1. Supportive interventions have failed and the individual announces that he is going to “trash the place” What do you do? 2. The individual is clearly unable or unwilling to discuss the matter with the Center Manager. His intention to follow through with his threat to punch the Center Manager’s is clear. The Center Manager is due in any minute What do you do? 3. The individual continues to rant and rave – you determine that he is not de-escalating What do you do? 4. The depressed individual suggests that there are plenty of sharp objects around and he knew a kid who cut himself What do you do?
Positive Interventions Policy Place our policy here
Thank you for participating. © 1984, 2012, 2016. Handle With Care Behavior Management System, Inc. All rights reserved.
- Slides: 44